Abstract
Examination of changes in hypertension awareness, treatment, and control (i.e., the hypertension control cascade) by population subgroup can inform targeted efforts to improve hypertension control and reduce disparities. We analyzed 1999–2016 data from the National Health and Nutrition Examination Survey and examined trends across 6-year periods in hypertension awareness, treatment, and control by age, sex, and race/ethnicity. We included 39,589 participants (16,141 with hypertension). Hypertension awareness, treatment, and control increased from 1999 to 2016 among all age groups. However, there were few changes after 2010. Across all time periods, awareness, treatment, and control were higher among younger women (ages 25–44 years) than among younger men, while control was higher among older men (ages ≥65 years) than among older women. Hypertension control was persistently lower for blacks than for whites of all ages, and awareness, treatment, and control were lower among younger Hispanics. There have been few changes in hypertension awareness, treatment, and control since 2010. Disparities in hypertension control by sex highlight the need for effective interventions among younger men and older women. Concerted efforts are also needed to reduce persistent racial/ethnic disparities, particularly to improve treatment control among blacks and to further address gaps at all stages among younger Hispanics.
Keywords: blood pressure, health disparities, hypertension, surveillance
Hypertension (blood pressure ≥140/90 mm Hg) is a leading modifiable risk factor for cardiovascular disease, the number 1 cause of death in the United States and globally (1). Further, there are long-standing racial/ethnic disparities in cardiovascular risk factors, particularly hypertension (2).
The hypertension control cascade, which includes hypertension awareness, treatment, and control, has been proposed as a framework for improving blood pressure control in the population (3). The proportion of adults with hypertension who have their blood pressure controlled (<140/90 mm Hg) increased from the late 1990s through 2010 due to increases in both awareness of hypertension and control among those treated (4, 5).
However, national data show that there has been no change since, and currently, less than half of all US adults with hypertension have their blood pressure controlled (6). This plateau has occurred despite increased knowledge of effective strategies at the organizational, provider, and patient levels to improve control of hypertension (7). Communities (5) and health-care systems (8) around the country have demonstrated that it is possible to achieve much higher rates of blood pressure control, and with concerted efforts, it should be possible to reach 70% hypertension control in the population (9).
It is unclear whether the recent lack of progress in hypertension control is attributable to a lack of progress at a particular stage in the cascade and whether patterns are uniform across major demographic groups. Previous research has shown that barriers to hypertension control differ by age, sex, and race/ethnicity (3, 10). Additionally, there are a number of contextual changes which may have influenced approaches to hypertension management for different patient subgroups in recent years. Such changes include increases in the prevalence of obesity and diabetes, expanded insurance coverage, and the publication of multiple clinical practice guidelines for hypertension (11–14).
Understanding changes over time in hypertension awareness, treatment, and control overall and among different subpopulations can inform targeted efforts to improve hypertension management and reduce disparities. We conducted serial cross-sectional analyses of the most recent national data available from the National Health and Nutrition Examination Survey (NHANES) to better understand changes in the hypertension control cascade over time, overall and by subgroup.
METHODS
Data source
NHANES is a population-based survey which uses stratified, multistage probability sampling to produce nationally representative estimates of the civilian, noninstitutionalized population of the United States. The survey includes interview and examination components. Since 1999, NHANES data have been released in 2-year cycles. We analyzed data from 1999–2016.
Study population
There were 41,511 nonpregnant adults aged ≥25 years who completed the examination component of the survey. Participants who did not have at least 1 blood pressure measurement or for whom hypertension status could not be determined (n = 1,922) were excluded from all analyses. Those with missing data for hypertension status were more likely to be aged 25–44 years or aged ≥65 years (versus the middle age category), female (versus male), and non-Hispanic black, Hispanic, or of other race/ethnicity (versus non-Hispanic white) than those for whom hypertension status could be determined. The final analytical sample included 39,589 participants.
Primary exposure
Blood pressure measurements were obtained during the NHANES examination by trained physicians using a standard study protocol (15). After the participant had rested in a seated position for 5 minutes, 3 consecutive auscultatory blood pressure readings were obtained using a mercury sphygmomanometer and an appropriate-size blood pressure cuff. If a blood pressure measurement was interrupted or incomplete, a fourth attempt was made. All available blood pressure readings (i.e., up to 3 measurements) were used to calculate mean systolic and diastolic blood pressures (16). Hypertension was defined as mean systolic blood pressure ≥140 mm Hg, mean diastolic blood pressure ≥90 mm Hg, or current use of antihypertensive medication.
Outcome assessment
Among persons with hypertension, hypertension awareness was defined on the basis of the participant’s response to the question, “Have you ever been told by a doctor or health professional that you had hypertension, also called high blood pressure?”. Hypertension treatment was defined as self-reported current use of antihypertensive medication based on responses to the questions, “Because of your high blood pressure/hypertension, have you ever been told to take prescribed medicine?” and “Are you now taking prescribed medicine for high blood pressure?”. Hypertension control was defined as blood pressure <140/90 mm Hg; we assessed hypertension control among all persons with hypertension and among those who reported use of antihypertensive medication. We also examined blood pressure levels over time among persons with hypertension and persons with treated hypertension in mutually exclusive categories: <130/80 mm Hg, 130/80 to <140/90 mm Hg, 140/90 to <150/90 mm Hg, and ≥150/90 mm Hg.
Statistical analyses
Because hypertension prevalence varies by age, we stratified analyses by age, categorized as 25–44, 45–64, or ≥65 years. We combined data into 6-year periods to obtain more statistically stable estimates within subpopulations defined by age, sex, and/or race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic). We estimated the prevalence of hypertension and, among persons with hypertension, the prevalences of awareness, treatment, and control, as well as the prevalence of control among those treated. All analyses were weighted to account for the complex survey design and to produce results generalizable to the US population aged 25 years or older. We obtained standard errors using the Taylor series (linearization) method.
Within age groups, we used linear regression models with an indicator variable for survey cycle to assess absolute changes in prevalence during the period 2005–2010 or 2011–2016 as compared with 1999–2004. We used a linear combination of regression coefficients to compare estimates for 2011–2016 with the 2005–2010 period. We included interaction terms to assess whether differences by sex or race/ethnicity changed over time. In supplemental analyses, we also examined trends by 2-year NHANES survey cycle. We used χ2 tests to examine changes across periods by age group among persons with hypertension and among persons with treated hypertension with blood pressure <130/80 mm Hg, 130/80 to <140/90 mm Hg, 140/90 to <150/90 mm Hg, or ≥150/90 mm Hg. Participant blood pressure was categorized using the highest category of systolic or diastolic blood pressure.
To examine trends in hypertension control before and after adjustment for other individual characteristics, we used logistic regression to obtain predictive margins. Within age groups, we calculated the unadjusted prevalence of hypertension control and compared the prevalences of hypertension control across time periods using prevalence ratios. We sequentially adjusted for demographic characteristics (sex, race/ethnicity, age within age group), clinical characteristics (body mass index (weight (kg)/height (m)2) and self-reported diabetes), access to health care (insurance coverage and having a usual source of care), and hypertension awareness. Additionally, among persons who were aware of their hypertension, we adjusted for duration of hypertension. Duration of hypertension was calculated on the basis of the participant’s current age and the age at which they had been told they had hypertension. Information on duration of hypertension was available for 2007 onward; for this analysis, we compared hypertension control in 2011–2016 with that in 2007–2010.
All analyses were conducted in Stata, version 15.1 (StataCorp LLC, College Station, Texas), using the svy command package to account for the complex survey design. We used a 2-sided P value of 0.05 to define statistical significance. The NHANES protocol was approved by the institutional review board of the National Center for Health Statistics, and informed consent was obtained from all participants.
RESULTS
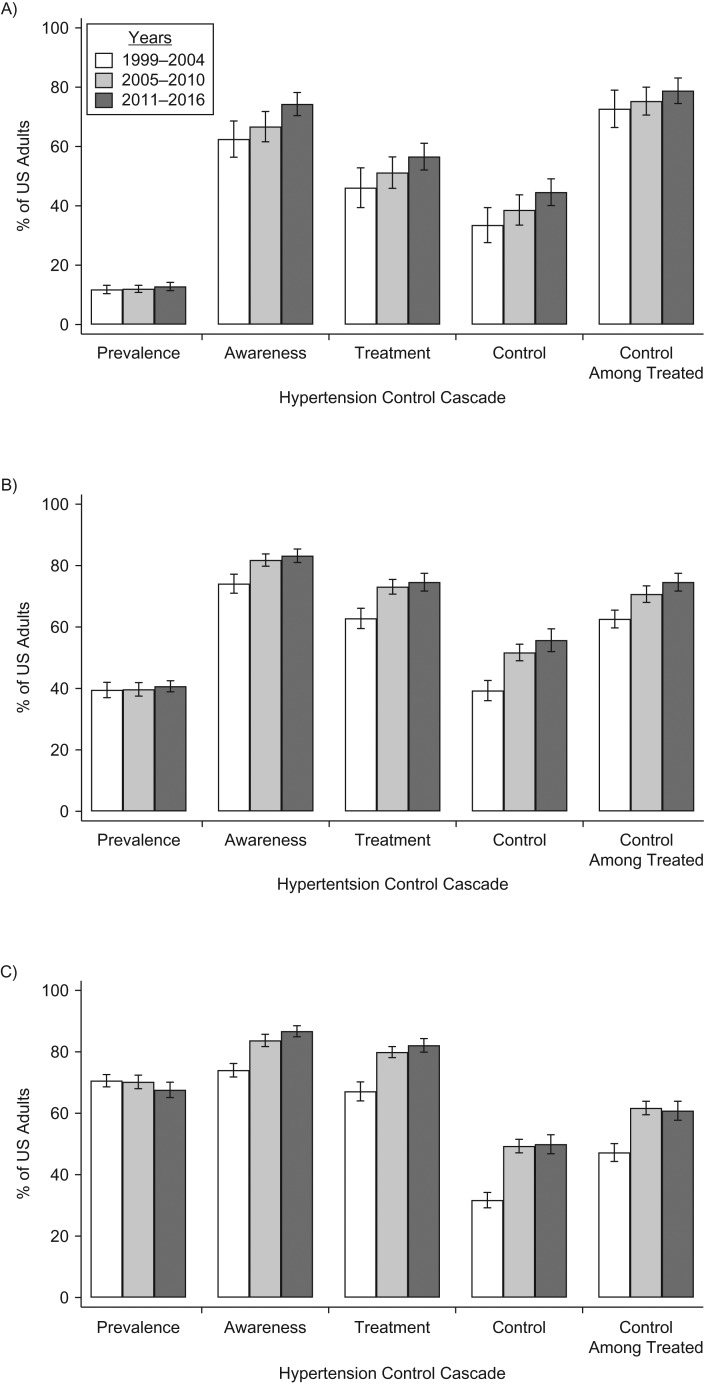
There were 39,589 participants (16,141 with hypertension) included in our analysis. During the study period, there was no significant change in hypertension prevalence in any age group (Figure 1; also see Web Table 1, which is available at https://academic.oup.com/aje).
Figure 1.
Hypertension prevalence, awareness, treatment, control, and control among those treated, by age group, in US adults aged ≥25 years, National Health and Nutrition Examination Survey, 1999–2016. A) Persons aged 25–44 years. Among those with hypertension, hypertension awareness was significantly higher (P < 0.05) in 2011–2016 than in 1999–2004 and 2005–2010. Hypertension treatment was significantly higher in 2011–2016 than in 2005–2010. Hypertension control was significantly higher in 2011–2016 than in 2005–2010. B) Persons aged 45–64 years. Among those with hypertension, hypertension awareness, treatment, control, and control among those treated were significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. C) Persons aged ≥65 years. Among those with hypertension, hypertension awareness was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004 and higher in 2011–2016 than in 2005–2010. Hypertension treatment, control, and control among those treated were significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Bars, 95% confidence intervals.
From 1999–2004 to 2011–2016, hypertension awareness, treatment, and control increased significantly in all age groups. However, changes primarily occurred between 1999–2004 and 2005–2010. Hypertension awareness, treatment, and control increased significantly from 1999–2004 to 2005–2010 among persons aged 45–64 years and ≥65 years. The only significant changes from 2005–2010 to 2011–2016 were increases in awareness among those aged 25–44 years and those aged ≥65 years. Meanwhile, supplemental analyses examining data in 2-year survey cycles showed that there was a significant decrease in hypertension control among persons aged ≥65 years from 2013–2014 to 2015–2016 (−8.2%). There were also significant decreases in hypertension control among those treated from 2013–2014 to 2015–2016 for persons aged 25–44 years (−10.3%) and persons aged ≥65 years (−8.1%) (Web Table 2).
Hypertension control cascade by age group and sex
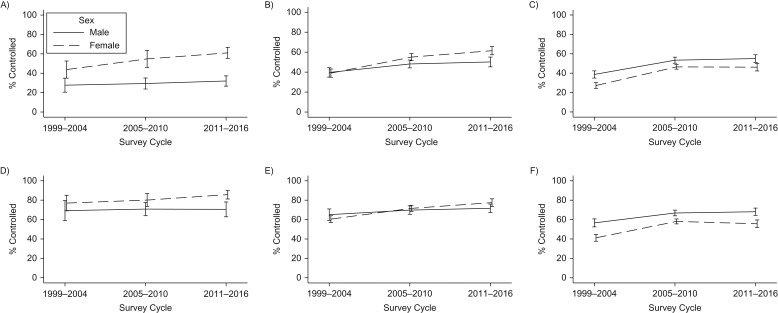
For persons aged 25–44 years, hypertension prevalence was significantly lower among women than among men in all time periods, though this difference was attenuated in the last survey period (Web Table 3, Figure 2). However, across all survey periods, hypertension awareness, treatment, and control were higher among women aged 25–44 years than among men aged 25–44 years. Hypertension control among treated persons was also higher in women than in men, but this difference was not statistically significant.
Figure 2.
Hypertension control among all persons with hypertension (top row) and among persons treated for hypertension (bottom row), by age group and sex, in US adults aged ≥25 years, National Health and Nutrition Examination Survey, 1999–2016. A) Persons aged 25–44 years with hypertension. Among females, hypertension control was significantly higher (P < 0.05) in 2011–2016 than in 1999–2004. Hypertension control was significantly higher among females than among males in 1999–2004, 2005–2010, and 2011–2016. B) Persons aged 45–64 years with hypertension. Among females, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004 and higher in 2011–2016 than in 2005–2010. Among males, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Hypertension control was significantly higher among females than among males in 2005–2010 and 2011–2016. There was a larger difference in hypertension control by sex in 2011–2016 than in 1999–2004. C) Persons aged ≥65 years with hypertension. Among males, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Among females, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Hypertension control was significantly higher among males than among females in 1999–2004, 2005–2010, and 2011–2016. D) Persons aged 25–44 years with treated hypertension. There were no statistically significant changes. E) Persons aged 45–64 years with treated hypertension. Among females with treated hypertension, hypertension control was significantly higher in 2011–2016 than in 1999–2004 and 2005–2010. Among males with treated hypertension, hypertension control was significantly higher in 2011–2016 than in 1999–2004. Among those treated, hypertension control was significantly higher in females than in males in 2011–2016, and the sex difference in hypertension control was significantly different in 2011–2016 than in 1999–2004. F) Persons aged ≥65 years with treated hypertension. Among males and females with treated hypertension, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Among those treated, hypertension control was significantly higher in males than in females in 2005–2010 and 2011–2016. The male-female sex difference in hypertension control among those treated was significantly smaller in 2005–2010 than in 1999–2004. Bars, 95% confidence intervals.
For persons aged 45–64 years, hypertension prevalence was lower among women than among men in 2011–2016 (38.2% vs. 43.3%), a significant change from 1999–2004, when there was no difference in hypertension prevalence. Hypertension awareness, treatment, and control increased among both men and women in this age group during the full study period. Nonetheless, women had higher levels of awareness, treatment, and control in 2005–2010 and 2011–2016. Among women aged 45–64 years, hypertension control and control among those treated significantly increased in both survey periods, and the sex difference in hypertension control and control among those treated was larger in 2011–2016 than in 1999–2004.
For persons aged ≥65 years, the prevalence of hypertension was higher among women than among men in all periods, though the sex differences were smaller in 2005–2010 and 2011–2016 than in 1999–2004. Hypertension awareness, treatment, and control increased among both men and women aged ≥65 years from 1999–2004 to 2011–2016; however, changes primarily occurred from 1999–2004 to 2005–2010. There were no sex differences in awareness or treatment, but hypertension control and control among those treated were lower among women aged ≥65 years than among men aged ≥65 years in all time periods.
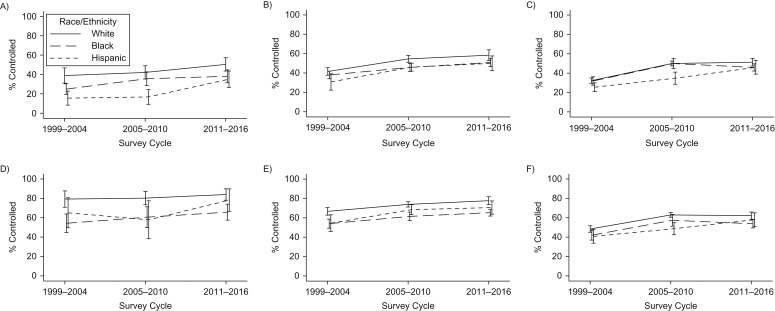
Hypertension control cascade by age group and race/ethnicity
Hypertension prevalence was significantly and consistently higher among blacks than among whites in all age groups and across all survey cycles (Web Table 4, Figure 3). Awareness and treatment were higher among blacks aged 45–64 and ≥65 years than among whites aged 45–64 and ≥65 years at the start of the study period, but there were greater increases in awareness and treatment among whites. By 2011–2016, differences in awareness and treatment by race/ethnicity were no longer statistically significant.
Figure 3.
Hypertension control among all persons with hypertension (top row) and among persons treated for hypertension (bottom row), by age group and race/ethnicity, in US adults aged ≥25 years, National Health and Nutrition Examination Survey, 1999–2016. A) Persons aged 25–44 years with hypertension. Among whites, hypertension control was significantly higher (P < 0.05) in 2011–2016 than in 1999–2004. Among blacks, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Among Hispanics, hypertension control was significantly higher in 2011–2016 than in 1999–2004 and 2005–2010. Hypertension control was significantly higher among whites than among blacks in 1999–2004 and 2011–2016. Hypertension control was significantly higher among whites than among Hispanics in 1999–2004, 2005–2010, and 2011–2016. B) Persons aged 45–64 years with hypertension. Among whites, blacks, and Hispanics, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Hypertension control was significantly higher among whites than among blacks in 1999–2004, 2005–2010, and 2011–2016. Hypertension control was significantly higher among whites than among Hispanics in 1999–2004 and 2005–2010. C) Persons aged ≥65 years with hypertension. Among whites, blacks, and Hispanics, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004; among Hispanics, hypertension control was also significantly higher in 2011–2016 than in 2005–2010. Hypertension control was significantly higher among whites than among blacks in 2011–2016. Hypertension control was significantly higher among whites than among Hispanics in 1999–2004 and 2005–2010, with a larger difference in 2005–2010 than in 1999–2004. D) Persons aged 25–44 years with treated hypertension. Among those with treated hypertension, hypertension control was significantly higher in whites than in blacks in 1999–2004, 2005–2010, and 2011–2016 and significantly higher in whites than in Hispanics in 1999–2004 and 2005–2010. E) Persons aged 45–64 years with treated hypertension. Among whites, blacks, and Hispanics with treated hypertension, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Among those treated, hypertension control was significantly higher in whites than in blacks in 1999–2004, 2005–2010, and 2011–2016. Among those treated, hypertension control was significantly higher in whites than in Hispanics in 1999–2004. F) Persons aged ≥65 years with treated hypertension. Among whites, blacks, and Hispanics with treated hypertension, hypertension control was significantly higher in 2005–2010 and 2011–2016 than in 1999–2004. Among those treated, hypertension control was significantly higher in whites than in blacks in 1999–2004 and 2011–2016. Among those treated, hypertension control was significantly higher in whites than in Hispanics in 2005–2010. Bars, 95% confidence intervals.
Hypertension control and control among those treated were generally lower for blacks than for whites aged 25–44 years and 45–64 years for the duration of the study period. Among those aged ≥65 years, hypertension control was significantly lower among blacks than among whites in 2011–2016, while control among those treated was generally lower throughout the study.
Meanwhile, hypertension prevalences were generally similar among Hispanic and white adults. Hypertension awareness, treatment, and control were lower among Hispanics aged 25–44 years than among whites aged 25–44 years, though there were increases among younger Hispanics between 2005–2010 and 2011–2016. Hypertension control and control among those treated were generally lower for Hispanics than for whites at all ages.
Blood pressure levels by age group
In all age groups, there were differences in the distribution of blood pressure levels among persons with hypertension and persons with treated hypertension during the overall study period (Table 1). Among those aged 25–44 years and 45–64 years, there were favorable changes from 1999–2004 to 2005–2010. The only statistically significant change between 2005–2010 and 2011–2016 was among those aged 45–64 years with treated hypertension.
Table 1.
Distribution (% (Standard Error)) of Blood Pressure Levels Among Persons With Hypertension and Persons With Treated Hypertension, by Age Group, in US Adults Aged ≥25 Years, National Health and Nutrition Examination Survey, 1999–2016
| Age Group (years) and Blood Pressure, mm Hg | Time Period | χ2P Value | ||||
|---|---|---|---|---|---|---|
| 1999–2004 (P1) | 2005–2010 (P2) | 2011–2016 (P3) | ||||
| P2 vs. P1 | P3 vs. P2 | P3 vs. P1 | ||||
| Persons With Hypertension | ||||||
| 25–44 | 0.23 | 0.14 | <0.001 | |||
| <130/80 | 15.3 (1.8) | 21.2 (1.9) | 28.4 (2.2) | |||
| 140/90 | 18.2 (2.2) | 17.4 (1.9) | 16.2 (1.8) | |||
| 150/90 | 18.2 (2.2) | 18.8 (2.2) | 16.8 (1.8) | |||
| ≥150/90 | 48.2 (3.3) | 42.7 (2.9) | 38.6 (2.3) | |||
| 45–64 | <0.001 | 0.13 | <0.001 | |||
| <130/80 | 22.2 (1.2) | 32.3 (1.4) | 37.2 (1.8) | |||
| 140/90 | 17.1 (1.1) | 19.5 (1.1) | 18.4 (1.3) | |||
| 150/90 | 19.4 (1.4) | 19.5 (1.2) | 17.1 (1.4) | |||
| ≥150/90 | 41.3 (1.8) | 28.8 (1.2) | 27.2 (1.4) | |||
| ≥65 | <0.001 | 0.65 | <0.001 | |||
| <130/80 | 17.2 (1.1) | 31.3 (1.1) | 31.6 (1.5) | |||
| 140/90 | 14.3 (0.8) | 18.0 (0.9) | 18.3 (1.1) | |||
| 150/90 | 21.1 (0.9) | 20.0 (1.0) | 21.4 (1.1) | |||
| ≥150/90 | 47.2 (1.5) | 30.7 (1.0) | 28.7 (1.4) | |||
| Persons With Treated Hypertension | ||||||
| 25–44 | 0.34 | 0.14 | 0.002 | |||
| <130/80 | 33.1 (3.2) | 41.3 (2.7) | 50.2 (3.3) | |||
| 140/90 | 39.5 (3.4) | 34.0 (3.1) | 28.6 (2.9) | |||
| 150/90 | 7.3 (1.8) | 6.7 (1.6) | 4.1 (1.1) | |||
| ≥150/90 | 20.0 (2.9) | 18.0 (2.1) | 17.1 (1.9) | |||
| 45–64 | <0.001 | 0.03 | <0.001 | |||
| <130/80 | 35.3 (1.6) | 44.1 (1.6) | 49.9 (2.0) | |||
| 140/90 | 27.2 (1.4) | 26.6 (1.5) | 24.7 (1.6) | |||
| 150/90 | 11.1 (1.1) | 13.0 (0.8) | 9.3 (1.1) | |||
| ≥150/90 | 26.3 (1.5) | 16.3 (1.2) | 16.1 (1.1) | |||
| ≥65 | <0.001 | 0.83 | <0.001 | |||
| <130/80 | 25.8 (1.5) | 39.2 (1.3) | 38.5 (1.7) | |||
| 140/90 | 21.4 (1.1) | 22.5 (1.1) | 22.3 (1.3) | |||
| 150/90 | 15.6 (0.9) | 14.7 (0.8) | 16.1 (1.1) | |||
| ≥150/90 | 37.2 (1.4) | 23.6 (0.9) | 23.1 (1.3) | |||
Abbreviation: P, period.
Trends in hypertension control before and after adjustment for participant characteristics
Within age groups, there was little change in the prevalence ratios for hypertension control when comparing 2005–2010 with 1999–2004, 2011–2016 with 1999–2004, and 2011–2016 with 2005–2010 after adjustment for demographic factors, clinical characteristics, access to health care, and hypertension awareness (Web Table 5). Among persons who were aware of their hypertension, additional adjustment for duration of hypertension did not change the prevalence ratios for hypertension control when comparing 2011–2016 with 2007–2010 (Web Table 6).
DISCUSSION
Our investigation of the hypertension cascade by population subgroup showed that hypertension awareness, treatment, and control increased during the study period, but improvements at each stage of the cascade primarily occurred from 1999–2004 to 2005–2010. There were few changes at any stage of the cascade after 2010 for any population subgroup. Meanwhile, hypertension prevalence remained stable over time across age groups. However, we observed persistent disparities in certain population subgroups. Namely, the prevalence of hypertension was higher among blacks than among whites, higher among younger men than among younger women, and higher among older women than among older men.
Although the proportion of hypertensive persons who are aware of their hypertension and are being treated has increased and there is less room for improvement, the lack of recent change highlights the need to implement strategies to detect and initiate treatment among those with hypertension. Consistent with previous studies, we found that awareness of hypertension is lower in younger populations than in middle-aged or older populations and is particularly low among younger men, which may due to lower health-care utilization (17). Additionally, among persons with self-reported hypertension, black and Hispanic adults are more likely than whites to be uninsured, to lack a regular physician or health-care provider, and to report being unable to visit a physician because of cost (18), which may account for the lower prevalence of awareness in these groups.
At the population level, there is a substantial drop-off in the hypertension cascade from treatment to control. In particular, lack of hypertension control among those treated is a major barrier to improving hypertension control among adults aged ≥65 years. Additionally, we observed nonsignificant decreases in control and control among those treated from 2005–2010 to 2011–2016 among blacks aged ≥65 years and women aged ≥65 years. Based on the distribution of blood pressure levels, there is a suggestion of potential deintensification of treatment among adults aged ≥65 years in the 2011–2016 period, which may reflect 2014 guideline recommendations (19) that adults aged 60 years or older without comorbidity be treated to a blood pressure level of <150/90 mm Hg rather than <140/90 mm Hg (see Web Table 7 for guideline-recommended hypertension treatment goals over time). Because NHANES data are cross-sectional, we could not determine whether any change in the proportion of people with blood pressure between 140/90 mm Hg and 150/90 mm Hg was the result of treatment deintensification among persons with previously lower blood pressure values or improved treatment among those with higher blood pressure values. Our findings warrant further investigation, as there has been limited research to date on changes in clinical practice before and after the issuance of the 2014 guideline (19) and the potential implications for disparities.
Sex differences in hypertension control at younger ages (more favorable for women than for men) and older ages (more favorable for men than for women) persisted during the study period. However, we found that sex differences in hypertension prevalence changed over time. The difference in hypertension prevalence narrowed during the study period among those aged 25–44 years (higher prevalence in men than in women) and among those aged ≥65 years (higher prevalence in women than in men). Among those aged 45–64 years, we found that hypertension prevalence increased in men but not in women. Additionally, we observed a greater increase in hypertension control and control among those treated for women aged 45–64 years than for men aged 45–64 years. To our knowledge, these changes by sex have not been reported previously. Additional studies are needed to understand sex differences in treatment patterns and facilitators and barriers to hypertension control by age and sex.
The only narrowing of black-white disparities we observed was whites’ catching up to blacks in terms of awareness and treatment of hypertension among those aged 45–64 years and ≥65 years. In addition, despite some progress from 2005–2010 to 2011–2016, younger Hispanics had persistently lower rates of hypertension treatment, control, and control among those treated. Among Hispanic adults, the hypertension control cascade may vary by Hispanic/Latino background (20). Increased understanding of the hypertension cascade by Hispanic/Latino origin, level of acculturation, preferred language, and other factors are needed to inform culturally appropriate interventions for improving blood pressure control.
Despite population-level changes during the study time frame, we did not find that factors such as obesity, diabetes, health insurance coverage, or duration of hypertension explained the stall in improving hypertension control. Additionally, education campaigns designed to warn people about the dangers of high blood pressure have not led to improvements in hypertension control in the population. With regard to health disparities, it is well-known that targeted efforts are required in order to achieve health equity (21). Targeted efforts in clinical care will be required in order to reduce observed differences in hypertension control by population subgroup (22). Special efforts will be needed to reach younger men and younger nonwhite individuals, who access health care less often than their respective counterparts, but most patients with uncontrolled hypertension have health insurance and access to the health-care system.
In 2017, the American College of Cardiology and the American Heart Association released an updated guideline for the prevention, detection, evaluation, and management of high blood pressure among adults (23). This guideline redefines hypertension at a lower level of blood pressure (≥130/80 mm Hg) and recommends treatment to a lower level of blood pressure (<130/80 mm Hg) for all population subgroups. If clinical and public health efforts achieve the lower threshold of <130/80 mm Hg, the guideline should also increase hypertension awareness, treatment, and control to the surveillance definition of <140/90 mm Hg. Although some professional societies have not endorsed the more stringent treatment goal (24, 25), it is important to highlight that even by the higher threshold of <140/90 mm Hg, many adults have uncontrolled hypertension. It is also important that the new guideline be broadly implemented across population subgroups in order to reduce rather than exacerbate disparities in hypertension control.
Our study had several limitations. First, because we combined data into 6-year periods to improve the stability of prevalence estimates by population subgroup, there may have been contextual changes that led to changes in hypertension management on a smaller time scale than was our focus. Our supplemental analyses using 2-year data cycles provided some information on changes which occurred within the broader 6-year periods used in the main analysis. Second, information on awareness and treatment of hypertension was based on self-reporting, and there may have been reporting biases. Third, we were not able to ascertain the prevalence of hypertension treatment with lifestyle modification, which may be recommended prior to pharmacotherapy. Fourth, we were not able to report data for other racial/ethnic groups because of limited sample sizes, nor were we able to report data by Hispanic/Latino origin. Our study also had a number of strengths, including the large study population, standardized blood pressure measurements, and nationally representative study design.
In conclusion, there has been no change in hypertension control overall since 2010. Since then, there have been few changes at any stage of the hypertension cascade overall or by population subgroup. Thus, barriers to achieving hypertension control and reducing disparities remain. In younger populations, particularly among men and Hispanics, there are gaps in awareness and treatment. For most subpopulations, however, the largest drop-off in the hypertension cascade is from treatment to control. Further, there are disparities in hypertension control among those treated by sex and race/ethnicity, including disparities for older women as compared with older men and for black and Hispanic adults of all ages as compared with their white counterparts. The persistence of disparities shows that hypertension remains a priority health equity issue. Targeted, culturally appropriate approaches to addressing barriers at specific stages of the hypertension cascade by population subgroup, as well as broader efforts to prioritize hypertension control in clinical practice, are needed in order to resume improvements in hypertension control and reduce disparities in cardiovascular health in the United States.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland (Kathryn Foti, Dan Wang, Lawrence J. Appel, Elizabeth Selvin); Welch Center for Prevention, Epidemiology, and Clinical Research, Johns Hopkins Medical Institutions, Baltimore, Maryland (Kathryn Foti, Dan Wang, Lawrence J. Appel, Elizabeth Selvin); and Division of General Internal Medicine, School of Medicine, Johns Hopkins University, Baltimore, Maryland (Lawrence J. Appel).
K.F. was supported by grant T32 HL007024 from the National Heart, Lung, and Blood Institute. E.S. was supported by grant K24 DK106414 from the National Institute of Diabetes and Digestive and Kidney Diseases.
An earlier version of this work was presented at the American Heart Association Epi|Lifestyle Scientific Sessions, New Orleans, Louisiana, March 20–23, 2018.
Conflict of interest: none declared.
Abbreviation
- NHANES
National Health and Nutrition Examination Survey.
REFERENCES
- 1. Benjamin EJ, Virani SS, Callaway CW, et al. . Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492. [DOI] [PubMed] [Google Scholar]
- 2. Van Dyke M, Greer S, Odom E, et al. . Heart disease death rates among blacks and whites aged ≥35 years—United States, 1968–2015. MMWR Surveill Summ. 2018;67(5):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wozniak G, Khan T, Gillespie C, et al. . Hypertension control cascade: a framework to improve hypertension awareness, treatment, and control. J Clin Hypertens (Greenwich). 2016;18(3):232–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303(20):2043–2050. [DOI] [PubMed] [Google Scholar]
- 5. Luepker RV, Steffen LM, Jacobs DR Jr, et al. . Trends in blood pressure and hypertension detection, treatment, and control 1980 to 2009: the Minnesota Heart Survey. Circulation. 2012;126(15):1852–1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fryar CD, Ostchega Y, Hales CM, et al. . Hypertension Prevalence and Control Among Adults: United States, 2015–2016 (NCHS Data Brief no. 289). Hyattsville, MD: National Center for Health Statistics; 2017. [PubMed] [Google Scholar]
- 7. Mills KT, Obst KM, Shen W, et al. . Comparative effectiveness of implementation strategies for blood pressure control in hypertensive patients: a systematic review and meta-analysis. Ann Intern Med. 2018;168(2):110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jaffe MG, Lee GA, Young JD, et al. . Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310(7):699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Egan BM, Laken MA. Is blood pressure control to less than 140/less than 90 mm Hg in 50% of all hypertensive patients as good as we can do in the USA: or is this as good as it gets? Curr Opin Cardiol. 2011;26(4):300–307. [DOI] [PubMed] [Google Scholar]
- 10. Valderrama AL, Gillespie C, Mercado C. Racial/ethnic disparities in the awareness, treatment, and control of hypertension—United States, 2003–2010. MMWR Morb Mortal Wkly Rep. 2013;62(18):351–355. [PMC free article] [PubMed] [Google Scholar]
- 11. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157(21):2413–2446. [DOI] [PubMed] [Google Scholar]
- 12. Chobanian AV, Bakris GL, Black HR, et al. . The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 Report. JAMA. 2003;289(19):2560–2572. [DOI] [PubMed] [Google Scholar]
- 13. James PA, Oparil S, Carter BL, et al. . 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. [DOI] [PubMed] [Google Scholar]
- 14. Wright JT Jr, Fine LJ, Lackland DT, et al. . Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160(7):499–503. [DOI] [PubMed] [Google Scholar]
- 15. National Center for Health Statistics National Health and Nutrition Examination Survey (NHANES) Physician Examination Procedures Manual Hyattsville, MD: National Center for Health Statistics; 2015. https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/manuals/2015_Physician_Examination_Procedures_Manual.pdf. Accessed July 25, 2019.
- 16. Crim MT, Yoon SS, Ortiz E, et al. . National surveillance definitions for hypertension prevalence and control among adults. Circ Cardiovasc Qual Outcomes. 2012;5(3):343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999–2014. Hypertension. 2017;70(4):736–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fang J, Yang Q, Ayala C, et al. . Disparities in access to care among US adults with self-reported hypertension. Am J Hypertens. 2014;27(11):1377–1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chang AR, Hartle JE, Appel L, et al. . Abstract P183: minimal impact of JAMA 2014 guidelines on blood pressure control in a large health system. Circulation. 2017;135(suppl 1):AP183 http://circ.ahajournals.org/content/135/Suppl_1/AP183. Accessed April 5, 2018. [Google Scholar]
- 20. Sorlie PD, Allison MA, Avilés-Santa ML, et al. . Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27(6):793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Purnell TS, Calhoun EA, Golden SH, et al. . Achieving health equity: closing the gaps in health care disparities, interventions, and research. Health Aff (Millwood). 2016;35(8):1410–1415. [DOI] [PubMed] [Google Scholar]
- 22. Institute of Medicine (US) Committee on Public Health Priorities to Reduce and Control Hypertension A Population-Based Policy and Systems Change Approach to Prevent and Control Hypertension. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 23. Whelton PK, Carey RM, Aronow WS, et al. . 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 24. American Academy of Family Physicians AAFP decides to not endorse AHA/ACC hypertension guideline. https://www.aafp.org/news/health-of-the-public/20171212notendorseaha-accgdlne.html. Accessed April 29, 2018.
- 25. Qaseem A, Wilt TJ, Rich R, et al. . Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166(6):430–437. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.