Abstract
Trichotillomania is a mental health condition characterized by repetitive pulling out of one’s hair, often leading to functional impairment and/or distress. A convenience sampling of 10,169 adults, aged 18-69 years, representative of the general US population, completed a survey to establish occurrence of trichotillomania, other mental health concerns, and impact of the illness. 175 (1.7%) identified as having current trichotillomania. Rates of trichotillomania did not differ significantly based on gender (1.8% of males and 1.7% of females). The mean age of onset for trichotillomania was 17.7 years. The mean age of onset differed significantly for males (mean 19.0 years) versus females (mean 14.8 years (p=0.020). The average amount of distress reported due to trichotillomania was relatively high, and 79% of people with trichotillomania had one or more mental health comorbidities, the most common being anxiety/depressive disorders, OCD, PTSD, and ADHD. This study suggests trichotillomania is relatively common in the general population and typically characterized by moderate-high distress and high rates of comorbidity.
Keywords: trichotillomania, prevalence, gender, comorbidity
1. Introduction
Trichotillomania (hair-pulling disorder) is a psychological condition characterized by recurrent pulling out of one’s own hair, leading to hair loss and oftentimes functional impairment (American Psychiatric Association, APA, 2013). Although discussed in the medical literature for decades (Grant & Chamberlain, 2016), trichotillomania was not officially included as a mental health disorder in the APA’s Diagnostic and Statistical Manual until the DSM-III-R (1987). In the 5th edition of the DSM (DSM-5), trichotillomania was included in the chapter on Obsessive-Compulsive and Related Disorders with obsessive compulsive disorder (OCD), excoriation (skin picking) disorder, body dysmorphic disorder, and hoarding disorder.
To date, no nationwide epidemiological studies of trichotillomania have been conducted in any global jurisdiction. Small studies examining the prevalence of trichotillomania among United States college students have reported varying rates of hair-pulling or trichotillomania, depending upon whether the behavior or the diagnostic entity was assessed. For example, studies of hair-pulling, not necessarily meeting criteria for trichotillomania, have found rates between 6.3% and 15% in university samples. Nearly all such studies examined college and university students, with sample sizes per study of 98 to 490 subjects (Mansueto et al., 2006; Rothbaum et al., 1993; Stanley et al., 1994; Graber & Arndt, 1993; Stanley et al., 1995). In the only community sample examining hair-pulling thus far, Duke and colleagues (2009) found that 6.5% of adults within the community (n=832 using an anonymous questionnaire) endorsed hair-pulling for purposes other than grooming.
Studies that have used more rigorous assessments of trichotillomania, have reported slightly lower prevalence rates (between 0.6% and 3.5%) than those reported for more general hair-pulling behavior, but these have also been performed using fairly small samples of convenience, and again typically in college or university settings. For example, an older study of 2579 college freshmen reported that 0.6% met DSM-III-R criteria for trichotillomania during their lifetimes, but when the tension reduction diagnostic criterion was dropped from the definition, 2.5% of subjects (1.5% of males and 3.4% of females) had at some point engaged in clinical levels of hair-pulling (Christenson et al., 1991). A recent study of 4335 university students using an electronic survey found that 0.7% met criteria for trichotillomania, and that 4.8% reported subclinical pulling (Houghton et al., 2018). Another recent online survey completed by 1378 participants in the community found that 2% met criteria for trichotillomania (Solley and Turner, 2018). A study of 339 medical students reported lifetime prevalence of trichotillomania of 3.5% (Grzesiak et al., 2017). Among adolescents in Israel (n=794) a lifetime prevalence of 1.0% and a point prevalence of 0.5% were reported for trichotillomania (King et al., 1995). Among adults hospitalized for psychiatric reasons, 3.4% had current trichotillomania and 4.4% met criteria for lifetime trichotillomania in two independent studies (n=204 adults, Grant et al., 2005; n=234 adults, Muller et al., 2011).
Based on these small samples, trichotillomania appears to have a female preponderance (4:1 female: male), although this has been questioned (Christenson et al., 1991) and in childhood, the sex distribution has been found to be equal (Chang et al., 1991). Some recent studies have raised questions regarding how pronounced the female preponderance actually is. In a study of 86 non-treatment seeking adults, who reported “hair-pulling at least once a week, for non-cosmetic purposes”, the authors found a male to female ratio of 1:1.1 (Ghisi et al., 2012). Similarly, in a study of students in three medical schools (n=210), 28 students met criteria for trichotillomania and the ratio of men to women was 1:1 (Siddiqui et al., 2012). Finally, in a study of 791 university students, the rates of trichotillomania did not significantly differ between men and women (3.5% of men compared to 4.1% of women; χ2 test = 0.1401; p=.708) (Odlaug et al., 2010). So, although clinical samples strongly support a female preponderance (Grant et al., 2016), other studies of community samples have called this into question.
Research on trichotillomania suggests that this disorder is associated with elevated rates of mental disorders, including anxiety disorders, mood disorders, and other obsessive-compulsive spectrum disorders (Christenson et al., 1991; Houghton et al., 2016). Although functional impairment has been well documented in many people with trichotillomania (Woods et al., 2006), previous studies, however, have not systematically assessed the relative impact of trichotillomania versus the co-occurring disorder.
The purpose of this study was to fill these gaps in knowledge. We sought to 1) determine the prevalence of trichotillomania in a large representative sample from the US population; 2) characterize the US trichotillomania population based on demographic variables such as age, sex, race, and socioeconomics, and compare prevalence across demographic variables; and 3) determine the incidence of psychiatric comorbidities among people with trichotillomania, and the relative impact on peoples’ lives of these comorbidities vs. trichotillomania.
2. Methods
2.1. Participants
The data collection was undertaken as part of market research for a client interested in providing a new treatment for trichotillomania. Data from this market research was subsequently made available in de-identified (anonymized) form to the current researchers, who were free to interpret and publish the findings unrestricted. The current paper thus constituted secondary analyses of de-identified data and was exempted from Institutional Review Board (IRB) procedures under current US guidelines. As part of the original data collection, all participants had provided informed consent and had agreed that their data could be shared in anonymized form with external researchers.
A convenience sampling method was used to screen people representative of the general US population, 18-69 years of age. The target sample size was approximately 10,000 individuals. Survey respondents were recruited from the Schlesinger Group using the “General Population” panel, a well-known provider of panels for online surveys. Quotas were used to assure a sample that was age and gender matched to the US Population (based on US Census Data). The Schlesinger Group is an ESOMAR member and adheres to the globally recognized code of conduct, the jointly developed ICC/ESOMAR Code, for marketing research. The procedures included a “double-opt-in” process for recruitment, requiring initial assent to the study participation policy, confirmation email being sent, and then the individual confirming assent by clicking an email link. This process of consent is standard for marketing research studies and is appropriate given the low level of risk to participants. The following quality control measures are used to validate the panel: photo ID validation (manual) at time of registration for panel; relevant ID and a programming (CAPTCHA) at registration to deter bots; a Red Herring survey to catch people outside of US, hidden questions in registration to catch bots, database checks to identify batches of similar email structure entering panel in short time period, profile checks to identify unlikely combinations of or too many combinations of ailments, and profile checks to identify selection of aberrant choices at different questions at registration and over time on the panel. The sponsor and all survey personnel were blinded to the identity of all survey subjects and had no access to any personally identifiable information. The incentive for survey participation was 300 points, which has a value of $3.00. Schlesinger uses a point system for survey participants, and once a panelist obtains 500 points, they are able exchange it for rewards, with options to use it for Amazon dollars, gift cards with various retailers, or charities. The survey took approximately 15 minutes to complete.
2.2. Assessments
Each participant underwent an Internet-based, self-administered survey with two segments: Part 1: Screening for prevalence: demographics and diagnosis of trichotillomania and comorbidities; and Part 2: Survey of people with current trichotillomania: detailed survey of diagnosis, severity, and life impact. Part 1 of the survey asked about multiple psychiatric disorders with one question (“Please indicate whether you currently have or have ever had any of the following medical conditions”). The general question was then followed by specific questions regarding who diagnosed the condition, age of onset, and treatment history. In addition, Part 2 of the survey asked about each of the following diagnostic criteria for trichotillomania: “Repeated pulling of my hair causing hair loss; repeated attempts to stop or decrease the hair pulling; the hair pulling is/was causing me personal distress or causing difficulty in areas of my life; realizing that the hair pulling, or hair loss was not related to some other medical problem or a skin condition; and the hair pulling was not done to try to improve my appearance or what I saw as a flaw.” Only if the person answered affirmatively to hair-pulling/trichotillomania in the list of medical conditions were they then prompted to answer Part 2. The survey was active from January 10 to January 24, 2019. The recruiting email did not make any mention of the purpose of the survey, no mention of “health”, “new treatment”, any diagnosis, or anything that could bias who opened/took the survey. The following quality assurance controls were used in the survey: non-leading survey invitation, to control for self-selection by panelists, a wide variety of diagnoses included in prevalence question, to control for self-selection by panelists, check of survey participant responses vs their information at panel registration, check for speeding and/or straight-lining in survey responses, and active monitoring of survey patterns and removal of respondents who display inauthentic behaviors.
2.3. Data Analysis
Data were presented descriptively. Where formal statistical tests were undertaken, these comprised independent sample t-tests for continuous variables, and Likelihood Ratio (LR) chi-square tests for categorical variables. Significance was defined as p<0.05.
3. Results
The study sample comprised 10,169 adults. Demographic characteristics of the total sample, and of those in the sample with trichotillomania, are provided in Table 1. The age, gender, education, race/ethnicity and annual household income of the screened sample of 10,169 adults mirrored that for the US population (U.S. Census Bureau 2017, 2018).
Table 1. Demographics of the Screened Population and Those with Trichotillomania (TTM).
| Demographic Variables | Screened Population (n=10,169)* | Trichotillomania/Total Screened | Current Prevalence of TTM in the stratum |
|---|---|---|---|
| Age, years | |||
| 18-29 | 2,551 (25.1%) | 65 / 2,551 | 2.6% |
| 30-49 | 3,852 (37.9%) | 84 / 3,852 | 2.2% |
| 50-69 | 3,766 (37.0%) | 26 / 3,766 | 0.7% |
| Gender* | |||
| Male | 5,045 (49.6%) | 89 / 5,045 | 1.8% |
| Female | 5,087 (50.0%) | 84 / 5,087 | 1.7% |
| Non-binary/third gender, not listed, or prefer not to answer | 37 (0.4%) | 2 / 37 | 5.4% |
| Education | |||
| High school diploma or less | 1,564 (15.4%) | 37 / 1,564 | 2.4% |
| Some college or Associate degree | 3,629 (35.7%) | 56 / 3,629 | 1.5% |
| Bachelor’s degree | 3,259 (32.1%) | 47 / 3,259 | 1.4% |
| Master’s, Doctorate, or Professional degree | 1,717 (16.9%) | 35 / 1,717 | 2.0% |
| Race/Ethnicity | |||
| American Indian or Alaska Native | 185 (1.8%) | 2 / 185 | 1.1% |
| Asian | 459 (4.5%) | 9 / 459 | 2.0% |
| Black or African American | 1,853 (18.2%) | 32 / 1,853 | 1.7% |
| Native Hawaiian or Other Pacific Islander | 49 (0.5%) | 1 / 49 | 2.0% |
| White | 7,525 (74.0%) | 127 / 7,525 | 1.7% |
| Other | 413 (4.1%) | 7 / 413 | 1.7% |
| Annual Household Income | |||
| < $25,000 | 1,359 (13.4%) | 32 / 1,359 | 2.4% |
| $25,000 - $50,000 | 2,362 (23.2%) | 48 / 2,362 | 2.0% |
| $50,001 - $75,000 | 2,043 (20.1%) | 36 / 2,043 | 1.8% |
| $75,001 - $125,000 | 2,344 (23.1%) | 30 / 2,344 | 1.3% |
| > $125,000 | 1,596 (15.7%) | 23 / 1,596 | 1.4% |
| Prefer not to answer | 465 (4.6%) | 6 / 465 | 1.3% |
Male population includes 11 who identified as transgender male and female population includes 9 who identified as transgender female.
In total, 175 participants in the sample (1.7%) identified as having current trichotillomania (Table 1). The lifetime rate of trichotillomania was (n=253; 2.5%). The current rates of trichotillomania did not differ based on gender (1.8% of males and 1.7% of females). The lifetime rates of trichotillomania also did not differ based on gender (2.5% of males and 2.4% of females).
The prevalence of trichotillomania appeared higher (2.2%-2.6%) in those under age 50 (Table 2). The prevalence of trichotillomania did not differ significantly as a function of household income (Likelihood Ratio, LR=4.016, p=0.547), education level (LR=7.658, p=0.264), or racial-ethnic group (all LR p>0.30). In terms of gender, there was a notable difference between trichotillomania prevalence in males and females among those aged 30-49 years (Table 2).
Table 2. Trichotillomania Prevalence by Age and Gender.
| Population | Trichotillomania / Total | Prevalence of TTM in the stratum |
|---|---|---|
| Male Total | 89 / 5,045 | 1.8% |
| 18-29 | 31 / 1,258 | 2.5% |
| 30-49 | 49 / 1,910 | 2.6% |
| 50-69 | 9 / 1,877 | 0.5% |
| Female Total | 84 / 5,087 | 1.7% |
| 18-29 | 33 / 1,272 | 2.6% |
| 30-49 | 34 / 1,933 | 1.8% |
| 50-69 | 17 / 1,882 | 0.9% |
Of the 175 participants with current trichotillomania, 110 (62.9%) reported that the diagnosis had been made by a healthcare professional (doctor, nurse, or psychologist/therapist). Using this number as a more conservative estimate of true prevalence, then we find that 0.98% had current trichotillomania for which attention had been sought from a healthcare professional. In these trichotillomania participants, the majority (61 participants, i.e. 55.5%) were male.
The mean age of onset for trichotillomania for the 175 participants with current trichotillomania was 17.7 years (range 1-61 years). The mean age of onset differed for males (mean 19.0 years) versus females (14.8 years), and this was statistically significant (t=2.36, p=0.020). The mean number of bodily areas pulled from was 2.5 (median=2).
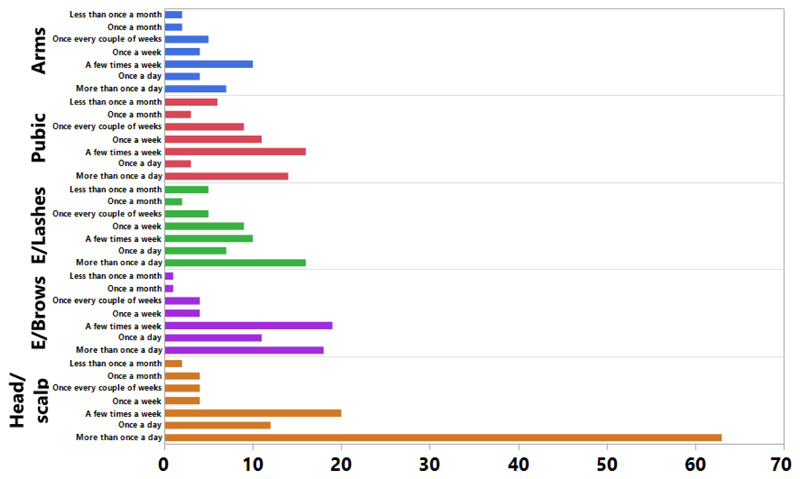
Of the 175 participants with current trichotillomania, on a scale of 1-7 for how noticeable hair loss was (with 1 being not noticeable at all, and 7 being highly noticeable), the mean score was 4.3 (SD=1.9). When asked how distressed they were about their hair-pulling (on a scale from 1 to 7, with 7 being the more distressing), the mean score was 5.1 (SD=1.8). In terms of how severe these participants reported hair pulling was (on a scale of 1 to 7, with 1 being very mild, 4 moderate, and 7 very severe), the averages were: at first diagnosis 4.4 (1.8), at its worst 5.2 (1.7), and currently 4.1 (1.8). Figure 1 shows how many of these participants reported pulling hair from particular body sites, and how frequently. It can be seen that head hair was the most common site pulled daily, followed by eyebrows, eyelashes, pubic hair, and then arm hair. In terms of gender, a significantly greater percentage of females (42% and 32%) compared to males (18% and 12% respectively; both p<.05) endorsed “severe” distress from hair-pulling and “major impact” on their lives from hair-pulling (i.e. a “7” on a scale from 1 to 7)
Figure 1. Number of participants with TTM reporting pulling hair from particular regions, shown in terms of frequency distributions. E=Eye.
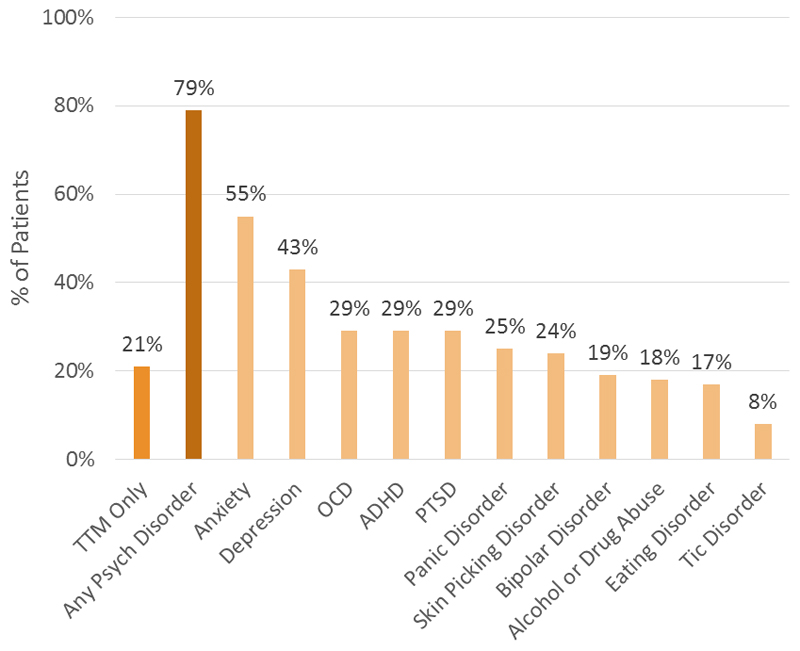
Figure 2 provides data on the comorbid conditions reported by those with trichotillomania. In the trichotillomania sample of 175 participants, 42 (24%) had current co-morbid skin picking disorder. The most common co-occurring disorders were “any anxiety” disorder (53%), depression (45%), ADHD (29%), PTSD (29%) and OCD (29%). Men and women with trichotillomania did not differ significantly in terms of rates of specific co-occurring disorders (all LR Chi-square p values >0.09).
Figure 2. Current Psychiatric Comorbidities Reported By 175 Adults with Trichotillomania.
Participants were asked to rank trichotillomania and their co-occurring conditions in order from the most bothersome to the least bothersome (most bothersome condition ranked as #1, the next most bothersome as #2, and so on). When anxiety co-occurred with trichotillomania (n=96), participants rated trichotillomania more bothersome than the anxiety in 32.2% of cases, which was similar to findings in depression (n=75) where 32.0% found trichotillomania more bothersome than depression. When trichotillomania co-occurred with obsessive compulsive disorder (n=51), 54.9% of the participants reported that trichotillomania was more bothersome than their OCD. When trichotillomania co-occurred with ADHD (n=47), 53.2% reported that trichotillomania was more bothersome than the ADHD. When trichotillomania co-occurred with PTSD (n=52), 52.0% reported that trichotillomania was more bothersome than the PTSD.
In addition to those with current trichotillomania, 78 participants reported that trichotillomania was a past problem (no symptoms currently), with 47.4% being male and 50.0% being female. The majority of these participants (60%) reported that their previous trichotillomania had been moderate to severe. Of the 78 participants who reported lifetime but not current trichotillomania, 15 (19.2%) said they had received treatment and stopped pulling their hair, and 63 (80.8%) said they stopped pulling their hair without treatment. Additionally, 31 (39.7%) reported their hair pulling had been mild, 41 (52.6%) moderate, and 6 (7.7%) severe. For participants who indicated having trichotillomania in the past, the age of onset was slightly numerically younger than those with current trichotillomania (15.1 compared to 17.7 years) though difference was not significant (p>0.10). For these participants, their hair-pulling stopped on average after 10.0 years (median 6; range 0 to 45).
4. Discussion
This study, the first large scale epidemiological survey of trichotillomania in the US general population, found that 1.7% of 18-69 year olds endorsed current trichotillomania. This prevalence rate for trichotillomania is in keeping with some of the smaller studies using samples of convenience (which reported rates ranging from 0.6% to 2.0%) (Christenson et al., 1991; King et al., 1995; Houghton et al., 2018; Solley & Turner, 2018). However, the current study extends beyond these previous studies substantially in terms of recruiting a representative sample of the general population (rather than focusing on e.g. students at one college), and in terms of the large sample size. It thus covers a wider age range and is more racially/ethnically diverse, with the findings being more likely to reflect the disorder at large. We found that the prevalence of trichotillomania was fairly consistent across different ethnic groups, and did not appear to differ significantly as a function of education level or income (of course the strata are large [e.g., 75-125K annual income] and prevalence declined nearly in linear fashion as income increased, with the lowest rate barely more than half the highest rate).
In terms of gender, this study found, contrary to some previous research (Grant et al., 2016), that trichotillomania appears to be as common in men as women. This is not completely surprising given that a couple of small studies have similarly found virtually no differences in rates of trichotillomania among men and women (Ghisi et al., 2012; Siddiqui et al., 2012; Odlaug et al., 2010). Having said that, it still prompts an important question concerning why the gender ratios differ among the various studies. One possible explanation would be that the findings from this study, the largest survey to date, are accurate and in alignment with the handful of previous smaller studies finding that trichotillomania is similarly common in men and women. Men have the disorder in equal numbers but because men may be less socially bothered by the pulling (i.e. they can shave if pulling from their beards or attribute hair loss to balding if pulling from their heads), they may come for treatment (i.e. something one step further than simply an assessment) less frequently than women, and therefore studies of clinical populations have missed these people (Christenson et al., 1994). Support for this interpretation is our finding that men reported less severe distress compared to women. Additional support is that it would be peculiar for people to endorse trichotillomania if they in fact did not have or strongly suspect themselves of having trichotillomania. Therefore, the results of this survey have a certain amount of face validity (further supported by the fact that the rates reported here in females is in keeping with most previous research). Of course, our study used survey data, whereas in-person clinical interview is the gold-standard for diagnosis. There were no follow-up contacts with those who endorsed trichotillomania in phase 1 to confirm these findings. An alternative explanation for these slightly more novel gender findings is that the survey itself suffered from methodological flaws that impacted the results and that the gender ratio therefore may not be equal in men and women as these findings suggest. Other than the lack of follow-up assessments, it is difficult to hypothesize what would have resulted in elevated rates only among men. There were no incentives for participants to endorse mental health problems.
One intriguing gender finding was that the prevalence of trichotillomania in men was significantly greater than in women in the 30-49 year old age cohort. It is unclear why this is the case. One possibility is that overall, trichotillomania is similarly prevalent in men and women, and the findings in this age bracket reflect chance variation. Another possibility is that prevalence rates in this particular bracket do differ between the genders in the background population. This could reflect different neurobiological processes in men and women at different age points; or men and women in this range tending to have different exposures to triggers (worsening factors) for hair-pulling. For example, men in this age bracket may be particularly sensitive to noticing hair-loss (whether due to trichotillomania or other causes such as alopecia), and so reading about trichotillomania and becoming aware that this is a recognized condition, due to its potential effects on self-esteem and intimacy. Until more is known about the etiological processes contributing to trichotillomania, including longitudinally, the reasons for this finding are unlikely to become apparent.
The comorbidity data in this study paints an important clinical picture of trichotillomania that perhaps clinicians have been unaware of. In general, the comorbidity data from this study are in keeping with previous studies showing that trichotillomania is frequently comorbid with multiple other mental health conditions, particularly OCD, anxiety, ADHD and PTSD (Christenson et al., 1991; Keuthen et al., 2016; Houghton et al., 2016; Lochner et al., 2019). Unlike previous research, however, that only vaguely touched on how trichotillomania compared to other comorbid conditions, this study found that the majority of people with trichotillomania found their hair-pulling more distressing than their OCD, ADHD and PTSD. Clinically this is important as these other conditions may garner more clinical attention. Thus clinicians should not only be thoughtful about screening for trichotillomania but should also consider prioritizing treatment of the various conditions after consultation with their patients and not assume one condition is more disabling than another.
This study has several positive features notably that it is the first large prevalence study of trichotillomania in the general population of the US (or indeed in any country). Several limitations, however, should be considered. First, the study was a survey and as such no direct in person interviews were performed. The gold standard for diagnosis is of course clinical interview by a healthcare professional, but this simply is not feasible for large scale epidemiological studies of trichotillomania. Of course, it would be unusual for people to answer the questions about trichotillomania unless they felt they had a problem with hair-pulling (i.e. it is doubtful that someone who pulled only rarely would answer the diagnosis question affirmatively). Second, the survey used a non-probability sample. Although the sample demographics paralleled national demographics, it still raises the possibility of selection biases based on personality factors, etc. Third, data on comorbidities are also per participant report and as such may have over- or under- reported specific conditions. Fourth, since this was a secondary analysis of externally collected market research anonymized data, it was not possible to examine other more detailed information that might have been of interest from a research perspective (for example, assessment of traits that might contribute to trichotillomania, or cognitive measures that may help to explain the biological processes contributing to the disorder).
In summary, this study examined the prevalence of trichotillomania in a large representative sample of adults in the USA, shedding new light on its prevalence, demographic associations, and co-morbid expression. Overall, trichotillomania was common (1.7%), equally prevalent in men and women, occurred across ethnic groups, and did not differ in prevalence significantly as a function of education level or income strata. Trichotillomania was reported by sufferers to be quite distressing (average 5.1 on a scale of 1-7, with 7 being more distressing), and 79% of affected individuals reported one or more comorbid mental health disorders.
Acknowledgements
The authors would like to thank Katie MacFarlane and Brian Zorn both from SmartPharma LLC who conducted the survey.
Footnotes
Disclosures: The researchers’ time for this study was funded by internal funds. The survey data were collected by Promentis Pharmaceuticals, Inc., and were made available for unrestricted use by the study authors.
The authors received no funding from Promentis Pharmaceuticals, Inc., for this study. Promentis Pharmaceuticals, Inc., has had no influence on the analyses of data or the writing of this manuscript. Dr. Grant has received research grants from TLC Foundation, and Otsuka Pharmaceuticals. Dr. Grant receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies and has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, and McGraw Hill. Dr. Chamberlain’s time on this study was supported in part by a Wellcome Trust Clinical Fellowship (110049/Z/15/Z). Dr. Chamberlain consults for Promentis Pharmaceuticals, Inc., on work unrelated to this manuscript, and Ieso Digital Health. Dr. Chamberlain receives a stipend for his work as Associate Editor at Neuroscience and Biobehavioral Reviews; and at Comprehensive Psychiatry.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; Washington, DC: 2013. [Google Scholar]
- Chamberlain SR, Odlaug BL, Boulougouris V, Fineberg NA, Grant JE. Trichotillomania: neurobiology and treatment. Neurosci Biobehav Rev. 2009;33:831–42. doi: 10.1016/j.neubiorev.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Chang CH, Lee MB, Chiang YC, Lu YC. Trichotillomania: A clinical study of 36 patients. J Formos Med Assoc. 1991;90:176–180. [PubMed] [Google Scholar]
- Christenson GA, Pyle RL, Mitchell JE. Estimated lifetime prevalence of trichotillomania in college students. J Clin Psychiatry. 1991;52:415–417. [PubMed] [Google Scholar]
- Christenson GA, Mackenzie TB, Mitchell JE. Characteristics of 60 adult chronic hair pullers. Am J Psychiatry. 1991;148:365–70. doi: 10.1176/ajp.148.3.365. [DOI] [PubMed] [Google Scholar]
- Christenson GA, MacKenzie TB, Mitchell JE. Adult men and women with trichotillomania. A comparison of male and female characteristics. Psychosomatics. 1994;35:142–9. doi: 10.1016/s0033-3182(94)71788-6. [DOI] [PubMed] [Google Scholar]
- Ghisi M, Bottesi G, Sica C, Ouimet AJ, Sanavio E. Prevalence, phenomenology and diagnostic criteria of hair-pulling in an Italian non-clinical sample: a preliminary study. J Obsessive-Compuls Relat Disord. 2013;2:22–29. doi: 10.1016/j.jocrd.2012.09.003. 2013. [DOI] [Google Scholar]
- Graber J, Arndt WB. Trichotillomania. Compr Psychiatry. 1993;34:340–346. doi: 10.1016/0010-440x(93)90021-u. [DOI] [PubMed] [Google Scholar]
- Grant JE, Levine L, Kim D, Potenza MN. Impulse control disorders in adult psychiatric inpatients. Am J Psychiatry. 2005;162:2184–2188. doi: 10.1176/appi.ajp.162.11.2184. [DOI] [PubMed] [Google Scholar]
- Grant JE, Williams KA, Potenza MN. Impulse-control disorders in adolescent psychiatric inpatients: co-occurring disorders and sex differences. J Clin Psychiatry. 2007;68:1584–1592. doi: 10.4088/jcp.v68n1018. [DOI] [PubMed] [Google Scholar]
- Grant JE, Chamberlain SR. Trichotillomania. Am J Psychiatry. 2016;173:868–874. doi: 10.1176/appi.ajp.2016.15111432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JE, Redden SA, Leppink EW, Chamberlain SR, Curley EE, Tung ES, Keuthen NJ. Sex differences in trichotillomania. Ann Clin Psychiatry. 2016;28:118–124. [PubMed] [Google Scholar]
- Grzesiak M, Reich A, Szepietowski JC, Hadryś T, Pacan P. Trichotillomania Among Young Adults: Prevalence and Comorbidity. Acta Derm Venereol. 2017;97:509–512. doi: 10.2340/00015555-2565. [DOI] [PubMed] [Google Scholar]
- Houghton DC, Maas J, Twohig MP, Saunders SM, Compton SN, Neal-Barnett AM, Franklin ME, Woods DW. Comorbidity and quality of life in adults with hair-pulling disorder. Psychiatry Res. 2016;239:12–9. doi: 10.1016/j.psychres.2016.02.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houghton DC, Alexander JR, Bauer CC, Woods DW. Body-focused repetitive behaviors: More prevalent than once thought? Psychiatry Res. 2018;270:389–393. doi: 10.1016/j.psychres.2018.10.002. [DOI] [PubMed] [Google Scholar]
- Keuthen NJ, Curley EE, Scharf JM, Woods DW, Lochner C, Stein DJ, Tung ES, Greenberg E, Stewart SE, Redden SA, Grant JE. Predictors of comorbid obsessive-compulsive disorder and skin-picking disorder in trichotillomania. Ann Clin Psychiatry. 2016;28:280–288. [PubMed] [Google Scholar]
- King RA, Zohar AH, Ratzoni G, Binder M, Kron S, Dycian A, Cohen DJ, Pauls DL, Apter A. An epidemiological study of trichotillomania in Israeli adolescents. J am Acad Child Adolesc Psychiatry. 1995;34:1212–1215. doi: 10.1097/00004583-199509000-00019. [DOI] [PubMed] [Google Scholar]
- Lochner C, Keuthen NJ, Curley EE, Tung ES, Redden SA, Ricketts EJ, Bauer CC, Woods DW, Grant JE, Stein DJ. Comorbidity in trichotillomania (hair-pulling disorder): A cluster analytical approach. Brain Behav. 2019;9:e01456. doi: 10.1002/brb3.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansueto CS, Thomas AM, Brice AL. Hair-pulling and its affective correlates in an African-American university sample. J Anxiety Disord. 2007;21:590–599. doi: 10.1016/j.janxdis.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Müller A, Rein K, Kollei I, Jacobi A, Rotter A, Schütz P, Hillemacher T, de Zwaan M. Impulse control disorders in psychiatric inpatients. Psychiatry Res. 2011;188:434–438. doi: 10.1016/j.psychres.2011.04.006. [DOI] [PubMed] [Google Scholar]
- Odlaug BL, Grant JE. Impulse-control disorders in a college sample: results from the self-administered Minnesota Impulse Disorders Interview (MIDI) Prim Care Companion J Clin Psychiatry. 2010;12 doi: 10.4088/PCC.09m00842whi. PCC.09m00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Shaw L, Morris R, Ninan PT. Prevalence of trichotillomania in a college freshman population. J Clin Psychiatry. 1993;54:72–73. [PubMed] [Google Scholar]
- Siddiqui EU, Naeem SS, Naqvi H, Ahmed B. Prevalence of body-focused repetitive behaviors in three large medical colleges of Karachi: a cross-sectional study. BMC Res Notes. 2012;5:614. doi: 10.1186/1756-0500-5-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solley K, Turner C. Prevalence and correlates of clinically significant body-focused repetitive behaviors in a non-clinical sample. Compr Psychiatry. 2018;86:9–18. doi: 10.1016/j.comppsych.2018.06.014. [DOI] [PubMed] [Google Scholar]
- Stanley MA, Borden JW, Bell GE, Wagner AL. Nonclinical hair-pulling: phenomenology and related psychopathology. J Anx Disord. 1994;8:119–130. doi: 10.1016/0887-6185(94)90010-8. [DOI] [Google Scholar]
- Stanley MA, Borden JW, Mouton SG, Breckenridge JK. Nonclinical hair-pulling: affective correlates and comparison with clinical samples. Behav Res Ther. 1995;33:179–186. doi: 10.1016/0005-7967(94)e0018-e. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Table 1. Educational Attainment of the Population 18 Years and Over, by Age, Sex, Race, and Hispanic Origin: 2017 (All Races) 2017 Retrieved from: https://www.census.gov/data/tables/2017/demo/education-attainment/cps-detailed-tables.html.
- U.S. Census Bureau. Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2017 (2017 Population Estimates) 2018 Retrieved from: https://www.census.gov/data/datasets/2017/demo/popest/nation-detail.html.
- U.S. Census Bureau. Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States: April 1, 2010 to July 1, 2017 more information (2017 Population Estimates) 2018 Retrieved from: https://www.census.gov/data/datasets/2017/demo/popest/nation-detail.html.
- Woods DW, Flessner CA, Franklin ME, Keuthen NJ, Goodwin RD, Stein DJ, Walther MR. Trichotillomania Learning Center-Scientific Advisory Board. The Trichotillomania Impact Project (TIP): exploring phenomenology, functional impairment, and treatment utilization. J Clin Psychiatry. 2006;67:1877–1888. doi: 10.4088/jcp.v67n1207. [DOI] [PubMed] [Google Scholar]