Abstract
Calcaneus malunion is a common sequela to calcaneal fractures and is a cause of pain and discomfort. Multiple approaches have been described to address the subtalar joint and the lateral wall. Type 2 malunion is the most commonly encountered problem, and is usually addressed by the sinus tarsi approach. This has some limitations, as exposure for lateral wall excision beneath the peroneal tendons maybe a problem. We have slightly modified the sinus tarsi approach by a more horizontal skin incision, which may even be extended proximally by 1–2 cm; this allows access to the lateral wall on either side of the peroneal tendons. The approach is described in detail.
Keywords: Calcaneus malunion, Subtalar fusion, Sub fibular impingement-sinus tarsi approach
1. Introduction
The problems after calcaneus malunion are significant, and range from impingement, arthritis, deformity, widened heel, loss of calcaneal height and associated anterior ankle impingement.1 Although the subtalar joint was considered the primary pain generator in the past, we now know that other sites could have issues that cause significant disability. Nevertheless, the subtalar joint is the area most commonly subjected to surgical intervention, depending upon the type of malunion. Decision making requires a thorough examination, and identification of the actual cause/site of pain or discomfort. There is a need for good quality radiographs to evaluate subtalar arthritis, heel widening and subfibular impingement, as well as deformity of the calcaneus body.2 Focused fine cut CT scans help to understand the pathoanatomy, and define surgical options. Subtalar arthrodesis is invariably part of most planned corrective procedures, and the fusion along with exostectomy is sufficient in the majority of type 2 malunions as classified by Sanders3
The primary goals of a subtalar arthrodesis are pain relief; this is achieved by bony fusion, and restoration of hindfoot alignment, which allows increased mobility.4 Associated loss of heel height/grossly depressed posterior facet results in anterior ankle impingement, where a distraction arthrodesis is required to restore calcaneal height, pitch and talar dorsiflexion. Failure to recognize associated subfibular impingement due to lateral wall exostosis can lead to persisting pain even after isolated subtalar fusion.5
Presently, the commonly used approaches for the subtalar arthrodesis include the posterolateral, lateral extensile and the sinus tarsi approach.5 These approaches have their own advantages. A sinus tarsi approach causes minimal damage to adjacent soft tissues, allows adequate exposure of subtalar joint, without damage to the talocalcaneal ligaments and calcaneofibular ligaments,6 and allows access for resection of lateral wall deformity.7 For Sanders Type 3 malunions, extensile approach is better as it allows easier correction of severe hind foot deformity.6 However, in most Type 2 malunions such extensive dissection may not be necessary. To avoid the complications of the extensile approach, and to gain additional access to the lateral wall, we have modified the sinus tarsi approach. This not only allows good visualization of the subtalar joint, but also allows complete removal of the deformed lateral calcaneal wall by appropriate peroneal retraction. The incision is placed more horizontally, and is extended more proximally. This approach has the potential to damage the sural nerve proximally. As this approach allows unimpeded access to the peronei, it allows a comfortable relocation of these tendons which maybe an issue is some malunions. This approach is centered directly over the posterior subtalar facet and facilitates easy, thorough and meticulous joint preparation.
1.1. Surgical technique
- Step 1: Preoperative planning
-
-.Thorough clinical examination including swelling of the lateral hindfoot, painful subtalar range of motion and sinus tarsi tenderness is performed.
-
-.Exclusion of excessive heel valgus or varus; this approach should be used in Type 2 Malunions only.
-
-.Weight bearing radiographs of the foot (AP, oblique, lateral), to assess heel height and need for distraction; Brodens view (for visualization of the extent of arthritis in posterior facet), Harris axial view (for heel widening causing subfibular impingement), and a Saltzman view (for objectively assessing alignment of the calcaneus relative to the tibia).
-
-.CT scan is helpful in surgical planning.
-
-.
- Step 2: Patient Positioning
-
-.The patient is positioned in a lateral decubitus position on a radiolucent table, and the knee of the opposite limb beneath is flexed (Fig. 1).
-
-.A rectangular bolster is placed beneath the affected leg, and the operative foot should come till the edge of the table, facilitating the surgeon’s access from the foot end of the table.
-
-.Procedure is usually performed under regional anaesthesia with pneumatic tourniquet.
-
-.C-arm is positioned at the opposite end
-
-.Sterile painting with betadine and spirit is carried out; the knee is draped free for access to proximal tibia, if additional bone graft is needed. If tricortical graft use is anticipated, the ipsilateral iliac crest is prepared and draped.
-
-.
- Step 3: Skin Incision
-
-.Mark the lateral malleolus and the base of 4th metatarsal.
-
-.Start the skin incision just distal to tip of fibula and extend it distally for 3–4 cm towards base of 4th metatarsal. (Fig. 1). This has a more proximal extent and is slightly more transverse than the standard sinus tarsi approach. If required we can go more posteriorly behind the lateral malleolus, but we should be careful to identify and prevent sural nerve branches from injury.
-
-.
- Step 4: Approach
-
-.Elevate thick flaps, being aware of the proximity of the sural nerve.
-
-.Identify the peroneal tendons which lies directly beneath the skin incision and incise their covering sheath (Fig. 2); they are initially retracted down and posteriorly for exposure of subtalar joint
-
-.Incise the floor of peroneal sheath and we will be directly over the subtalar joint (Fig. 3). In case of joint distortion by an overhanging lateral wall, special care has to be taken, and a fluoroscopic image can be taken for identification of the subtalar joint.
-
-.Pass a 2.5 mm Kirschner wire through one hole of Hintermann retractor into the talus, superior and anterior to the posterior facet and parallel to it. Pass a second 2.5 mm Kirschner wire through the other hole of the Hintermann retractor into calcaneus posterior and inferior to the posterior facet and parallel to it (Fig. 4).
-
-.Identify the posterior facet of the joint, as this is crucial in subtalar fusion.
-
-.The capsule of the posterior facet is opened, exposing the subtalar joint. By gradual opening of Hintermann, the joint can be progressively opened, and the posterior capsule of the subtalar joint can be easily seen which can be incised to allow better opening of the joint.
-
-.All fatty and ligamentous tissue is debrided.
-
-.
- Step 5: Joint preparation
-
-.Care is taken to prevent injury to the peroneal tendons by proper retraction.
-
-.Sharp osteotomes are used to denude the cartilage from the posterior subtalar joint from both the talar and the calcaneal surfaces.
-
-.The osteotome should be used with care at the posteromedial edge of the joint, as the flexor hallucis longus tendon is in close proximity. Visualization of the flexor hallucis longus indicates good debridement of the joint surfaces. Special care should be taken to denude the medial joint, as failure to do so can result in residual valgus at subtalar joint. Use of Hintermann retractor easily permits access to deepest medial side of subtalar joint.
-
-.Debridement of the joint is done till presence of healthy, bleeding subchondral bone. It is important to maintain the shape of the joint and not remove excessive normal bone as it will cause difficulty in compression while fusion.
-
-.Irrigation of joint is to be done to remove debris and improve visualization.
-
-.Use of 1.8 mm drill bit with sleeve is used to drill multiple equally spaced drill holes in the raw surfaces to increase bleeding and exposure of marrow elements (Fig. 5).
-
-.The need for distraction is assessed; bone graft can be taken from the distal tibia, proximal tibia or the iliac crest as per need.
-
-.Use of burr is usually not recommended, due to issues with heat necrosis.
-
-.
- Step 6: Lateral wall Exostectomy
- -.
-
-.Use a periosteum elevator (or a curved broad osteotome) to elevate the soft tissues from the lateral wall
-
-.The lateral wall bump can be easily appreciated; if needed, this can be marked and predrilled with k wire, and the excessive bump can be removed using osteotome. The initial excision is done from posterior and superior part of lateral wall.
-
-.The tendons are then retracted upwards and proximally to evaluate the distal aspect of the lateral calcaneal wall, and excess bone is now removed. This bone can be used to aid fusion at the subtalar joint.
-
-.A finger should be easily inserted between to fibula and the calcaneus at the end of the procedure.
- Step 7: Reduction and Fixation
-
-.Subtalar fixation is usually done with cannulated cancellous screws. Partially threaded screws are used to achieve compression, when distraction is not done, In case of distraction arthrodesis, fully threaded screws are used after impacting the joint with graft, to maintain the heel height that is gained.
-
-.Guide wires are inserted through small stab incisions that are given over the posterior aspect of the heel.
-
-.The foot is held reduced in 50of valgus, taking care to avoid varus angulation
-
-.The first guidewire is inserted in the lateral half of the calcaneus, directed toward the body of the talus. The second guidewire is inserted in the medial half of the calcaneus, directed toward the neck of the talus. The guide wires are inserted under fluoroscopic guidance using lateral view, AP view and Harris axial view (Fig. 7).
-
-.Advance the guidewires through the calcaneus while visualizing where they exit the posterior facet through the distracted joint. The first wire should exit in the mid substance of the posterior facet, while the second should exit approximately 1 cm anterior to the first
-
-.The wires are inserted up to the subchondral bone of the talus.
-
-.Measure the required screw length and choose a screw 10 mm shorter than the measured length. The screws are inserted over the guide wires through the stab incisions. In exceptionally hard bone, it may be wise to use appropriate taps to avoid distraction of joint surfaces by the screw passage (Fig. 8). Some element of compression at the fusion site is desirable, but not at the cost of heel height loss.
-
-.Reduction of subtalar joint and length of screws should be confirmed on radiography (Fig. 9).
-
-.
- Step 8: Wound Closure
-
-.Irrigate wound with copious amount of normal saline.
-
-.Closure of the joint capsule followed by skin closure.
-
-.A back slab with ankle in neutral position is applied.
-
-.
Fig. 1.
Skin incision marking-starting from just distal to tip of fibula and extending it distally for 3–4 cm towards base of 4th metatarsal.
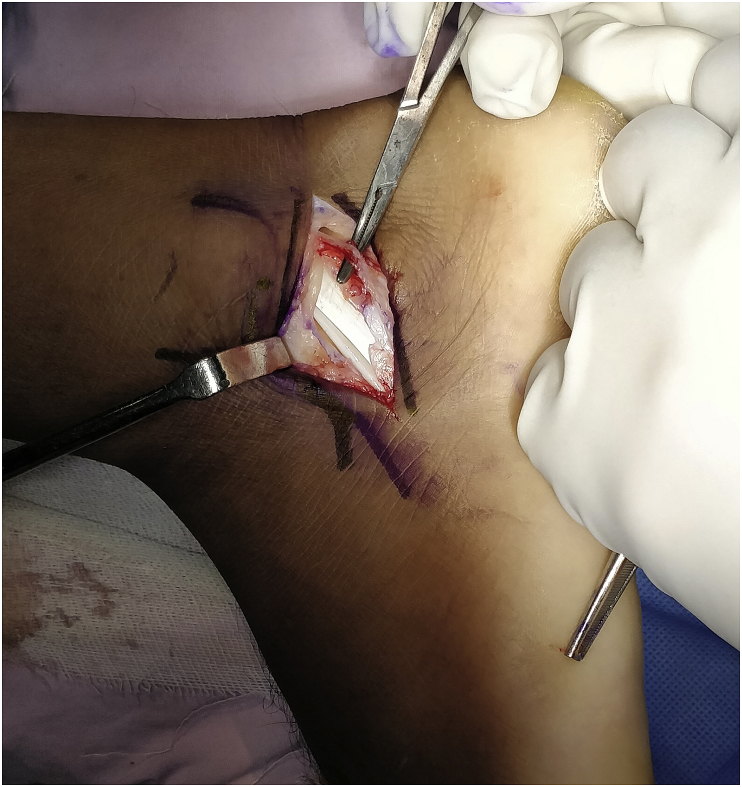
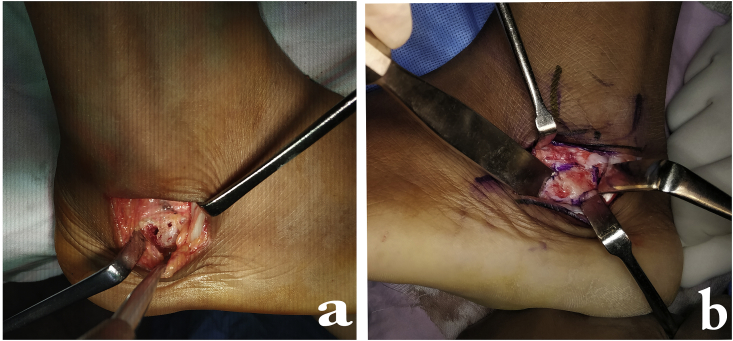
Fig. 2.
After incising the peroneal sheath, the peroneal tendons are visible.
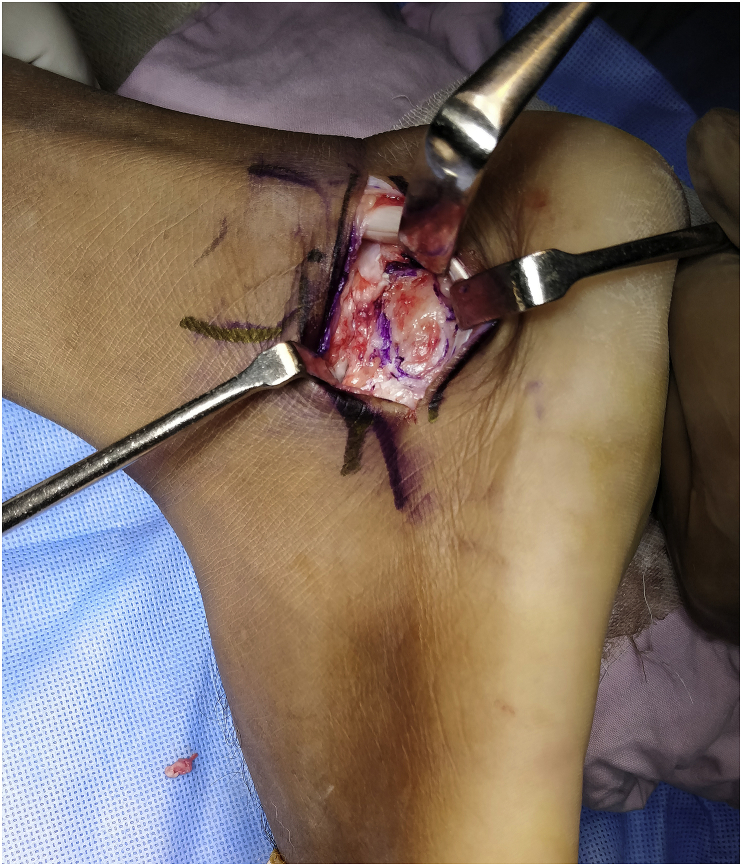
Fig. 3.
Peronei tendon retracted posteriorly after incising the floor of sheath.
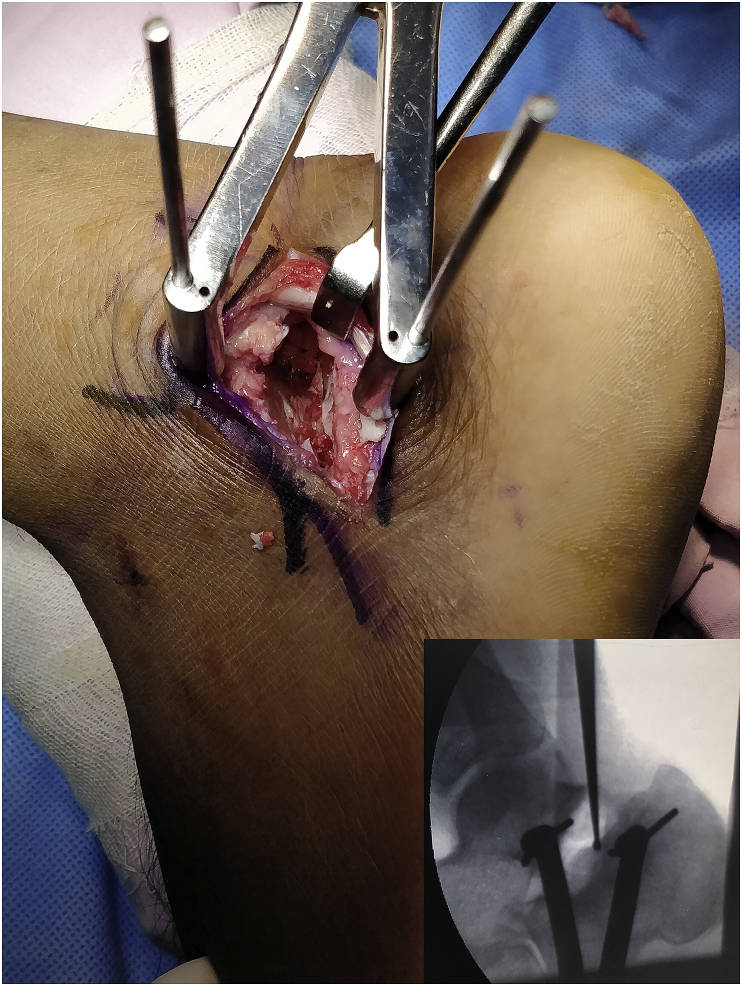
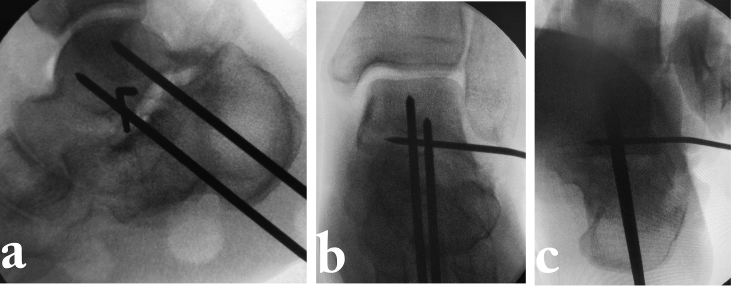
Fig. 4.
Exposure of the subtalar joint- Note the Peronei retracted posteriorly, Hintermann retractor applied with 1 K wire applied in talus and the other k wire into calcaneus (Inset- C arm picture depicting one k wire in either side of the posterior facet of subtalar joint).
Fig. 5.
Drilling of prepared joint surfaces with 2.0 mm k wire or 1.8 mm drill bit.
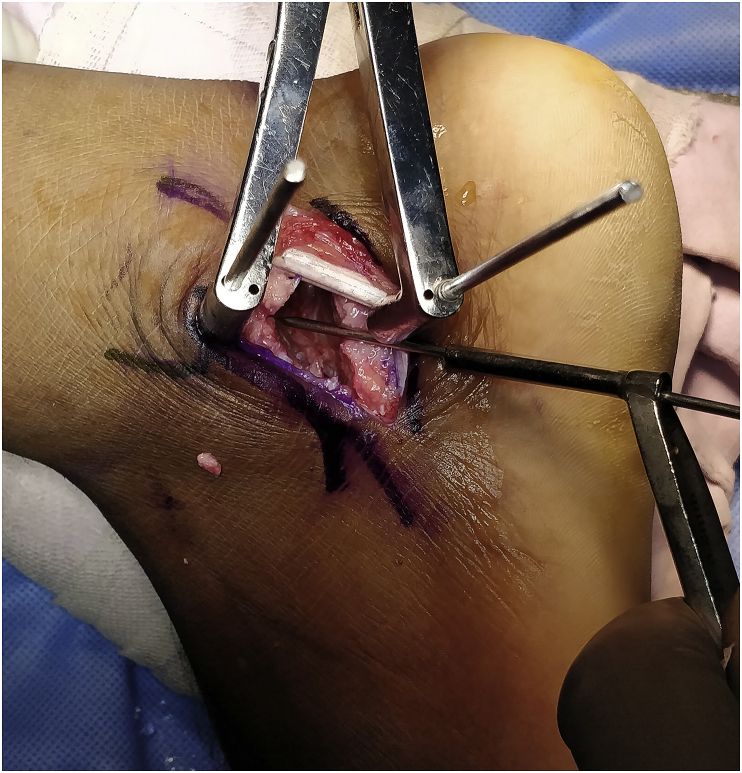
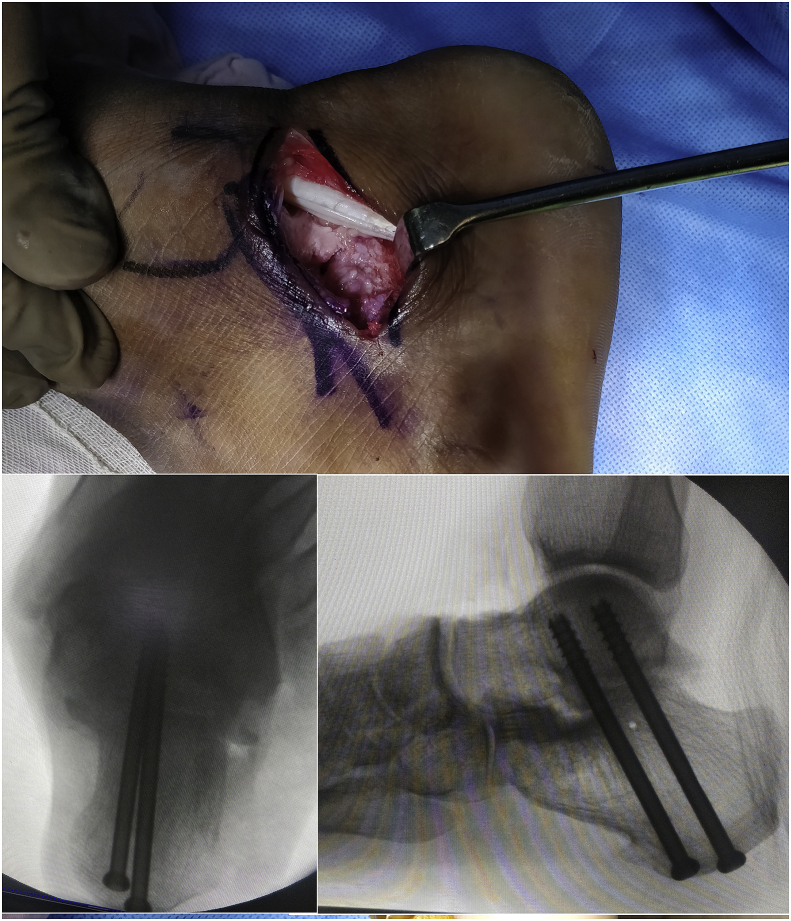
Fig. 6.
Exposure for lateral wall exostectomy. In Fig. 6A peronei are retracted anteriorly and the bump is visible. In Fig. 6B peronei are retracted posteriorly and the lateral wall bump is marked with marker and note the osteotome in position for exostectomy.
Fig. 7.
C arm Picture of two parallel adequately spaced and well centered guide wires with the tips in body of talus at subchondral area away from ankle joint line. 7A- Lateral view hind foot, 7B- AP view ankle and 7C harris axial view.
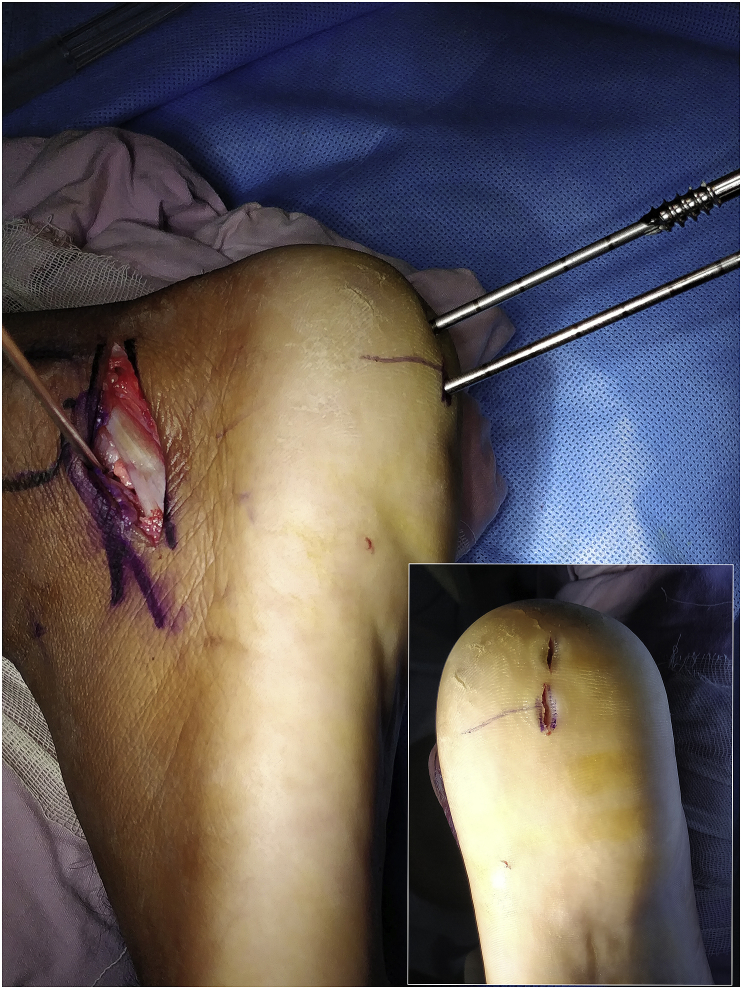
Fig. 8.
Note stab incisions in heel and the screw being advanced through parallel guide wires.
Fig. 9.
Obliteration of subtalar joint depicting good compression. (Inset-Final Harris view and lateral view of Hind foot after screw insertion and compression).
2. Post-operative care
-
-.
Back slab is applied till 7-10 days for soft tissue healing.
-
-.
Ankle Range of motion is started immediately after slab removal.
-
-.
Suture removal is done at 2 weeks (Fig. 10), following which patient is mobilized full weight bearing with aid of pneumatic Ankle Foot Orthosis.
Fig. 10.
Clinical image of foot after suture removal, note the small 3 cm healed scar.
3. Discussion
Calcaneus malunions are associated with post traumatic arthritis, lateral wall exostosis and subfibular impingement, anterior tibiotalar impingement and decreased motion at calcaneal-cuboid joint; additional varus hindfoot deformity in type 3 malunions leads to significant pain and disability.8,9 Type 2 malunions, with minimal varus can be treated well by subtalar arthrodesis and lateral wall exostectomy, which is associated with good functional outcomes and high fusion rates. The surgical factors influencing the efficacy of subtalar fusion are the operative approach, adequate cartilage removal, addition of bone graft, and stable fixation.10 The soft tissues in this area are especially sensitive to insult, and this is the reason for the decline of the extensile approach in both acute fracture fixations, and in late reconstructions. The selection of the operative approach plays a critical role in clearly exposing the subtalar joint, for removing cartilage, effectively protecting nerves and blood vessels, and preventing complications.7 In type 2 malunions, the approach should allow lateral wall excision and in Type 3 malunions, it should allow an additional calcaneal osteotomy for varus correction.
Gallie11 described subtalar fusion by a posterolateral approach; Carr et al.8 modified this approach to use a straight posterior incision. However it was not possible to debride the lateral wall to reduce the fibular impingement, release the calcaneocuboid joint, or reposition the subluxed and dislocated peroneal tendons. The main objective of their approach was to restore talocalcaneal height.
The most commonly used approach nowadays for calcaneal malunions is the extensile lateral approach. This approach provides extensive exposure, good exposure of subtalar joint, and can be used to correct severe hind foot deformity.6 However, it is associated with complications such as wound infection and reflex sympathetic dystrophy. Al-ashhab12 reported 2 cases of superficial wound infection and 3 cases of RSD in a series of 11 patients with otherwise excellent clinical results (Mean AOFAS score = 69). Clare et al.13 reported 93% fusion rates in 45 cases; however, 11 of them had wound infection of which 1 had deep infection and 29 (64%) had mild residual pain. Bednarz et al.14 reported good functional outcomes (96%) in a series of 29 cases, but documented 4 cases of nonunions and 2 varus malunions. Burton et al.15 reported satisfactory outcomes at an average follow up of 47 months in a series of 13 cases. Myerson and Quill1 utilized the subtalar distraction bone block fusion technique in 14 feet after calcaneal fracture. After an average 34-month follow-up, they graded their results as 7 good, 3 fair, and 4 poor. Poor outcomes were attributed to two varus malunions and two tibial nerve entrapments.
Isbister9 was the first to describe calcaneofibular abutment as a cause of pain in calcaneus malunion. Braly et al.16 evaluated lateral decompression without subtalar arthrodesis as a treatment alternative for malunited calcaneal fractures. They reported satisfactory results in 9 of the 11 patients at average follow up of 28 months. This is now classified as Type 1 malunion by Sanders, and constitutes a small number of cases encountered in real life.
The most common problem is a type 2 malunion; Our approach is a modification of sinus tarsi approach where in it helps to address the subtalar joint as well as the lateral wall. The advantage of the approach we use is multifold; it avoids damage to the lateral flap as it is less invasive, allows good subtalar joint exposure by using Hintermann retractors, and allows excision of the whole lateral wall by tendon retraction to anteriorly and posteriorly. Dislocating tendons can be replaced and the sheath stitched to address this problem. It is easy to do, limits damage to the lateral soft tissues and allows early mobilization. However, in severe cases needing a calcaneal corrective osteotomy, and those with involvement of calcaneocuboid joint, we prefer the extensile approach. The downside of proximal extension of the incision, even by 1–2 cm, is the risk of damage to the Sural nerve. This must be kept in mind, especially when working below the peronei, and careful identification and retraction are the key.
4. Conclusions
We present a minor modification of the sinus tarsi approach to allow subtalar fusion and lateral wall excision in type 2 calcaneal malunions. This is a simple approach, and allows good exposure; peroneal tendon pathology is easily addressed after excision of the lateral wall.
Contributor Information
Mandeep S. Dhillon, Email: drdhillon@gmail.com.
Sandeep Patel, Email: sandeepdrpatelortho@gmail.com.
Karan Jindal, Email: karan.121@hotmail.com.
Siddhartha Sharma, Email: sids82@gmail.com.
References
- 1.Myerson M.S., Quill G.E. Late complications of fractures of the calcaneus. J Bone Joint Surg. 1993;75A(3):331–341. doi: 10.2106/00004623-199303000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Ferrao P.N., Saragas N.P., Strydom A. Isolated subtalar arthrodesis. JBJS essential surgical techniques. 2016 Mar 23;6(1) doi: 10.2106/JBJS.ST.15.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stephens H.M., Sanders R. Calcaneal malunions: results of a prognostic computed tomography classification system. Foot Ankle Int. 1996 Jul;17(7):395–401. doi: 10.1177/107110079601700707. [DOI] [PubMed] [Google Scholar]
- 4.Greisberg J., Sangeorzan B. Hindfoot arthrodesis. J Am Acad Orthop Surg. 2007 Jan;15(1):65–71. doi: 10.5435/00124635-200701000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Vulcano E., Ellington J.K., Myerson M.S. The spectrum of indications for subtalar joint arthrodesis. Foot Ankle Clin. 2015 Jun;20(2):293–310. doi: 10.1016/j.fcl.2015.02.002. Epub 2015 Apr 11. [DOI] [PubMed] [Google Scholar]
- 6.Myerson M.S., Neufeld S.K., Uribe J. Fresh-frozen structural allografts in the foot and ankle. J Bone Joint Surg Am. 2005;87:113–120. doi: 10.2106/JBJS.C.01735. [DOI] [PubMed] [Google Scholar]
- 7.Savva N., Saxby T.S. In situ arthrodesis with lateral-wall ostectomy for the sequelae of fracture of the os calcis. J Bone Joint Surg Br. 2007;89:919–924. doi: 10.1302/0301-620X.89B7.18926. [DOI] [PubMed] [Google Scholar]
- 8.Carr J.B., Hansen S.T., Benirschke S.K. Subtalar distraction bone block fusion lor late complications of os calcis fractures. Foot Ankle. 1988;9:81–86. doi: 10.1177/107110078800900204. [DOI] [PubMed] [Google Scholar]
- 9.lsbister J.F. Calcaneo-fibular abutment following crush fracture of the calcaneus. J Bone Joint Surg Br. 1974;56:274–278. [PubMed] [Google Scholar]
- 10.Tuijthof G.J.M., Beimers L., Kerkhoffs G., Dankelman J., van Dijk C.N. Overview of subtalar arthrodesis techniques: options, pitfalls and solutions. J Foot Ankle Surg. 2010;16:107–116. doi: 10.1016/j.fas.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Gallie W.E. Subtalar arthrodesis in fracture of the os calcis. J Bone Joint Surg Am. 1943;25:731–736. [Google Scholar]
- 12.Al-Ashhab M.E. Treatment for calcaneal malunion. Eur J Orthop Surg Traumatol. 2013 Dec 1;23(8):961–966. doi: 10.1007/s00590-012-1110-0. [DOI] [PubMed] [Google Scholar]
- 13.Clare M.P., Lee W.E., Sanders R.W. Intermediate to long-term results of a treatment protocol for calcaneal fracture malunions. J Bone Joint Surg Am. 2005;87(5):963–973. doi: 10.2106/JBJS.C.01603. [DOI] [PubMed] [Google Scholar]
- 14.Bednarz P.A., Beals T.C., Manoli A. Subtalar distraction bone block fusion: an assessment of outcome. Foot Ankle Int. 1997;18:785–791. doi: 10.1177/107110079701801206. [DOI] [PubMed] [Google Scholar]
- 15.Burton D., Olney W., Horton G. Late results of subtalar distraction fusion. Foot Ankle Int. 1998;19(4):197–202. doi: 10.1177/107110079801900402. [DOI] [PubMed] [Google Scholar]
- 16.Braly G.W., Bishop J.O., Tullos H.S. Lateral decompression for malunited os calcis fractures. Foot Ankle. 1985;6(2):90–92. doi: 10.1177/107110078500600207. [DOI] [PubMed] [Google Scholar]