Abstract
Objectives
Bimekizumab selectively neutralises both interleukin (IL)-17A and IL-17F. We report efficacy and safety in a phase IIb dose-ranging study in patients with active ankylosing spondylitis (AS).
Methods
Adults with AS (fulfilling modified New York criteria) were randomised 1:1:1:1:1 to bimekizumab 16 mg, 64 mg, 160 mg, 320 mg or placebo every 4 weeks for 12 weeks (double-blind period). At week 12, patients receiving bimekizumab 16 mg, 64 mg or placebo were re-randomised 1:1 to bimekizumab 160 mg or 320 mg every 4 weeks to week 48; other patients continued on their initial dose (dose-blind period). The primary end point was Assessment of SpondyloArthritis international Society (ASAS) 40 response at week 12 (non-responder imputation (NRI) for missing data).
Results
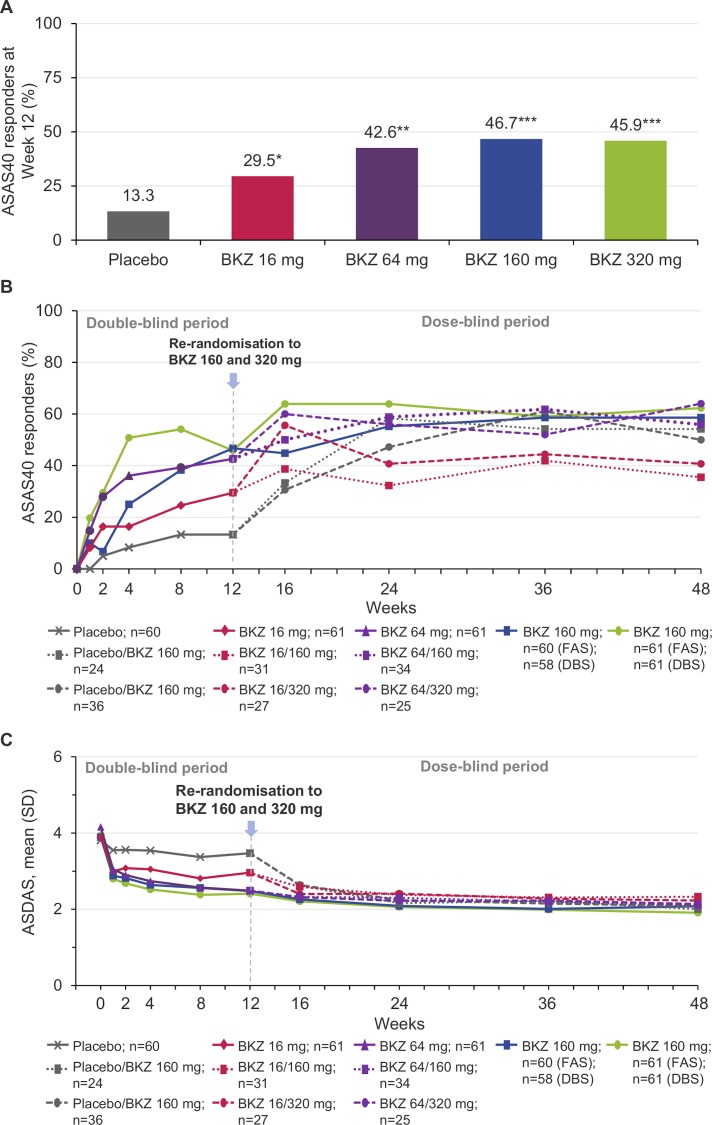
303 patients were randomised: bimekizumab 16 mg (n=61), 64 mg (n=61), 160 mg (n=60), 320 mg (n=61) or placebo (n=60). At week 12, significantly more bimekizumab-treated patients achieved ASAS40 vs placebo (NRI: 29.5%–46.7% vs 13.3%; p<0.05 all comparisons; OR vs placebo 2.6–5.5 (95% CI 1.0 to 12.9)). A significant dose-response was observed (p<0.001). The primary end point was supported by all secondary efficacy outcomes. At week 48, 58.6% and 62.3% of patients receiving bimekizumab 160 and 320 mg throughout the study achieved ASAS40, respectively (NRI); similar ASAS40 response rates were observed in re-randomised patients. During the double-blind period, treatment-emergent adverse events occurred in 26/60 (43.3%) patients receiving placebo and 92/243 (37.9%) receiving bimekizumab.
Conclusions
Bimekizumab provided rapid and sustained improvements in key outcome measures in patients with active AS, with no unexpected safety findings versus previous studies.
Trial registration number
Keywords: ankylosing spondylitis, spondyloarthritis, DMARDs (biologic), treatment
Key messages.
What is already known about this subject?
There remains a need for treatment options in ankylosing spondylitis (AS) that can provide sustained, long-term disease control and improve patient quality of life.
What does this study add?
Bimekizumab, a monoclonal antibody that neutralises both interleukin (IL)-17A and IL-17F, has shown clinically relevant improvements in both psoriasis and psoriatic arthritis, leading to its evaluation in other IL-17-mediated diseases.
This is the first study to assess bimekizumab in patients with active AS.
A significant dose-response was observed with bimekizumab for ASAS40 at week 12 (p<0.05), with a rapid onset and greater ASAS40 response rates for all doses of bimekizumab versus placebo, which continued to increase to week 48.
A similar pattern was observed across secondary outcomes, representing improvements in quality of life measures versus placebo and over time.
Safety was in line with previous bimekizumab studies and comparable with the IL-17A inhibitor class.
How might this impact on clinical practice or future developments?
Results from this study contribute to the growing body of evidence supporting dual neutralisation of IL-17A and IL-17F with bimekizumab as a novel therapeutic option for the treatment of AS.
Phase III studies in patients with AS and non-radiographic axial spondyloarthritis are ongoing.
Introduction
Ankylosing spondylitis (AS) is a chronic disease, characterised by inflammation of the axial skeleton.1 It is also referred to as radiographic axial spondyloarthritis (r-axSpA). AS can often be accompanied by other manifestations such as peripheral enthesitis and arthritis, uveitis, inflammatory bowel disease (IBD) and psoriasis.1 2 Expression of human leucocyte antigen (HLA)-B27 is strongly associated with the disease, and patients often have elevated levels of inflammatory markers such as C reactive protein (CRP).1 Patients experience chronic pain and functional impairment, impacting on sleep, daily activities and overall quality of life,3–5 with some patients experiencing physical disability due to structural damage of the spine.6
Non-steroidal anti-inflammatory drugs (NSAIDs) are a first-line treatment to provide symptomatic relief to patients with AS.7 However, response to NSAIDs may be inadequate or they may be contraindicated. Conventional synthetic disease-modifying antirheumatic drugs, such as methotrexate or sulfasalazine, are not efficacious in axial disease, although the latter may be effective for patients with peripheral arthritis.7 Tumour necrosis factor (TNF) inhibitors are the first-line biologic in patients with high disease activity, but not all patients achieve adequate disease control or tolerate treatment.8 9 Interleukin (IL)-17A inhibitors are effective second-line therapies10 11; however, some patients may still experience unsatisfactory response and require alternative treatments.
The IL-17 axis represents an established target in AS treatment, and inflammation is associated with an increase in IL-17-producing innate immune cells.12 Two members of the IL-17 cytokine family, IL-17A and IL-17F, share ~50% structural homology and have similar pro-inflammatory function, signalling via the same receptor complex.13 14 Preclinical evidence from human in vitro assays has shown that IL-17A and IL-17F cooperate with other mediators of inflammation, such as TNF, to amplify inflammatory responses.15 The contribution of IL-17F, in addition to IL-17A, to pathological bone formation has been shown in a human periosteum-derived stem cell model of osteogenic differentiation, indicating that neutralisation of both cytokines inhibits this process to a greater extent than IL-17A alone.16 17 In addition, levels of IL-17A and IL-17F have been found to be higher in the serum of patients with AS versus healthy controls, correlating with markers of systemic inflammation.18 19
Bimekizumab is a monoclonal antibody developed to selectively neutralise both IL-17A and IL-17F,20 and has been previously evaluated in a first-in-human study in patients with mild psoriasis, a proof-of-concept study in patients with moderate-to-severe psoriatic arthritis (PsA) and a phase IIb dose-ranging study in patients with moderate-to-severe plaque psoriasis.15 20 21 The overlap in symptoms between psoriasis, PsA and AS,2 22 and involvement of the IL-17 pathway, led to the evaluation of bimekizumab as a potential therapeutic option in AS. Here, we report results of the phase IIb BE AGILE study, the first dose-ranging clinical study evaluating the efficacy and safety of bimekizumab in patients with active AS.
Methods
Study design
This phase IIb, randomised, 48-week, double-blind, placebo-controlled, parallel-group, dose-ranging study (BE AGILE) (online supplementary files 1; 2) was conducted at 74 centres across 10 countries in Europe and the USA.
annrheumdis-2020-216980supp001.pdf (1.7MB, pdf)
annrheumdis-2020-216980supp002.pdf (118.4MB, pdf)
Patient and public involvement
Patients with AS were consulted to understand treatment needs and recommend ways to facilitate study participation while minimising the burden of study visits. Study participants were recruited by the study sites and provided written consent to participate.
Participants
Eligible patients were ≥18 years of age with AS, as determined by documented radiographic sacroiliitis (X-rays were centrally read by two readers and a third in case of discrepancy), fulfilling the modified New York (mNY) criteria for AS,23 symptom duration of ≥3 months, age at onset of <45 years, with active disease as defined by Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score of ≥4 and spinal pain ≥4 on a 0–10 numerical rating scale (NRS) (from BASDAI question 2). Patients were required to have at least one of the following: inadequate response to NSAIDs (defined as a lack of response for ≥4 weeks of continuous NSAID therapy or the lack of response to ≥2 NSAIDs at the maximum tolerated dose for ≥4 weeks), intolerance to ≥1 NSAID or contraindication(s) to NSAIDs. Prior treatment with up to one TNF inhibitor was permitted, which must have been discontinued because of inadequate response, intolerance or loss of access.
Patients with active/symptomatic Crohn’s disease or ulcerative colitis (UC) were excluded; previous history of Crohn’s disease or UC was not an exclusion criterion. Other exclusion criteria were total ankylosis of the spine, a concurrent or history of malignancy during the past 5 years, a diagnosis of other inflammatory conditions (eg, rheumatoid arthritis), active infection or infection requiring antibiotics within 2 weeks of baseline, a history of chronic or recurrent infections or a serious/life-threatening infection within 6 months of baseline, presence of significant, uncontrolled neuropsychiatric disorder, active suicidal ideation, or positive suicide behaviour within the past 6 months.
Interventions
Initially, patients were randomised 1:1:1:1:1 to receive subcutaneous bimekizumab 16 mg, 64 mg, 160 mg, 320 mg or placebo every 4 weeks. At the end of the double-blind period at week 12, following all assessments, patients were re-allocated treatment for the dose-blind period as follows: patients initially receiving placebo, bimekizumab 16 mg or 64 mg were randomised 1:1 to receive bimekizumab 160 or 320 mg every 4 weeks through to week 48. Patients in the bimekizumab 160 and 320 mg groups continued on the same schedule through to week 48 (figure 1; see online supplementary methods for additional information on interventions and randomisation and masking).
Figure 1.
(A) ASAS40 response at week 12 (primary efficacy end point; FAS, NRI). *P value vs placebo calculated from a logistic regression model including fixed effects for treatment, geographic region and prior TNF inhibitor exposure; *p<0.05, **p<0.01, ***p<0.001. (B) ASAS40 responses over 48 weeks; FAS, NRI (weeks 0–12); DBS, NRI (weeks 12–48). (C) ASDAS over time; FAS, MI (weeks 0–12); DBS, MI (weeks 12–48). ASAS40, Assessment of SpondyloArthritis international Society improvement of ≥40%; ASDAS, Ankylosing Spondylitis Disease Activity Score; BKZ, bimekizumab; DBS, dose-blind set; FAS, full analysis set; MI, multiple imputation; NRI, non-responder imputation.
Outcomes
The primary efficacy end point was the percentage of patients with an Assessment of SpondyloArthritis international Society (ASAS) 40 response at week 12, defined according to the ASAS Handbook.24
Secondary efficacy end points were ASAS20 response, ASAS5/6 response, change from baseline in BASDAI, Bath Ankylosing Spondylitis Functional Index (BASFI) and Ankylosing Spondylitis Disease Activity Score with CRP (ASDAS), all at week 12. Additional efficacy end points included ASAS40, ASAS20, ASDAS inactive disease (ID; <1.3), ASDAS low disease activity (ASDAS-LDA; 1.3–<2.1),25 ASDAS major improvement (ASDAS-MI; reduction ≥2.0 from baseline), ASAS partial remission (PR), change from baseline in the linear version of the Bath Ankylosing Spondylitis Metrology Index (BASMI)26 and change from baseline in Maastricht Ankylosing Spondylitis Enthesitis Score (MASES) index. Additional outcomes included measurement of high-sensitivity CRP (hs-CRP) levels in blood samples and MRI performed in a subset of patients (20 planned per treatment group) to evaluate the effect of bimekizumab on objective signs of inflammation (see online supplementary methods for additional information).
Patient-reported outcomes (PROs) included change from baseline in Ankylosing Spondylitis Quality of Life (ASQoL), 36-Item Short Form Survey (SF-36) and sleep quality (Medical Outcomes Study (MOS)-12 item scale). Post hoc analyses included patients achieving a ≥50% improvement in BASDAI response (BASDAI 50) and change from baseline in fatigue (BASDAI question 1).
Safety monitoring included incidence of adverse events (AEs), serious AEs (SAEs), withdrawal due to AEs and AEs of special interest. AEs identified for additional safety monitoring included: serious infections including opportunistic and tuberculosis, cytopenia, severe hypersensitivity reactions, IBD, suicide ideation or behaviour, depression and anxiety, major cardiovascular events (MACE), malignancies and liver function test changes.
Statistical analysis
The sample size was calculated using a two-sided test for detecting a linear trend across proportions at a significance level of 0.05.27 Assuming 57 patients in each treatment group, the test for detecting the overall dose response based on ASAS40 treatment response was powered at >99%. Sample size calculations were based on ASAS40 response data from phase III studies of TNF inhibitors and secukinumab in patients with AS,11 28 29 performed using nQuery Advisor 7.0.
The full analysis set (FAS) consisted of all randomised patients who received ≥1 dose of study drug and had a valid measurement of the ASAS components at baseline. All patients starting the dose-blind period and who received ≥1 dose of study drug were included in the dose-blind set. The per-protocol set (PPS) consisted of all patients in the FAS who had no important protocol deviation affecting the primary efficacy end point. The safety set (SS) consisted of all randomised patients who received at least one dose of study drug.
The primary analysis was based on a Mantel-Haenszel test30 and modified ridit scores with the corresponding p value. Non-responder imputation (NRI) was used to account for missing data. Pairwise comparisons of each bimekizumab dose versus placebo for ASAS40 at week 12 were based on a logistic regression model with fixed effects for treatment, region and prior TNF inhibitor exposure. Multiplicity was accounted for using a fixed sequence testing procedure with each bimekizumab dose tested sequentially versus placebo from the highest to lowest dose; each test was only conducted if the previous test reached significance at a two-sided significance level of α=0.05, to control the overall type 1 error rate. Further information is provided in the online supplementary files 1 and supplementary file 2. Other categorical end points (ASAS20 response and ASAS5/6) were analysed as for the primary efficacy end point, using NRI to account for missing patient data. For continuous end points (ASDAS, BASDAI and BASFI), multiple imputation (MI) was used to account for missing patient data. Data for the secondary and additional efficacy end points are descriptive only. Post hoc analyses and safety data were summarised using descriptive statistics by each visit.
Results
In total, 601 patients were screened, with 303 randomised and included in the FAS and SS, and 282 in the PPS. The majority of screening failures were patients not fulfilling radiographic sacroiliitis according to mNY criteria (online supplementary figure 2).
The majority of patients (98.0%; 297/303) completed the double-blind period (online supplementary figure 2); 89.5% (265/296) completed the dose-blind period.
Patient demographics and baseline disease characteristics were similar across dose groups (table 1). The study population was typical of a cohort of patients with highly active, established AS; mean ASDAS was >3.5 (3.8–4.2) in all treatment groups and mean time since diagnosis was 7.9 (6.6–8.8) years.
Table 1.
Patient demographics and baseline disease characteristics (FAS)
| Placebo Q4W (n=60) |
BKZ 16 mg Q4W (n=61) | BKZ 64 mg Q4W (n=61) | BKZ 160 mg Q4W (n=60) | BKZ 320 mg Q4W (n=61) | All patients (n=303) |
|
| Age, years, mean (SD) | 39.7 (10.3) | 43.3 (12.6) | 40.4 (10.9) | 42.4 (13.1) | 45.0 (11.4) | 42.2 (11.8) |
| Sex (male), n (%) | 49 (81.7) | 53 (86.9) | 52 (85.2) | 52 (86.7) | 50 (82.0) | 256 (84.5) |
| Caucasian, n (%) | 60 (100) | 58 (95.1) | 60 (98.4) | 59 (98.3) | 61 (100) | 298 (98.3) |
| HLA-B27 positive, n (%) | 57 (95.0) | 51 (83.6) | 56 (91.8) | 52 (86.7) | 54 (88.5) | 270 (89.1) |
| Time since onset of first symptoms, years, mean (SD) | 14.1 (8.4) | 16.2 (10.6) | 12.4 (8.3) | 14.8 (10.3) | 15.3 (10.6) | 14.6 (9.7) |
| Time since diagnosis, years, mean (SD) | 6.6 (7.2) | 8.0 (9.4) | 7.3 (7.8) | 8.8 (9.2) | 8.8 (8.8) | 7.9 (8.5) |
| ASDAS, mean (SD) | 3.8 (0.9) | 3.9 (0.7) | 4.2 (0.8) | 3.9 (0.8) | 3.9 (0.7) | 3.9 (0.8) |
| hs-CRP, mg/L, mean (SD) | 17.6 (24.6) | 15.2 (17.7) | 23.5 (21.6) | 20.5 (19.3) | 18.4 (20.6) | 19.0 (20.9) |
| BASDAI, mean (SD) | 6.5 (1.4) | 6.7 (1.4) | 6.7 (1.3) | 6.3 (1.3) | 6.5 (1.6) | 6.5 (1.4) |
| BASFI, mean (SD) | 5.6 (2.0) | 5.9 (1.7) | 6.0 (1.8) | 5.6 (2.2) | 5.9 (2.0) | 5.8 (2.0) |
| BASMI, mean (SD) | 4.4 (1.6) | 4.8 (1.7) | 4.7 (1.7) | 4.6 (1.8) | 4.8 (1.8) | 4.7 (1.7) |
| Spinal pain score, mean (SD) | 7.0 (1.7) | 7.2 (1.9) | 7.4 (1.6) | 6.6 (2.0) | 7.3 (1.5) | 7.1 (1.7) |
| PGADA, mean (SD) | 7.0 (1.7) | 7.1 (1.5) | 7.3 (1.6) | 6.5 (1.8) | 7.1 (1.9) | 7.0 (1.7) |
| Previous TNF inhibitor therapy, n (%) | 7 (11.7) | 8 (13.1) | 7 (11.5) | 7 (11.7) | 5 (8.2) | 34 (11.2) |
| Current NSAID therapy, n (%) | ||||||
| 1 | 51 (85.0) | 53 (86.9) | 50 (82.0) | 54 (90.0) | 56 (91.8) | 264 (87.1) |
| 2 | 2 (3.3) | 3 (4.9) | 1 (1.6) | 1 (1.7) | 1 (1.6) | 8 (2.6) |
| Receiving csDMARDs, n (%) | 13 (21.7) | 9 (14.8) | 18 (29.5) | 18 (30.0) | 21 (34.4) | 79 (26.1) |
ASDAS, Ankylosing Spondylitis Disease Activity Score; BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; BASFI, Bath Ankylosing Spondylitis Functional Index; BASMI, Bath Ankylosing Spondylitis Metrology Index; BKZ, bimekizumab; CRP, C reactive protein; csDMARD, conventional synthetic disease-modifying antirheumatic drug; HLA-B27, human leucocyte antigen-B27; NSAID, non-steroidal anti-inflammatory drug; PGADA, patient global assessment of disease activity; Q4W, every 4 weeks; TNF, tumour necrosis factor.
Efficacy
Double-blind period (to week 12)
The primary efficacy end point was reached with significantly more patients achieving ASAS40 at week 12 in all bimekizumab-treated groups (16 mg: 29.5%, OR vs placebo 2.6 (95% CI: 1.0 to 6.5); 64 mg: 42.6%, OR 4.5 (95% CI: 1.8 to 10.9); 160 mg: 46.7%, OR 5.5 (95% CI: 2.3 to 13.5); 320 mg: 45.9%, OR 5.3 (95% CI: 2.2 to 12.9)) compared with placebo (13.3%; all comparisons p<0.05) (figure 1A, table 2 and online supplementary table 1). A statistically significant dose response was observed for ASAS40 at week 12 (p<0.001), with a dose-response effect observed across bimekizumab 16–160 mg doses and similar ASAS40 response between the 160 and 320 mg groups. Rapid responses with bimekizumab were observed, with 8.2%–19.7% and 16.4%–50.8% of patients achieving ASAS40 at week 1 and at week 4 vs 0% and 8.3% receiving placebo, respectively (figure 1B and online supplementary figure 3).
Table 2.
Primary and secondary efficacy end points (week 12; FAS, NRI/MI)
| Placebo Q4W (n=60) | BKZ 16 mg Q4W (n=61) | BKZ 64 mg Q4W (n=61) | BKZ 160 mg Q4W (n=60) | BKZ 320 mg Q4W (n=61) | |
| ASAS40*, n (%) | |||||
| Week 12 | 8 (13.3) | 18 (29.5) | 26 (42.6) | 28 (46.7) | 28 (45.9) |
| ASAS20*, n (%) | |||||
| Week 12 | 17 (28.3) | 25 (41.0) | 38 (62.3) | 35 (58.3) | 44 (72.1) |
| ASAS5/6*, n (%) | |||||
| Week 12 | 4 (6.7) | 18 (29.5) | 30 (49.2) | 32 (53.3) | 33 (54.1) |
| BASDAI†, mean (SD) | |||||
| Baseline | 6.5 (1.4) | 6.7 (1.4) | 6.7 (1.3) | 6.3 (1.3) | 6.5 (1.6) |
| Week 12 | 5.5 (2.2) | 5.0 (2.1) | 3.9 (2.1) | 3.8 (2.0) | 3.7 (2.1) |
| Change from baseline | −1.0 (1.7) | −1.7 (2.3) | data-fill="true"−2.7 (2.2) | −2.5 (1.8) | −2.9 (2.2) |
| BASFI, mean (SD), | |||||
| Baseline | 5.6 (2.0) | 5.9 (1.7) | 6.0 (1.8) | 5.6 (2.2) | 5.9 (2.0) |
| Week 12 | 5.0 (2.4) | 4.6 (2.4) | 4.1 (2.3) | 3.9 (2.2) | 3.7 (2.5) |
| Change from baseline | −0.6 (1.9) | −1.4 (2.2) | −1.9 (2.4) | −1.7 (1.8) | −2.2 (2.0) |
| ASDAS†, mean (SD), | |||||
| Baseline | 3.8 (0.9) | 3.9 (0.7) | 4.2 (0.8) | 3.9 (0.8) | 3.9 (0.7) |
| Week 12 | 3.5 (1.1) | 3.0 (0.9) | 2.5 (0.9) | 2.5 (1.0) | 2.4 (0.9) |
| Change from baseline | −0.4 (0.7) | −0.9 (1.0) | −1.7 (1.1) | −1.4 (0.9) | −1.5 (0.9) |
*NRI.
†MI.
ASAS, Assessment of SpondyloArthritis international Society; ASDAS, Ankylosing Spondylitis Disease Activity Score; BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; BASFI, Bath Ankylosing Spondylitis Functional Index; BKZ, bimekizumab; FAS, full analysis set; MI, multiple imputation; NRI, non-responder imputation; Q4W, every 4 weeks.
The primary end point was supported by all secondary efficacy end points (online table 2). At week 12, a higher proportion of patients achieved ASAS20 and ASAS5/6 in the bimekizumab-treated groups compared with placebo. In addition, reductions from baseline in BASDAI, BASFI and ASDAS were greater in the bimekizumab-treated groups compared with placebo (table 2 and figure 1C). Other efficacy end points also indicated improvements from baseline at week 12. ASDAS-MI was achieved by 18.0%–34.4% of bimekizumab-treated patients vs 0% receiving placebo; ASDAS-ID was achieved by 3.3%–10.0% vs 0%, ASDAS-LDA was achieved by 14.8%–32.8% vs 13.3%, while ASAS-PR was achieved by 8.2%–23.0% vs 3.3%, respectively. Reductions from baseline in the MASES index were observed in patients with baseline enthesitis across bimekizumab dose groups (table 3). In post hoc analyses, BASDAI 50 was achieved by 37.9% and 47.5% of patients receiving bimekizumab 160 and 320 mg, respectively (table 3).
Table 3.
Other efficacy end points up to 48 weeks of bimekizumab treatment (DBS, NRI and MI)
| n (%) | Placebo → | BKZ 16 mg → | BKZ 64 mg → | BKZ 160 mg (n=58) | BKZ 320 mg (n=61) | ||||
| BKZ 160 mg (n=24) | BKZ 320 mg (n=36) | BKZ 160 mg (n=31) | BKZ 320 mg (n=27) | BKZ 160 mg (n=34) | BKZ 320 mg (n=25) | ||||
| ASAS40* | Baseline | – | – | – | – | – | – | – | – |
| Week 12 | 5 (20.8) | 3 (8.3) | 12 (38.7) | 6 (22.2) | 16 (47.1) | 10 (40.0) | 28 (48.3) | 28 (45.9) | |
| Week 48 | 13 (54.2) | 18 (50.0) | 11 (35.5) | 11 (40.7) | 19 (55.9) | 16 (64.0) | 34 (58.6) | 38 (62.3) | |
| ASAS20* | Baseline | – | – | – | – | – | – | – | – |
| Week 12 | 9 (37.5) | 8 (22.2) | 14 (45.2) | 11 (40.7) | 21 (61.8) | 17 (68.0) | 35 (60.3) | 44 (72.1) | |
| Week 48 | 17 (70.8) | 22 (61.1) | 17 (54.8) | 14 (51.9) | 25 (73.5) | 20 (80.0) | 45 (77.6) | 46 (75.4) | |
| ASAS5/6* | Baseline | – | – | – | – | – | – | – | – |
| Week 12 | 2 (8.3) | 2 (5.6) | 10 (32.3) | 8 (29.6) | 19 (55.9) | 11 (44.0) | 32 (55.2) | 33 (54.1) | |
| Week 48 | 15 (62.5) | 16 (44.4) | 13 (41.9) | 13 (48.1) | 21 (61.8) | 20 (80.0) | 37 (63.8) | 40 (65.6) | |
| ASAS-PR* | Baseline | 0 | 0 | 0 | 0 | 0 | 0 | 1.7 | 0 |
| Week 12 | 1 (4.2) | 1 (2.8) | 3 (9.7) | 2 (7.4) | 5 (14.7) | 4 (16.0) | 10 (17.2) | 14 (23.0) | |
| Week 48 | 8 (33.3) | 8 (22.2) | 4 (12.9) | 8 (29.6) | 7 (20.6) | 7 (28.0) | 17 (29.3) | 21 (34.4) | |
| ASDAS-MI† | Baseline | – | – | – | – | – | – | – | – |
| Week 12 | 0 | 0 | 7 (22.6) | 4 (14.8) | 13 (38.2) | 8 (32.0) | 15 (25.9) | 19 (31.1) | |
| Week 48 | 8 (33.3) | 11 (30.6) | 11 (35.5) | 9 (33.3) | 20 (58.8) | 10 (40.0) | 24 (41.4) | 34 (55.7) | |
| ASDAS-ID† | Baseline | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Week 12 | 0 | 0 | 1 (3.2) | 1 (3.7) | 3 (8.8) | 3 (12.0) | 6 (10.3) | 6 (9.8) | |
| Week 48 | 4 (16.7) | 5 (13.9) | 3 (9.7) | 6 (22.2) | 6 (17.6) | 4 (16.0) | 15 (25.9) | 15 (24.6) | |
| ASDAS-LDA† | Baseline | 0 | 0 | 0 | 0 | 0 | 0 | 1.7 | 0 |
| Week 12 | 3 (12.5) | 5 (13.9) | 6 (19.4) | 3 (11.1) | 10 (29.4) | 9 (36.0) | 16 (27.6) | 20 (32.8) | |
| Week 48 | 9 (37.5) | 16 (44.4) | 10 (32.3) | 7 (25.9) | 13 (38.2) | 8 (32.0) | 17 (29.3) | 23 (37.7) | |
| Mean (SD) | |||||||||
| ASDAS† | Baseline | 3.71 (0.83) | 3.88 (0.93) | 3.96 (0.72) | 3.84 (0.65) | 4.12 (0.80) | 4.18 (0.74) | 3.86 (0.76) | 3.94 (0.74) |
| Change from baseline | Week 12 | −0.31 (0.73) | −0.37 (0.62) | −1.11 (1.07) | −0.85 (1.01) | −1.72 (0.99) | −1.64 (1.21) | −1.40 (0.94) | −1.52 (0.94) |
| Week 48 | −1.70 (0.89) | −1.80 (0.89) | −1.63 (1.05) | −1.61 (0.93) | −2.01 (1.12) | −2.04 (0.95) | −1.78 (0.95) | −2.03 (0.92) | |
| BASDAI 50* | Baseline | – | – | – | – | – | – | – | – |
| Week 12 | 3 (12.5) | 4 (11.1) | 9 (29.0) | 5 (18.5) | 14 (41.2) | 12 (48.0) | 22 (37.9) | 29 (47.5) | |
| Week 48 | 11 (45.8) | 20 (55.6) | 12 (38.7) | 10 (37.0) | 20 (58.8) | 14 (56.0) | 30 (51.7) | 35 (57.4) | |
| Geometric mean (median) | Baseline | 6.2 (6.1) | 9.3 (10.9) | 11.4 (10.7) | 8.1 (9.9) | 14.2 (16.7) | 14.7 (17.6) | 12.0 (16.0) | 10.4 (11.3) |
| hs-CRP† | Week 12 | 9.1 (9.4) | 8.0 (9.4) | 5.6 (5.5) | 3.8 (4.3) | 2.9 (3.0) | 5.3 (6.1) | 3.7 (4.3) | 3.8 (3.5) |
| Week 48 | 2.9 (2.2) | 2.9 (3.0) | 4.0 (5.0) | 3.0 (3.8) | 3.4 (3.5) | 4.1 (3.9) | 3.9 (4.7) | 3.0 (3.6) | |
| BASFI† | Baseline | 5.8 (1.8) | 5.5 (2.2) | 5.8 (1.7) | 5.9 (1.9) | 5.6 (1.8) | 6.2 (1.8) | 5.5 (2.2) | 5.9 (2.0) |
| Change from baseline | Week 12 | −1.0 (2.1) | −0.3 (1.7) | −1.7 (2.0) | −1.1 (2.5) | −1.6 (2.5) | −2.1 (2.3) | −1.7 (1.8) | −2.2 (2.0) |
| Week 48 | −2.9 (2.2) | −2.4 (2.2) | −2.3 (1.5) | −2.5 (2.0) | −2.8 (2.4) | −2.9 (2.4) | −2.5 (2.0) | −2.9 (2.2) | |
| Spinal pain† | Baseline | 6.9 (1.4) | 7.0 (1.9) | 6.8 (2.1) | 7.7 (1.4) | 7.4 (1.5) | 7.4 (1.8) | 6.6 (2.0) | 7.3 (1.5) |
| Change from baseline | Week 12 | −1.5 (1.6) | −0.7 (1.7) | −2.2 (2.4) | −2.2 (2.4) | −3.3 (2.2) | −3.2 (2.7) | −2.6 (2.2) | −3.6 (2.4) |
| Week 48 | −3.7 (2.0) | −3.7 (2.6) | −3.0 (2.9) | −3.8 (2.7) | −4.2 (2.4) | −4.1 (2.2) | −3.8 (2.4) | −4.7 (2.1) | |
| Morning stiffness† | Baseline | 6.9 (1.7) | 6.7 (2.0) | 6.7 (2.0) | 6.4 (1.9) | 6.5 (2.2) | 7.2 (1.7) | 6.5 (1.8) | 6.6 (2.1) |
| Change from baseline | Week 12 | −1.5 (1.7) | −1.1 (1.5) | −2.6 (3.0) | −1.7 (2.8) | −2.9 (2.9) | −3.5 (2.5) | −2.8 (2.0) | −3.4 (2.7) |
| Week 48 | −3.9 (2.2) | −3.6 (2.4) | −3.7 (3.0) | −3.2 (2.3) | −3.9 (2.8) | −4.4 (2.0) | −3.9 (2.2) | −4.4 (2.4) | |
| BASMI† | Baseline | 4.3 (1.6) | 4.5 (1.6) | 4.7 (1.7) | 4.9 (1.8) | 4.5 (1.8) | 4.9 (1.5) | 4.6 (1.8) | 4.8 (1.8) |
| Change from baseline | Week 12 | −0.3 (0.6) | −0.1 (0.8) | −0.5 (1.0) | −0.4 (0.6) | −0.5 (0.8) | −0.4 (0.7) | −0.3 (0.7) | −0.7 (0.7) |
| Week 48 | −0.9 (1.0) | −0.7 (1.0) | −0.7 (1.1) | −0.9 (0.7) | −0.6 (0.7) | −0.9 (0.7) | −0.5 (1.0) | −1.0 (0.9) | |
| Fatigue† | Baseline | 6.4 (1.7) | 6.8 (1.6) | 7.1 (1.6) | 7.1 (1.6) | 6.8 (1.2) | 6.7 (1.5) | 6.4 (1.7) | 6.4 (1.9) |
| Change from baseline | Week 12 | −0.7 (2.5) | −1.0 (1.7) | −1.6 (2.2) | −1.6 (2.3) | −2.4 (2.1) | −2.6 (2.4) | −2.1 (2.2) | −2.1 (2.5) |
| Week 48 | −2.7 (2.2) | −2.8 (2.4) | −2.7 (2.0) | −3.2 (2.7) | −3.5 (2.3) | −3.1 (2.0) | −3.1 (2.1) | −3.3 (2.4) | |
| PGADA† | Baseline | 7.0 (1.5) | 6.9 (1.9) | 7.0 (1.7) | 7.4 (1.3) | 7.4 (1.5) | 7.1 (1.8) | 6.5 (1.8) | 7.1 (1.9) |
| Change from baseline | Week 12 | −1.5 (1.8) | −0.7 (1.6) | −1.9 (2.9) | −2.0 (2.4) | −3.3 (2.3) | −3.2 (2.7) | −2.2 (2.6) | −3.2 (2.2) |
| Week 48 | −3.8 (2.3) | −3.5 (2.7) | −3.3 (3.1) | −3.4 (2.6) | −4.0 (2.4) | −4.0 (2.4) | −3.5 (2.3) | −4.5 (2.3) | |
| MASES‡ | Placebo → | BKZ 16 mg → | BKZ 64 mg → | BKZ 160 mg (n=40) | BKZ 320 mg (n=42) | ||||
| BKZ 160 mg(n=17) | BKZ 320 mg(n=23) | BKZ 160 mg(n=21) | BKZ 320 mg(n=18) | BKZ 160 mg(n=22) | BKZ 320 mg(n=11) | ||||
| Change from baseline | Baseline | 4.1 (3.0) | 5.0 (3.5) | 3.5 (2.4) | 5.9 (3.4) | 4.6 (3.4) | 3.9 (2.5) | 3.8 (2.2) | 4.6 (3.2) |
| Week 12 | −2.5 (2.1) | −2.1 (3.7) | −1.2 (4.1) | −2.0 (3.1) | −2.4 (1.9) | −3.6 (2.2) | −2.5 (2.3) | −2.7 (2.4) | |
| Week 48 | −3.8 (3.1) | −4.4 (3.6) | −2.5 (3.0) | −4.6 (2.8) | −3.1 (2,7) | −3.2 (2.6) | −3.3 (2.2) | −3.4 (3.2) | |
*NRI.
†MI.
‡In patients with enthesitis at baseline.
ASAS, Assessment of SpondyloArthritis international Society; ASAS-PR, ASAS partial remission; ASDAS, Ankylosing Spondylitis Disease Activity Score; ASDAS-ID, ASDAS inactive disease; ASDAS-LDA, ASDAS low disease activity; ASDAS-MI, ASDAS major improvement; BASDAI 50, Bath Ankylosing Spondylitis Disease Activity Index ≥50% improvement; BASFI, Bath Ankylosing Spondylitis Functional Index; BASMI, Bath Ankylosing Spondylitis Metrology Index; BKZ, bimekizumab; DBS, dose-blind set; hs-CRP, high-sensitivity C reactive protein; MASES, Maastricht Ankylosing Spondylitis Enthesitis Score; MI, multiple imputation; NRI, non-responder imputation; NRS, numerical rating scale; PGADA, patient global assessment of disease activity.
Rapid reductions from baseline in hs-CRP were observed with bimekizumab treatment compared with placebo (table 3). In the 31 patients with MRI follow-up, reductions from baseline in Spondyloarthritis Research Consortium of Canada Sacroiliac (SPARCC SI) joint score were observed at week 12 in all bimekizumab treatment groups, and in spine Berlin score were observed in the three highest bimekizumab dose groups at week 12 (online supplementary figure 4).
Improvements in patient global assessment of disease activity (PGADA), spinal pain, morning stiffness and BASFI were observed compared with baseline scores, and greater reductions from baseline in BASMI were seen in all bimekizumab-treated patients compared with placebo at week 12 (table 3). From post hoc analyses, reductions from baseline to week 12 in fatigue were observed in all patients, with the greatest reductions in the bimekizumab 160 and 320 mg groups (table 3). Change from baseline to week 12 in MOS Sleep Disturbance and Sleep Problems Index II were greater with bimekizumab in all dose groups versus placebo (table 4). Improvements in patient QoL were observed in all bimekizumab dose groups compared with placebo (table 4). Consistent with this, patient perception of physical health improved, with increases in SF-36 physical component summary (PCS) scores observed in all bimekizumab dose groups and higher scores with bimekizumab compared with placebo (table 4). SF-36 mental component summary (MCS) scores were similar to baseline, with all patients within the normal range.
Table 4.
Patient-reported outcomes (week 12 (FAS) and week 48 (DBS); MI)
| Mean (SD) | Placebo → | BKZ 16 mg → | BKZ 64 mg → | BKZ 160 mg (n=58) |
BKZ 320 mg (n=61) |
||||
| BKZ 160 mg (n=24) |
BKZ 320 mg (n=36) |
BKZ 160 mg (n=31) |
BKZ 320 mg (n=27) |
BKZ 160 mg (n=34) |
BKZ 320 mg (n=25) |
||||
| MOS Sleep Disturbance | Baseline | 45.3 (8.3) | 46.2 (6.8) | 48.4 (8.3) | 44.6 (10.0) | 47.6 (9.6) | 47.8 (7.5) | 47.3 (8.1) | 48.0 (8.9) |
| Change from baseline | Week 12 | 2.3 (8.4) | 1.8 (6.0) | 1.9 (8.4) | 4.7 (8.7) | 5.8 (7.9) | 4.7 (5.6) | 5.8 (6.2) | 6.6 (7.5) |
| Week 48 | 7.3 (7.8) | 6.9 (7.0) | 3.8 (7.9) | 8.8 (8.1) | 7.6 (8.9) | 6.7 (7.4) | 6.6 (6.3) | 6.7 (7.7) | |
| MOS Sleep Problems Index II | Baseline | 45.5 (8.1) | 45.3 (7.9) | 48.2 (8.7) | 42.4 (10.1) | 47.6 (9.4) | 47.5 (7.1) | 46.9 (7.5) | 47.2 (9.4) |
| Change from baseline | Week 12 | 2.1 (8.3) | 1.8 (6.8) | 2.2 (9.4) | 5.9 (9.3) | 5.9 (8.1) | 4.9 (6.1) | 5.6 (6.7) | 6.8 (7.5) |
| Week 48 | 7.6 (8.7) | 8.0 (9.1) | 4.1 (7.5) | 10.0 (9.0) | 8.1 (8.6) | 8.0 (7.2) | 6.5 (6.1) | 8.0 (7.92) | |
| ASQoL | Baseline | 8.4 (4.7) | 9.2 (4.7) | 8.4 (4.4) | 9.2 (4.1) | 7.9 (4.2) | 9.6 (4.0) | 8.4 (4.3) | 8.7 (4.3) |
| Change from baseline | Week 12 | −1.3 (5.5) | −1.3 (3.7) | −2.8 (5.2) | −1.9 (5.4) | −3.5 (3.6) | −5.0 (4.2) | −3.5 (4.3) | −4.6 (4.8) |
| Week 48 | −4.2 (5.6) | −5.3 (5.6) | −3.9 (4.6) | −5.0 (4.7) | −5.0 (4.1) | −6.3 (4.4) | −4.9 (4.1) | −5.4 (4.8) | |
| SF-36 PCS | Baseline | 32.8 (6.9) | 33.0 (8.4) | 32.5 (8.7) | 30.9 (6.5) | 31.9 (7.8) | 30.3 (5.6) | 33.0 (8.2) | 32.4 (7.7) |
| Change from baseline | Week 12 | 5.8 (6.9) | 2.0 (6.2) | 7.8 (7.4) | 7.4 (9.3) | 8.9 (8.8) | 9.5 (8.4) | 8.5 (7.6) | 8.2 (7.2) |
| Week 48 | 12.8 (9.4) | 10.9 (8.1) | 10.1 (7.4) | 12.6 (9.2) | 12.9 (10.2) | 13.4 (7.8) | 12.0 (9.1) | 12.0 (8.5) | |
| SF-36 MCS | Baseline | 54.0 (9.1) | 53.6 (8.7) | 54.6 (9.5) | 52.0 (7.8) | 55.8 (7.4) | 54.4 (7.2) | 53.8 (8.1) | 54.4 (8.5) |
| Change from baseline | Week 12 | −0.4 (8.5) | 0.3 (7.2) | −0.1 (7.9) | 3.8 (8.2) | 1.7 (6.9) | 4.0 (8.1) | 1.0 (7.4) | 3.4 (6.9) |
| Week 48 | 1.3 (10.2) | 1.5 (7.8) | 1.8 (7.8) | 6.2 (8.4) | 2.2 (6.6) | 4.0 (7.0) | 1.72 (8.2) | 3.0 (7.7) | |
ASQoL, Ankylosing Spondylitis Quality of Life; BKZ, bimekizumab; DBS, dose-blind set; FAS, full analysis set; SF-36 MCS, SF-36 mental component summary; MI, multiple imputation; MOS, Medical Outcomes Study; SF-36 PCS, SF-36 physical component summary; SF-36, 36-Item Short Form Questionnaire.
Dose-blind period (weeks 12–48)
The ASAS40 response rates with bimekizumab treatment continued to increase after the first 12 weeks and were maintained to week 48 in patients continuing on the same bimekizumab dose (160 mg: 58.6%, 320 mg: 62.3%; table 3 and figure 1B). Of patients initially randomised to placebo, ≥50% achieved ASAS40 response at week 48 following re-randomisation to bimekizumab 160 or 320 mg (54.2% and 50.0%, respectively). ASAS20, ASAS5/6, ASDAS-MI, ASDAS-ID and ASAS-PR responses continued to increase from week 12 to week 48 (table 3). ASDAS levels continued to decrease after week 12 and were maintained to week 48 (figure 1C). In patients with baseline enthesitis, further reductions from baseline in MASES index were observed, with similar reductions seen across all bimekizumab dose groups (table 3). In post hoc analyses, BASDAI 50 response rates increased to week 48, with patients re-randomised from placebo to bimekizumab 160 or 320 mg achieving similar responses to patients receiving 160 and 320 mg throughout the study (table 3).
Following rapid reductions from baseline to week 12, hs-CRP levels were maintained in the bimekizumab 160 and 320 mg groups; in re-randomised patients, hs-CRP levels were similar to those who remained on the same bimekizumab dose throughout the study (table 3). SPARCC SI scores were low but marked reductions from baseline were observed at week 48, with the greatest reductions observed in the group re-randomised from placebo to bimekizumab 160 and 320 mg. MRI data were only available for two patients receiving bimekizumab 160 mg throughout the study and their baseline SPARCC SI scores were low; therefore, reductions in SPARCC SI were not observed in this dose group. Reductions from baseline in spine Berlin score at week 48 were also observed in bimekizumab-treated patients (online supplementary figure 4).
Improvements in PROs continued to week 48, with reductions from baseline in PGADA, spinal pain, morning stiffness, and BASFI observed in all treatment groups (table 3). Continued improvements in mobility were observed, with bimekizumab-treated patients experiencing reductions from baseline in BASMI (table 3). At week 48, similar reductions from baseline in fatigue were observed across bimekizumab dose groups (table 3). Improvements in Sleep Disturbance and Sleep Problems Index II seen at week 12 were maintained to week 48 in bimekizumab-treated patients (table 4). Patients who initially received placebo and were re-randomised to bimekizumab reported similar reductions in ASQoL during the dose-blind period as those receiving bimekizumab 160 and 320 mg from the start of the study (table 4). After initial improvements in SF-36 PCS scores over the first 12 weeks, scores were maintained in bimekizumab-treated patients; scores in SF-36 MCS remained similar to the double-blind period (table 4).
Safety
During the double-blind period, treatment-emergent AEs (TEAEs) were reported by 37.9% (92/243) of bimekizumab-treated patients compared with 43.3% (26/60) of patients receiving placebo. Overall, up to week 48, 77.6% (235/303) of patients reported TEAEs while receiving bimekizumab (table 5); the majority were mild or moderate in severity. The most frequently reported TEAE (≥10% of patients in any treatment group) in bimekizumab-treated patients was nasopharyngitis (11.2%, 34/303; table 5). There was no apparent dose relationship with type or frequency of TEAEs.
Table 5.
Summary of safety results (SS)
| Double-blind period | Overall treatment period | |||||||
| Placebo Q4W (n=60) n* (%) (#) |
BKZ 16 mg Q4W (n=61) n* (%) (#) |
BKZ 64 mg Q4W (n=58) n* (%) (#) |
BKZ 160 mg Q4W (n=63) n* (%) (#) |
BKZ 320 mg Q4W (n=61) n* (%) (#) |
BKZ 160 mg Q4W (n=149) n (EAIR) |
BKZ 320 mg Q4W (n=150) n (EAIR) |
All BKZ† (n=303) n (EAIR) |
|
| Any TEAE | 26 (43.3) (41) | 26 (42.6) (50) | 17 (29.3) (33) | 20 (31.7) (33) | 29 (47.5) (61) | 103 (168.7) | 122 (221.1) | 235 (186.2) |
| Nasopharyngitis | 0 | 2 (3.3) (2) | 1 (1.7) (1) | 3 (4.8) (3) | 0 | 13 (12.0) | 19 (16.6) | 34 (13.7) |
| Pharyngitis | 0 | 0 | 0 | 2 (3.2) (2) | 1 (1.6) (1) | 11 (10.0) | 7 (6.1) | 18 (7.1) |
| Bronchitis | 1 (1.7) (1) | 0 | 2 (3.4) (2) | 0 | 0 | 4 (3.6) | 12 (10.4) | 18 (7.1) |
| Upper respiratory tract infection | 1 (1.7) (1) | 0 | 1 (1.7) (1) | 0 | 1 (1.6) (1) | 5 (4.5) | 11 (9.5) | 17 (6.7) |
| Oral candidiasis | 0 | 0 | 0 | 0 | 3 (4.9) (3) | 8 (7.2) | 8 (7.0) | 16 (6.3) |
| Serious TEAEs | 2 (3.3) (2) | 0 | 2 (3.4) (5) | 1 (1.6) (2) | 0 | 5 (4.4) | 6 (5.1) | 13 (5.1) |
| Permanent withdrawal of study medication due to TEAEs | 1 (1.7) (1) | 2 (3.3) (2) | 1 (1.7) (1) | 1 (1.6) (2) | 2 (3.3) (2) | 7 (6.2) | 10 (8.7) | 20 (7.9) |
| Drug-related TEAEs | 6 (10.0) (8) | 9 (14.8) (12) | 6 (10.3) (10) | 7 (11.1) (8) | 12 (19.7) (17) | 48 (52.0) | 54 (58.7) | 110 (54.0) |
| Death | 0 | 0 | 0 | 1 (1.6) (1) | 0 | 1 (0.9) | 0 | 1 (0.4) |
| TEAEs of special interest | 5 (8.3) (5) | 9 (14.8) (10) | 6 (10.3) (9) | 3 (4.8) (3) | 5 (8.2) (7) | |||
| Opportunistic infection | 0 | 1 (1.6) (1) | 0 | 0 | 0 | 0 | 0 | 1 (0.38) |
| Candida infections | 0 | 0 | 0 | 0 | 3 (4.9) (3) | 10 (9.1) | 9 (7.9) | 19 (7.5) |
| Neutropenia | 0 | 0 | 0 | 0 | 0 | 1 (0.9) | 0 | 1 (0.4) |
| Severe hypersensitivity reactions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Suicide ideation | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Psychiatric disorder | 2 (3.3) (2) | 1 (1.6) (1) | 0 | 0 | 0 | 0 | 0 | 1 (0.3) |
| Major cardiovascular events | 0 | 0 | 0 | 1 (1.6) (1) | 0 | 2 (1.8) | 0 | 2 (0.8) |
| Hepatic events | 2 (3.3) (2) | 6 (9.8) (6) | 4 (6.9) (7) | 1 (1.6) (1) | 1 (1.6) (2) | 13 (12.1) | 12 (10.4) | 33 (13.6) |
| ALT increased | 0 | 1 (1.6) (1) | 1 (1.7) (1) | 0 | 1 (1.6) (1) | 5 (4.5) | 6 (5.1) | 13 (5.1) |
| AST increased | 0 | 0 | 1 (1.7) (1) | 0 | 1 (1.6) (1) | 3 (2.7) | 5 (4.3) | 9 (3.5) |
| GGT increased | 1 (1.7) (1) | 2 (3.3) (2) | 2 (3.4) (3) | 0 | 0 | 6 (5.4) | 4 (3.4) | 13 (5.1) |
| Hepatic enzyme increased | 1 (1.7) (1) | 2 (3.3) (2) | 1 (1.7) (1) | 0 | 0 | 0 | 3 (2.5) | 6 (2.3) |
| Malignancies | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Inflammatory bowel disease | 0 | 1 (1.6) (1) | 0 | 0 | 0 | 1 (0.9) | 2 (1.7) | 4 (1.5) |
In addition, one patient received doses of 160 and 320 mg in error and was therefore included in both the 160 and 320 mg groups, but only once in the all-BKZ group; (#) the number of individual occurrences of the AE.
*Number of patients reporting at least one TEAE.
†The all-BKZ group included 5 patients who received BKZ in the double-blind period but did not receive BKZ 160 or 320 mg: 2 patients in the 16 mg group and 2 patients in the 64 mg group discontinued before re-randomisation; 1 patient in the 16 mg group did not start the dose-blind period.
ALT, alanine aminotransferase; AST, aspartate aminotransferase; BKZ, bimekizumab; EAIR, exposure-adjusted incidence rate per 100 patient-years; GGT, gamma-glutamyltransferase; Q4W, every 4 weeks; SS, safety set; TEAE, treatment-emergent adverse event.
During the double-blind period, SAEs were reported by 1.2% (3/243) of bimekizumab-treated patients and 3.3% (2/60) of those receiving placebo. Thirteen of 303 (4.3%) patients receiving bimekizumab experienced SAEs during the 48-week study duration (see online supplementary file). TEAEs leading to discontinuation were reported by 2.5% (6/243) of bimekizumab-treated patients vs 1.7% (1/60) of patients receiving placebo in the double-blind period. Overall, 6.6% (20/303) of patients discontinued due to TEAEs.
Oral candidiasis was reported by 3 (4.9%) patients in the bimekizumab 320 mg group during the double-blind period (table 5) and 16/303 (5.3%) of bimekizumab-treated patients in total. All cases were mild to moderate, resolved with systemic or topical antifungal treatment and no events led to patients withdrawing from the study.
Four cases of IBD were reported (further details in online supplementary file). Two cases were new diagnoses of Crohn’s disease and were mild to moderate in intensity. One case (bimekizumab 320 mg group) occurred during the dose-blind period, was identified as related to treatment and resolved, the other (bimekizumab 160 mg group) was considered unrelated to treatment, with diagnosis confirmed after the patient had withdrawn from the study. Two cases were UC, one with a history of UC and one new diagnosis; both were considered mild and unrelated to treatment. The new diagnosis of UC occurred during the double-blind period (bimekizumab 16 mg, week 4). The other case was an exacerbation of UC during the dose-blind period in a patient with a history of UC who was receiving concomitant mesalazine (bimekizumab 320 mg, week 24). Overall, the exposure adjusted incidence rate (EAIR) per 100 patient-years for Crohn’s disease and UC was 0.77 each.
There were four cases of acute anterior uveitis during the study; two of these occurred in patients receiving bimekizumab, one during treatment and one after discontinuation (see online supplementary file). Overall, 15.2% of patients in the study reported a history of uveitis or iridocyclitis at baseline (patients with a recent history of uveitis were not excluded); the incidence rate of uveitis in patients receiving bimekizumab was 0.53 (EAIR 0.77).
Two cases adjudicated as MACE were reported: one SAE (described in the online supplementary file), and one myocardial infarction (bimekizumab 160 mg), which resolved, was considered unrelated to treatment and did not lead to treatment discontinuation.
No malignancies, severe hypersensitivity reactions or suicidal ideation were reported during the 48-week study (table 5).
No clinically meaningful changes from baseline in vital sign measurements (systolic and diastolic blood pressure, and pulse rate), or ECG results were observed in any treatment group during the overall study.
Discussion
This was the first phase IIb study of bimekizumab in patients with active AS. Bimekizumab-treated patients had rapid and significant ASAS40 responses versus placebo at week 12 and these were supported by all secondary efficacy end points, as well as additional QoL and patient-reported measures of function and disease activity. All outcomes further improved from week 12 and were sustained to week 48. This study offers insights into the potential efficacy of bimekizumab for the treatment of patients with AS and provides further support for the encouraging findings from clinical and preclinical studies of bimekizumab,15 21 31 that dual neutralisation of IL-17A and IL-17F may be effective in the treatment of IL-17-mediated inflammatory diseases.
TNF and IL-17A inhibitors are currently recommended for the management of patients with AS7 9; the novel biological DMARD bimekizumab may provide an alternative therapeutic approach. A significant dose response was observed in ASAS40 at week 12 with increasing bimekizumab dose from 16 to 320 mg; responses were generally similar for the three highest doses and the greatest response was in the 160 mg group. The parallel study of bimekizumab in PsA also demonstrated the greatest ACR50 response in the 160 mg dose group.31 In patients with moderate-to-severe plaque psoriasis,21 the greatest responses were observed with bimekizumab 320 mg; this differing dose response may be due to differences between patient populations and efficacy in axial or joint disease compared with skin manifestations. Here, for all measures of disease activity, response rates increased and were sustained from week 12 through week 48 in patients continuing on bimekizumab 160 and 320 mg. Notably, patients re-randomised at week 12 responded rapidly and achieved similar response rates from week 24 to week 48 to patients receiving bimekizumab 160 or 320 mg continuously throughout the study. Although there was a rapid onset of response for the primary and secondary efficacy end points, more stringent outcomes, such as ASDAS-ID, required observation over a longer time period; by week 48, one-quarter of this patient population with highly active disease achieved inactive disease in both the bimekizumab 160 and 320 mg groups.
Levels of inflammation, as measured by hs-CRP, decreased rapidly with bimekizumab treatment, with low levels of inflammation maintained to week 48 in all bimekizumab-treated patients. SPARCC SI and spine Berlin scores generally improved from week 12 through week 48 across bimekizumab groups; however, results should be interpreted with caution due to the small number of patients per treatment group (range, 2–12) who had MRI assessments.
AS has a substantial impact on patients’ QoL in many key areas such as completion of daily activities, fatigue and sleep, with pain acknowledged as one of the most burdensome symptoms.32 Bimekizumab rapidly improved patient-reported spinal pain and improvements continued over the duration of the study. Changes from baseline to week 12 in sleep disturbance and sleep problems suggested that bimekizumab treatment improved sleep outcomes for patients, which were maintained to week 48. In addition, reductions in fatigue from baseline to week 12 and week 48 indicated sustained improvements for patients in another key symptom of their disease. Changes from baseline in SF-36 PCS domain indicated positive improvements in the physical aspects of patients’ disease.
Overall, bimekizumab was generally well tolerated across the treatment groups. The safety profile in patients with active AS was as expected given previous studies of bimekizumab in patients with psoriasis or PsA.15 21 Consistent with the mechanism of action of therapies targeting the IL-17 pathway, 16 cases (5%) of oral candidiasis were reported in bimekizumab-treated patients across the 48 weeks of treatment.11 33 However, all cases were mild or moderate and did not lead to discontinuation. Four cases of IBD were reported, including one in a patient with a history of UC; incidence of IBD is a known side effect of IL-17A inhibition but is also a recognised manifestation of axSpA. The incidence of IBD reported in this study of bimekizumab is comparable to that seen with TNF inhibitors,34 secukinumab35 and ixekizumab in AS.36 To date, IBD has not been reported with bimekizumab in studies involving patients with psoriasis or PsA.21 31
The ASAS40 responses and secondary outcomes observed with bimekizumab in this phase IIb study compare favourably with those observed with ixekizumab10 and secukinumab11 in recent phase III studies in AS, involving similar numbers of patients. The 48-week duration of this study, providing long-term efficacy data for bimekizumab ahead of completion of the phase III studies and demonstrating maintenance of responses over time, represents a strength of the study design. Study limitations include the relatively short placebo control period of 12 weeks, small patient numbers per treatment group due to the nature of the study design, a high number of Caucasian patients and MRI data being available for only a subset of patients.
In summary, bimekizumab may provide a promising therapeutic option for patients with AS. Bimekizumab treatment resulted in rapid and sustained improvements across multiple outcomes of disease activity, QoL and function. These results support phase III evaluation of bimekizumab in axSpA (BE MOBILE 1, NCT03928704; BE MOBILE 2, NCT03928743) to determine the clinical benefits that may be associated with neutralising IL-17F in addition to IL-17A.
Acknowledgments
The authors would like to acknowledge Alexandra Webster, MSc, of iMed Comms, an Ashfield Company, part of UDG Healthcare, for medical writing support that was funded by UCB Pharma in accordance with Good Publications Practice (GPP3) guidelines (http://www.ismpp.org/gpp3). The authors would also like to thank Simone E Auteri, MSc PhD EMS, of UCB Pharma for publication coordination and critical review, Natasha de Peyrecave, DPhil, of UCB Pharma for critical review, and Rajan Bajracharya, MBBS MPH MFPM, of UCB Pharma for review of the safety reporting in the manuscript.
Footnotes
Handling editor: Josef S Smolen
Contributors: All authors were involved in designing the study, analysing and interpreting the study data, and critically reviewing the manuscript. All authors approved the final version for submission.
Funding: The study (NCT02963506) was funded by UCB Pharma.
Competing interests: DvdH reports personal fees from AbbVie, Amgen, Astellas, AstraZeneca, BMS, Boehringer Ingelheim, Celgene, Cyxone, Daiichi, Eisai, Eli Lilly, Galapagos, Gilead, GlaxoSmithKline, Janssen, Merck, Novartis, Pfizer, Regeneron, Roche, Sanofi, Takeda and UCB Pharma, and is Director of Imaging Rheumatology BV. LSG reports grants and personal fees from AbbVie, Amgen, Novartis, Pfizer and UCB Pharma, and personal fees from Galapagos, Janssen and Eli Lilly. AD reports personal fees from Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Galapagos and Janssen, and grants and personal fees from AbbVie, Eli Lilly, GlaxoSmithKline, Novartis, Pfizer and UCB. DP reports personal fees from UCB Pharma, BMS, Roche and Celgene, and grants and personal fees from AbbVie, Eli Lilly, MSD, Novartis and Pfizer. XB reports personal fees from AbbVie, Bristol-Myers Squibb, Celgene, Chugai, Janssen, MSD, Novartis, Pfizer and UCB Pharma, and grant/research support from Abbvie, MSD and Novartis. AK reports research support from Altoona Centernical Research, PC, during the conduct of the study; Advisory Committee or Review Panel for AbbVie, Janssen, UCB Pharma and Boehringer Ingelheim; speaking and teaching for Celgene, Horizon, Merck and Novartis; Advisory Committee or Review Panel, speaking and training for Genzyme; Advisory Committee or Review Panel, speaking/training; consultant, and stocks for Pfizer and Sanofi; Advisory Committee or Review Panel, speaking/training and consultant for Regeneron; consultant for SUN Pharma Advanced Research; Speaker and Steering Committee for Flexion; Stocks from Amgen, Gilead and GSK and Speaker for AbbVie. MO, DB and NG are employees of UCB Pharma and own stocks and stock options. JC is an employee of UCB Pharma. MKF was an employee of UCB Pharma at the time the study was conducted (current employee of Kezar Life Sciences). MD reports grants and personal fees from UCB, Eli Lilly, Novartis, Pfizer, AbbVie and Merck.
Patient and public involvement: Patients and/or the public were involved in the design, conduct, reporting or dissemination plans of this research. Refer to the 'Methods' section for further details.
Patient consent for publication: Not required.
Ethics approval: The study was conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonisation Guidance for Good Clinical Practice. Independent institutional review board approvals were obtained, and all patients provided written informed consent in accordance with local requirements.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Underlying data from this manuscript may be requested by qualified researchers six months after product approval in the US and/or Europe, or global development is discontinued, and 18 months after trial completion. Investigators may request access to anonymized IPD and redacted study documents which may include: raw datasets, analysis-ready datasets, study protocol, blank case report form, annotated case report form, statistical analysis plan, dataset specifications, and clinical study report. Prior to use of the data, proposals need to be approved by an independent review panel at www.Vivli.org and a signed data sharing agreement will need to be executed. All documents are available in English only, for a pre-specified time, typically 12 months, on a password protected portal.
References
- 1. Sieper J, Poddubnyy D. Axial spondyloarthritis. Lancet 2017;390:73–84. 10.1016/S0140-6736(16)31591-4 [DOI] [PubMed] [Google Scholar]
- 2. de Winter JJ, van Mens LJ, van der Heijde D, et al. . Prevalence of peripheral and extra-articular disease in ankylosing spondylitis versus non-radiographic axial spondyloarthritis: a meta-analysis. Arthritis Res Ther 2016;18:196 10.1186/s13075-016-1093-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Halvorsen S, Vøllestad NK, Fongen C, et al. . Physical fitness in patients with ankylosing spondylitis: comparison with population controls. Phys Ther 2012;92:298–309. 10.2522/ptj.20110137 [DOI] [PubMed] [Google Scholar]
- 4. Landewé R, Dougados M, Mielants H, et al. . Physical function in ankylosing spondylitis is independently determined by both disease activity and radiographic damage of the spine. Ann Rheum Dis 2009;68:863–7. 10.1136/ard.2008.091793 [DOI] [PubMed] [Google Scholar]
- 5. Li Y, Zhang S, Zhu J, et al. . Sleep disturbances are associated with increased pain, disease activity, depression, and anxiety in ankylosing spondylitis: a case-control study. Arthritis Res Ther 2012;14:R215 10.1186/ar4054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Machado P, Landewé R, Braun J, et al. . A stratified model for health outcomes in ankylosing spondylitis. Ann Rheum Dis 2011;70:1758–64. 10.1136/ard.2011.150037 [DOI] [PubMed] [Google Scholar]
- 7. van der Heijde D, Ramiro S, Landewé R, et al. . 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 2017;76:978–91. 10.1136/annrheumdis-2016-210770 [DOI] [PubMed] [Google Scholar]
- 8. Sepriano A, Regel A, van der Heijde D, et al. . Efficacy and safety of biological and targeted-synthetic DMARDs: a systematic literature review Informing the 2016 update of the ASAS/EULAR recommendations for the management of axial spondyloarthritis. RMD Open 2017;3:e000396 10.1136/rmdopen-2016-000396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ward MM, Deodhar A, Gensler LS, et al. . 2019 update of the American College of Rheumatology/Spondylitis association of America/Spondyloarthritis research and treatment network recommendations for the treatment of ankylosing spondylitis and Nonradiographic axial spondyloarthritis. Arthritis Care Res 2019;71:1285–99. 10.1002/acr.24025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van der Heijde D, Cheng-Chung Wei J, Dougados M, et al. . Ixekizumab, an interleukin-17A antagonist in the treatment of ankylosing spondylitis or radiographic axial spondyloarthritis in patients previously untreated with biological disease-modifying anti-rheumatic drugs (COAST-V): 16 week results of a phase 3 randomised, double-blind, active-controlled and placebo-controlled trial. Lancet 2018;392:2441–51. 10.1016/S0140-6736(18)31946-9 [DOI] [PubMed] [Google Scholar]
- 11. Baeten D, Sieper J, Braun J, et al. . Secukinumab, an interleukin-17A inhibitor, in ankylosing spondylitis. N Engl J Med 2015;373:2534–48. 10.1056/NEJMoa1505066 [DOI] [PubMed] [Google Scholar]
- 12. Rezaiemanesh A, Abdolmaleki M, Abdolmohammadi K, et al. . Immune cells involved in the pathogenesis of ankylosing spondylitis. Biomed Pharmacother 2018;100:198–204. 10.1016/j.biopha.2018.01.108 [DOI] [PubMed] [Google Scholar]
- 13. Hymowitz SG, Filvaroff EH, Yin JP, et al. . IL-17s adopt a cystine knot fold: structure and activity of a novel cytokine, IL-17F, and implications for receptor binding. EMBO J 2001;20:5332–41. 10.1093/emboj/20.19.5332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yang XO, Chang SH, Park H, et al. . Regulation of inflammatory responses by IL-17F. J Exp Med 2008;205:1063–75. 10.1084/jem.20071978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Glatt S, Baeten D, Baker T, et al. . Dual IL-17A and IL-17F neutralisation by bimekizumab in psoriatic arthritis: evidence from preclinical experiments and a randomised placebo-controlled clinical trial that IL-17F contributes to human chronic tissue inflammation. Ann Rheum Dis 2018;77:523–32. 10.1136/annrheumdis-2017-212127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ammari M, Presumey J, Ponsolles C, et al. . Delivery of miR-146a to Ly6C(high) monocytes inhibits pathogenic bone erosion in inflammatory arthritis. Theranostics 2018;8:5972–85. 10.7150/thno.29313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shah M, Maroof A, Al-Hosni RN, et al. . Bimekizumab blocks T cell-mediated osteogenic differentiation of periosteal stem cells: coupling pathological bone formation to IL-17A and IL-17F signaling [abstract]. Arthritis Rheumatol 2017;69 (suppl 10):1936. [Google Scholar]
- 18. Gracey E, Yao Y, Green B, et al. . Sexual dimorphism in the Th17 signature of ankylosing spondylitis. Arthritis Rheumatol 2016;68:679–89. 10.1002/art.39464 [DOI] [PubMed] [Google Scholar]
- 19. Poddubnyy D, Vicari A, Haibel H, et al. . Interleukin-17 serum levels are associated with markers of systemic inflammation in patients with active ankylosing spondylitis [abstract]. ACR/ARHP Annual Meeting 2013;2493. [Google Scholar]
- 20. Glatt S, Helmer E, Haier B, et al. . First-In-Human randomized study of bimekizumab, a humanized monoclonal antibody and selective dual inhibitor of IL-17A and IL-17F, in mild psoriasis. Br J Clin Pharmacol 2017;83:991–1001. 10.1111/bcp.13185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Papp KA, Merola JF, Gottlieb AB, et al. . Dual neutralization of both interleukin 17A and interleukin 17F with bimekizumab in patients with psoriasis: results from BE ABLE 1, a 12-week randomized, double-blinded, placebo-controlled phase 2b trial. J Am Acad Dermatol 2018;79:277–86. e10 10.1016/j.jaad.2018.03.037 [DOI] [PubMed] [Google Scholar]
- 22. Kaeley GS, MacCarter DK, Pangan AL, et al. . Clinical responses and synovial vascularity in obese rheumatoid arthritis patients treated with adalimumab and methotrexate. J Rheumatol 2018;45:1628–35. 10.3899/jrheum.171232 [DOI] [PubMed] [Google Scholar]
- 23. van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 1984;27:361–8. 10.1002/art.1780270401 [DOI] [PubMed] [Google Scholar]
- 24. Sieper J, Rudwaleit M, Baraliakos X, et al. . The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 2009;68(Suppl 2):ii1–44. 10.1136/ard.2008.104018 [DOI] [PubMed] [Google Scholar]
- 25. Machado P, Landewé R, Lie E, et al. . Ankylosing spondylitis disease activity score (ASDAS): defining cut-off values for disease activity states and improvement scores. Ann Rheum Dis 2011;70:47–53. 10.1136/ard.2010.138594 [DOI] [PubMed] [Google Scholar]
- 26. Jenkinson TR, Mallorie PA, Whitelock HC, et al. . Defining spinal mobility in ankylosing spondylitis (AS). The Bath AS Metrology Index. J Rheumatol 1994;21:1694–8. [PubMed] [Google Scholar]
- 27. Nam JM. A simple approximation for calculating sample sizes for detecting linear trend in proportions. Biometrics 1987;43:701–5. 10.2307/2532006 [DOI] [PubMed] [Google Scholar]
- 28. Landewé R, Braun J, Deodhar A, et al. . Efficacy of certolizumab pegol on signs and symptoms of axial spondyloarthritis including ankylosing spondylitis: 24-week results of a double-blind randomised placebo-controlled phase 3 study. Ann Rheum Dis 2014;73:39–47. 10.1136/annrheumdis-2013-204231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. van der Heijde D, Schiff MH, Sieper J, et al. . Adalimumab effectiveness for the treatment of ankylosing spondylitis is maintained for up to 2 years: long-term results from the ATLAS trial. Ann Rheum Dis 2009;68:922–9. 10.1136/ard.2007.087270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959;22:719–48. [PubMed] [Google Scholar]
- 31. Ritchlin CT, Kavanaugh A, Merola JF, et al. . Dual neutralization of IL-17A and IL-17F with bimekizumab in patients with active PsA: results from a 48-week phase 2b, randomized, double blind, placebo-controlled, dose-ranging study [abstract]. Arthritis Rheumatol 2018;70 (Suppl 10). [Google Scholar]
- 32. Garrido-Cumbrera M, Hillmann O, Mahapatra R, et al. . Improving the management of psoriatic arthritis and axial spondyloarthritis: roundtable discussions with healthcare professionals and patients. Rheumatol Ther 2017;4:219–31. 10.1007/s40744-017-0066-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. van der Heijde D, Gladman DD, Kishimoto M, et al. . Efficacy and safety of ixekizumab in patients with active psoriatic arthritis: 52-week results from a phase III study (SPIRIT-P1). J Rheumatol 2018;45:367–77. 10.3899/jrheum.170429 [DOI] [PubMed] [Google Scholar]
- 34. Braun J, Baraliakos X, Listing J, et al. . Differences in the incidence of flares or new onset of inflammatory bowel diseases in patients with ankylosing spondylitis exposed to therapy with anti-tumor necrosis factor alpha agents. Arthritis Rheum 2007;57:639–47. 10.1002/art.22669 [DOI] [PubMed] [Google Scholar]
- 35. Schreiber S, Colombel J-F, Feagan BG, et al. . Incidence rates of inflammatory bowel disease in patients with psoriasis, psoriatic arthritis and ankylosing spondylitis treated with secukinumab: a retrospective analysis of pooled data from 21 clinical trials. Ann Rheum Dis 2019;78:473–9. 10.1136/annrheumdis-2018-214273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Marzo-Ortega H, Mysler E, Tetsuya T, et al. . Long-term safety of ixekizumab in patients with radiographic axial spondyloarthritis/ankylosing spondylitis: an integrated analysis of COAST-V and COAST-W [abstract]. Ann Rheum Dis 2019;78:885–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
annrheumdis-2020-216980supp001.pdf (1.7MB, pdf)
annrheumdis-2020-216980supp002.pdf (118.4MB, pdf)