Introduction
Reports in literature of the presence of cutaneous findings in patients who have tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV2), which causes coronavirus disease 2019 (COVID-19), have ranged from 20.4%1 to 0.2% of cases.2 Reported cutaneous manifestations span from nonpruritic to pruritic erythematous morbilliform eruptions involving the trunk, to localized or widespread urticaria, to chickenpox-like vesicles.1 Petechial rash has also been described at the initial presentation of the COVID-19 disease,3 along with confluent erythematous-yellowish papules on heels bilaterally that presented 13 days after the onset of COVID-19 and which progressed to pruritic, hard, erythematous plaques.4 The timing of the reported cutaneous manifestations observed has also varied, with some patients presenting with cutaneous findings at the onset of the COVID-19 symptoms, whereas others develop cutaneous involvement after infection has progressed and they have been hospitalized.1 Herein, we present a novel cutaneous finding, a dusky red, nonpruritic, nonblanching, periorbital dyschromia that we have observed in several patients who have received a diagnosis of COVID-19. This rash appeared before the development of any of the systemic symptoms of COVID-19, and we believe that it can potentially serve as an early sign of patients' developing COVID-19.
Case report
Patient 1, an otherwise heathy 43-year-old woman, presented with dusky red, nonpruritic, nonblanching periorbital dyschromia (Fig 1). There was no conjunctivitis, other ocular symptoms, or any systemic findings of COVID-19 reported when the periorbital dyschromia appeared. Two days after the appearance of the rash, the patient reported that she had developed fever, cough, sore throat, muscle weakness, myalgias, and shortness of breath. She was prescribed alclometasone dipropionate 0.05% ointment. She was followed via telemedicine encounters and reported that she subsequently tested positive for the SARS-CoV2. She reported that she was using prescribed ointment twice a day and her rash completely resolved within a few days of using the ointment, along with improvement in her systemic symptoms. After this initial improvement in the systemic symptoms, and approximately 10 days after she developed initial periorbital dyschromia, she again developed the periorbital changes. As before, 2 days after developing periorbital dyschromia, she again became febrile, with worsening cough, myalgias, and shortness of breath, in what appeared to be the second phases of COVID-19 that have been reported in the literature. She requested another telemedicine consultation when the periorbital changes reappeared (Fig 2) and was told to use alclometasone dipropionate 0.05% ointment, which led to complete resolution of periorbital dyschromia (Fig 3). She completely recovered from COVID-19 and no further periorbital dyschromia was observed.
Fig 1.
At initial presentation of periorbital dyschromia. (The photograph was obtained via telemedicine visits with consent of the patient.)
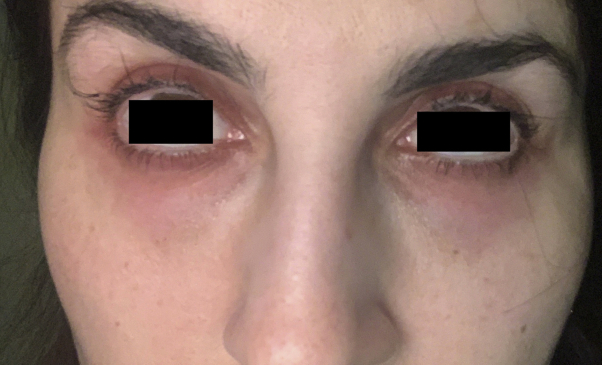
Fig 2.
At recurrence of periorbital dyschromia. (The photograph was obtained via telemedicine visits with consent of the patient.)
Fig 3.
At resolution of periorbital dyschromia. (The photograph was obtained via telemedicine visits with consent of the patient.)
Patient 2 was an otherwise healthy 50-year-old man who developed similar periorbital dyschromia, without any ocular changes, 2 days before onset of systemic symptoms including fever, shortness of breath, myalgias, and syncope. No images were obtained because he was hospitalized for his systemic symptoms of COVID-19 and tested positive for the SARS-CoV2 while he was in the hospital. No creams or ointments were applied for his periorbital dyschromia during his hospitalization, and he reported that the rash resolved on its own, with improvement in the systemic symptoms of COVID-19. As with patient 1, patient 2 reported that he again noticed periorbital dyschromia 2 days before worsening of the systemic symptoms, with recurrence of fever, worsening cough, and shortness of breath after reappearance of the periorbital dyschromia. Periorbital dyschromia once again resolved, with the resolution of systemic symptoms of COVID-19.
Discussion
COVID-19, a disease caused by SARS-CoV2, has afflicted millions of people worldwide during the past several months. Although there are multiple reports of systemic findings observed in patients with COVID-19, cutaneous manifestations of this disease have not been as widely described. Anecdotal and incidental cutaneous findings associated with COVID-19 have appeared in the literature, but no systematic review of the cutaneous manifestation of COVID-19 has been composed to date, to our knowledge. Some of the cutaneous manifestations of COVID-19 that have been described in the literature have ranged from erythematous eruptions involving the trunk, to widespread erythema and chickenpox-like vesicles,1 to rash with petechia,3 to confluent erythematous-yellowish papules on heels bilaterally that progressed to hard erythematous plaques.4
Furthermore, COVID-19 patients seem to be prone to coagulation dysfunction with signs of small blood vessel occlusion, as is evident by systemic, as well as cutaneous, findings of ischemia in the limbs. These cutaneous manifestations of microcirculation disorder that patients with COVID-19 may be developing can clinically present as findings ranging from petechiae or tiny bruises, to nonpruritic blanching livedoid vascular eruptions on extremities, to plantar plaques, plantar vesicles, dry gangrene, or just bruising in the fingers and toes.5 Perhaps the periocular dyschromia that we have noticed is a part of the coagulation dysfunction affecting the periocular vasculature. Although much more research is needed to evaluate the cutaneous manifestations that accompany COVID-19, herein we present our findings of periorbital dyschromia that presents a few days before the onset of systemic manifestations of COVID-19 and does not have any ocular findings, unlike in other reported studies.6 We believe that appearance of periorbital dyschromia may serve as an early cutaneous manifestation of COVID-19 and as a precursor of the systemic symptoms that seem to follow this presentation.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 2.Guan W., Ni Z., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joob B., Wiwanitkit V. COVID-19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol. 2020;82(5):e177. doi: 10.1016/j.jaad.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Estébanez A., Pérez-Santiago L., Silva E. Cutaneous manifestations in COVID-19: a new contribution. J Eur Acad Dermatol Venereol. 2020;34(6):e250–e251. doi: 10.1111/jdv.16474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y., Xiao M., Zhang S. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382(17):e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu P., Duan F., Luo C. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138(5):575–578. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]