Introduction
The novel coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has led to a pandemic affecting health care centers across the globe. With an estimated case fatality rate of 3.5%1,2 and a wide range of age groups affected, providers are rapidly adjusting their patterns of care to mitigate the negative impact of infection to cancer patients. In particular, oncologic patients have been reported to be at increased risk of infection and at a greater risk of severe events.1 As such, patients undergoing active cancer therapy are considered more vulnerable to significant morbidity from COVID-19.3,4
The current management for COVID-19 is maximum supportive care, and early diagnosis may help minimize adverse outcomes among patients.5 However, asymptomatic carriers may represent up to 42% of all infected patients,6 confirmed by the observation of high viral titers in the absence of symptoms.7,8 In addition, reverse transcription polymerase chain reaction (RT-PCR) laboratory testing has raised concerns regarding processing speed, sensitivity, and availability.9 Thus, novel detection strategies are necessary to supplement traditional screening methods and facilitate early diagnosis and mitigation of viral transmission.
Indeed, recent data support the diagnostic consistency and potential value of diagnostic computed tomography (CT) scans to aid early diagnosis of COVID-19. Sensitivity with CT has been reported to be as high as 97%9—significantly higher than that of RT-PCR alone, particularly during early phases of disease.10 A direct comparison of the 2 detection methods among 1014 Wuhan patients resulted in positive confirmations among 88% with CT imaging versus 59% with RT-PCR, and up to 93% of patients were deemed positive with CT before confirmation via RT-PCR testing.9 That being said, specificity of CT was 25% alone9; thus, imaging serves as more of a complement to rapid detection before RT-PCR confirmation.
Volumetric imaging with CT-on-rails (CTOR) or cone beam CT (CBCT) is commonly employed in patients undergoing radiation therapy as part of daily alignment. Previous reports have shown that imaging as part of a radiation therapy treatment course may identify nononcologic findings such as effusion, postobstructive atelectasis, or infection. Likewise, posttreatment imaging after radiation therapy often identifies well-characterized imaging changes such as radiation pneumonitis.11, 12, 13 Such imaging findings may often be confounded with infection and may be particularly problematic when assessing patients at risk for COVID-19.
This case series describes the presentation of SARS-CoV-2 infections among oncologic patients undergoing radiation therapy from a multi-institutional group of radiation oncology centers in the United States. In this article, we highlight the clinical symptoms, daily imaging findings, potential confounders, and clinical workflow to triage these patients to the next level of care.
Cases
Case 1
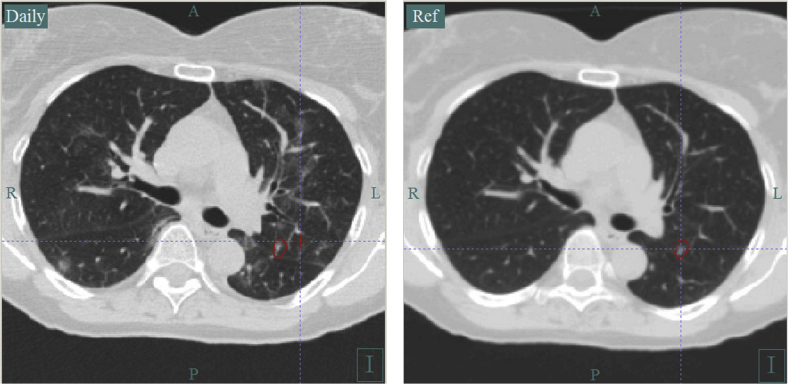
Case 1 was a 63-year-old woman, a former smoker without significant comorbidities, with recurrent adenocarcinoma who presented for definitive stereotactic ablative radiation therapy to 50 Gy in 4 fractions for a 7-mm tumor of the left upper lobe.14 CTOR, obtained for image guidance and patient set-up before treatment delivery, revealed new multifocal ground glass opacities (GGOs) of the bilateral lungs, compared with her CT-simulation scan obtained just 20 days beforehand for treatment planning (shown in Fig 1). The treatment was performed (before the first of 4 planned fractions), and she was referred to the emergency department with the CTOR images uploaded into the patient’s electronic health record for provider review. Although the patient was asymptomatic without fever or acute respiratory symptoms and her examination was unremarkable, she tested positive for SARS-CoV-2 via nasopharyngeal swab RT-PCR. Upon notification, the patient was instructed on home quarantine precautions, and treatment was subsequently deferred as per departmental policy. All staff members involved in her treatment were rapidly notified, screened, and cleared without quarantine. Of note, a repeat test 18 days later again returned as positive, despite the absence of symptom development. She has been tentatively rescheduled for another CT simulation for treatment replanning 14 days after this second positive test, assuming she remains asymptomatic during this interval.
Figure 1.
The reference image on the right represents the computed tomography (CT) simulation study obtained 20 days before the start of stereotactic body radiation therapy (SBRT) to a left upper lobe non-small cell lung cancer (NSCLC). The daily CT-on-rails (CTOR) imaging from the first fraction of treatment demonstrated new bilateral multifocal ground glass opacities concerning for coronavirus disease 2019 (COVID-19) infection.14
Case 2
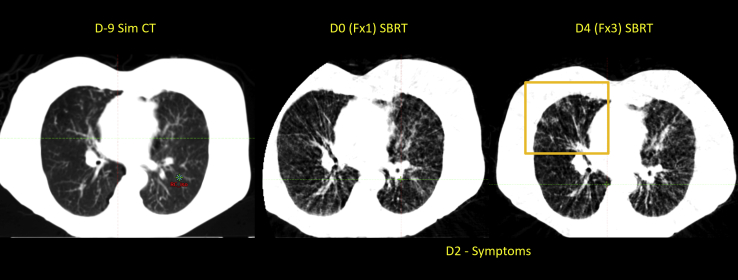
Case 2 was a 64-year-old woman who presented in early February with a diagnosis of cT1bN0M0 left upper lobe non-small cell lung cancer, diagnosed after surveillance lung CT demonstrated growth of a nodule. The patient’s past medical history was significant for chronic obstructive pulmonary disease (% of forced expiratory volume at 1 second [FEV1] predicted at 63%, and % of diffusion capacity for carbon monoxide [DLCO] predicted of 42%). She had a history of being a former smoker, with a 70-pack year history. Based on the nodule’s growth on surveillance lung CT and fluorodeoxyglucose-avidity on positron emission tomography and CT (30.3), a clinical diagnosis of non-small cell lung cancer was made. After the patient was deemed to be a high-risk operable candidate, she was recommended for stereotactic body radiation therapy (SBRT) as definitive management. She underwent CT simulation in mid-March for SBRT (55 Gy/5 daily consecutive fractions), and her first treatment was delivered 10 calendar days later. However, at the time of her on-treatment visit the patient reported increased severity of her baseline cough and shortness of breath, several episodes of posttussive emesis, and increased fatigue not relieved by rest. On review of her CBCT imaging, it was found that she had new GGOs in the right lower lobe (Fig 2). Based on these symptoms and findings, the institution’s COVID hotline was immediately notified on April 1, 2020. However, because the patient did not meet the criteria at that time for COVID-19 screening (fever, sick contacts, or travel), she was not recommended for testing. Given the continued clinical concern for both her symptoms and new findings on CBCT, direct communication was made with an infectious disease physician at the institution, who recommended she be treated as a presumed COVID-19-positive patient, and she was approved for testing. She was given a mask and instructed to start home quarantine. Three days later her test returned as negative for SARS-CoV-2 RNA. However, given the continued high index of suspicion for COVID-19, the patient remains in quarantine, with a plan to complete her final 2 fractions of SBRT once she has been asymptomatic for 3 days. The new imaging findings are still attributed to her potential COVID-19 diagnosis, in the absence of any confirmed alternative.
Figure 2.
The first image is an axial image from the computed tomography (CT) simulation study of case 2, obtained 9 days before start of stereotactic body radiation therapy (SBRT) to the left upper lobe lesion (not shown). The second image is the cone beam CT (CBCT) taken before the first fraction of treatment. On day 2, the patient began to experience increasing shortness of breath and cough. On the third fraction of treatment, peripheral ground glass opacities were seen in the right upper lobe, out of the treatment field, which were new compared with the first 2 images shown here.
Case 3
Case 3 was a 66-year-old woman with T1bN2M0, stage IIIA small cell lung cancer of the right upper lobe. The patient’s medical history includes emphysema, obstructive sleep apnea, and nonspecific pulmonary nodules that had been followed on chest CT, ultimately leading to the current diagnosis. The patient was a former smoker who quit over a decade ago but had a 74-pack-year smoking history. The patient was treated with curative intent twice-daily thoracic radiation therapy concurrent with carboplatin and etoposide. All institutional radiation dose-volume parameters were within tolerance, the mean lung radiation dose was 9.3 Gy, and the volume of lung receiving ≥20 Gy was 19.8%. Chemoradiation was well tolerated with acute toxicities including grade 1 cough and grade 1 esophagitis. Approximately 9 weeks after radiation therapy, the patient called reporting a 2-day history of a new nonproductive cough with increased dyspnea and increased use of albuterol. The patient denied fever, fatigue, or a decreased appetite. The patient asked if her current symptoms could be toxicities from her radiation treatment. At the time of her call, there was an intensification of the local COVID-19 epidemic. The patient was counseled on radiation pneumonitis (RP) and the potential need to start treatment with a high-dose corticosteroid taper. No repeat imaging was obtained at the time. However, out of caution she was recommended to undergo testing for COVID-19. The COVID-19 qualitative RNA test returned positive. The patient was not treated for RP, but rather, referred for COVID-19 management.
Discussion
Radiation oncology clinics around the world are currently working diligently to protect both patients and staff from the morbidity and mortality of COVID-19.15,16 However, this pandemic has presented at a time when many patients are either beginning or currently receiving cancer treatment. There continues to be a fine balance between triaging patient symptoms (which for thoracic patients may have some overlap with COVID-19 symptoms) and not introducing delays in oncologic care. In this series of teaching cases, we presented a range of presentations of COVID-19. Although the cases here represent patients who had both positive and negative COVID-19 testing, it should be noted that even patients with negative testing were still clinically managed as presumed positives with home quarantine and symptom surveillance.
Incidental imaging findings suspicious for COVID-19 on diagnostic chest CTs have been increasingly reported.17 Early features described to date include bilateral peripheral GGOs, which can be multifocal or multilobar in appearance.18, 19, 20 With increasing clinical severity, imaging demonstrates increased extent, density, and number of these GGOs.21,22 Resolution is accompanied by decrease and resorption of nodular opacities bilaterally.
The use of CT image guidance for patients receiving radiation therapy to the chest or thorax for lung, esophageal, and breast malignancies presents a unique opportunity to screen for COVID-specific lung changes. This was recently highlighted as a case study on the Radiation Oncology Incident Learning System (RO-ILS).23 Recommendations from RO-ILS included having radiation therapists, physicists, dosimetrists, and physicians become familiar with and screen for these characteristic COVID-19 findings daily and triage patients with findings for further evaluation. It was also recommended that clinical practices report these events to RO-ILS to help determine the prevalence of these findings.
Note that a prudent differential is still necessary, as patients being treated for thoracic malignancies may have significant baseline pulmonary comorbidities. Additionally, patients who have a history of systemic therapy, particularly immunotherapy, may also have pulmonary parenchymal changes over time.24 However, as shown in the cases presented here, the rapidity of infiltrate appearance on treatment should prompt immediate attention by the treating physician for symptom screening, vital signs, and appropriate triage to institutional COVID testing. Conversely, negative CBCTs should not be used to clinically “clear” patients who are having other COVID-associated symptoms, such as fever, new or worsening cough, new or worsening shortness of breath, or pleuritis. In a retrospective series of more than 120 COVID-19-positive patients across 4 medical centers in China, diagnostic CT images were compared by duration of time between symptom presentation and imaging.25 For patients receiving CT imaging 0 to 2 days from initiation of symptoms, 56% of these “early scans” were negative, whereas only 10% of intermediate scans at 3 to 5 days from symptoms and 4% of late scans at 6 to 12 days from symptoms were negative. Therefore, prescreening of patient symptoms via nursing staff before CT simulation study and daily screening questions before treatment still represent a crucial part of clinical practice.
Another clinical scenario presented here illustrates the need to have a high index of suspicion for COVID-19 for patients who are weeks to months out from the time of completion of thoracic radiation therapy. During this pandemic, patients with a history of thoracic radiation therapy who are suspected of having RP require attention. The characteristic symptoms of RP include progressive shortness of breath, cough, and fatigue, with or without a low-grade fever occurring weeks to several months after thoracic radiation. These symptoms overlap with those of COVID-19. Given the increasing prevalence of COVID-19, patients who present for RP evaluation should be tested for COVID-19, especially if they are to be started on empirical high-dose corticosteroids. Data indicate that corticosteroid therapy can worsen COVID-19-associated lung injury.26 Additionally, careful review of chest CT imaging, if available, is recommended given that the diffuse and multilobar radiographic features of COVID-1927 contrast with the classic CT appearance of RP that is mostly limited to the radiation field.
Patients actively undergoing radiation therapy should have treatment paused upon suspicion for COVID-19, pending screening test results. For those who test positive, robust data are lacking regarding the appropriate timeframe for radiation therapy resumption. The Centers for Disease Control has provided guidelines on nontesting strategy criteria for ending transmission-based precautions in the health care setting,28,29 which may be adopted for these scenarios pending stronger evidence. A test-based strategy is also outlined requiring 2 consecutive negative test results (collected at least 24 hours apart), although implementation may be limited owing to lack of test availability and capacity. Per nontesting strategy for symptomatic patients (case 2), Centers for Disease Control requirements entail the passage of (a) ≥7 days since first appearance of symptoms and (b) ≥3 days since recovery (defined as resolution of fever and improvement of respiratory symptoms). However, these guidelines are admittedly specific to isolation. Thus, more stringent criteria and timeframes may be warranted for patients with active cancer. As for asymptomatic patients (case 1), our institution requires ≥14 days to pass from first positive COVID-19 result (typically without need for retesting), although this 14-day timeline was cautiously reapplied toward the patient’s second positive test date (ordered through her local provider).
Although usual treatment volume has decreased at many radiation oncology centers during the COVID-19 pandemic, there are still many patients who have recently received treatment or are currently on treatment. Although measures such as screening questions and temperature measurements before department check-in certainly play a crucial role in appropriate patient triage, we are in a unique position to use an additional resource to monitor our high-risk patients with on-treatment daily CT imaging. Although this manuscript described 3 scenarios for patients with thoracic malignancies, we would recommend that both the initial simulation CT and on-board CTs acquired as part of daily image guidance of any patient where the imaging field of view encompasses the chest be reviewed for new or increasing infiltrates, particularly in patients with new symptoms. The entire image set should be reviewed, superiorly to inferiorly, to assess for potential changes. Owing to the observation that radiologic changes may precede physical symptoms, and considering a false negative rate ranging from 10% to 30%,9 this routine part of our daily cancer care gives us an additional tool to monitor our patients during this unprecedented time.
Footnotes
Sources of support: Supported in part by Cancer Center Support (Core) Grant CA016672 from the National Cancer Institute, National Institutes of Health, USA, to The University of Texas MD Anderson Cancer Center.
Disclosures: The authors report no conflicts of interest, financial or otherwise, to disclose with respect to this work.
Research data are not available at this time.
References
- 1.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 3.Kutikov A., Weinberg D.S., Edelman M.J. A war on two fronts: Cancer care in the time of COVID-19. Ann Intern Med. 2020;172:756–758. doi: 10.7326/M20-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burki T.K. Cancer care in the time of COVID-19. Lancet Oncol. 2020;21:628. doi: 10.1016/S1470-2045(20)30201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shankar A., Saini D., Roy S. Cancer care delivery challenges amidst coronavirus disease - 19 (COVID-19) outbreak: Specific precautions for cancer patients and cancer care providers to prevent spread. Asian Pac J Cancer Prev. 2020;21:569–573. doi: 10.31557/APJCP.2020.21.3.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nishiura H., Kobayashi T., Suzuki A. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020;94:154–155. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zou L., Ruan F., Huang M. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li D., Wang D., Dong J. False-negative results of real-time reverse-transcriptase polymerase chain reaction for severe acute respiratory syndrome coronavirus 2: Role of deep-learning-based CT diagnosis and insights from two cases. Korean J Radiol. 2020;21:505–508. doi: 10.3348/kjr.2020.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clarke E., Curtis J., Brada M. Incidence and evolution of imaging changes on cone-beam CT during and after radical radiotherapy for non-small cell lung cancer. Radiother Oncol. 2019;132:121–126. doi: 10.1016/j.radonc.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Elsayad K., Kriz J., Reinartz G. Cone-beam CT-guided radiotherapy in the management of lung cancer: Diagnostic and therapeutic value. Strahlenther Onkol. 2016;192:83–91. doi: 10.1007/s00066-015-0927-y. [DOI] [PubMed] [Google Scholar]
- 13.Kwint M., Conijn S., Schaake E. Intra thoracic anatomical changes in lung cancer patients during the course of radiotherapy. Radiother Oncol. 2014;113:392–397. doi: 10.1016/j.radonc.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 14.McGinnis G., Ning M., Nitsch P. Rapid detection of asymptomatic COVID-19 by CT image-guidance for stereotactic ablative radiotherapy. J Thorac Oncol. 2020;15:1085–1087. doi: 10.1016/j.jtho.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Samiee S., Hadjilooei F., Alamolhoda M. New policy and regulation for a radiology-oncology center at the time of COVID-19 outbreak in Tehran-Iran. Adv Radiat Oncol. 2020;5:550–557. doi: 10.1016/j.adro.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noticewala S., Koong A., Bloom E. Strategies to flatten the curve during the COVID-19 pandemic in radiation oncology: Experience from a large tertiary cancer center. Adv Radiat Oncol. 2020;5:567–572. doi: 10.1016/j.adro.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qu J., Yang R., Song L. Atypical lung feature on chest CT in a lung adenocarcinoma cancer patient infected with COVID-19. Ann Oncol Off J Eur Soc Med Oncol. 2020 doi: 10.1016/j.annonc.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pan F., Ye T., Sun P. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pan Y., Guan H., Zhou S. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): A study of 63 patients in Wuhan, China. Eur Radiol. 2020;30:3306–3309. doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shi H., Han X., Zheng C. Evolution of CT manifestations in a patient recovered from 2019 novel coronavirus (2019-nCoV) pneumonia in Wuhan, China. Radiology. 2020;295:20. doi: 10.1148/radiol.2020200269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung M., Bernheim A., Mei X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoon S.H., Lee K.H., Kim J.Y. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): Analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Society for Radiation Oncology website (ASTRO) https://www.astro.org/Patient-Care-and-Research/Patient-Safety/RO-ILS/Case-Study-05 Available at.
- 24.Kalisz K., Ramaiya N.H., Laukamp K.R. Immune checkpoint inhibitor therapy related pneumonitis: Patterns and management. Radiographics. 2019;39:1923–1937. doi: 10.1148/rg.2019190036. [DOI] [PubMed] [Google Scholar]
- 25.Bernheim A, Mei XY, Huang MQ, et al. Chest CT findings in coronavirus disease-19 (COVID-19): Relationship to duration of infection. Radiology.doi/pdf/10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed]
- 26.Russell C.D., Millar J.E., Baillie J.K. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395:473–475. doi: 10.1016/S0140-6736(20)30317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choi Y.W., Munden R.F., Erasmus J.J. Effects of radiation therapy on the lung: Radiologic appearances and differential diagnosis. Radiographics. 2004;24:985–997. doi: 10.1148/rg.244035160. discussion, 98. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention (CDC) Discontinuation of Isolation for Persons with COVID-19 Not in Healthcare Settings (Interim Guidance) https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html Available at.
- 29.Centers for Disease Control and Prevention (CDC) Discontinuation of Transmission-Based Precautions and Disposition of Patients with COVID-19 in Health care Settings (Interim Guidance) https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html Available at.