Abstract
Introduction
Temporomandibular disorders (TMDs) are abnormalities affecting the temporomandibular joint, jaw muscles, or both. An intrinsic relationship reportedly exists between TMDs and psychosocial factors, including stress. Parafunctional habits such as bruxism and clenching are also known to be responsible for TMDs.
Objective
To determine the association of anxiety, depression, and bruxism with TMD symptoms and their relationship with age and sex.
Methods
Patients included in the study reported, as their chief concern, pain lasting for more than a week in the temporomandibular joint area and/or masticatory muscles. The patients were divided into age groups as follows: Younger than 20 years, 21 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, and above 60 years. Patients were examined clinically and were asked to complete an anamnestic questionnaire (modified version of Helkimo Anamnestic Index) and the Hospital Anxiety and Depression Scale (HADS).
Results
Seventy-five patients (55 women, 20 men) were included in the study. The prevalence of TMDs was higher in female patients, of whom 33 (60%) had moderate to severe TMDs. Of the 20 male patients, 12 (60%) had signs and symptoms of moderate TMDs. Anxiety and depression scores were higher in female patients. No significant correlation was found between degree of malocclusion and TMDs.
Discussion
We found correlations between the degree of TMD with age, sex, parafunctional habits, and psychosocial factors. Symptoms of TMD seemed to increase in patients with parafunctional habits, from younger to older age groups, and with increased anxiety and depression scores.
Conclusion
The degree of TMDs is higher in women, and TMDs are associated with higher anxiety and depression scores. Correlation between these factors paves the way for preventive actions aimed at those with moderate and severe signs of TMDs.
Keywords: Hospital Anxiety and Depression Scale, parafunctional habits, psychosocial factors, temporomandibular disorder
INTRODUCTION
Temporomandibular disorders (TMDs) are a group of abnormalities affecting the temporomandibular joint (TMJ), jaw muscles, or both. Pain, malocclusion, deviated mouth opening, limited jaw function, and headache are some of the most commonly noticed signs and symptoms of TMDs. A multifactorial etiology of pain and dysfunction resulting from biopsychosocial factors has been proposed.1–3 Alteration of form can cause changes in the stomatognathic system, eventually leading to malocclusion, which is recognized as one of the primary causes of TMDs. Several authors have studied the different types of malocclusion, including posterior crossbite, anterior open bite, and horizontal and vertical overlap. The authors have concluded that these changes can cause various degrees of TMD symptoms.4,5 Approximately 1.5 to 2 times more common in women than in men, TMDs are most prevalent in the 20- to 40-year age group and are least common in children and elderly individuals.
Various studies have provided an irrefutable evidence of a significantly appreciable relationship between bruxism and TMDs.6–8 A clear and decisive relationship was found between TMDs and bruxism in a case-control study conducted by Molina et al.6 In a study done by Michelotti et al,7 a habit such as sustained contact between the teeth was seen to be an important risk factor in triggering myofascial pain. Kanehira et al8 concluded that stress is an important factor and is intimately connected with parafunctional habits such as bruxism during sleep and daytime clenching. Considering the complexity of TMDs involving psychosocial factors and parafunctional habits, our study was undertaken to determine the association of anxiety, depression, and bruxism with TMD symptoms and their correlation with age and sex.
METHODS
Patients
This cross-sectional study was conducted in patients reporting to the Department of Oral Medicine and Radiology, Manipal College of Dental Sciences, Mangalore, India. Ethical clearance was obtained from the institutional ethical committee (MCODSMLR/2017.1414).
Patients with pain lasting for 1 week or more in the TMJ region and/or the masticatory muscle and absence of any systemic conditions were included in the study. The exclusion criteria were as follows:
History of trauma or congenital abnormalities to the TMJ
Odontogenic infections or any other pathologic swellings in relation to the TMJ
Metastatic tumors, cysts, or carcinomas of the oral cavity affecting the TMJ
Regular intake of medicines such as analgesics or antianxiety drugs.
With a 95% confidence level and 80% power, the sample size was estimated to be 75.a
Procedures
The study participants were asked to fill out an anamnestic questionnaire containing 10 questions (a modified version of the Helkimo Anamnestic Index) consisting of TMD symptom-related questions (see Sidebar: Anamnestic Questionnaire), which was validated by a professor in the Department of Community Medicine, Kasturba Medical College, Mangalore. The participants were later asked to complete the Hospital Anxiety and Depression Scale (HADS) questionnaire (developed by Zigmond and Snaith9 in 1983), consisting of 14 questions, equally distributed for anxiety and depression.
Anamnestic Questionnaire1.
Q1) Do you have difficulty in opening your mouth? Yes/no
Q2) Do you have difficulty in moving or using your jaw? Yes/no
Q3) Do you have tenderness or muscular pain when chewing? Yes/no
Q4) Do you have frequent headaches? Yes/no
Q5) Do you have neck aches or shoulder pain? Yes/no
Q6) Do you have pain in or about the ears? Yes/no
Q7) Are you aware of noises in the jaw joints? Yes/no
Q8) Do you consider your bite “normal”? Yes/no
Q9) Do you use only one side of your mouth when chewing? Yes/no
Q10) Do you have morning facial pain? Yes/no
References
- 1.Conti A, Freitas M, Conti P, Henriques J, Janson G. Relationship between signs and symptoms of temporomandibular disorders and orthodontic treatment: A cross-sectional study. Angle Orthod. 2003 Aug;73(4):411–417. doi: 10.1043/0003-3219(2003)073<0411:RBSASO>2.0.CO;2. DOI: https://10.1043/0003-3219(2003)073<0411:RBSASO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
The patients were then examined clinically and the findings, especially the hard-tissue findings (for parafunctional habits), were recorded in a case history pro forma. Palpation of the muscles of mastication was done using the 2014 Diagnostic Criteria for Temporomandibular Disorders (DC/TMD),10 followed by a thorough examination of the TMJ.
Two investigators participated in the study. The first investigator (UY) performed the clinical examination of patients and evaluation of the modified anamnestic questionnaires, and the second investigator (JA) evaluated anxiety and depression using the HADS questionnaire in the Department of Psychiatry, KMC Hospital, Attavar, Mangalore. Both investigators were unaware of each other’s findings.
Data Analysis
Association of the role of bruxism with the severity of TMD cases was performed using χ2 test.
Simple linear regression analysis to predict the TMD score with the variables of age, sex, bruxism, anxiety and depression was conducted to derive the equation.
RESULTS
A total of 75 patients who reported with a chief complaint of pain in the TMJ region were included in the study; 55 patients (80%) were women and 20 (20%) were men. Of these 75 patients, 63 (84%) had Angle class 1 malocclusion and the remaining 12 (16%) had Angle class 2 malocclusion (Table 1).
Table 1.
Distribution of participants with temporomandibular disorder (TMD) by age, sex, Malocclusion, bruxism, and anxiety and depression scores
| Variable | TMD free, no. (%) | Mild TMD, no. (%) | Moderate TMD, no. (%) | Severe TMD, no. (%) | Chi square value | p valuea |
|---|---|---|---|---|---|---|
| Age, y | ||||||
| ≤ 20 | 1 (33.3) | 4 (14.8) | 8 (23.5) | 1 (9.1) | 16.3 | 0.365 |
| 21–30 | 1 (33.3) | 15 (55.6) | 13 (38.2) | 2 (18.2) | ||
| 31–40 | 0 (0) | 4 (14.8) | 6 (17.6) | 2 (18.2) | ||
| 41–50 | 0 (0) | 1 (3.7) | 3 (8.8) | 3 (27.3) | ||
| 51–60 | 1 (33.3) | 1 (3.7) | 4 (11.8) | 2 (18.2) | ||
| > 60 | 0 (0) | 2 (7.4) | 0 (0) | 1 (9.1) | ||
| Sex | ||||||
| Female | 2 (66.7) | 21 (77.8) | 22 (64.7) | 10 (90.9) | 3.3 | 0.338 |
| Male | 1 (33.3) | 6 (22.2) | 12 (35.3) | 1 (9.1) | ||
| Occlusion | ||||||
| Class 1 | 2 (66.7) | 23 (85.2) | 29 (85.3) | 11 (100) | 2.8 | 0.417 |
| Class 2 | 1 (33.3) | 4 (14.8) | 5 (14.7) | 0 (0) | ||
| Bruxism | ||||||
| Absent | 0 (0) | 19 (70.4) | 12 (35.3) | 1 (9.1) | 16.5 | 0.001 |
| Present | 3 (100) | 8 (29.6) | 22 (64.7) | 10 (90.9) | ||
| Anxiety score | ||||||
| Normal | 2 (66.7) | 17 (63) | 13 (38.2) | 3 (27.3) | 9.9 | 0.354 |
| Mild | 0 (0) | 2 (7.4) | 11 (32.4) | 4 (36.4) | ||
| Moderate | 1 (33.3) | 7 (25.9) | 9 (26.5) | 3 (27.3) | ||
| Severe | 0 (0) | 1 (3.7) | 1 (2.9) | 1 (9.1) | ||
| Depression score | ||||||
| Normal | 1 (33.3) | 21 (77.8) | 22 (64.7) | 7 (63.6) | 8.2 | 0.221 |
| Mild | 2 (66.7) | 5 (18.5) | 11 (32.4) | 2 (18.2) | ||
| Moderate | 0 (0) | 1 (3.7) | 1 (2.9) | 2 (18.2) | ||
| Severe | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
Boldface indicates significant.
The patients were divided into 6 groups by age as follows: 1) 20 years and younger, 2) 21 to 30 years, 3) 31 to 40 years, 4) 41 to 50 years, 5) 51 to 60 years, and 6) more than 60 years.
According to the DC/TMD criteria,10 patients were categorized into these 4 subgroups:
Mild TMD: Mild myofascial pain, recurring in nature
Moderate TMD: An intra-articular mechanical disturbance that interfered with a joint’s smooth action
Severe TMD: Signs and symptoms of arthralgia and arthritis (clinically evident joint pain with inflammation or swelling)
TMD free: Only occasional pain with a duration of less than 1 year.
Bruxism was most prevalent among women aged 21 to 30 years and 31 to 40 years (Table 1). Of 11 patients who had a diagnosis of severe TMD, 10 had bruxism, a significant finding (p = 0.001; Table 1). Our study findings revealed that the degree of TMDs increased from the youngest group to the oldest group and was significant (p = 0.04; Table 2).
Table 2.
Correlation of degree of temporomandibular disorder (TMDs) with age, sex, bruxism, anxiety, and depression
| Model 1 | Unstandardized coefficientsa | Standardized coefficients,a β | t | p valueb | 95% Confidence interval for B | ||
|---|---|---|---|---|---|---|---|
| B | Standard error | Lower bound | Upper bound | ||||
| (Constant) | 7.482 | 1.869 | 4.003 | <0.001 | 3.754 | 11.211 | |
| Age | 0.747 | 0.357 | 0.256 | 2.093 | 0.040 | 0.035 | 1.459 |
| Sex | −0.608 | 1.039 | −0.067 | −0.585 | 0.561 | −2.680 | 1.465 |
| Bruxism | 2.335 | 0.927 | 0.286 | 2.519 | 0.014 | 0.486 | 4.184 |
| Anxiety | 0.086 | 0.144 | 0.081 | 0.595 | 0.554 | −0.202 | 0.373 |
| Depression | −0.116 | 0.172 | −0.094 | −0.672 | 0.504 | −0.460 | 0.228 |
Dependent variable: TMD Score = 7.482 + 0.747 (Age) − 0.608 (Sex [male 2, female 1]) + 2.335 (Bruxism 1, 0) + 0.086 (Anxiety) − 0.116 (Depression)
Boldface indicates significant.
In the present study, female participants had an increased degree of TMDs compared with male participants (Table 1).
Results for the anxiety and depression score revealed higher scores among the 21- to 30-year age group vs other age groups and an increased rate of prevalence among female patients compared with male patients (Table 1).
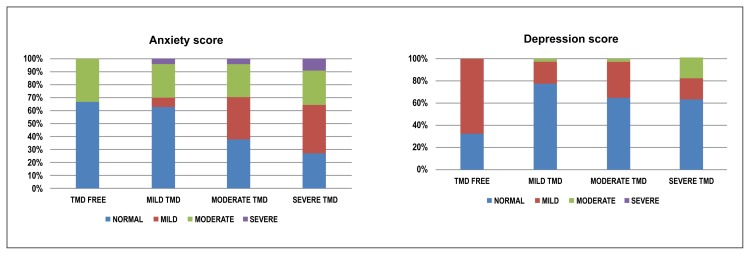
In our study, patients with TMDs showed moderate depression scores, notably seen among women in the age group of 31 to 40 years. In the severe TMD group, 12 patients had raised HADS scores and 10 had normal HADS scores, which was a clinically significant finding but not statistically significant (Figure 1).
Figure 1.
Correlation of degree of temporomandibular disorders with anxiety and depression score.
Linear regression analysis was conducted to derive a formula to calculate the TMD score as follows:
where the score for male sex = 2 and for female sex = 1, and the score for having bruxism = 0, and no bruxism = 1.
DISCUSSION
TMDs are distinctively identified as a triad of clinically apparent signs and symptoms that include muscle and/or TMJ pain, TMJ sounds, and restriction and deviation of the mouth in its opening path.11
The prevalence of TMD is debatable, owing to the lack of uniformity in the diagnostic criteria adapted by various investigators. Evidence toward an increasing prevalence of TMD signs and symptoms in the general population has been noted in several studies. Because of the dissimilar clinical criteria used among various studies, there appears to be an irregularity in the literature regarding the prevalence of clinical signs and symptoms. Studies have suggested that between 1% and 75% of the population showed at least 1 objective TMD sign, and 5% to 33% reported subjective symptoms.12
A peak incidence for TMD symptoms was recorded between age 20 and 40 years, with a lower incidence seen in younger or elderly patients.13 Graff-Radford et al,14 in a 1989 study, found that patients had TMDs prevalent at ages 21 to 30 years followed by above 50 years. In the present study, among 75 patients aged between 0 and 70 years, it was noted that 80% of the patients had TMDs, and most of these patients were in the 21- to 30-year group followed by 20 years of age or younger.
Esposito et al15 reviewed records of 425 consecutive patients having TMDs. They concluded that TMD primarily affects women, because more than 84% of those affected were women. Bonjardim et al16 conducted a study in 217 patients and found that women were more commonly affected by TMDs. In the present study, we found that 73.3% of patients having signs and symptoms of TMDs were women. According to a study by Syed et al17 in 2012, women were seen to have higher degree of TMDs, attributed to higher anxiety and depression scores with the habit of bruxism. The authors state that because bruxism results in overuse of masticatory muscles, it can eventually lead to a higher possibility of developing TMDs.17 In the our study, with an increase in anxiety score, it was noticed that the degree of TMDs also increased.
The results of our study reinforce the assumption that there is an association between TMD and bruxism. Although the association between psychological factors and TMD is inconsistent in the literature, there is biological plausibility for this association in our study.
Bonjardim et al18 conducted a study in 196 young adults in which 101 were women and 95 were men. They noted that participants who had moderate or severe TMD exhibited class 1 malocclusion, which was seen to be nonsignificant.18 Similar findings were observed in our study, wherein the patients with class 1 malocclusion had moderate to severe TMD symptoms but the results were nonsignificant.
Wieckiewicz et al19 conducted a study in 456 Polish university students to assess the occurrence of TMDs and parafunctional habits and their correlation with psychological and emotional factors. Symptoms of TMDs were noticed in 246 students. A total of 164 female students were found to have TMDs, anxiety, and depression. The authors observed a significant correlation between TMD and psychological problems. The incidence of TMD symptoms was seen to be higher in women, and emotional issues appeared to be an important predisposing factor for the occurrence of muscular disorders.19
In our study, we found that 73.3% of patients with TMD diagnosis were female. Bruxism was more common in female patients than in male patients. Hence, female patients appeared to have higher chances of TMDs compared with male patients. Anxiety and depression scores were seen to be higher in women with signs and symptoms of TMDs. Hence, the degree of TMDs appeared to be higher in female patients with a bruxism habit and high anxiety and depression scores.
In our study we found a correlation between the degree of TMD with age, sex, bruxism, anxiety, and depression. The degree of TMD increases from younger to older age groups and is significant. Additionally, women have increased intensity of TMDs, and the degree of TMD significantly increases in patients with the habit of bruxism. Finally, patients having increased anxiety and depression scores appear to be more susceptible to an increased degree of TMD.
The most important stage of a treatment protocol in TMD is education about the habit of bruxism among patients with such parafunctional habits and the start of relaxation therapy. It is important to explain to the patient the background of the disorders, especially the role of one’s emotional stress, and to prescribe counseling and behavioral therapy to reduce anxiety.20
As explained in the Results section, we performed linear regression analysis to derive a formula to calculate the TMD score using the variables age, sex, bruxism, anxiety, and depression. Association of the prediction of the TMD score with the variables showed a significant association with age (p = 0.040) and bruxism (p = 0.014) with anxiety and depression. However sex did not appear to play a significant role. In a study by Montero-Martín et al,21 clinical variables of pain duration and pain interference with activities of daily living, as well as the biopsychosocial variables of depression and jaw disability were used to calculate the TMD score. All the variables they used to calculate the TMD score were significant in their regression model.
CONCLUSION
The present study revealed that the degree of TMDs is higher in the female population and increases from younger to older age groups. The correlation between malocclusion and degree of TMD is not significant, but the parafunctional habit of bruxism is significantly associated with a higher degree of TMD symptoms. Anxiety and depression scores are higher in women, and the degree of TMDs, especially in women, increases with the increase in anxiety and depression scores. The existing correlation between these factors paves the way for preventive actions aimed at those with moderate and severe signs of TMD. An interdisciplinary approach should be created for this population to reduce parafunctional habits and TMDs.
Acknowledgments
Kathleen Louden, ELS, of Louden Health Communications performed a primary copy edit.
Footnotes
Using the formula n = Zα2 p q/E2, where Zα = 95% confidence level, p = Proportion from reference, q = 100 − p, and E = 20/100 × p.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.LeResche L. Epidemiology of temporomandibular disorders: Implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997;8(3):291–305. doi: 10.1177/10454411970080030401. [DOI] [PubMed] [Google Scholar]
- 2.Weinberg LA. Temporomandibular dysfunctional profile: A patient-oriented approach. J Prosthet Dent. 1974 Sep;32(3):312–25. doi: 10.1016/0022-3913(74)90036-5. [DOI] [PubMed] [Google Scholar]
- 3.Oral K, Bal Küçük B, Ebeoğlu B, Dinçer S. Etiology of temporomandibular disorder pain. Agri. 2009 Jul;21(3):89–94. [PubMed] [Google Scholar]
- 4.Bonjardim LR, Lopes-Filho RJ, Amado G, Albuquerque RL, Jr, Goncalves SR.Association between symptoms of temporomandibular disorders and gender, morphological occlusion, and psychological factors in a group of university students Indian J Dent Res 2009. April–June202190–4. 10.4103/0970-9290.52901 [DOI] [PubMed] [Google Scholar]
- 5.Valle-Corotti K, Pinzan A, do Valle CV, Nahás AC, Corotti MV. Assessment of temporomandibular disorder and occlusion in treated class III malocclusion patients. J Appl Oral Sci. 2007 Apr;15(2):110–4. doi: 10.1590/S1678-77572007000200007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Molina OF, dos Santos J, Jr, Nelson SJ, Grossman E. Prevalence of modalities of headaches and bruxism among patients with craniomandibular disorder. Cranio. 1997 Oct;15(4):314–25. doi: 10.1080/08869634.1997.11746026. [DOI] [PubMed] [Google Scholar]
- 7.Michelotti A, Cioffi I, Festa P, Scala G, Farella M. Oral parafunctions as risk factors for diagnostic TMD subgroups. J Oral Rehabil. 2010 Mar;37(3):157–62. doi: 10.1111/j.1365-2842.2009.02033.x. [DOI] [PubMed] [Google Scholar]
- 8.Kanehira H, Agariguchi A, Kato H, Yoshimine S, Inoue H. Association between stress and temporomandibular disorder. Nippon Hotetsu Shika Gakkai Zasshi. 2008 Jul;52(3):375–80. doi: 10.2186/jjps.52.375. [DOI] [PubMed] [Google Scholar]
- 9.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983 Jun;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 10.Schiffman E, Ohrbach R, Truelove E, et al. International RDC/TMD Consortium Network, International Association for Dental Research, Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 2014 Winter;28(1):6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fricton JR, Schiffmann EL. Epidemiology of temporomandibular disorders. In: Fricton JR, Dubner R, editors. Orofacial pain and temporomandibular disorders. New York, NY: Raven; 1995. pp. 295–303. [Google Scholar]
- 12.De Kanter RJ, Truin GJ, Burgersdijk RC, et al. Prevalence in the Dutch adult population and a meta-analysis of signs and symptoms of temporomandibular disorder. J Dent Res. 1993 Nov;72(11):1509–18. doi: 10.1177/00220345930720110901. [DOI] [PubMed] [Google Scholar]
- 13.Anastassaki Köhler A, Hugoson A, Magnusson T. Prevalence of symptoms indicative of temporomandibular disorders in adults: Cross-sectional epidemiological investigations covering two decades. Acta Odontol Scand. 2012 May;70(3):213–23. doi: 10.3109/00016357.2011.634832. [DOI] [PubMed] [Google Scholar]
- 14.Graff-Radford SB, Reeves JL, Baker RL, Chiu D. Effects of transcutaneous electrical nerve stimulation on myofascial pain and trigger point sensitivity. Pain. 1989 Apr;37(1):1–5. doi: 10.1016/0304-3959(89)90146-2. [DOI] [PubMed] [Google Scholar]
- 15.Esposito CJ, Panucci PJ, Farman AG. Associations in 425 patients having temporomandibular disorders. J Ky Med Assoc. 2000 May;98(5):213–5. [PubMed] [Google Scholar]
- 16.Bonjardim LR, Garião MB, Pereira LJ, Castelo PM.Anxiety and depression in adolescence and their relationship with signs and symptoms of temporomandibular disorders Int J Prosthodont 2005. July–August184347–52. [PubMed] [Google Scholar]
- 17.Syed RA, Syeda AR, Katti G, Arora V.Prevalence of temporomandibular joint disorders in outpatients at Al-Badar Dental College and Hospital and its relationship to age, gender, occlusion and psychological factors J Indian Acad Oral Med Radiol 2012. October–December244261–8. [Google Scholar]
- 18.Bonjardim LR, Lopes-Filho RJ, Amado G, Albuquerque RL, Jr, Gonçalves SR.Association between symptoms of temporomandibular disorders and gender, morphological occlusion, and psychological factors in a group of university students Indian J Dent Res 2009. April–June202190–4. 10.4103/0970-9290.52901 [DOI] [PubMed] [Google Scholar]
- 19.Wieckiewicz M, Grychowska N, Wojciechowski K, et al. Prevalence and correlation between TMD based on RDC/TMD diagnoses, oral parafunctions and psychoemotional stress in Polish university students. Biomed Res Int. 2014;2014 doi: 10.1155/2014/472346. 472346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freesmeyer WB, Fussnegger MR, Ahlers MO. Diagnostic and therapeutic-restorative procedures for masticatory dysfunctions. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2005;4 Doc19. [PMC free article] [PubMed] [Google Scholar]
- 21.Montero-Martín J, Bravo-Pérez M, Albaladejo-Martínez A, Hernández-Martín LA, Rosel-Gallardo EM. Validation the Oral Health Impact Profile (OHIP-14sp) for adults in Spain. Med Oral Patol Oral Cir Bucal. 2009 Jan 1;14(1):E44–50. [PubMed] [Google Scholar]