Background: The U.S. health care system is grappling with distinct challenges in delivering patient care during the coronavirus disease 2019 (COVID-19) pandemic (1, 2). First, both patients and clinicians are at risk for COVID-19 exposure during routine clinical visits. Second, the advanced care needs of patients admitted to intensive care units (ICUs) are limited by the availability of intensivists (3). Telehealth is a possible solution to delivering routine outpatient care without the risk for COVID-19 exposure (4) and to enabling access to critical care specialists to meet the staffing needs of ICUs (3). However, the availability of established infrastructure for these telemedicine services at hospitals across the country is poorly understood.
Objective: To determine the availability of telemedicine services at U.S. hospitals in 2018.
Methods and Findings: Using the 2018 American Hospital Association survey, we evaluated the proportion of hospitals that reported availability of 2 telemedicine services: telehealth consultation and office visits, which represent virtual care delivery in the outpatient setting, and tele-ICU, which denotes the use of audio-visual communication to allow virtual staffing of ICU patients by remote critical care specialists (5). Of the 6210 hospitals in the American Hospital Association, 4400 responded to the survey in 2018. All responding hospitals completed the telehealth questions. To supplement observations among nonresponding hospitals in 2018, availability of telehealth services was obtained from the 2017 survey (an additional 311 hospitals). The assessment of tele-ICU availability was restricted to hospitals with at least 1 ICU bed in 2018 (n = 2816). We evaluated differences in hospital characteristics on the basis of availability of telemedicine services using the χ2 test. The analysis was done with Stata, version 15 (StataCorp), using simple survey analyses.
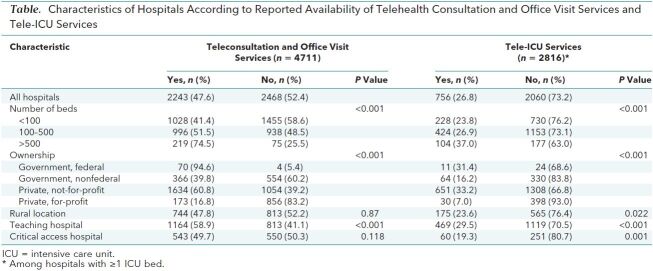
Of 4711 hospitals, 2243 (47.6%) reported providing telehealth-based consultation and office visit services. Hospitals with outpatient telemedicine services were more frequently large, private, not-for-profit, teaching hospitals than those without these services. The proportion of rural and critical access hospitals was not significantly different between these hospitals. Of the 2816 hospitals with ICUs, 756 (26.8%) reported tele-ICU capabilities. Tele-ICU hospitals were more frequently not-for-profit, private hospitals, and compared with hospitals without tele-ICU capabilities, a smaller proportion were rural or critical access hospitals (Table).
Table. Characteristics of Hospitals According to Reported Availability of Telehealth Consultation and Office Visit Services and Tele-ICU Services.
There was substantial regional variation in availability of telehealth-based consultation and office visit services across the United States, with 25 states or territories reporting these services in fewer than half of the hospitals (Figure, top). The proportion of hospitals with ICU beds that were equipped with tele-ICU facilities also varied widely, from no tele-ICU at hospitals in Puerto Rico to nearly 4 in 5 hospitals in Wisconsin (Figure, bottom).
Figure.
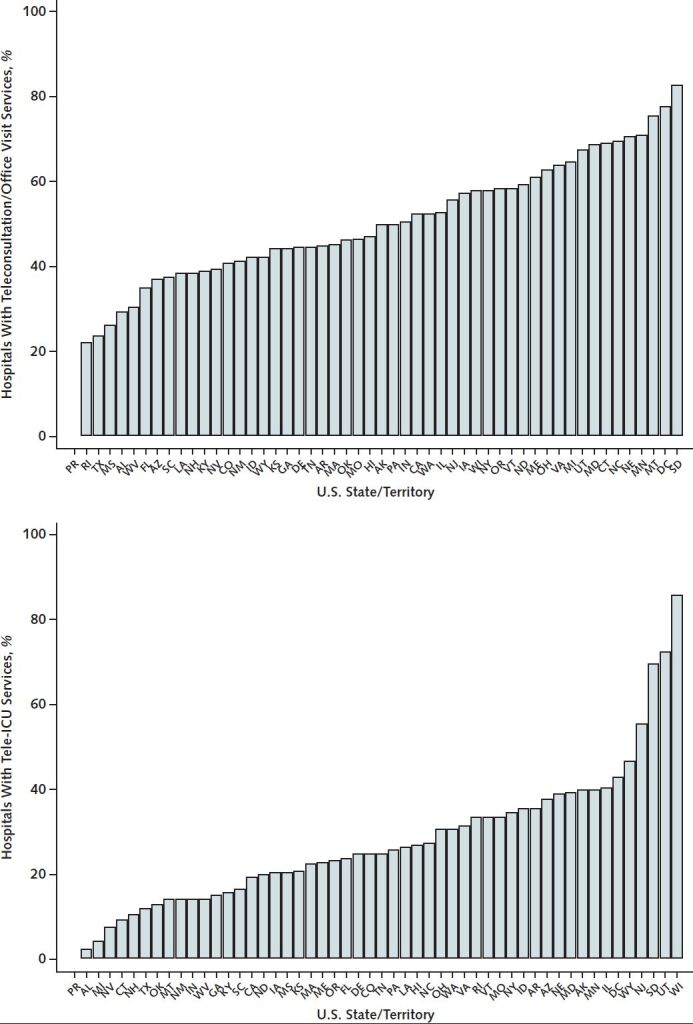
Distribution of telehealth services at hospitals across U.S. states and territories in 2018.
ICU = intensive care unit. Top. Proportion of hospitals in each state/territory that reported availability of services for telehealth consultation and office visits (presented as percentage of all hospitals that responded to the American Hospital Association survey in each state/territory). Bottom. Proportion of hospitals with ICU beds that reported availability of tele-ICU services (presented as percentage of all ICU-equipped hospitals in each state/territory that responded to the American Hospital Association survey).
Discussion: In 2018, half of U.S. hospitals reported provisions for telemedicine office visits, and 1 in 4 of those with ICUs were equipped with tele-ICU capabilities, with large variation in access to these services nationally. Given that COVID-19 requires reorganization of health care delivery, a large proportion of hospitals will need to develop infrastructure for both office visits and tele-ICU.
Our study has limitations. First, our report of telemedicine availability was limited to hospitals responding to the survey. On the basis of findings among responders, nonresponders in the American Hospital Association surveys are more frequently nonteaching, small, for-profit hospitals and would be less likely to have had telemedicine services. Second, our analysis focused on telemedicine consultation and office visits at hospital-based practices and does not include private clinics or standalone telemedicine businesses. Therefore, our study appraises availability of telehealth services at hospitals but not of the totality of the telehealth landscape. Third, we evaluated the presence of telemedicine services but were unable to quantify capacity across U.S. hospitals; some hospitals may have broad, well-developed programs, whereas others may not. Finally, our study cannot account for changes in telemedicine program development and expansion that have already taken place since the rapid spread of COVID-19 in the United States.
In conclusion, a large proportion of U.S. hospitals did not have existing telemedicine programs and will likely require rapid investment in developing the infrastructure needed to deliver patient care remotely and share limited health care resources across hospitals in light of the COVID-19 pandemic.
Biography
Financial Support: Dr. Khera is supported by the National Center for Advancing Translational Sciences (UL1TR001105) of the National Institutes of Health.
Disclosures: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M20-1201.
Reproducible Research Statement: Study protocol: Described in methods.. Statistical code: Available from Dr. Jain (e-mail, snigdha.89@gmail.com). Data set: Proprietary data set available from the American Hospital Association.
Corresponding Author: Harlan M. Krumholz, MD, SM, Center for Outcomes Research and Evaluation, Yale-New Haven Hospital, 1 Church Street, Suite 200, New Haven, CT 06510; e-mail, harlan.krumholz@yale.edu.
Footnotes
This article was published at Annals.org on 30 April 2020.
References
- 1. Centers for Disease Control and Prevention. Cases of coronavirus disease (COVID-19) in the U.S. Accessed at www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. on 17 March 2020.
- 2. doi: 10.1056/NEJMe2002387. Fauci AS, Lane HC, Redfield RR. Covid-19—navigating the uncharted [Editorial]. N Engl J Med. 2020;382:1268-1269. [PMID: 32109011] doi:10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed]
- 3. Halpern NA, Tan KS; SCCM Ventilator Taskforce. U.S. ICU resource availability for COVID-19. Accessed at https://sccm.org/getattachment/Blog/March-2020/United-States-Resource-Availability-for-COVID-19/United-States-Resource-Availability-for-COVID-19.pdf?lang=en-US. on 18 March 2020.
- 4. doi: 10.1056/NEJMp2003539. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020. [PMID: 32160451] doi:10.1056/NEJMp2003539. [DOI] [PubMed]
- 5. American Hospital Association. The promise of telehealth for hospitals, health systems and their communities. Accessed at www.aha.org/guidesreports/2015-01-20-promise-telehealth-hospitals-health-systems-and-their-communities. on 18 April 2020.