Abstract
Purpose
To report anterior segment evaluation in patients with mucopolysaccharidosis 1 using anterior segment optical coherence tomography and in vivo confocal microscopy.
Observations
Case 1 involved a 26-year-old man with mucopolysaccharidosis 1 Hurler–Scheie syndrome who presented with a corrected distance visual acuity of 20/67 in the right eye and 20/50 in the left eye because of bilateral corneal opacification. He had undergone bone marrow transplantation at the age of 7 years. Anterior segment optical coherence tomography revealed a very narrow anterior chamber angle; a flat, thickened cornea; and astigmatism with the rule. Confocal microscopy demonstrated hyper-refractive deposits in the corneal epithelial basal layer, decreased subepithelial nerves, and depletion of keratocytes in the anterior and posterior stroma. Endothelial cells were not visible.
Case 2 involved an 18-year-old woman who presented with increased corneal opacity in both eyes. Her medical history included mucopolysaccharidosis 1 Hurler syndrome and bone marrow transplantation at the age of 2 years. Her corrected distance visual acuity could not be measured because of severe intellectual disability. Anterior segment optical coherence tomography demonstrated a flat and thick cornea.
Conclusions and importance
Anterior segment optical coherence tomography can provide detailed morphological information for the anterior segment in patients with severe corneal opacification associated with mucopolysaccharidosis 1. Moreover, in vivo confocal microscopy facilitates the detailed observation of corneal cellular changes. Thus, these tools can provide data that would contribute to an increased understanding of corneal changes in patients with mucopolysaccharidosis 1.
Keywords: Mucopolysaccharidosis, Anterior segment optical coherence tomography, In vivo confocal microscopy
1. Introduction
Mucopolysaccharidosis type 1 (MPS1) is an autosomal recessive disease characterized by the accumulation of heparin sulfate and dermatan sulfate due to the loss of α-L-iduronidase.1 MPS1 is further divided into three subgroups according to the presentation and severity of symptoms: Hurler syndrome, Hurler–Scheie syndrome, and Sheie syndrome. Systemic treatments include enzyme replacement therapy and hematopoietic stem cell transplantation. Patients with MPS1 often develop corneal opacification that can be successfully treated by keratoplasty.2
Here, we describe the use of anterior segment optical coherence tomography (AS-OCT) and in vivo confocal microscopy for evaluation of the anterior segment in two cases of MPS1. To the best of our knowledge, this is the first report on the use of AS-OCT for morphological analysis of the anterior segment in patients with MPS1.
2. Findings
2.1. Case 1
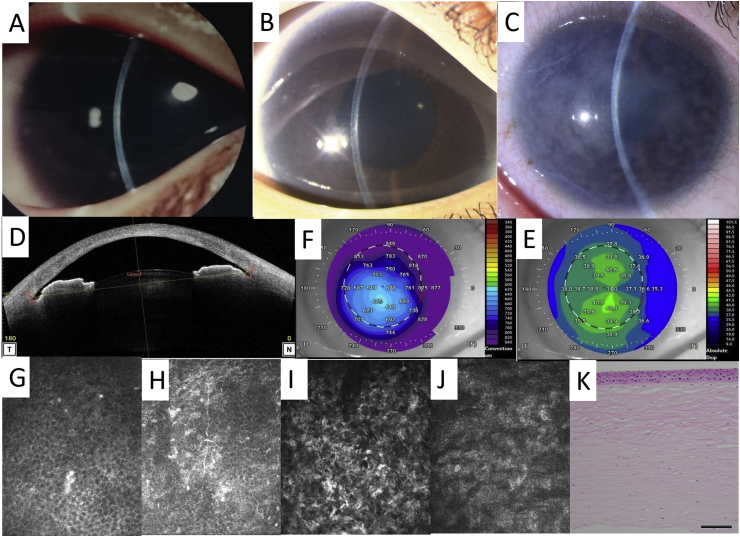
A 26-year-old man with MPS1 Hurler–Scheie syndrome presented with decreased visual acuity. He had received bone marrow transplantation at the age of 7 years, and bilateral corneal opacification was first documented at the age of 5 years, following which it gradually worsened with age (Fig. 1 A–C). The corrected distance visual acuity (CDVA) was 20/67 in the right eye and 20/50 in the left eye. The spherical equivalents were +0.75 and + 2.0 diopters, respectively. AS-OCT (CASIA2; Tomey, Nagoya, Japan) revealed a very narrow anterior chamber angle (Fig. 1 D). The temporal angle-opening distance (AOD 500) was 0.143 mm. In addition, the cornea appeared thick and flat, and astigmatism with the rule was observed (Fig. 1E and F). In vivo confocal microscopy using the Rostock Corneal Module (HRTIII; Heidelberg Engineering GmbH, Dossenheim, Germany) demonstrated hyper-refractive deposits in the corneal epithelial basal layer, decreased subepithelial nerves, and depletion of keratocytes in the anterior and posterior stroma (Fig. 1 G–J). Endothelial cells were not visible. Glaucoma and retinal degeneration were not present.
Fig. 1.
Anterior segment findings in the right eye of a 26-year-old man with mucopolysaccharidosis type 1 Hurler-Scheie syndrome
(A, B, C) Slit-lamp photographs of the right eye obtained at the age of 5 (A), 9 (B), and 26 (C) years
(D, E, F) A B-scan (D), a corneal topography shown by axial map (E), and a pachymetry map generated by anterior segment optical coherence tomography (F). (G, H, I, J) In vivo confocal microscopy showing the corneal basal epithelium (G), subepithelial nerve layer (H), anterior stroma (I), and posterior stroma (J) (K)Hematoxylin–eosin staining of the excised corneal button
Bar = 200 um.
Deep anterior lamellar keratoplasty was performed for both eyes, following which CDVA in the right and left eyes recovered to 20/50 and 20/33, respectively. Hematoxylin–eosin staining of the excised corneal button revealed a decrease in the number of keratocytes. The findings were not consistent with those of in vivo confocal microscopy, probably because of the corneal opacification.
2.2. Case 2
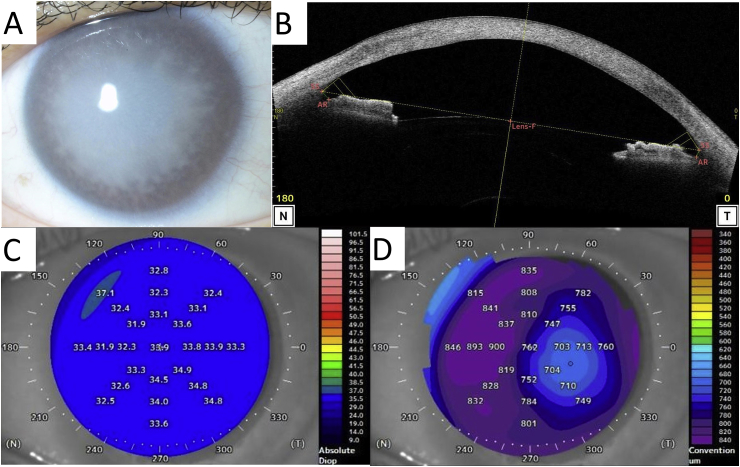
An 18-year-old woman presented with progressive bilateral corneal opacities (Fig. 2 A). Her medical history included MPS1 Hurler syndrome and bone marrow transplantation at the age of 2 years. CDVA could not be measured because of the lack of co-operation due to severe intellectual disability. AS-OCT (CASIA2; Tomey) revealed a flat, thickened cornea with a wide anterior chamber angle (Fig. 2B and C, D). It was impossible to confirm other ocular comorbidities because of severe corneal opacification.
Fig. 2.
Corneal findings in the left eye of an 18-year-old woman with mucopolysaccharidosis type 1 Hurler syndrome
(A) A slit-lamp photograph of the left eye
(B, C, D) A B-scan (B), the corneal topography shown by an axial map (C), and a pachymetry map generated by anterior segment optical coherence tomography (D).
3. Discussion
We experienced two cases of MPS1 complicated by severe corneal opacification even after bone marrow transplantation. AS-OCT revealed similar morphological characteristics, including a flat, thickened cornea and regular astigmatism, in both cases. Patients with MPS1 reportedly exhibit reduced corneal refraction and hyperopic changes,3 which are presumably caused by the accumulation of glycosaminoglycans in the corneal stroma, with subsequent corneal swelling and increased rigidity. Therefore, a blue topography map with a low keratometric value could be a useful imaging biomarker for MPS. In addition, increased corneal haze detected by the Pentacam imaging system has already been reported.4 AS-OCT uses infrared light with a wavelength that is longer than that of light used by the Pentacam, and it can evaluate the morphology of the posterior corneal surface, which is necessary for generating a pachymetry map. This imaging modality is considered useful for preoperative evaluation in patients scheduled for deep anterior lamellar keratoplasty, considering the importance of precise evaluation of the corneal thickness in order to prevent intraoperative perforation. Furthermore, assessment of the intensity of the cornea can be helpful for determining the timing of keratoplasty.
Aragona et al.5 found that confocal microscopy showed basal epithelial cells with diffuse or granular hyper-reflectivity. Highly reflective keratocytes resulting in a web-shaped stromal appearance were also observed, while endothelial cells were barely visible. Case 1 described in the present report showed similar findings for the basal epithelial cells and endothelial cells, although the stromal changes were more severe, possibly because of the higher disease severity. There could be two possible reasons for the decrease in subepithelial nerves observed by confocal microscopy: an actual decrease in the nerves or difficulty in observation of the nerves because of increased intensity of the cornea.
4. Conclusions
In conclusion, the findings from our cases suggest that AS-OCT can provide detailed morphological information for the anterior segment of patients with severe corneal opacification associated with MPS1. Moreover, in vivo confocal microscopy facilitates the detailed observation of corneal cellular changes. Thus, these tools can provide data that would contribute to an increased understanding of corneal changes in patients with MPS1.
Patient consent
The patients who are the subjects of these Case reports provided informed consent for publication of this report.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Declaration of competing interest
The authors declare no conflicts of interest related to the submitted manuscript.
Acknowledgements
None.
References
- 1.Muenzer J., Wraith J.E., Clarke L.A. Mucopolysaccharidosis I: management and treatment guidelines. Pediatrics. 2009;123(1):19–29. doi: 10.1542/peds.2008-0416. [DOI] [PubMed] [Google Scholar]
- 2.Ohden K.L., Pitz S., Ashworth J. Outcomes of keratoplasty in the mucopolysaccharidoses: an international perspective. Br J Ophthalmol. 2017;101(7):909–912. doi: 10.1136/bjophthalmol-2016-308807. [DOI] [PubMed] [Google Scholar]
- 3.Fahnehjelm K.T., Tornquist A.L., Winiarski J. Ocular axial length and corneal refraction in children with mucopolysaccharidosis (MPS I-Hurler) Acta Ophthalmol. 2012;90(3):287–290. doi: 10.1111/j.1755-3768.2010.01934.x. [DOI] [PubMed] [Google Scholar]
- 4.Elflein H.M., Hofherr T., Berisha-Ramadani F. Measuring corneal clouding in patients suffering from mucopolysaccharidosis with the Pentacam densitometry programme. Br J Ophthalmol. 2013;97(7):829–833. doi: 10.1136/bjophthalmol-2012-302913. [DOI] [PubMed] [Google Scholar]
- 5.Aragona P., Wylegala E., Wroblewska-Czajka E. Clinical, confocal, and morphological investigations on the cornea in human mucopolysaccharidosis IH-S. Cornea. 2014;33(1):35–42. doi: 10.1097/ICO.0000000000000005. [DOI] [PubMed] [Google Scholar]