Abstract
Background:
Most longitudinal or treatment studies in bipolar disorder have used symptomatic or syndromal status as the primary outcome variable. More recently, psychosocial functioning has been highlighted as a key domain of outcome. Patients with bipolar disorder appear to be impaired in all functional domains, although the factors that cause impairment have not been clearly specified.
Methods:
This paper reviews cross-sectional and longitudinal studies on functional impairment and its relationship to symptomatic, neurocognitive, personality, and stress variables in bipolar disorder; and the implications of these relationships for defining treatment targets. 93 articles were located through comprehensive MEDLINE, SCOPUS and Web of Science searches.
Results and discussion:
Functional recovery following a mood episode consistently lags behind symptomatic and syndromal recovery. Longer term functional impairment is only partly explained by the number of manic/hypomanic episodes. Depression (including subsyndromal states) and persistent neurocognitive impairment are the strongest correlates of functional impairment in bipolar disorder, with personality and psychosocial stressors playing secondary roles. Possible treatment options include: more aggressive treatment of subthreshold depressive states, pharmacotherapies that target cognition (e.g., stimulants), and adjunctive psychotherapies including cognitive remediation.
Keywords: Neurocognition, Cognitive remediation, Depression, Mania, Mood stabilizers, Stimulants
1. Introduction
The natural history of bipolar disorder is characterized by frequent and recurrent mood episodes. Since Kraepelin’s seminal studies distinguishing manic depressive insanity (bipolar disorder) from dementia praecox (schizophrenia) (Kraepelin, 1921), it has been clear that the natural history of bipolar disorder is characterized by recurrent episodes. Despite the evolution of multiple effective mood stabilizers that prevent manias, depressions or both (Gitlin and Frye, 2012), naturalistic studies repeatedly demonstrate breakthrough episodes of mania or depression with relapse rates over 1–4 years in treated groups ranging from 40% to 60%, and 4–5 year relapse rates range from 60% to 85% (Goodwin and Jamison, 2007; Gignac et al., 2015).
Additionally, modern studies have documented moderate to severe functional impairment associated with bipolar disorder in any and all domains evaluated (Coryell et al., 1993; MacQueen et al., 2001; Keck, 2006; Judd et al., 2008; Sanchez-Moreno et al., 2009; Wingo et al., 2009). Bipolar I and II patients still have significant functional impairment after statistically controlling for the concurrent level of depression (Sanchez-Moreno et al., 2009; Coryell et al., 1989; Judd et al., 2005; Ruggero et al., 2007). Highlighting the importance of functional vs. syndromal outcomes, it has been estimated that 79% of the societal cost of bipolar disorder is due to indirect costs such as occupational impairment as opposed to direct treatment costs such as hospitalization (Dilsaver, 2011). In fact, BD is the fifth leading cause among psychiatric disorders of lost years of work (Ferrari et al., 2016).
The two methods of measuring outcome- symptomatic/syndromal vs. functional - highlight a number of questions that will be addressed in this review:
What is measured by these different outcome variables?
What are the relationships between syndromal or subsyndromal symptoms and different types of functional outcome in bipolar disorder?
What are the non-symptomatic (e.g., neurocognitive) correlates of functional outcome?
Finally, what are the implications of these findings for the pharmacological or psychosocial management of bipolar disorder?
2. Methods
2.1. Studies were identified through MEDLINE, SCOPUS, and Web of Science
The search terms included blocks pertaining to bipolar disorder (bipolar, mania, depression, hypomania, manic-depression) and functioning (impairment, psychosocial, occupational, disability, work, cognition, neurocognition, stress, remediation). The searches were limited to the period between Jan. 1, 1980 and Sept. 1, 2016. We also screened articles cited in existing reviews of the literature on functional outcomes, stress, and psychosocial interventions (Andreou and Bozikas, 2013; Cardenas et al., 2016; Cullen et al., 2016; Levy and Manove, 2012; Miklowitz and Johnson, 2009a; Salcedo et al., 2016).
This article addresses some of the same topics covered in earlier reviews (e.g., Andreou and Bozikas, 2013; Levy and Manove, 2012). However, we also address several issues that had not been fully investigated previously: the effects of subsyndromal symptoms on functional impairment, either in conjunction with or independent of neurocognitive factors; the influence of personality traits on social-occupational functioning; new pharmacological strategies (e.g., non-dopaminergic stimulants); and new psychosocial methods (e.g., functional remediation) for treating functional disability associated with bipolar disorder or its comorbid disorders.
We screened 2418 peer-reviewed articles for eligibility. Eligibility was based on direct relevance of the article to (1) the prevalence or extent of functional impairment in bipolar disorder (accounting for 278 citations), (2) the roles of symptoms and neurocognition (611 citations); (3) the roles of comorbid disorders or personality variables in functional impairment (663 citations); and (4) treatment studies or clinical position papers (866 citations). After excluding duplicate citations or papers that did not address these questions, we selected 93 articles for inclusion.
2.2. Measuring outcome in bipolar disorder
Psychopharmacological studies typically measure outcome by counting the number of and severity of symptoms, or (for maintenance trials), computing time to relapse or recurrence. A variation on the theme of symptom-based measurement is constructing cumulative measures of symptoms, similar to the area under the curve in which the relevant unit of measurement is symptom severity over time. Cumulative measures of depression equate, for example, six months of mild depression with three months of more severe depression. Cumulative measures of psychopathology taking into account symptom severity and time provide a somewhat richer and more accurate picture of a patient’s course compared to simply measuring relapse rates or survival curves, and may be more strongly correlated with functional outcome measures than are symptom measures from a single time point (Gitlin et al., 1995).
2.3. Functional outcome and its measurement
Focusing solely on the evolution of symptoms as the only outcome may falsely estimate the “success” of a treatment. As an example, treating a patient to symptomatic recovery (i.e., prolonged euthymia) but not functional recovery (i.e., working at full capacity, having strong interpersonal supports and reporting a high quality of life) would be considered a successful treatment in a study focusing only on symptomatic outcomes.
These limitations in symptom-based outcome definitions have given rise to efforts in measuring functional outcomes – the degree of success of patients’ lives. A variety of reliable measures of functioning in bipolar disorder exist (e.g. Rosa et al., 2007) but none has achieved the type of acceptance comparable to that of the Hamilton Depression Rating Scale (Hamilton, 1960) or the Young Mania Rating Scale (Young et al., 1978). Although some studies use the single dimensional Global Assessment of Functioning Scale (Endicott et al., 1976), most functioning scales assess at least two domains- role function and social function- with some assessing recreation or life satisfaction. Role function includes the relative ability to handle work, school or household roles, allowing patients in different social contexts to be compared in a crude way. Social functioning may include romantic relationships, interactions with family members or friendships.
Since the available scales may differ substantially in what is measured, and few studies include more than one functioning measure, the results across studies may differ based on measurement variance as opposed to outcomes. Some studies use self-report measures of functioning whereas others use observer-based measures. Thus, in one study functioning may the reflect patients’ assessment of their progress relative to other phases of one’s life, whereas in another study functioning may mean relative to other patients.
A less frequently used outcome measure is ‘quality of life’ (QOL) which measures whether individuals feel satisfied or fulfilled. Compared to both symptom based or function based measurements, quality of life is more subjective since the former evaluate individuals according to an objective (if culturally determined) standard, whereas QOL is entirely based on the individuals’ subjective appraisal. Given the inherent subjectivity in its definition, there is no consensus on the optimal rating scales to use in measuring QOL, although reliable measures have been proposed (e.g., Michalak et al., 2005). Additionally, mood states, especially depression, are likely to affect functioning and especially, QOL measures. Therefore, QOL measures need to be obtained during euthymic as well as symptomatic periods to avoid simply measuring the cognitive distortions associated with mood states.
Overall, bipolar patients score lower than control populations on QOL measures (Michalak et al., 2005). This is especially so in those who are evaluated while depressed. Perhaps counterintuitively, manic/hypomanic patients also rate their QOL as lower than controls; whether this group difference reflects the common admixture of depressive symptoms within manic states, or the recognition that one’s life is impaired despite current feelings of elation or heightened energy, is not clear (Michalak et al., 2005).
2.4. Relationships between functional and syndromal outcomes in bipolar disorder
It is generally assumed that a prime determinant of functional outcome is symptomatic outcome (see Fig. 1): patients who are more symptomatic, who have.
Fig. 1.
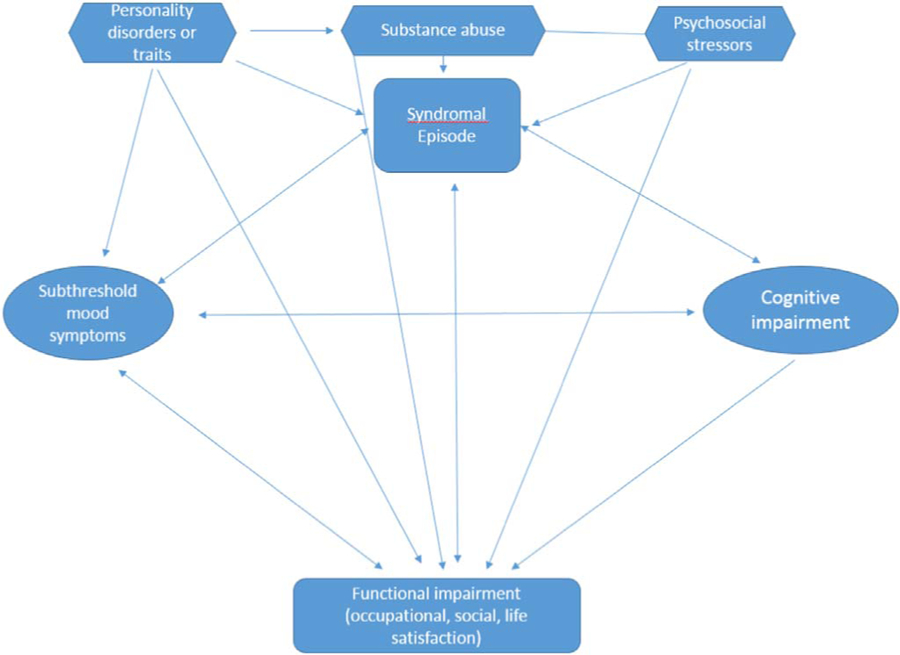
Predictors of functional impairment. This model hypothesizes the primacy of symptomatic (both syndromal and subsyndromal) variables and cognitive impairment as predictors of long-term functional impairment. These variables are mutually influential and are bidirectionally associated with functioning variables. These strength of these predictor/outcome relationships will be affected by other clinical variables that can be assessed after an acute episode, such as substance abuse or dependence, axis II disorders or traits, medication adherence, and psychosocial stressors (i.e., life events or family conflicts).
more episodes, worse episodes, and more hospitalizations will have poorer functional outcome compared to those with more benign symptomatic courses. In general, this assumption is correct. Yet, as has been repeatedly noted (MacQueen et al., 2001), a large percentage of bipolar patients who have become asymptomatic continue to be functionally impaired. In an early and dramatic example of this, six months after a hospitalization for mania, 84% of patients were syndromally recovered while only 30% had achieved their premorbid levels of function (Tohen et al., 2000). Two year follow-up data on the same cohort showed 98% syndromal remission (i.e., full symptom remission) in contrast to a 38% return to premorbid psychosocial function. These findings are consistent with subsequent studies (Conus et al., 2006, Bonnín et al., 2010, Rosa et al., 2011). Additionally, the relationship between syndromal and functional outcome may not be linear or unidirectional. Low functional status predicts a shorter time to a new mood episode (Gitlin et al., 1995; Weinstock and Miller, 2008).
Mood symptoms are inherently cyclical in bipolar disorder, but the ups and downs of the illness are not always accompanied by predictable changes in functioning. Functioning during a depressive episode may appear to improve as patients recover, but instability or subthreshold mood fluctuations when patients are in partial remission may stall further functional improvement. Mania or psychosis episodes may remit more rapidly than depression, but may also leave “scars” (e.g., cognitive impairment). Cognitive impairments that are present when patients are acutely ill may not remit fully when patients symptomatically recover (Cullen et al., 2016). From this perspective, it is not surprising that patients are less likely to achieve their pre-illness levels of functioning than full symptomatic remission (e.g., Keck et al., 1998).
Another reasonable interpretation of findings concerning persistence of functional impairment is that poor functioning is associated with chronic stressors - financial difficulties, impoverished social support, and family distress are obvious and common examples. Acute stressful life events (Johnson et al., 2008) and high conflict family relationships (Miklowitz et al., 1988) are associated with a greater vulnerability to mood recurrences in both bipolar and unipolar disorders, and patients with mood disorders have been found to generate high levels of interpersonal stress (Hammen et al., 2011). Thus, the relationship between syndromal and functional outcome should be considered to be circular, with symptoms/difficulties in either domain predicting poorer outcome in the other domain.
3. Correlates of functional outcome in bipolar disorder
Understanding the factors associated with functional impairment is a first step towards constructing and testing treatment strategies that might improve the functioning of bipolar individuals.
3.1. Syndromal status
As described above, the cumulative effect of bipolar psychopathology predicts functional outcome. Mood episodes disrupt normal functioning in all spheres. Although mild hypomanias can be associated with normal or even enhanced occupational performance, full blown manias and depressions diminish both occupational and social function (Levy and Manove, 2012; Goodwin and Jamison, 2007). Core manic symptoms such as distractibility, poor judgment and inappropriate social behavior would decrease occupational function and damage interpersonal relationships. For depression, decreased concentration, decreased motivation and fatigue diminish occupational function while social withdrawal, apathy and depressed mood may impair social relationships. Of course, mood symptoms severe enough to require time off work or school and/or hospitalization can result in getting fired or withdrawing from school.
As noted above, global and dimensional measures of psychopathology may predict impairment as well or better than indices such as number of prior episodes. In one study, a cumulative measure of psychopathology was more strongly correlated with functional outcome than was the number of mood episodes (Gitlin et al., 1995). This latter finding implies that either current subsyndromal symptoms or the length of mood episodes may be more prognostically important than chronicity or recurrence.
In an average 3-year follow-up of euthymic bipolar patients, subsyndromal symptoms- both manic and depressed- as well as mood instability were associated with functional disability (Strejilevich et al., 2013). Somewhat counterintuitively, however, depression is consistently found to be more disabling than mania (Gitlin et al., 1995; Bauer et al., 2001; Simon et al., 2007; Gyulai et al., 2008; Tse et al., 2014). In the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD), severity of depression symptoms contributed 61% to the total variance in overall functioning (Gyulai et al., 2008). The results are tempered by the fact that all participants in STEP-BD began in a depressive episode. In another study, interpersonal function correlated with the number of prior episodes of depression but not the number of manic episodes (Gitlin et al., 1995). Additionally, the number of weeks with depression correlated with Global Assessment of Functioning scales scores, whereas the number of weeks of mania did not (Bauer et al., 2001). Similarly, Simon et al. (2007) found that depression correlated more strongly with function (as measured by SF-36 scores) over time than did mania scores. As depressive symptoms improved, some measures of function, specifically social function, correspondingly improved.
Even milder depressive symptoms in bipolar patients are associated with functional impairment (Judd et al., 2005; Bauer et al., 2001; Altshuler et al., 2002, 2006; Samaline et al., 2016). Even Hamilton Depression scores of 7–13, far lower than would be typically seen in major depressive episodes, were associated with lower GAF scores in one study (Altshuler et al., 2002). In a larger multicenter study, subsyndromal depression, as measured by the Inventory of Depressive Symptoms (Ruth et al., 1996) was associated with functional impairment in all domains, with impairment scores more similar in severity to those of patients with fully syndromal depression than to patients who are euthymic (Altshuler et al., 2006). Similar findings were seen in the STEP-BD study (Marangell et al., 2009).
Finally, in a study examining functional recovery from a manic/hypomanic episode in syndromally recovered individuals, the only predictor of functional non-recovery was Hamilton Depression (21-item) score (Gitlin et al., 2011). Of note, the mean Hamilton score of those who were not functionally recovered was only 7.3, compared to 3.5 in the functionally recovered group, again demonstrating that even relatively mild depressive symptoms are associated with functional impairment.
3.2. Neurocognitive factors
It has long been apparent that during mood episodes, both manic and depressed, cognitive abnormalities are substantial and impairing (Cullen et al., 2016). It was initially assumed that these impairments were state specific and resolved with the mood episode’s resolution. However, dozens of studies and multiple meta-analyses have consistently demonstrated the cognitive impairment of euthymic bipolar individuals (Depp et al., 2012; Bourne et al., 2013; Baune and Malhi, 2015; Porter et al., 2015), with a lower bound of 30% (Holmes et al., 2008) and an upper bound of 57.7% (Cullen et al., 2016). Impairment is seen in all cognitive domains studied (Bourne et al., 2013). Across domains, effect sizes range between 0.26 and 0.63, indicating small to medium effects. A review of 23 studies by Cardenas et al. (2016) indicated that patients consistently had impairments in attention, processing speed, verbal learning/memory, and verbal fluency, with more impairment than their unaffected relatives. Although less well studied, bipolar II patients also show impairments that are comparable to bipolar I individuals (Porter et al., 2015; Martino et al., 2014).
Although residual symptoms such as mild depression and medication effects may explain some of these impairments (Bora et al., 2011), they cannot account for a substantial proportion of the deficits seen (Bourne et al., 2013). Psychosis during mood episodes is associated with greater cognitive impairment although the confound of greater symptom severity in psychotic episodes may play a role in this relationship (Porter et al., 2015).
Cognitive deficits in bipolar disorder are seen early in the course of the disorder, even after a first manic episode (Lee et al., 2014; Daglas et al., 2015). Whether the cognitive deficits progress over time is unclear, with some aggregate analyses indicating some degree of “tracking” over time (Bourne et al., 2013; Porter et al., 2015; Strejilevich et al., 2015) and others indicating no consistent evidence of progression of cognitive impairment over a mean of 4.6 years (Samamé et al., 2014). Changes in cognition over longer time frames (i.e., decades) have not been frequently examined (Burdick et al., 2010; Torrent et al., 2012). In one study, cognitive impairment in bipolar disorder was stable over a period of 6.7–11.1 years although verbal fluency and cognitive flexibility worsened over time (Torrent et al., 2012).
Most but not all studies find that both aggregate and specific neurocognitive deficits correlate with functional impairment in bipolar disorder (Sanchez-Moreno et al., 2009; Tse et al., 2014; Wingo et al., 2009, Andereou et al., 2013). In a few studies, these impairments also predict impairment at one-year follow-up (Jaeger et al., 2007; Tabarés-Seisdedos et al., 2008) and four years (Bonnin et al., 2010).
There is little consistency across studies as to which specific neurocognitive domains- attention, executive function vs. working memory- explain the variability in functional outcomes, although one study found that working memory may be the most affected, at least early in the course of the disorder (Daglas et al., 2015). The linkage between mood disturbance and neurocognitive dysfunction appears to be relatively consistent across studies, but mood is not a consistent mediator of cognitive dysfunction in longitudinal studies (Porter et al., 2015). Additionally, there may be different longitudinal predictors of occupational vs. interpersonal functioning. Although neurocognitive variables predict psychosocial functioning in bipolar II patients, it is not clear whether the same domains of cognition are affected in bipolar II vs. I disorder (Martino et al., 2001; Sole et al., 2012).
3.3. Conjoint prediction by depression and neurocognitive functioning
Depression and neurocognitive impairment appear to have independent contributions to functional impairment in bipolar disorder. However, the associations between specific neurocognitive variables and degree of functional impairment can be quite complex.
For example, depression and a single measure of cognitive impairment (free delayed recall) together accounted for 36% of the variance in overall functional outcome in one 4-year study (Bonnín et al., 2010). For any individual patient, of course, one factor may be more relevant in explaining functioning than the others.
Specific contributions of depression and neurocognition may also differ by the specific functional domains considered. For example, occupational outcome and social outcome may both be influenced by depression, but we would expect occupational outcome to be more strongly influenced by inattention or distractibility. In the 4-year study cited above, depression severity and digits recalled backwards (a measure of executive functioning) accounted for 28% of the variance in occupational functioning at follow-up (Bonnín et al., 2010).
Bowie et al. (2010) found that depression and neurocognition were both associated with work skills in bipolar disorder through mediation by social competence (i.e., limited social capacity in simulated interpersonal situations), although depression also had a direct effect on work skills. In the same sample, Depp et al. (2010) showed that a subgroup of patients with bipolar disorder had impaired social competence, which may potentiate the impact of depression and neurocognitive impairment on social performance in real-world settings. These mediational relationships do not appear to be specific to bipolar disorder (Bowie et al., 2010). Additionally, in one study, verbal memory was a mediating variable in the relationship between subsyndromal depression and functional outcomes (Bonnín Cdel et al., 2014).
Few of the studies cited in this article have made the distinction between non-social cognition (i.e., attention, vigilance, working memory, verbal or visual memory using non-social stimuli) vs. social cognition (i.e., processes that involved in the perception and interpretation of social information, such as mentalizing or facial affect identification) and their direct or indirect impact on functional impairment. In patients with bipolar disorder, social cognition appears to be less impaired than non-social cognition, whereas for patients with schizophrenia, social cognition is relatively more impaired (Lee et al., 2014). In schizophrenia, social cognition is more closely associated with community functioning than is non-social cognition (Fett et al., 2011), and appears to mediate the relationship between non-social cognition and functioning. Similar studies comparing the influence of these two domains have not been conducted in bipolar disorder.
3.4. Personality features and substance dependence
As indicated in the model in Fig. 1, personality features clearly predict symptomatic outcomes in bipolar disorder (Fan and Hassell, 2008). In one study, 24% of the variance for social functioning was explained by the N (neuroticism) scale score on the Eysenck Personality Inventory (EPI) (Eysenck and Eysenck, 1964; Pope et al., 2007). Similarly, personality pathology was associated with functional impairment in a small study of bipolar I disorder (Loftus and Jaeger, 2006), although personality features were not independent of mood symptoms. In two studies, personality pathology demonstrated a larger effect size (0.49) for prediction of occupational/employment outcomes than either number of prior hospitalizations (−0.35) or verbal memory performance (0.33; Tse et al., 2014).
Comorbid alcohol dependence is also relevant to the cognitive and functional trajectory of patients with bipolar disorder. Hospitalized bipolar patients with a recent history of alcohol dependence had lower scores on measures of visual memory, verbal memory and executive functioning than bipolar patients without a history of alcohol dependence. Between hospital discharge and follow-up, the group without SUD showed greater gains on verbal and visual memory and cognitive flexibility than those with alcohol dependence, suggesting a degree of dependency between substance use and functional outcomes (Levy et al., 2012).
3.5. Psychosocial stress
Social support and life events are associated with functional impairment, although the causal relationships between these variables are almost certainly multidirectional (Miklowitz and Johnson, 2009b). Family relationships have been found to be associated with both symptomatic and social outcomes in bipolar patients. In a small study, Miklowitz et al. (1988) found that negative parent/offspring interactions during the interval following a hospitalization were associated with poorer social functioning over a 9-month post-hospital period among young adult bipolar I patients. In another longitudinal study, high self-reported levels of social support were associated with better psychosocial functioning, although these two variables were not fully independent of each other (Johnson et al., 2000).
3.6. Relationships between symptom, personality, and functional impairment
Fig. 1 summarizes the relationships described above. Some variables appear to be related in a bidirectional manner, such as the associations between syndromal or subsyndromal states and functional impairment. Other relationships, although based on more limited empirical data, are presumed to be unidirectional (e.g., psychosocial stressors or personality traits affecting syndromal status and functioning). Substance and alcohol abuse are presumed to be predictors of syndromal episodes but also may have unique causal influences on functioning. Research on the causal or temporal primacy of these variables in relation to each other is lacking in bipolar disorder, yet critical to developing targeted treatments to enhance functioning.
4. Treatment implications
Given the evidence just reviewed that depressive symptoms, including subsyndromal symptoms and neurocognitive impairment are the two central factors contributing to functional impairment in bipolar disorder, treatment should focus on more aggressively addressing these two psychopathological domains and the variables that change with them. Table 1 summarizes the suggestions made above, stratified by targeted domain and treatment considerations for each.
Table 1.
“Summary of Proposed Treatment Interventions to enhance function in bipolar individuals”.
| Summary of Proposed Treatment Interventions to enhance function in bipolar individuals | |||
|---|---|---|---|
| Primary | Secondary | Tertiary | Treatment Intervention(s) |
| Prevention of mood episode | Aggressive mood stabilization | ||
| Subsyndromal depression | Aggressive treatment of depression | ||
| Cognitive impairment | Cognitive enhancers Cognitive medication | ||
| Personality disorder/traits | Psychosocial interventions | ||
| Substance abuse | Chemical dependency treatment | ||
| Psychosocial stressors | Psychosocial interventions | ||
Studies over the last twenty years have consistently demonstrated that, even though mania is the defining pole of bipolar disorder, depression is the dominant pole. For both bipolar I and bipolar II disorder, patients spend far more time depression than mania/hypomania (Judd et al., 2002, 2003; Baldessarini et al., 2010). Classifying patients as to their “predominant polarity” by illness history (e.g., a greater proportion of depressive vs. manic episodes) may help identify patients for whom residual states of illness will be particularly disabling (Rosa et al., 2008).
In contrast to mania for which there are consistent treatment algorithms, there is a profound lack of consensus on optimal treatment regimens for bipolar depression. The critical issue is the controversy on both the efficacy and potential dangers of antidepressants in bipolar disorder. More details on the risks and benefits of various treatment approaches can be found in a number of excellent reviews, guidelines and meta-analyses (Ghaemi et al., 2008; Sidor and MacQueen, 2012; Pacchiarotti et al., 2013; Vázquez et al., 2013). Regardless of the treatment algorithm used, even mild depressive symptoms are associated with functional impairment (Altshuler et al., 2002, 2006; Gitlin et al., 2011). Thus, we need to aggressively treat depressive symptoms to remission, regardless of the specific approach used to treat the symptoms.
4.1. Cognitive or functional remediation
Treating/minimizing the neurocognitive impairment associated with bipolar disorder is hampered by the sheer lack of studies examining almost any therapeutic approach. There are a small number of short-term studies indicating that cognitive remediation, analogous to what has been more extensively studied in schizophrenia (Bryce et al., 2016) has positive effects in bipolar disorder (e.g., Anaya et al., 2012). A related psychological therapy, functional remediation, which combines cognitive techniques with training, education and problem-solving has also demonstrated efficacy in both enhancing cognition and psychosocial function (Torrent et al., 2013; Sole et al., 2015; Bonnín et al., 2016; Zyko et al., 2016). In one study, the efficacy of individualized cognitive remediation was superior to treatment as usual but not to superior to group psychoeducation (Torrent et al., 2013). At one year follow-up, the gains in cognition and in function remained for cognitive remediation but not for group psychoeducation (Bonnín et al., 2016).
4.2. Pharmacological approaches
Research on pharmacotherapeutic approaches to treat cognitive impairment in bipolar disorder is even less available. Logically, stimulants would be the agents to consider. Unfortunately, classic dopaminergic stimulants, which are widely used to treat attention deficit hyperactivity disorder (ADHD) have been evaluated only in open studies in bipolar depression (see Corp et al. (2014) for a review). Further, only effects on mood, not cognition, have been reported. Concerns - both reasonable and excessive- about the abuse potential and the potential mood destabilizing effects of dopaminergic stimulants have limited their clinical use.
In another study, the D2/D3 receptor agonist pramipexole was evaluated in a controlled study as a cognitive enhancing agent in bipolar I and II patients (Burdick et al., 2012). Although pramipexole was not more effective than placebo in the entire sample (n=45), it was more effective in the smaller subgroup of euthymic patients, suggesting that in the group with mild subsyndromal depressive symptoms, a cognitive enhancing medication might be less useful.
Nondopaminergic stimulants such as modafanil and armodafanil should also be considered as cognitive enhancing agents. Although studies on their efficacy as adjunctive agents in treating bipolar depression have yielded mixed results (Frye et al., 2015), earlier studies in ADHD suggested potential efficacy in enhancing cognition (Kumar, 2008; Kahbazi et al., 2009). In the bipolar depression studies, modafanil/armodafanil were not associated with increased mania switch rates.
Over the last decade, pharmacotherapeutic agents have been developed specifically targeting the cognitive impairment in schizophrenia. These agents vary in their receptor profile but include targeting dopamine, glutamate and nicotinic subreceptors (Keefe et al., 2013). Those agents that show promise in schizophrenia patients should be tested for their efficacy in bipolar disorder.
4.3. Treatment of comorbid disorders
Aside from depression and cognitive impairment, other areas for therapeutic intervention that might enhance functioning are those related to comorbid disorders. Comorbid personality pathology is associated with poorer function in bipolar individuals (Fan and Hassell, 2008), but there are no treatment studies of bipolar disorder with comorbid personality disorder in which functioning is the targeted outcome. Treating comorbid (e.g. borderline personality disorder) patients using one of the many structured manualized psychotherapies might result in enhanced function in both the interpersonal and occupational domains (Swartz et al., 2005). Similarly, treating comorbid substance use disorders in community groups that also focus on mood management may lead to improvements in overall clinical outcome (Weiss et al., 2009).
4.4. Psychosocial treatments
The clinical implications of the proposed circular relationship between syndromal and functional outcome, in which a poor outcome in either domain predicts greater difficulties in the other domain, are clear: intervention should be optimally considered in both areas with the possibility of improvement in both domains. Thus, preventing mood episodes and enhancing syndromal outcome will result in less functional impairment. Conversely, improving functional outcome-whether through cognitive remediation, other forms of psychotherapy, environmental manipulation or stress management - could result in a decrease in life stress and fewer mood episodes which, in turn, would be likely to enhance functioning. One review found that psychotherapies for bipolar disorder – most of which were psychoeducational - reduced relapses of bipolar disorder with odds ratios averaging 0.57 (95% CI, 0.39–0.82), and enhanced psychosocial functioning with odds ratios averaging 1.2 (95% CI, 0.3 – 2.1) (Scott, 2006).
The STEP-BD trial found that over 9 months, pharmacotherapy and family-focused therapy, interpersonal and social rhythm therapy, or CBT were all more effective than usual care (3 sessions of a self-care psychoeducation manual and pharmacotherapy) in improving life satisfaction and social functioning, although there were no effects on vocational functioning (Miklowitz et al., 2007). A study in adolescents with BD found that FFT and pharmacotherapy were associated with greater improvements over 2 years in some (but not all) domains of quality of life, including family relationships and physical well-being, than brief psychoeducation and pharmacotherapy (O’Donnell et al., in preparation).
In the Pittsburgh Maintenance Therapies in Bipolar Disorder Trial, interpersonal and social rhythm therapy was associated with faster improvements in occupational functioning than an equally paced individual care management treatment (Frank et al., 2008). This finding may suggest a role for sleep/wake rhythm regularity in the maintenance of occupational gains.
5. Conclusion
Although symptomatic episodes, recurrences and mood states continue to dominate as the primary outcome variables in studies of bipolar disorder, functional outcome is increasingly being recognized as an important domain that can be reliably measured. One could argue that functional outcome is even more important than syndromal outcome since the ability to fulfill role expectations at work, at home or at school, and the quality of interpersonal relationships are often cited as the most important outcomes to patients with bipolar disorder and their family members (Michalak et al., 2016). We suggest that functional outcome be considered a primary outcome variable in any and all future bipolar studies. More attention must also be given towards minimizing the effects of syndromal and subsyndromal depression and neurocognitive impairment, treating comorbid disorders, and giving greater considering to the role of psychosocial stress in order to optimize our patients’ ability to lead fulfilling lives.
Footnotes
Conflicts of interest
None for both authors.
References
- Altshuler LL, Gitlin MJ, Mintz J, et al. , 2002. Subsyndromal depression in associated with functional impairment in patients with bipolar disorder. J. Clin. Psychiatry 63, 807–811. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Post Rm, Black DO, et al. , 2006. Subsyndromal depressive symptoms are associated with functional impairment in patients with bipolar disorder: results of a large, multisite study. J. Clin. Psychiatry 67, 1551–1560. [DOI] [PubMed] [Google Scholar]
- Anaya C, Martinez-Aran A, Ayuso-Mateos JL, et al. , 2012. A systematic review of cognitive remediation for schizo-affective and affective disorders. J. Affect Disord 142, 13–21. [DOI] [PubMed] [Google Scholar]
- Andreou C, Bozikas, 2013. The predictive significance of neurocognitive factors for functional outcome in bipolar disorder. Curr. Opin. Psychiatry 26, 54–59. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Salvatore P, Khalsa HM, Gebre-Medhin P, et al. , 2010. Morbidity in 303 first-episode bipolar I disorder patients. Bipolar Disord 12, (264–27). [DOI] [PubMed] [Google Scholar]
- Bauer MS, Kirk GF, Gavin C, et al. , 2001. Determinants of outcome and healthcare costs in bipolar disorder: a high-intensity follow-up study. J. Affect Disord 65, 231–241. [DOI] [PubMed] [Google Scholar]
- Baune BT, Malhi GS, 2015. A review on the impact of cognitive dysfunction on social, occupational and general functional outcomes in bipolar disorder. Bipolar Disord 17, 41–55. [DOI] [PubMed] [Google Scholar]
- Bonnín CM, Martínez-Arán A, Torrent C, et al. , 2010. Clinical and neurocognitive predictors of functional outcome in bipolar euthymic patients: a long-term, follow-up study. J. Affect Disord 121, 156–160. [DOI] [PubMed] [Google Scholar]
- Bonnín CM, Torrent C, Arango C, et al. , 2016. Functional remediation in bipolar disorder: 1-year follow-up of neurocognitive and functional outcome. B J. Psych 208, 87–93. [DOI] [PubMed] [Google Scholar]
- Bonnín Cdel M, González-Pinto A, Solé B, Reinares M, González-Ortega I, Alberich S, Crespo JM, Salamero M, Vieta E, Martínez-Arán A, Torrent C, CIBERSAM Functional Remediation Group, 2014. Verbal memory as a mediator in the relationship between subthreshold depressive symptoms and functional outcome in bipolar disorder. J. Affect Disord 160, 50–54. [DOI] [PubMed] [Google Scholar]
- Bora E, Yucel M, Pantelis C, et al. , 2011. Meta-analytic review of neurocognition in bipolar II disorder. Acta Psychiatr. Scand 123, 165–174. [DOI] [PubMed] [Google Scholar]
- Bourne C, Aydemir O, Balanza-Martinez V, et al. , 2013. Neuropsychological testing of cognitive impairment in euthymic bipolar disorder: an individual patient data meta-analysis. Acta Psychiatr. Scand 128, 149–162. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Depp C, McGrath JA, et al. , 2010. Prediction of real-world functional disability In chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am. J. Psychiatry, 167–1124. [DOI] [PMC free article] [PubMed]
- Bryce S, Sloan E, Lee S, et al. , 2016. Cognitive remediation in schizophrenia: methodological appraisal of systematic reviews and meta-analyses. J. Psychiatr. Res 75, 91–106. [DOI] [PubMed] [Google Scholar]
- Burdick KE, Goldberg JF, Harrow M, 2010. Neurocognitive dysfunction and psychosocial outcome in patients with bipolar I disorder at 15-year follow-up. Acta Psychiatr. Scand 122 (6), 499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick KE, Braga RJ, Nnadi CU, et al. , 2012. Placebo-controlled adjunctive trail of pramipexole in patients with bipolar disorder: targeting cognitive dysfunction. J. Clin. Psychiatry 73, 103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardenas SA, Kassem L, Brotman MA, et al. , 2016. Neurocognitive functioning in euthymic patients with bipolar disorder and unaffected relatives: a review of the literature. Neurosci. Biobehav. Rev 69, 193–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conus P, Cotton S, Abdel-Baki A, et al. , 2006. Symptomatic and functional outcome 12 months after a first episode of psychotic mania: barriers to recovery in a catchment area sample. Bipolar Disord 8, 221–231. [DOI] [PubMed] [Google Scholar]
- Corp SA, Gitlin MJ, Althsuler LL, 2014. A review of the use of stimulants and stimulant alternatives in treating bipolar depression and major depressive disorder. Am. J. Psychiatry 75, 1010–1018. [DOI] [PubMed] [Google Scholar]
- Coryell W, Keller M, Endicott J, et al. , 1989. Bipolar II illness: course and outcome over a five-year period. Psychol. Med 64, 1483–1494. [DOI] [PubMed] [Google Scholar]
- Coryell W, Scheftner W, Keller M, et al. , 1993. The enduring psychosocial consequences of mania and depression. Am. J. Psychiatry 150, 720–727. [DOI] [PubMed] [Google Scholar]
- Cullen B, Ward J, Graham NA, et al. , 2016. Prevalence and correlates of cognitive impairment in euthymic adults with bipolar disorder: a systematic review. J. Affect Disord 205, 165–181. [DOI] [PubMed] [Google Scholar]
- Daglas R, Yucel M, Cotton S, et al. , 2015. Cognitive impairment in first-episode mania: a systematic review of the evidence in the acute and remission phases of the illness. Int. J. Bipolar Disord. 10.1186/s40345-015-0024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depp CA, Mausbach BT, Harvey PD, et al. , 2010. Social competence and observer-related social functioning in bipolar disorder. Bipolar Disord 12, 843–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depp CA, Mausbach BT, Harmell AL, et al. , 2012. Meta-analysis of the association between cognitive abilities and everyday functioning in bipolar disorder. Bipolar Disord 14, 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilsaver SC, 2011. An estimate of the minimum economic burden of bipolar I and II disorders in the United States: 2009. J. Affect Disord 129, 79–83. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, 1976. The global assessment scale: a procedure for measuring overall severity of psychiatric disturbance. Arch. Gen. Psychiatry 33, 766–771. [DOI] [PubMed] [Google Scholar]
- Eysenck SB, Eysenck HJ, 1964. An improved short questionnaire for the measurement of extraversion and neuroticism. Life Sci 3, 1103–1109. [DOI] [PubMed] [Google Scholar]
- Fan AH, Hassell J, 2008. Bipolar disorder and comorbid personality psychopathology: a review of the literature. J. Clin. Psychiatry 69, 1794–1803. [DOI] [PubMed] [Google Scholar]
- Ferrari AJ, Stockings E, Khoo JP, Erskine HE, Degenhardt L, Vos T, Whiteford HA, 2016. The prevalence and burden of bipolar disorder: findings from the Global Burden of disease study 2013. Bipolar Disord 18 (5), 440–450. [DOI] [PubMed] [Google Scholar]
- Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L, 2011. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci. Biobehav. Rev 35 (3), 573–588. 10.1016/j.neubiorev.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Frank E, Soreca I, Swartz HA, et al. , 2008. The role of interpersonal and social rhythm therapy in improving occupational functioning in in patients with bipolar I disorder. Am. J. Psychiatry 165, 1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye MA., et al. , Amchin J, Bauer M, 2015. Randomized, placebo-controlled adjunctive study of armodafinil for bipolar I depression: implications of novel drug design and heterogeneity of concureent bipolar maintenance treatments. Int. J. Bipolar Disord 1 (34). 10.1186/s40345-015-0034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaemi SN, Wingo AP, Filkowski MA, Baldessarini RJ, 2008. Long-term antidepressant treatment in bipolar disorder: meta-analyses of benefits and risks. Acta Psychiatr. Scand 118, 347–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gignac A, McGirr A, Lam RW, et al. , 2015. Recovery and recurrence following a first episode of mania: a systematic review and meta-analysis of prospectively characterized cohorts. J. Clin. Psychiatry 76, 1241–1248. [DOI] [PubMed] [Google Scholar]
- Gitlin M, Frye MA, 2012. Maintenance therapies in bipolar disorders. Bipolar Disord 14, 51–65. [DOI] [PubMed] [Google Scholar]
- Gitlin MJ, Swendsen J, Heller TL, et al. , 1995. Relapse and impairment in bipolar disorder. Am. J. Psychiatry 152, 1635–1640. [DOI] [PubMed] [Google Scholar]
- Gitlin MJ, Mintz J, Sokolski K, et al. , 2011. Subsyndromal depressive symptoms after symptomatic recovery from mania are associated with delayed functional recovery. J. Clin. Psychiatry 72, 692–697. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR, 2007. Manic-Depressive Illness 2nd ed. Oxford University Press, New York, 119–155. [Google Scholar]
- Gyulai L, Bauer MS, Marangell LB, et al. , 2008. Correlates of functioning in bipolar disorder. Psychopharmacol. Bull 41, 51–64. [PubMed] [Google Scholar]
- Hamilton M, 1960. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Le Brocque R, 2011. Youth depression and early childrearing: stress generation and intergenerational transmission of depression. J. Consult Clin. Psychol 79, 353–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes MK, Erickson K, Luckenbaugh DA, et al. , 2008. A comparison of cognitive functioning in medicated and unmedicated subjects with bipolar depression. Bipolar Disord 10, 806–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaeger J, Berns S, Loftus S, et al. , 2007. Neurocognitive test performance predicts functional recovery from acute exacerbation leading to hospitalization in bipolar disorder. Bipolar Disord 9, 93–102. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Meyer B, Winett C, et al. , 2000. Social support and self-esteem predict changes in bipolar depression but not mania. J. Affect Disord 58, 79–86. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Cuellar A, Ruggero C, et al. , 2008. Life events as predictors of mania and depression in bipolar I disorder. J. Abnorm Psychol 117, 268–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, et al. , 2002. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch. Gen. Psych 59, 530–537. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, et al. , 2003. A prospective investigation of the natural history investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch. Gen. Psych 60, 261–269. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, et al. , 2005. Psychosocial disability in course of bipolar I and II disorders: a prospective, comparative, longitudinal study arch. Gen. Psych 62, 1322–1330. [DOI] [PubMed] [Google Scholar]
- Judd LL, Schettler PJ, Solomon DA, et al. , 2008. Psychosocial disability and work role function compared across the long-term course of bipolar I, bipolar II and unipolar major depressive disorders. J. Affect Disord 108, 49–58. [DOI] [PubMed] [Google Scholar]
- Kahbazi M, Ghoreishi A, Rahiminejad F, et al. , 2009. A randomized, double-blind and placebo-controlled trial of modafinil in children and adolescents with attention deficit and hyperactivity disorder. Psychiatry Res 168, 234–237. [DOI] [PubMed] [Google Scholar]
- Keck PE, 2006. Long-term management strategies to achieve optimal function in patients with bipolar disorder. J. Clin. Psychiatry 67, 19–24. [PubMed] [Google Scholar]
- Keck PEJ, McElroy SL, Strakowski SM, et al. , 1998. Twelve-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am. J. Psychiatry 155, 646–652. [DOI] [PubMed] [Google Scholar]
- Keefe RS, Buchanan RW, Marder SR, et al. , 2013. Clinical trials of potential cognitive-enhancing drugs in schizophrenia: what have we learned so far? Schizophr. Bull 39, 417–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraepelin E, 1921. Manic Depressive Insanity and Paranoia Livingstone, Edinburgh, E.S.. [Google Scholar]
- Kumar R, 2008. Approved and investigational uses of modafinil. Drugs 68, 1803–1839. [DOI] [PubMed] [Google Scholar]
- O’Donnell L Axelson DA Kowatch RA Sugar C Schneck CD Miklowitz DJ, 2016. Two-year effects of family-focused treatment on quality of life among adolescents with bipolar disorder Manuscript Under Review. [DOI] [PMC free article] [PubMed]
- Lee RS, Hermens DF, Scott J, et al. , 2014. A meta-analysis of neuropsychological functioning in first-episode bipolar disorders. J Psychiatr. Res 57, 1–11. [DOI] [PubMed] [Google Scholar]
- Levy B, Manove E, 2012. Functional outcome in bipolar disorder: the big picture. Depr. Res. Treatm 949248, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B, Manove E, Weiss RD, 2012. Recovery of cognitive functioning in patients with co-occurring bipolar disorder and alcohol dependence during early remission from an acute mood episode. Ann. Clin. Psychiatry 24, 143–154. [PMC free article] [PubMed] [Google Scholar]
- Loftus ST, Jaeger J, 2006. Psychosocial outcome in bipolar I patients with a personality disorder. J. Nerv. Ment. Dis 194, 967–970. [DOI] [PubMed] [Google Scholar]
- MacQueen GM, Young LT, Joffe RT, 2001. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatr. Scand 103, 163–170. [DOI] [PubMed] [Google Scholar]
- Marangell LB, Dennehy EB, Miyahara S, et al. , 2009. The functional impact of subsyndromal depressive symptoms in bipolar disorder: data from STEP-BD. J. Affect Disord 114, 58–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino DJ, Igoa A, Marengo E, et al. , 2001. Neurocognitive impairments and their relationship with psychosocial functioning and euthymic bipolar II disorder. J. Nerv. Ment. Dis 199, 459–646. [DOI] [PubMed] [Google Scholar]
- Martino DJ, Strejilevich SA, Marengo E, et al. , 2014. Toward the identification of neurocognitive subtypes in euthymic patients with bipolar disorder. J. Affect Disord 167, 118–124. [DOI] [PubMed] [Google Scholar]
- Michalak EE, Yatham LN, Lam RW, 2005. Quality of life in bipolar disorder: a review of the literature. Health Qual. Life Outcomes 10.1186/1477-7525-3-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak EE, Jones S, Lobban F, et al. , 2016. Harnessing the potential of community-based participatory research approaches in bipolar disorder. Int. J. Bipolar Disord. 10.1186/s40345-016-00485-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Johnson SL, 2009a. Social and familial risk factors in bipolar disorder: basic processes and relevant interventions. Clin. Psychol.: Sci. Pract 16 (2), 281–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Johnson SL, 2009b. Social and familial factors in the course of bipolar disorder: basic processes and relevant interventions. Clin. Psychol. N.Y 16, 281–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Nuechterlein KH, et al. , 1988. Family factors and the course of bipolar affective disorder. Arch. Gen. Psychiatry 45, 225–231. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, et al. , 2007. Psychosocial treatments for bipolar depression: a 1-year randomized trial from the systematic treatment enhancement program. Arch. Gen. Psych 64, 419–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacchiarotti I, Bond DJ, Baldessarini RJ, et al. , 2013. The international society of bipolar disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am. J. Psychiatry 167, 792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope M, Dudley R, Scott J, 2007. Determinant of social functioning in bipolar disorder. Bipolar Disord 9, 38–44. [DOI] [PubMed] [Google Scholar]
- Porter RJ, Robinson LJ, Malhi GS, et al. , 2015. The neurocognitivie profile of mood disorders – a review of the evidence and methodological issues. Bipolar Disord 17, 21–40. [DOI] [PubMed] [Google Scholar]
- Rosa AR, Sanchez-Moreno J, Martinez-Aran A, et al. , 2007. Validity and reliability of the functioning assessment short test (FAST) in bipolar disorder. Clin. Pract. Epidemiol. Ment. Health 10.1186/1745-0179-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa AR, Reinares M, Amann B, et al. , 2011. Six-month functional outcome of a bipolar disorder cohort in context of a specialized-care program. Bipolar Disord 13, 679–686. [DOI] [PubMed] [Google Scholar]
- Rosa AR 1, Andreazza AC, Kunz M, et al. , 2008. Validity and reliability of the functioning assessment short test (FAST) in bipolar disorder. Clin. Pract. Epidemiol. Ment. Health 107, 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggero CJ, Chelminsky I, Young D, et al. , 2007. Psychosocial impairment associated with bipolar II disorder. J. Affect Disord 104, 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruth AJ, Gullion CM, Basco MR, et al. , 1996. The inventory of depressive symptomatology (IDS): psychometric properties. Psychol. Med 26, 477–486. [DOI] [PubMed] [Google Scholar]
- Salcedo S, Gold AK, Sheikh S, Marcus PH, Nierenberg AA, Deckersbach T, Sylvia LG, 2016. Empirically supported psychosocial interventions for bipolar disorder: current state of the research. J. Affect. Disord 201, 203–214. [DOI] [PubMed] [Google Scholar]
- Samaline L, de Chazeron I, Vieta E, et al. , 2016. Residual symptoms and specific functional impairments in euthymic patients with bipolar disorder. Bipolar Disord 18, 164–173. [DOI] [PubMed] [Google Scholar]
- Samamé C, Martino DJ, Strejilevich SA, 2014. Longitudinal course of cognitive deficits in bipolar disorder: a meta analytic study. J. Affect Disord 164, 130–138. [DOI] [PubMed] [Google Scholar]
- Sanchez-Moreno J, Martinez-Aran A, Tabarés-Seisdedos R, et al. , 2009. Functioning and disability in bipolar disorder: an extensive review. Psychother. Psychosom 78, 285–297. [DOI] [PubMed] [Google Scholar]
- Scott J, 2006. Psychotherapy for bipolar disorders: efficacy and effectiveness. J. Psychopharmacol 20, 46–50. [DOI] [PubMed] [Google Scholar]
- Sidor MM, MacQueen GM, 2012. An update on antidepressant use in bipolar depression. Curr. Psychiatry Rep 14, 696–704. [DOI] [PubMed] [Google Scholar]
- Simon GE, Bauer MS, Ludman EJ, et al. , 2007. Mood Symptoms, functional impairment, and disability in people with bipolar disorder: specific effects of mania and depression. J. Clin. Psychiatry 68, 1237–1245. [DOI] [PubMed] [Google Scholar]
- Sole B, Bonnin CM, Torrent C, et al. , 2012. Neurocognitive impairment and psychosocial functioning in bipolar disorder. Acta Psychiatr. Scand 125, 309–371. [DOI] [PubMed] [Google Scholar]
- Sole B, Bonnin CM, Mayoral M, et al. , 2015. Functional remediation for patients with bipolar II disorder: improvement of functioning and subsyndromal symptoms. Eur. Neuropsychopharmacol 25, 257–264. [DOI] [PubMed] [Google Scholar]
- Strejilevich SA, Martino DJ, Murru A, et al. , 2013. Mood instability and functional recovery in bipolar disorder. Acta Psychiatr. Scand 128, 194–202. [DOI] [PubMed] [Google Scholar]
- Strejilevich SA, Samame C, Martino DJ, 2015. The trajectory of neuropsychological dysfunctions in bipolar disorders: a critical examination of hypothesis. J. Affect Disord 175, 396–402. [DOI] [PubMed] [Google Scholar]
- Swartz HA, Pilkonis PA, Frank E, et al. , 2005. Acute treatment outcomes in patients with bipolar I disorder and co-morbid borderline personality disorder receiving medication and psychotherapy. Bipolar Disord 7, 192–197. [DOI] [PubMed] [Google Scholar]
- Tabarés-Seisdedos R, Balanzá-Martínez V, Sánchez-Moreno J, et al. , 2008. Neurocognitive and clinical predictors of functional outcome in patients with schizophrenia and bipolar I disorder at one-year follow up. J. Affect Disord 109, 286–299. [DOI] [PubMed] [Google Scholar]
- Tohen M, Hennen J, Zarate CM Jr, et al. , 2000. Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am. J. Psychiatry 157, 220–228. [DOI] [PubMed] [Google Scholar]
- Torrent C, Martinez-Arán A, del Mar Bonnin C, Reinares M, Daban C, Solé B, Rosa AR, Tabarés-Seisdedos R, Popovic D, Salamero M, Vieta E, 2012. Long-term outcome of cognitive impairment in bipolar disorder. J. Clin. Psychiatry 73, e899–e905. [DOI] [PubMed] [Google Scholar]
- Torrent C, Bonnin CM, Anabel Martinez-Aran, et al. , 2013. Efficacy of functional remediation in bipolar disorder: a multicenter randomized controlled study. Am. J. Psychiatry 170, 852–859. [DOI] [PubMed] [Google Scholar]
- Tse S, Chan S, Ng KL, et al. , 2014. Meta-analysis of predictors of favorable employment outcomes among individuals with bipolar disorder. Bipolar Disord 16, 217–229. [DOI] [PubMed] [Google Scholar]
- Vázquez GH, Tondo L, Undurraga J, Baldessarini RJ, 2013. Overview of antidepressant treatment of bipolar depression. Int. J. Neuropsychopharmacol 16, 1673–1685. [DOI] [PubMed] [Google Scholar]
- Weinstock LM, Miller IW, 2008. Functional impairment as a predictor of short-term symptom course in bipolar I disorder. Bipolar Disord 10, 437–442. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Jaffee, et al. , 2009. A community-friendly” version of integrated group therapy for patients with bipolar disorder and substance dependence: a randomized controlled trial. Drug Alcohol Depend 104, 212–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo AP, Harvey PD, Baldessarini RJ, et al. , 2009. Neurocognitive impairment in bipolar disorder patients: functional implications. Bipolar Disord 11 (2), 113–125. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, et al. , 1978. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry 133, 429–435. [DOI] [PubMed] [Google Scholar]
- Zyko S, Jabben N, Schulte P, et al. , 2016. A pilot study of combined group and individual functional remediation program for patients with bipolar I disorder. J. Affect Disord 194, 9–15. [DOI] [PubMed] [Google Scholar]


