Abstract
The National Health Policy (2017) of India advocates Universal Health Coverage through inclusive growth, decentralization, and rebuilding a cohesive community through a participatory process. To achieve this goal, understanding social organization, and community relationships – defined as social capital – is critical. This study aimed to explore the influence of individual and community-level social capital on a critical health system performance indicator, three-doses of diphtheria–pertussis–tetanus (DPT3) immunization among 12–59 month children, in rural Uttar Pradesh (UP), India. The analysis is based on a cross-sectional survey from two districts of UP, which included 2239 children 12–59 months of age (level 1) from 1749 households (level 2) nested within 346 communities (level 3). We used multilevel confirmatory factor analysis to generate standardized factor scores of social capital constructs (Organizational Participation, Social Support, Trust and Social Cohesion) of the household heads and mothers both at individual and community level, which were then used in the multilevel logistic regressions to explore the independent and contextual effect of social capital on a child's DPT3 immunization status. The result showed only community-level Social Cohesion of the mothers was associated with a child's DPT3 immunization status (Adjusted odds ratio = 1.25, 95% confidence interval = 1.12–1.54; p = 0.04). Beyond its independent effect on utilization of immunization service, the collective Social Cohesion of the mothers significantly modified the relationship of child age, mother's knowledge of immunization, community wealth, and communities' contact with frontline workers with immunization status of the child. With a strong theoretical underpinning, the result substantially contributes to understanding the individual and contextual predictors of immunization service utilization and further advancing the literature of social capital in India. This study can serve as a starting point to catalyze social capital within the health interventions for achieving wellbeing and the collective development of society.
Keywords: Uttar Pradesh, India, Social capital, Immunization, Multi-level modelling, SASCAT
Highlights
-
•
Social capital mainly operates at the community-level in the rural population of Uttar Pradesh, India.
-
•
Mothers' collective Social Cohesion positively influences immunization care utilization for children.
-
•
Mothers' community-level Social Cohesion also has modification effects.
-
•
Coverage of DPT3 vaccination within the study sample was 57% (n = 1282).
-
•
Social capital of household heads or male members do not influence a child's immunization.
1. Introduction
Childhood immunization is considered one of the “Best Buys,” and the net return of immunization is predicted to be 44 times the cost of the program in low and middle-income countries (Ozawa et al., 2016). For the last decade, globally, the coverage of three doses of diphtheria, tetanus, and pertussis (DTP3)1 vaccine is stagnant around 86%, and around 20 million children remained unvaccinated (World Health Organization, 2019). While the coverage of DPT3 vaccine in South Asia and India is almost similar to the Global scale – 87% and 89% accordingly – due to the sheer size of the population, more than 2.6 million children remain unvaccinated in India today (UNICEF, 2019).
However, if we take a more in-depth look, it appears there is still a significant inequality in immunization coverage across states of India. According to the latest National Family and Health Survey (NFHS), only 62% of the children aged 12–23 months receive all immunization – ranging from 91% in Puducherry to 35% in Nagaland. Among the northern states of India, Uttar Pradesh (UP) has seen a 28% increase in immunization coverage since 2005, yet it is one of the low performing states of India with only 51% of full immunization coverage (International Institute for Population Sciences & ICF, 2017).
Immunizing children not only depends on parental preference or the efficiency of the health system but also social context and the everyday interaction among individuals and communities. The contextual characteristics associated with the missing opportunity of immunization include – but not limited to – lack of social interaction (Rainey et al., 2011; Sridhar, Maleq, Guillermet, Colombini, & Gessner, 2014), mistrust towards vaccine, healthcare provider or institutions (Benin, Wisler-Scher, Colson, Shapiro, & Holmboe, 2006; MacDonald, Schopflocher, & Vaudry, 2014; Smith, Marcuse, Seward, Zhao, & Orenstein, 2015), peer influence and conformity with norms (Bults, Beaujean, Richardus, Steenbergen, & Voeten, 2011). Cumulatively all these contextual factors can be linked with social capital.
Social capital is the aggregated resources embedded within the social network and relationships of individuals and groups (Bourdieu, 1986). These resources can be exclusively available for the people within that social network. Beyond its utility as a private good, social capital is also conceptualized as the characteristics of social organization such as cohesiveness, norms, and trust, which can be used for coordinated actions for mutual benefits (Putnam, 1995). Social capital can be classified into structural and cognitive components. Structural social capital indicates the associational network among individuals and the community (Bourdieu, 1986). It is measured by civic engagement, community participation, collective action, and transaction of social support. In the time of need, structural social capital can be used to gain information, acquire financial assistance or access health services, etc. (Lindström, 2008). On the other hand, cognitive social capital is defined by the perception of trust, social cohesion, or solidarity among individuals and groups. Trust is necessary to facilitate the sharing of information and resources and to incentivize societal cooperation (Buchan, Croson, & Solnick, 2008). Social cohesion implies the depth of connections and perception of belongingness of individuals or groups to their community (Kawachi & Subramanian, 2007).
1.1. Social capital and immunization service utilization
Literature indicates five different pathways through which social capital can influence health-seeking. First, civic engagement and community participation (structural social capital) – allow the dissemination of information and initiate coordinated actions within the social network. As an example, the women's self-help group in India was able to significantly improve maternal and child health by formalizing a network of impoverished women (Saha, Annear, & Pathak, 2013). Secondly, structural social capital can influence health-related behavior when a person tried to access the “actual and potential” resources embedded within his/her social network. These resources (cash, in-kind support, transportation, etc.) can be instrumental in accessing and utilizing healthcare. As the third pathway, people can also invest in their social network to build reciprocity. In the time of need – such as taking the child to the health facility for immunization – this “credit slip” can help to acquire social support and buffer any stress.
Being a part of the community or a group often offers power and exclusivity, which can provide greater access to healthcare. As an example, health insurance only allows its contributing members to access the pooled fund while paying for care (Donfouet & Mahieu, 2012). Lastly, trust and cohesiveness among community members can foster collective action or impose informal social control to regulate health-related behaviors. If immunization is considered as a social norm, a cohesive community will work together to remove any barrier to the immunization service (Seid, Hesse, & Bloomfield, 2015). In reverse, members of the anti-vaccine campaigns also demonstrate a higher level of cohesiveness and refrain from vaccination (Mitra, Counts, & Pennebaker, 2016).
1.2. Immunization program in UP, India
The Expanded Program of Immunization (EPI) was started in India in 1978, followed by the Universal Immunization Program (UIP) in 1985 (Lahariya, 2014). Later in 2005, to re-strengthen the primary care service – including the immunization program – a systemwide reform was initiated through the National Health Mission (NHM) (Ministry of Health and Family Welfare, 2005). NHM introduced a new cadre of frontline workers (FLWs) called Accredited Social Health Activist (ASHA), Village Health, Sanitation and Nutrition Committee (VHSNC), and, most importantly, Mission Indradhanush – an intensified immunization campaign targeting 90% coverage of full immunization by 2020.
Since the inception of NHM, at the community level, the immunization campaign is led by ASHA, Anganwadi Workers (AWW, an FLW tenured by Ministry of Women and Child Development), and Auxiliary Nurse Midwife (ANM) – a government health worker assigned at the village-level health facilities. Every month the triad of FLWs organized Village Health Nutrition Day (VHND) to provide routine immunization to the children in the community. The organization and functioning of VHND are supported by VHSNC, which includes FLWs, local leaders, and other community-based organizations (Ministry of Health and Family Welfare, 2005). VHSNC assists FLWs by ensuring community participation, raising awareness, and tracking children who dropped out of the immunization schedule (Government of India, 2013).
Despite having a well-structured immunization program in paper, contextual factors such as trust, social norms, functioning of community organization, power dynamics in the community were shown to be associated with the immunization of children in India (Sahu, Pradhan, Jayachandran, & Khan, 2010; Scott, George, Harvey, Mondal, Patel, Ved, et al., 2017; Story, 2014). Moreover, recognized demand-side barriers for immunization care – such as age and gender of the child, mother's education, place of residence, social caste, religion, and socioeconomic status – are still relevant in the context of UP (Gupta, Prakash, & Srivastava, 2015; Shrivastwa, Gillespie, Kolenic, Lepkowski, & Boulton, 2015).
In a unique caste-based social structure of rural UP, where social norms, trust, and community support influence health-seeking behavior, considering social capital as a determinant for immunization is imperative. This study aimed to examine the association of individual and community-level social capital on DPT3 immunization among 12–59 month children using a multilevel analytical framework.
2. Method
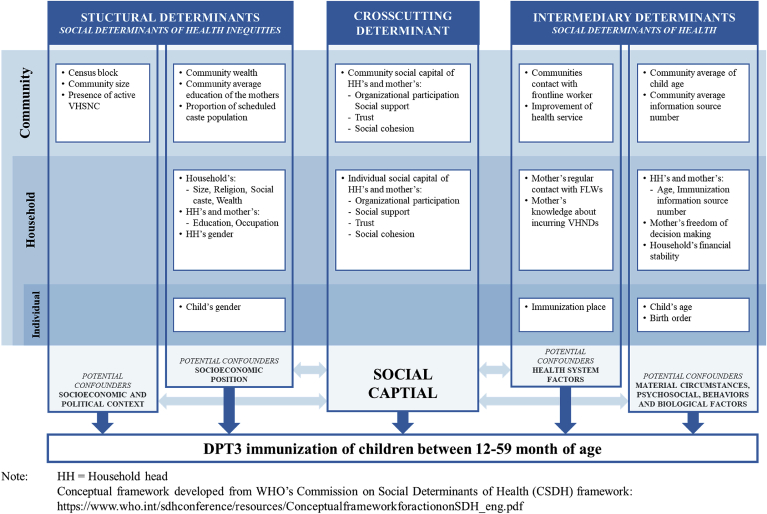
2.1. Conceptualizing social capital within the framework of social determinant of health
Social capital can not influence care-seeking practice in a void. It interacts with other social determinants (Marmot, 2005). Thus, we considered the World Health Organization's (WHO) Commission on Social Determinants of Health (CSDH) framework to understand social capital's influence on the utilization of immunization service (Fig. 1). This framework was initially drafted in 2005 (Commission on Social Determinants of Health, 2005), however, to develop our conceptual framework (Fig. 1), we adopted the final version of the framework by WHO (2010).
Fig. 1.
Conceptual framework to explore the role of social capital as a determinant of DPT3 immunization among 12-59-month-old children in UP, India.
Our conceptual framework stratified social determinants into three broad categories. First – as the structural determinant – socioeconomic position and socio-political context have to be included. Socioeconomic position includes – gender, household wealth, race/ethnicity, education, etc., and socio-political context includes governance, social policy, and cultural values of the community. These determinants collectively represent the social context, which grants differential levels of power and social position to individuals and groups (Graham, 2004). The second category of predictors is the intermediary social determinants. They are broadly divided into two groups. The first group includes – psychosocial, behavioral, and biological factors of individual or group, which represents life's material circumstances. Socially disadvantaged groups living with unfavorable material circumstances often engage in health-damaging behavior leading to poor health outcomes (World Health Organization, 2010). The health system's characteristics were considered as the second group of the intermediary determinants. If we consider India's community-based vaccination program, a robust health system can reduce inequality and financial burden among the poor and also generate social capital through building social support networks, solidarity, and social cohesion.
In between structural and intermediary social determinants of health, social capital is situated as the cross-cutting determinant (World Health Organization, 2010). The constructs of social capital (e.g., trust, cohesiveness, social support, social participation) can independently influence healthcare utilization and also indirectly influence other structural and intermediary determinants (Kawachi, Ichiro, Subramanian, , & Kim, 2008).
2.2. Study design and population
The analysis of this study was based on a multi-topic cross-sectional household survey conducted in two rural districts of UP. The multi-topic survey was a part of the baseline evaluation of a rural development initiative called “Project Samuday” led by the HCL Foundation (2018). The survey was implemented in randomly selected 6218 households from 346 rural communities – also know as Gram Panchayats (GPs) – from June to August 2017. The study design and sampling process of the survey were mentioned elsewhere (Hasan et al., 2019). Trained data collectors interviewed 6218 household heads (≥18years) and all women between 15-49 years of age (n = 6826) after receiving verbal informed consent.
During the survey, ever-married women responded to the maternal and child care utilization module where they reported the immunization status of under 59-month children. As it is possible that a child did not receive all vaccinations before 12 months of age (Wagner, Shenton, Gillespie, Mathew, & Boulton, 2019), to avoid partially immunized children, we considered 12–59 month children as the unit of analysis (n = 2239). With a 96.52% response rate, the final analytical sample for the regression analysis was 2161 children from 1705 households in 346 communities. Ethical approval of the study was received from the Institutional Review Board Office of Johns Hopkins Bloomberg School of Public Health, Maryland, USA, and locally from the Center for Media Studies, New Delhi, India.
2.3. Response variable
This study considered the DPT3 immunization status of a child as the dependent variable. DPT3 coverage is internationally used to monitor health system performance (World Health Organization, 2018) and indicates individual and community level immunization service utilization (Acharya, Kismul, Mapatano, & Hatløy, 2018; Fatiregun & Etukiren, 2014). During the survey, immunization information was extracted using both immunization records and mothers’ reporting following the current standardized method (International Institute for Population Sciences & ICF, 2017). DPT3 immunization status was defined as a binary indicator by assigning the value “1” for those children who received all three DPT vaccines before 12 months and “0” otherwise.
2.4. Explanatory variables
The primary explanatory variable of the analysis was social capital, which was considered as the cross-cutting social determinant of health. Other individuals, household and community level covariates, were classified according to the social determinant of health framework into structural or intermediary determinants. Table 1 maps out the explanatory variables included in the analysis (See supplemental materials for the detail list and definition of the covariates).
Table 1.
Covariates included in the analysis classified according to the social determinant of health framework and across the level of analysis.
| Levels of Analysis | Variables included in the analysis classified according to the social determinant of health framework |
|||
|---|---|---|---|---|
| Structural determinants | Intermediary determinants | Social capital | ||
| Level 1: Individual child |
|
|
||
| Level 2: Household | Mother |
|
|
|
| Household head |
|
|
|
|
| Household |
|
|
||
| Level 3: Community |
|
|
|
|
Note: FLWs = Front line health workers; GP = Gram Panchayat; VHSNC = Village Health Sanitation and Nutrition Committee; VHND = Village Health and Nutrition Day.
2.4.1. Social capital: the cross-cutting determinant
Social capital was measured by a contextually modified Shortened and adapted Social Capital Assessment Tool in India (SASCAT-I). The development and validation of the SASCAT-I were detailed elsewhere (Hasan et al., 2019). During the survey, participants responded to 13 SASCAT-I questions related to their participation in community groups, collective action with community, acquired social support, perception of trust, and cohesiveness. The SASCAT-I responses were converted into 12 categorical indicators, and multilevel confirmatory factor analytical (MCFA) models were implemented separately for the household heads and the mothers. MCFA generated four theoretically unique latent social capital constructs – Organizational participation, Social Support, Trust, and Social Cohesion. In total, 16 standardized factor scores were extracted as composite indicators of social capital – four indicators for each household head and mother both at individual and community-level. (See supplemental materials for the complete SASCAT-I and the methodological details of conducting MCFA).
2.4.2. Level 1 covariates: individual child's characteristics
Covariates related to individual children were classified into structural and intermediary determinants. A child's gender was considered as the only individual-level structural determinant. Biological factors such as the reported age of the child and birth order were considered as intermediary determinants. Also, we included the type of health facility where the child received most of his/her immunizations as health system-related intermediary determinants.
2.4.2. Level 2 covariates: mother, household head and household characteristics
From each household, mother's education and occupation were included as structural determinants. Her self-reported age, perceived ability of decision making (How much freedom do you have in making personal decisions?) (Babalola, 2009; Glatman-Freedman & Nichols, 2012) and knowledge about immunization (the number of sources from where the mother received information about immunization) are included as intermediary determinants. The individual mother's interaction with the health system was accounted for by including her regular contact with the FLWs and her knowledge of incurring VHNDs. Three household head's characteristics (gender, education and occupation) were included as structural determinants. In addition, household head's age, and knowledge about immunization were considered as intermediary determinants.
At the household-level, household size, religion, social caste, and wealth were included as structural determinants. We considered the number of people living in the household for the last 6 months as the indicator of the household size. Religion was categorized into “Hindu” and “Muslim and Others”. Caste was categorized into “General”, “Scheduled Castes or Scheduled Tribes” and “Other backward caste and others”. As a measure of household wealth, each household was assigned a wealth quintile of a linear index created by principal components analysis (PCA) of household assets (Filmer & Pritchett, 2001). As an intermediary determinant of the household's everyday material circumstances, household head's reported financial stability was included and categorized into “Worsen” or “Stable or Improved”.
2.4.3. Level 3 covariates: community characteristics
Other than individual and community levels social capital measure, child characteristics, and household-level compositional covariates, the analysis included several contextual covariates. Community-level structural determinants were further divided into two types. The first group was the sociopolitical context of the community – including administrative boundary (census blocks), community (GP) size, and the presence of active VHSNC in the community. The second set reflected the socioeconomic context of the community – including community wealth (average asset index of all households from a community included in the survey), average educational attainment of the mothers, and proportion of Scheduled Caste population in the community.
Other contextual variables incorporated in the analysis as intermediary determinants included – average age of the children living in the community, average of total number of immunization information sources reported by household heads and mothers, communities contact with FLWs (percentage of mothers in the community with regular contact with FLWs) and improvement of the health service (average response of household heads to the question about any improvement of the functioning of government health services in the village since last year).
2.4. Statistical analysis
As the descriptive analysis, the distribution of DPT3 immunization across covariates were explored as number and percentages. Next, the study implemented multilevel mixed-effect logistic regressions to assess the association of social capital measure with DPT3 immunization considering individual children as level 1, households as level 2, and GPs or communities as level 3. First, the effect of each individual, household, and community-level covariates on DPT3 immunization status was independently estimated. Covariates that presented a p-value ≤ 0.2 in the bivariate regression models were included in the multivariate regressions (Maldonado & Greenland, 1993). Next, to estimate the adjusted fixed-effect of social capital measure, seven multilevel mixed-effect logistic models were sequentially fitted to the data considering household and community as random intercepts. Model 1 (M1) was a null model without any covariate, which decomposed the total variance of DPT3 immunization between households and the community level. Model 2 (M2) only included child-related covariates. Model 3 (M3) extended M2 by including the characteristics of mothers and household heads. Model 4 (M4) further extended M3 by including standardized factor scores of individual mothers and household heads social capital. Model 5 (M5) and Model 6 (M6) were expanded by sequentially adding the household and community-level covariates. The last model (M7) incorporated all covariates from M6 and included community-level standardized factor scores of mothers' and household heads’ social capital. We have also examined several interactions between significant social capital measures with other covariates, which presented a statistically significant association with DPT3 immunization. MCFA models were implemented using Mplus 8.1 (Muthén & Muthén, 2017), and data management, descriptive and regression analysis were performed using Stata 15.1 (StataCorp, 2017).
3. Result
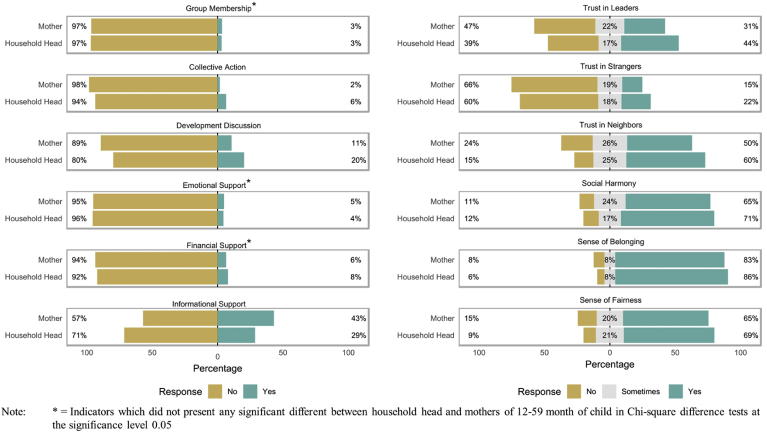
Table 2 presents the descriptive statistics of 12–59 months old children disaggregated by their DPT3 immunization status. Within the study sample, 57% (n = 1282) of children have been immunized by the DPT3 vaccine before 12 months of age. Fig. 2 presents the distribution of the 12 social capital indicators among household heads (n = 1749) and mothers (n = 1779). Among the 12 indicators, group membership, emotional, and financial support did not present any statistically significant difference between the household heads and mothers (χ2 p-value > 0.05).
Table 2.
Demography of children between 12-59 months in two districts of UP, India (N = 2239).
| DPT vaccination status |
Total (n = 2239) |
||||||
|---|---|---|---|---|---|---|---|
| Yes (n = 1282) |
No (n = 957) |
P-Value |
|||||
| n | % | n | % | n | % | ||
| Child's age category a | |||||||
| 12–23 month | 358 | 67.17 | 175 | 32.83 | 0.00 | 533 | 100.00 |
| 24–35 months | 345 | 63.42 | 199 | 36.58 | 544 | 100.00 | |
| 36–47 months | 330 | 55.56 | 264 | 44.44 | 594 | 100.00 | |
| 48–59 months | 235 | 46.91 | 266 | 53.09 | 501 | 100.00 | |
| Child's birth order a | |||||||
| Firstborn | 1016 | 57.05 | 765 | 42.95 | 0.00 | 1781 | 100.00 |
| Not firstborn (Second/third/fourth born) | 252 | 64.45 | 139 | 35.55 | 391 | 100.00 | |
| Child's gender a | |||||||
| Boy | 661 | 57.83 | 482 | 42.17 | 0.44 | 1143 | 100.00 |
| Girl | 621 | 56.71 | 474 | 43.29 | 1095 | 100.00 | |
| Facility where most vaccinations received a | |||||||
| AWC or VHND | 758 | 62.59 | 453 | 37.41 | 0.00 | 1211 | 100.00 |
| Sub-Centers | 326 | 60.93 | 209 | 39.07 | 535 | 100.00 | |
| PHC, CHC or Hospital | 177 | 60.41 | 116 | 39.59 | 293 | 100.00 | |
| Mother's age category a | |||||||
| 15–19 years | 25 | 65.79 | 13 | 34.21 | 38 | 100.00 | |
| 20–29 years | 856 | 60.54 | 558 | 39.46 | 1414 | 100.00 | |
| 30–39 years | 358 | 52.65 | 322 | 47.35 | 680 | 100.00 | |
| 40–49 years | 38 | 39.58 | 58 | 60.42 | 96 | 100.00 | |
| Mother's education a | |||||||
| Illiterate | 572 | 50.57 | 559 | 49.43 | 0.00 | 1131 | 100.00 |
| Up to Primary | 318 | 60.00 | 212 | 40.00 | 530 | 100.00 | |
| Above Primary | 387 | 68.25 | 180 | 31.75 | 567 | 100.00 | |
| Mother's occupation a | |||||||
| Unemployed/Housewife | 1215 | 57.34 | 904 | 42.66 | 0.73 | 2119 | 100.00 |
| Employed | 62 | 56.88 | 47 | 43.12 | 109 | 100.00 | |
| Mother's regular communication with FLWs | |||||||
| Yes | 795 | 61.58 | 496 | 38.42 | 0.00 | 1291 | 100.00 |
| No | 487 | 51.37 | 461 | 48.63 | 948 | 100.00 | |
| Mother knew about incurring VHNDs | |||||||
| Yes | 658 | 60.81 | 424 | 39.19 | 0.00 | 1157 | 100.00 |
| No | 624 | 53.93 | 533 | 46.07 | 1082 | 100.00 | |
| Mother's Freedom of decision-making a | |||||||
| No freedom at all | 193 | 51.60 | 181 | 48.40 | 0.00 | 374 | 100.00 |
| Freedom in very few decisions | 304 | 62.42 | 183 | 37.58 | 487 | 100.00 | |
| Freedom in some decisions | 377 | 60.32 | 248 | 39.68 | 625 | 100.00 | |
| Freedom in most decisions | 226 | 52.56 | 204 | 47.44 | 430 | 100.00 | |
| Freedom in all decisions | 181 | 56.92 | 137 | 43.08 | 318 | 100.00 | |
| Head's age category a | |||||||
| 18–29 years | 160 | 54.98 | 131 | 45.02 | 0.00 | 291 | 100.00 |
| 30–39 years | 291 | 54.91 | 239 | 45.09 | 530 | 100.00 | |
| 40–49 years | 323 | 60.60 | 210 | 39.40 | 533 | 100.00 | |
| 50–59 years | 243 | 58.84 | 170 | 41.16 | 413 | 100.00 | |
| 60–69 years | 184 | 55.93 | 145 | 44.07 | 329 | 100.00 | |
| More than 70 years | 78 | 56.52 | 60 | 43.48 | 138 | 100.00 | |
| Head's education | |||||||
| Illiterate | 516 | 57.14 | 387 | 42.86 | 0.38 | 903 | 100.00 |
| Up to Primary | 307 | 55.12 | 250 | 44.88 | 557 | 100.00 | |
| Above Primary | 459 | 58.92 | 320 | 41.08 | 779 | 100.00 | |
| Head's occupation | |||||||
| Cultivator | 693 | 58.83 | 485 | 41.17 | 0.13 | 1178 | 100.00 |
| Wage laborer | 250 | 52.63 | 225 | 47.37 | 475 | 100.00 | |
| Salaried Worker | 170 | 59.03 | 118 | 40.97 | 288 | 100.00 | |
| Unemployed | 169 | 56.71 | 129 | 43.29 | 298 | 100.00 | |
| Religion | |||||||
| Hindu | 1102 | 57.10 | 828 | 42.90 | 0.70 | 1930 | 100.00 |
| Muslim and Others | 180 | 58.25 | 129 | 41.75 | 309 | 100.00 | |
| Caste | |||||||
| General | 205 | 58.91 | 143 | 41.09 | 0.40 | 348 | 100.00 |
| Scheduled Caste and Schedule Tribe | 598 | 58.17 | 430 | 41.83 | 1028 | 100.00 | |
| Other Backward Caste and others | 479 | 55.50 | 384 | 44.50 | 863 | 100.00 | |
| Wealth Quintile | |||||||
| Quintile 1 | 168 | 52.50 | 152 | 47.50 | 0.08 | 320 | 100.00 |
| Quintile 2 | 196 | 58.51 | 139 | 41.49 | 335 | 100.00 | |
| Quintile 3 | 266 | 58.72 | 187 | 41.28 | 453 | 100.00 | |
| Quintile 4 | 287 | 54.25 | 242 | 45.75 | 529 | 100.00 | |
| Quintile 5 | 365 | 60.63 | 237 | 39.37 | 602 | 100.00 | |
| Census Block | |||||||
| Behadar | 257 | 58.54 | 182 | 41.46 | 0.92 | 439 | 100.00 |
| Kachhauna | 158 | 60.77 | 102 | 39.23 | 260 | 100.00 | |
| Kothwan | 232 | 53.58 | 201 | 46.42 | 433 | 100.00 | |
| Kasmanda | 203 | 54.57 | 169 | 45.43 | 372 | 100.00 | |
| Machhrehta | 202 | 62.15 | 123 | 37.85 | 325 | 100.00 | |
| Sidhauli | 230 | 56.10 | 180 | 43.90 | 410 | 100.00 | |
| District | |||||||
| Hardoi | 647 | 57.16 | 485 | 42.84 | 0.92 | 1132 | 100.00 |
| Sitapur |
635 |
57.36 |
472 |
42.64 |
1107 |
100.00 |
|
| Total | 1282 | 57.26 | 957 | 42.74 | 2239 | 100.00 | |
| Mean |
SD |
Mean |
SD |
Mean |
SD |
||
| Mother's information source for immunization | 1.49 | 1.17 | 1.20 | 1.03 | 0.00 | 1.37 | 1.12 |
| Head's information source for immunization | 1.30 | 1.52 | 1.16 | 1.48 | 0.03 | 1.24 | 1.50 |
| Individual standardized social capital score | |||||||
| Mother's Organizational Participation | 0.02 | 0.96 | 0.00 | 1.05 | 0.58 | 0.01 | 1.00 |
| Mother's Social Support | -0.01 | 0.96 | 0.00 | 1.05 | 0.82 | -0.01 | 1.00 |
| Mother's Trust | 0.07 | 0.99 | -0.04 | 0.99 | 0.01 | 0.03 | 0.99 |
| Mother's Social Cohesion | 0.06 | 1.00 | -0.04 | 0.97 | 0.03 | 0.02 | 0.99 |
| Head's Organizational Participation | 0.01 | 0.98 | -0.03 | 1.03 | 0.34 | 0.00 | 1.00 |
| Head's Social Support | 0.02 | 0.99 | -0.03 | 1.02 | 0.22 | 0.00 | 1.00 |
| Head's Trust | -0.03 | 1.00 | 0.04 | 1.00 | 0.08 | 0.00 | 1.00 |
| Head's Social Cohesion | -0.03 | 1.00 | 0.04 | 1.02 | 0.09 | 0.00 | 1.01 |
Note: Table presents row percentage, a = Variable present missing values,
AWC = Anganwadi Center, CHC = Community Healthcare Center, FLW = Front Line Health Workers, VHND = Village Health and Nutrition Day, PHC = Primary Healthcare Center.
Fig. 2.
Distribution of social capital indicators of household heads (n = 1749) and mothers (n = 1779) of 12-59-month-old children in UP, India.
Table 3 presents the crude odds ratios (COR) and adjusted odds ratios (AOR) between DPT3 immunization and covariates. After adjusting for individual, household, and community-level covariates, only community-level Social Cohesion of the mothers presented a significant association with a child's DPT3 immunization status in the final model (M7). Between two communities that differ by one standard deviation (SD) of mothers' collective Social Cohesion, a child living in the community with higher Social Cohesion of the mothers had 25% higher odds (AOR = 1.25, 95% Confidence Intervals [CI] = 1.12–1.54; p = 0.04) compared to a child from a community with lower Social Cohesion of the mothers.
Table 3.
Comparison of three-level mixed-effect models for fixed and random-effect estimates for DPT3 immunization among children between 12-59 months in two districts of Uttar Pradesh, India.
| Fixed effects | COR | M1 |
M2 |
M3 |
M4 |
M5 |
M6 |
M7 |
95% CI |
|---|---|---|---|---|---|---|---|---|---|
| AOR | AOR | AOR | AOR | AOR | AOR | AOR | |||
| Child's characteristics | |||||||||
| Age categories (Ref- 48 to 59 months) | |||||||||
| 12–23 months | 5.05*** | 4.87*** | 3.94*** | 3.97*** | 4.00*** | 4.61*** | 4.50*** | [2.65, 7.64] | |
| 24–35 months | 3.73*** | 3.66*** | 3.26*** | 3.25*** | 3.26*** | 3.77*** | 3.79*** | [2.36, 6.08] | |
| 36–47 months | 1.90** | 1.87** | 1.78** | 1.79** | 1.80** | 1.96** | 1.99** | [1.32, 3.00] | |
| Birth order (Ref- Firstborn) | |||||||||
| Not firstborn (second or third) | 2.26*** | 1.04 | 1.13 | 1.13 | 1.13 | 1.07 | 1.08 | [0.72, 1.63] | |
| Gender (Ref- Boy) | |||||||||
| Girl | 0.95 | ||||||||
| Facility for vaccination (Ref- AWC/VHND) | |||||||||
| Sub-centers | 0.92 | ||||||||
| PHC, CHC or Hospital | 0.71 | ||||||||
| Mother's characteristics | |||||||||
| Age categories (40–49 years) | |||||||||
| 15–19 year | 6.12** | 2.62 | 2.72 | 2.40 | 2.49 | 2.57 | [0.64, 10.32] | ||
| 20–29 years | 4.22*** | 2.27* | 2.36* | 2.18* | 2.32* | 2.35* | [1.10, 5.01] | ||
| 30-30 years | 2.42* | 1.76 | 1.78 | 1.69 | 1.72 | 1.77 | [0.83, 3.78] | ||
| Education (Ref-Illiterate) | |||||||||
| Up to primary | 1.86*** | 1.65* | 1.66* | 1.64* | 1.69** | 1.66* | [1.12, 2.46] | ||
| Above primary | 3.32*** | 2.60*** | 2.57*** | 2.53*** | 2.58*** | 2.59*** | [1.66, 4.02] | ||
| Occupation (Ref-Unemployed) | |||||||||
| Employed | 0.86 | ||||||||
| Knowledge of immunization | 1.51*** | 1.47*** | 1.47*** | 1.46*** | 1.43*** | 1.42*** | [1.19, 1.69] | ||
| Regular communication with FLWs (Ref- No) | |||||||||
| Yes | 1.74*** | 1.41* | 1.35 | 1.33 | 0.99 | 1.00 | [0.69, 1.45] | ||
| Knew about incurring VHNDs (Ref- No) | |||||||||
| Yes | 1.44* | 1.18 | 1.18 | 1.17 | 1.20 | 1.23 | [0.89, 1.70] | ||
| Freedom of decision making (Ref- No freedom at all) | |||||||||
| Freedom in very few decisions | 1.66* | 1.56 | 1.53 | 1.47 | 1.37 | 1.29 | [0.78, 2.14] | ||
| Freedom in some decisions | 1.63* | 1.61 | 1.62* | 1.58 | 1.42 | 1.35 | [0.84, 2.18] | ||
| Freedom in most decisions | 1.04 | 1.09 | 1.06 | 1.00 | 0.89 | 0.84 | [0.50, 1.42] | ||
| Freedom in all decisions | 1.26 | 1.06 | 1.02 | 0.97 | 0.93 | 0.87 | [0.49, 1.55] | ||
| Mother's Individual social capital | |||||||||
| Organizational participation | 1.02 | ||||||||
| Social support | 0.99 | ||||||||
| Trust | 1.13ᵃ | 1.27 | 1.26 | 1.24 | 1.09 | [0.77, 1.54] | |||
| Social cohesion | 1.11ᵃ | 0.90 | 0.91 | 0.93 | 1.02 | [0.74, 1.40] | |||
| Household Head's characteristics | |||||||||
| Gender (Ref: Male) | |||||||||
| Female | 0.86 | ||||||||
| Age categories (18–29 years) | |||||||||
| 30–39 years | 0.89 | ||||||||
| 40–49 years | 1.38 | ||||||||
| 50–59 years | 1.23 | ||||||||
| 60–69 years | 0.93 | ||||||||
| More than 70 years | 1.07 | ||||||||
| Occupation (Ref- Cultivator) | |||||||||
| Wage laborer | 0.80 | ||||||||
| Salaried worker | 1.16 | ||||||||
| Unemployed/Student/Housewife | 0.94 | ||||||||
| Education (Ref- Illiterate) | |||||||||
| Up to primary | 0.99 | ||||||||
| Above primary | 1.16 | ||||||||
| Knowledge of immunization | 1.09ᵃ | 1.03 | 1.03 | 1.03 | 1.02 | 1.02 | [0.9, 1.16] | ||
| Household Head's Individual social capital | |||||||||
| Organizational participation | 1.02 | ||||||||
| Social support | 1.04 | ||||||||
| Trust | 0.87ᵃ | 0.91 | 0.92 | 0.94 | 1.01 | [0.70, 1.47] | |||
| Social cohesion | 0.88ᵃ | 0.95 | 0.93 | 0.94 | 0.90 | [0.63, 1.29] | |||
| Household's characteristics | |||||||||
| Household Size (Member Number) | 0.95ᵃ | 0.96 | 0.95 | 0.95 | [0.88, 1.02] | ||||
| Religion (Ref- Hindu) | |||||||||
| Muslim and Others | 1.15 | ||||||||
| Caste (Ref- General) | |||||||||
| Scheduled Caste/Scheduled Tribe | 0.92 | ||||||||
| Other backward caste and others | 0.83 | ||||||||
| Household wealth (Ref- Quintile 1) | |||||||||
| Quintile 2 | 1.71* | 1.51 | 1.49 | 1.50 | [0.85, 2.65] | ||||
| Quintile 3 | 1.46ᵃ | 1.51 | 1.45 | 1.44 | [0.84, 2.44] | ||||
| Quintile 4 | 1.15 | 1.09 | 1.08 | 1.07 | [0.64, 1.78] | ||||
| Quintile 5 | 1.66* | 1.70* | 1.69* | 1.67* | [1.00, 2.77] | ||||
| Household financial stability (Ref- Worsen) | |||||||||
| Stable or Improved | 1.19 | ||||||||
| Community characteristics | |||||||||
| Census Block (Ref- Behadar) | |||||||||
| Kachhauna | 1.10 | ||||||||
| Kothwan | 0.70 | ||||||||
| Kasmanda | 0.75 | ||||||||
| Machhrehta | 1.29 | ||||||||
| Sidhauli | 0.86 | ||||||||
| Community size (Ref- Small) | |||||||||
| Medium | 0.71 | 0.69 | 0.67 | [0.43, 1.06] | |||||
| Large | 0.67ᵃ | 0.58* | 0.56* | [0.35, 0.89] | |||||
| Community-level scheduled caste population (Ref: Low) | |||||||||
| Medium | 1.18 | ||||||||
| High | 1.20 | ||||||||
| Community wealth | 1.37*** | 1.39** | 1.34** | [1.09, 1.64] | |||||
| Community average age of children (Months) | 1.03ᵃ | 1.06** | 1.05** | [1.02, 1.09] | |||||
| Community average mothers' education | 1.69* | 0.76 | 0.77 | [0.46, 1.29] | |||||
| Community average knowledge of immunization | 1.25** | 1.10 | 1.11 | [0.93, 1.34] | |||||
| Communities contact with the FLWs | 4.05*** | 4.80*** | 4.74*** | [2.12, 10.58] | |||||
| Improvement of the health service (Ref- No) | |||||||||
| Yes | 1.02 | ||||||||
| Presence of active VHSNC (Ref- No) | |||||||||
| Yes | 1.66** | 1.58* | 1.58* | [1.08, 2.32] | |||||
| Mothers' community-level social capital | |||||||||
| Organizational participation | 1.03 | ||||||||
| Social support | 0.86ᵃ | 0.84 | [0.67, 1.05] | ||||||
| Trust | 0.85ᵃ | 0.89 | [0.71, 1.11] | ||||||
| Social cohesion | 1.18ᵃ | 1.25* | [1.12, 1.54] | ||||||
| Household Head's community-level social capital | |||||||||
| Organizational participation | 1.02 | ||||||||
| Social support | 0.96 | ||||||||
| Trust | 0.88ᵃ | 0.86 | [0.7, 1.05] | ||||||
| Social cohesion | 0.98 | ||||||||
| Random effects | |||||||||
| Level 3: Community level variation (variance) | 1.16*** | 1.58*** | 1.39*** | 1.31*** | 1.34*** | 0.93*** | 0.88*** | [0.49, 1.59] | |
| ICC | 0.17 | 0.19 | 0.18 | 0.17 | 0.18 | 0.13 | 0.13 | [0.08, 0.20] | |
| Level 2: Household level variation (Variance) | 2.20*** | 3.42*** | 3.03*** | 2.97*** | 2.79*** | 2.94*** | 2.89*** | [1.62, 5.17] | |
| ICC |
0.51 |
0.60 |
0.57 |
0.57 |
0.56 |
0.54 |
0.53 |
[0.41, 0.66] |
|
| Observations | 2161 | 2161 | 2161 | 2161 | 2161 | 2161 | 2161 | ||
| Log-likelihood (LL) | -1407.59 | -1370.16 | -1323.65 | -1320.41 | -1316.25 | -1292.51 | -1288.06 | ||
| Akaike information criterion (AIC) | 2821.2 | 2754.3 | 2687.3 | 2688.8 | 2690.5 | 2659.0 | 2658.1 | ||
Note: *** = p < 0.001, ** = p < 0.01, * = p < 0.05, ᵃ = p < 0.2.
Regressions include data from 2161children of 12–59 months from 1705 households within 346 Gram Panchayats (PSU).
AOR = Adjusted odds ratio, AWC = Anganwadi Center, CHC = Community Healthcare Center, COR = Crud odds ratio, FLW = Front Line Health Workers, ICC = intra-class correlation, PHC = Primary Healthcare Center, VHND = Village Health and Nutrition Day, VHSNC = Village Health Sanitation and Nutrition Committee.
Among other covariates, mother's education and the child's age category presented robust and significant association. After adjusting for all covariates and random effects, a child whose mother attained primary educations had 66% higher odds (AOR = 1.66, 95%CI = 1.12–2.46; p < 0.001) and a child whose mother attained above primary education had 159% higher odds (AOR = 2.59, 95%CI = 1.66–4.02; p < 0.001) of being immunized by DPT3, compared to a child of an illiterate mother. Additionally, adjusting for all confounders, mother's knowledge of immunization, community wealth, presence of active VHSNC in the community, and community's contact with FLWs were significantly associated with DPT3 immunization (p < 0.05).
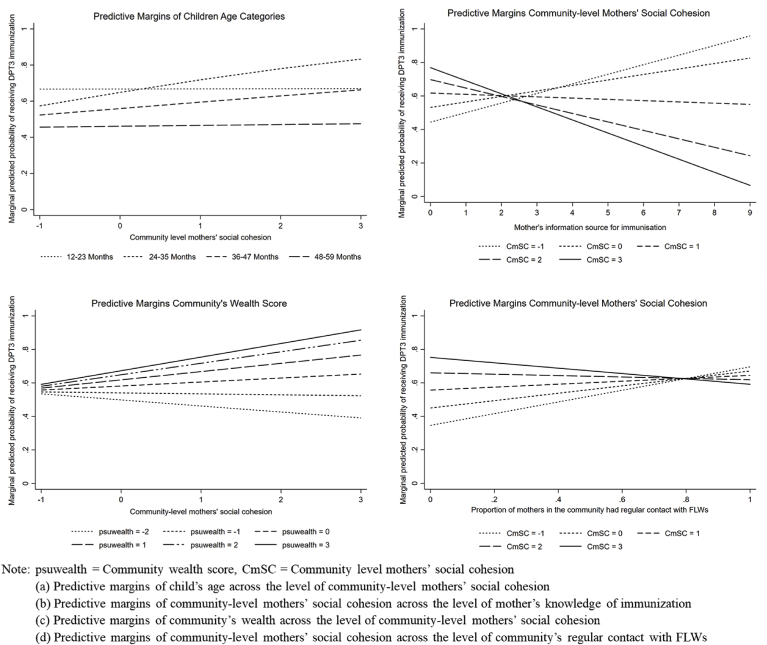
We identified four significant interactions between community-level Social Cohesion of the mothers and other covariates – child age, mother's knowledge of immunization, community wealth, and communities' contact with FLWs (Fig. 3). Among the age categories, 24–35 months presented the highest interaction effect of 1.69 (95%CI = 1.11–2.57; p < 0.05). This indicated that the synergistic effect of mothers' Social Cohesion is 69% higher among 24–35 month children compared to the oldest age category (48–59 months). The interaction between community-level Social Cohesion of the mothers and community wealth presented a positive effect (Exponentiated coefficient = 1.24, 95%CI = 1.03–1.50; p < 0.05).
Fig. 3.
Modification effect of community-level social cohesion of mothers on the association between covariates and predicted the probability of a child receiving DPT3 immunization.
The cross level-interaction effect with individual mother's knowledge of immunization presented a negative correlation with DPT3 immunization (Exponentiated coefficient = 0.72, 95%CI = 0.60–0.86; p < 0.001). If a child lived in a community with lower collective Social Cohesion among mothers, his/her probability of receiving DPT3 vaccine increased proportionately with his/her mother's knowledge of immunization (Fig. 3b), and living in a community with higher Social Cohesion among mothers had the opposite effect. A negative interaction was also observed between the community's contact with FLWs and Social Cohesion among mothers (Exponentiated coefficient = 0.38, 95%CI = 0.19–0.76; p < 0.001). Regardless of the negative interaction effect, we observed an increase in the direct effect of both collective Social Cohesion of mothers (AOR = 2.16, 95%CI = 1.37–3.40; p < 0.001) and community's contact with FLWs (AOR = 5.06, 95%CI = 2.26–11.31; p < 0.001) in the interaction model. (See supplemental materials for the result of the interaction analysis)
4. Discussion
4.1. Discussion of the result
Just more than half of the children in the sample received all three doses of DPT vaccine before the age of 12 months. The coverage among 12–35 month children was 67%, which is very similar to the latest estimates of UP (66.5%), reported by the NHFS of 2015 (International Institute for Population Sciences & ICF, 2017). Social capital – especially Social Cohesion of the mothers – appears to be a contextual characteristic of the community, which positively correlates with the utilization of immunization care for children. This finding was also reported by William T. Story (2014) and other studies exploring self-rated health (Mohnen, Groenewegen, Völker, & Flap, 2011), mental health (De Silva, Huttly, Harpham, & Kenward, 2007) and other health behaviors (Chuang & Chuang, 2008). Emerged from the collective human relations, a community's Social Cohesion can positively influence the community's behavior by performing coordinated action for the common good (Kim & Kawachi, 2017; Putnam, 1995) – here, utilization of immunization service. In UP, where vaccination service is embedded within the community and largely depends on the coordination between the health providers and community organizations (VHND), the role of Social Cohesion becomes particularly important. The collective cohesiveness of the mother would empower the community, foster entitlement, and create an enabling environment to access health services (Kim & Kawachi, 2017). However, Story (2014) did not observe any association with the Social Cohesion of mothers with complete childhood immunization. The study was conducted with a national level representative sample and did not report a state-level disaggregated result. The socioeconomic and cultural diversity of northern India – especially in UP – may explain the dissimilarity of the result.
The result also showed community-level Social Cohesion of the mothers acted as an effect modifier by differentially influencing both structural and intermediary determinants of health. Knowledge about immunization is an established social determinant of immunization, and our finding corroborates this (Glatman-Freedman & Nichols, 2012). However, moving from lower to a higher degree of community-level mother's Social Cohesion, the association between mother's knowledge of immunization and DPT3 immunization gradually attenuated and then moved towards negative (Fig. 3b). This may indicate the influence of informal social control of a highly cohesive community. The existing social norm and values of a tightly bonded community often discourage its members from adopting behaviors even the members have adequate knowledge to perform that activity (Vikram, Vanneman, & Desai, 2012).
The direct effect of the community's contact with FLWs – both in the adjusted model (Table 3) and in the interaction model (see supplemental materials) – had a strong positive relationship with the child's DPT3 immunization status. Provider-parent engagement is critical for building trust in immunization (Ames, Glenton, & Lewin, 2017; Connors, Slotwinski, & Hodges, 2017). However, we also found that community-level mother's Social Cohesion could modify the relationship between community-FLW's interconnection and child's immunization status. When the collective Social Cohesion of mothers were low, higher engagement with FLWs and the community had a positive relationship with DPT3 immunization of a child. With an increasing level of cohesiveness among mothers, this effect gradually attenuated and leading to a null level when the cohesiveness among mothers was highest (Fig. 3d). While we have identified literature independently supporting the positive association of social cohesion (Kim & Kawachi, 2017) and provider-parent interaction (Ames et al., 2017; Connors et al., 2017) with immunization, this study was first to report this type of heterogeneous effect modification of social capital. It might be the case that health workers had to proactively engage with those communities where the mothers' Social Cohesion is low to ensure immunization of the children. On the other hand, communities with higher Social Cohesion among mothers were able to organize themselves, ensuring child immunization irrespective of the level of FLW's interaction with them.
Historically, in rural India, gender-based discrimination, caste, and class hierarchies restricted people to avail benefits of the health services (Scott, George, Harvey, Mondal, Patel, & Sheikh, 2017; Singh, 2016). Thus, the strategy of health sector reforms in India primarily focused on developing a community-centered primary care system to reduce the barriers for access, utilization, and healthcare cost (Ministry of Health & Family Welfare, 2017; Rao, Arora, & Ghaffar, 2014). Some progress is evident as gender, religion, social caste, or class did not appear to influence the utilization of immunization service in our study.
Among household heads (who were mostly men), no covariates – including measures of social capital – presented any significant associations with DPT3 immunization. Previous studies in India and Uttar Pradesh also reported no male involvement in childhood immunization, whereas they generally participated in family planning, institutional delivery, antenatal, and postnatal care (Caleb-Varkey et al., 2004; Sahu et al., 2016). As immunization service is delivered within the community through VHNDs, the involvement of the household head may not be necessary to access or utilize the care.
4.2. Strengths and limitations of the study
This is the first study that included the social capital measure of both mother and household head to explore the contextual effect of social capital on child immunization. Applying multilevel analysis, we were able to distinguish the influence of individual and community level social capital. The use of a validated measurement scale and application of MCFA were significant steps forward to reduce measurement bias in the analysis. Moreover, having a strong theoretical underpinning with a holistic conceptual framework is the major strength of our study.
However, the result must be interpreted, considering some limitations. We only explored the correlation between social capital and DPT3 immunization. Any causal inference cannot be made due to the cross-sectional nature of the data. As the information source of immunization status, we considered mother's report for those children who did not have an available immunization card - which is the current standard of analysis (International Institute for Population Sciences & ICF, 2017). While we acknowledge the mother's reporting may have recall bias, excluding the self-reported data would lead to sample attrition and overestimation of the immunization coverage (Babalola, 2009). The study measured the current social capital of the respondents. However, the recall period for self-reported immunization status of the child was up to five years preceding the survey.
5. Conclusion
This study will significantly contribute to understanding the influence of social capital as a determinant of immunization in rural UP and further advancing the literature of social capital in India. The primary finding of the study indicated social capital – specifically mothers collective Social Cohesion – operates mainly at the community-level. It was also able to modify – both positively and negatively – the relationship of other social determinants of immunization.
As India is striving towards Universal Health Coverage, building cohesiveness and solidarity to promote health and equality became a core tenant of the central and the state government of UP (Ministry of Health & Family Welfare, 2017; National Informatics Centre (NIC), Ministry of Electronics & Information Technology, Government of India, 2018). Social capital or cohesiveness does not emerge in a vacuum. They are generated through social interaction among people, and reciprocally influence their everyday life. There is no cookie-cutter solution to build social capital in any context. So, more in-depth exploration is warranted to understand how social capital is generated within the complex social structure of rural UP. Building social cohesion may lead to significant positive externalities on the overall wellbeing and healthcare utilization. We recommend further research to explore the causal pathways between social capital and healthcare utilization, and the implications of synergistic and antagonistic effects of improving social capital as a health policy tool.
Funding
This work was supported by the HCL Foundation India (Grant Number- JHU: 124005). The funding organization did not have any participation in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Ethical approval
Ethical approval of the study was received from the Institutional Review Board Office of Johns Hopkins Bloomberg School of Public Health, Maryland, USA (IRB No: 00007469) and locally from the Center for Media Studies, New Delhi, India (IRB No: IRB00006230).
CRediT authorship contribution statement
Md Zabir Hasan: Conceptualization, Methodology, Formal analysis, Visualization, Writing - original draft. Lorraine T. Dean: Conceptualization, Methodology, Writing - review & editing. Caitlin E. Kennedy: Conceptualization, Writing - review & editing. Akshay Ahuja: Project administration, Writing - review & editing. Krishna D. Rao: Conceptualization, Methodology, Writing - review & editing. Shivam Gupta: Conceptualization, Supervision, Project administration, Funding acquisition, Writing - review & editing.
Declaration of competing interest
None.
Footnotes
DPT = Diphtheria–Pertussis–Tetanus, NFHS = National Family and Health Survey, UP = Uttar Pradesh, EPI = Expanded Program of Immunization, UIP = Universal Immunization Program, NHM = National Health Mission, FLWs = Frontline Workers, ASHA = Accredited Social Health Activist, VHSNC = Village Health, Sanitation and Nutrition Committee, AWW = Anganwadi Workers, VHND = Village Health Nutrition Day, WHO = World Health Organization, CSDH = Commission on Social Determinants of Health, GP = Gram Panchayat, SASCAT-I = Shortened and Adapted Social Capital Assessment Tool in India, MCFA = Multilevel Confirmatory Factor Analysis, PCA = Principal Components Analysis, COR= Crude Odds Ratio, AOR = Adjusted Odds Ratio, CI = Confidence Intervals, NIC = National Informatics Centre
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100545.
Contributor Information
Md Zabir Hasan, Email: mhasan10@jhu.edu, mhasan10@jhu.edu.
Lorraine T. Dean, Email: ldean9@jhu.edu.
Caitlin E. Kennedy, Email: caitlinkennedy@jhu.edu.
Akshay Ahuja, Email: ahuja_akshay@spp.ceu.edu.
Krishna D. Rao, Email: kdrao@jhu.edu.
Shivam Gupta, Email: sgupta23@jhu.edu.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Acharya P., Kismul H., Mapatano M.A., Hatløy A. Individual- and community-level determinants of child immunization in the democratic republic of Congo: A multilevel analysis. PloS One. 2018;13(8) doi: 10.1371/journal.pone.0202742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ames H.M., Glenton C., Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: A synthesis of qualitative evidence. Cochrane Database of Systematic Reviews. 2017;2017(2) doi: 10.1002/14651858.CD011787.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babalola S. Determinants of the uptake of the full dose of diphtheria–pertussis–tetanus vaccines (DPT3) in northern Nigeria: A multilevel analysis. Maternal and Child Health Journal. 2009;13(4):550–558. doi: 10.1007/s10995-008-0386-5. [DOI] [PubMed] [Google Scholar]
- Benin A.L., Wisler-Scher D.J., Colson E., Shapiro E.D., Holmboe E.S. Qualitative analysis of mothers' decision-making about vaccines for infants: The importance of trust. Pediatrics. 2006;117(5):1532–1541. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- Bourdieu P. The forms of capital. In: Richardson J., editor. Handbook of theory and research for the sociology of education. 1986. pp. 241–258.http://architecturalnetworks.research.mcgill.ca/assets/w06_bourdieu.pdf Greenwood. [Google Scholar]
- Buchan N.R., Croson R.T.A., Solnick S. Trust and gender: An examination of behavior and beliefs in the Investment Game. Journal of Economic Behavior & Organization. 2008;68(3):466–476. doi: 10.1016/j.jebo.2007.10.006. [DOI] [Google Scholar]
- Bults M., Beaujean D.J.M.A., Richardus J.H., Steenbergen J. E. van, Voeten H.A.C.M. Pandemic influenza A (H1N1) vaccination in The Netherlands: Parental reasoning underlying child vaccination choices. Vaccine. 2011;29(37):6226–6235. doi: 10.1016/j.vaccine.2011.06.075. [DOI] [PubMed] [Google Scholar]
- Caleb-Varkey L., Mishra A., Das A., Ottolenghi E., Huntington D., Adamchak S. Population Council; 2004. Involving men in maternity care in India. [DOI] [Google Scholar]
- Chuang Y.-C., Chuang K.-Y. Gender differences in relationships between social capital and individual smoking and drinking behavior in Taiwan. Social Science & Medicine. 2008;67(8):1321–1330. doi: 10.1016/j.socscimed.2008.06.033. [DOI] [PubMed] [Google Scholar]
- Commission on Social Determinants of Health . World Health Organization; 2005. Towards a conceptual framework for analysis and action on the social determinants of health: Discussion paper for the commission on the social determinants of health.https://www.who.int/social_determinants/resources/csdh_framework_action_05_07.pdf [Draft] [Google Scholar]
- Connors J.T., Slotwinski K.L., Hodges E.A. Provider-parent communication when discussing vaccines: A systematic review. Journal of Pediatric Nursing. 2017;33:10–15. doi: 10.1016/j.pedn.2016.11.002. [DOI] [PubMed] [Google Scholar]
- De Silva M.J., Huttly S.R., Harpham T., Kenward M.G. Social capital and mental health: A comparative analysis of four low income countries. Social Science & Medicine. 2007;64(1):5–20. doi: 10.1016/j.socscimed.2006.08.044. [DOI] [PubMed] [Google Scholar]
- Donfouet H.P.P., Mahieu P.-A. Community-based health insurance and social capital: A review. Health Economics Review. 2012;2(1):5. doi: 10.1186/2191-1991-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatiregun A.A., Etukiren E.E. Determinants of uptake of third doses of oral polio and DTP vaccines in the Ibadan North Local Government Area of Nigeria. International Health. 2014;6(3):213–224. doi: 10.1093/inthealth/ihu027. [DOI] [PubMed] [Google Scholar]
- Filmer D., Pritchett L.H. Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of India*. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Glatman-Freedman A., Nichols K. The effect of social determinants on immunization programs. Human Vaccines & Immunotherapeutics. 2012;8(3):293–301. doi: 10.4161/hv.19003. [DOI] [PubMed] [Google Scholar]
- Government of India Village health sanitation & nutrition committee (VHSNC) 2013. http://www.nhm.gov.in/communitisation/village-health-sanitation-nutrition-committee.html
- Graham H. Social determinants and their unequal distribution: Clarifying policy understandings. The Milbank Quarterly. 2004;82(1):101–124. doi: 10.1111/j.0887-378X.2004.00303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta P., Prakash D., Srivastava J.P. Determinants of immunization coverage in Lucknow district. North American Journal of Medical Sciences. 2015;7(2):36–40. doi: 10.4103/1947-2714.152076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan M.Z., Leoutsakos J.-M., Story W.T., Dean L.T., Rao K.D., Gupta S. Exploration of factor structure and measurement invariance by gender for a modified shortened adapted social capital assessment tool in India. Frontiers in Psychology. 2019;10:2641. doi: 10.3389/fpsyg.2019.02641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HCL Foundation . HCL; 2018. Project Samuday.http://www.hclfoundation.org/hcl-samuday [Google Scholar]
- International Institute for Population Sciences, & ICF . IIPS and ICF; 2017. India national family health survey NFHS-4 2015-16.http://dhsprogram.com/pubs/pdf/FR339/FR339.pdf [Google Scholar]
- Kawachi I., Subramanian S.V. Neighbourhood influences on health. Journal of Epidemiology & Community Health. 2007;61(1):3–4. doi: 10.1136/jech.2005.045203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Subramanian S.V., Kim D., editors. Social capital and health. Springer; 2008. [Google Scholar]
- Kim E.S., Kawachi I. Perceived neighborhood social cohesion and preventive healthcare use. American Journal of Preventive Medicine. 2017;53(2):e35–e40. doi: 10.1016/j.amepre.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahariya C. A brief history of vaccines & vaccination in India. Indian Journal of Medical Research. 2014;139(4):491–511. [PMC free article] [PubMed] [Google Scholar]
- Lindström M. Social capital and health-related behaviors. In: Kawachi I., Subramanian S.V., Kim D., editors. Social capital and health. Springer New York; 2008. pp. 215–238. [DOI] [Google Scholar]
- MacDonald S.E., Schopflocher D.P., Vaudry W. Parental concern about vaccine safety in Canadian children partially immunized at age 2: A multivariable model including system level factors. Human Vaccines & Immunotherapeutics. 2014;10(9):2603–2611. doi: 10.4161/21645515.2014.970075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldonado G., Greenland S. Simulation study of confounder-selection strategies. American Journal of Epidemiology. 1993;138(11):923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- Marmot M. Social determinants of health inequalities. 2005. http://www.ernaehrungsdenkwerkstatt.de/fileadmin/user_upload/EDWText/Personen/Marmot_Social_Inequalitites_Health_Lancet_365_1099_UCL.pdf 365(9464) [DOI] [PubMed]
- Ministry of Health & Family Welfare National health policy 2017. 2017. http://164.100.158.44/index1.php?lang=1&level=1&sublinkid=6471&lid=4270
- Ministry of Health and Family Welfare National rural health mission: Mission document. 2005. http://www.pbnrhm.org/docs/mission_doc.pdf
- Mitra T., Counts S., Pennebaker J.W. Understanding anti-vaccination attitudes in social Media. ICWSM. 2016:269–278. http://comp.social.gatech.edu/papers/icwsm16.vaccine.mitra.pdf [Google Scholar]
- Mohnen S.M., Groenewegen P.P., Völker B., Flap H. Neighborhood social capital and individual health. Social Science & Medicine. 2011;72(5):660–667. doi: 10.1016/j.socscimed.2010.12.004. [DOI] [PubMed] [Google Scholar]
- Muthén L.K., Muthén B.O. Muthén & Muthén; 2017. Mplus user's guide. [Google Scholar]
- National Informatics Centre (NIC), Ministry of Electronics & Information Technology, Government of India . National Portal of India; 2018. Ayushman Bharat—national health protection mission.https://www.india.gov.in/spotlight/ayushman-bharat-national-health-protection-mission [Google Scholar]
- Ozawa S., Clark S., Portnoy A., Grewal S., Brenzel L., Walker D.G. Return on investment from childhood immunization in low-and middle-income countries, 2011–20. Health Affairs. 2016;35(2):199–207. doi: 10.1377/hlthaff.2015.1086. [DOI] [PubMed] [Google Scholar]
- Putnam R.D. Bowling alone: America's declining social capital. Journal of Democracy. 1995;6(1):65–78. [Google Scholar]
- Rainey J.J., Watkins M., Ryman T.K., Sandhu P., Bo A., Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: Findings from a systematic review of the published literature. Vaccine. 2011;29(46):8215–8221. doi: 10.1016/j.vaccine.2011.08.096. 1999-2009. [DOI] [PubMed] [Google Scholar]
- Rao K.D., Arora R., Ghaffar A. Health systems research in the time of health system reform in India: A review. Health Research Policy and Systems. 2014;12:37. doi: 10.1186/1478-4505-12-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S., Annear P.L., Pathak S. The effect of Self-Help Groups on access to maternal health services: Evidence from rural India. International Journal for Equity in Health. 2013;12:36. doi: 10.1186/1475-9276-12-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu D., Dutta T., Kumar S., Mishra N.R., Neogi S., Mondal S. Effects of women's autonomy and male involvement on reproductive and child health (RCH) service utilization in Uttar Pradesh. Open Journal of Preventive Medicine. 2016;6(11):720–726. doi: 10.4236/ojpm.2016.611024. [DOI] [Google Scholar]
- Sahu D., Pradhan J., Jayachandran V., Khan N. Why immunization coverage fails to catch up in India? A community-based analysis. Child: Care, Health and Development. 2010;36(3):332–339. doi: 10.1111/j.1365-2214.2009.01003.x. [DOI] [PubMed] [Google Scholar]
- Scott K., George A.S., Harvey S.A., Mondal S., Patel G., Sheikh K. Negotiating power relations, gender equality, and collective agency: Are village health committees transformative social spaces in northern India? International Journal for Equity in Health. 2017;16(1):84. doi: 10.1186/s12939-017-0580-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott K., George A.S., Harvey S.A., Mondal S., Patel G., Ved R. Beyond form and functioning: Understanding how contextual factors influence village health committees in northern India. PloS One. 2017;12(8) doi: 10.1371/journal.pone.0182982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seid A.k., Hesse M., Bloomfield K. ‘Make it another for me and my mates’: Does social capital encourage risky drinking among the Danish general population? Scandinavian Journal of Public Health. 2015;44(3):240–248. doi: 10.1177/1403494815619536. [DOI] [PubMed] [Google Scholar]
- Shrivastwa N., Gillespie B.W., Kolenic G.E., Lepkowski J.M., Boulton M.L. Predictors of vaccination in India for children aged 12–36 months. American Journal of Preventive Medicine. 2015;49(6):S435–S444. doi: 10.1016/j.amepre.2015.05.008. [DOI] [PubMed] [Google Scholar]
- Singh P., editor. How solidarity works for Welfare: Subnationalism and social development in India. Cambridge University Press; Cambridge Core: 2016. Subnationalism and social development across Indian states; pp. 197–242. [DOI] [Google Scholar]
- Smith P.J., Marcuse E.K., Seward J.F., Zhao Z., Orenstein W.A. Children and adolescents unvaccinated against measles: Geographic clustering, parents' beliefs, and missed opportunities. Public Health Reports. 2015 doi: 10.1177/003335491513000512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sridhar S., Maleq N., Guillermet E., Colombini A., Gessner B.D. A systematic literature review of missed opportunities for immunization in low- and middle-income countries. Vaccine. 2014;32(51):6870–6879. doi: 10.1016/j.vaccine.2014.10.063. [DOI] [PubMed] [Google Scholar]
- StataCorp . StataCorp LLC; 2017. Stata statistical software: Release 15.https://www.stata.com/new-in-stata/ [Google Scholar]
- Story W.T. Social capital and the utilization of maternal and child health services in India: A multilevel analysis. Health & Place. 2014;28:73–84. doi: 10.1016/j.healthplace.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . UNICEF DATA; 2019, July. Vaccination and immunization statistics.https://data.unicef.org/topic/child-health/immunization/ [Google Scholar]
- Vikram K., Vanneman R., Desai S. Linkages between maternal education and childhood immunization in India. Social Science & Medicine. 2012;75(2):331–339. doi: 10.1016/j.socscimed.2012.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner A.L., Shenton L.M., Gillespie B.W., Mathew J.L., Boulton M.L. Assessing the timeliness of vaccine administration in children under five years in India, 2013. Vaccine. 2019;37(4):558–564. doi: 10.1016/j.vaccine.2018.12.035. [DOI] [PubMed] [Google Scholar]
- World Health Organization A conceptual framework for action on the social determinants of health: Debates, policy & practice, case studies. 2010. http://apps.who.int/iris/bitstream/10665/44489/1/9789241500852_eng.pdf (Paper 2)
- World Health Organization World health statistics 2018: Monitoring health for the SDGs. 2018. http://apps.who.int/iris/bitstream/handle/10665/272596/9789241565585-eng.pdf?ua=1
- World Health Organization . World Health Organization; 2019, July 15. 20 million children miss out on lifesaving measles, diphtheria and tetanus vaccines in 2018.https://www.who.int/news-room/detail/15-07-2019-20-million-children-miss-out-on-lifesaving-measles-diphtheria-and-tetanus-vaccines-in-2018 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.