Abstract
Background
Numerous publications of the late 20th century have presented the radiological outcome of open technique for distal metatarsal osteotomy for mild to moderate hallux valgus and the clinical outcomes by means of well-established scoring systems which have been published and make these open techniques today’s benchmark and gold standard. Minimally invasive procedures reduce surgical trauma because they are performed without large incisions, and injury to the soft tissues is limited. This has the theoretical advantages of improved recovery and decreased rehabilitation times. There is however limited literature to prove the same for minimally invasive surgery for hallux valgus.
Our aim was thus to pool all available comparative literature on minimally invasive hallux valgus surgery done for mild to moderate hallux valgus versus open surgical approaches.
Methods
A PubMed, Embase and Scopus search was performed using the keywords (‘hallux valgus’ OR bunion) AND (‘minimally invasive’ OR percutaneous) AND osteotomy. A total of 473 records were identified and out of which nine studies were included in the final review.
Results
Most available studies are either randomized control trials, or prospective cohort studies providing good level of evidence. Radiological analysis showed similar correction with both MIS and open osteotomies. In functional analysis results were different with open techniques providing better results in terms of AOFAS score. (p < 0.0001). VAS score and complication rate were similar in both groups.
Discussion/conclusion
We conclude that based on available literature MIS provides equivalent radiological outcomes with respect to open surgery but functionally despite the promising results (good to excellent in most series), the outcomes in terms of function are not as good as open surgery. MIS techniques provide satisfactory outcomes for mild-to-moderate severity of hallux valgus though not as good as open surgery. There is evolving literature for this relatively new procedure. Longer duration of follow up and bigger numbers would allow for more meaningful data analysis and conclusions to be drawn as more studies come forward.
Keywords: Hallux valgus, Bunion, Foot deformity, Osteotomy, Minimally invasive surgery, Percutaneous surgery
1. Introduction
Hallux valgus is one of the most common deformities of the foot. Bunion is the most visible component of the deformity seen in this condition. Pain is associated with irritation of the dorsal cutaneous nerve of the great toe and bursal inflammation over the bunion. More than 150 different operative procedures have been described for the treatment of hallux valgus with none of them having proven superiority over the other.1
Numerous publications of the late 20th century have presented the radiological outcome of open technique for distal metatarsal osteotomy for mild to moderate hallux valgus2,3 and the clinical outcomes by means of well-established scoring systems4,5 have been published which makes these open techniques today’s benchmark and gold standard. More recent literature has shown these open approaches to the metatarsophalangeal (MTP) joint lead to soft tissue scarring and joint stiffness. Moreover, extensive bony exposure required for open procedures increases the risk of infection, osteonecrosis, and pain from hardware material6 Soft tissue scaring and cosmetically unappealing skin scars with open surgery have led to development of several minimally invasive techniques in recent years.7, 8, 9 Minimally invasive procedures reduce surgical trauma because they are performed without large incisions, and thus injury to the soft tissues is limited.
These minimally invasive techniques claim, as one of their advantages compared to open techniques, to have minor soft tissue complications. There is however not enough evidence to favor MIS over traditional open techniques which is largely due to the fact that the majority of studies are case series without comparison or control groups.10 Minimally invasive techniques are being adopted in all surgical specialties essentially because of the advantages of less operative trauma and preserving the blood supply of the healing soft tissues. This has the theoretical advantages of decreasing recovery and rehabilitation times. There is however limited literature to prove the same for minimally invasive surgery for hallux valgus.
Our aim was thus to pool all available comparative literature on minimally invasive hallux valgus surgery done for mild to moderate hallux valgus and present a meta-analysis which can conclusively prove which techniques provides superior function and radiological correction while simultaneously assessing other determinants of outcome including complication rates, operative time and other parameters.
2. Methods
A PubMed, Embase and Scopus search was performed using the keywords and Boolean operators (‘hallux valgus’ OR bunion) AND (‘minimally invasive’ OR percutaneous) AND osteotomy. Identification of studies was done independently by three review authors. The review was submitted for PROSPERO registration (ID 166659) and data extraction was performed using extraction forms with specified outcomes with at least two review authors. Flow diagram is presented for the number of studies included in Fig. 1. This systematic review and meta-analysis incorporates the PRISMA statement (http://www.prisma-statement.org/). Systematic literature search in electronic databases was done for 20 years to January 2020 using combinations of the keywords mentioned above.
Fig. 1.
Flow diagram showing method of shortlisting studies.
For all continuous data, mean, standard deviation and sample size was extracted for both the groups from each article included in the study. Number of events and sample size were recorded for categorical variables for both the groups. All data coded or selected for extraction were recorded in a table or spreadsheet as set out in the a-priori protocol. This included the data used in the synthesis for each study, e.g outcome metrics or effect size, and meta-data. Data coded or extracted from each study was cross checked by at least two independent reviewers. Any process for obtaining and confirming missing or unclear information or data from authors were also described before data analysis.
We used the following formula11 to have same measures for the meta-analysis. If the author reported the data as median, we converted the data using the formula below and used mean and standard deviation for meta-analysis for all continuous variables.
Each eligible publication was carefully checked in order to identify additional records. Duplicate articles were removed and abstract was assessed based on inclusion and exclusion criteria. Three authors independently read the full manuscript and judged on the basis of inclusion and exclusion criteria to finally include in systematic review. In case of any disagreement, all of the authors discussed the reasons for their decisions and a final decision was made by consensus using Delphi Method. Quantitative data synthesis was used for included studies that are sufficiently homogenous in nature.
Quantitative studies were combined based on each outcome and summarized through meta-analysis using RevMan 5.0 software. Odds Ratio (OR) with 95% Confidence Interval (CI) & Mean Difference (MD) with 95% CI were presented including forest plots.
2.1. Risk of bias assessment
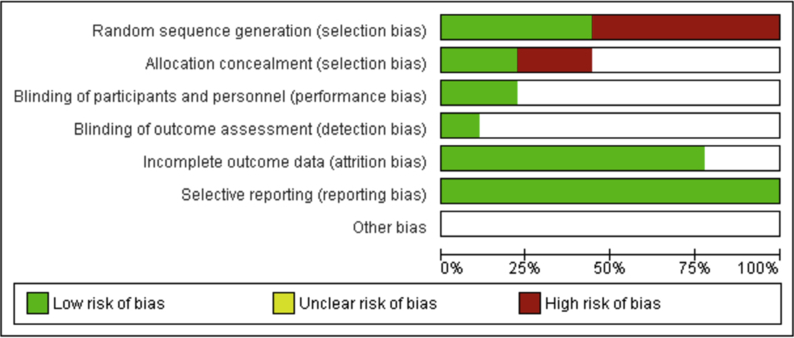
The modified Cochrane Collaboration tool was used to assess risk of bias for randomized controlled trials as well as retrospective cohort studies. Risk of bias graph and risk of bias summary is presented in Fig. 2(a) and Fig. 2(b) respectively. Also the forest plot for comparing IMA in both the groups is presented (see Fig. 3).
Fig. 2a.
Risk of Bias graph.
Fig. 2b.
Risk of bias summary.
Fig. 3.
Forest plot for comparing IMA in both the groups (MIS vs OPEN).
3. Results
A total of 473 records were identified and out of which nine studies were included in the final review after removing duplicates, screening abstracts, and obtaining full texts. A flowchart of the studies included in this review is presented in Fig. 1. Three independent reviewers screened the articles based on inclusion and exclusion criteria excluded duplicates. In case of discrepancy Delphi method was used to reach a consensus. Of the records excluded 124 were not relevant, five were in languages other than English and 179 didn’t have a comparative group, 39 had a different Intervention (Minimally invasive Distal Metatarsal Osteotomies for Hallux valgus), 60 didn’t have clinical and radiological outcomes of interest and 45 were case series. The results of these studies are summarized in Table 1, Table 2. The references from each of the selected studies were also reviewed in an attempt to locate additional relevant reports that were not identified during the initial PubMed search. The data from these 9 studies were compiled and subsequently analyzed, with particular emphasis placed on the basic demographic data, level of evidence provided, MIS and open technique used, radiological outcomes, functional outcomes and complication rate (Table 1, Table 2).
Table 1.
Demographic analysis of studies included for final analysis.
| Author (year) | Feet number (at final FU) | Mean Age (years) | Mean FU (months) | Study design | Females | MIS technique used |
|---|---|---|---|---|---|---|
| Maffuli (2009) | 36 MIS 36 Open | 51.5 ± 3.1y for Open and 52.6± 3y for MIS | 30 m (25.2m–38.4 m) | Retrospective cohort | 56/59 MIS and 93/102 open | Bosch technique |
| Radwan (2012) | 29 MIS 31 Open | 32.7 ± 7.4y for MIS and 35.7 ± 6.9y for open | 21.7 m for MIS group and 19.5 m months for open group (range 12–36 months) | RCT | 25/28 forMIS and 28/31 for open | Percutaneous distal metatarsal osteotomy |
| Giannini (2013) | 20 MIS 20 Open | 53 ± 11y | 84 m for both | RCT | 20/20 MIS and 20/20 Open | Krammer/SERI technique |
| Brogan (2016) | 49 MIS 32 Open | 53 ± 10.8y MIS and 57 ± 10.9y open | 31 m months MIS 37 m months Open | Retrospective cohort | 46/49 MIS and 32/32 Open | Percutaneous chevron |
| Lee (2017) | 25 MIS 25 Open | 52.6 (range, 20–76) for MIS and 53.4 (range, 25–75) for open | 6 months (both groups) | RCT | 23/25 MIS and 22/25 open | Percutaneous chevron + Akin |
| Lai (2017) | 29 MIS 58 Open | 54.3 ± 12.8y for MIS and 54.3 ± 12.7y for open | 24 months (both groups) | Retrospective cohort | 25/29 MIS 52/58 Open | Percutaneous chevron + Akin |
| Kaufmann (2018) | 25 MIS 22 Open | 44 ± 12y for Open and 52 ± 7y for MIS | 9 months | RCT | 21/25 MIS and 19/22 Open | Percutaneous chevron |
| Boksh (2018) | 16 MIS 21 Open | 46 ± 13.2 years for Open and 52.2 ± 14.0 years for MIS | 28 ± 12.2 months | Prospective cohort | NS | Mini scarf |
| Poggio (2015) | 69 MIS and 133 Open | 62.5y±8.9 for MIS and 52.9y±(10.0) for open | 12 months (both groups) | Retrospective cohort | 56/59 MIS and 93/102 Open | Krammer/SERI technique |
Table 2.
Compiled summary of results of included studies.
| Author |
Mean AOFAS score |
Mean Intermetatarsal angle (IMA) |
Mean VAS score |
Mean Hallux Valgus Angle (HVA) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop AOFAS score MIS group | Postop AOFAS score MIS group | Preop AOFAS score Open group | Postop AOFAS score Open group | Preop MIS group | Postop MIS group | Preop Open Group | Postop Open group | Preop VAS score | Postop VAS score MIS group | Postop VAS score Open group | Preop MIS group | Postop MIS group | Preop Open Group | Postop Open group | |
| Radwan (2012) | NS | NS | NS | NS | 12.5 | 7.79 | 12.03 | 8.23 | NS | NS | NS | 27.59 | 13.14 (2.83) | 26.13 | 12.84 |
| Kaufmann (2018) | 65 | 90 | 66.5 | 90 | 14 | 15.15 | 6 | 1 | 0 | 26.4 | 6.9 | 28.25 | 8.5 | ||
| Brogan (2016) | – | – | 11.7 | 6.8 | 13.4 | 6.7 | NS | NS | NS | 26.6 | 10.4 (5.7) | 30.8 | 9.9 | ||
| Lai (2017) | 58.6 | 87.4 | 53.2 | 88.4 | 14.6 | 14.6 | 4.9 | 0.7 | 0.4 | 29.9 | 8.8 | 30.6 | 13.8 | ||
| Lee (2017) | 61.3 | 88.7 | 58.5 | 83 | 15.6 | 6.4 | 15.7 | 7.6 | 6.9 | 0.3 | 0.5 | 31.4 | 7.6 (1.2) | 31.2 | 10.1 |
| Boksh (2018) | 10 | 3.38 | 5.4 | NS | NS | NS | 24.4 | 10.9 | 35.4 | 12.6 | |||||
| Maffulli (2009) | 54 | 85 | 51 | 86 | 15 | 8 | 14 | 8 | NS | NS | NS | 27 | 17 (4) | 28 | 20 |
| Giannini (2013) | 51 | 81.2 | 48 | 77.6 | 16.1+ - 3.9 | 6.8 + - 4.3 | 16.1 + - 3.8 | 8.3 + - 3.4 | NS | NS | NS | 35.8 + - 3.5 | 21.8+ - 4.1 | 35.5 + - 4.7 | 20.1 + - 3.6 |
| Poggio (2015) | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
NS=Not Specified.
Of the included studies, highest level of evidence has been provided by Kauffman, Radwan, Lee et al. and Giannini et al. who conducted a randomized control trial.10,12, 13, 14 Boksh et al. conducted a prospective cohort study.15 The study by Lai et al.,5 Maffuli7 and Brogan (16) are retrospective cohort studies whereas Poggio et al. did a retrospective analysis of two independent patient cohorts.16, 17, 18, 19
3.1. Demography
Most patients included in studies are females (512/666 patients 76.9%) as hallux valgus is more prevalent in females. In the analysis of 20 bilateral hallux valgus by Gianinni et al. with one side undergoing MIS and the other side open surgery, all 20 patients were female.14 The follow-up duration is extremely variable between studies with Lee et al. doing an analysis at 6 months while Gianini et al. analyzed their results for all patients at 8 years follow-up.13,14 The mean age in most studies ranges from 40 to 60 years with the exception of Radwan et al. where the mean age is 32.7 years for MIS group and 35.7 years for open which is younger than all other studies.12
3.2. Surgical technique
The surgical techniques for the included studies despite the mild differences are grossly similar and all studies have used distal metatarsal osteotomies in their percutaneous technique. The SERI technique (Simple Effective Rapid and Inexpensive) technique which is also called the Krammer technique is a type of percutaneous distal metatarsal osteotomy. The technique has been compared to open scarf technique by Giannini et al. (14) in their study published in 2013 where they have compared it to open scarf osteotomy in 20 patients. Poggio et al. also retrospectively compared SERI to a cohort of 133 scarf osteotomy feet in their analysis (2015).19 Boksh et al. have compared mini-scarf with open scarf.15
Kauffman, Brogan, Lai and Lee et al. have used the percutaneous chevron osteotomy in their comparison with open technique where Kauffman and Lee et al. have conducted their analysis prospectively while Lai el al have done a retrospective cohort analysis.10,13,16,17 Lai and Lee et al. have added percutaneous Akins’ to their osteotomies to correct the interphalangeal component of the deformity.13,17 This has been referred to as the PECA technique. Maffuli et al. have used the Bosch technique in their study which is similar to the distal metatarsal osteotomy used by Radwan et al.12,18
-
1.
Radiological analysis
Since most studies have included patients with different preoperative characteristics in the form of radiological severity as assessed by their preoperative Hallux Valgus angle (HVA), Intermetatarsal angle (IMA), and Distal metatarsal articular angle (DMAA); we decided to find out difference between postoperative and preoperative IMA and HVA which suggests a change or improvement in the radiological parameters.
-
a.
Analysis of change in Intermetatarsal angle (IMA)
Eight studies were reported comparison of IMA between MIS and OPEN group. We combined the results in the form of mean difference (MD). Fig. 1 shows the pooled estimate which was not found to be significant (MD = 0.20; 95%CI: 0.70 – 1.10; I2 = 74.0%; p = 0.660). Hence the pooled results are comparable between MIS and open groups with no significant.
-
b.
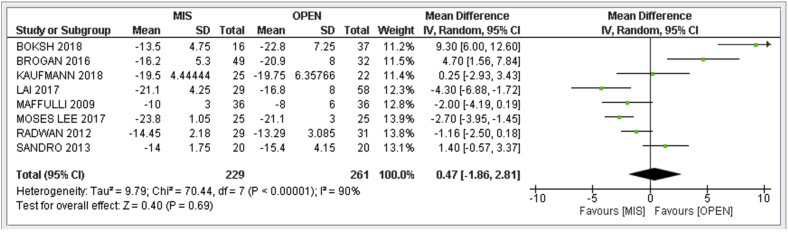
Analysis of change in hallux valgus angle (HVA)
Similarly, after pooling eight studies data for HVA comparing two groups, the pooled mean difference was not found to be significant (MD = 0.47; 95%CI: 1.86 – 2.81; I2 = 90%; p = 0.690) (Fig. 4).
-
2.Functional analysis
-
a.Analysis of VAS score
-
a.
Fig. 4.
Forest plot for comparing HVA in both the groups (MIS vs OPEN).
Fig. 5 depicts the forest plot for VAS score. The pooled mean difference was not found to be significant (MD = 0.80; 95%CI: 0.58 – 2.19; I2 = 86%; p = 0.260). Three articles reported VAS score.1,3,6 The combined result show no major difference between the two groups and comparable VAS between MIS and Open group.
-
b.
Analysis of AOFAS score
Fig. 5.
Forest plot for comparing VAS in both the groups (MIS vs OPEN).
Six studies were combined and forest plot is presented in Fig. 6 for AOFAS score. The pooled mean difference was found to be statistically significant (MD = −4.87; 95%CI: 7.06 to −2.68; I2 = 31%; p < 0.0001) with open techniques have better AOFAS score as compared to MIS.
Fig. 6.
Forest plot for comparing AOFAS in both the groups (MIS vs OPEN).
4. Analysis of difference in complication rate
Fig. 7 represents the forest plot of complications with eight studies. Different studies reported different complications such as pin tract infection, skin irritation and paraesthesia in MIS group. Similarly complications like wound dehiscence, metatarsalgia and recurrence for open technique. We counted number of complications reported by each article and did the meta-analysis. The pooled relative risk for complications was not found to be significantly different for different groups (RR = 1.91; 95%CI: 0.79–4.62; I2 = 62%; p = 0.150).
Fig. 8.
Forest plot for comparing satisfaction level in both the groups (MIS vs OPEN).
Fig. 7.
Forest plot for comparing complications in both the groups (MIS vs OPEN).
Four studies reported satisfaction level in terms of four scale i.e completely satisfied (very satisfied), satisfied with minor reservation (satisfied), satisfied with major reservation (don’t know) and dissatisfied (not satisfied). We counted satisfied numbers by combining first two categories and estimated the pooled relative risk for complications which was not found to be significant (RR = 1.01; 95% CI: 0.95–1.08; I2 = 0.0%; p = 0.690) (Fig 8).
5. Analysis for duration of surgery
Four studies were combined for duration of surgery.12,14,17,20 Fig. 9 depicts the forest plot for duration of surgery. The pooled mean difference was found to be statistically significant (MD = −14.23; 95%CI: 18.81 to −9.64; I2 = 85%; p < 0.00001) and the pooled results show that duration of surgery is less in MIS group as compared to open group.
Fig. 9.
Forest plot for comparing duration of surgery in both the groups (MIS vs OPEN).
6. Discussion
The surgical correction of hallux valgus presents more than 150 different operative techniques. Minimally invasive surgery for the management of patients with hallux valgus is increasingly common, including arthroscopic, minimal approach and percutaneous methods.18 Percutaneous surgery is performed through the smallest possible working incision without direct visualization of the underlying target structures, using a mini-blade for soft tissue incision, a power rotatory burr for bony procedures under intraoperative fluoroscopy control.21 The aim of this paper is to review and analyze the available literature comparing percutaneous surgical management with the conventional open techniques of hallux valgus correction to highlight strengths and weakness of these techniques and at the same time provide a sum up of comparison between these two methods.
Most cases studied by authors had mild to moderate type of hallux valgus which made them amenable to MIS approaches requiring correction by soft tissue bunion releases and osteotomy that can be controlled with minimal approach and percutaneous methods. Our inclusion and exclusion criteria have been specially restrictive, in order to include only those studies that have compared MIS distal metatarsal osteotomy with traditional open approaches and simultaneously deduce the variables deriving from surgical techniques performed and their outcomes.
There are several important points of discussion retrieved from our literature review. One of these is the outcomes as we have done a detailed analysis of the clinical and radiological outcomes at the described follow-up were substantially comparable to the minimally invasive techniques available as well as a demographic description of the available comparative studies on their essential characteristics.
The follow-up duration is variable and ranges from 6 months (Lee at al) to 7 years in the study done by Giannini et al.13,14 But the study by Kaufmann et al. shows that outcome stabilizes after 3 months (10) and the AOFAS score deteriorates between 2 year and 7 years follow-up as found by Giannini et al.14 Case selection was rather straightforward in the study by Giannini et al. (2013) where they have included bilateral hallux valgus and have operated one side by MIS (SERI technique) and the other side by open scarf osteotomy. In more recent studies Kaufmann, Lee and Radwan et al. have randomized feet into either MIS or Open surgery.10,12,13 Brogan et al. have specified that initial patients were managed with open scarf surgery and as their experience evolved they moved to minimally invasive scarf osteotomy.16 Maffuli et al. mention that the surgeries performed by the lead author are done using minimally invasive Bosch technique while the other authors have performed open scarf surgeries that have been used for their comparison.20 Lai et al. mention a similar method of choosing between open and MIS techniques.17 Boksh et al. (miniscarf vs open scarf) and Poggio et al. (SERI vs scarf) have not specified how the cases were divided amongst the two groups in their methodology.15,19
For functional assessment, most common outcome evaluation tool for hallux valgus surgery is the AOFAS score while authors have also chosen subjective patient satisfaction and VAS score. AOFAS rating system has been developed by the American Orthopaedic Foot and Ankle Society to provide a standard method of reporting clinical status of the ankle and foot and is universally accepted. The systems incorporate both subjective and objective factors into numerical scales to describe function, alignment, and pain.22 Moreover there is literature to show that assessment of satisfaction closely correlates with functional outcome and several authors have assessed the same as an outcome measure.6,10,12,13,16
Radiological analysis included for our analysis is hallux valgus angle and intermetatarsal angle. These 2 radiological parameters have been uniformly assessed by authors as they not only quantify the deformity but also guides management. Distal first metatarsal osteotomies traditionally have been indicated for correction of mild-to-moderate deformities with an intermetatarsal angle (IMA) as much as 20 and for correction of the distal metatarsal articular angle (DMAA).2
Our pooled results show that radiologically MIS techniques provide equivalent radiological correction as compared to traditional open approaches. In relation to the functional analysis, AOFAS score of open surgery was found to be better than MIS in the analysis (p < 0.0001). While most authors state that AOFAS score in MIS and open techniques are comparable, their pooled results are somewhat different. The overall result shows that MIS doesn’t provide equivalent AOFAS score in comparison to open approaches. This is a significant finding that despite comparable radiological parameters post operatively the AOFAS scores at final follow-up are significantly better in the open group. In terms of VAS and patient satisfaction both groups are similar. The complication risk has also been assessed among both groups in all studies provided and they appear equivalent statistically. Duration of surgery has been studied in 4 studies and duration for MIS is statistically lesser with respect to open surgery.
The limitation in our analysis lies in the heterogeneity of the surgical techniques used both in MIS and open group. However we have included only distal osteotomies done for hallux valgus of mild to moderate severity. The number of studies doing this analysis is only nine. Also scores at final analysis may bias the findings as timing final analysis is different for different studies ranging up to 7 years by Giannini et al.
Literature shows that MIS techniques are on the rise but the efficiency of correction, as well as the clinical outcome of these minimally invasive techniques have not been conclusively proven. While most studies present a good clinical and radiological outcome, Romero et al. have found insufficient radiographic correction.23 However even they report low post-operative pain levels and high patient satisfaction with MIS. In the systematic review of minimally invasive hallux surgery by Caravelli et al., a clear recommendation has not been made although they state that early results of multiple studies are encouraging24
Our literature review and meta-analysis has included more recent literature and we feel to be in a position to make a consensus statement with regards to management of hallux valgus with minimally invasive surgery. We conclude that MIS provides equivalent radiological outcomes with respect to open surgery but functionally despite the promising results (good to excellent in most series), the outcomes in terms of function are not as good as open surgery. The inherent bias against minimally invasive hallux valgus surgery is thus partially justified but MIS techniques provide satisfactory outcomes for mild-to-moderate severity of hallux valgus though not as good as open surgery. There is evolving literature for this relatively new procedure. Longer duration of follow up and bigger numbers would allow for more meaningful data analysis and conclusions to be drawn as more studies come forward.
Declaration of competing interest
There are no conflicts of interest.
References
- 1.Coughlin M.J., Jones C.P. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007 Jul;28(7):759–777. doi: 10.3113/FAI.2007.0759. http://journals.sagepub.com/doi/10.3113/FAI.2007.0759 [Internet] [cited 2020 Feb 21]. Available from. [DOI] [PubMed] [Google Scholar]
- 2.Oh I.S., Kim M.K., Lim K.Y., Bae J.H. Modified technique of distal metatarsal osteotomy for hallux valgus. Foot Ankle Int. 2007 Apr;28(4):527–528. doi: 10.3113/FAI.2007.0527. http://journals.sagepub.com/doi/10.3113/FAI.2007.0527 [Internet] [cited 2020 Feb 17]. Available from. [DOI] [PubMed] [Google Scholar]
- 3.Choi W.J., Yoon H.K., Yoon H.S., Kim B.S., Lee J.W. Comparison of the proximal chevron and ludloff osteotomies for the correction of hallux valgus. Foot Ankle Int. 2009 Dec;30(12):1154–1160. doi: 10.3113/FAI.2009.1154. http://journals.sagepub.com/doi/10.3113/FAI.2009.1154 [Internet] [cited 2020 Feb 21]. Available from. [DOI] [PubMed] [Google Scholar]
- 4.Thordarson D., Ebramzadeh E., Moorthy M., Lee J., Rudicel S. Correlation of hallux valgus surgical outcome with AOFAS forefoot score and radiological parameters. Foot Ankle Int. 2005 Feb;26(2):122–127. doi: 10.1177/107110070502600202. http://journals.sagepub.com/doi/10.1177/107110070502600202 [Internet] [cited 2020 Feb 21]. Available from. [DOI] [PubMed] [Google Scholar]
- 5.Park C.-H., Jang J.-H., Lee S.-H., Lee W.-C. A comparison of proximal and distal chevron osteotomy for the correction of moderate hallux valgus deformity. The Bone & Joint Journal. 2013 May;95–B(5):649–656. doi: 10.1302/0301-620X.95B5.30181. http://online.boneandjoint.org.uk/doi/10.1302/0301-620X.95B5.30181 [Internet] [cited 2020 Feb 21]. Available from. [DOI] [PubMed] [Google Scholar]
- 6.Vopat B.G., Lareau C.R., Johnson J., Reinert S.E., DiGiovanni C.W. Comparative Study of Scarf and Extended Chevron Osteotomies for Correction of Hallux Valgus [Internet] Foot & Ankle Specialist. 2013 Dec;6(6):409–416. doi: 10.1177/1938640013508431. http://journals.sagepub.com/doi/10.1177/1938640013508431 [cited 2020 Feb 17] [DOI] [PubMed] [Google Scholar]
- 7.Jowett C.R.J., Bedi H.S. Preliminary results and learning curve of the minimally invasive chevron akin operation for hallux valgus. J Foot Ankle Surg. 2017 May;56(3):445–452. doi: 10.1053/j.jfas.2017.01.002. https://linkinghub.elsevier.com/retrieve/pii/S1067251617300029 [Internet] [cited 2020 Feb 21]. Available from. [DOI] [PubMed] [Google Scholar]
- 8.Brogan K., Voller T., Gee C., Borbely T., Palmer S. Third-generation minimally invasive correction of hallux valgus: technique and early outcomes. Int Orthop. 2014 Oct;38(10):2115–2121. doi: 10.1007/s00264-014-2500-1. http://link.springer.com/10.1007/s00264-014-2500-1 (SICOT) [Internet] [cited 2020 Feb 21]. Available from. [DOI] [PubMed] [Google Scholar]
- 9.Redfern D., Perera A.M. Minimally invasive osteotomies. Foot Ankle Clin. 2014 Jun;19(2):181–189. doi: 10.1016/j.fcl.2014.02.002. https://linkinghub.elsevier.com/retrieve/pii/S108375151400014X [Internet] [cited 2020 Feb 21]. Available from. [DOI] [PubMed] [Google Scholar]
- 10.Kaufmann G., Dammerer D., Heyenbrock F., Braito M., Moertlbauer L., Liebensteiner M. Minimally invasive versus open chevron osteotomy for hallux valgus correction: a randomized controlled trial. Int Orthop. 2019 Feb;43(2):343–350. doi: 10.1007/s00264-018-4006-8. http://link.springer.com/10.1007/s00264-018-4006-8 [Internet] [cited 2020 Feb 14]. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014 Dec;14(1):135. doi: 10.1186/1471-2288-14-135. http://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-14-135 [Internet] [cited 2020 Feb 21]. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Radwan Y.A., Mansour A.M.R. Percutaneous distal metatarsal osteotomy versus distal chevron osteotomy for correction of mild-to-moderate hallux valgus deformity. Arch Orthop Trauma Surg. 2012 Nov;132(11):1539–1546. doi: 10.1007/s00402-012-1585-5. http://link.springer.com/10.1007/s00402-012-1585-5 [Internet] [cited 2020 Feb 14]. Available from. [DOI] [PubMed] [Google Scholar]
- 13.Lee K., Park Y., Jegal H., Kim K., Young K., Kim J. Factors associated with recurrent fifth metatarsal stress fracture. Foot Ankle Int. 2013 Dec;34(12):1645–1653. doi: 10.1177/1071100713507903. [DOI] [PubMed] [Google Scholar]
- 14.Giannini S., Cavallo M., Faldini C., Luciani D., Vannini F. The SERI distal metatarsal osteotomy and scarf osteotomy provide similar correction of hallux valgus. Clin Orthop Relat Res. 2013 Jul;471(7):2305–2311. doi: 10.1007/s11999-013-2912-z. http://link.springer.com/10.1007/s11999-013-2912-z [Internet] [cited 2020 Feb 14]. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boksh K., Qasim S., Khan K., Tomlinson C., Mangwani J. A comparative study of mini-scarf versus standard scarf osteotomy for hallux valgus correction. J Foot Ankle Surg. 2018 Sep;57(5):948–951. doi: 10.1053/j.jfas.2018.03.039. https://linkinghub.elsevier.com/retrieve/pii/S106725161830111X [Internet] [cited 2020 Feb 15]. Available from. [DOI] [PubMed] [Google Scholar]
- 16.Brogan K., Lindisfarne E., Akehurst H., Farook U., Shrier W., Palmer S. Minimally invasive and open distal chevron osteotomy for mild to moderate hallux valgus. Foot Ankle Int. 2016 Nov;37(11):1197–1204. doi: 10.1177/1071100716656440. http://journals.sagepub.com/doi/10.1177/1071100716656440 [Internet] [cited 2020 Feb 14]. Available from. [DOI] [PubMed] [Google Scholar]
- 17.Lai M.C., Rikhraj I.S., Woo Y.L., Yeo W., Ng Y.C.S., Koo K. Clinical and radiological outcomes comparing percutaneous chevron-akin osteotomies vs open scarf-akin osteotomies for hallux valgus. Foot Ankle Int. 2018;39(3):311–317. doi: 10.1177/1071100717745282. http://journals.sagepub.com/doi/10.1177/1071100717745282 [Internet] Mar [cited 2020 Feb 14]. Available from. [DOI] [PubMed] [Google Scholar]
- 18.Maffulli N., Longo U.G., Marinozzi A., Denaro V. Hallux valgus: effectiveness and safety of minimally invasive surgery. A systematic review. Br Med Bull. 2011 Mar 1;97(1):149–167. doi: 10.1093/bmb/ldq027. https://academic.oup.com/bmb/article-lookup/doi/10.1093/bmb/ldq027 [Internet] [cited 2020 Feb 17]. Available from. [DOI] [PubMed] [Google Scholar]
- 19.Poggio D., Melo R., Botello J., Polo C., Retana P.F., Asunción J. Comparison of postoperative costs of two surgical techniques for hallux valgus (Kramer vs. scarf) Foot Ankle Surg. 2015;21(1):37–41. doi: 10.1016/j.fas.2014.09.004. https://linkinghub.elsevier.com/retrieve/pii/S1268773114001155 [Internet] Mar [cited 2020 Feb 14]. Available from. [DOI] [PubMed] [Google Scholar]
- 20.Maffulli N., Longo U.G., Oliva F., Denaro V., Coppola C. Bosch osteotomy and scarf osteotomy for hallux valgus correction. Orthop Clin N Am. 2009 Oct;40(4):515–524. doi: 10.1016/j.ocl.2009.06.003. https://linkinghub.elsevier.com/retrieve/pii/S0030589809000418 [Internet] [cited 2020 Feb 14]. Available from. [DOI] [PubMed] [Google Scholar]
- 21.Botezatu I., Marinescu R., Laptoiu D. Minimally invasive-percutaneous surgery - recent developments of the foot surgery techniques. J Med Life. 2015;8:87–93. Spec Issue. [PMC free article] [PubMed] [Google Scholar]
- 22.Kitaoka H.B., Alexander I.J., Adelaar R.S., Nunley J.A., Myerson M.S., Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994 Jul;15(7):349–353. doi: 10.1177/107110079401500701. http://journals.sagepub.com/doi/10.1177/107110079401500701 [Internet] [cited 2020 Feb 17]. Available from. [DOI] [PubMed] [Google Scholar]
- 23.Crespo Romero E., Peñuela Candel R., Gómez Gómez S. Percutaneous forefoot surgery for treatment of hallux valgus deformity: an intermediate prospective study. Musculoskelet Surg. 2017 Aug;101(2):167–172. doi: 10.1007/s12306-017-0464-1. http://link.springer.com/10.1007/s12306-017-0464-1 [Internet] [cited 2020 Feb 17]. Available from. [DOI] [PubMed] [Google Scholar]
- 24.Caravelli S., Mosca M., Massimi S. Percutaneous treatment of hallux valgus: what’s the evidence? A systematic review. Musculoskelet Surg. 2018 Aug;102(2):111–117. doi: 10.1007/s12306-017-0512-x. http://link.springer.com/10.1007/s12306-017-0512-x [Internet] [cited 2020 Feb 17]. Available from. [DOI] [PubMed] [Google Scholar]