Abstract
Lisfranc injuries may occur in the form of fracture-dislocations or pure ligamentous dislocations or subluxations. These innocuous appearing injuries have the potential for significant morbidity and long-term sequelae resulting in permanent deformities. Ligamentous subluxations account for 20% of these injuries and cases with partial incongruity are amenable to percutaneous fixation. In this article, we present step-by-step percutaneous fixation of these injuries as well as the post-operative management.
Keywords: Lisfranc injury, Foot, Tarsometatarsal joint, Internal fixation, Percutaneous, Minimally invasive
1. Introduction
The term Lisfranc injury refers to a spectrum of injuries involving the tarsometatarsal (TMT) complex; these have the potential for significant morbidity. Ligamentous subluxations account for 20% of these injuries and are frequently missed on the initial radiographs.1 Percutaneous fixation techniques are indicated for purely ligamentous disruptions with partial incongruity (i.e. Myerson type B injuries).2,3 Recommendations for conversion to open reduction include >2 mm of residual TMT joint displacement or more than 15°of persistent talo–first metatarsal angulation after attempts at closed reduction.4 In this article, we present step-by-step percutaneous fixation of these injuries.
1.1. Surgical technique
Step 1: Positioning
The patient is positioned supine with a sandbag under the ipsilateral hip to aid in intra-operative rotation of the limb. The leg is draped so as to permit knee flexion freely. A tourniquet is applied but not inflated; it is used if conversion to open reduction is needed. A sterile triangle or bolster is placed under the flexed knee to keep the foot flat on the operating table (Fig. 1). The image intensifier is positioned to come in from the opposite side.
Fig. 1.
a) Patient positioning: the patient is positioned with the knee flexed and foot flat on the table b) Intra-operative AP radiograph demonstrates a subtle shift of the 2nd metatarsal base, typical of a Myerson type B Lisfranc injury.
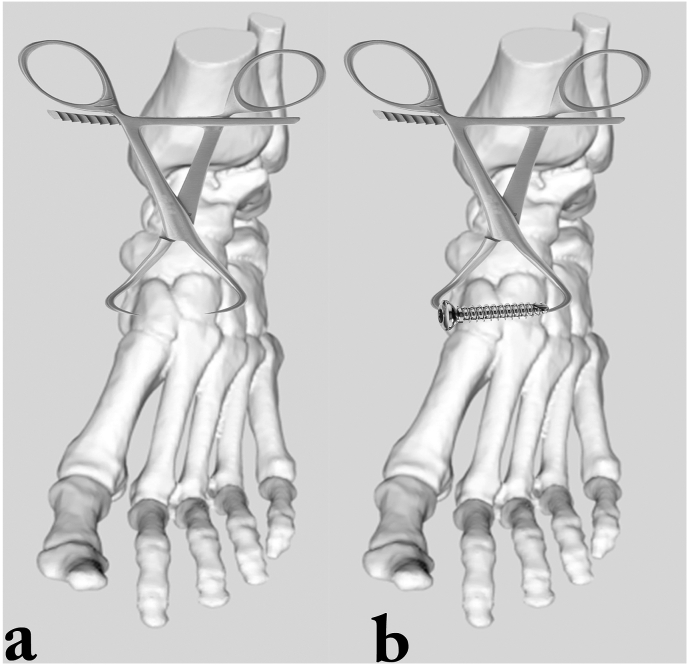
Step 2: Reduction of intercuneiform joint
If deemed unstable, the articulation between medial cuneiform (C1) and intermediate cuneiform (C2) is reduced with a pointed reduction clamp. After confirming the reduction, a 3.5 mm cortical screw is inserted from the proximal aspect of C1 into C2 (Fig. 2). Alternatively, a 4.0 mm cannulated cancellous screw (CCS) may be used. In the sagittal plane, the screw lies in the centre of C1 and C2.
Fig. 2.
Reduction of the intercuneiform joint a) A pointed reduction clamp is applied to the medial and intermediate cuneiforms b) After reduction, a 3.5 mm cortical screw or 4.0 mm cannulated screw is inserted.
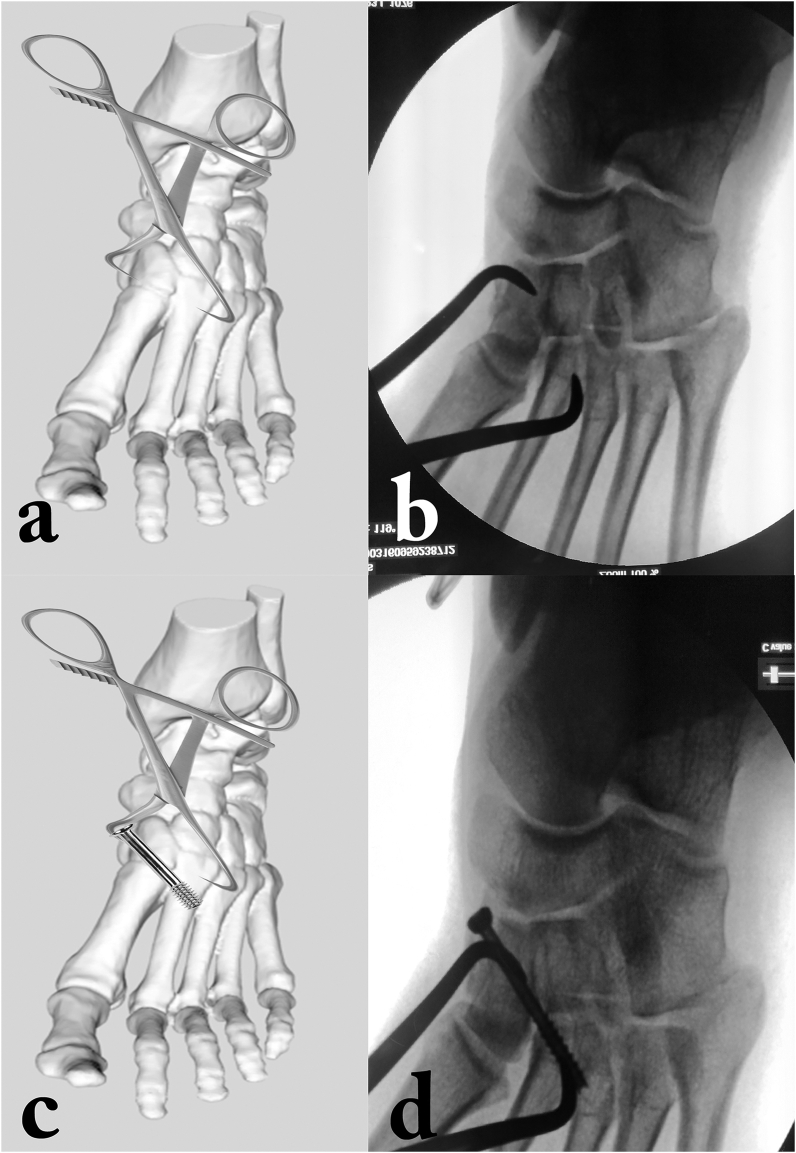
Step 3: Reduction of Lisfranc joint and ‘home-run’ screw placement
A pointed reduction clamp is applied from C1 to the second metatarsal (MT2). The prongs of the clamp rest dorsomedially on C1 and plantar-laterally on MT2. Tightening the clamp results in reduction of the Lisfranc joint. The ‘home-run’ screw is inserted in the direction of the reduction clamp, taking care to penetrate the lateral cortex of MT2 for optimal stability (Fig. 3).
Fig. 3.
Reduction of the Lisfranc joint a) and b) A pointed reduction clamp is applied from the medial cuneiform to the base of 2nd metatarsal c) and d) insertion of the ‘home-run’ screw. (In this case, there was no intercuneiform instability, hence manoeuvre described inFig. 2has not been depicted.)
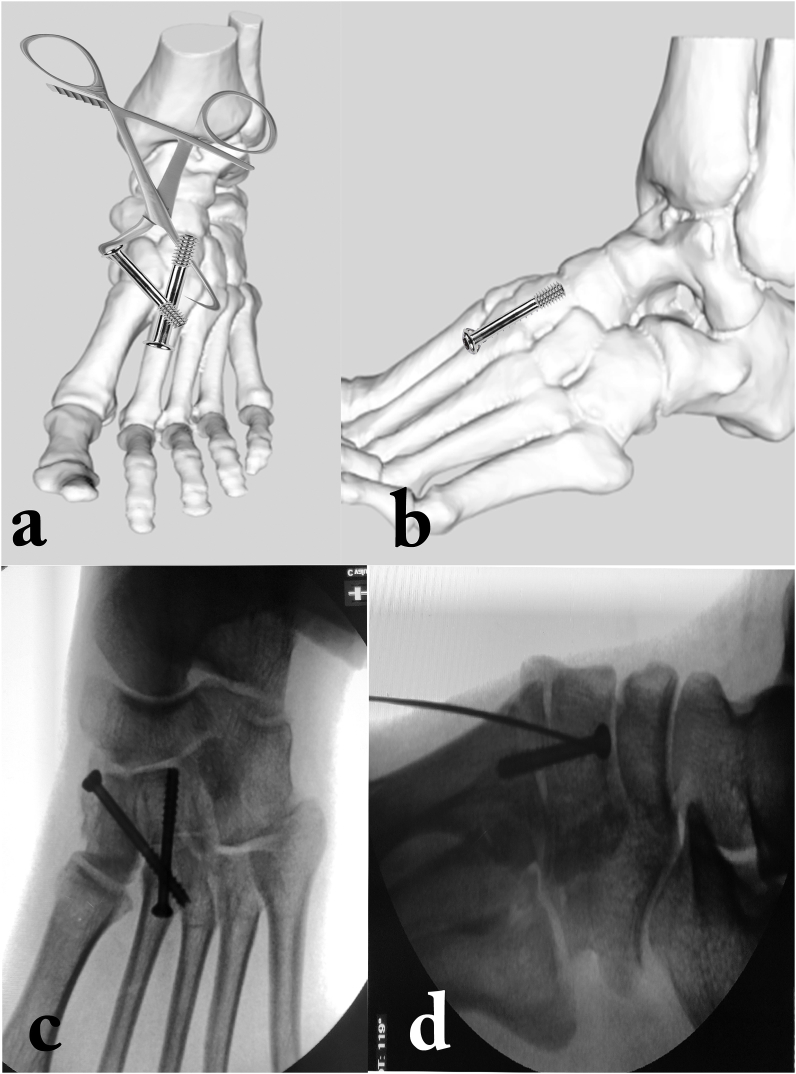
Step 4: Fixation of TMT 2
A screw is placed from just MT2 into C2. Care is taken to start the screw position distal to the MT2 base, so as to avoid superficial screw placement and dorsal cut-out (Fig. 4).
Fig. 4.
Fixation of the 2nd tarsometatarsal joint a) insertion of a screw across the 2nd tarsometatarsal joint b) the screw insertion should start just distal to the base of the 2nd metatarsal, so as avoid cut-out c) and d) intraoperative AP and Lateral images.
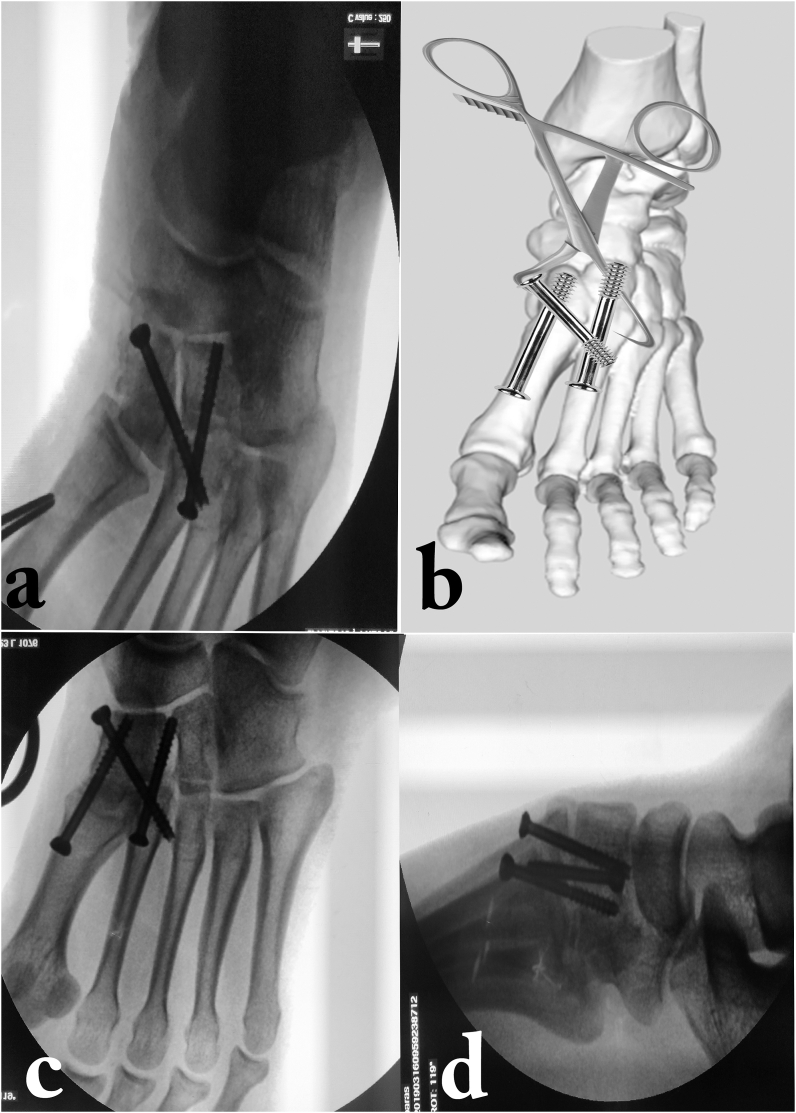
"Step 5: Fixation of TMT 1
The first metatarsal (MT1) can be reduced by applying a plantar force. One or two 1.5 mm K wires are used to provisionally hold the reduction. Fixation is achieved with a screw inserted from the base of MT1 into C1. It is important to start this screw distally from the MT1 shaft, so as to prevent superficial screw placement. Often, the assistant has to lift the leg off the table and plantar-flex the great toe, to securely drill from MT1 into C1 (Fig. 5).
Fig. 5.
a) Intra-operative stress testing of the 1st tarsometatarsal joint reveals instability b) fixation of the 1st TMT joint with a screw c) and d) intra-operative AP and Lateral images.
1.2. Postoperative protocol
Sutures are removal after 14 days. If swelling is present, the patient is mobilized initially in a back slab for a week. Thereafter, partial weight bearing is commenced in an ankle foot orthosis and ankle and toe range of motion is started. Radiographs are obtained at monthly intervals till 3 months and three-monthly thereafter. At 3 months, the orthosis is discontinued and full weight bearing is permitted in a moulded medial arch support for another 3 months. Screw removal is done at 6 months.
Declaration of competing interest
The authors declare no conflict of interest.
Contributor Information
Siddhartha Sharma, Email: sids82@gmail.com.
Mandeep S. Dhillon, Email: drdhillon@gmail.com.
Chirag Arora, Email: aro.chirag@gmail.com.
Sandeep Patel, Email: sandeepdrpatelortho@gmail.com.
References
- 1.Clare M.P. Lisfranc injuries. Curr Rev Musculoskelet Med. 2017;10:81–85. doi: 10.1007/s12178-017-9387-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vosbikian M., O’Neil J.T., Piper C., Huang R., Raikin S.M. Outcomes after percutaneous reduction and fixation of low-energy lisfranc injuries. Foot Ankle Int. 2017;38:710–715. doi: 10.1177/1071100717706154. [DOI] [PubMed] [Google Scholar]
- 3.Wagner E., Ortiz C., Villalón I.E., Keller A., Wagner P. Early weight-bearing after percutaneous reduction and screw fixation for low-energy lisfranc injury. Foot Ankle Int. 2013;34:978–983. doi: 10.1177/1071100713477403. [DOI] [PubMed] [Google Scholar]
- 4.Stavrakakis I.M., Magarakis G.E., Christoforakis Z. Percutaneous fixation of Lisfranc joint injuries: a systematic review of the literature. Acta Orthop Traumatol Turcica. 2019;53:457–462. doi: 10.1016/j.aott.2019.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]