Abstract
Aim/hypothesis
Sodium-glucose transporter-2 (SGLT2) inhibitors constitute a new class of glucose-lowering drugs, but they increase glucagon secretion which may counteract their glucose-lowering effect. Previous studies using static incubation of isolated human islets or the glucagon secreting cell line α-TC1 suggested that this results from direct inhibition of alpha-cell SGLT1/2-activity.
Methods
We assessed the importance of SGLT2-activity on glucagon secretion using isolated perfused rat pancreas; a physiological model for glucagon secretion. Furthermore, we investigated Slc5a2 (gene encoding SGLT2) expression in rat islets as well as in mice and human islets and in mouse and human α, β, and δ cells to test for potential inter-species variations. SGLT2 protein content was also investigated in mouse, rat and human islets.
Results
Glucagon output decreased 3-5 fold within minutes of shifting from low (3.5 mmol/l) to high (10 mmol/l) glucose (low glucose = 4.0±0.5 pmol/15 min vs. 1.3±0.3 pmol/15 min, P<0.05), but was unaffected by inhibition of SGLT1/2 with dapagliflozin or phloridzin or by addition of the SGLT1/2 substrate α-methylglucopyranoside whether at low or high glucose concentrations (P=0.29-0.95). Insulin and somatostatin secretion (potential paracrine regulators) was also unaffected. Slc5a2 expression and SGLT2 protein were marginal or below detection limit in rat, mouse and human islets and in mouse and human α, β and δ-cells.
Conclusion
Our combined data show that increased plasma glucagon during SGLT2-inhibitor treatment is unlikely to result from direct inhibition of SGLT2 in α-cells, but instead may occur downstream of their blood glucose lowering effects.
Keywords: Alpha-cells, Direct regulation of glucagon secretion, Endogenous glucose production, Sodium-glucose transporter-2, Sodium-glucose transporter-2 inhibitors, Sodium-glucose transporter 2 expression by the alpha cell, Type-2-diabetes
Introduction
Sodium-glucose transporter-2 (SGLT2) inhibitors represent the newest addition to the armamentarium for treatment of type 2 diabetes [1]. SGLT2 inhibitor treatment lowers blood glucose, but is at the same time associated with increased hepatic glucose production and increased glucagon secretion [2–4] which appears to counteract their glucose-lowering effects. The mechanism whereby SGLT2 inhibitors stimulate glucagon secretion is not well understood but has, based on static incubations of isolated human islets, been proposed to involve a direct effect of SGLT2-inhibitors on the α-cell [5]. Thus, the aim of this study was to test whether the effects of SGLT2 on glucagon secretion demonstrated in vitro could be reproduced in a more physiological setting. As glucagon secretion is tightly regulated by blood glucose, which is lowered by SGLT2 inhibitors, we chose the isolated perfused rat pancreas as experimental model [6, 7], where perfusate glucose are kept constant, and studied the effects of the SLGT2 inhibitor dapagliflozin, the SGLT1/2 inhibitor phloridzin, and the metabolically inert SGLT-specific substrate, methyl-α-D-glucopyranoside (α-MGP) on glucagon secretion. We also measured insulin and somatostatin secretion, both known to powerfully influence glucagon secretion. In addition, we performed a thorough expression analysis of SGLT1 and -2, as well as glucose transporters 1-5 for comparison, in mouse, rat and human islets as well as in α, β, δ-cells from mice and humans; the latter using two different human populations. Finally, we investigated SGLT2 protein expression by Western blot and immunohistochemistry.
Methods
Ethical considerations
Animal studies in Copenhagen were approved by the Danish Animal Experiments Inspectorate (2013-15-2934-00833) and the local ethics committee and performed in accordance with the guidelines of Danish legislation governing animal experimentation (1987) and the National Institutes of Health (publication number 85-23). Animal studies in Cambridge, UK (isolation of mouse pancreatic tissue) were approved by the University of Cambridge Animal Welfare and Ethical Review Body, conformed to the Animals (Scientific Procedures) Act 1986 Amendment Regulations (SI 2012/3039) and were performed under the UK Home Office Project License 70/7824. Human islets were obtained from European Consortium for Islet Transplantation (ECIT) (Milan, Italy) and received in fully anonymised form. Human kidney cDNA was derived from kidneys surgically removed due to renal cell carcinoma. Kidney tissue was obtained from Sahlgrenska Hospital (Gothenburg, Sweden) in accordance with relevant ethical guidelines and patient consent. Human kidney and pancreas tissue used for immunohistochemistry were anonymous archival tissue.
Animals
Rats
Male Wistar rats were from Janvier (Saint Berthevin Cedex, France) and housed two per cage with ad libitum access to standard chow and water, and kept on a 12:12-h light-dark cycle. Animals acclimatized at least one week.
Chicken
Chickens were housed with ad-libitum access to std. chow and drinking water for at least two weeks before experiments.
Isolated perfused rat pancreas procedure
Non-fasted rats were anesthetized with Hypnorm/Midazolam and the pancreas was isolated by removing the stomach, spleen, small and large intestine (except for the part of duodenum connected to pancreas) and by tying off the renal stalks. The abdominal aorta was tied off just below the diaphragm and immediately after a catheter was inserted retrogradely into the abdominal aorta just distally to the renal arteries, so that the aorta now exclusively supplied the pancreas (through both the coeliac and the superior mesenteric arteries). The pancreas was perfused by use of a UP100 Universal Perfusion System from Hugo Sachs (5.0 mL/min, 37°C) with a Krebs-Ringer-bicarbonate buffer gassed with 95% O2, 5% CO2 [8]. A catheter was inserted into the portal vein for collection of venous effluent. After start of perfusion, the rat was killed by diaphragm perforation. The preparation was allowed to stabilize for 25 min where after 1-min samples were collected, transferred to ice and stored at -20°C. Glucose concentration was 3.5 and 10 mmol/l as indicated in results. Following reagents were administered: the SGLT1/2-specific and metabolically inert substrate α-methyl-glucopyranoside (α-MGP, 20 mmol/l), the SGLT1/2 inhibitor phloridzin dihydrate (100 µmol/l), and the SGLT2 inhibitor dapagliflozin (0.5 µmol/l, and L-arginine (10 mmol/l. pos. control). Dapagliflozin was from Seleckchem.com (Cat. No. S1548, Munich, Germany). The remaining were from Sigma Aldrich (Cat. no. M9376, 274313 and A92600). Perfusion pressure and flow were closely monitored and remained stable during the perfusion.
Ussing chamber experiments
Chickens were euthanized by cervical dislocation and the colon was immediately isolated by a midline insertion in the lower abdomen. The colon was cleaned from its luminal content, folded open by cutting once along the long side of the intestine and placed in Krebs-Ringer buffer (room temperature). Few minutes after, the mucosa was separated from the muscularis by a carefully scrape and rapidly placed in Ussing-chambers with oxygenated (95% O2 and 5% CO2) Krebs-Ringer buffer (37°C). The preparation was left for ~35 min to stabilize, then clamped at a potential difference of 0 mV from 10 min before start until the end of the experiment. Short circuit currents (IScc), potential difference (mV) and resistance (Ω) were recorded every 2s and shown in real time by use of Clampdata software. Glucose, dapagliflozin or phloridzin was added to the luminal side of the mucosal layer (final concentration = 100 mmol/l, 55 µmol/l and 100 µmol/l, respectively), corresponding to ~ 50 x IC50 on human SGLT1[9] in case of dapagliflozin). L-lysin (10 mmol/l)) was included as pos. control.
Immunohistochemistry
Formalin fixed tissue from rat, mouse and human kidney and pancreas (n=3 for all tissue types) was embedded in paraffin. Five µm de-waxed tissue sections were first pre-treated by boiling for 15 minutes in a microwave oven in EGTA buffer at pH 9 (antigen retrieval), preincubated in PBS with 10% (w/v) BSA for 10 minutes and incubated with the primary antibody (Cat. No. LS-A2810, LSbio Seattle, WA, USA), 1:1000 in PBS with 10% (w/v) BSA over night at 4°C. Next day, the tissues were incubated with biotin goat anti rabbit IgG 1:200 (Vector Labs, Burlingame, CA, USA), ABC (PK4000, Vector labs) and DAB, lightly counterstained with haematoxylin and coverslipped with Pertex mounting medium. The sections were viewed in Leitz orthoplan microscope and the pictures taken with AxioCam IcC5 camera mounted onto the microscope.
Western blot
Rat islets, human donor islets and rat kidney tissue were lysed on ice with NP-40 lysis buffer containing protease inhibitor cocktail (Life Technologies) and stored at -20°C. Total protein concentration was measured by Bradford protein assay kit (Cat. no. 5000001, Bio Rad Laboratories, Denmark). Ten µg of protein lysate/sample was loaded and separated by 4-20% SDS-PAGE and blotted on a PDVF membrane. To avoid stripping membranes when staining for multiple proteins, membrane was cut according to the desired molecular weight (MW) range. Membranes were then stained separately with SGLT2 antibody (Cat. no. LS-A2810-50, LSbio Seattle, WA, USA) or alpha-tubulin (loading control) (Cat. no. T6074, Sigma Aldrich, Brøndby, Denmark); both diluted to a concentration of 0.5 µg/ml. Blots were developed with the chemiluminescence detection system using Super Signal (Life Technologies). Light emission was captured using an Alpha imager system (Alpha-Innotech, Broager, Denmark).
Gene expression procedures
Pancreatic islets from non-diabetic one week-old rats (n=5) were isolated as described previously[10]. Rat and donated human islets (anthropometric data supplied in ESM table 1) were cultured for 72h at 37°C (95% O2, 5% CO2) in RPMI-glutamax medium supplemented with 10% (v/v) FBS, 1% (v/v) P/S and 5.6 mmol/l glucose [10]. Total RNA was extracted by use of Nucleo-Spin kit (Macheray-Nagel, Bethlehem, USA). Quality and quantity of the extracted RNA were assessed using a NanoDrop-1000 (Thermo Scientific). Five-hundred ng total RNA were used for cDNA synthesis with the iScript™-cDNA Kit (BioRad, Copenhagen, Denmark). Real-time Reverse Transcriptase-quantitative PCR (RT-qPCR) was performed on 12 ng cDNA with SYBR Green PCR mastermix (Life Technologies) using specific primers (ESM table 2) and run in a real-time PCR machine (Applied-Biosystems, Naerum, Denmark). Gene expression levels were normalised to the house keeping mRNA Hprt1 (Hypoxanthine-guanine phosphoribosyltransferase-1) through the -∆Ct method. Methods are described in detail elsewhere [11]. As positive control, kidney tissue from rats and human donors were subjected to same procedure.
Mouse islets were isolated as described previously [12] and RNA from homogenized tissues was extracted using TRI reagent (Sigma Aldrich, UK) or RNeasy Plus Micro Kit (Qiagen, UK). Genomic DNA was removed via treatment with DNAse1 (Thermo Fisher Scientific, UK) or through the RNeasy Plus gDNA eliminator spin columns. Purified RNA was reverse transcribed using Supercript II kit (Thermo Fisher Scientific, UK). Quantitative RT-PCR was performed with a QuantStudio 7 Flex Real-Time PCR System (Applied Biosystems). The PCR reaction mix consisted of first-strand cDNA template, 6-carboxyfluorescein/quencher probe/primer mixes (Thermo Fisher Scientific, UK) and PCR Master Mix (Thermo Fisher Scientific, UK) and was amplified for 40 cycles. Expression of selected targets was normalised to that of the house-keeping mRNA Actb, and expression levels calculated as above.
Single-cell RNA-sequencing of human pancreatic islet cells
Population 1
Single cell expression levels of SGLT1, -2 and GLUT1-5 in human α, β and δ-cells were investigated by RNA sequencing based analysis by two different independent groups of investigators, using their own methodology and populations. In population 1, expression was determined by reanalyzing published human islet single cell sequencing data, from type-2-diabetic and non-diabetic donors (T2D: n = 4, ND: n = 6) [13]. FastQ files were downloaded from ArrayExpress (accession: E-MTAB-5061). Data were analyzed with bcbio-nextgen (https://github.com/chapmanb/bcbio-nextgen), using the hisat2 algorithm [14] to align reads to human genome version hg38 and the Salmon algorithm [15] for quantitation of gene counts. Only cells that passed the quality control in the original study [13] were maintained for further analysis: non-diabetic donors/diabetic donors: α-cells = 443/443, β-cells = 171/99, and δ-cells = 59/55. Cell type classification from the original study was maintained. Log2 transformed counts per million (CPM) were plotted for individual cells.
Population 2
Publicly available RNA sequencing data two different population sets from (GSE85241, GSE81608) [16, 17] were used for this analysis. Only non-diabetic individuals were included in the analyses: combined sample size = 26. RPKM values for SGLT1, 2 and GLUT1-5 from the respective data bases were uploaded to the Jupyter Notebook (http://jupyter.org/). Data were then log2 transformed, and means were calculated for SGLT1, 2 and GLUT1-5 in α, β, and δ-cells, respectively. Further details about the donors, isolation of cells and RNA-sequencing methods can be found in the original studies [16, 17].
Biochemical measurements
The in-house glucagon RIA employed a C-terminal directed antibody (code nr. 4305 [18]). Insulin and somatostatin (total: SST-14 and SST-28) concentrations were determined by in-house RIA (code nr. 2006-3 and 1758-5 [19, 20]). Sensitivities of the assays were around 1 pmol/L, allowing detection of secretory outputs as low as 5 fmol/min.
Data presentation and statistical analysis
Data are presented as means±SEM. For perfusion data, averaged basal and response outputs were calculated by taking an average of output values over the entire stimulus administration (response, 15 min) and the period leading immediately up to stimulus administration (15 min, baseline). Output (fmol/min) was the product of peptide concentration (pmol/l) and flow rate (ml/min). Averaged short circuit currents (IScc) at baseline, and after glucose and dapagliflozin were calculated over at least 50 consecutive recordings within the terminal part of the respective periods. Statistical significance was assessed by one-way ANOVA for repeated measurements followed by Bonferroni multiple comparison test using GraphPad Prism software (La Jolla, CA). Graphs were constructed in GraphPad and edited in Adobe Illustrator (San Jose, CA). p<0.05 was considered significant.
Results
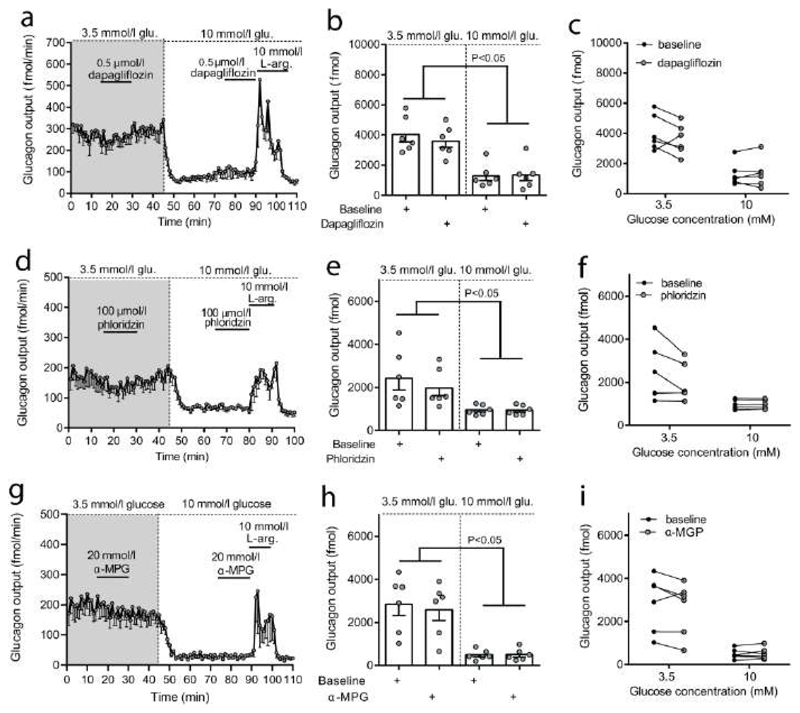
Glucagon secretion was tightly regulated by the glucose concentration in the perfusion buffer, decreasing to about 20-30 % within minutes after changing the concentration from 3.5 mmol/l to 10 mmol/l, but dapagliflozin had no effect regardless of glucose concentration (15 min output at 3.5 mmol/l glucose: 4.0±0.5 pmol vs. dapagliflozin = 3.6±0.4 pmol, P = 0.53; at 10 mmol/l glucose: 1.3±0.3 pmol vs. dapagliflozin = 1.4±0.4 pmol, P = 0.95, n = 6, fig. 1 a-c). Changing the order of glucose concentration, starting with 10 mmol/l and shifting to 3.5 mmol/l, gave similar results – no effects of dapagliflozin on glucagon secretion (data shown in ESM figure 1). Phloridzin also had no effect on glucagon secretion at 3.5 or 10 mmol/l glucose (Fig. 1d-f). Addition of the SGLT specific substrate α-MGP (20 mmol/l) had no significant effect on glucagon secretion at 3.5 or 10 mmol/l glucose (15 min output at 3.5 mmol/l glucose: 2.9±0.5 pmol vs. α-MGP = 2.6±0.5 pmol, P=0.48 and at 10 mmol/l glucose: 0.5±0.01 pmol vs. α-MGP = 0.5±0.1 pmol, P=0.99, n = 6, Fig. 1g-i). In all experiments, glucagon output was significantly lower at high glucose and L-arginine (10 mmol/l, positive control) markedly stimulated secretion (Fig. 1 a, d, g).
Figure 1. Effects of SGLT activity on glucagon secretion from isolated perfused rat pancreas.
Male Wistar rats were used. Data are shown as means ± SEM. A: Glucagon output (fmol/min) at 3.5 and 10 mmol/l glucose in absence or presence of dapagliflozin (0.5 µmol/l). B: Averaged total glucagon output (fmol) during dapagliflozin (0.5 µmol/l) administration (15 min) or at baseline (15 min immediately before stimulation), C: Connected glucagon outputs from individual animals. D-F: Same as A-C, respectively, but with administration of phloridzin (100 µmol/l)) rather than dapagliflozin. G-I: Glucagon output (fmol/min) in response to α-MGP (20 mmol/l; a SGLT-specific substrate). G: Total glucagon output during α-MGP administrations (15 min) or at respective baselines (15 min leading up to the respective administrations). L-arginine, a known glucagon secretagogue, was added at the end of all experiments to control for responsiveness (10 mmol/l, pos. control). n: = 6 for all, In B, E and H outputs from separate experiments are shown as dots. Statistical significance was tested by One-way ANOVA for repeated measurements followed by Bonferroni posthoc test. *p<0.05. Non-significant p-values: 3.5 mmol/l glucose: Baseline vs. dapagliflozin = 0.53, baseline vs. phloridzin = 0.29, baseline vs. α-MGP = 0.48, 10 mmol/l glucose: Baseline vs. dapagliflozin = 0.95, baseline vs. phloridzin = 0.71, baseline vs. α-MGP = 0.99.
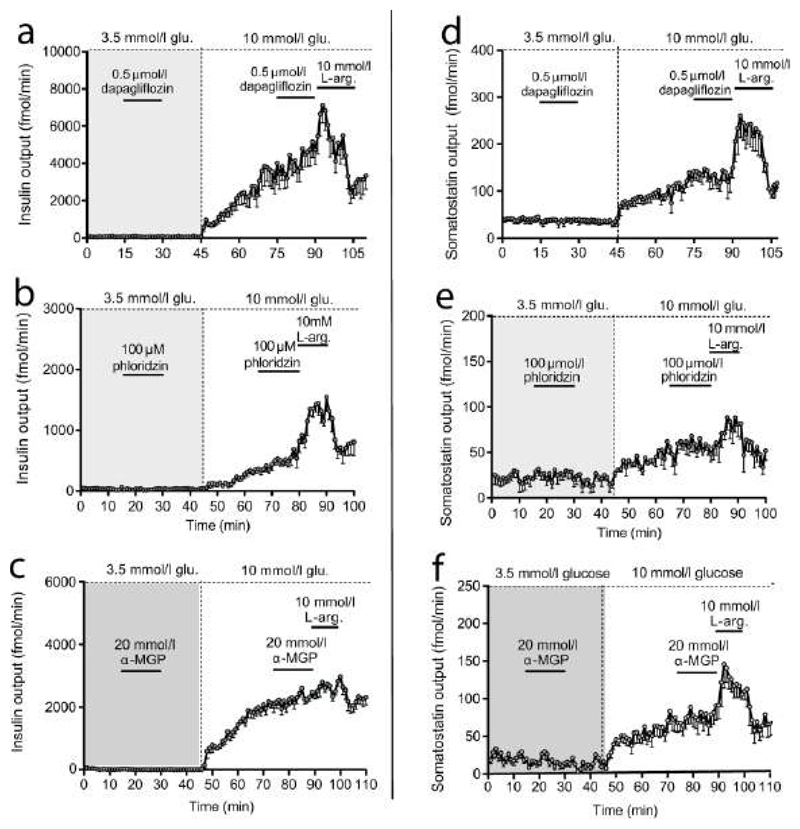
Insulin and somatostatin secretion increased shifting glucose 3.5 to 10 mmol/l. Neither dapagliflozin nor phloridzin affected the secretion (P-values for insulin/somatostatin in response to test substancen compared to baseline: dapagliflozin (3.5 mmol/l: P = 0.99/0.36; 10 mmol/l: P = 0.69/0.29; phloridzin (3.5 mmol/l: P = 0.85/0.64; 10 mmol/l: P = 0.43/0.98, n=6 in all cases, Fig. 2a, b and 2. d, e) and infusions of α-MGP were similarly ineffective (insulin/somatostatin (3.5 mmol/l: P = 0.73/0.65; 10 mmol/l: P = 0.53/0.42, n=6, Fig. 2b and 2e).
Figure 2. Effects of SGLT1/2 activity on insulin and somatostatin secretion from isolated perfused rat pancreas.
Male Wistar rats were used. Data are shown as means ± SEM. A-C: Insulin output (fmol/min) at 3.5 and 10 mmol/l glucose as indicated and in absence or presence of dapagliflozin (A), phloridzin(B) or α-MGP (0.5 µmol/l, 100 µmol/l, and 20 mmol/l, respectively); (C). D-F: Somatostatin outout (fmol/min) at 3.5 and 10 mmol/l glucose as indicated in absence or presence of dapagliflozin(D), phloridzin (E) or α-MGP (F) (0.5 µmol/l, 100 µmol/l, and 20 mmol/l, respectively). L-arginine, a known insulin and somatostatin secretagogue, was added at the end of all experiments (10 mmol/l) to control for responsiveness (pos. control). n= 6. Non-significant p-values: Insulin at 3.5 mmol/l glucose: Baseline vs. dapagliflozin = 0.99, baseline vs. phloridzin = 0.85, baseline vs. α-MGP = 0.72, insulin at 10 mmol/l glucose: Baseline vs. dapagliflozin = 0.69, baseline vs. phloridzin = 0.64, baseline vs. α-MGP = 0.53, somatostatin at 3.5 mmol/ glucose: Baseline vs. dapagliflozin = 0.36, baseline vs. phloridzin = 0.43, baseline vs. α-MGP = 0.65, somatostatin at 10 mmol/l glucose: Baseline vs. dapagliflozin = 0.29, baseline vs. phloridzin = 0.98, baseline vs. α-MGP = 0.42.
Effects of dapagliflozin on glucose-sensitive currents
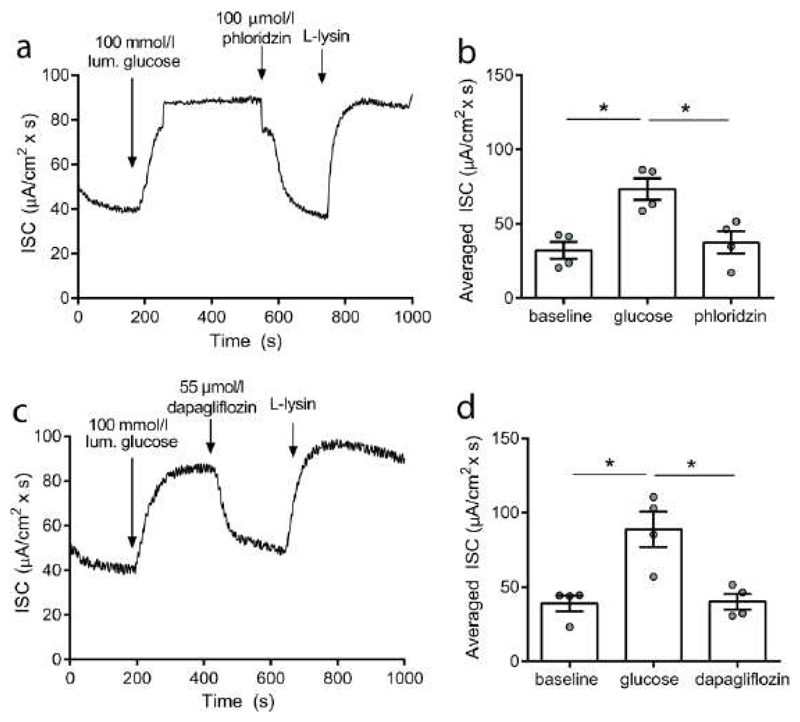
Bioactivity of the used dapagliflozin and phloridzin on SGLT-1-mediated glucose absorption was investigated using the Ussing chamber technique, by recording the SGLT1-sensitive short circuit current (IScc) in real time. Glucose administration (100 mmol/l) to the luminal side of the mucosa doubled the IScc (from ~40µA/cm2) but this response was abolished by the SGLT1/2 inhibitor phloridzin (100 µmol/l, pos. control) (Fig. 3a and b). Importantly, dapagliflozin also eliminated the glucose-sensitive current when applied in a concentration well above (55 µmol/l) the IC50 on human SGLT1 (1.3 µmol/l[9]) (Fig. 3c and d).
Figure 3. Effects of dapagliflozin on colonic glucose-sensitive currents in chicken mucosa (mirroring SGLT-1).
A and C: representative experimental traces (µA/cm2) at baseline or in response to 100 mmol/l luminal glucose, 55 µmol/l dapagliflozin (A)/ 100 µmol/l phloridzin (C: positive control) and 10 mmol/l luminal L-lysin. B and D: Collected responses (means ± SEM) to the stimuli shown in A and C. n: A and C = 1, B and D = 6. Statistical significance was tested by One-way ANOVA for repeated measurements followed by Bonferroni post hoc test. *p<0.05.
Expression of glucose transporters in rat, human and mouse islets
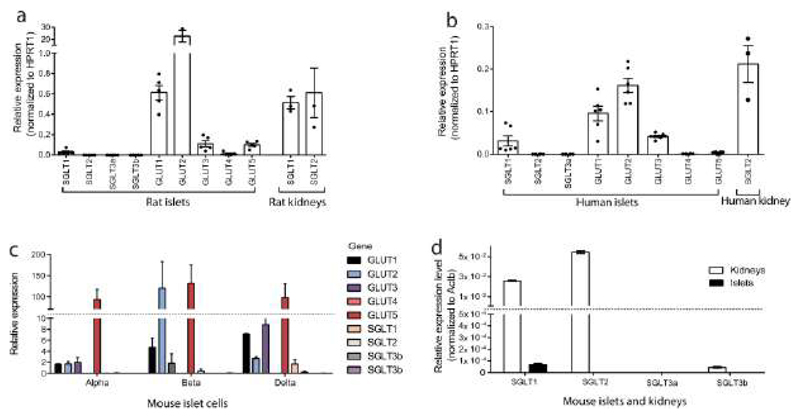
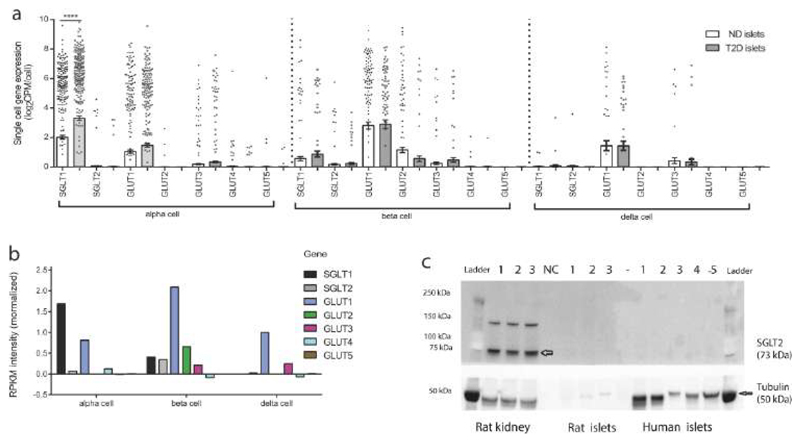
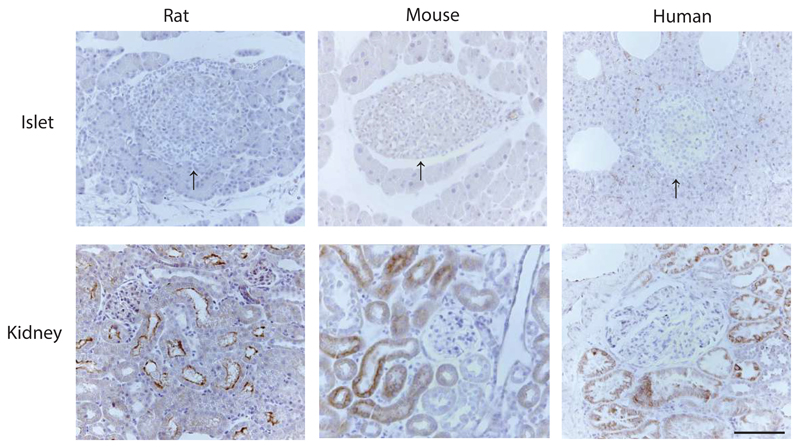
Expression of Slc5a2 (the gene encoding SGLT2) was investigated in rat as well as in human and mouse pancreatic islets to test for potential species differences. In all tested species, expression was below detection limit (Ct=35). In apparent contradiction to these results, high SLC5A2 expression in human islets was detected in our initial analysis (ESM figure 2), using primers annealing to the N-terminal part of the gene. However, we later discovered that this expression most likely reflects amplification of two highly expressed unrelated genes (AC026471.6 and C16orf58) that overlap with SGLT2 and are highly expressed in islets (ESM figure 3). SGLT1 expression (Slc5a1) was low in mouse, rat and human islets in comparison to GLUT1 (Slc2a1) and in particular to GLUT2 (Slc2a2), but still detectable (Fig. 4 a-d). Consistently, Slc5a2 expression, as well as SGLT3a (Slc5a4a) and SGLT3a (Sglt4b), was below detection limit in sorted α, β, δ from the mouse, whereas GLUT1 and GLUT2 were expressed at varying levels depending on the cell type (Fig. 4c). In the mouse, low levels of SGLT1 were detected in β and δ-cells, but not in α-cells. As positive control, we used the same respective primer sets to amplify SGLT1 and SGLT2 in mouse, rat and human kidney tissue. In all cases, high expression was detected (Fig. 4 a,b and d). In addition to the qPCR-based expression analysis on human islets, we investigated the expression of glucose transporters in dispersed islet cells, using publicly available RNA sequencing data. Population 1 consisted of donor tissue from both non-diabetic and type-2-diabetic donors) whereas population 2 only included non-diabetic donors. In both populations, SGLT2 expression was practically absent in all α, β, and δ-cells, and expression was not altered in cells from patients with type 2 diabetes (Fig. 5a and b). SGLT1 was expressed in α-cells in both human populations, and the expression was up regulated approximately 1.5 fold in type-2-diabetic donors (Fig. 5a, P<0.0001). GLUT1 was highly expressed in all three cell types in all two populations, whereas GLUT2 and 3 were mostly expressed by β-cells (Fig. 5a and b). Expression of GLUT1-5 was not statistically different between non-diabetic and type-2-diabetic donors. Consistent with the low expression level, SGLT2 protein was not detected in rat and human islet lysates or in pancreatic islets from mice, rats or humans using immunohistochemistry as detection methodSGLT2 was, however, detected in kidney tissue (positive control) by both Western blot and immunohistochemistry (Fig. 5c and 6; uncropped Western blots are shown in ESM Fig. 4).
Figure 4. Expression of glucose-transporters in rat, human and mouse pancreatic islets.
Data are presented as mean values ±SEM. Relative expression levels of SGLT1, SGLT2, SGLT3a/3b and GLUT1-5 in rat, human and mouse islets are presented as indicated. a: rat islets and rat kidney tissue (positive control), b: Human islets and human kidney (positive control), c: Fractionated expression in α, β, and δ cells from the mouse, d: Mouse islets and mouse kidney (positive control). Expression was assessed by qPCR (a, b, d) or by RNA sequencing (c). n: a= 5, b=3, c=3, d =3.
Figure 5. Expression of glucose-transporters in human α, β, and δ cells and SGLT2 protein in rat and human islets.
a: Single cell expression in human α, β, and δ cells, consisting of both non-diabetic and type-2-diabetic donors (population 1), b:combined single cell expression from two different populations, all non-diabetic donors (population 2). c: Protein level of SGLT2 in protein lysates from human and rat islets and rat kidney tissue lysate (pos. control). Uncropped data are provided in ESM Fig. 4. Expression was investigated by RNA sequencing. n: a=10, b = 26, c=3-5, as indicated. ****p<0.0001. Statistical significance was assessed by One-way ANOVA followed by Bonferroni post hoc test.
Figure 6. Sodium-glucose transporter 2 (SGLT2) stainings in rat, mouse and human pancreas.
Representative images for immunohistochemical stainings against SGLT2 in rat, mouse and human pancreas and kidney (positive control). Top panel shows representative pancraetic slets (indicated with black arrows), bottom panel shows kidney tissue staining. Repressentative images are shown from (n = 3 in all cases). Left side: rat, middle: mouse and right side: human tissue. All pictures are in the same scale. Scale bar is shown in the lower right picture is 100 µm.
Discussion
The use of SGLT2 inhibitors is associated with increased plasma glucagon concentrations, which may limit their therapeutic effectiveness as glucagon is a powerful stimulus for hepatic glucose production, which increases during SGLT2 inhibitor therapy [2, 3, 21]. Based on studies on human islets or from the glucagon secreting cell line α-TC1 it was suggested that the hyperglucagonemia might be a direct effect of the inhibitors on the pancreatic α-cell [5, 22], leading to reduced glucose uptake by the α-cell. Indeed, a mathematical model based on the study by Bonner et al. [5] supported that SGLT2 activity in the α-cell leads to small depolarizations and subsequent inactivation of voltage-gated ion channels, resulting in reduced glucagon secretion [23]. In continuation hereof, attenuation of SGLT2 activity by SGLT2 inhibitors was predicted to partly relieve the suppressive actions of glucose on glucagon secretion [23]. However, this model assumes that SGLT2 is expressed by the α-cell and contrasts to our findings in this study.
We used the physiologically relevant isolated perfused rat pancreas model [7] and found that SGLT2 activity had no effect on glucagon secretion whether transporter activity was inhibited by dapagliflozin/phloridzin or whether it was activated by the SGLT-specific substrate α-MGP. Of note, the dapagliflozin concentration used (0.5 µmol/l) matches peak plasma concentration in humans after intake of therapeutic doses (5-10 mg/day) [24], and in all experiments, secretion was tightly regulated by the glucose concentration so glucagon secretion was high at low glucose. We have previously shown that α-MGP-mediated activation of SGLT1 in the perfused rat small intestine stimulates GLP-1 secretion [25], supporting the use of α-MGP as a suitable experimental tool. Besides being directly regulated by glucose, glucagon secretion is also thought to be regulated by paracrine effects of insulin and/or somatostatin [26–28], but neither insulin nor somatostatin secretion was affected by acute dapagliflozin, phloridzin or α-MGP administration. Our data, therefore, do not support a recent report linking intra-islet cross talk to the activation of SGLT2 in δ-cells downstream of insulin[29], but it is possible that SGLT2 recruitment requires the higher insulin concentrations used in static islet incubation studies, or exhibits species differences.
Our results also contrast the studies by Bonner and Solini [5, 22]. However, although these two studies both report a stimulatory effect on glucagon secretion, they are inconsistent with respect to the suggested mechanisms of action. Thus, one [5] showed expression of SGLT2 in human islets and concluded that the stimulatory effect of dapagliflozin on glucagon secretion was attributable to a direct effect of SGLT2 inhibition at the level of the α-cell, whereas in the other [22] SGLT2 expression was nearly undetectable in human pancreatic islets, mouse islets and the α-TC1 cell line. Instead, the authors found that dapagliflozin acutely resulted in up regulation of SGLT1 expression, which they concluded leads to increased glucose-stimulated glucagon secretion through a SGLT1 dependent mechanism [22]. Similar conclusion have been reached by another group[30]. The inconsistency between our study and the two previous studies is difficult to explain, but the lack of responses to dapagliflozin is unlikely to be dose-related, as the concentration we used was almost 500 times higher than the IC50 for SGLT2, and it is also unlikely to reflect inactivity of the dapagliflozin or phloridzin used in these in vitro experiments, since both compounds eliminated glucose-sensitive currents across intestinal mucosal preparations in Ussing chambers. Instead, the inconsistencies between our studies may be related to differences between the use of the intact perfused pancreas and static incubations of isolated islets from which secreted peptides and co-secreted molecules (both metabolites and active molecules like somatostatin) accumulate in the medium and may feedback influence further secretion, whereas with perfusion secreted molecules are instantly removed like in vivo. Supporting this, in a study with perifusion of mouse islets both insulin and glucagon secretion was similar between global SGLT2 knockout mice and wildtype littermates[31]. In another study, employing an experimental setup similar to ours, dapagliflozin suppressed glucagon secretion from perfused rat pancreata perfused at 2.5 mmol/l glucose. However, these studies were carried out in type-1-diabetic rats, and the relevance of this observation for normal or type-2-diabetic islets warrants further investigation[32]. To investigate whether the inconsistencies between the two studies reporting acute stimulatory effects on glucagon secretion [5, 22] and our present findings could result from inter-species differences, we investigated SGLT1 and 2 expression in rat, mouse and human islets as well as in mouse and human α, β, δ-cells as well. For comparison, expression of GLUT1-5 was also investigated. In rat, human and mouse islets, SGLT2 expression was below detection limit and so was the expression in fractionated mouse α, β, δ-cells. In human islet cells from both non-diabetic and diabetic donors, expression was below detection limit in (>98%) of the investigated α-cells and expression levels were low in the few positive cells. Moreover, SGLT2 protein was not detected by Western blot or immunohistochemistry in rat, mouse and human pancreatic extracts/islets, while clear signals were evident in the control tissue (kidney). Our results agree with those of Solini et al. showing no detectable SLGT2 in mouse and human islets [22], but disagree with those of Bonner et al. [5]. However, in the latter, expression levels were only provided as relative levels (comparing levels in different groups of individuals), making it impossible to assess whether expression was high or close to detection limit. Furthermore, the data cannot easily be reproduced as the primer sets employed are not listed and comparisons to the primary glucose transporters GLUT1 and 2 are also lacking, again making the interpretation of these results difficult. In addition, the signal detected by Bonner et al. may reflect non-protein coding SGLT2 transcripts as there are two additional overlapping genes (AC026471.6 and C16orf58) at the SGLT2 locus that may contribute to the signal, depending on the annealing sites of the primers. Indeed, we found C16orf58 to be highly expressed in all islet cell types (ESM Fig. 3). Furthermore, for SGLT2 there may be expression of several non-protein coding transcript variants and our RNA-sequencing-based analysis (on population 1) identified seven putatively expressed SGLT2 transcript variants in islet cells (based on ENSEMBL build hg38), among which only one codes for full-length protein-coding SGLT2, and this was generally low or undetectable in all cells. In an initial round of qPCR in human islets, we detected very high SGLT2 expression (ESM Fig. 2) but later found by sequence analysis that the first primer set annealed to a sequence that overlapped with eight different SGLT2 transcript variants that did not code for full-length protein-coding SGLT2 protein. Consistently, subsequent sequencing of the amplicon confirmed that irrelevant transcripts of non-coding SGLT2 variants had been amplified. Our results suggest that the lack of SGLT2-activity modulation on glucagon secretion measured using the isolated perfused rat pancreas is unlikely to be a species-dependent phenomenon. Rather, the increased circulating glucagon levels observed in patients treated with SGLT2 inhibitors may result from the glucose-lowering effect of the drugs which in itself would be expected to increase glucagon secretion. In support of this, dapagliflozin did not increase plasma glucagon concentrations measurably in mice, rats or humans under clamped isoglycemic conditions [30, 32, 33], although in another study in humans, dapagliflozin, but not placebo, increased plasma glucagon concentrations[2]. At any rate, the clinically relevant question is whether endogenous glucose production (EGP) caused by SGLT2 inhibitors is mediated downstream of increased glucagon secretion or by other mechanisms. In this context, it should be considered that the reported increases in plasma glucagon are marginal (0.5-1.5 pM) [2, 3, 21], and perhaps too small to cause a quantitatively relevant increase in EGP. In support of this, a recent study in humans concluded that increased EGP after SGLT2 inhibition resulted from the glucose-lowering actions rather than from direct effects on glucagon and insulin secretion [33].
Supplementary Material
Tweet.
Sodium-glucose transporter-2 (SGLT2) activity does not regulate glucagon, insulin or somatostatin secretion from perfused rat pancreas and expression is marginal or undetectable in islets from mouse, rat and humans and in mouse and human alpha-cells.
#glucagon-secretion, #islets, #perfusedratpancreas, #SGLT2, #T2D. @UCPH_health.
Please use fig. 1 as “tweet” figure.
Research in context.
What is already known about this subject?
-
⊠
Sodium-glucose transporter-2 inhibitors (SGLT2i) lower blood glucose but lead to plasma glucagon increases, which may counteract their efficacy.
-
⊠
It has been reported that SGLT2 is expressed by α-cells and that SGLT2i stimulate glucagon secretion from static-incubated human islets and from a murine α-cell line, α-TC1. However, it remains controversial whether SGLT2i-mediated increase in plasma glucagon results from direct or indirect effects on the α-cells.
What is the key question?
Is SGLT2 really expressed by the α-cells and does SGLT2i stimulate glucagon secretion in a physiologically relevant model?
What are the new findings?
-
⊠
SGLT2 inhibition had no effects on glucagon secretion from perfused rat pancreas whether at high or low glucose concentrations.
-
⊠
SGLT2 expression was marginal in rat, mouse and human islets and in mouse and human α-, β-, and δ-cells.
-
⊠
Slc5a2 (SGLT2 gene) overlaps with two highly expressed unrelated genes (AC026471.6 and C16orf58). Previous detection of Slc5a2 in α-cells may therefore reflect expression of these genes.
How might this impact on clinical practice in the foreseeable future?
The stimulatory actions of SGLT2i on glucagon secretion are not a result of interference with SGLT2 activity by the α-cell. The effectiveness of SGLT2i is therefore not compromised by off-target effects on the α-cell.
Acknowledgements
We thank Mark Lal for providing the human kidney tissue.
Funding
Rune E. Kuhre was supported by a postdoc scholarship from the Lundbeck foundation (Lundbeckfonden, R264-2017-3492). Lihua Chen was supported by a postdoc scholarship from the AstraZeneca postdoc program. The isolated perfused rat pancreas studies, immunohistochemistry, qPCR on human and rat islets and Western blot were supported by an unrestricted grant to Prof. Jens Juul Holst from the Novo Nordisk Center for Basic Metabolic Research (Novo Nordisk Foundation, Denmark), a separate grant from the Novo Nordisk Foundation (grant no. NNF15OC0016574), a grant to Prof. Holst from the European Research Council (Grant no.695069) and the European Union’s Seventh Framework Programme for Research, Technological Development, and Demonstration Activities (Grant No. 266408). Gene expression analysis on mouse tissue was supported by grants to Frank Reimann and Fiona M. Gribble from: grants to Frank Reimann and Fiona M. Gribble from Wellcome (106262/Z/14/Z and 106263/Z/14/Z) and the MRC (MRC_MC_UU_12012/3). The study sponsors had no involvement in the conception of study, study design, interpretation of data or writing of the manuscript. Prof. Holst is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Abbreviations
- EGP
Endogenous glucose production
- α-MGP
methyl-α-D-glucopyranoside
- IScc
short circuit current
- SGLT2
Sodium-glucose transporter-2
Footnotes
Data availability
Data are available upon request to Prof. Jens Juul Holst.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript. AA, LC and BT are employed by AstraZeneca. AstraZeneca had no involvement in the conception of study, design and execution of experiments, interpretation of data or writing of the manuscript.
Contributions
REK and JJH: conception of study. REK and DBA performed isolated perfused rat pancreas experiments and assayed for glucagon, insulin and somatostatin concentrations. REK performed using chamber experiments, and constructed figures. REK and JJH: interpreted pancreas perfusion data. SMG and TM-P did qPCR expression and Western blot analysis on rat and human islets/kidney: production of data and interpretation of these. AA and BT did the glucose-transporter analysis on sorted human alpha-, beta- and delta-cells, and population 1. LC did qPCR analyses of human kidney. NW provided intellectual content. NJWA did the expression analysis of glucose transporters, population 2. CØ performed and interpreted the immunohistochemistry on mouse, rat and human pancreas and kidney. AEA, FMG and FR did all work related to the expression of SGLT2 and other glucose transporters in mouse pancreatic cells: production of data and interpretation of these. REK drafted the manuscript. REK, SMG, AEA, DBA, AA, NJWA, CØ, TM-P, FMG, FR, NW, BT and JJH critical revised and edited the manuscript. All authors approved the final version of the manuscript.
References
- [1].Cuypers J, Mathieu C, Benhalima K. SGLT2-inhibitors: a novel class for the treatment of type 2 diabetes introduction of SGLT2-inhibitors in clinical practice. Acta clinica Belgica. 2013;68:287–293. doi: 10.2143/ACB.3349. [DOI] [PubMed] [Google Scholar]
- [2].Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. The Journal of clinical investigation. 2014;124:509–514. doi: 10.1172/JCI70704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ferrannini E, Muscelli E, Frascerra S, et al. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. The Journal of clinical investigation. 2014;124:499–508. doi: 10.1172/JCI72227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Martinez R, Al-Jobori H, Ali AM, et al. Endogenous Glucose Production and Hormonal Changes in Response to Canagliflozin and Liraglutide Combination Therapy. Diabetes. 2018;67:1182–1189. doi: 10.2337/db17-1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bonner C, Kerr-Conte J, Gmyr V, et al. Inhibition of the glucose transporter SGLT2 with dapagliflozin in pancreatic alpha cells triggers glucagon secretion. Nature medicine. 2015;21:512–517. doi: 10.1038/nm.3828. [DOI] [PubMed] [Google Scholar]
- [6].Kuhre RE, Wewer Albrechtsen NJ, Larsen O, et al. Bile acids are important direct and indirect regulators of the secretion of appetite- and metabolism-regulating hormones from the gut and pancreas. Molecular metabolism. 2018;11:84–95. doi: 10.1016/j.molmet.2018.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Christiansen CB, Svendsen B, Holst JJ. The VGF-Derived Neuropeptide TLQP-21 Shows No Impact on Hormone Secretion in the Isolated Perfused Rat Pancreas. Hormone and metabolic research = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 2015;47:537–543. doi: 10.1055/s-0034-1395615. [DOI] [PubMed] [Google Scholar]
- [8].Kuhre RE, Frost CR, Svendsen B, Holst JJ. Molecular mechanisms of glucose-stimulated GLP-1 secretion from perfused rat small intestine. Diabetes. 2014;64:370. doi: 10.2337/db14-0807. [DOI] [PubMed] [Google Scholar]
- [9].Meng W, Ellsworth BA, Nirschl AA, et al. Discovery of dapagliflozin: a potent, selective renal sodium-dependent glucose cotransporter 2 (SGLT2) inhibitor for the treatment of type 2 diabetes. Journal of medicinal chemistry. 2008;51:1145–1149. doi: 10.1021/jm701272q. [DOI] [PubMed] [Google Scholar]
- [10].Nielsen JH, Svensson C, Galsgaard ED, Moldrup A, Billestrup N. Beta cell proliferation and growth factors. Journal of molecular medicine (Berlin, Germany) 1999;77:62–66. doi: 10.1007/s001090050302. [DOI] [PubMed] [Google Scholar]
- [11].Ghiasi SM, Krogh N, Tyrberg B, Mandrup-Poulsen T. The No-Go and Nonsense-Mediated RNA Decay Pathways Are Regulated by Inflammatory Cytokines in Insulin-Producing Cells and Human Islets and Determine beta-Cell Insulin Biosynthesis and Survival. Diabetes. 2018;67:2019–2037. doi: 10.2337/db18-0073. [DOI] [PubMed] [Google Scholar]
- [12].Adriaenssens AE, Svendsen B, Lam BY, et al. Transcriptomic profiling of pancreatic alpha, beta and delta cell populations identifies delta cells as a principal target for ghrelin in mouse islets. Diabetologia. 2016;59:2156–2165. doi: 10.1007/s00125-016-4033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Segerstolpe A, Palasantza A, Eliasson P, et al. Single-Cell Transcriptome Profiling of Human Pancreatic Islets in Health and Type 2 Diabetes. Cell metabolism. 2016;24:593–607. doi: 10.1016/j.cmet.2016.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kim D, Langmead B, Salzberg SL. HISAT: a fast spliced aligner with low memory requirements. Nature methods. 2015;12:357–360. doi: 10.1038/nmeth.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Patro R, Duggal G, Love MI, Irizarry RA, Kingsford C. Salmon provides fast and bias-aware quantification of transcript expression. Nature methods. 2017;14:417–419. doi: 10.1038/nmeth.4197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Xin Y, Kim J, Okamoto H, et al. RNA Sequencing of Single Human Islet Cells Reveals Type 2 Diabetes Genes. Cell metabolism. 2016;24:608–615. doi: 10.1016/j.cmet.2016.08.018. [DOI] [PubMed] [Google Scholar]
- [17].Muraro MJ, Dharmadhikari G, Grun D, et al. A Single-Cell Transcriptome Atlas of the Human Pancreas. Cell systems. 2016;3:385–394.e383. doi: 10.1016/j.cels.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Orskov C, Jeppesen J, Madsbad S, Holst JJ. Proglucagon products in plasma of noninsulin-dependent diabetics and nondiabetic controls in the fasting state and after oral glucose and intravenous arginine. The Journal of clinical investigation. 1991;87:415–423. doi: 10.1172/JCI115012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Brand CL, Jorgensen PN, Knigge U, et al. Role of glucagon in maintenance of euglycemia in fed and fasted rats. The American journal of physiology. 1995;269:E469–477. doi: 10.1152/ajpendo.1995.269.3.E469. [DOI] [PubMed] [Google Scholar]
- [20].Holst JJ, Bersani M. Assays for Peptide Products of Somatostatin Gene Expression. Metods Neurosciences. 1991;5:3–22. [Google Scholar]
- [21].Martinez F, Rizza R, Romero J. High-fructose feeding elicits insulin resistance, hyperinsulinism, and hypertension in normal mongrel dogs. Hypertension. 1994;23:456–463. doi: 10.1161/01.hyp.23.4.456. [DOI] [PubMed] [Google Scholar]
- [22].Solini A, Sebastiani G, Nigi L, Santini E, Rossi C, Dotta F. Dapagliflozin modulates glucagon secretion in an SGLT2-independent manner in murine alpha cells. Diabetes Metab. 2017;43:512–520. doi: 10.1016/j.diabet.2017.04.002. [DOI] [PubMed] [Google Scholar]
- [23].Pedersen MG, Ahlstedt I, El Hachmane MF, Gopel SO. Dapagliflozin stimulates glucagon secretion at high glucose: experiments and mathematical simulations of human A-cells. Scientific reports. 2016;6:31214. doi: 10.1038/srep31214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kasichayanula S, Liu X, Lacreta F, Griffen SC, Boulton DW. Clinical pharmacokinetics and pharmacodynamics of dapagliflozin, a selective inhibitor of sodiumglucose co-transporter type 2. Clinical pharmacokinetics. 2014;53:17–27. doi: 10.1007/s40262-013-0104-3. [DOI] [PubMed] [Google Scholar]
- [25].Kuhre RE, Bechmann LE, Wewer Albrechtsen NJ, Hartmann B, Holst JJ. Glucose stimulates neurotensin secretion from the rat small intestine by mechanisms involving SGLT1 and GLUT2, leading to cell depolarization and calcium influx. American journal of physiology Endocrinology and metabolism. 2015;308:E1123–1130. doi: 10.1152/ajpendo.00012.2015. [DOI] [PubMed] [Google Scholar]
- [26].de Heer J, Rasmussen C, Coy DH, Holst JJ. Glucagon-like peptide-1, but not glucose-dependent insulinotropic peptide, inhibits glucagon secretion via somatostatin (receptor subtype 2) in the perfused rat pancreas. Diabetologia. 2008;51:2263–2270. doi: 10.1007/s00125-008-1149-y. [DOI] [PubMed] [Google Scholar]
- [27].Cooperberg BA, Cryer PE. Insulin reciprocally regulates glucagon secretion in humans. Diabetes. 2010;59:2936–2940. doi: 10.2337/db10-0728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Cejvan K, Coy DH, Efendic S. Intra-islet somatostatin regulates glucagon release via type 2 somatostatin receptors in rats. Diabetes. 2003;52:1176–1181. doi: 10.2337/diabetes.52.5.1176. [DOI] [PubMed] [Google Scholar]
- [29].Vergari E, Knudsen JG, Ramracheya R, et al. Insulin inhibits glucagon release by SGLT2-induced stimulation of somatostatin secretion. Nature communications. 2019;10:139. doi: 10.1038/s41467-018-08193-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Suga T, Kikuchi O, Kobayashi M, et al. SGLT1 in pancreatic alpha cells regulates glucagon secretion in mice, possibly explaining the distinct effects of SGLT2 inhibitors on plasma glucagon levels. Molecular metabolism. 2018;19:1–12. doi: 10.1016/j.molmet.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Jurczak MJ, Lee HY, Birkenfeld AL, et al. SGLT2 deletion improves glucose homeostasis and preserves pancreatic beta-cell function. Diabetes. 2011;60:890–898. doi: 10.2337/db10-1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Wang MY, Yu X, Lee Y, et al. Dapagliflozin suppresses glucagon signaling in rodent models of diabetes. Proceedings of the National Academy of Sciences of the United States of America. 2017;114:6611–6616. doi: 10.1073/pnas.1705845114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Lundkvist P, Pereira MJ, Kamble PG, et al. Glucagon Levels During Short-Term SGLT2 Inhibition Are Largely Regulated by Glucose Changes in Patients With Type 2 Diabetes. The Journal of clinical endocrinology and metabolism. 2019;104:193–201. doi: 10.1210/jc.2018-00969. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.