Bacillus Calmette–Guérin (BCG) vaccination has been reported to decrease susceptibility to respiratory tract infections, an effect proposed to be mediated by the general long-term boosting of innate immune mechanisms, also termed trained immunity. Here, we discuss the non-specific beneficial effects of BCG against viral infections and whether this vaccine may afford protection to COVID-19.
Subject terms: Innate immunity, Live attenuated vaccines, SARS-CoV-2
Could the BCG vaccine be used to bridge the gap until a specific COVID-19 vaccine is developed? Luke O’Neill and Mihai Netea discuss the science behind this approach.
COVID-19 is a new form of respiratory tract infection that can be complicated by severe pneumonia and acute respiratory distress syndrome (ARDS). It is caused by a newly identified viral pathogen named on 11 February 2020 as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Most individuals infected with SARS-CoV-2 remain asymptomatic or develop a mild-to-moderate disease that is mainly characterized by upper respiratory tract symptoms. However, a significant minority of patients progress to severe pneumonia with ARDS, respiratory insufficiency and even death, particularly older patients1. At the time of writing, SARS-CoV-2 has killed more than 264,000 people, with over 2 million infected, and has given rise to a global economic shutdown, which is predicted to lead to a depression more serious than the great depression of the 1930s. While aggressive containment measures have been initiated by many parts of the world, the number of cases is still rising, with Europe and the United States now being the hot spots of the pandemic, but with an increasing number of cases in developing countries, stoking fears of a severe global health crisis. It is expected that the infection will remain entrenched in the population in the years to come, with regular outbreaks when quarantine measures are relaxed, or during winter when spread might be more common. Only an effective vaccine can curb the spread of the virus but that is expected to take at least 12–18 months to develop. In the meantime, other measures for preventing the spread of the virus are urgently needed. The BCG vaccine may well be a bridge to a specific COVID-19 vaccine.
BCG reprogrammes innate immunity
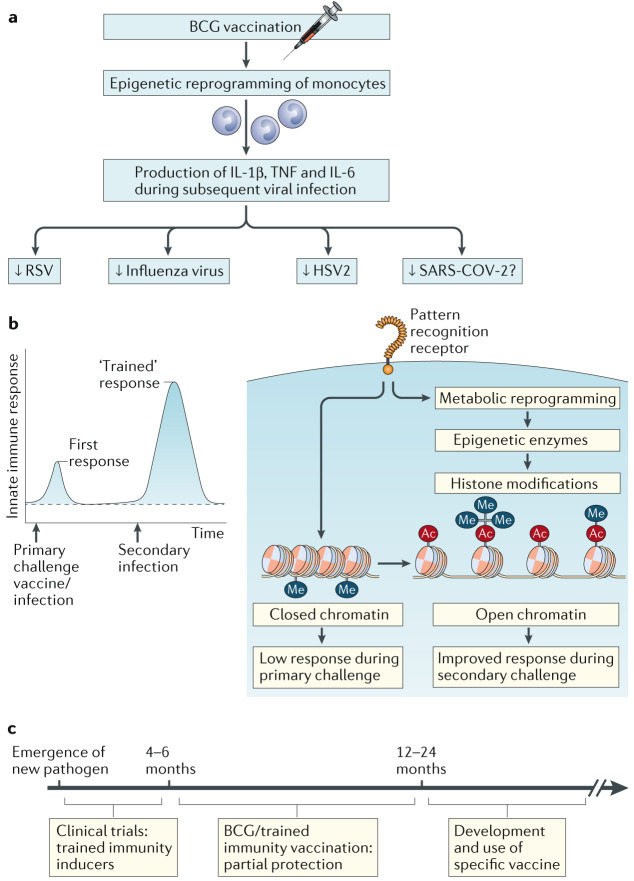
Bacillus Calmette–Guérin (BCG) is a live attenuated vaccine that was developed against tuberculosis at the beginning of the 20th century at the Institut Pasteur in Paris. Since then, it has been the most used vaccine in the world, with around 130 million children vaccinated every year. Interestingly, however, soon after its introduction in Europe in the 1920s, epidemiological studies reported that BCG vaccination strongly reduced infant mortality, and this could not be explained by a reduction in tuberculosis alone (reviewed previously2). Later on, similar studies in other locations, including randomized controlled trials, showed an up to 50% reduction of mortality induced by BCG in young infants3. This reduction in childhood mortality by BCG appeared to be due to the protection against unrelated infectious agents and especially respiratory tract infections and neonatal sepsis. Although the authors did not discriminate between bacterial and viral infections in these studies, it is well known that viral pathogens are the main cause of respiratory tract infections in children. This hypothesis was strengthened by a study in Guinea-Bissau showing that BCG reduced the incidence of respiratory syncytial virus infection4. A similar protective effect of BCG on respiratory tract infections was found in older individuals in Indonesia5, and a clinical trial performed in Japan demonstrated protection against pneumonia in tuberculin-negative older individuals6. Last, a recent study in adolescents in South Africa also reported a 70% reduction of respiratory tract infections by BCG vaccination7. Figure 1a illustrates the range of viral infections that BCG vaccination has been shown to protect against.
Fig. 1. Trained immunity antiviral host defence.
a | Bacillus Calmette–Guérin (BCG) vaccination has been shown to protect against multiple viral pathogens, including respiratory syncytial virus (RSV), influenza A virus and herpes simplex virus type 2 (HSV2). Will it protect against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)? b | Trained immunity leading to enhanced innate immune responses to different pathogens after a vaccination is mediated by metabolic and epigenetic rewiring in innate immune cells, which leads to increased gene transcription and improved host defence. c | Trained immunity as a tool for enhancing population immunity during a pandemic ahead of the availability of a specific vaccine. TNF, tumour necrosis factor.
These clinical trials have been complemented by experimental studies trying to decipher the mechanisms through which BCG induces these protective effects. Spencer et al.8 showed that BCG reduced viral titres of influenza A virus in mice, an effect dependent on macrophages. BCG vaccination also protected from herpes simplex virus type 2 (HSV2) in a controlled infection model with newborn mice9, while subcutaneous administration of muramyl dipeptide (MDP), a component of the mycobacterial cell wall, protected against vaccinia virus and HSV2 infections in mice10. This effect was mediated by peritoneal macrophages10, suggesting strong effects of BCG on the innate immune component of host defence. In line with this, a recent murine study showed that intravenous BCG delivery led to increased cytokine production by both splenocytes and peritoneal macrophages upon ex vivo restimulation with various unrelated pathogens.
The cellular and molecular mechanisms responsible for these beneficial effects of BCG against viral infection have been studied in detail only in the last decade11. BCG vaccination of healthy human volunteers results in enhanced production of pro-inflammatory cytokines, such as IL-1β, tumour necrosis factor (TNF) and IL-6, when monocytes from these individuals are stimulated ex vivo with unrelated pathogens12. Interestingly, these effects are accompanied by transcriptional, epigenetic and metabolic reprogramming of the myeloid cells in the BCG-vaccinated individuals. The epigenetic changes are manifested as chemical modifications (methylation and acetylation) of the histone, resulting in enhanced chromatin accessibility, easier transcription of genes important for antimicrobial responses and improved cell function13. In addition, metabolic reprogramming leads to selective accumulation or depletion of certain metabolites that regulate this process, owing to their function as cofactors for several classes of enzymes that mediate the epigenetic changes (Fig. 1b).
The long-term changes seen in innate immune cell phenotypes after BCG vaccination amount to a de facto induction of innate immune memory, which has been termed trained immunity. It has been hypothesized that induction of trained immunity is at least partly the mechanism through which BCG vaccination induces its beneficial effects. The idea here is that BCG leads to epigenetically trained populations of monocytes and/or natural killer cells, which most likely reside in the bone marrow. Upon challenge with pathogen-associated molecular patterns (PAMPs; which could be from bacteria or viruses) these innate immune cells then show an enhanced response, promoting host defence. This might explain why a vaccine for tuberculosis leads to protection against multiple pathogens.
In a recent study in healthy human volunteers, it has been shown that BCG vaccination reduces viraemia in response to the yellow fever vaccine (which is a live attenuated vaccine). This response is associated with epigenetic changes in monocytes that correlate with improved antiviral responses14. Taken together, these findings suggest that the induction of trained immunity by BCG vaccination results in significant protection against multiple viral infections.
BCG vaccination: a tool against COVID-19?
On the basis of these data, it has been hypothesized that BCG vaccination might be a potent preventive measure against SARS-CoV-2 infection and/or may reduce COVID-19 disease severity. Ecological studies have suggested that countries and regions that mandate BCG vaccination for the population have a lower number of infections and a reduced mortality from COVID-19 (ref.15). While these data could indeed suggest a protective effect of BCG vaccination, such studies cannot provide definitive proof of causality, owing to several inherent biases. These include differences in, one, demographic and genetic structure of the populations in different locations; two, differences in the non-pharmaceutical interventions being adopted in different locations (such as quarantine or social distancing); three, differences in diagnosing and reporting COVID-19 cases; and, four, differences in the positions on the epidemic curve of each location. Notwithstanding these issues, the link to BCG and COVID-19 from these studies is intriguing. It is not known whether older people would maintain a pool of trained monocytes many years after BCG vaccination. A possible explanation is that children who have been vaccinated with BCG are less susceptible to infection with SARS-CoV-2 and so there is less spread of the virus to older populations, although this would need to be demonstrated.
Because of these important limitations, randomized controlled trials are needed to provide the highest quality proof for the hypothesis that BCG vaccination may protect against COVID-19. Given the immediate threat of the SARS-CoV-2 pandemic, trials should be designed and started as pragmatic studies with feasible primary end points that can be performed rapidly and that could provide results in a short period. It is reasonable to propose that these are first initiated in populations at high risk of infection or with a high risk of mortality, such as hospital staff working in close contact with patients with COVID-19 or older individuals. Indeed, trials assessing the efficacy of BCG vaccination in these categories of individuals are currently being performed in the Netherlands, Australia and Greece, while other trials are being planned in the United States, UK, Denmark, France, Uruguay, Tanzania, Uganda and South Africa. This is a remarkable turn of events and reflects the seriousness of COVID-19 for global health.
One important aspect relates to the boosting of the innate immune response by BCG. Might this be deleterious, considering the fact that an exaggerated cytokine response has been associated with complications in patients with COVID-19 (ref.16)? We would argue that in healthy individuals vaccinated with BCG, in which innate antimicrobial mechanisms would be boosted by trained immunity, this is most likely to lead to inhibited viral replication, decreased viral loads and subsequently less inflammation and symptoms. This hypothesis is supported by the decrease in viraemia seen following yellow fever vaccination of individuals who were previously vaccinated with BCG15. By contrast, an initial defective antiviral response in some individuals at high risk (for example, older individuals) can result in high viral loads, stimulation of an inefficient systemic inflammation and severe disease. Breaking the loop of systemic inflammation could have beneficial effects in these patients.
We thus propose that induction of trained immunity by BCG could provide protection against COVID-19, but this hypothesis needs to be tested in rigorous randomized clinical trials. The use of approaches to induce trained immunity for protection against COVID-19 may not be restricted to BCG: indeed, there is speculation that oral polio vaccine might protect against non-related viral infections, and the new recombinant BCG-based vaccine VPM1002 may have similar effects and is also being considered for clinical trials. One could finally envisage using trained immunity as an important tool against emerging pathogens. BCG (or other stimuli that induce trained immunity) could be rapidly tested and eventually used at the beginning of a pandemic, bridging the 1–2 year period until a specific vaccine can be developed (Fig.1c). Indeed, although it is likely we will have a vaccine for SARS-CoV-2 within this time frame, it is not guaranteed. This prospect therefore carries particular force currently, where there is a desperately urgent need to develop strategies to restrain SARS-CoV-2 and limit the pandemic, which has put one-third of the Earth’s population under quarantine.
Acknowledgements
L.A.J.O.N. was supported by a European Research Council (ERC) advanced grant (no. 834370) and a Wellcome Trust Investigator Award. M.G.N. was supported by an ERC advanced grant (no. 833247) and a Spinoza grant of the Netherlands Association for Scientific Research.
Author contributions
The authors contributed equally to all aspects of the article.
Competing interests
The authors declare no competing interests.
References
- 1.Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shann F. The non-specific effects of vaccines. Arch. Dis. Child. 2010;95:662–667. doi: 10.1136/adc.2009.157537. [DOI] [PubMed] [Google Scholar]
- 3.Aaby P, et al. Randomized trial of BCG vaccination at birth to low-birth-weight children: beneficial nonspecific effects in the neonatal period? J. Infect. Dis. 2011;204:245–252. doi: 10.1093/infdis/jir240. [DOI] [PubMed] [Google Scholar]
- 4.Stensballe LG, et al. Acute lower respiratory tract infections and respiratory syncytial virus in infants in Guinea-Bissau: a beneficial effect of BCG vaccination for girls community based case-control study. Vaccine. 2005;23:1251–1257. doi: 10.1016/j.vaccine.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Wardhana, et al. The efficacy of Bacillus Calmette-Guerin vaccinations for the prevention of acute upper respiratory tract infection in the elderly. Acta Med. Indones. 2011;43:185–190. [PubMed] [Google Scholar]
- 6.Ohrui T, et al. Prevention of elderly pneumonia by pneumococcal, influenza and BCG vaccinations [Japanese] Nihon Ronen Igakkai Zasshi. 2005;42:34–36. doi: 10.3143/geriatrics.42.34. [DOI] [PubMed] [Google Scholar]
- 7.Nemes E, et al. Prevention of M. tuberculosis infection with H4:IC31 vaccine or BCG revaccination. N. Engl. J. Med. 2018;379:138–149. doi: 10.1056/NEJMoa1714021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spencer JC, Ganguly R, Waldman RH. Nonspecific protection of mice against influenza virus infection by local or systemic immunization with Bacille Calmette-Guerin. J. Infect. Dis. 1977;136:171–175. doi: 10.1093/infdis/136.2.171. [DOI] [PubMed] [Google Scholar]
- 9.Starr SE, et al. Effects of immunostimulants on resistance of newborn mice to herpes simplex type 2 infection. Proc. Soc. Exp. Biol. Med. 1976;152:57–60. doi: 10.3181/00379727-152-39327. [DOI] [PubMed] [Google Scholar]
- 10.Ikeda S, Negishi T, Nishimura C. Enhancement of non-specific resistance to viral infection by muramyldipeptide and its analogs. Antivir. Res. 1985;5:207–215. doi: 10.1016/0166-3542(85)90025-7. [DOI] [PubMed] [Google Scholar]
- 11.Moorlag S, et al. Non-specific effects of BCG vaccine on viral infections. Clin. Microbiol. Infect. 2019;25:1473–1478. doi: 10.1016/j.cmi.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Kleinnijenhuis J, et al. Bacille Calmette-Guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc. Natl Acad. Sci. USA. 2012;109:17537–17542. doi: 10.1073/pnas.1202870109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Netea MG, et al. Trained immunity: a program of innate immune memory in health and disease. Science. 2016;352:aaf1098. doi: 10.1126/science.aaf1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arts RJW, et al. BCG vaccination protects against experimental viral infection in humans through the induction of cytokines associated with trained immunity. Cell Host Microbe. 2018;23:89–100. doi: 10.1016/j.chom.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 15.Gursel M, Gursel I. Is global BCG vaccination-induced trained immunity relevant to the progression of SARS-CoV-2 pandemic? Allergy. 2020 doi: 10.1111/all.14345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehta P, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]