Abstract
Objectives
In this study, we aim to determine the effect of metformin on osteoarthritis (OA) development and progression.
Methods
Destabilisation of the medial meniscus (DMM) surgery was performed in 10-week-old wild type and AMP-activated protein kinase (AMPK)α1 knockout (KO) mice. Metformin (4 mg/day in drinking water) was given, commencing either 2 weeks before or 2 weeks after DMM surgery. Mice were sacrificed 6 and 12 weeks after DMM surgery. OA phenotype was analysed by micro-computerised tomography (μCT), histology and pain-related behaviour tests. AMPKα1 (catalytic alpha subunit of AMPK) expression was examined by immunohistochemistry and immunofluorescence analyses. The OA phenotype was also determined by μCT and MRI in non-human primates.
Results
Metformin upregulated phosphorylated and total AMPK expression in articular cartilage tissue. Mild and more severe cartilage degeneration was observed at 6 and 12 weeks after DMM surgery, evidenced by markedly increased Osteoarthritis Research Society International scores, as well as reduced cartilage areas. The administration of metformin, commencing either before or after DMM surgery, caused significant reduction in cartilage degradation. Prominent synovial hyperplasia and osteophyte formation were observed at both 6 and 12 weeks after DMM surgery; these were significantly inhibited by treatment with metformin either before or after DMM surgery. The protective effects of metformin on OA development were not observed in AMPKα1 KO mice, suggesting that the chondroprotective effect of metformin is mediated by AMPK signalling. In addition, we demonstrated that treatment with metformin could also protect from OA progression in a partial medial meniscectomy animal model in non-human primates.
Conclusions
The present study suggests that metformin, administered shortly after joint injury, can limit OA development and progression in injury-induced OA animal models.
Keywords: arthritis, osteoarthritis, treatment, chondrocytes
Key messages.
What is already known about this subject?
Metformin is the first-line medication for the treatment of type 2 diabetes.
Metformin has been shown to activate AMP-activated protein kinase (AMPK).
Osteoarthritis (OA) phenotype induced by destabilisation of the medial meniscus was accelerated in AMPKα1 (catalytic alpha subunit of AMPK) knockout (KO) mice.
What does this study add?
Metformin had chondroprotective effect to decelerate OA development and progression.
Metformin enhanced AMPK expression and phosphorylation in articular chondrocytes in mice.
Metformin lost its chondroprotective effect on OA development in AMPKα1 KO mice, suggesting that the chondroprotective effect of metformin is mediated by AMPK signalling.
Metformin had chondroprotective effect on OA development in non-human primates.
How might this impact on clinical practice or future developments?
This study suggests that metformin may be used in clinics to treat patients with OA.
Introduction
Metformin is the first-line medication for the treatment of type 2 diabetes1 and the fourth-most prescribed medication in the USA in 2016 (https://www.medicinenet.com/top_drugs_prescribed_in_the_us/views.htm). Evidence suggests that metformin is generally well tolerated and seems to also be beneficial for a number of age-related diseases.2 3 Metformin could influence metabolic and cellular processes, such as inflammation, oxidative damage, diminished autophagy, cell senescence and apoptosis.4–7
Metformin has been shown to activate AMP-activated protein kinase (AMPK), a master regulator of energy balance and metabolism. Dysregulation of AMPK is linked to multiple age-related diseases including diabetes, atherosclerosis, cardiovascular disease, cancer, neurodegenerative diseases and osteoarthritis (OA).8–12 Reduced AMPK activity, assessed by phosphorylation of a specific threonine in the catalytic alpha subunit of AMPK (AMPKα1), is observed in both human and mouse knee OA cartilage.12–14 Decreased phosphorylation of AMPKα1 is also seen in chondrocytes after biomechanical injury or in response to interleukin-1β (IL-1β) and tumour necrosis factor-α (TNF-α).15 The administration of metformin could reverse these catabolic responses.16 17 These findings suggest that sustained AMPK activity in chondrocytes may be important for cartilage homeostasis. Indeed, it has been shown that AMPKα1 deficiency in chondrocytes accelerates development of both injury-induced and age-related spontaneous OA in mice.12
Patients with diabetes are nearly twice as likely to have arthritis, indicating a diabetes-arthritis connection.18 19 Diabetes can damage joints, a condition called diabetic arthropathy.19 Joint pain may be a response to an illness, injury or arthritis. AMPK has been identified as a novel target for pain treatment and metformin has been shown to decrease sensitivity to mechanical and thermal allodynia.20 21
OA is the most common form of arthritis and the leading cause of chronic disability among elderly people. According to estimates published in 2015, up to 240 million people around the world suffer from OA.22 Symptomatic knee OA occurs in 10% of men and in 13% of women aged 60 years or older.23 The number of people affected with symptomatic OA is likely to increase because of the ageing of the population and the obesity epidemic.15 Given the role of AMPK in OA and pain and metformin being an AMPK activator,12 20 21 in the present studies, we investigated the effects of metformin on prevention and treatment of OA both structurally and functionally in an OA mouse model induced by destabilisation of the medial meniscus (DMM). We also determined whether metformin limits OA development and progression through activation of AMPK signalling using AMPKα1 knockout (KO) mice. To further determine the therapeutic effect of metformin in OA pathogenesis in large animals, we performed a pilot experiment testing the effect of metformin on OA treatment in a partial medial meniscectomy (PMM) model using a non-human primate. Our findings demonstrated that metformin possesses chondroprotective effects on OA development and progression in rodents and in non-human primates through activation of AMPK signalling. Our studies suggest that metformin may be used in clinical interventions of OA disease.
Materials and methods
See online supplementary materials and methods.
annrheumdis-2019-216713supp001.pdf (522.5KB, pdf)
Results
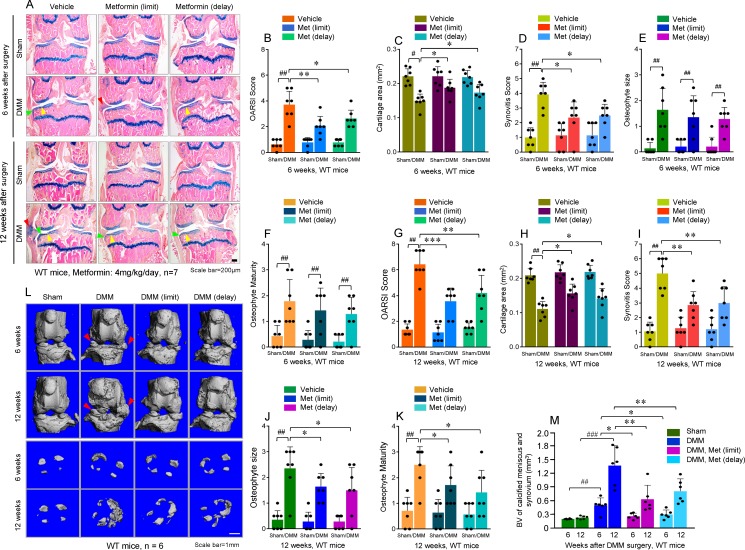
Metformin limited OA development and delayed OA progression in the mouse DMM model
To examine the effect of metformin on OA development and progression, we performed DMM surgery in 10-week-old male C57 wild-type (WT) mice with or without metformin administration commencing either 2 weeks before (limit or prevention) or 2 weeks after (delay or treatment) DMM surgery (see online supplementary figure S1A). We carried out histological analyses to assess knee joint damage including articular cartilage degradation, synovial tissue hyperplasia and osteophyte formation 6 and 12 weeks after DMM surgery. As expected, cartilage degeneration was mild at 6 weeks and became more severe at 12 weeks after DMM surgery, evidenced by markedly increased Osteoarthritis Research Society International (OARSI) scores (figure 1A, B, G), as well as reduced cartilage areas, quantified by histomorphometrical analysis of the Alcian blue stained articular cartilage areas. The administration of metformin (4 mg/day in drinking water, until the animals were sacrificed), commencing either 2 weeks before or 2 weeks after DMM surgery, caused partial but significant reduction in cartilage degradation (figure 1C, H). Prominent synovial hyperplasia (figure 1D, I) and osteophyte formation (figure 1E, F, J, K) analysed by synovitis score and osteophyte size and maturity were observed at both 6 and 12 weeks after DMM surgery; both were significantly inhibited by treatment with metformin either before or after DMM surgery. Results of micro-computerised tomography (µCT) analysis also showed that significantly increased osteophyte formation was observed in mice 6 and 12 weeks after DMM surgery (figure 1L, M) and this effect was significantly inhibited by treatment with metformin administered commencing either before or after DMM surgery (figure 1L, M). Considering OA progression during the 6 to 12 weeks period after DMM surgery, we found that in terms of the OARSI score, cartilage area and synovitis score, the progression rates were similar with or without metformin treatment in WT mice (see online supplementary figure S1B–D). However, in terms of osteophyte size and osteophyte maturity, the progression rates were significantly reduced after metformin treatment in WT mice (see online supplementary figure S1E, F). We also analysed changes in subchondral bone mass and found that subchondral bone mass was significantly increased 6 and 12 weeks after DMM surgery in WT mice (see online supplementary figure S1L) and metformin had no significant effect on DMM-induced subchondral bone mass increase (see online supplementary figure S1L). These results suggest that metformin can limit OA development and delay OA progression in the injury-induced OA mouse model, administered shortly after joint injury.
Figure 1.
Metformin limited osteoarthritis (OA) development and delayed OA progression in the mouse destabilisation of the medial meniscus (DMM) model. (A) Representative histology images of osteoarthritic knee joints, that were collected 6 and 12 weeks after DMM surgery. Yellow arrowheads indicate articular cartilage degradation, green arrowheads indicate osteophytes and red arrowheads indicate synovial hyperplasia. n=7; scale bar: 200 µm. (B, G) The severity of OA-like phenotype was analysed by grading histological sections in medial femoral condyles (MFCs) and the medial tibial plateau (MTP) using the Osteoarthritis Research Society International (OARSI) score system. (C, H) The articular cartilage areas of MFCs and MTPs were quantified by tracing the Alcian blue positive stained areas using the OsteoMeasure system. (D, I) The degree of synovitis was semi-quantified by the number of synovial lining layers. (E, F, J, K) Osteophytes were semi-quantified by evaluating the osteophyte formation score consisting of two domains, size (E, F) and maturity (J, K). n=7. (L, M) The osteophyte formation was analysed by micro-computerised tomography in mice with or without metformin treatment 6 and 12 weeks after DMM surgery. The volume of calcified meniscus and synovial tissue was quantified. n=6; scale bar: 1 mm. Statistical analysis was conducted using two-way analysis of variance followed by the Tukey-Kramer test. # p<0.05, ## p<0.01, compared between sham and DMM groups; *p<0.05, **p<0.01, ***p<0.001, compared between groups with or without metformin treatment in mice with DMM surgery. Met, metformin; WT, wild type.
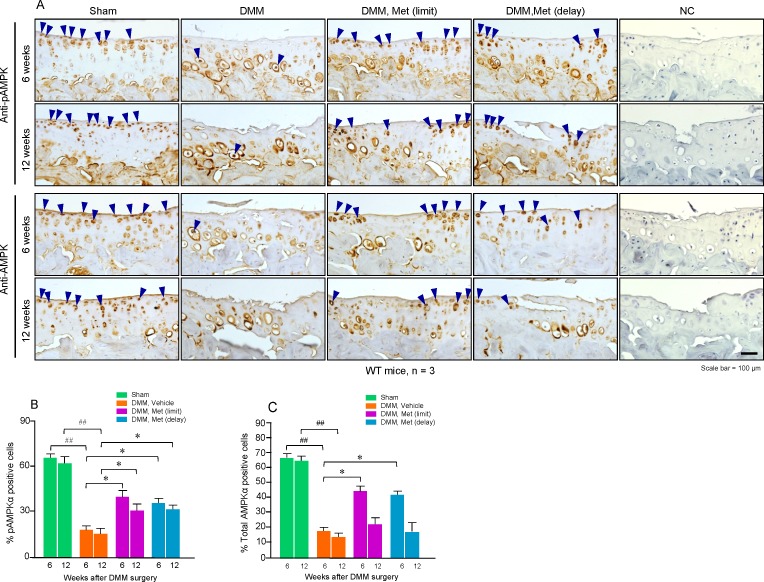
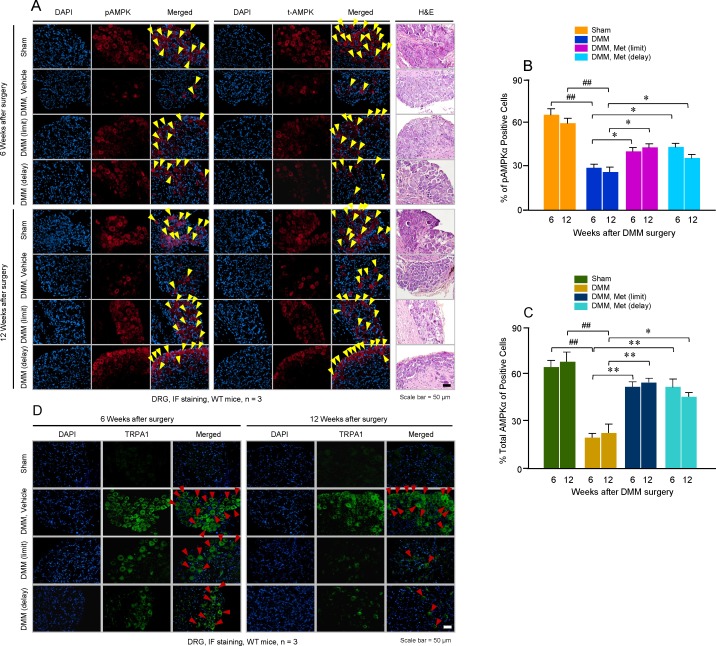
Metformin induced AMPK phosphorylation and expression
Because metformin is a known AMPK activator,24 we examined, using immunohistochemistry (IHC) analysis, whether metformin upregulates the phosphorylation and expression of AMPKα1 in articular cartilage tissue. We found that metformin, either given before or after DMM surgery, significantly increased phosphorylated AMPKα1 expression in articular chondrocytes of knee cartilage at both 6 and 12 weeks after DMM surgery (figure 2A, B). Notably, metformin also increased total AMPKα1 expression in articular chondrocytes at the 6-week time point when it was given before or after DMM surgery (figure 2A, C).
Figure 2.
Metformin induced AMP-activated protein kinase (AMPK) phosphorylation and expression. (A) Knee joint sections from sham, destabilisation of the medial meniscus (DMM) surgery (6 or 12 weeks after DMM surgery) or treatment with or without metformin were analysed for AMPK expression using immunohistochemistry methods. Results showed that expression of both phosphorylated AMPKα (pAMPKα) (upper panel) and total AMPKα (catalyticalpha subunit of AMPK) (lower panel) was upregulated by the treatment with metformin. The cells present in the non-calcified regions of femoral and tibial cartilage were subjected to further analysis. (B, C) Cells with positive staining for pAMPKα and total AMPKα were quantified (n=3). Statistical analysis was conducted using two-way analysis of variance followed by the Tukey-Kramer test. ## p<0.01, compared between sham and DMM groups; *p<0.05, compared between groups with or without metformin treatment in mice with DMM surgery. Met, metformin; NC, negative control; WT, wild type.
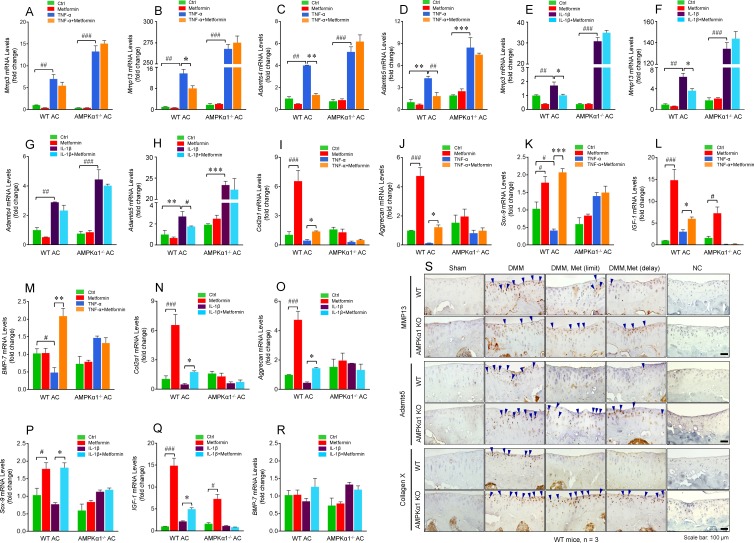
AMPK mediated chondroprotective effect of metformin
Next, we performed an in vitro study to determine the effect of metformin on TNF-α and IL-1β-induced catabolic response. We found that expression of Mmp3, Mmp13, Adamts4 and Adamts5 was significantly upregulated by TNF-α (figure 3A–D) and IL-1β (figure 3E–H) in primary murine articular chondrocytes derived from WT mice. The addition of metformin significantly inhibited TNF-α and IL-1β-induced Mmp13 expression (figure 3B, F) and IL-1β-induced Mmp3 expression (figure 3E). In addition, metformin inhibited TNF-α-induced Adamts4 expression (figure 3C) and TNF-α- and IL-1β-induced Adamts5 expression (figure 3D, H) in WT chondrocytes. We also examined effects of metformin on expression of TNF-α- and IL-1β-induced chondrocyte catabolic marker genes in articular chondrocytes derived from AMPKα1-/- mice. Metformin had no significant effects on expression of TNF-α and IL-1β-induced chondrocyte marker genes in articular chondrocytes derived from AMPKα1-/- mice (figure 3A–H). These findings suggest that metformin is a potent drug inhibiting catabolic responses caused by inflammatory cytokines. In addition to catabolic genes, we also examined expression of anabolic genes. We found that metformin upregulated expression of Col2a1, aggrecan, Sox9 and IGF-1 in articular chondrocytes of WT mice (figure 3I–L, N–Q). In contrast, metformin had no significant effect on Bmp7 expression (figure 3M, R). Metformin also reversed the inhibitory effects of TNF-α on expressions of Col2a1, aggrecan, Sox9, IGF-1 and Bmp7 (figure 3I–M). In addition, except upregulation of IGF-1 expression (figure 3L, Q), metformin had no significant effects on other anabolic genes in AMPKα1-/- mice. These results suggest that metformin exerts its chondroprotective effect not only by inhibition of catabolic genes but also by upregulation of anabolic genes through an AMPK-dependent mechanism. IHC results further demonstrated that expression of MMP13, Adamts5 and Col-X proteins was upregulated in mice performed with DMM surgery (see online supplementary figure 3S). The administration of metformin, commencing either before or after DMM surgery, could significantly inhibit MMP13, Adamts5 and Col-X expression (see online supplementary figure 3S) in WT mice. However, no significant attenuation effect of metformin on MMP13, Adamts5 and Col-X expression in AMPKα1-/- mice was seen (see online supplementary figure 3S). We also examined the effect of metformin on AMPK phosphorylation in human articular chondrocytes and found that metformin significantly upregulated AMPK phosphorylation within 16 hours time period (see online supplementary figure S2A). TNF-α and IL-1β inhibited AMPK phosphorylation and these inhibitory effects could be reversed by treatment with metformin (see online supplementary figure S2B). In addition, IL-1β-induced nitric oxide release could be inhibited by metformin in a dose-dependent manner in articular chondrocytes derived from WT mice; this effect was abolished in articular chondrocytes derived from AMPKα1-/- mice (see online supplementary figure S2C). In our previous studies, we have shown that expressions of phosphorylated and total AMPKα1 are reduced in both primary chondrocytes isolated from knee joint tissues of OA patients (by Western blot analysis) and articular cartilage tissues collected from OA patients (by IHC), compared with normal primary knee chondrocytes and normal knee cartilage, respectively.15
Figure 3.
AMP-activated protein kinase (AMPK) mediated chondroprotective effect of metformin. (A–H) Murine articular chondrocytes were treated with metformin (2 mg) and then incubated with tumour necrosis factor-α (TNF-α; 100 ng/mL) (A–D) or interleukin-1β (IL-1β; 10 ng/mL) (E–H) for 6 hours. Expression of Mmp3, Mmp13, Adamts4 and Adamts5 mRNAs were analysed by real-time polymerase chain reaction (PCR) (n=3). (I) Immunohistochemistry (IHC) assays were performed using histological sections collected from mice with sham operation or destabilisation of the medial meniscus (DMM) surgery with metformin treatment. Expression of MMP13, Adamts5 and Col-X was examined (n=3). AMPKα1, catalytic alpha subunit of AMPK; KO, knockout; Met, metformin; mRNA, messenger RNA; WT, wild type.
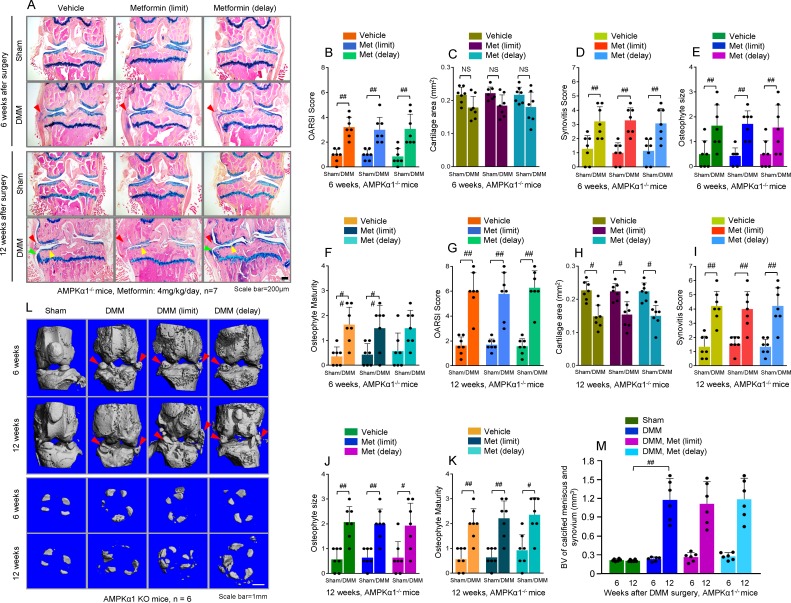
We then went on to test the effects of metformin on OA development in AMPKα1-/- mice. We found that AMPKα1-/- mice administered metformin still exhibited the OA phenotype to an extent similar to that of WT mice not administered metformin. This was demonstrated by analysing histological changes (figure 4A) and changes in OARSI scores (figure 4B, G), cartilage area (figure 4C, H), synovitis score (figure 4D, I), osteophyte size (figure 4E, J) and osteophyte maturity (figure 4F, K). Results of µCT analysis showed that significant osteophyte formation was observed 6 and 12 weeks after DMM surgery in AMPKα1-/- mice (figure 4L, M). Treatment with metformin, commencing either before or after DMM surgery, had no significant effect on inhibition of osteophyte formation in AMPKα1-/- mice (figure 4L, M). Considering the OA progression rate, all parameters reflecting OA progression, including OARSI scores, cartilage areas, synovitis score, osteophyte size and osteophyte maturity, had no significant changes in AMPKα1-/- mice (see online supplementary figure S1G–K). In addition, we found that subchondral bone mass was significantly increased 6 and 12 weeks after DMM surgery in AMPKα1-/- mice (see online supplementary figure S1M). Metformin had no significant effect on DMM-induced subchondral bone mass increase (see online supplementary figure S1M). These results suggest that the chondroprotective effect of metformin was mediated by AMPK.
Figure 4.
Metformin had no protective effect on destabilisation of medial meniscus (DMM)-induced osteoarthritis (OA) in AMP-activated protein kinase (AMPK) α1 knockout (KO) mice. (A) DMM surgery or sham operation was performed in 10-week-old AMPKα1 KO mice. Metformin (4 mg/kg/day in drinking water, until the animals were sacrificed) was administered to the mice 2 weeks before or 2 weeks after DMM surgery. Representative histology images of osteoarthritic knee joints demonstrated that metformin had no significant effect on OA development in AMPKα1 KO mice. Yellow arrowheads indicate articular cartilage degradation, green arrowheads indicate osteophytes and red arrowheads indicate synovial hyperplasia. n=7; scale bar: 200 µm. (B–K) Quantification or semi-quantification assessments, including Osteoarthritis Research Society International (OARSI) score (B, G), cartilage area (C, H), synovitis score (D, I), osteophyte size (E, J) and osteophyte maturity (F, K) were performed using histological sections. n=7. (L, M) Osteophyte formation was analysed by micro-computerised tomography in mice with or without metformin treatment 6 and 12 weeks after DMM surgery. The volume of calcified meniscus and synovial tissue was quantified (n=6). Statistical analysis was conducted using two-way analysis of variance followed by the Tukey-Kramer test. # p<0.05, ## p<0.01, compared between sham and DMM surgery groups. AMPKα1, AMP-activated protein kinase α1; Met, metformin.
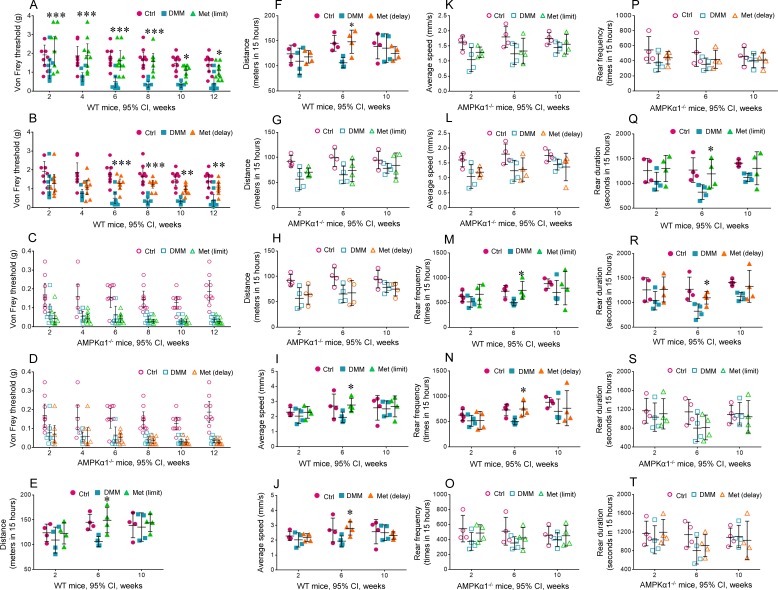
Metformin attenuated OA pain
We then performed a series of tests to determine if metformin lowers OA pain sensitivity. The results of von Frey tests showed that significantly reduced paw withdrawal response thresholds were observed after DMM surgery in mice without metformin treatment in WT mice (figure 5A, B). The administration of metformin (4 mg/day in drinking water, until the animals were sacrificed), commencing either 2 weeks before or 2 weeks after DMM surgery, could significantly increase paw withdrawal response threshold, reflecting reduced pain sensitivity in WT mice (figure 5A, B). In contrast, metformin had no significant effect on reversing paw withdrawal response threshold and reducing pain sensitivity in AMPKα1-/- mice (figure 5C, D). We also tested spontaneous activity of the mice in response to DMM surgery and metformin treatment using the Laboratory Animal Behaviour Observation, Registration and Analysis System (LABORAS). We found that travel distance (figure 5E, F), average walking speed (figure 5I, J), rearing frequency (figure 5M, N) and rearing duration (see online supplementary figure 5R, S) were significantly decreased 6 weeks after DMM surgery without metformin treatment. Treatment with metformin, commencing either before or after DMM surgery, could significantly reverse reduced spontaneous activity caused by DMM surgery (figure 5E, F, I, J, M, N, R, S), indicating that in addition to the inhibition of mechanically-induced pain sensitivity, metformin could also reverse reduced spontaneous activity observed in mice with DMM surgery. In contrast, treatment with metformin had no significant effect on reduced spontaneous activity caused by DMM surgery in AMPKα1-/- mice (figure 5G, H, K, L, P, Q). These results are consistent with those of von Frey tests.
Figure 5.
Metformin attenuated osteoarthritis pain. (A, B) Metformin (4 mg/kg/day in drinking water, until the animals were sacrificed) was administered 2 weeks before (limit group) or after (delay group) destabilisation of the medial meniscus (DMM) surgery. Mechanical sensitivity was measured using von Frey filaments biweekly after DMM surgery. n=10. Statistical analysis was conducted using two-way analysis of variance (ANOVA) followed by the Tukey-Kramer test. *p<0.05, **p<0.01, ***p<0.001, compared between groups with or without metformin treatment in mice with DMM surgery. (C–J) Changes in spontaneous activity, including travel distance (C, D), average walking speed (E, F), rearing frequency (G, H) and rearing duration (I, J) were evaluated using the Laboratory Animal Behaviour Observation Registration and Analysis System (LABORAS, Metris, Netherlands) 2, 6 and 10 weeks after DMM surgery (n=4). Statistical analysis was conducted using two-way ANOVA followed by the Tukey-Kramer test. *p<0.05, compared between groups with or without metformin treatment in mice with DMM surgery. AMPKα1, catalytic alpha subunit of AMPK; Met, metformin; WT, wild type.
Because metformin possesses a protective effect against DMM-induced OA pain, we examined whether metformin affects phosphorylation and expression of AMPKα1 in dorsal root ganglia (DRG) using immunofluorescence (IF) staining. We found that expressions of pAMPKα1 and total AMPKα1 were significantly reduced 6 and 12 weeks after DMM surgery (figure 6A–C). Treatment with metformin upregulated pAMPKα1 and total AMPKα1 expression in DRG cells after DMM surgery (figure 6A–C). AMPKα1 expression was mainly detected in the cell membrane (figure 6A). We then analysed expression of a pain-related marker downstream of AMPK, transient receptor potential ankyrin 1 (TRPA1), and found that TRPA1 expression was significantly upregulated 6 and 12 weeks after DMM surgery (figure 6D). Treatment with metformin, commencing either before or after DMM surgery, significantly inhibited TRPA1 expression in DRG tissues (figure 6D). In addition, we also analysed expressions of a series of pain-related marker genes in articular chondrocytes isolated from 4-day-old WT and AMPKα1-/- mice. We found that TNF-α and IL-1β significantly upregulated pain-related marker genes, such as MCP-1, CCR2, NGF, TNF-α in both WT and AMPKα1-/- mice (see online supplementary figure S3A–J). Treatment with metformin significantly inhibited expressions of these marker genes induced by TNF-α and IL-1β in WT chondrocytes but not in AMPKα1-deficient chondrocytes (see online supplementary figure S3A–J). These results suggest that metformin may upregulate AMPKα1 expression and phosphorylation and further inhibit pain-related signals in DRG and cartilage tissues.
Figure 6.
Metformin upregulated AMP-activated protein kinase (AMPK) expression in the dorsal root ganglia (DRG). (A) Immunofluorescence (IF) assays were performed in histological sections of DRG tissues in the mice 6 and 12 weeks after destabilisation of the medial meniscus (DMM) surgery; expression of pAMPKα1 and total AMPKα1 was examined by IF staining. (B, C) Results of quantification analysis demonstrated that AMPKα1 expression (phosphorylated and total AMPK α1) was significantly reduced after DMM surgery. Metformin significantly increased the expression of pAMPKα1 and total AMPK α1 protein levels in DRG tissues (n=3). Statistical analysis was conducted using two-way analysis of variance followed by the Tukey-Kramer test. ##p<0.01, compared between sham and DMM groups; *p<0.05, **p<0.01, compared between groups with or without metformin treatment in mice with DMM surgery. pAMPK, phosphorylated AMPK; t-AMPK, total AMPK; TRPA1, transient receptor potentialankyrin 1; WT, wild type.
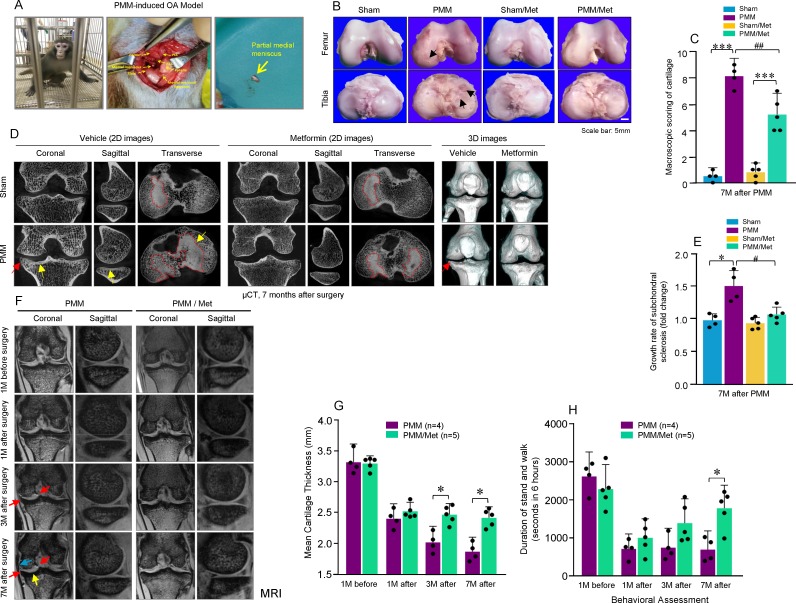
Metformin alleviated OA development in non-human primates
To further investigate the role of metformin in large animals, we determined the effect of metformin on OA development in non-human primates. We performed PMM surgery on male rhesus macaques with 8.5 to 11.4 years of age which were treated with vehicle (n=4) or metformin (n=5) 1 month after PMM surgery (see online supplementary figure S4). The PMM surgery was performed on the left knee joint and a sham operation was performed on the right knee joint (figure 7A). OA-like lesions were observed in rhesus macaques 7 months after PMM surgery at the macroscopic level (figure 7B). The semi-quantification score of cartilage damage for femoral and tibial condyles showed that the treatment with metformin significantly alleviated the cartilage lesions (figure 7C). μCT analysis showed that subchondral bone mass was significantly increased in the rhesus macaques 7 months after PMM surgery (figure 7D). In contrast, subchondral bone mass was significantly reduced by treatment with metformin in the rhesus macaques 7 months after PMM surgery (figure 7D, E). MRI analysis showed that treatment with metformin protected against cartilage loss, demonstrated by higher cartilage thickness observed in metformin treated rhesus macaques 3 and 7 months after PMM surgery (figure 7F, G). Results of pain-related behaviour test also showed that the duration of standing and walking was significantly increased by treatment with metformin 7 months after PMM surgery (figure 7H). Because metformin inhibits OA development in non-human primates, these findings suggest that metformin may be used to treat patients with OA disease.
Figure 7.
Metformin alleviates partial medial meniscectomy (PMM)-induced osteoarthritis (OA) development in non-human primates. (A) The PMM surgery was performed on the left knee joint and the sham operation was performed on the right knee joint in rhesus macaques with 8.5 to 11.4 years of age. (B, C) Cartilage damage was observed in rhesus macaques 7 months after the PMM surgery. The administration of metformin inhibited articular cartilage damage in rhesus macaques with PMM surgery (yellow arrows: articular cartilage damage). (D, E) Two-dimensional and three-dimensional images of micro-computerised tomography (μCT) scans were obtained 7 months after PMM surgery (yellow arrow: subchondral sclerosis and red arrow: osteophyte). (F) Knee OA was monitored by MRI 1 month before surgery and 1, 3 and 7 months after surgery (red arrows: osteophytes; yellow arrow: subchondral sclerosis; blue arrow: knee joint medial collateral ligament). (G) The medial articular cartilage thickness including medial femoral condyles and the medial tibial plateau was quantified using MRI. Control group: rhesus macaques received PMM surgery and were treated with vehicle (n=4); experimental group: Rhesus macaques received PMM surgery and were treated with metformin (n=5). (H) Changes in animal behaviour were observed and recorded. *p<0.05, compared between groups with or without metformin treatment. Met, metformin.
Discussion
We have made several key observations in the studies presented here. (1) We found that metformin, administered shortly after joint injury, limits OA development and delays OA progression. Metformin also relieves OA-associated pain sensitivity in mice. (2) We found that metformin upregulates AMPKα1 expression and that metformin lost its chondroprotective effect in AMPKα1 KO mice; this suggests that the chondroprotective effect of metformin is mediated by activation of AMPK signalling. (3) To determine the role of metformin in large animals, we performed a pilot experiment using non-human primates. We found that metformin also possesses a chondroprotective effect in non-human primates. In addition, we also analysed the OA progression rates during 6 to 12 weeks period after DMM surgery. We found that, during this period, the progression rates of some OA features, including OARSI score, cartilage area and synovitis score, were not significantly changed after metformin administration; in contrast, the progression rates of some other OA features, including osteophyte size and osteophyte maturity were significantly reduced after metformin administration. Our findings suggest that metformin may be used clinically to treat patients with OA and that selective OA symptoms may be improved after metformin administration shortly after joint injury.
OA is the most common form of arthritis and the leading cause of chronic disability among older people. More than 50% of people over the age of 65 years have radiological evidence of OA, with approximately 10% of men and 18% of women suffering symptomatic OA.25 In a population-based cohort study, the lifetime risk of symptomatic knee OA was 45%.26 There is currently no medication available to cure OA disease or to decelerate OA progression; thus disease-modifying OA drugs are urgently needed to not only alleviate pain and improve function, but also to delay the structural progression of the disease. None of drugs currently being tested in Phase II and Phase III clinical trials for OA treatment are aimed at targeting AMPK signalling; thus, a drug, such as metformin, acting on activation of AMPK signalling, represents a novel class of drugs to treat OA disease.
AMPK signalling has been suggested to be involved in OA development27 and AMPK deficiency in chondrocytes accelerates the progression of OA induced by DMM surgery or ageing in adult mice.12 However, opposite results have also been reported, showing that no significant difference in OA development was observed in chondrocyte-specific AMPKα1 KO mice.28 It has also been reported that activation of AMPK signalling negatively regulates chondrocyte differentiation.29 In the present studies, we found that the knee joint phenotype induced by DMM surgery in AMPKα1 KO mice was not significantly different from that of WT mice; however, metformin has protective effect on OA progression in WT mice, but not in AMPKα1 KO mice. These results suggest that normal levels of AMPKα1 may not be required for maintaining joint tissue homeostasis and that metformin does play a chondroprotective effect through activation of AMPK signalling. The AMPKα1 KO mice used in our study are AMPKα1 global KO mice, but not chondrocyte-specific KO mice reported in previous studies.12 28 In addition to mature chondrocytes, AMPKα1 gene was also deleted in mesenchymal progenitor cells in AMPKα1 global KO mice so both mesenchymal progenitor cells and mature chondrocytes may contribute to the observations that deletion of AMPKα1 blocks the chondroprotective effect of metformin in the current studies.
AMPK exists as a heterotrimeric complex composed of a catalytic α subunit and regulatory β and γ subunits. Binding of AMP to the γ subunit allosterically activates the complex, making it a more attractive substrate for phosphorylation on Thr172 in the activation loop of the α subunit by its major upstream AMPK kinase, liver kinase B1 (LKB1).30 The activity of AMPK and its upstream regulator LKB1 is reduced in cartilage from aged mice and mice with OA, as well as in bovine chondrocytes after dynamic compression-induced biomechanical injury.31
In our in vitro studies, we found that metformin upregulated pAMPKα1 expression within a short period of time, but not the total AMPKα1 protein. In contrast, we found that metformin significantly upregulated total AMPKα1 expression in articular chondrocytes and in DRG cells. This difference may be due to the duration of treatment. In vivo treatment with metformin was 6 and 12 weeks. The long-term effect of metformin on the upregulation of total AMPKα1 may also contribute to the effect of metformin on OA treatment. In addition to the treatment duration, the endogenous AMPK levels may also affect the effectiveness of metformin treatment. OA is a heterogeneous disease. Metformin may be specifically effective for OA patients with low AMPK levels. In the future, we may further stratify OA patients into two groups with high and low AMPK levels to further determine the effectiveness of metformin on OA pathogenesis.
In this study, we also found that metformin is an effective drug to relieve OA pain. Pain is the most common reason that OA patients seek medical attention and is frequently a symptom of underlying joint injury. AMPK activation plays an important role in blocking pain sensitivity.32 33 Pain hypersensitivity resulting from injury or disease is often paralleled by increased excitability of peripheral sensory neurons in the DRG.15 The TRPA1 channel is a widely recognised chemical and thermal sensor that plays vital roles in pain transduction.34 Metformin, as an AMPK activator, inhibited TRPA1 activity in DRG neurons by inhibiting membrane-associated TRPA1 expression and metformin also inhibited TRPA1-mediated calcium influx.35 These findings suggest that AMPK is a key regulator of TRPA1 channels and that metformin may inhibit pain sensitivity through activation of AMPK signalling in DRGs. In the present studies, we found that treatment with metformin significantly upregulated phosphorylated and total AMPKα1 expression in DRG tissues and also inhibited the increased pain sensitivity caused by DMM surgery. These findings suggest that metformin may inhibit pain-mediating calcium channel activities through activation of AMPK signalling in DRG tissues. From our limited time-course studies, it seems that pain relieving effect of metformin may be related to its chondroprotective effect on DMM-induced OA pathology.
The current study has several limitations. First, our study suggests that metformin could be used clinically for young patients shortly after their joint injury to limit OA development and progression. However, one critical question that we could not address in this study is whether metformin is able to delay OA progression when OA is fully developed. Our long-term goal is to perform a longitudinal study to investigate the effect of metformin on OA progression and OA associated pain when OA is fully developed; for example, 8 and 12 weeks after DMM surgery. Second, to further determine the role of metformin in OA treatment, we tested effects of metformin in non-human primates. Although a positive effect of metformin on OA treatment has been obtained using non-human primates in the pilot study, one limitation of this study is that animal numbers were relatively small. The effect of metformin on large animals needs to be further investigated. Third, in the presented studies, we have used young, healthy and male mice and male rhesus macaques for OA studies, to further determine the chondroprotective effects of metformin, we will test the effects of metformin on female mice, on ageing-associated OA models and on obese mice. These studies will provide full spectrum of chondroprotective effects of metformin.
Our studies suggest that metformin may be used clinically to treat young patients shortly after their joint injury. In human clinical studies, metformin application has been demonstrated to have a beneficial effect on long-term knee joint outcomes in those with knee OA and obesity.36 In contrast, a retrospective cohort study was conducted using information of 3217 patients with type 2 diabetes in the UK. Patients had recorded type 2 diabetes and treatment with metformin. The outcome was the record of OA during follow-up. The results demonstrated that treatment with metformin had no significant effect on OA progression.37 This discrepancy could be the result of different dosages and treatment durations that were administered. Randomised controlled clinical trials are needed to determine whether metformin could be used as a potential disease-modifying drug for knee OA with or without the obese phenotype.
Acknowledgments
We would like to express our gratitude to Ms Lily Yu for her assistance on processing and staining histological samples and Dr Benoit Viollet (INSERM, U1016, Paris, France) for providing us with AMPKα1 KO mice.
Footnotes
Handling editor: Josef S Smolen
JL and BZ contributed equally.
Contributors: Conception and Design: DC, RL-B and SF. Data Acquisition: JL, BZ, W-XL, KL, TW, DY, JH, LZ and CX. Analysis and Interpretation of Data: DC, RL-B, JL, HP, GN, GX. Manuscript Preparation: DC and JL. Manuscript Revision: DC, JL, RL-B and SF. Manuscript Final Approval: DC.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: Institutional review Board of Rush University Medical Center and Tianjin Medical University General Hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository. The data that support the findings of this study are available within the article and its Supplementary Information files or from the corresponding author upon reasonable request.
References
- 1. Nasri H, Rafieian-Kopaei M. Metformin: current knowledge. J Res Med Sci 2014;19:658–64. [PMC free article] [PubMed] [Google Scholar]
- 2. Paneni F, Lüscher TF. Cardiovascular protection in the treatment of type 2 diabetes: a review of clinical trial results across drug classes. Am J Cardiol 2017;120:S17–27. 10.1016/j.amjcard.2017.05.015 [DOI] [PubMed] [Google Scholar]
- 3. Novelle MG, Ali A, Diéguez C, et al. Metformin: a hopeful promise in aging research. Cold Spring Harb Perspect Med 2016;6:a025932 10.1101/cshperspect.a025932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen K, Lin Z-W, He S-M, et al. Metformin inhibits the proliferation of rheumatoid arthritis fibroblast-like synoviocytes through IGF-IR/PI3K/AKT/m-TOR pathway. Biomed Pharmacother 2019;115:108875 10.1016/j.biopha.2019.108875 [DOI] [PubMed] [Google Scholar]
- 5. Teodoro JS, Nunes S, Rolo AP, et al. Therapeutic options targeting oxidative stress, mitochondrial dysfunction and inflammation to hinder the progression of vascular complications of diabetes. Front Physiol 2018;9:1–18. 10.3389/fphys.2018.01857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li Q, Jia S, Xu L, et al. Metformin‐induced autophagy and irisin improves INS-1 cell function and survival in high-glucose environment via AMPK/SIRT1/PGC-1α signal pathway. Food Sci Nutr 2019;7:1695–703. 10.1002/fsn3.1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen D, Xia D, Pan Z, et al. Metformin protects against apoptosis and senescence in nucleus pulposus cells and ameliorates disc degeneration in vivo. Cell Death Dis 2016;7:e2441 10.1038/cddis.2016.334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Forouzandeh F, Salazar G, Patrushev N, et al. Metformin beyond diabetes: pleiotropic benefits of metformin in attenuation of atherosclerosis. J Am Heart Assoc 2014;3:e001202 10.1161/JAHA.114.001202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zi F, Zi H, Li Y, et al. Metformin and cancer: an existing drug for cancer prevention and therapy. Oncol Lett 2018;15:683–90. 10.3892/ol.2017.7412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rena G, Lang CC. Repurposing metformin for cardiovascular disease. Circulation 2018;137:422–4. 10.1161/CIRCULATIONAHA.117.031735 [DOI] [PubMed] [Google Scholar]
- 11. Rotermund C, Machetanz G, Fitzgerald JC. The therapeutic potential of metformin in neurodegenerative diseases. Front Endocrinol 2018;9:400 10.3389/fendo.2018.00400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou S, Lu W, Chen L, et al. AMPK deficiency in chondrocytes accelerated the progression of instability-induced and ageing-associated osteoarthritis in adult mice. Sci Rep 2017;7:43245 10.1038/srep43245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stein SC, Woods A, Jones NA, et al. The regulation of AMP-activated protein kinase by phosphorylation. Biochem J 2000;345:437–43. 10.1042/bj3450437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. June RK, Liu-Bryan R, Long F, et al. Emerging role of metabolic signaling in synovial joint remodeling and osteoarthritis. J Orthop Res 2016;34:2048–58. 10.1002/jor.23420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Terkeltaub R, Yang B, Lotz M, et al. Chondrocyte AMP-activated protein kinase activity suppresses matrix degradation responses to proinflammatory cytokines interleukin-1β and tumor necrosis factor α. Arthritis Rheum 2011;63:1928–37. 10.1002/art.30333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guma M, Wang Y, Viollet B, et al. AMPK activation by A-769662 controls IL-6 expression in inflammatory arthritis. PLoS One 2015;10:e0140452 10.1371/journal.pone.0140452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu-Bryan R, Terkeltaub R. Emerging regulators of the inflammatory process in osteoarthritis. Nat Rev Rheumatol 2015;11:35–44. 10.1038/nrrheum.2014.162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Arthritis Foundation, Rheumatoid vs. osteoarthritis and diabetes. Available: www.arthritis.org/living-with-arthritis/comorbidities/diabetes-and-arthritis/rheumatoid-arthritis-vs-osteoarthritis-diabetes.php [Accessed 2 Apr 2019].
- 19. Diabetologia Press release. study links diabetes to elevated risk of osteoporosis and arthritis. October 2, 2018. Berlin. European Association for the Study of Diabetes (EASD) annual meeting. Available: www.eurekalert.org/pub_releases/2018-10/d-sld093018.php
- 20. Asiedu MN, Dussor G, Price TJ. Targeting AMPK for the alleviation of pathological pain. Exp Suppl 2016;107:257–85. 10.1007/978-3-319-43589-3_11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Weng W, Yao C, Poonit K, et al. Metformin relieves neuropathic pain after spinal nerve ligation via autophagy flux stimulation. J Cell Mol Med 2019;23:1313–24. 10.1111/jcmm.14033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. The Burden of Musculoskeletal Diseases in the United States Bone and joint decade. 2nd edn, 2011. [Google Scholar]
- 23. Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med 2010;26:355–69. 10.1016/j.cger.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Meng S, Cao J, He Q, et al. Metformin activates AMP-activated protein kinase by promoting formation of the αβγ heterotrimeric complex. J Biol Chem 2015;290:3793–802. 10.1074/jbc.M114.604421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ 2003;81:646–56. [PMC free article] [PubMed] [Google Scholar]
- 26. Murphy L, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum 2008;59:1207–13. 10.1002/art.24021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yui N, Kobayashi H, Terauchi K, et al. The role of ALP-activated protein kinase (AMPK) in the chondrocyte energy balance and IL-1β-induced production of MMP-13 in osteoarthritis(OA). Osteoarthritis Cartilage 2016;24:S154–5. 10.1016/j.joca.2016.01.304 [DOI] [Google Scholar]
- 28. Yang C, Li Z, Lai P, et al. Chondrocyte-specific ablation of AMPKα1 does not affect bone development or pathogenesis of osteoarthritis in mice. DNA Cell Biol 2016;35:156–62. 10.1089/dna.2015.3074 [DOI] [PubMed] [Google Scholar]
- 29. Bandow K, Kusuyama J, Kakimoto K, et al. AMP-activated protein kinase (AMPK) activity negatively regulates chondrogenic differentiation. Bone 2015;74:125–33. 10.1016/j.bone.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 30. Shackelford DB, Shaw RJ. The LKB1-AMPK pathway: metabolism and growth control in tumour suppression. Nat Rev Cancer 2009;9:563–75. 10.1038/nrc2676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Petursson F, Husa M, June R, et al. Linked decreases in liver kinase B1 and AMP-activated protein kinase activity modulate matrix catabolic responses to biomechanical injury in chondrocytes. Arthritis Res Ther 2013;15:R77 10.1186/ar4254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Asiedu MN, Han C, Dib-Hajj SD, et al. The AMPK activator A769662 blocks voltage-gated sodium channels: discovery of a novel pharmacophore with potential utility for analgesic development. PLoS One 2017;12:e0169882 10.1371/journal.pone.0169882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tillu DV, Melemedjian OK, Asiedu MN, et al. Resveratrol engages AMPK to attenuate ERK and mTOR signaling in sensory neurons and inhibits incision-induced acute and chronic pain. Mol Pain 2012;8:5 10.1186/1744-8069-8-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Story GM, Peier AM, Reeve AJ, et al. ANKTM1, a TRP-like channel expressed in nociceptive neurons, is activated by cold temperatures. Cell 2003;112:819–29. 10.1016/S0092-8674(03)00158-2 [DOI] [PubMed] [Google Scholar]
- 35. Wang S, Kobayashi K, Kogure Y, et al. Negative regulation of TRPA1 by AMPK in primary sensory neurons as a potential mechanism of painful diabetic neuropathy. Diabetes 2018;67:98–109. 10.2337/db17-0503 [DOI] [PubMed] [Google Scholar]
- 36. Wang Y, Hussain SM, Wluka AE, et al. Association between metformin use and disease progression in obese people with knee osteoarthritis: data from the osteoarthritis Initiative-a prospective cohort study. Arthritis Res Ther 2019;21:127 10.1186/s13075-019-1915-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Barnett LA, Jordan KP, Edwards JJ, et al. Does metformin protect against osteoarthritis? An electronic health record cohort study. Prim Health Care Res Dev 2017;18:623–8. 10.1017/S1463423617000287 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
annrheumdis-2019-216713supp001.pdf (522.5KB, pdf)