Abstract
COVID-19 pandemic is an emerging, rapidly evolving situation. Migraine is one of the commonest and highly disabling chronic neurological diseases in the world. During the pandemic and lockdown, migraine patients are facing an enormous problem in getting optimum care because of difficulty in access, forced social isolation, and encountering a health system that is getting rapidly overwhelmed. It is important that they must be protected by minimizing their visits to the clinics and emergency departments. Paradoxically multiple triggers are in operation which is likely to increase their headache frequency. Hence physicians should be made aware of the new rules of the game in treating migraines during this time of the pandemic so that these patients get optimum treatment and care and don’t feel left out. This review tries to answer a series of questions related to managing migraines in the times of COVID-19 pandemic.
Keywords: Coronavirus, COVID-19, migraine, treatment
INTRODUCTION
Since its isolation from the patients of unexplained pneumonia in Wuhan province of China, a new type of coronavirus belonging to the genus b and named COVID-19 has spread rapidly to almost all parts of the world in the last 4 and half months. On March 11, 2020, the World Health Organization has declared COVID-19 as a pandemic. The impact of the COVID-19 pandemic has been humongous. The world is staring at an uncertain future and finding it extremely difficult to win the war against this virus. Health care delivery systems have been overwhelmed in many countries because of the rapidity of the spread of infection and substantial mortality and morbidity associated with COVID-19 infection. At the time of writing, there are more than 18 lakh confirmed COVID-19 cases with more than 110,000 deaths globally.
India is also facing unprecedented challenges as the number of confirmed cases and deaths are rising steadily despite undertaking a complete nationwide lockdown since 24 March 2020. Whereas the major thrust of health care has been early detection, isolation, contact tracing and treatment of COVID-19 patients, considerable thought has also been given to provide adequate care to other chronic illnesses which can also adversely affect the nation’s health.
Migraine is a chronic neurological disorder which is the 6th commonest and 2nd most disabling medical condition in the world.[1] Worldwide, the 1-year period prevalence of migraine is 14.7%.[1] However, Indians have more migraines than the rest of the world. As per the epidemiological data from two parts of the country, namely Karnataka[2] and NCT of Delhi (unpublished data), a 1-year prevalence is more than 25%. Thus, at least one in four persons in India suffers from migraines. Even with a conservative estimate, at least 25% of these patients visit the physicians or hospitals periodically for the treatment of their migraine. Further, 2–4% of emergency department (ED) visits occur due to nontraumatic headaches[3,4,5] and out of that, about 35% of the visits occur due to migraines. It has been estimated that about 1.2 million migraine patients visit ED in Canada per year.[6]
Therefore, it is critical that this large number of patients must be protected by limiting their exposure to COVID-19. During these trying times physicians, neurologists and headache medicine specialists are trying to help individuals with a migraine so that they are not required to visit the emergency department or a clinic, thereby, avoiding the chance of exposure as social distancing is the key to fight COVID-19. Also, face-to-face visits and procedural treatment of migraines need to be decreased for the same reason. This reduction by creating effective strategies to treat migraine patients at home shall also help in decreasing the load on health care personnel, many of whom have already been recruited to fight the COVID-19 pandemic.
In this review, we shall try to answer some of the pertinent questions regarding how to manage migraine patients during this period of lock-down due to the COVID-19 pandemic. These are as follows:
Question 1: How can we minimize face-to-face visits by migraine patients to the clinic and hospital?
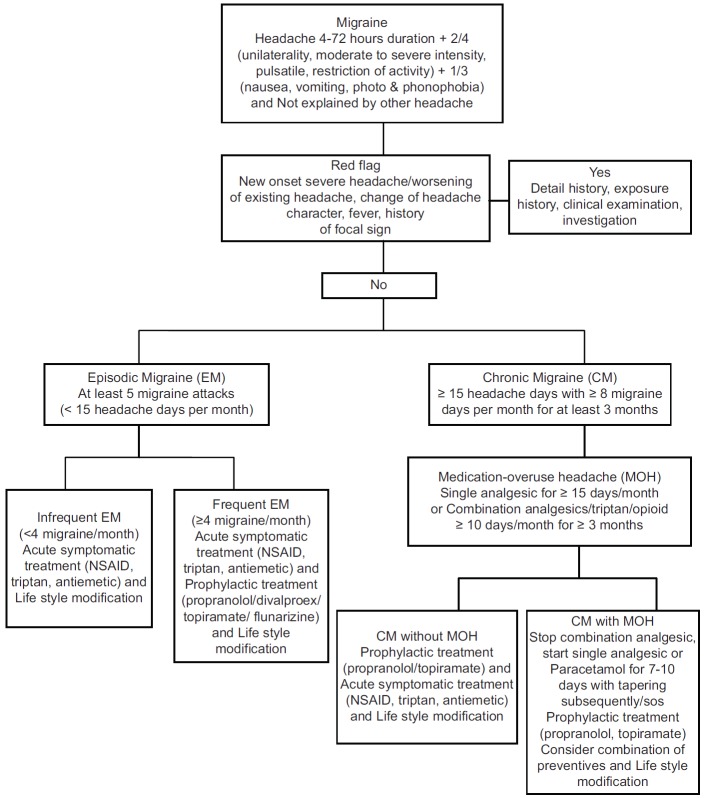
Telemedicine should be practiced to minimize direct face-to-face visits. There shall be three groups of patients suffering from migraines. First will be those with diagnosed migraines which are infrequent. They need reassurance and minimal intervention. The second group of migraine patients will be those with frequent migraines with headache frequency falling in episodic range (4–14 headache days/month) and those with chronic migraine (>15 headache days/month). Both these groups shall need regular periodic consultations and optimization of their therapy. Great effort must be made to facilitate therapies that they can avail at home effectively so than the chances of their visits to ED or the clinic are minimized. Then, there will be patients with newly diagnosed migraines who will not only need viable treatment options but a lot of educational support as well. Headache disorders are primarily diagnosed by clinical history and only in a small proportion of patients additional investigations are required to rule out the secondary cause. Therefore, telemedicine can play a big role in the diagnosis and management of headache disorders provided physicians are aware of the diagnostic criteria and current treatment guidelines of migraine [Figure 1]. Also, physicians should be aware of the red flags which may suggest a secondary cause that may necessitate a face-to-face evaluation. Studies have already shown that telemedicine consultations when compared to face-to-face consultations, lead to an equally high satisfaction rate for the patients[7] and non-inferior outcome,[8] even in pediatric headaches.[9] American Academy of Neurology telemedicine workgroup has also shown the utility of telemedicine in chronic neurological diseases.[10] India has got one of the largest numbers of smart-phone (502.2 million)[11] and internet users (451 million).[12] Most Indian families, therefore, can access and use telemedicine. With the current availability of various apps which can facilitate real-time interactive audio and video communication between patients and doctor who are placed remotely from each other, teleconsultations are possible. There have been concerns about the use of prescriptions, patient’s confidentiality and privacy, issues regarding physicians licensing, malpractices, and modalities of reimbursement. All these issues are complex. However, due to the current unprecedented situation where social and physical distancing for both patients and doctors are needed, telemedicine is possibly the easiest way to provide effective and satisfactory treatment to migraine patients. Hence, the professional bodies, organizations of doctors, and health authorities must facilitate such an approach and advocacy groups should advise the government for reframing laws, regulations, coding, and reimbursement options. Even in the foreseeable future when staggered ease of lock-down will be contemplated by the government, patients need not travel long distances to come to doctors’ clinics or hospitals; thereby, decreasing the chance of their exposure to COVID-19 infection. Physicians can also supply some common educational material or provide references for good and reliable internet sites where many of the frequently asked questions about migraine and its management are answered. However, since a large number of Indian population is illiterate or does not know English, resource material in vernacular languages or verbal communication including posting a simple video of dos and don’ts for migraine sufferers can be of much value.
Figure 1.
Diagnosis and treatment of migraine
Question 2: Which headache can be considered as a red flag during the COVID-19 pandemic?
Headache has been described as one of the symptoms of COVID-19 infection. Although uncommon it has been seen in approximately 8% of patients with COVID-19 infection.[13,14] Further, some gastrointestinal symptoms such as nausea, vomiting reported in COID-19 infection can mimic the symptoms of migraine. Therefore, any new-onset severe headache or worsening of existing headache in terms of frequency and severity or change in the character of existing headache under current circumstances must raise suspicion of COVID-19 infection. These patients must be asked about their exposure risk and should be assessed in detail for co-existing symptoms such as fever, dry cough, fatigue, sputum production, shortness of breath, muscle and joint pains, sore throat, chills, nausea and vomiting, nasal congestion, and diarrhea that have been associated with COVID-19 infection.
Question 3: Which acute treatments can be advised safely to migraine patients?
Migraine patients are likely to see a spike in their attacks during the lockdown and also new-onset migraine can develop in susceptible individuals during this time. The reason may be an abundance of migraine triggers. Recurrent migraine triggers play a significant role not only in precipitating migraine attacks in susceptible individuals but also in maintaining a continuous cycle of pain which may be difficult to disrupt. This is more so in the time of COVID-19 pandemic and lockdown which has resulted in anxiety, depression, social isolation, and changes in daily routine and activity. Following the lockdown in India, a lot of movement of migrant workers across the states has taken place. These individuals are also vulnerable to recurrent migraine attacks due to unusual physical exertion, hunger, and considerable mental stress (which all are potent migraine triggers). Due to the increased frequency of attacks in either group, these patients are prone to overuse acute medications and also many of them may visit ED simply because they become non-responsive to the usual acute medications. Hence, it is important that acute therapies for treating migraine attacks should be used judiciously in these patients. The patients should be advised to use acute medications in the early phase of headache with adequate doses so that they get an optimum response.[15] Inadequate treatment of acute attacks is an important cause of migraine chronification.[16]
Current guidelines suggest that the uses of nonsteroidal anti-inflammatory drugs (NSAIDs), triptans and narcoleptics are safe for the acute treatment of migraine attacks. There were some initial concerns about the uses of Ibuprofen in COVID-19 patients as WHO suggested that NSAIDs may exacerbate COVID-19 symptoms.[17] However, this recommendation was retracted later. As per the latest FDA guideline, it has been suggested that there is no scientific data that suggests the role of NSAID in worsening of COVID-19 symptoms, although the agency is further investigating in the matter.[18] However, because of changing dynamics of COVID-19 pandemics and convergence of new data from affected countries, recommendations may change and clinicians should be vigilant about updating themselves with changing recommendations. Triptans and antiemetics like metoclopramide, chlorpromazine, and prochlorperazine can also be considered for acute therapy. Sometimes, these can be advised in combination to ameliorate a severe acute attack.[19] Some of the newer acute treatment options that have been approved by the FDA in 2019 namely small molecule calcitonin gene-related peptide (CGRP) antagonists called Gepants (ubrogepant and rimegepants) and 5HT-1F agonist called “ditans” (lasmiditan) are not available in India yet but have been used in the US as acute therapy of migraine. New neuromodulation devices have been shown to be effective for both acute and preventive therapy of migraines and can be home delivered in the US and Europe. However, most of these devices are costly and are not available in India. Table 1 lists the acute treatment options.
Table 1.
Acute treatment for migraine
| Drug | Strength and dosage schedule | Max dose per day | May repeat dose | Side effects | |
|---|---|---|---|---|---|
| Acetaminophen | Paracetamol Paracetamol domperidone combination |
500-1000 mg 500 + 10 mg |
3000 mg 1500 + 30 mg |
4 hour | Nausea, stomach pain, jaundice |
| NSAIDs | Naproxen Ibuprofen Diclofenac Tolfenamic acid |
250-500 mg 400 mg 50-100 mg 200 mg |
1000 mg 2400 mg 200 mg 400 mg |
3-4 h 1-2 h |
Heartburn, stomach pain, tinnitus, dizziness, allergic reaction, high BP |
| Triptans | Sumatriptan Oral Intranasal Rizatriptan Oral Zolmitriptan Oral Intranasl Naratriptan Oral Almotriptan Oral Eletriptan Oral |
25 mg, 50 mg, 100 mg 5 mg, 20 mg 5 mg, 10 mg 2.5 mg, 5 mg 5 mg 1 mg, 2.5 mg 6.25 mg, 12.5 mg 20 mg, 40 mg |
200 mg 40 mg 30 mg 10 mg 10 mg 5 mg 25 mg 80 mg |
2 h 2 h 2 h 2 h 2 h 4 h 2 h 2 h |
Tingling, flushing, sense of fullness in head, neck, and chest, somnolence. Contraindicated in coronary insufficiency, untreated hypertension, ischemic stroke, peripheral vascular disease, pregnancy |
| Triptans + NSAIDs | Sumatriptan + Naproxen | 85 mg + 500 mg | |||
| Neuroleptics | Prochlorperazine Promethazine Metoclopramide Chlorpromazine |
5-10 mg 12.5-50 mg 5-10 mg 25 mg |
40 mg 100 mg 40 mg 75 mg |
6-8 h 6-8 h 6-8 h 6-8 h |
Dizziness, somnolence, extra-pyramidal symptoms, prolong QT interval |
Question 4: How to break a continuous cycle of recurrent pain in patients of migraine?
Sometimes the patients of migraines have continuous cycles of severe pain not relieved by first-line agents like NSAID, triptans, or neuroleptics. These patients often visit ED. To limit these emergency visits, a number of strategies have been suggested which however do not have an adequate evidence base. It has been suggested that NSAIDs, neuroleptics, longer-acting triptans, and anti-epileptics like valproate may be advised for a short period of 5–7 days to break the headache cycle.[19] It is advisable to add a proton pump inhibitor to decrease gastric irritation when the NSAIDs are given for a longer period of time. These have been tabulated in Table 2. Another useful drug in this situation that has been used clinically during non-COVID times, namely corticosteroids should be avoided. CDC recommends this because corticosteroids have been shown to prolong viral replication in MERS-COV patients.[20] An alternate route of drug administration for acute medications may also be tried such as intranasal lidocaine, ketorolac, and dihydroergotamine. Unfortunately, these are not easily available in India. However, side effects potentials of these drugs are high and hence only a patient who can understand the potential risk-benefit of these treatments can be considered for this. By and large, opioids and barbiturates should be avoided. Physicians should refrain as far as possible to use drugs like tramadol and ergotamine preparations (ergotamine with combinations like barbiturates and caffeine) as there is a great risk of producing medication overuse headache which shall be very difficult to treat in the home setting.
Table 2.
Rescue Treatment to break the pain cycle in migraine
| Drug | Strength and dosage schedule | Max dose per day | Side effects | |
|---|---|---|---|---|
| Acetaminophen | Paracetamol Paracetamol domperidone combination |
500 mg/650 mg TID × 7 days 500 mg + 10 mg TID × 3 days |
1500 mg/ 1950 mg 1500 + 30 mg |
Nausea, stomach pain, jaundice |
| NSAIDs | Ibuprofen Indomethacin Ketorolac Naproxen Naproxen domperidone combination Nabumetone Diclofenac Mefenamic acid |
400 mg TID × 3-5 days 50 mg TID × 7 days 10 mg TID × 3 days. 500 mg BID × 5-14 days 500 mg + 10 mg TID × 3 days 500 mg BID × 7 days 50 mg BID × 3-5 days 250 mg TID × 3-5 days |
1200 mg 150 mg 30 mg 1500 1500 + 30 mg 1000 100 750 |
Heartburn, stomach pain, tinnitus, dizziness, allergic reaction, high BP |
| Neuroleptics | Prochlorperazine Promethazine Metoclopramide Chlorpromazine |
5-10 mg TID × 3 days. 12.5-50 mg TID × 3 days. 5-10 mg TID × 3 days. 25 mg TID × 3 days. |
30 mg 150 mg 30 mg 75 mg |
Dizziness, somnolence, extrapyramidal symptoms, prolong QT interval |
| Long acting triptans | Frovatriptan Naratriptan |
2.5 mg BID × 3 days. 1 mg or 2.5 mg, BID × 3 days. |
5 mg 5 mg |
Generally safe but occasionally can cause. Tingling, flushing, sense of fullness in head, neck, and chest, somnolence. Contraindicated in coronary insufficiency, untreated hypertension, ischemic stroke, peripheral vascular disease, pregnancy |
| Antiepileptics | Valproic Acid | 500-1000 mg qhs × 5 days | 1000 mg | Contraindicated in woman of child bearing potential. Somnolence, hyperammonemia, tremor, liver dysfunction |
Question 5: What are the recommendations and concerns regarding preventive therapies in migraine during this COVID-19 pandemic?
Conventional preventive therapies with class I evidence like propranolol, metoprolol, Divalproex, topiramate, flunarizine, and amitriptyline can all be used safely [Table 3]. Angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARB) such as candesartan and lisinopril have been found to be useful as a migraine preventive.[21] There have been some concerns regarding their use because angiotensin receptor type 2 has been shown to be the entry point of the human cells for SERS-COV. However, at the moment there are no clinical or experimental data showing an adverse outcome of using ACEI, ARB, and renin-angiotension-aldosterone system (RAAS) antagonist in COVID-19 patients. Hence, in patients who are already on these medications because of cardiovascular disease or migraine and incidentally acquire COVID-19 infection, the clinician should judge the risk-benefit ratio for the continuation of these agents in these patients on a case to case basis.[22] However, ACEI and ARB may not be considered as the first choice in migraine patients who need to be started on a new preventive medication.
Table 3.
First-line preventive treatment for migraine
| Drug | Strength and dosage schedule | Max dose per day | Side effects | |
|---|---|---|---|---|
| Beta-blocker | Propranolol | 20-120 mg bid | 240 mg | Reduced energy, tiredness, postural symptoms Contraindicated in asthma |
| Metoprolol | 25-100 mg bid | 200 mg | ||
| Anticonvulsant | Valproate | 400-600 mg bid | 1200 mg | Drowsiness, weight gain, tremor, hair fall, fetal abnormality, contraindicated in women of child bearing potential |
| Topiramate | 12.5-100 mg bid | 200 mg | Paresthesia, weight loss, glaucoma, nephrolithiasis | |
| Antidepressants | Amitriptyline | 10-75 mg qd | 75 mg | Drowsiness, dry mouth |
| Nortriptyline | 10-75 mg qd | 75 mg | ||
| Venlafaxine | 75-150 mg qd | 150 mg | ||
| Calcium channel blocker | Flunarizine | 5-10 mg qd | 10 mg | Drowsiness, weight gain, depression, parkinsonism |
Many patients of migraines on single preventive therapy may not derive adequate benefit especially those with chronic migraines, and hence, the combination of preventive medications may be needed. Literature is scanty in this regard. However, a combination of propranolol and flunarizine is available in India. Propranolol or flunarizine can also be combined with amitriptyline in many of these patients. It is better to combine drugs with different mechanisms of action.[23] Further, drugs like melatonin and other nutriceuticals like magnesium, riboflavin and coenzyme Q can also be combined with first-line agents if they do not produce an adequate response.[24] Botulinum toxin and greater occipital nerve blocks are minimally invasive procedures and require close contact with the patients. They should be avoided in the current situation. Recently monoclonal antibodies (mAbs) against CGRP and CGRP receptors have been approved by the FDA as preventive therapy for episodic and chronic migraines. Three of these mAbs namely erenumab, galcanezumab, and fremanezumab can be self-injected by autoinjector at home subcutaneously every month.[25,26,27,28,29,30,31,32] However, these products are yet to be approved in India. Because of their high cost, these are generally recommended for those patients who have failed at least two first-line preventive drugs given at optimum dose and duration of time.[33] However, because of their salutary effects, there are reports of patients braving the odds of lockdown for getting these medications from the hospitals in Italy.[34]
Question 6: What are the concerns of health care workers (HCW) fighting the COVID-19 pandemic who have a migraine?
Doctors, nurses and other health care professionals have higher migraine risks than the general population.[35] During this COVID-19 pandemic, these individuals have been put to major stress, both in terms of workload and increased probability of acquiring the infection. Working for grueling shifts of 6–8 h wearing personal protective equipment (PPE), self quarantining themselves for the next 16–18 h and then again reporting for duty has been an extremely demanding task for them. In a recent study,[36] it was found that 81% of HCW developed de novo PPE associated headaches. More interestingly, a preexisting primary headache and PPE wearing for >4 h were independently associated with the development of PPE associated headaches. 90% with pre-existing primary headaches reported that with PPE usage their background headaches became uncontrolled resulting in poor performance. I have been telephonically contacted by six doctors and nurses in the last month who are on COVID-19 ICU duty that their migraines were getting out of hand. A simple 10-point advice prepared by us can help the HCW with migraine as how to manage their migraines during the COVID-19 pandemic [Table 4].
Table 4.
10-point advice for the health care workers with migraine who are fighting the COVID-19 pandemic
| 1. | Strictly follow the standard operating procedure (SOP) of COVID-19 care of your institution |
| 2. | If your migraines are controlled by preventive treatment, continue the same and don’t miss the dose. Have an adequate supply of your migraine drugs. |
| 3. | If the preventive medications are failing to work, ask your physician for any change in the dose or add-ons. Use telephone or web-based interactive platforms (telemedicine) to reach out to your physician |
| 4. | Avoid preventives with sedative action |
| 5. | Treat your acute attacks early |
| 6. | Don’t miss your meals |
| 7. | You shall not be allowed to eat or drink during your duty hours. Hence, adjust your meal timings and drink adequate fluids before reporting for duty |
| 8. | Get adequate sleep |
| 9. | After returning from duty, do some yoga and meditation in your quarantine room. Try to be calm. Think positively. Epidemics always have a curve of rise, plateau, and fall. |
| 10. | Try to be in touch with your family and friends during your off duty hours. Share your experiences and seek mental support from them if needed. |
Question 7: What are the general guidelines for the non-pharmacological treatment of migraines during COVID-19 pandemic?
First and foremost, the physicians should tell migraine patients that they are not more vulnerable to COVID-19 infection because of their migraines. Migraine patients prefer a regulated routine life because by the experience they know that it helps. Lifestyles and daily routines have however been modified to a large extent due to lockdown. However, migraine patients should be advised to try to stick to a routine as much as possible. For example, persons working from home should continue to do work as they were doing from the office and take the necessary breaks. They should eat at regular intervals. They should stop the work at the stipulated time and may change their clothes as they were doing after coming home. Maintaining regular sleep cycle, doing aerobic exercises, taking regular meals, maintaining good hydration by drinking adequate fluids, reducing stress by doing meditation, yoga, and avoiding known triggers can be very rewarding in preventing migraine attacks. A regular and good diet is also important to boost up immunity. Social isolation can be circumvented by interacting in social media, talking to friends and relatives. It is important to share how one is feeling. Suicides have been reported after the onset of the pandemic due to panic, isolation, fear, and psychological trauma and previous experience with the SARS epidemic has also shown a spike in suicide rates especially among the elderly.[37] Chronic migraine patients, especially those with aura have increased suicidal ideation and attempts and these are independently associated with migraine frequency.[38] Hence, during the COVID-19 pandemic where there is likely to be an increased frequency of migraine attacks due to multiple factors, these patients shall be at higher risk of suicides than the general population. Physicians should suggest helplines and other internet-based resources to migraine patients for their mental health problems. Finally, the general care for preventing the COVID-19 infection should be reemphasized by the physicians, namely social distancing, frequent handwashing with soap or sanitizer, minimal face touching, and general hygiene. Sanitizers and soaps with strong odors should be avoided as they can trigger a migraine attack.
CONCLUSION
Managing migraines during the times of COVID-19 can be challenging. Hospital and ED visits must be minimized. Telemedicine and internet-based consultations shall become the new norm. Physicians should be well versed in the diagnosis and management of migraine. The recommendations and guidelines may also see rapid changes and hence physicians should update themselves frequently. Social distancing shall result in more social interactions on virtual platforms. Physicians need to quickly adapt to this new world to deliver effective care to their migraine patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016 [published correction appears in Lancet 2017 Oct 28;390 (10106):e38] Lancet. 2017;390:1211–59. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kulkarni GB, Rao GN, Gururaj G, Stovner LJ, Steiner TJ. Headache disorders and public ill-health in India:Prevalence estimates in Karnataka State. J Headache Pain. 2015;16:67. doi: 10.1186/s10194-015-0549-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramirez-Lassepas M, Espinosa CE, Cicero JJ, Johnston KL, Cipolle RJ, Barber DL. Predictors of intracranial pathologic findings in patients who seek emergency care because of headache. Arch Neurol. 1997;54:1506–9. doi: 10.1001/archneur.1997.00550240058013. [DOI] [PubMed] [Google Scholar]
- 4.Goldstein JN, Camargo CA, Jr, Pelletier AJ, Edlow JA. Headache in United States emergency departments:Demographics, work-up and frequency of pathological diagnoses. Cephalalgia. 2006;26:684–90. doi: 10.1111/j.1468-2982.2006.01093.x. [DOI] [PubMed] [Google Scholar]
- 5.Torelli P, Campana V, Cervellin G, Manzoni GC. Management of primary headaches in adult Emergency Departments:A literature review, the Parma ED experience and a therapy flow chart proposal. Neurol Sci. 2010;31:545–53. doi: 10.1007/s10072-010-0337-y. [DOI] [PubMed] [Google Scholar]
- 6.Edmeads J, Findlay H, Tugwell P, Pryse-Phillips W, Nelson RF, Murray TJ. Impact of migraine and tension-type headache on life-style, consulting behaviour, and medication use:A Canadian population survey. Can J Neurol Sci. 1993;20:131–7. doi: 10.1017/s0317167100047697. [DOI] [PubMed] [Google Scholar]
- 7.Muller KI, Alstadhaug KB, Bekkelund SI. A randomized trial of telemedicine efficacy and safety for non acute headaches. Neurology. 2017;89:153–62. doi: 10.1212/WNL.0000000000004085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muller KI, Alstadhaug KB, Bekkelund SI. Telemedicine in the management of non-acute headaches:A prospective, open-labelled non-inferiority, randomized clinical trial. Cephalalgia. 2017;37:855–63. doi: 10.1177/0333102416654885. [DOI] [PubMed] [Google Scholar]
- 9.Qubty W, Patniyot I, Gelfand A. Telemedicine in a pediatric headache clinic:A prospective survey. Neurology. 2018;90:e1702–5. doi: 10.1212/WNL.0000000000005482. [DOI] [PubMed] [Google Scholar]
- 10.Hatcher-Martin JM, Adams JL, Anderson ER, Bove R, Burrus TM, Chehrenama M, et al. Telemedicine in neurology:Telemedicine Work Group of the American Academy of Neurology update. Neurology. 2020;94:30–8. doi: 10.1212/WNL.0000000000008708. [DOI] [PubMed] [Google Scholar]
- 11. [Last accessed on 2020 Apr 11]. Available from: https://www.news18.com/news/tech/smartphone-users-in-india-crossed-500-million-in-2019--states-report-2479529.html30th January 2020 .
- 12. [Last accessed on 2020 Apr 11]. Available from: https://www.statista.com/topics/2157/internet-usage-inindia/31st March 2020 .
- 13.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China:A descriptive study. Lancet. 2020;395:507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19:A systematic review and meta-analysis. Travel Med Infect Dis. 2020:101623. doi: 10.1016/j.tmaid.2020.101623. doi:10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silberstein SD, Marmura MJ. Acute migraine treatment. Headache. 2015;55:1–2. doi: 10.1111/head.12504. [DOI] [PubMed] [Google Scholar]
- 16.May A, Schulte LH. Chronic migraine:Risk factors, mechanisms and treatment. Nat Rev Neurol. 2016;12:455–64. doi: 10.1038/nrneurol.2016.93. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Could Ibuprofen Worsen Disease for People With COVID-19? Geneva: World Health Organization; 2020. [Google Scholar]
- 18.Food and Drug Administration. FDA Advises Patients on Use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) for COVID-19 [online] [Last accessed on 2020 Apr 11]. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-advises-patients-use-non-steroidal-anti-inflammatory-drugs -nsaids-covid -19. 19/3/2020 .
- 19.Szperka CL, Ailani J, Barmherzig R, Klein BC, Minen MT, Halker Singh RB, et al. Migraine care in the era of COVID-19:Clinical pearls and plea to insurers. Headache. 2020 doi: 10.1111/head.13810. doi:10.1111/head.13810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. [Last accessed on 2020 Apr 11]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html#Medications .
- 21.Dorosch T, Ganzer CA, Lin M, Seifan A. Efficacy of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in the preventative treatment of episodic migraine in adults. Curr Pain Headache Rep. 2019;23:85. doi: 10.1007/s11916-019-0823-8. [DOI] [PubMed] [Google Scholar]
- 22.Bozkurt B, Kovacs R, Harrington BB. HFSA/ACC/AHA Statement Addresses Concerns Re:Using RAAS Antagonists in COVID-19 [online] [Last accessed on 20 Mar 24]. Available from: https://www.acc.org/lates t-in-cardi ology/artic les/2020/03/17/08/59/hfsa-acc-aha-statement-addresses concerns-re-using -raas-antagonists-in-covid-19 . [DOI] [PMC free article] [PubMed]
- 23.D'Antona L, Matharu M. Identifying and managing refractory migraine:Barriers and opportunities? J Headache Pain. 2019;20:89. doi: 10.1186/s10194-019-1040-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.D'Onofrio F, Raimo S, Spitaleri D, Casucci G, Bussone G. Usefulness of nutraceuticals in migraine prophylaxis. Neurol Sci. 2017;38:117–20. doi: 10.1007/s10072-017-2901-1. [DOI] [PubMed] [Google Scholar]
- 25.Dodick DW, Ashina M, Brandes JL, Kudrow D, Lanteri-Minet M, Osipova V, et al. ARISE:A phase 3 randomized trial of erenumab for episodic migraine. Cephalalgia. 2018;38:1026–37. doi: 10.1177/0333102418759786. [DOI] [PubMed] [Google Scholar]
- 26.Tepper S, Ashina M, Reuter U, Brandes JL, Doležil D, Silberstein S, et al. Safety and efficacy of erenumab for preventive treatment of chronic migraine:A randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol. 2017;16:425–34. doi: 10.1016/S1474-4422(17)30083-2. [DOI] [PubMed] [Google Scholar]
- 27.Goadsby PJ, Reuter U, Hallstrom Y, Broessner G, Bonner JH, Zhang F, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med. 2017;377:2123–32. doi: 10.1056/NEJMoa1705848. [DOI] [PubMed] [Google Scholar]
- 28.Stauffer VL, Dodick DW, Zhang Q, Carter JN, Ailani J, Conley RR. Evaluation of galcanezumab for the prevention of episodic migraine:The EVOLVE-1 randomized clinical trial. JAMA Neurol. 2018;75:1080–8. doi: 10.1001/jamaneurol.2018.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Detke HC, Goadsby PJ, Wang S, Friedman DI, Selzler KJ, Aurora SK. Galcanezumab in chronic migraine:The randomized, double-blind, placebo-controlled REGAIN study. Neurology. 2018;91:e2211–21. doi: 10.1212/WNL.0000000000006640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Skljarevski V, Matharu M, Millen BA, Ossipov MH, Kim BK, Yang JY. Efficacy and safety of galcanezumab for the prevention of episodic migraine:Results of the EVOLVE-2 Phase 3 randomized controlled clinical trial. Cephalalgia. 2018;38:1442–54. doi: 10.1177/0333102418779543. [DOI] [PubMed] [Google Scholar]
- 31.Silberstein SD, Dodick DW, Bigal ME, Yeung PP, Goadsby PJ, Blankenbiller T, et al. Fremanezumab for the preventive treatment of chronic migraine. N Engl J Med. 2017;377:2113–22. doi: 10.1056/NEJMoa1709038. [DOI] [PubMed] [Google Scholar]
- 32.Dodick DW, Silberstein SD, Bigal ME, Yeung PP, Goadsby PJ, Blankenbiller T, et al. Effect of fremanezumab compared with placebo for prevention of episodic migraine:A randomized clinical trial. JAMA. 2018;319:1999–2008. doi: 10.1001/jama.2018.4853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sacco S, Bendtsen L, Ashina M, Reuter U, Terwindt G, Mitsikostas DD, et al. European headache federation guideline on the use of monoclonal antibodies acting on the calcitonin gene related peptide or its receptor for migraine prevention [published correction appears in J Headache Pain, 2019 May 23;20 (1):58] J Headache Pain. 2019;20:6. doi: 10.1186/s10194-018-0955-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silvestro M, Tessitore A, Tedeschi G, Russo A. Migraine in the time of COVID-19 [published online ahead of print, 2020 Apr 8] Headache. 2020 doi: 10.1111/head.13803. doi:10.1111/head.13803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuo WY, Huang CC, Weng SF, Lin HJ, Su SB, Wang JJ, et al. Higher migraine risk in healthcare professionals than in general population:A nationwide population-based cohort study in Taiwan. J Headache Pain. 2015;16:102. doi: 10.1186/s10194-015-0585-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jy Ong J, Bharatendu C, Goh Y, Goh Y, Zy Tang J, Wx Sooi K, et al. Headaches associated with personal protective equipment-A cross-sectional study amongst frontline healthcare workers during COVID-19 (HAPPE Study) [published online ahead of print, 2020 Mar 30] Headache. 2020 doi: 10.1111/head.13811. doi:10.1111/head.13811. [DOI] [PubMed] [Google Scholar]
- 37. [Last accessed on 2020 Apr 11]. Available from: https://blogs.scientificamerican.com/observations/covid-19-is-likely-to-lead-to-an-increase-in-suicides/
- 38.Lin YK, Liang CS, Lee JT, Lee MS, Chu HT, Tsai CL, et al. Association of suicide risk with headache frequency among migraine patients with and without aura. Front Neurol. 2019;10:228. doi: 10.3389/fneur.2019.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]