Abstract
Ankle arthritis is a common condition. It causes a significant socioeconomic burden, and is associated with significant morbidity. Patients with ankle arthritis are either elderly with significant co-morbidities, or young adults who have previously suffered with ankle injuries, resulting in post-traumatic arthritis. There is a wide variation in the management of these patients with ankle arthritis. We therefore present an overview of the current evidence based management of patients with symptomatic ankle arthritis.
Keywords: Ankle arthritis, Replacement, Arthroscopy, Osteotomy, Arthroplasty, Arthrodesis, Tibiotalar joint
1. Introduction
Ankle arthritis causes a substantial socioeconomic burden to society, with an estimated 29,000 patients being referred to foot and ankle specialist clinics yearly in the United Kingdom alone.1,2 This, however, is significantly lower than the incidence of hip or knee arthritis due to a combination of biomechanical and anatomical factors which protect the ankle joint from developing primary degenerative arthritis. Biomechanically, the ankle movement involves mainly rolling, whereas the knee moves with a combination of rolling, gliding and rotating motions. The higher range of motion of the knee predisposes it to developing primary osteoarthritis, whereas the ankle remains relatively protected.3 Anatomically, studies suggest that even though the ankle joint has thinner cartilage compared to that of the hip or knee, the cartilage is more uniform, stiffer and resistant to indentation. It does not produce matrix metalloproteinase 8 (MMP8) mRNA, an enzyme which is expressed by normal knee cartilage and which causes cartilage degradation. Additionally, ankle cartilage is less sensitive to the effects of cytokines that have been implicated in the development of primary osteoarthritis.4 On the other hand, ankle fractures and/or chronic instability of the ankle joint, results in disruption of the ankle cartilage with altered joint biomechanics, leading to the development of post - traumatic arthritis.
Epidemiological and cadaveric studies suggest that up to 1 in 10 patients over the age of 65, suffer from some degree of ankle arthritis.3 Despite the relatively high incidence, there is still a wide variation in the management of such patients, especially with regards to the surgical procedure offered. We therefore present an overview of the current evidence – based management of patients with symptomatic ankle arthritis.
2. Clinical presentation
Patients with ankle arthritis usually present with pain around the ankle joint that is worse with movements, often causing them to discontinue sports. In the later stages of the disease, they then develop nocturnal inflammatory pain, which may be associated with symptoms of ankle instability, locking and stiffness. Patients generally tend to seek medical help when their symptoms start affecting their ability to walk or work, especially if they are manual labourers.
History taking is key in such patients, as it not only helps us in understanding the impact of the symptoms on their quality of life, but also what the diagnosis is and where the pathology might lie. For example, patients who present with ankle pain that is worse on adopting a specific position such as the “ski-pose”, or whilst ascending stairs may be suffering from anterior bony spurs or osteophytes [Fig. 1].
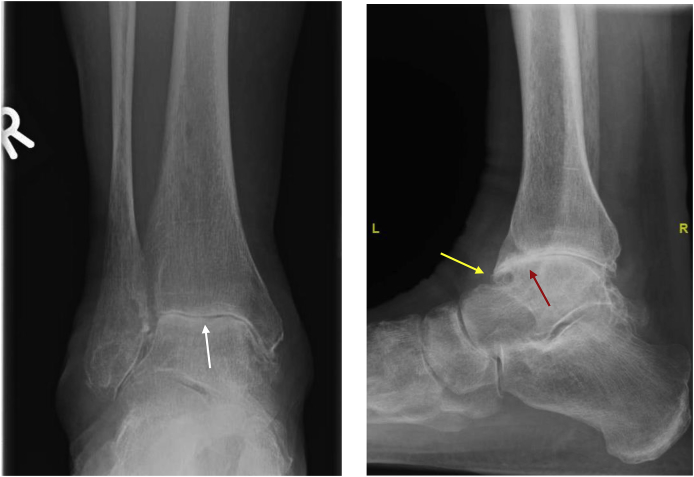
Fig. 1.
Anteroposterior (AP) and lateral radiographs of an ankle joint indicating severe ankle arthritis with a large anterior osteophyte (white arrow).
As mentioned above, primary degenerative arthritis in the ankle joint is less common compared to post-traumatic ankle arthritis. It is therefore imperative to ascertain whether there is a history of an ankle injury, recurrent sprains or previous surgical intervention. Moreover, establishing the level of disability a patient has due to his/her symptoms by enquiring about their dependency on analgesics, walking aid use and assessing their expectations from surgery are important factors in determining initial management priorities.
Significant co-morbidities can have an impact on both, the patient’s symptoms as well as their surgical management. Patients with haemophilia often present with episodes of recurrent atraumatic ankle swelling and warmth, which is generally indicative of synovial bleeds, whilst patients with rheumatoid arthritis complain of increased pain and disability with poor response to anti-inflammatory medication. Lastly, patients with poorly controlled diabetes may have associated peripheral neuropathy and be at a higher risk of wound related complications.5 These patients therefore require a multi-disciplinary approach when it comes to the management of their ankle arthritis.
The first “corridor – encounter”, when a patient walks from the waiting room to the examination room, is often what helps in the diagnosis of ankle arthritis. The rocker phase in a patient’s ankle during the gait cycle can be disrupted providing a clue to the diagnosis. Patients may also use walking aids, surgical shoes with rocker-soles or ankle orthotics to help in mobilisation. Signs of primary osteoarthritis in the hands, such as Bouchards and Heberden’s nodes, are less likely to be observed with traumatic or degenerative arthritis of the ankle. However, patients with inflammatory joint disease may have hand deformities in addition to ankle arthritis.
Clinical examination should include not only an assessment of ankle and hindfoot motion, but also of the entire lower limb to look for knee deformities secondary to arthritis or other causes such as previous tibial fracture mal-union. Proximal mal-alignment invariably requires correction prior to performing surgery for ankle arthritis. It is also important to perform a full neurovascular examination of the lower limb to ensure that patients do not have undiagnosed peripheral vascular disease or neuropathy, which may have a significant impact on the outcomes of surgery.
3. Investigations
Weight bearing ankle mortise and lateral plain radiographs form the mainstay of investigation for ankle arthritis. They may demonstrate signs of osteoarthritis which include joint space narrowing, marginal osteophytes, subchondral cysts and sclerosis [Fig. 2]. Comparative views of the contralateral normal or less affected ankle may be helpful in quantifying the reduced joint space, although this is less commonly used. Magnetic resonance imaging (MRI) tends to be more useful when a discrete osteochondral lesion is suspected to be the underlying cause of pain [Fig. 3], or when plain standing radiographs demonstrate mild ankle arthritis which is not in keeping with the patient’s symptoms.
Fig. 2.
Anteroposterior (AP) and lateral radiographs of an ankle joint indicating severe ankle arthritis with reduced joint space (white arrow), anterior osteophytes (yellow arrow) and sclerosis (red arrow).
Fig. 3.
MRI coronal view of an ankle showing an osteochondral defect (red arrow).
Another imaging modality that is becoming increasingly popular is the standing computed tomography (CT). It combines the benefits of plain radiographs and MRI scanning, and allows simultaneous, comparative imaging of both ankles. Using this, clinicians can obtain a detailed assessment of the state of the ankle and subtalar joints, as well as appreciate deformities of the joints in three dimensions, thereby being able to plan adjunctive procedures, such as a calcaneal osteotomy, which may be required in addition to surgery on the ankle.
4. Classification
The Takakura classification (Table 1) divides ankle arthritis into 5 categories based on ankle mortise plain radiograph findings. It is particularly useful when monitoring the progression of arthritis, but fails to guide surgical management. It also does not account for the state of the surrounding joints, contractures of the Achilles tendon or other deformities.6
Table 1.
The Takakura classification of ankle arthritis.
| Stage | Radiographic findings |
|---|---|
| I | Osteophytes and early sclerosis. No joint space narrowing. |
| II | Narrowed medial joint space. No subchondral contact. |
| IIIa | No remaining medial joint space. |
| IIIb | Subchondral bone contact over talar dome. |
| IV | Obliteration of joint space with complete bone contact |
The Canadian Orthopaedic Foot and Ankle Society (COFAS) classification system [Table 2] on the other hand divides ankle arthritis into 4 categories, taking into account clinical and radiological findings of not only the ankle joint, but also of adjacent joints and Achilles tendon tightness. Therefore, this classification system tends to be more commonly used in clinical practice, and has also been shown to have acceptable intra- and interobserver reliability.7
Table 2.
The COFAS classification of ankle arthritis.
| Type | Description |
|---|---|
| 1 | Isolated ankle arthritis |
| 2 | Ankle arthritis, with intra-articular varus or valgus deformity and/or a tight achilles |
| 3 | Ankle arthritis with hindfoot deformity, tibial malunion, midfoot abduction or adduction, supinated midfoot and a plantarflexed 1st ray |
| 4 | Types 1–3 plus subtalar, calcaneocuboid or talonavicular arthritis |
5. Non – operative management of ankle arthritis
This mainly includes strategies to limit weight bearing forces through the ankle joint including activity modification, weight reduction, use of walking aids and discontinuation of impact sports, instead focusing on non – weight bearing exercises such as swimming and cycling. Patients may also benefit from ankle braces or boots, and from shoe outsole modifications to a rocker – sole, which result in limiting ankle joint motion.8 In addition, a trial of physiotherapy, analgesics and anti-inflammatory medication should be offered prior to any surgical intervention.
6. Intra-articular joint injections
The National Institute for Health and Care Excellence (NICE)9 recommends intra-articular corticosteroid injections (methylprednisolone acetate or triamcinolone hexacetonide), as a first line treatment for patients with moderate to severe ankle arthritis, as studies have shown a short term benefit (usually weeks) in terms of pain relief, when compared with placebos [Fig. 4]. This is due to the anti-inflammatory effect of corticosteroids which is thought to reduce joint synovitis, and thus have an impact on arthritis related pain.10 Intra-articular corticosteroid injections can also be used as a differential test in situations where the source of pain is doubtful because of the presence of coexisting conditions, such as both ankle and hindfoot arthritis, helping to confirm or refute the diagnosis. They may also be useful in cases where invasive surgery is contraindicated due to a patient’s comorbidities.
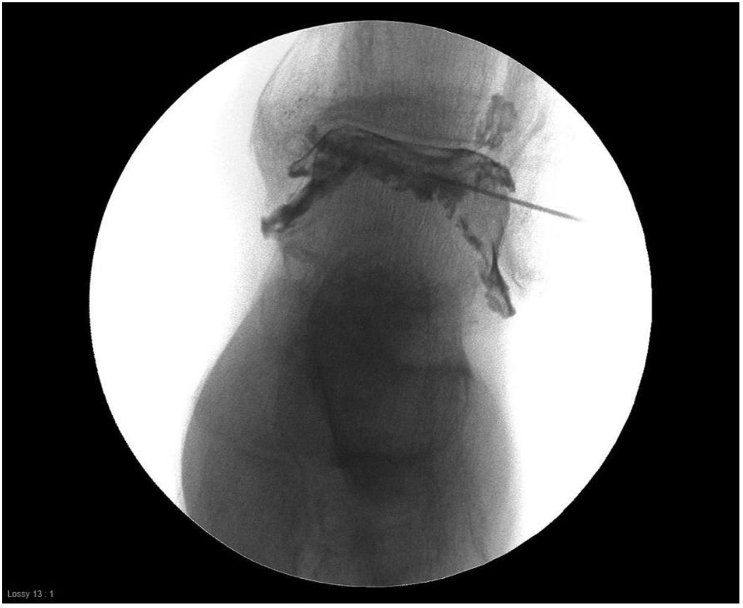
Fig. 4.
Fluoroscopy guided left ankle corticosteroid injection.
Risks associated with intra-articular corticosteroid injections are small, and include infection, transient increase in pain and local fat atrophy which may result in a cosmetic defect, and a risk of cartilage loss following repeated multiple injections, although the evidence supporting this is controversial.11
Intra-articular hyaluronic acid (HA) injections have also been used, as HA is thought to help with synovial lubrication, and the production of it is greatly reduced in arthritic joints. However, NICE does not recommend it, as the studies demonstrating the benefits of HA injections when compared with placebos were small, poor quality studies,12 and trials comparing intra-articular HA injections with oral anti-inflammatories did not find a statistically significant difference in symptom relief.13
Patients whose symptoms are refractory to non-operative treatment options, should be considered for surgical management of their ankle arthritis.
7. Ankle arthroscopy
The role of arthroscopic ankle debridement [Fig. 5] is limited to where there is a defined, localised surgical target such as anterior osteophytes causing anterior impingement, loose bodies or discrete osteochondral lesions.
Fig. 5.
Photograph showing the standard intra-operative set up for an ankle arthroscopy.
A prospective study by van Dijk CN et al.14 demonstrated good outcomes for arthroscopic ankle debridement of anterior soft tissue and bone spurs in patients with mild ankle osteoarthritis and anterior impingement, but not for diffuse arthritis. Moreover, arthroscopic ankle debridement with removal of loose bodies and microfracture for localized chondral defects has also produced good clinical results in soccer players with moderate arthritic changes in the ankle.15
Another prospective study by Tol JL et al.16 found that over 75% of patients with grade I arthritic changes and 53% of patients with grade II changes were satisfied following arthroscopic ankle debridement. However, reformation of osteophytes and narrowing of joint space was seen in a large number of patients (66% and 47% respectively) at the long term follow up. Conversely, Amendola A et al.17 have reported improvement with ankle arthroscopy and debridement in only 2 out of 11 patients with ankle arthritis, compared with clinical improvement in 80% of patients with anterior bony impingement alone.
The available evidence therefore supports the use of arthroscopic ankle joint debridement for patients with anterior bony impingement with early arthritis, and not for patients with moderate to advanced ankle arthritis.
8. Periarticular osteotomy
The aim of a realignment osteotomy in ankle arthritis is to increase the surface contact across the ankle, and in turn decrease the load per unit area. It also increases the stability of the ankle, thereby improving joint biomechanics and alleviating patients’ symptoms. This procedure potentially may defer the need for a total ankle arthroplasty or arthrodesis, and is therefore an attractive surgical option in young, active patients. Moreover, with restoration of ankle alignment, the longevity of a subsequent ankle arthroplasty is likely to be improved.
Realignment procedures performed at or above the ankle include plafond-plasty (an intra-articular opening wedge osteotomy of the distal medial tibia), mortise-plasty, and distal tibial oblique osteotomy (DTOO), where the centre of correction is at the level of the syndesmosis. More proximal osteotomies such as supra-malleolar osteotomy [Fig. 7a and b] and high tibial osteotomy performed for the varus knee can also restore alignment at the ankle joint. In the selection of the most appropriate osteotomy, standing long-leg alignment radiographs from the hips to the ankles are helpful in judging the origin of the deformity and its effect on the mechanical axis of the limb.
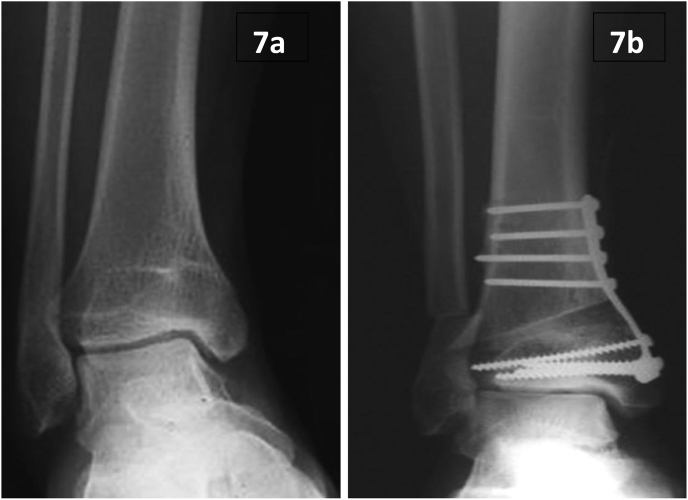
Fig. 7.
a and b – AP plain radiographs of an ankle joint pre- and post-operatively following a supramalleolar osteotomy. The patient had a varus ankle joint alignment with medial ankle joint arthritis (Images reproduced from Takakura Y et al. Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients. J Bone Joint Surg Br. 1995; 77: 50–54.18).
Corrective osteotomies below the ankle, such as on the calcaneum for hindfoot varus or valgus, and on the medial column of the foot for correction of cavovarus or planovalgus deformities, are often combined with ankle replacement or arthrodesis in order to achieve a plantigrade, stable foot with optimal walking biomechanics. Standing CT scanning can be utilised to analyse multiplanar deformities and to help anticipate the requirement for performing adjunctive osteotomies in patients undergoing ankle replacement or fusion.
A study of 294 patients by Krähenbühl N et al.,19 who underwent supra-malleolar osteotomy for Takakura grade 1 to 3a ankle arthritis showed an average improvement in the American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scores from 53.2 pre-operatively to 72.7 postoperatively. At a mean follow-up of 5 years, the overall survival of the native joint was 88%, with only 12% requiring further surgery in the form of total ankle replacement or ankle arthrodesis.
Even with advanced ankle arthritis, it seems that there are potential benefits in performing an ankle osteotomy. Termoto T et al.20 demonstrated good outcomes with distal tibial oblique osteotomy (DTOO) in patients with ankle varus deformity, provided there was at least 10° of motion remaining in the arthritic joint. Mann HA et al.21 reported good outcomes in 15 out of 19 patients with lateral ankle instability and medial-sided ankle arthritis, who were treated with lateral ligament reconstruction and plafond-plasty.
Periarticular osteotomy is therefore a viable option in the young active patient with ankle arthritis, periarticular deformity and/or instability. In this patient group, it is preferable to preserve the ankle joint provided there is good residual ankle movement. In these cases, it is beneficial to pre-operatively image the ankle using MRI to thoroughly examine residual cartilage in addition to a standing CT when the deformity is close to the ankle, or long-leg alignment radiographs when the deformity is more proximal.
9. Ankle distraction arthroplasty
Distraction arthroplasty [Fig. 8] aims to unload the ankle joint by allowing articular cartilage to undergo a reparative process. It is commonly used for the treatment of early ankle arthritis in younger patients, where there is good residual joint motion. A spanning external fixator is applied across the ankle joint in either a hinged or a static mode, aiming to distract the ankle by 5–10 mm. Adjunctive procedures such as Achilles tendon lengthening, arthroscopic debridement, and correction of malalignment of the limb may also be carried out in the same setting as the distraction arthroplasty.22
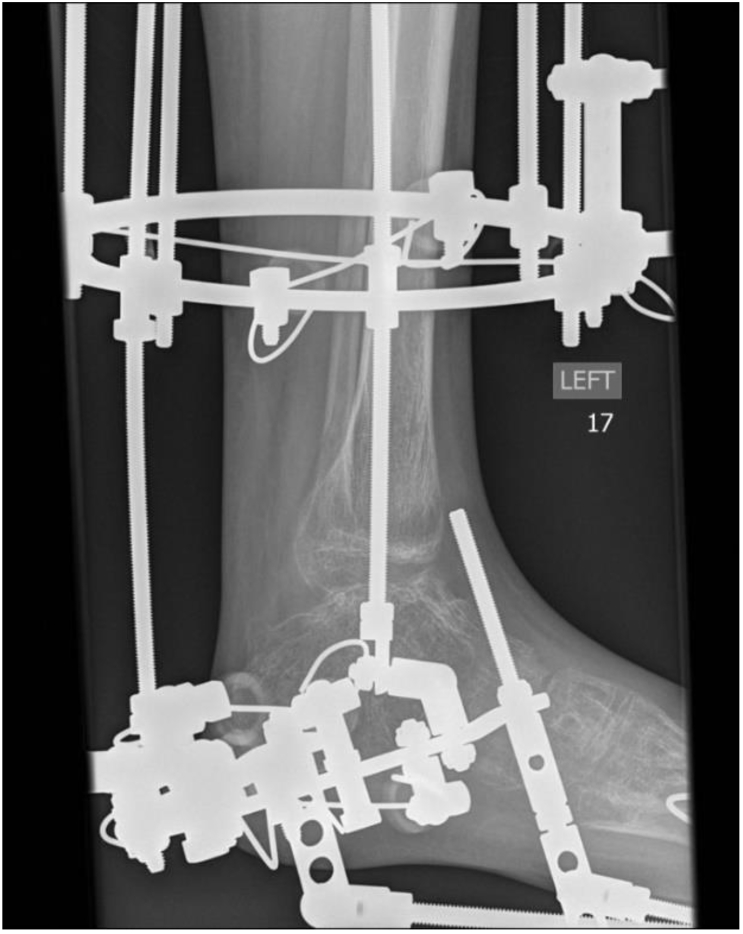
Fig. 8.
A lateral plain radiograph of a left ankle showing an Ilizarov frame assisted distraction ankle arthroplasty.
In a midterm follow-up study of thirty-six patients who underwent distraction arthroplasty of the ankle with a mean follow up of 8.3 years, Amendola A et al.23 found that 55% of patients did not require further surgery, as opposed to 45% who required revision surgery in the form of either an ankle arthrodesis or a total ankle arthroplasty. In this study, higher ankle scores at two years post-operatively, and older age at the time of the distraction arthroplasty were positive predictors of ankle survival. Marijnissen ACA et al.24 have shown similar re-operation rates in patients undergoing distraction arthroplasty.
Though distraction arthroplasty may offer young patients several years of retaining their native ankle joint, a significant proportion require joint-sacrificing procedures in the mid-term. Frame-wear can be onerous for young patients, and they often need intensive counselling about the prolonged use of the distraction device and the inevitable need for more definitive surgery in the future. Currently, there is no high quality evidence to make a recommendation for or against its use in ankle osteoarthritis.
10. Ankle arthrodesis
Arthrodesis is the gold standard surgical treatment option for a painful, stiff, deformed or unstable ankle in patients with end-stage arthritis, where loss of motion is unlikely to compromise overall function.25 The goal of arthrodesis is to eliminate pain, correct the underlying deformity and obtain a plantigrade, stable foot. When meticulous surgical technique is employed in appropriately selected patients, ankle arthrodesis is a reliable procedure to treat ankle arthritis with union rates ranging from 85 to 100%.26
The desired position for an ankle after arthrodesis is neutral flexion and extension, 5° of external rotation, 5° of valgus, and a slight posterior translation of the talus under the tibia. Leg length discrepancy should be less than 2.5 cm. Suboptimal position outside of these values can lead to disadvantageous biomechanics. For example, anterior translation of the talus under the tibia can lead to a vaulting type gait pattern by reducing the lever arm of the gastro-soleus complex. A posteriorly translated talus in external rotation provides the theoretical advantage of improving push off due to the pronation mechanism occurring normally.27 Fusion of the ankle in a plantarflexed position must be avoided at all costs as it will lead to a back-kneeing gait and potential worsening of symptoms.
10.1. Arthroscopic versus open ankle fusion
Although traditionally, ankle arthrodesis is done through an open approach, arthroscopic fusion has gained popularity in the last decade with potential advantages of a shorter hospital stay, reduced time to fusion and less blood loss. In a multicentric case series comparing open versus arthroscopic ankle arthrodesis, Townshend D et al.28 reported shorter hospital stay and significant improvement in the Ankle Osteoarthritis Scale Score in the arthroscopic group at 2 years. There was no difference in radiographic alignment, complications and surgical time between the 2 groups. Many authors recommend the arthroscopic technique only when the deformity is less than 15° due to difficulty in achieving adequate correction in a severe deformity.29 However Dannawi Z et al.30 showed high union rates (88%) and low complication rates with arthroscopic ankle arthrodesis in patients with ankle deformities greater than 15°, with good to excellent results using the Mazur ankle grading system. Schmid T et al.31 also demonstrated that clinical and radiological outcomes following arthroscopic ankle arthrodesis are not dependent on the degree of preoperative ankle deformity.
10.2. Indications and contraindications for ankle arthrodesis
Ankle fusion can be considered for patients with ankle arthritis of various aetiologies, who have limitation of motion and chronic pain that is not amenable to non-operative treatment. It is considered the treatment of choice for young patients with end stage arthritis, and for those patients who engage in high activity levels such as manual labourers.32 Contraindications to ankle arthrodesis include vascular impairment of the limb, poor soft tissues and untreated infection.
10.3. Ankle arthrodesis and gait
A potentially obvious drawback of an ankle arthrodesis is that it leads to an altered gait pattern when compared with a normal, disease free ankle joint. However, when compared with the pre-operative gait in an arthritic ankle, temporal and spatial data demonstrate that it results in an increase in step length and velocity, along with a diminished total support time on the unaffected leg. Pre- and post-operative gait analysis also demonstrates improvement in other kinematic and kinetic parameters.33
Moreover, several biomechanical factors inherent in the ankle joint make it particularly suitable for an arthrodesis. During normal gait, only 10–12° of ankle dorsiflexion and 20° of ankle plantarflexion is required, so loss of motion following an arthrodesis can be accommodated for, without significant compromise, by the mobility of the transverse tarsal joint.34 Despite this, a rocker-sole shoe may be occasionally required.
10.4. Arthroscopic ankle arthrodesis
This is most often performed through anteromedial and anterolateral portals [as shown in Fig. 5]; however, it is perfectly feasible to prepare the ankle joint through a posterior arthroscopic portal. Arthroscopic fusion [Fig. 9, Fig. 10] offers shorter inpatient hospital stays and earlier post-operative rehabilitation, with fusion rates comparable with that of open arthrodesis.35 Additional advantages of an arthroscopic technique include potentially reducing complications associated with wound healing, especially when the soft tissue has been compromised due to previous trauma or surgery. It is therefore the preferred technique for patients who are at a high risk of developing a postoperative infection, secondary to a systemic issue such as Diabetes Mellitus, or because they are on long term immunosuppressants. Contraindications for an arthroscopic fusion include a significant, irreducible deformity, significant bone loss, previous attempts at arthrodesis, or broad-based avascular necrosis of the talus which requires bone grafting.
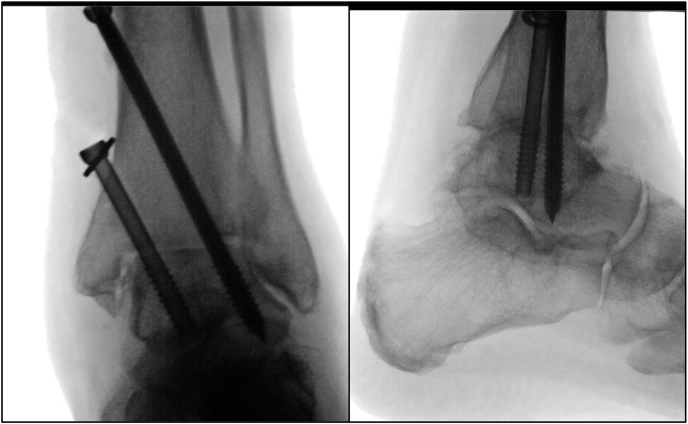
Fig. 9.
Intra-operative fluoroscopy images showing AP and lateral views of an ankle joint after an arthroscopic arthrodesis.
Fig. 10.
AP and plain ankle radiographs of the same patient, taken approximately 6 months after surgery, demonstrating complete bony fusion.
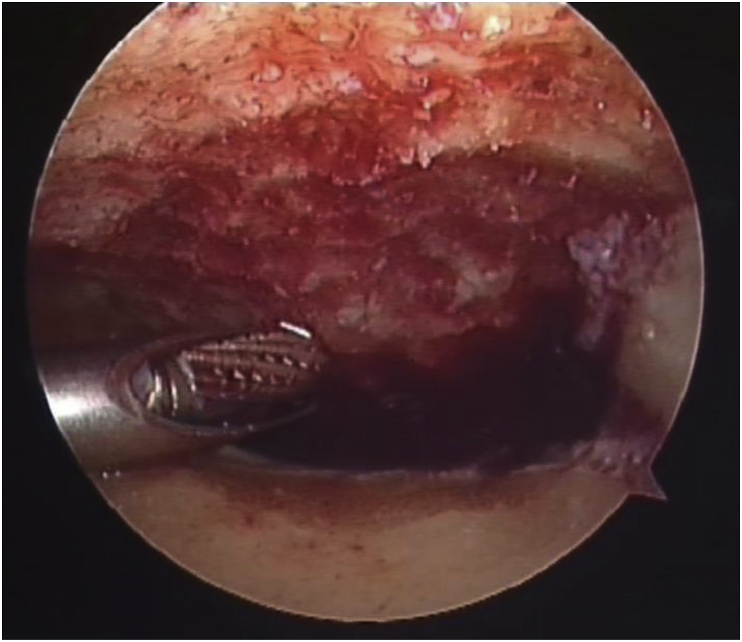
Following adequate removal of residual articular cartilage and decortication to bleeding cancellous bone [Fig. 6], optimal positioning of the ankle joint is carried out, and fixation secured using two or three cannulated, partially-threaded 6.5 mm diameter cancellous screws. Screw direction should ideally be from posteromedial in the tibia to distal anterolateral or anteromedial/central in the talus. The screw directed anterocentrally/medially in the talus should aim to pull the talar neck up towards the tibia to obtain a plantigrade position. Screws should be countersunk and threads should all cross the ankle joint to ensure adequate compression. Compression occurs predominantly across the medial gutter and it is therefore not necessary to prepare the lateral gutter, with studies confirming that non-union of the lateral gutter does not affect the clinical outcome of fusion.29
Fig. 6.
Intra-operative image taken during an ankle arthroscopy illustrating bleeding subchondral bone.
Additionally, some adjunctive procedures may be required at the time of the arthroscopic ankle arthrodesis in order to achieve an optimal outcome. Traditionally, the degree of coronal plane deformity that can feasibly be corrected with arthroscopic fusion is up to 15°. However, some studies report adequate correction up to 25° of deformity.29 If there is still some minor residual coronal plane deformity following arthrodesis, it can usually be addressed by performing a calcaneal osteotomy. Achilles tendon lengthening is also commonly performed as an adjunct, for correction of ankle equinus, and to achieve the desired sagittal plane correction before arthrodesis.29
10.5. Open ankle arthrodesis
Post-traumatic ankle arthritis is frequently associated with significant deformity, large bone defects, and avascular necrosis of the talus that is likely to require bone grafting. These situations are more amenable to treatment with open arthrodesis. Other indications for an open surgical approach include the need to remove implants from previous fracture fixation surgeries or when converting from a total ankle arthroplasty.
Open arthrodesis can be undertaken through several approaches including the commonly used anterior approach, which is between the tendons of extensor hallucis longus and extensor digitorum longus, or through two mini-incisions using extensions of the anteromedial and anterolateral arthroscopic portals. The lateral trans-fibular approach with partial or total sacrifice of the lateral malleolus is generally performed to accommodate more robust implants such as lateral plates. A sagittal osteotomy of the distal fibula can also be used, with fixation of the lateral part onto the ankle fusion site, providing a “live” onlay graft. The trans-fibular approach is particularly useful for correcting severe deformity and when preparation of the subtalar joint is desired for a tibio-talo-calcaneal fusion. The excised part of the fibula is an ideal cortico-cancellous graft to fill any bone defects. The trans-Achilles posterior approach is also useful for tibio-talo-calcaneal fusion with posterior plate fixation and is used when anterior soft tissue compromise is evident.
10.6. Complications following ankle arthrodesis
Aside from the general complications of wound infection and delayed wound healing, the most feared complication of ankle arthrodesis is non-union. Enhancing patient biological factors pre-operatively to reduce this risk is therefore essential. This can be done by identifying and started treatment for undiagnosed type 2 diabetes, particularly in obese patients, using fasting blood glucose analysis and serum glycosylated haemoglobin, and ensuring complete smoking cessation.36 Soft tissue status, compromised limb vascularity, osteonecrosis, and stability of fixation, all have a significant bearing on union rates.37 Chalayon O et al.38 reported a 9% non-union rate at 6 months in a study of 440 patients with uncomplicated, primary open ankle arthrodesis. They found that patients with a previous subtalar arthrodesis were 3 times more likely to have a non-union, probably due to the negative effect of a greater lever arm on the ankle joint and partial disruption of the blood supply to the talus following a subtalar fusion. Moreover, patients with a varus ankle mal-alignment were twice as likely to develop a non-union, which the authors attributed was due to the stretching of the nutrient vessel that enters the medial side of the talus.
Paying attention to post-operative analgesic regimes in patients is also important in an effort to reducing the rates of non-union following ankle arthrodesis. Patients should be counselled pre-operatively about the need to avoid Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) which can have a significant deleterious effect on bone healing.39 Additionally, correction of a Vitamin D deficiency is advocated due to its increased prevalence in patients with a non-union following ankle fusion.40
The stiffening of the ankle joint undoubtedly imparts additional weight-bearing stress onto adjacent joints during normal gait, particularly the subtalar joint. Adjacent joint arthritis is usually noted in the majority of patients pre-operatively, although patients may be asymptomatic. Prospective ankle fusion patients therefore need to be counselled about the presence of adjacent joint arthritis, and the potential need for future surgical procedures on the diseased adjacent joints.
11. Total ankle replacement
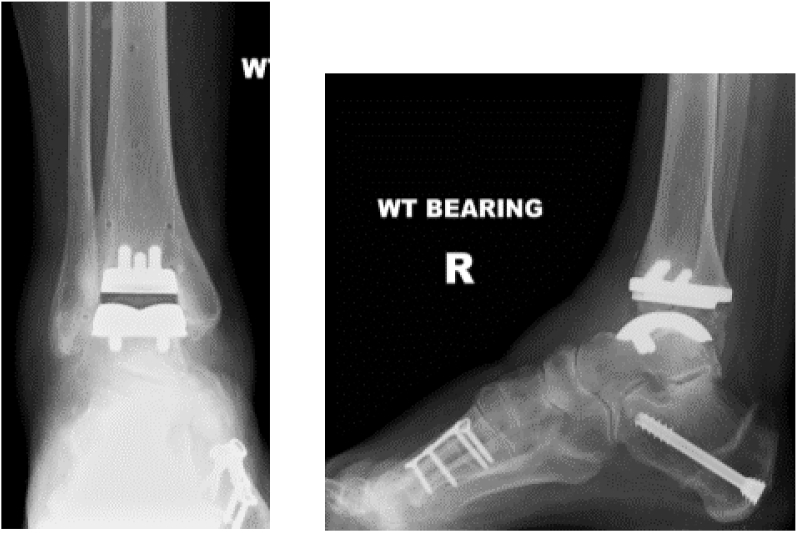
With an ever improving prosthesis design, instrumentation, and understanding of surgical techniques, total ankle replacement [Fig. 11] has been shown to result in successful functional outcomes and maintenance of limb biomechanics.
Fig. 11.
AP and lateral plain radiographs demonstrating a fixed-bearing total ankle replacement in situ, along with a simultaneous correction of hindfoot varus using a minimally invasive calcaneal osteotomy, and a first metatarsal dorsiflexion osteotomy.
11.1. Prosthesis design
Since the inception of ankle replacements in the 1970s, various systems have been developed. First generation designs were constrained and stable, but needed significant bone resection and were cemented. They failed in significant numbers due to loosening, subsidence and extensive osteolysis. Second generation implants were mostly uncemented and less constrained, however they too had significant failure rates due to increased polyethylene wear. Modern, third generation implants have a semi-constrained design and use ultra-high molecular weight polyethylene as a bearing surface. They are either a two part, fixed-bearing prosthesis, with the polyethylene component rigidly fixed to the tibial component, or a three-part, mobile-bearing prosthesis, where the polyethylene has some mobility underneath the tibia.
Mobile-bearing prostheses are most commonly used in Europe, while the majority of implants used in the United States of America (USA) are fixed-bearing cemented designs. The STAR (Scandinavian Total Ankle Replacement) prosthesis is the only non-fixed-bearing ankle replacement approved for use by the Food and Drug Administration (FDA) for non-cemented use in the USA. Currently there is no consensus as to the superiority of one implant type over the other. There seems to be little difference in clinical outcomes between the 2 groups, although talar cyst formation with potential component subsidence remains a concern with mobile-bearing designs.41 Moreover, according to the United Kingdom (UK) National Joint Registry (NJR),42 only 5% of implants are either fully or partially-cemented.
What is probably more important for modern, third generation implant survival is the accuracy of implantation and reproducibility of the operative technique. Increasingly, implant instrumentation is being refined, often incorporating extramedullary alignment jigs, along with the use of intra-operative fluoroscopy. Use of pre-operative CT planning and patient-specific instrumentation has evolved to further reduce operative time and fluoroscopic exposure without compromising on implant position.43
11.2. Indications and contraindications
The ideal patient for an ankle replacement is one who is fifty years of age or older, has a Body Mass Index (BMI) of less than 30, undertakes low demand physical activity, and who has a manageable deformity.44 Pre-existing ipsilateral hindfoot, hip or knee arthritis, may make total ankle arthroplasty more desirable than ankle fusion in certain patient groups. Patient contraindications to total ankle arthroplasty include relative youth, heavy manual workers, heavy smokers, diabetics (especially those with peripheral neuropathy), vascular insufficiency, severe ankle instability, significant bone loss and active local/systemic infection.45
11.3. Deformity evaluation
Weight bearing CT scanning and, where necessary, long-leg alignment radiographs are commonly used in the pre-operative planning of ankle arthroplasty. Minor intra-articular deformities of the ankle can be corrected by judicious soft tissue release and adequate symmetrical component tensioning across the joint.46 More significant coronal intra-articular deformity (up to 15°), with asymmetrical bone loss, can be corrected by removing adequate bone on either side of the joint. However, if major hind-, mid- or forefoot re-alignment is needed, it may be necessary to perform this as a separate procedure before the arthroplasty is carried out. With experience though, simultaneous hindfoot arthrodesis or corrective osteotomy may also be completed along with a total ankle replacement in the same sitting.47
Commonly, after trial component implantation, it becomes necessary to undertake a percutaneous Achilles lengthening to obtain adequate ankle dorsiflexion. In addition, any residual minor hindfoot varus or valgus can be addressed with a calcaneal osteotomy.
If there is a varus deformity of the hindfoot, it is important to remember that its origin maybe secondary to a plantarflexed first ray. In such a case, a dorsal closing-wedge osteotomy through the medial column must be performed in order to protect the ankle replacement from asymmetrical loading. Often, it is necessary to perform both hindfoot and forefoot osteotomies to achieve a plantigrade foot. Rarely is it necessary to address extra-articular varus or valgus deformity above the ankle joint with a supramalleolar osteotomy, plafondplasty and medial or lateral ligament reconstruction.
It is important to recognise with ankle arthroplasty surgery that implantation of the ankle replacement is only one step in a critical sequence. It is crucial to correct the underlying bony deformity and ligament insufficiency, to obtain a balance of forces across the ankle.
11.4. Outcomes
Ankle replacement is gaining popularity amongst patients due to the main advantage of retaining ankle motion. In a study of 197 patients, the average one-year postoperative total sagittal-plane motion of the ankle and foot, recorded with radiographic parameters, was 25.9°, with 68% arising from the ankle prosthesis and the remaining motion arising from the hindfoot.48 Indeed, in comparison to ankle fusion, ankle replacement offers increased average gait velocity by improving stride length and cadence.49
Studies into implant survival rates have shown acceptable longevity, including over 70% survivorship of STAR ankle replacements at an average of fifteen years.50,51 Hoffman KJ et al.52 reported 97% implant survival at a mean of 5.2 years with the fixed-bearing Salto-Talaris prosthesis.
In a comparative study of 321 patients (232 ankle replacements and 89 ankle arthrodesis procedures), with a mean follow up of 5.5 years, ankle arthrodesis patients had a re-operation rate of 7% compared to 17% in ankle arthroplasty patients. The rate of major complications was also higher in patients who had undergone arthroplasty (19%) compared with those who had had an arthrodesis (7%). However, patients in the ankle arthroplasty group reported better functional outcomes in terms of pain and disability scores.53 A systematic review by Haddad SL et al.54 demonstrated that the intermediate outcomes of ankle arthroplasty were similar to those of ankle arthrodesis, however high level evidence was lacking. Recently, a retrospective, cross-sectional cohort study, comparing the clinical outcomes of total ankle replacement, arthroscopic ankle arthrodesis and open ankle arthrodesis in patients with non-deformed, isolated, end stage ankle arthritis revealed comparable clinical outcomes. It also found that although the revision rates were similar for all three groups, the total ankle replacement group required significantly more additional surgical procedures.55
11.5. Complications
Complications reported with ankle arthroplasty include intra-operative and post-operative fractures, infection, wound healing problems, aseptic loosening and osteolysis, chronic pain, soft tissue injury (nerve or tendon), thromboembolism, complex regional pain syndrome and amputation.56
The incidence of medial malleolar fracture is approximately 9.7%, while that of lateral malleolus fracture is much less common (1.4%).43 Intra-operative fractures of the medial malleolus should be secured with screws whilst lateral malleolar fractures require a separate surgical approach to undertake plate and screw fixation. This is particularly important to avoid early implant subsidence and migration.57 Early post-operative fractures (within four months) are rare on the lateral side and can usually be treated with a boot or a cast, whereas medial malleolar fractures should most often undergo internal fixation. Late post-operative fractures of either malleoli are usually stress fractures and need fixation.
Wound healing complications account for 1–14% of all complications.43 Particular risk factors for this include diabetes mellitus, rheumatoid arthritis, immunosuppression, obesity, poor tissue handling and extensive use of self-retaining retractors. The reported rate of superficial infection ranges from 1 to 4%, however with superficial infection there is always concern about a subsequent prosthetic joint infection. The incidence of a deep periprosthetic infection is approximately 0.5%, and this usually necessitates implant removal with staged revision joint replacement, implantation of permanent antibiotic spacers, arthrodesis or a trans-tibial amputation.43,58
Regular follow-up and surveillance for the delayed complication of aseptic loosening is important. Reported incidence ranges from 3 to 19%. Particular risk factors for osteolysis and aseptic loosening include mal-alignment of the hindfoot, poor prosthesis alignment and polyethylene component incongruity.43 Management options commonly include conversion to ankle arthrodesis, although revision arthroplasty using modular stemmed components is gaining popularity. Hintermann B et al.59 looked at 117 revision arthroplasties that were carried out for a failed total ankle replacement. They reported an 83% survival rate at the 6 year follow up stage, where recurrent component loosening was taken as the end-point.
Table 3 summarises the management algorithm for ankle arthritis.
Table 3.
Management algorithm for ankle arthritis.
| Stage | Age | Condition of ankle joint | Surgical procedure |
|---|---|---|---|
| I | Any age | Impingement only | Arthroscopic debridement |
| II | Any age | Anatomy well preserved | Arthroscopic debridement |
| Malalignment at supra-articular level | Supramalleolar osteotomy | ||
| Malalignment of heel | Calcaneal osteotomy | ||
| III | Any age | Ankle anatomy distorted and not restorable/neurological conditions previous infection/severe osteoporosis | Arthrodesis |
| Age ≥ 55 | Normal or restored anatomy with no degenerative disease in adjacent joint | Arthrodesis or Total ankle arthroplasty | |
| Normal or restored anatomy with degenerative disease in adjacent joints | Total ankle arthroplasty |
12. Conclusion
Early stage ankle arthritis is initially treated with non-pharmacological methods like weight reduction, activity modification and assistive devices. Intra-articular steroids can be considered when these measures fail. Carefully selected patients with early arthritis of the ankle joint benefit from surgical interventions such arthroscopic debridement, periarticular osteotomy and distraction arthroplasty. Arthroscopic debridement is especially effective in treating anterior impingement pain, whilst re-alignment procedures help in cases where there are focal arthritic changes due to malalignment.
Ankle arthrodesis, open or arthroscopic, remains the gold standard treatment for advanced arthritis of the ankle. Current trends in the management of end-stage ankle arthritis are rapidly evolving. Though open ankle arthrodesis has traditionally been the surgical option of choice, recent evidence shows that arthroscopic arthrodesis is a reliable technique with reproducible results in patients.
Total ankle replacement is an established surgical option in advanced arthritis, and is gaining in popularity. Complications of ankle replacement surgery are more significant and frequent than ankle fusion, but are largely manageable. Advances in pre-operative planning software and instrumentation have improved reproducibility of surgical technique and accessibility. Patient selection is key, with total ankle replacements currently being offered to older patients with low physical demand and a smaller degree of deformity. The ongoing ‘TARVA’ trial,60 which is a multi-centre randomised control trial comparing cost effectiveness and clinical outcomes of total ankle replacement versus arthrodesis in end stage ankle arthritis, will hopefully provide comprehensive information on these two procedures.
Declaration of competing interest
The authors declare that there is no conflict of interest.
Contributor Information
V. Adukia, Email: vidhiadukia@gmail.com.
J. Mangwani, Email: jmangwani@hotmail.com.
R. Issac, Email: renjit.issac@uhl-tr.nhs.uk.
S. Hussain, Email: shakir_haider@yahoo.com.
L. Parker, Email: lee.parker@londonorthopaedic.com.
References
- 1.Goldberg A.J., MacGregor A., Dawson J., Singh D., Cullen N. The demand incidence of symptomatic ankle osteoarthritis presenting to foot and ankle surgeons in the United Kingdom. Foot. 2012;22(3):163–166. doi: 10.1016/j.foot.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Glazebrook M., Daniels T., Younger A., Foote C.J., Penner M. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008 Mar;90(3):499–505. doi: 10.2106/JBJS.F.01299. [DOI] [PubMed] [Google Scholar]
- 3.Thomas R.H., Daniels T.R. Ankle arthritis. J Bone Joint Am. 2003 May;85(5):923–936. doi: 10.2106/00004623-200305000-00026. [DOI] [PubMed] [Google Scholar]
- 4.Shepherd D.E., Seedhom B.B. Thickness of human articular cartilage in joints of the lower limb. Ann Rheum Dis. 1999 Jan;58(1):27–34. doi: 10.1136/ard.58.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lanzetti R.M., Lupariello D., Venditto T., Guzzini M., Ponzo A. The role of diabetes mellitus and BMI in the surgical treatment of ankle fractures. Diabetes Metab Res Rev. 2018 Feb;34(2) doi: 10.1002/dmrr.2954. [DOI] [PubMed] [Google Scholar]
- 6.Takakura Y., Aoki T., Sugimoto K. The treatment for osteoarthritis of the ankle joint. Jpn J Joint Dis. 1986;5:347–352. [Google Scholar]
- 7.Krause F.G., Di Silvestro M., Penner M.J., Wing K.J., Glazebrook M.A. Inter- and intraobserver reliability of the COFAS end-stage ankle arthritis classification system. Foot Ankle Int. 2010 Feb;31(2):103–108. doi: 10.3113/FAI.2010.0103. [DOI] [PubMed] [Google Scholar]
- 8.Huang Y.C., Harbst K., Kotajarvi B., Hansen D., Koff M.F. Effects of ankle – foot orthoses on ankle and foot kinematics in patients with ankle osteoarthritis. Arch Phys Med Rehabil. 2006 May;87(5):710–716. doi: 10.1016/j.apmr.2005.12.043. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence Osteoarthritis: care and management clinical guideline [CG177] 2014. https://www.nice.org.uk/guidance/cg177/chapter/1-Recommendations#pharmacological-management [PubMed]
- 10.Ostergaard M., Stoltenberg M., Gideon P., Sorensen K., Henriksen O., Lorenzen I. Changes in synovial membrane and joint effusion volumes after intraarticular methylprednisolone. J Rheumatol. 1996;23:1151–1161. [PubMed] [Google Scholar]
- 11.Juni P. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev. 2015 Oct;(10):CD005328. doi: 10.1002/14651858.CD005328.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bellamy N., Campbell J., Welch V., Gee T.L., Bourne R., Wells G.A. Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;(2):CD005321. doi: 10.1002/14651858.CD005321.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bannuru R.R., Vaysbrot E.E., Sullivan M.C., McAlindon T.E. Relative efficacy of hyaluronic acid in comparison with NSAIDs for knee osteoarthritis: a systematic review and meta-analysis. Semin Arthritis Rheum. 2014 Apr;43(5):593–599. doi: 10.1016/j.semarthrit.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Van Dijk C.N., Verhagen R.A., Tol J.L. Arthroscopy for problems after ankle fracture. J Bone Joint Surg Br. 1997 Mar;79(2):280–284. doi: 10.1302/0301-620x.79b2.7153. [DOI] [PubMed] [Google Scholar]
- 15.Osti L., Del Buono A., Maffulli N. Arthroscopic debridement of the ankle for mild to moderate osteoarthritis: a midterm follow-up study in former professional soccer players. J Orthop Surg Res. 2016 Mar;11:37. doi: 10.1186/s13018-016-0368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tol J.L., Verheyen C.P., van Dijk C.N. Arthroscopic treatment of anterior impingement in the ankle. J Bone Joint Surg Br. 2001 Jan;83(1):9–13. doi: 10.1302/0301-620x.83b1.10571. [DOI] [PubMed] [Google Scholar]
- 17.Amendola A., Petrik J., Webster-Bogaert S. Ankle arthroscopy: outcome in 79 consecutive patients. Arthroscopy. 1996;12:565–573. doi: 10.1016/s0749-8063(96)90196-6. [DOI] [PubMed] [Google Scholar]
- 18.Takakura Y., Tanaka Y., Kumai T., Tamai S. Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients. J Bone Joint Surg Br. 1995;77:50–54. [PubMed] [Google Scholar]
- 19.Krahenbuhl N., Zwicky L., Bolliger L., Schadelin S., Hintermann B. Mid to long – term results of supramalleolar osteotomy. Foot Ankle Int. 2017 Feb;38(2):124–132. doi: 10.1177/1071100716673416. [DOI] [PubMed] [Google Scholar]
- 20.Teramoto T., Harada S., Takaki M., Asahara T., Kato N. The Teramoto distal tibial oblique osteotomy (DTOO): surgical technique and applicability for ankle osteoarthritis with varus deformity. Strat. Trauma Limb Reconstr. 2018 Apr;13(1):43–49. doi: 10.1007/s11751-018-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mann H.A., Filippi J., Myerson M.S. Intra-articular opening medial tibial wedge osteotomy (plafond-plasty) for the treatment of intra-articular varu ankle arthritis and instability. Foot Ankle Int. 2012 Apr;33(4):255–261. doi: 10.3113/FAI.2012.0255. [DOI] [PubMed] [Google Scholar]
- 22.Tellisi N., Fragomen A.T., Kleinman D., O’Malley M.J., Rozbruch S.R. Joint preservation of the osteoarthritic ankle using distraction arthroplasty. Foot Ankle Int. 2009 Apr;30(4):318–325. doi: 10.3113/FAI.2009.0318. [DOI] [PubMed] [Google Scholar]
- 23.Amendola A., Beaman D.N., Saltzman C.L. Ankle joint distraction arthroplasty: why and how? Foot Ankle Clin. 2013 Sep;18(3):459–470. doi: 10.1016/j.fcl.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 24.Marijnessen A.C.A., Hoekstra M.C.L., Pre B.C., van Roermund P.M., van Melkebeek J. Patient characteristics as predictors of clinical outcome of distraction in treatment of severe ankle osteoarthritis. J Orthop Res. 2014 Jan;32(1):96–101. doi: 10.1002/jor.22475. [DOI] [PubMed] [Google Scholar]
- 25.Parker L., Singh D. Principles of foot and ankle arthrodesis, mini symposium. Foot Ankle. 2009 Dec;23(6):385–394. [Google Scholar]
- 26.Abidi N.A., Gruen G.S., Conti S.F. Ankle arthrodesis: indications and technique. J Am Acad Orthop Surg. 2000;8(3):200–209. doi: 10.5435/00124635-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Hefti F.L., Baumann J.U., Morscher E.W. Ankle joint fusion – determination of optimal position by gait analysis. Arch Orthop Trauma Surg. 1980;96(3):187–195. doi: 10.1007/BF00457782. [DOI] [PubMed] [Google Scholar]
- 28.Townshend D., Di Silvestro M., Krause F., Penner M., Younger A. Arthroscopic verus open ankle arthrodesis: a multicentre comparative case series. J Bone Joint Surg Am. 2013 Jan;95(2):98–102. doi: 10.2106/JBJS.K.01240. [DOI] [PubMed] [Google Scholar]
- 29.Glick J.M., Morgan M.S., Myerson T.G., Sampson T.G., Mann J.A. Ankle arthrodesis using an arthroscopic method: long term follow up of 34 cases. Arthroscopy. 2006;12:428–434. doi: 10.1016/s0749-8063(96)90036-5. [DOI] [PubMed] [Google Scholar]
- 30.Dannawi Z., Nawabi D.H., Patel A., Leong J.J.H., Moore D.J. Arthroscopic ankle arthrodesis: are results reproducible irrespective of pre-operative deformity? Foot Ankle Surg. 2011;17:294–299. doi: 10.1016/j.fas.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Schmid T., Krause F., Penner M.J., Veljkovic A., Younger A.S.E. Effect of preoperative deformity on arthroscopic and pen ankle fusion outcomes. Foot Ankle Int. 2017 Dec;38(12):1301–1310. doi: 10.1177/1071100717729491. [DOI] [PubMed] [Google Scholar]
- 32.Winson I.G., Robinson D.E., Allen P.E. Arthroscopic ankle arthrodesis. J Bone Joint Surg. 2005 Mar;87 – B(3):343–347. doi: 10.1302/0301-620x.87b3.15756. [DOI] [PubMed] [Google Scholar]
- 33.Brodsky J.W., Kane J.M., Coleman S., Bariteau J., Tenenbaum S. Abnormalities of gait caused by ankle arthritis are improved by ankle arthrodesis. Bone Joint Lett J. 2016 Oct;98 – B(10):1369–1375. doi: 10.1302/0301-620X.98B10.37614. [DOI] [PubMed] [Google Scholar]
- 34.Lynch A.F., Bourne R.B., Rorabeck C.H. The long term results of ankle arthrodesis. J Bone Joint Surg Br. 1988;70:113–116. doi: 10.1302/0301-620X.70B1.3339041. [DOI] [PubMed] [Google Scholar]
- 35.Yasui Y., Hannon C.P., Seow D., Kennedy J.G. Ankle arthrodesis: a systematic approach and review of the literature. World J Orthoped. 2016 Nov;7(11):700–708. doi: 10.5312/wjo.v7.i11.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cobb T.K., Gabrielson T.A., Campbell D.C., Wallrichs S.L., Ilstrup D.M. Cigarette smoking and nonunion after ankle arthrodesis. Foot Ankle Int. 1994 Feb;15(2):64–67. doi: 10.1177/107110079401500202. [DOI] [PubMed] [Google Scholar]
- 37.Thevendran G., Shah K., Pinney S.J., Younger A.S. Perceived risk factors for non-union following foot and ankle arthrodesis. J Orthop Surg (Hong Kong) 2017 Jan;25(1) doi: 10.1177/2309499017692703. [DOI] [PubMed] [Google Scholar]
- 38.Chalayon O., Wang B., Blankenhorn B., Jackson J.B., Beals T. Factors affecting the outcomes of uncomplicated primary open ankle arthrodesis. Foot Ankle Int. 2015;36(10):1170–1179. doi: 10.1177/1071100715587045. [DOI] [PubMed] [Google Scholar]
- 39.Simon A.M., Manigrasso M.B., O’Connor J.P. Cyclo-oxygenase 2 function is essential for bone fracture healing. J Bone Miner Res. 2002;17:963–976. doi: 10.1359/jbmr.2002.17.6.963. [DOI] [PubMed] [Google Scholar]
- 40.Moore K.R., Howell M.A., Saltrick K.R., Caranzariti A.R. Risk factors associated with non-union after elective foot and ankle reconstruction: a case control study. J Foot Ankle Surg. 2017;56(3):457–462. doi: 10.1053/j.jfas.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 41.Nunley J.A., Adams S.B., Easley M.E. Prospective randomised trial comparing mobile – bearing and fixed – bearing total ankle replacement. Foot Ankle Int. 2019 Sep;40(11):1239–1248. doi: 10.1177/1071100719879680. [DOI] [PubMed] [Google Scholar]
- 42.National joint Registry for england, wales, northern Ireland and the Isle of Man. 16th annual report. 2019. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2016th%20Annual%20Report%202019.pdf
- 43.Saito G.H., Saners A.E., O’Malley M.J., Deland J.T., Ellis S.J. Accuracy of patient-specific instrumentation in total ankle arthroplasty: a comparative study. Foot Ankle Surg. 2019;25(3):383–389. doi: 10.1016/j.fas.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 44.Schipper O.N., Denduluri S.K., Zhu Y., Haddad S.L. Effect of obesity on total ankle arthroplasty outcomes. Foot Ankle Int. 2016;37(1):1–7. doi: 10.1177/1071100715604392. [DOI] [PubMed] [Google Scholar]
- 45.Krause F.G., Windolf M., Bora B., Penner M.J., Wing K.J. Impact of complications in total ankle replacement and ankle arthrodesis analysed with a validated outcome measurement. J Bone Joint Surg Am. 2011 May;93(9):830–839. doi: 10.2106/JBJS.J.00103. [DOI] [PubMed] [Google Scholar]
- 46.Chou L.B., Coughlin M.T., Hansen S., Jr., Haskell A., Lundeen G. Osteoarthritis of the ankle: the role of arthroplasty. J Am Acad Orthop Surg. 2008 May;16(5):249–259. doi: 10.5435/00124635-200805000-00003. [DOI] [PubMed] [Google Scholar]
- 47.Trincat S., Kouyoumdjian P., Asencio G. Total ankle arthroplasty and coronal plane deformities. Orthop Traumatol Surg Res. 2012 Feb;98(1):75–84. doi: 10.1016/j.otsr.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 48.Dekker T.J., Hamid K.S., Easley M.E., DeOrio J.K., Nunley J.A. Ratio of range of motion of the ankle and surrounding joints after total ankle replacement. A radiographic cohort study. J Bone Joint Surg Am. 2017 Apr;99(7):576–582. doi: 10.2106/JBJS.16.00606. [DOI] [PubMed] [Google Scholar]
- 49.Singer S., Klejman S., Pinsker E., Houck J., Daniels T. Ankle arthroplasty and ankle arthrodesis: gait analysis compared with normal controls. J Bone Joint Surg Am. 2013 Dec;95(24):1–10. doi: 10.2106/JBJS.L.00465. e191. [DOI] [PubMed] [Google Scholar]
- 50.Palanca A., Mann R.A., Mann J.A., Haskell A. Scandinavian total ankle replacement: 15 year follow up. Foot Ankle Int. 2018 Feb;39(2):135–142. doi: 10.1177/1071100717738747. [DOI] [PubMed] [Google Scholar]
- 51.Clough T., Bodo K., Majeed H., Davenport J., Karski M. Survivorship and long term outcomes of a consecutive series of 200 Scandinavian total ankle replacement (STAR) implants. Bone Joint Lett J. 2019 Jan;101 – B(1):47–54. doi: 10.1302/0301-620X.101B1.BJJ-2018-0801.R1. [DOI] [PubMed] [Google Scholar]
- 52.Hofmann K.J., Shabin Z.M., Ferkel E., Jockel J., Slovenkai M.P. Salto Talaris total ankle arthroplasty: clinical results at a mean of 5.2 years in 78 patents treated by a single surgeon. J Bone Joint Surg Am. 2016 Dec;98(24):2036–2046. doi: 10.2106/JBJS.16.00090. [DOI] [PubMed] [Google Scholar]
- 53.Daniels T.R., Younger A.S., Penner M., Wing K., Dryden P.J. Intermediate term results of total ankle replacement and ankle arthrodesis: a COFAS multicentre study. J Bone Joint Surg Am. 2014 Jan;96(2):135–142. doi: 10.2106/JBJS.L.01597. [DOI] [PubMed] [Google Scholar]
- 54.Haddad S.L., Coetzee J.C., Estok R., Fahrbach K., Banel D. Intermediate and long term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007 Sep;89(9) doi: 10.2106/JBJS.F.001149. [DOI] [PubMed] [Google Scholar]
- 55.Velikovic A.N., Daniels T.R., Glazebrook M.A., Dryden P.J., Penner M.J. Outcomes of total ankle replacement, arthroscopic ankle arthrodesis and open ankle arthrodesis for isolated non-deformed end stage ankle arthritis. J Bone Joint Surg Am. 2019 Sep;101(17):1523–1529. doi: 10.2106/JBJS.18.01012. [DOI] [PubMed] [Google Scholar]
- 56.Clough T.M., Alvi F., Majeed H. Total ankle arthroplasty: what are the risks? A guide to surgical consent and a review of the literature. Bone Joint Lett J. 2018 Oct;100 – B(10):1352–1358. doi: 10.1302/0301-620X.100B10.BJJ-2018-0180.R1. [DOI] [PubMed] [Google Scholar]
- 57.Myerson M.S., Mroczek K. Perioperative complications of total ankle arthroplasty. Foot Ankle Int. 2003;24(1):17–21. doi: 10.1177/107110070302400102. [DOI] [PubMed] [Google Scholar]
- 58.Myerson M.S., Shariff R., Zonno A.J. The management of infection following total ankle replacement: demographics and treatment. Foot Ankle Int. 2014;35:855–862. doi: 10.1177/1071100714543643. [DOI] [PubMed] [Google Scholar]
- 59.Hintermann B., Zwicky L., Knupp M., Henninger H.B., Barg A. Hintegra revision arthroplasty for failed total ankle prostheses. J Bone Joint Surg Am. 2013 Jul;95(13):1166–1174. doi: 10.2106/JBJS.L.00538. [DOI] [PubMed] [Google Scholar]
- 60.Muller P., Skene S.S., Chowdhury K., Cro S., Goldberg A.J. TARVA study group. A randomised, multi-centre trial of total ankle replacement versus ankle arthrodesis in the treatment of patients with end stage ankle osteoarthritis (TARVA): statistical analysis plan. Trials. 2020 Feb;21(1):197. doi: 10.1186/s13063-019-3973-4. [DOI] [PMC free article] [PubMed] [Google Scholar]