Abstract
Effective communication, where all parties share a common understanding, is necessary to realize the promise of Genomic Medicine. It is especially salient given the imperative to increase the participation of diverse populations in genomics research and to expand the reach of clinical genomics. We have previously shown that cancer genetic counseling is suboptimal for patients with limited health literacy. To address this finding, we implemented a pilot study to improve verbal communication between genetic counselors and their patients of limited health literacy that consisted of: i) curriculum development and delivery of a Genetic Counselors (GC) communication workshop; ii) two-month post-workshop interviews with GC participants (n = 9); iii) observations/audio recordings of counseling sessions involving 24 patients and two GC workshop participants; iv) post-counseling interviews with patients (n = 9). The 4.5-h workshop presented evidenced-based principles and strategies for effective communication with limited health literacy patients (e.g. use of plain language and teach-back), and offered specific techniques and exercises to practice adoption of such practices in the genetic counseling context. GCs expressed appreciation for the opportunity to refine their skills; however, they reported that some strategies were challenging given their professional training and communication habits. For example, GCs were concerned that use of plain language could undermine efforts to obtain informed consent and provide scientifically accurate information. Observations and patient interviews after the workshop revealed that GCs were able to employ the communication strategies with positive effects, with patients indicating sufficient understanding of the genetic test and its implications as well as satisfaction with the counselors’ communication. While derived from research on communication with those of limited health literacy, the communication approaches taught in the GC workshop could benefit most patients, given the high rates of low health literacy in many countries, and the many factors beyond health literacy that can contribute to reduced comprehension in health care environments.
Keywords: Health literacy, Genomic literacy, Patient-provider communication, Practice guidelines, Psychosocial counseling, Health disparities
1. Introduction
Genetic testing and genomic sequencing have become standard components of cancer care across the continuum from screening and prevention to treatment and survivorship. Insurance coverage for hereditary cancer services has expanded and sequencing costs have declined, making such services more accessible. Yet access alone is not sufficient to ensure quality of care and equity in genomic medicine. The 2013 National Human Genome Research Institute report on the status of genomics literacy in the US, and other studies, have found genomic health literacy to be lacking in the US population (Hurle et al., 2013 and references therein). Genomic health literacy, based on the Institute of Medicine definition of health literacy, is “the capacity to obtain, process, understand, and use genomic information for health-related decision-making” (Ratzan and Parker, 2000 p. vi). It includes oral, print, numeracy and cultural/conceptual domains (Nielsen Bohlman et al., 2004). While a recent study found that limited health literacy (LHL) was associated with lower genetic knowledge (Kaphingst et al., 2016), experts have not come to a common understanding of the specific information needed for genomic literacy. Rather, the focus has been on the ability to use genomic information for appropriate decision-making (Ratzan and Parker, 2000).
Gaps in effective communication (where all parties share a common understanding) are widely recognized as a major contributor to health disparities (US DHHS, 2010). Individuals with limited health literacy (LHL – fully one-third of US adults (Goodman et al., 2013; Nielsen-Bohlman et al., 2004) are less likely to actively participate in health care decision-making discussions and more likely to struggle with health management tasks, such as navigating the health care system (Martin and Parker, 2011). Poor health literacy is a stronger independent predictor of a person’s health than age, income, employment status, education level, and race/ethnicity (Berkman et al., 2011; Weiss et al., 2005). At the same time, health and genomic literacy is not simply a reflection of individual capacity or lack thereof, but rather a manifestation of the demands and complexities that the health care system places on people who use it (Archer et al., 2015; Brach et al., 2012; Shim, 2010).
Researchers and healthcare practitioners have begun to explore new models of genetic counseling due to the shortage of genetic counselors, the increasing demand for their services, and the growing complexity of testing brought about by genome and exome sequencing (Bradbury et al., 2015; Hooker et al., 2014). Some have called for a shift away from a ‘teaching model of counseling’ toward a ‘psychosocial model’ (Biesecker et al., 2017; Meiser et al., 2008). A few studies indicate that culturally tailored communication may increase awareness of genetic risk, satisfaction (Charles et al., 2006), and communication effectiveness (Barlow-Stewart et al., 2006). Other studies have identified communication practices that impede effective genetic counseling communication, such as non-directiveness, jargon, and complex risk information (Browner et al., 2003; Cheng et al., 2017; Eichmeyer et al., 2005; Joseph et al., 2017; Kamara et al., 2018; Penchaszadeh, 2001; Rapp, 1993). A systematic review of communication interventions in clinical genetics showed that emotionally supportive elements of counseling were more beneficial than information alone (Edwards et al., 2008). Uncertainty in genomics has been identified as an area particularly difficult to communicate (Himes et al., 2016; Solomon et al., 2017). Relatively little observational or interventional research has been conducted on the communication of genetic counselors (GCs) with underserved patients (Ellington et al., 2007; Erby et al., 2007; Lea et al., 2011; Roter et al., 2007), or on the potential of communication barriers to reinforce or exacerbate documented disparities in the translation of genomic medicine (Butrick et al., 2015; Cragun et al., 2015; Mai et al., 2014; Walcott et al., 2014). A recent landscape review of research on communication related to cancer genetic testing identified the need for more research that includes minority and medically underserved populations, accounts for health literacy, and explores patient, provider and system level factors in genetics communication (Peterson et al., 2018).
Our study of communication between GCs and their hereditary cancer risk counseling patients in public “safety net” hospitals assessed communication effectiveness from the patients’ perspectives (Cheng et al., 2017; Joseph et al., 2017; Kamara et al., 2018; Lara-Otero et al., 2018). Through observations of 170 genetic counseling sessions with English, Spanish and Chinese-speaking patients in public hospitals and in-depth interviews with both patients and counselors, we identified a fundamental mismatch between the information provided by the GCs and the information that patients desired, deemed useful, and understood. Components of GC-patient communication that contributed to this mismatch included GCs’ provision of too much information; GCs’ use of complex terminology and conceptually difficult information; patient perception of information as not relevant; and discussions of screening and prevention recommendations that were overly vague (Joseph et al., 2017). These characteristics of the communication appeared to inhibit patient engagement and question-asking, further deepening the disconnect. Based on these results, we developed the pilot intervention described here, with the goal of providing GCs with specific strategies and techniques for more effective communication.
2. Methods
This multi-method pilot study consisted of four components: i) curriculum development and delivery of a GC communication workshop; ii) two-month post workshop interviews with GC participants; iii) observations/audio recordings of counseling sessions with trained GCs and their patients undergoing counseling for risk of hereditary cancer; iv) post-counseling interviews with patients. All study protocols were approved by the IRBs of the participating institutions.
2.1. GC communication workshop
We developed a 4.5-h communication workshop for GCs with three learning objectives: 1) to convey key evidence-based strategies for effective communication with LHL patients; 2) to explain evidence-based strategies for effective risk communication with LHL patients; and 3) to adapt these strategies to the GC context and practice applying them to facilitate patient engagement and comprehension. The curriculum was designed by co-authors with expertise in public health communication (RP), communication with patients of limited health literacy (DS) and genetic counseling communication (GJ). The workshop was delivered by RP and GJ.
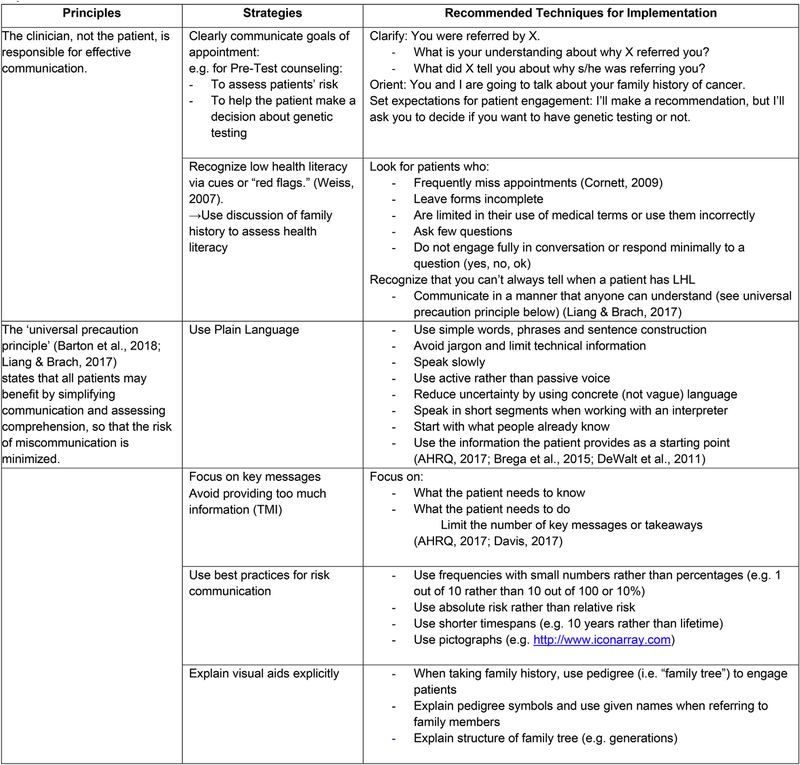
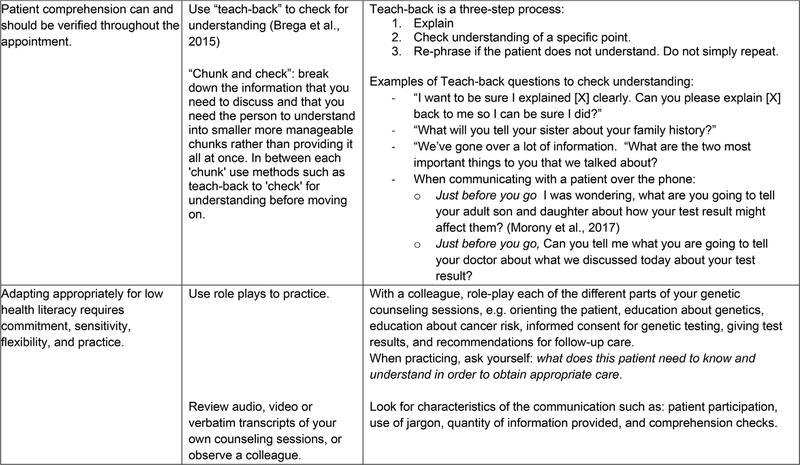
The workshop curriculum consisted of: i. background on the LHL and numeracy skills of the US population, findings from our prior study (Joseph et al., 2017), and information on the growing availability of genetic counseling/testing for diverse, low socioeconomic status (SES) populations in the US; ii. evidenced-based principles and strategies for effective communication with LHL patients developed through research in other fields of medicine, along with techniques and examples of how to implement them in the genetic counseling context (Fig. 1); and iii. exercises and role plays (e.g. providing a plain language explanation of genetics) designed for GCs to practice the strategies and techniques.
Fig. 1.
Evidence-based principles and strategies for effective communication with LHL patients, and recommended techniques for implementation.
The workshop was audio-recorded. At the end of the workshop, participants were asked to complete a questionnaire, which included demographic questions and an evaluation of the utility and perceived applicability of the communication principles and strategies, the value of the role-play exercises, and the novelty and clarity of the training content. We then asked participants to apply the communication strategies taught in the workshop in their regular clinical practice, and invited them to participate in telephone interviews two months later to discuss their experiences.
We invited all 10 counselors who had been observed during our prior study to attend the workshop and related activities. Of these, 4 attended. Five additional counselors who had either been invited by one of the original 10, or had expressed interest in the study through professional networks also participated. The 9 participating GCs received a $100 gift card in appreciation of their time and effort.
2.2. GC interviews
Interviews were conducted by phone, lasted 30–45 min and covered topics such as: the perceived relevance of the training for GCs’ daily practice; techniques used or considered; and experience with implementing the techniques.
2.3. Observations of counseling sessions
After the GC interviews were completed, and GCs had had an opportunity to practice the strategies, we observed 24 patients undergo pre-test genetic counseling with two participating counselors (11 with GC7 and 13 with GC4) from one of the prior study’s collaborating public hospitals. Observations and post-counseling patient interviews followed the same protocol as the prior study (Joseph et al., 2017). All English-, Spanish- and Chinese-speaking patients who had appointments when a language concordant researcher was available were eligible for inclusion in the study. Except for the occasions when a patient asked not to be recorded (n = 3), the researcher directly observed and audio-recorded patient-genetic counselor pre-test appointments (n = 24). For the 3 patients who preferred not to be recorded, the researcher took detailed field notes.
2.4. Patient interviews
We interviewed 9 patients (3 each in Spanish, Cantonese and English), all of whom had been offered testing and had been recorded (4 were counseled by the first GC, 5 by the second). As in the prior study, we used the audio recordings to stimulate recall and probe specific aspects of the communication (Lyle, 2013; O’Brien et al., 2008).
2.5. Data analysis
To analyze the workshop discussions, we listened to the audio recording and took notes to summarize significant points of discussion. After analysis of the GC telephone interviews, select sections of the workshop discussion related to the emerging themes were transcribed for further analysis.
All qualitative interviews with GCs, as well as post-visit interviews for the 9 patients, were digitally recorded, professionally transcribed, and translated if needed. Atlas ti 8.0 qualitative analysis software was used to code and analyze all transcripts. Three members of the research team read and independently coded each set of transcripts (GC interviews, patient interviews and appointments) using a combination of open coding, codes established in the prior study, and codes related to the communication strategies covered in the workshop. Three members of the research team (PI and two research assistants) met regularly to discuss and reconcile coding of the first few transcripts of each data set to develop a codebook. We continued to meet regularly to reconcile differences in subsequent coding and to identify the themes presented here.
3. Results
3.1. Participants
Tables 1 and 2, respectively, present characteristics of GCs who participated in the workshop and follow-up interviews, and of the observed and interviewed patients. GC participants estimated the percentage of their patient population who were of LHL to be between 5% and 85%, with the majority (5 out of 9) estimating the percentage to be between 60% and 85%.
Table 1.
Genetic counselor characteristics (N = 9).
| Age, range mean (SD) | 29–61 38.7 (11.89) |
|---|---|
| Race, n | |
| Asian | 1 |
| White | 7 |
| Black/African American | 1 |
| Education, n | |
| Master's of Science, Genetic Counseling | 8 |
| NP with advanced training in genetics | 1 |
| Practicing as genetic counselor, range in years | .5–31 |
| Practice Setting n | |
| Private (non-profit) hospital or health care system | 4 |
| Academic medical center and public/county hospital | 2 |
| Public/county hospital | 2 |
| For-profit testing company | 1 |
| Perceived proportion of low health literacy patients in | 5–10%-85% |
| practice, range mean (SD) | 55.55 (29.1) |
| Use of medical interpreter during practice, range in % | 0–50 |
Table 2.
Demographic characteristics of patient interview sample by Language (N = 9).
| English (n = 3) | Spanish (n = 3) | Chinese (n = 3) | Total (n = 9) | |
|---|---|---|---|---|
| Age, Mean (SD) | 33 (5.67) | 46.33 (8.73) | 49.66 (15.56) | 43 (12.06) |
| Marital status, n | ||||
| Married/with a long-term partner | 1 | 2 | 3 | 6 |
| Never married | 0 | 0 | 0 | 0 |
| Legally separated or Divorced | 2 | 1 | 0 | 3 |
| Highest level of education, n | ||||
| Less than high school | 0 | 3 | 1 | 4 |
| High school or equivalent | 1 | 0 | 1 | 2 |
| Some college or higher | 2 | 0 | 1 | 3 |
| Race/ethnicity, n | ||||
| aAsian | 1 | 0 | 3 | 4 |
| Hispanic/Latino | 0 | 3 | 0 | 3 |
| White | 2 | 0 | 0 | 2 |
| Years in the U.S. | ||||
| Range | 11–39 | 20–33 | 3–16 | 3–39 |
| Mean | 26 | 24.33 | 11.5 | 20.61 |
| Language(s) Spoken at home, n | ||||
| bOnly non-English | 0 | 2 | 1 | 3 |
| More non-English language than English | 0 | 1 | 0 | 1 |
| Both equally | 0 | 0 | 2 | 2 |
| More English than non-English language | 1 | 0 | 0 | 1 |
| Only English | 2 | 0 | 0 | 2 |
| Preferred Language with your doctor and nurses, n | ||||
| English | 3 | 0 | 0 | 3 |
| Spanish | 0 | 2 | 0 | 2 |
| Cantonese/Mandarin | 0 | 0 | 2 | 2 |
| Combination | 0 | 1 | 1 | 2 |
“Asian” includes 3 Chinese and 1 Filipino/Black.
“Only Non-English” includes 1 Hoi Ping Cantonese and 2 Spanish.
Patient participants were diverse not only in terms of educational level, but also in terms of their prior knowledge of hereditary cancer and reasons for seeking genetic counseling. Two participants sought counseling because they had close relatives with BRCA mutations, whereas others had no prior knowledge of hereditary cancer and had been referred to genetic counseling by a clinician with little or no explanation as to why (by patient report).
Eight of the nine GC participants completed the post-workshop evaluations. Participants indicated overall satisfaction with the workshop content: 75% found all of the information in the workshop to be useful. For a majority, at least half of the material covered was new; 75% or more of participants found each of the exercises and two of the three role-plays very useful. All participants found the information to be very clearly presented. More than one-third of participants indicated that having more time to practice the techniques would increase the likelihood that they would use them in daily practice.
3.2. Qualitative interview and observation themes
Analysis of the GC interviews indicated that all but one participating GC recognized the need for LHL strategies among their own patient populations and were eager to communicate more effectively. Several indicated that they often could sense that patients were not understanding (e.g. they could see eyes glazing over); however, they did not know what to do differently. Further, GCs noted the difficulty in breaking old habits, and acknowledged that taking up these new strategies would require substantial practice. Some counselors requested more time in future workshops to practice with their peers before attempting to apply the strategies with patients; others pointed out that these approaches differed substantially from how they had been taught to counsel and the basis on which they were evaluated during their graduate training. Despite these challenges, in the 24 genetic counseling sessions we observed the counselors were able to successfully apply many of the strategies we had proposed in the workshop. To illustrate, we present the four themes derived from the multiple forms of data (GC interviews, clinic observations and patient interviews) as they related to key strategies taught in the workshop: (1) Adapting Genetic Counseling for Low Health Literacy; (2) Using Plain Language and Avoiding Too Much Information (TMI); (3) Changing the Balance Between Information/Education and Psychosocial Counseling; (4) Assessing Comprehension and Engaging Patients with Teach-Back.
3.2.1. Adapting Genetic Counseling for Low Health Literacy
3.2.1.1. Recognizing varied health literacy levels
Two months after the workshop, GCs indicated that they were paying more attention to what they perceived their patients’ health literacy levels to be. While some reported treating all patients similarly by assuming low or high health literacy, others looked for cues and adjusted their communication style accordingly. One counselor, who tended to have more highly educated patients, described heightened awareness of her patients’ health literacy in terms of genetic knowledge.
… it’s now the lens that I’m seeing my patient communication through. And so, I’m paying closer attention to some cues around literacy. So, like a really overly simplistic example is that I’ve started noticing that a lot of my patients talk about carrying genes, rather than carrying mutations in genes. … in the last couple of weeks, I’ve had, like, a dozen instances where it was just so clear that people did not understand the fact that they already had the genes that are on the panel and we were testing for mutations or variants in those genes. I think I’ve been more attuned to the fact that basic information about genes and heredity is really hard to understand. That’s why I’ve stopped assuming that people are coming at the process with a basic working knowledge of genetics. (GC1)
After the workshop, this counselor was more aware of both her own assumptions about her patients’ genetics knowledge and of common misunderstandings, even among patients she perceived as highly educated. Other counselors recalled the idea discussed in the workshop that all patients could benefit from clear communication, and acknowledged that even highly educated individuals could have knowledge gaps and could therefore benefit from LHL communication strategies.
A few GCs indicated that the techniques introduced in the workshop were not relevant to their patients because they were highly educated. In such instances, they described applying these techniques in a case-by-case manner, only using plain language or teach-back if they perceived an individual to be of limited health literacy.
… a lot of my patients that I’m dealing with are engineers and physicians. I have a really highly educated population. But when I’m dealing with a highly-educated individual versus when I’m dealing with patients who English is their second language I’m noticing the terminology that I use. (GC6)
In this instance, the GC conflated a number of characteristics–language, education and health literacy—that may or may not overlap with each other. This comment reflects content presented in the workshop that some populations are more likely to be of lower health literacy than others (including limited English proficient (LEP) patients). This example also illustrates how difficult it can be to identify who is of lower health literacy, highlighting the benefit of using the precautionary principle to avoid assessing health literacy incorrectly or stereotyping. Overall, in their interviews, GCs did not mention using the specific cues we had suggested (e.g. multiple no-shows, forms not filled out; see Fig. 1), but rather focused more on patient characteristics, such as English language proficiency and status as an immigrant.
Another GC, who worked in a public hospital, assumed most patients had LHL and did not perceive much need to try to assess health literacy. She thought patients’ health literacy level became evident very quickly.
Well, not consciously because obviously, our patient population is so low health literacy that in almost all of my cases it’s probably the right thing to do. Whether they are low literacy or high literacy it comes off very, very quickly. It’s not something that I have to pay much mind to. (GC8)
While it was not always possible to observe health literacy assessment as it can be an unspoken cognitive process, we did observe a number of instances in which GCs asked questions to assess the patient’s prior knowledge of genetics, a component of genomic literacy. For example, after explaining why someone would choose to undergo genetic testing, one counselor asked:
GC: Hearing this, or in the conversations you’ve just had with people, is this something that you’ve kind of thought about or, or heard about, about cancer running in the family, or does this all seem kind of new, and ….?
Interpreter: And with respect to what I just mentioned and what you’ve spoken about with other people, that cancer can be hereditary, is this something that you had already considered? Had you heard that before, or is all of this information new to you?
Patient: Well I, I hadn’t had the idea that I could have inherited it because I would have thought, if it were inherited, is that my mother or my grandmother would have had a woman’s cancer. My, since my brother had it, I thought that the kind he had, there wasn’t a possibility that I inherited it.
(Pilot 04-SP; GC4)
This exchange enabled the counselor to elicit the common misconception that women’s cancers can only be inherited from women and men’s cancers only from men. The counselor was then able to correct the misunderstanding about inheritance and to contextualize the patient’s family history and hereditary risk.
In another case, a GC attempted to ascertain her English-speaking patient’s familiarity with certain preventive options by asking if she was familiar with the case of Angelina Jolie, the Hollywood actress who publicly shared her story of undergoing prophylactic surgeries after learning she had a BRCA mutation. The following exchange occurred directly after the GC described some of the enhanced screening available, should the genetic test come back positive:
GC: We do all that [the additional recommended screening] so, in the hopes that if cancer occurs, we catch it at the, at a very early, early stage. Um, so that is something that we would, um, you know recommend at your age if you have a mutation. Some women, I don’t know if you ever read about the Angelina Jolie story. Did you?
Patient: Yeah. Well, not really, but I know she has that too, so …
GC: Right. So, some women, um, decide to get, we think of it as a risk-reducing bilateral mastectomy. So, having their breasts removed as a way of taking away the breast cancer risk. Obviously, that’s a very, that’s a huge …
Patient: Yeah.
GC: … thing to do. And …
Patient: And I’m not Angelina Jolie either.
GC: (laughs)
(Pilot 10-ENG; GC4)
Here the counselor uses “cultural or conceptual knowledge”, another component of health literacy, by leveraging an example from popular media (awareness of Angelina Jolie’s personal history of prophylactic mastectomy) in order to illustrate a complicated decision. The patient responded by saying that she is not Angelina Jolie. The patient’s response is a reminder that while the case of Angelina Jolie may be salient in showing preventive options that people can choose, it is also laden with a specific set of social norms and values as well as perceived or real access to healthcare that do not apply across all social groups.
3.2.2. Using Plain Language and Avoiding Too Much Information (TMI) 3.2.2.1. Challenges
During the workshop, GCs were encouraged to use plain, clear language to explain complex genetic concepts to their patients, and to provide only as much information as the patient needed. Many counselors expressed both in the workshop and the interviews the concern that the LHL strategies conflict with basic National Comprehensive Cancer Network (NCCN) requirements (Daly et al., 2018), and with their graduate training. Many counselors noted the substantial discrepancy between what is taught in GC Masters’ programs and the LHL approach, pointing out requirements to cover complex topics (e.g. how genes are sequenced; how a counselor makes her risk assessment) in detail during clinical rotations. Referring to this material, one GC said during the workshop:
Well, I think that those … are the things that are ingrained in us. They’re in our [graduate] programs. Like, that’s what we role-play. That’s what we get graded on. That’s what we get critiqued on by our supervisors when we’re in clinic.
In their interviews, several counselors referenced a discussion that occurred during the workshop in which they expressed concern that using plain language instead of technical and precise genetics terminology would require sacrificing accuracy.
… something we talked about was sacrificing some accuracy for clarity. And I have a, it’s hard for us to say anything that’s not exactly accurate. … (GC4)
This GC voiced her concern that using alternate plain language to explain genetic concepts would result in providing inaccurate information to her patients, and when probed, indicated that it was an internalized or individual pressure to use the technical language, rather than an external professional pressure or concern about liability. This was a pressure other GCs reported as well.
GCs also expressed concerns about the potential for inconsistencies between how they spoke to a patient and how they documented the clinical encounter. One indicated that while she felt comfortable using different language with the patient than in her chart notes, she tried to “at least touch on” all the topics in the NCCN guidelines listed under Principles of Cancer Risk Assessment and Counseling.
It’s very good … for us to remember what is more anxiety-provoking versus empowering, I think is the bottom line of it. But I think it’s within, all that you said [in the workshop], it definitely was in NCCN guidelines. … I think even if we just touch on – at least we discuss a tiny– you know, what’s written in the NCCN guidelines, and I would – how I write in my note that bilateral mastectomy, oophorectomy – I write that in my note, yet I tell the patient it’s a surgery to remove your ovaries and tubes. … I think as long as we cover and make sure, it’s fine, but the language, yeah, is definitely different. (GC2)
GCs who were farther out from their training, and who serve as clinical supervisors for training programs, described the difficulty of breaking habits in order to adopt plain language explanations.
Um … I just think certain phrases that I use, or have used for so many years are hard to get rid of. … Things that are so ingrained that I just don’t even think about it, they just come out. (GC3)
So, I think it’s harder for me, as someone who’s been doing this so long. Like I feel like it’s kind of a bit of a handicap to have – like I’m so on autopilot. (GC7)
3.2.2.2. Ease of use
A few counselors reported that, in an effort to reduce the amount of information they provided, they were using less “science,” meaning less detailed information about genetics and mutations.
… it’s hard for people to understand words like cells and conception and all of that, genetic mutations, whereas I say when someone’s born and they have a high risk for cancer, it’s usually already there. Whether or not they develop cancer, that is where chance comes into play. And so even if someone has something that they were born with, it’s never 100% that they’re going to develop cancer. And then I don’t have to use the term cells or mutations or anything like that. (GC6)
This counselor found that she was able to translate the “two-hit hypothesis” into something that was easier to understand. She described explaining the concept of risk in a clear and concise manner that avoids overwhelming patients with statistics and complex details about genetics.
3.2.2.3. Patient impact
Our goal in introducing techniques such as plain language was to ensure patients’ understanding GCs’ key messages about how hereditary cancer may affect them, and that there is something they can do about it. We observed several instances in which counselors were able to adopt the strategies of using plain talk and avoiding TMI, resulting in patient understanding of key information and take-home messages. When we asked patients to describe the most useful, helpful or important thing they learned in genetic counseling, most answered by restating one or more of the key take home messages.
Well they have some sort of plan after. So, I thought that was pretty good. I was like, what are you going to do if, you know–If I have it. Alright let’s wait, you know, like at least like they have like a little program for it … which, I thought that was interesting. (10-ENG)
Well, that if it comes out positive, I’ll have help … (06-SP)
These patients didn’t report details of the help or plan/program, but importantly they understood that they would be monitored more closely in order to prevent or find cancer early. Other patients emphasized the preventive aspect of the plan or help that would be provided.
I learned that genetic factors can affect the measures that I need to take to prevent cancers in the future. I also learned that if I carry the genes, I need to be more aware and also increase awareness within my family as well. (03-CHI)
I think the most important thing that we learned is that the test can give us a chance to take preventive measures if the cancer is hereditary. (01-CHI)
By contrast, we observed some instances in which the GC did not use plain language, resulting in patient confusion. In the following example, the GC used terminology such as “mutation”, “screening”, and “increased risk” to describe the complex concept of pleiotropy in hereditary cancer syndromes. But then, prompted by the patient, the same GC was able to greatly simplify something that was otherwise utterly confusing.
GC: Um, the other reason … The other reason why we might want to know if this is what’s causing the cancer in your family is because some of these genes are related to more than one type of cancer. So, we might be thinking for you, melanoma, uterine cancer, these other things you should look out for. And, that might be. But, if we found a mutation in a gene that was say related to breast and ovarian cancer like the BRCA gene, right now we’re not even thinking about ovarian cancer, right? Because it’s not in your family. But sometimes finding out what the cause is can give us a heads up to what you’re actually at an increased risk for. And so, it can target kind of what we’re gonna be looking at for you in terms of screening.
PATIENT: Okay.
GC: Does that make sense?
PATIENT: If you can repeat a little bit then that … Yeah.
GC: Yeah, um, so for example like that BRCA gene. It doesn’t mean that if you have that mutation that you have a high risk for every cancer.
PATIENT: Yeah. Okay.
GC: It’s really breast and ovarian.
PATIENT: Okay. It’s a limited …
GC: Mm-hmm (affirmative). And so that, if, if that was what we found, for example, in your family, we are not worried about colon cancer.
PATIENT: Mm-hmm (affirmative).
GC: So, we do what everyone else does. But, what we are really going to be upping your screening for is breast and ovarian cancer because we know those are the main risks.
PATIENT: Got it. Okay. And, so if … Because, my dad had kidney and colon cancer you are going to be testing for that? Is that …
GC: We will be testing for that. Um, but most of the time all of these cancers, especially kidney cancer for example, they are not genetic. (Pilot-03-ENG; GC4)
Here, the patient was able to admit that she did not understand, and to ask the GC to repeat the information. The GC explained it again in a simpler manner, resulting in the patient asking appropriate follow-up questions about her risk that indicated she understood.
To varying degrees, we observed GCs limiting the amount of jargon, risk percentages, and technical information in their counseling sessions. SEven when GCs felt uncertain about limiting the information they provided to patients, many agreed that the value of providing clear and concise information outweighed the desire to include additional details about genetic concepts. In interviews, many patients demonstrated understanding key information about the purpose of testing and the benefits of knowing about a mutation, such as preventive options.
3.2.3. Changing the Balance Between Information/Education and Psychosocial Counseling
Several GCs mentioned that psychosocial counseling was one of the primary values of their profession. When reporting on their use of LHL strategies, they were pleased to find that spending less time on detailed explanations of genetics allowed for more time to address psychosocial issues.
I was just thinking of my patient today who I met with, who was a little bit of a lower literacy, lower SES kind of a patient, and she really responded well when I just kept it at that, and didn’t go into much more detail. I think that along the way she really expressed understanding and I also, you know, it just gave me more time, I think, to delve into psychosocial issues with her that sometimes, maybe, just with all my explanations I don’t always go as deep in that area as I’d like to. So that was a kind of a positive outcome from my case today. I was able to get through the information about the genetic testing and the multi-gene panel more quickly, but I also didn’t necessarily feel like I lost anything along the way, or that she didn’t get as good of an informed consent as anybody else. (GC3)
By successfully limiting the amount of information that she provided in her session, this counselor was able to focus more on the patient’s experience without negatively impacting the quality of patient care or informed consent for testing, a concern some counselors had expressed during the training. Another counselor told the following story when asked about limiting information:
I’ve definitely done that, the limiting of information. So just one instance comes to mind where we were giving a diagnosis to a mom and she just was taking it really hard emotionally and it was a diagnosis of Marfan Syndrome ….And I had planned to give kind of a talk about the genetics of Marfan syndrome and the particular mutation that was in the family and all that. And I just decided not to do any of it because she just—I don’t think that she would’ve listened. And I just said, do you want to talk about this right now or do you want me to phone you at a later time or you can come back in? And she almost couldn’t even give me an answer. She was like, I don’t know. I don’t know. I don’t know what to do right now … So, I just kind of made the decision for her and just said: You know what, let’s not right now. So, I definitely, yeah, I am trying to be really careful about that, about how much information I’m giving. (GC5)
This counselor recalled interrupting her own plan to share details about the genetics underlying the patient’s diagnosis in order to attend more fully to the patient’s emotional response. She assessed her patient’s needs and shared only the information that was necessary in that moment. Importantly, limiting the amount of information did not mean that the GC would withhold information, but rather providing in the appropriate context, when the patient would be ready to hear and utilize it. The counselor’s awareness of the option to provide less information enabled her to attend more fully to her patient’s experience and provide her with the emotional support she needed more than anything else.
3.2.3.1. Using empathy to Engage Patients
In keeping with these counselors’ descriptions, we observed GCs taking more time than in the prior study to demonstrate empathy as a way to engage with their patients. We observed them checking in with their patients and acknowledging the emotions that might surround testing. The use of empathy seemed to create an opportunity for rapport-building and thus for patient agency (e.g. asking questions), resulting in better communication. In the following example, a counselor uses empathy to check for understanding:
GC: Yeah. I’m wondering what’s going on in your mind right now. If you think you would find this information useful, or if it would be scary. (Interpreter)
PATIENT: Well, I do want to know so that my family can take preventative measures.
(04-SP; GC4)
Here, the GC engaged the patient from an emotional perspective by asking how the patient was receiving the information. As a result, the patient was able to share her concerns about her family. We observed a similar pattern across other sessions as illustrated here:
GC: We will find out. Do you think waiting this five weeks is gonna be difficult or stressful?
Patient: I got somebody dying at home right now (laughs).
GC: Are you-
Patient: I’m already stressed out.
GC: Are you, then- are you helping take care of them and all of that?
Patient: Trying not to, but, you know. All his siblings work, and so they’re like, “Well, since you guys work from home, why don’t you just work from here.”
GC: This is your husband’s mother?
Patient: Yeah. So. It’s one of those things.
GC: So, you’re dealing with a lot right now.
Patient: Yeah. I’m always dealing with a lot.
GC: Mm-hmm (affirmative).
(04-ENG; GC4)
By engaging with the patient at an emotional level, the counselor gave the patient space to share how her genetic test and cancer risk fit into other aspects of her life. In her interview, this patient shared her positive feelings about the GC, and reported finding her easy to understand and to talk to.
Well I really like my genetic counselor and, you know, I can’t speak for all of them but I can speak for her. She’s awesome …. She uses very plain English, very easy to understand ….The family tree thing, I think it helped her more to understand exactly who’s got what and where. And like for me I know, you know, my family relationship, obviously but, you know, I think it’s a good tool for her so she can better understand where the cancer’s coming from or not where the cancer’s coming from but how closely related I am to those that have it? (04-ENG; GC4)
Through interviews and observations, we found that employing LHL techniques may have allowed for more psychosocial counseling and empathic connections, providing a balance of information and emotional support.
Interviewer: What do you think about the amount of information that was given to you? Was it too much, too little, or just right?
Patient: It was the appropriate amount, not too much and not too little. It was my first time learning about that, so I needed just enough information for me to understand. (03-CH; GC7)
GCs were generally pleased to discover this collateral benefit of the LHL strategies. Further, this outcome suggested to GCs that not only had little been lost by limiting the amount of technical information, but much was gained.
The GCs’ ability to cultivate empathy with their patients seemed to have the biggest impact on whether or not a patient would engage with the information presented. While having a basic knowledge of genes and inheritance certainly helped patients’ ability to absorb the information that the GC provided, we also observed the GCs engage effectively with patients who had no prior knowledge by using some of the LHL techniques throughout the session, as well as establishing rapport by demonstrating empathy.
3.2.4. Assessing Comprehension and engaging the patients with teach-back
Both during the workshop and interviews, counselors expressed concerns about using the teach-back method (Fig. 1) to assess comprehension. Some worried that they would come across as testing or interrogating their patients:
I don’t want the person I’m speaking to to feel like I’m quizzing them, or that I’m, you know, like in a position somehow of punishing them if they get something wrong. I just really want to communicate that I’m on their side and I’m helping them. I want to make sure that I explained it accurately. And somehow it feels really uncomfortable to put them on the spot and ask them to show me, to really demonstrate that they comprehended the information. Almost it’s a challenge for their intelligence or something. (GC1)
Given her worry that teach-back would result in the patient feeling challenged or punished, this GC avoided teach-back to maintain rapport. Other GCs reported that they were able to use teach-back and found it beneficial. For example, one GC mentioned that she felt badly about putting her patients on the spot, but was more comfortable asking her patients how they would explain this information to a family member. Another GC found a way to fit it in with the flow of the conversation:
I have tried using the teach-back a couple times now. And for the most part that’s been going well. … Like, if someone says, for example, oh, I can’t wait to tell my daughter the good news. I might just kind of interject, oh, what are, how are you going to tell her, what are you going to explain? And for the most part I’ve had good reactions. Some patients are shy and don’t really, aren’t forthcoming. They’re like, oh I’ll just show her. Or something like that. But I think that it’s a good way also for me to check in with them. To make sure and to maybe make slight adjustments if something that they say isn’t quite right. So, I think that’s been, in that way I, I have noticed, at least for me, it’s a good tool. (GC4)
Another counselor reported only using teach-back when working with an interpreter and/or someone she perceived as low health literacy:
Yeah, you know, I generally only use that when I’m working with an interpreter. And someone [who] was, and/or someone with obviously low health literacy … because I just, I feel like I’m … could be insulting the higher educated person. (LAUGHS) Like it’s too obvious. (GC9)
Most counselors reported attempting to incorporate this strategy into their appointments following the workshop although even those who did adopt this strategy expressed the need for further practice for it to become effortless.
We also observed teach-back employed successfully during visits. For example, one GC used teach-back to ensure that her patient understood the purpose of the test:
GC: Can you explain to me, though, just so I make sure you understand, what we’re going to learn from the test that we’re doing? Just so I can make sure that I explained it well.
Interpreter: She says, so that I know whether I explained it to you well, tell me, what are we going to learn from the test that we’re going to do?
Patient: What I understood her to say is that this test that we’re going to do is to see if it comes from the family, hereditary. And to see if, like she says, to check if it comes from there, then to get more prevention for me from other cancers and my family.
Interpreter: To see if this is, from hereditary, from the family. And if it is hereditary, that’s to prevent for the any other cancer myself and my family.
GC: Exactly, exactly.
Interpreter: Exactly. [SP-01; GC7]
Here, the GC was able to ensure that the patient understood a key message about the availability of early detection and prevention if she were found to be at high risk. The interpreter also appeared familiar with the technique and translated it effectively. Despite the apprehension described by GCs about using teach-back as a tool to assess comprehension, none of the patients we interviewed reported any negative experiences with it.
While the GCs tried putting teach-back into practice, they continued to check for understanding in a variety of alternate ways. In the following exchange, the counselor paused to check in with her patient at the end of the session, after explaining the various preventive options available to her.
GC: So, um, I’ve given a lot of information. What kinds of questions or thoughts do you have?
Patient: Um … nothing I can think about right now. Um, yeah.
(10-ENG; GC7)
In this example, the GC acknowledged that she had covered a lot of ground during the appointment; nevertheless, it was not until minute 20 of a 25 min session that she paused to assess comprehension. Despite asking an open-ended question, the GC did not tie her question to any specific piece of the information she had given, nor did she explicitly check for understanding at various points during the appointment (using the “chunk and check” technique). In this instance, the patient did not respond with any questions.
Other times, GCs assessed comprehension by asking about specific aspects of the session that they had just covered, such as preventive options, and by asking closed-ended, yes/no questions. As we see in the following example, the GC asked her patient specifically about her understanding of the possible test results which she had just explained:
GC: Any thoughts or questions about the kinds of results we could get back?
Interpreter: Any thoughts or questions about the kinds of results we could get back?
Patient: No.
(06-SP; GC4)
Here, the patient was not able to articulate any questions, although it became clear during the patient interview that she had left the appointment confused about the overall purpose of the test. As discussed in the workshop, the inability to articulate questions sometimes can be a sign of LHL.
4. Discussion
This is one of the first studies to evaluate health literacy (HL) communication training (Coleman and Fromer, 2015; Kripalani et al., 2006; Mackert et al., 2011), and to our knowledge, the only one to do so with Master’s level Genetic Counselors. Prior HL training assessments have addressed the integration of health literacy into core medical, nursing and other curricula (e.g. Toronto and Weatherford, 2015), or in workshops such as ours for practicing professionals (Kripalani et al., 2006). Unique to our study was our in-depth, multi-method, qualitative evaluation of the training workshop and subsequent provider practice. We interviewed GC participants about their experiences implementing the strategies over the two months following the workshop, observed and audio-recorded two of the GCs as they counseled patients, and then interviewed their patients. Across these various forms of data, a consistent pattern emerged. GCs were able to employ the communication strategies and techniques taught in the workshop some of the time, resulting in more time for psychosocial counseling and more attention to empathic connections with patients. Patients expressed satisfaction, as well as understanding of key concepts, and articulated no concerns with comprehension checks using teach-back.
Overall, nearly all of the counselors reported that, following the workshop, they were more attentive to health literacy in their practice and took steps to adjust their communication. We did note a discrepancy between what we taught in the workshop about low health literacy cues and the cues GCs reported using, such as English language proficiency and status as an immigrant. In providing background about HL in the workshop, we cited data showing that individuals in certain demographic categories are more likely to be of lower health literacy (e.g. limited English proficiency, elderly, poor, less educated, Latino, African American, and those on Medicaid or Medicare) (Berkman et al., 2011; Rikard et al., 2016; Thomas et al., 2004; US DHHS, 2010; Weiss et al., 2005). We also provided specific, non-demographic cues that research has shown can be used to identify patients of LHL (e.g. multiple no shows, forms not filled out) (Cornett, 2009; Weiss, 2007). It appears that we neglected to sufficiently emphasize that demographic characteristics cannot take the place of assessing an individual’s health literacy, and that using demographic criteria could result in harmful stereotyping.
Among the communication strategies and techniques we taught, GCs were most able to limit the amount of jargon and technical genetic language that they used in their sessions, adopt plain language and focus clearly on key messages (Kripalani et al., 2006; Stableford and Mettger, 2007). While some counselors worried about the implications of providing their patients with less information, or “sacrificing accuracy for clarity,” we emphasized that giving too much information would likely result in less understanding, and further, that plain language does not require “dumbing down” the communication or providing inaccurate information (Stableford and Mettger, 2007). Framing information in a way that enables patients to leverage their understanding, and in turn gain agency over medical decision-making, is necessary to diminish disparities in care (Natta et al., 2017; Shim, 2010). The use of the “universal precaution principle” (AHRQ, 2017; Brega et al., 2015; DeWalt et al., 2011; Liang and Brach, 2017), where plain language is used for all patients, may help to avoid stereotyping based on demographic characteristics, while simultaneously ensuring that the communication about genetics is accessible for all. While the US has particularly high rates of low literacy (PIACC, 2018), Canada, European countries and others also face challenges with regard to health literacy (Stableford and Mettger, 2007). Beyond health literacy, other factors can contribute to reduced comprehension in health care environments. For example, stressful medical situations, such as a cancer diagnosis or identification of high cancer risk, can make comprehension difficult (USDHH, 2005). Thus, the communication approaches taught in the GC workshop, while derived from research on communication with those of limited health literacy, could benefit most patients (Barton et al., 2018; Liang and Brach, 2017).
Counselors also reported checking for comprehension more frequently following the workshop. While they continued to use a wide range of approaches, they also tried out teach-back despite their concerns about offending patients or feeling awkward. Contrary to their apprehensions, patient responses were positive and provided useful information to the GCs. These results are consistent with research showing that teach-back is an effective tool for improving patient-provider communication (Gupta and Speer, 2017) and patient comprehension (Kripalani et al., 2008; White et al., 2013).
Perhaps most important among our findings, GCs reported the unanticipated benefit that adopting these communication strategies and techniques allowed more time for psychosocial counseling, and we observed that showing empathy effectively engaged patients. Attending to psychosocial issues is a key component of genetic counseling (Biesecker et al., 2014; Trepanier et al., 2004; Weil, 2003; Eijzenga et al., 2014), and previous research has found emotional connections to be a more important component of counseling than information alone (Edwards et al., 2008). Nevertheless, numerous studies have found that information and provider speech dominate GC sessions (Edwards et al., 2008; Paul et al., 2015). While GCs’ commitment to, and excitement about, the evolving science of genetics is necessary to do their jobs well, it must be balanced with the recognition that their patients may not share their perspective.
Many of the GCs in our study found that adopting LHL strategies and techniques resulted in improved communication. At the same time, they pointed out that professional guidelines (NCCN) (Daly et al., 2018), expectations established in graduate training programs (Accreditation Council for Genetic Counseling, 2015), and deeply ingrained communication habits that result from these guidelines and expectations challenged their ability to implement the communication approaches taught in the workshop. The fact that these strategies and techniques for effective communication are at odds with GC training and professional standards suggests a critical need to revisit both. Our training intervention aligns with theoretical perspectives that identify health literacy as part of a broader set of social and institutional dynamics rather than an individual deficit (Archer et al., 2015; Brach et al., 2012; Shim, 2010). Thus, the remedies for varying levels of health and genomic literacy and communication gaps such as those we see in genetic counseling, lie in addressing provider training and institutional structures of practice, rather than individual patient behavior or perceived deficits.
4.1. Limitations
Given the small sample included in the observations (2 counselors, 24 observations and 9 interviews with patients), we did not reach theoretical saturation for the observational data (O’Reilly and Parker, 2013). Though we see trends, further research is needed to test the intervention described here. Counselor training was conducted in a single session. Additional training or ongoing support for counselors as they transition to employing these communication strategies and techniques is needed to fully assess feasibility and effectiveness of the training content.
5. Conclusions
This pilot training intervention found that counselors were able to begin to make some changes in their communication following the workshop, compared with our prior study (Cheng et al., 2017; Joseph et al., 2017; Kamara et al., 2018). Overall, the communication strategies and techniques deployed by the counselors appeared to improve patient understanding of key information, such as the implications of genetic testing for oneself and one’s family. Furthermore, in contrast to the prior study, the pilot study patients did not report feeling overwhelmed by the amount of information provided, and were aware of their next steps should the test come back positive. Counselors’ expressions of empathy generally resulted in increased comprehension and better communication overall.
These findings, along with the prior study (Joseph et al., 2017), have been used to design a randomized controlled trial that will compare “usual care” counseling to a “modified” counseling protocol incorporating LHL principles, strategies and techniques (Fig. 1) for the disclosure of exome sequencing results to diverse patients in the CHARM (Cancer Health Assessments Reaching Many) study. The counselors delivering the modified protocol will receive more robust training and participate in practice role plays over a period of several months. CHARM is part of the National Human Genome Research Institute’s Clinical Sequencing Evidence-Generating Research (CSER) Consortium, which requires the inclusion of at least 60% medically underserved populations in each of the six consortium sites across the country (Amendola et al., 2018), and thus we expect CHARM participants to have varied levels of health and genomic literacy. The results of CHARM’s RCT will provide evidence needed to support structural changes in GC training and the practice of genomic medicine. Given the limited health literacy and genomic literacy of adults in the US and in other nations, it is imperative that the genetic counseling profession act sooner rather than later to address the gap between professional training and current practice on the one hand, and on the other, the realities counselors increasingly face in their clinics.
Acknowledgements
We are grateful to the courageous genetic counselors who allowed us to observe them in their daily practice, and who openly participated in the workshop and interviews. We also greatly appreciate the patient participants’ contributions. Working collaboratively with the members of CHARM study genetic counseling working group has enhanced our thinking about this intervention in critical ways as we developed this manuscript.
Funding
Susan G. Komen for the Cure IIR12221854 (Joseph, PI) and National Human Genome Research Institute 5U01HG007292-06 (Goddard & Wilfond, MPI)
References
- O’Brien MA, Whelan TJ, Charles C, Ellis PM, Gafni A, Lovrics P, et al. , 2008. Women’s perceptions of their treatment decision-making about breast cancer treatment. Patient Educ. Counsel 73 (3), 431–436. 10.1016/j.pec.2008.07.015. [DOI] [PubMed] [Google Scholar]
- O’Reilly M, Parker N, 2013. ‘Unsatisfactory Saturation’: a critical exploration of the notion of saturated sample sizes in qualitative research. Qual. Res 13 (2), 190–197. 10.1177/1468794112446106. [DOI] [Google Scholar]
- Accreditation Council for Genetic Counseling, 2015. ACGC Practice-based Competencies for Genetic Counselors. Accreditation Council for Genetic Counseling; Retrieved from. www.gceducation.org. [Google Scholar]
- AHRQ Agency for Healthcare Research and Quality, Rockville, M.D., 2017. AHRQ Health Literacy Universal Precautions Toolkit; Retrieved April 17, 2018, from. http://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/index.html. [Google Scholar]
- Amendola LM, Berg JS, Horowitz CR, Angelo F, Bensen JT, Biesecker BB,, et al. , 2018. The clinical sequencing evidence-generating research consortium: integrating genomic sequencing in diverse and medically underserved populations. Am. J. Hum. Genet 103 (3), 319–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archer L, Dawson E, DeWitt J, Seakins A, Wong B, 2015. “Science capital”: a conceptual, methodological, and empirical argument for extending bourdieusian notions of capital beyond the arts. J. Res. Sci. Teach 52 (7), 922–948. [Google Scholar]
- Barlow-Stewart K, Yeo SS, Meiser B, Goldstein D, Tucker K, Eisenbruch M, 2006. Toward cultural competence in cancer genetic counseling and genetics education: lessons learned from Chinese- Australians. Genet. Med 8, 24. [DOI] [PubMed] [Google Scholar]
- Barton AJ, Allen PE, Boyle DK, Loan LA, Stichler JF, Parnell TA, 2018. Health literacy: essential for a culture of health. J. Cont. Educ. Nurs 49 (2), 73–78. 10.3928/00220124-20180116-06. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K, 2011. Low health literacy and health outcomes: an updated systematic review. Ann. Intern. Med 155 (2), 97 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Biesecker B, Klein W, Lewis KL, Fisher TC, Wright MF, Biesecker LG, Han PK, 2014. How do research participants perceive “uncertainty” in genomic sequencing? Genet. Med.: Offic. J. Am. Coll. Med. Gene 16 (12), 977–980. 10.1038/gim.2014.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biesecker B, Austin J, Caleshu C, 2017. Theories for psychotherapeutic genetic counseling: fuzzy trace theory and cognitive behavior theory. J. Genet. Counsel 26 (2), 322–330. 10.1007/s10897-016-0023-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brach C, Keller D, Hernandez LM, Baur C, Dreyer B, Schyve P, et al. , 2012. Ten Attributes of Health Literate Health Care Organizations. Institute of Medicine of the National Academies, Washington, DC. [Google Scholar]
- Bradbury AR, Patrick-Miller L, Long J, Powers J, Stopfer J, Forman A, et al. , 2015. Development of a tiered and binned genetic counseling model for informed consent in the era of multiplex testing for cancer susceptibility. Genet. Med.: Offic. J. Am. Coll. Med. Gene 17 (6), 485–492. 10.1038/gim.2014.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brega AG, Freedman MAG, LeBlanc WG, Barnard J, Mabachi NM, Cifuentes M, et al. , 2015. Using the health literacy universal precautions toolkit to improve the quality of patient materials. J. Health Commun 20 (Suppl. 2), 69–76. 10.1080/10810730.2015.1081997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browner CH, Preloran HM, Casado MC, Bass HN, Walker AP, 2003. Genetic counseling gone awry: miscommunication between prenatal genetic service providers and Mexican-origin clients. Soc. Sci. Med 56 (9), 1933–1946 1982. [DOI] [PubMed] [Google Scholar]
- Butrick M, Kelly S, Peshkin BN, Luta G, Nusbaum R, Hooker GW, et al. , 2015. Disparities in uptake of BRCA1/2 genetic testing in a randomized trial of telephone counseling. Genet. Med 17 (6), 467–475. 10.1038/gim.2014.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles S, Kessler L, Stopfer JE, Domchek S, Halbert CH, 2006. Satisfaction with genetic counseling for BRCA1 and BRCA2 mutations among African American women. Patient Educ. Counsel 63 (1), 196–204. 10.1016/j.pec.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Cheng JKY, Guerra C, Pasick RJ, Schillinger D, Luce J, Joseph G, 2017. Cancer genetic counseling communication with low-income Chinese immigrants. J. Commun. Gene 1–14. 10.1007/s12687-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman CA, Fromer A, 2015. A health literacy training intervention for physicians and other health professionals. Fam. Med 47 (5), 388–392. [PubMed] [Google Scholar]
- Cornett S, 2009. Assessing and addressing health literacy. OJIN: Online J. Iss. Nurs 14 (3). https://doi.org/DOI: 10.3912/OJIN.Vol14No03Man02. [DOI] [Google Scholar]
- Cragun D, Bonner D, Kim J, Akbari MR, Narod SA, Gomez-Fuego A, et al. , 2015. Factors associated with genetic counseling and BRCA testing in a population-based sample of young Black women with breast cancer. Breast Canc. Res. Treat 151 (1), 169–176. 10.1007/s10549-015-3374-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly MB, Pilarski R, Berry M, Buys SS, Farmer M, Friedman S, et al. , 2018. Version). NCCN Clinical Practice Guidelines in Oncology. Genetic/Familial High-risk Assessment: Breat and Ovarian. National Comprehensive Cancer Network. [Google Scholar]
- DeWalt DA, Broucksou KA, Hawk V, Brach C, Hink A, Rudd R, Callahan L, 2011. Developing and testing the health literacy universal precautions toolkit. Nurs. Outlook 59 (2), 85–94. 10.1016/j.outlook.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards A, Gray J, Clarke A, Dundon J, Elwyn G, Gaff C, et al. , 2008. Interventions to improve risk communication in clinical genetics: systematic review. Patient Educ. Counsel 71 (1), 4–25. 10.1016/j.pec.2007.11.026. [DOI] [PubMed] [Google Scholar]
- Eichmeyer JN, Northrup H, Assel MA, Goka TJ, Johnston DA, Williams AT, 2005. An assessment of risk understanding in hispanic genetic counseling patients. J. Genet. Counsel 14 (4), 319–328. 10.1007/s10897-005-0759-5. [DOI] [PubMed] [Google Scholar]
- Ellington L, Maxwel A, Baty BJ, Roter D, Dudley WN, Kinney AY, 2007. Genetic counseling communication with an African American BRCA1 kindred. Soc. Sci. Med 64 (3), 724–734. 10.1016/j.socscimed.2006.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erby LH, Roter D, Larson S, Cho J, 2007. The rapid estimate of adult literacy in genetics (REAL-G): a means to assess literacy deficits in the context of genetics. Am. J. Med. Genet 146A (2), 174–181. 10.1002/ajmg.a.32068. [DOI] [PubMed] [Google Scholar]
- Goodman M, Finnegan R, Mohadjer L, Krenzke T, Hogan J, 2013. Literacy, Numeracy, and Problem Solving in Technology-Rich Environments Among U.S. Adults: Results from the Program for the International Assessment of Adult Competencies 2012: First Look (NCES 2014–008). U.S. Department of Education. National Center for Education Statistics, Washington, DC: Retrieved December 12, 2018 from. http://nces.ed.gov/pubsearch. [Google Scholar]
- Gupta A, Speer ME, 2017. Health literacy and effective health communication in pediatric practices and health systems: creating shame-free environments and patient-friendly institutions In: Health Literacy and Child Health Outcomes. Springer, Cham, pp. 51–56. 10.1007/978-3-319-50799-6_5. [DOI] [Google Scholar]
- Himes DO, Clayton MF, Donaldson GW, Ellington L, Buys SS, Kinney AY, 2016. Breast cancer risk perceptions among relatives of women with uninformative negative BRCA1/2 test results: the moderating effect of the amount of shared information. J. Genet. Counsel 25 (2), 258–269. 10.1007/s10897-015-9866-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooker GW, Ormond KE, Sweet K, Biesecker BB, 2014. Teaching genomic counseling: preparing the genetic counseling workforce for the genomic era. J. Genet. Counsel 23 (4), 445–451. 10.1007/s10897-014-9689-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurle B, Citrin T, Jenkins JF, Kaphingst KA, Lamb N, Roseman JE, Bonham VL, 2013. What does it mean to be genomically literate? National human genome research Institute meeting report. Genet. Med.: Offic. J. Am. Coll. Med. Gene 15 (8), 658–663. 10.1038/gim.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph G, Pasick RJ, Schillinger D, Luce J, Guerra C, Cheng JKY, 2017. Information mismatch: cancer risk counseling with diverse underserved patients. J. Genet. Counsel 26 (5), 1090–1104. 10.1007/s10897-017-0089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamara D, Weil J, Youngblom J, Guerra C, Joseph G, 2018. Cancer counseling of low-income limited English proficient latina women using medical interpreters: implications for shared decision-making. J. Genet. Counsel 27 (1), 155–168. 10.1007/s10897-017-0132-5. [DOI] [PubMed] [Google Scholar]
- Kaphingst KA, Blanchard M, Milam L, Pokharel M, Elrick A, Goodman MS, 2016. Relationships between health literacy and genomics-related knowledge, self-efficacy, perceived importance, and communication in a medically underserved population. J. Health Commun 21 (Suppl. 1), 58–68. 10.1080/10810730.2016.1144661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripalani S, Jacobson KL, Brown S, Manning K, Rask KJ, Jacobson TA, 2006. Development and implementation of a health literacy training program for medical residents. Med. Educ. Online 11 (1), 4612 10.3402/meo.v11i.4612. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Bengtzen R, Henderson LE, Jacobson TA, 2008. Clinical research in low-literacy populations: using teach-back to assess comprehension of informed consent and privacy information. IRB 30 (2), 13–19. [PubMed] [Google Scholar]
- Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW, 2011. Communicating genetic and genomic information: health literacy and numeracy considerations. Public Health Genomics 14 (4–5), 279–289. 10.1159/000294191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang L, Brach C, 2017. Health literacy universal precautions are still a distant dream: analysis of U.S. Data on health literate practices. HLRP: Health Liter. Res. Pract 1 (4), e216–e230. 10.3928/24748307-20170929-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyle J, 2013. Stimulated recall: a report on its use in naturalistic research. Br. Educ. Res. J 29 (6), 861s–878. 10.1080/0141192032000137349. [DOI] [Google Scholar]
- Mackert M, Ball J, Lopez N, 2011. Health literacy awareness training for healthcare workers: improving knowledge and intentions to use clear communication techniques. Patient Educ. Counsel 85 (3), e225–e228. 10.1016/j.pec.2011.02.022. [DOI] [PubMed] [Google Scholar]
- Mai PL, Vadaparampil ST, Breen N, McNeel TS, Wideroff L, Graubard BI, 2014. Awareness of cancer susceptibility genetic testing: the 2000, 2005, and 2010 national health interview surveys. Am. J. Prev. Med 46 (5), 440–448. 10.1016/j.amepre.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LT, Parker RM, 2011. Insurance expansion and health literacy. J. Am. Med. Assoc. 306 (8), 874–875. 10.1001/jama.2011.1212. [DOI] [PubMed] [Google Scholar]
- Meiser B, Irle J, Lobb E, Barlow-Stewart K, 2008. Assessment of the content and process of genetic counseling: a critical review of empirical studies. J. Genet. Counsel. 17 (5), 434–451. 10.1007/s10897-008-9173-0. [DOI] [PubMed] [Google Scholar]
- Natta MV, Burke NJ, Yen IH, Rubin S, Fleming MD, Thompson-Lastad A, Shim JK, 2017. Complex care and contradictions of choice in the safety net. Sociol. Health Illness 40 (3), 538–551. 10.1111/1467-9566.12661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen-Bohlman L, Panzer AM, Kindig DA, Institute of Medicine (U.S.), & Committee on Health Literacy, 2004. Health Literacy: a Prescription to End Confusion. National Academies Press, Washington, D.C: Retrieved from. http://public.eblib.com/choice/publicfullrecord.aspx?p=3376906. [PubMed] [Google Scholar]
- Paul J, Metcalfe S, Stirling L, Wilson B, Hodgson J, 2015. Analyzing communication in genetic consultations—a systematic review. Patient Educ. Counsel 98 (1), 15–33. 10.1016/j.pec.2014.09.017. [DOI] [PubMed] [Google Scholar]
- Penchaszadeh VB, 2001. Genetic counseling issues in Latinos. Genet. Test 5 (3), 193–200. 10.1089/10906570152742236. [DOI] [PubMed] [Google Scholar]
- Peterson EB, Chou W-YS, Gaysynsky A, Krakow M, Elrick A, Khoury MJ, Kaphingst KA, 2018. Communication of cancer-related genetic and genomic information: a landscape analysis of reviews. Translational Behavioral Medicine 8 (1), 59–70. 10.1093/tbm/ibx063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapp R, 1993. Amniocentesis in sociocultural perspective. J. Genet. Counsel 2 (3), 183–196. 10.1007/BF00962079. [DOI] [PubMed] [Google Scholar]
- Ratzan SC, Parker RM, 2000. Introduction In: Zorn M, Ratzan SC, Parker RM (Eds.), National Library of Medicine Current Bibliographies in Medicine: Health Literacy. NLM Pub. No. CBM 2000–1. Selden CR. National Institutes of Health, U.S. Department of Health and Human Services, Bethesda, MD. [Google Scholar]
- Rikard RV, Thompson MS, McKinney J, Beauchamp A, 2016. Examining health literacy disparities in the United States: a third look at the National Assessment of Adult Literacy (NAAL). BMC Public Health 16 (1). 10.1186/s12889-016-3621-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter DL, Erby LH, Larson S, Ellington L, 2007. Assessing oral literacy demand in genetic counseling dialogue: preliminary test of a conceptual framework. Soc. Sci. Med 65 (7), 1442–1457. 10.1016/j.socscimed.2007.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim JK, 2010. Cultural health capital: a theoretical approach to understanding health care interactions and the dynamics of unequal treatment. J. Health Soc. Behav 51 (1), 1–15. 10.1177/0022146509361185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon I, Harrington E, Hooker G, Erby L, Axilbund J, Hampel H, et al. , 2017. Lynch syndrome limbo: patient understanding of variants of uncertain significance. J. Genet. Counsel 26 (4), 866–877. 10.1007/s10897-017-0066-y. [DOI] [PubMed] [Google Scholar]
- Stableford S, Mettger W, 2007. plain language: a strategic response to the health literacy challenge. J. Publ. Health Pol 28 (1), 71–93. 10.1057/palgrave.jphp.3200102. [DOI] [PubMed] [Google Scholar]
- Thomas SB, Fine MJ, Ibrahim SA, 2004. Health disparities: the importance of culture and health communication. Am. J. Public Health 94 (12), 2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toronto CE, Weatherford B, 2015. Health literacy education in health professions schools: an integrative review. J. Nurs. Educ 54 (12), 669–676. 10.3928/01484834-20151110-02. [DOI] [PubMed] [Google Scholar]
- Trepanier A, Ahrens M, McKinnon W, Peters J, Stopfer J, Grumet SC, et al. , 2004. Genetic cancer risk assessment and counseling: recommendations of the national society of genetic counselors. J. Genet. Counsel 13 (2), 83–114. 10.1023/B:JOGC.0000018821.48330.77. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services, 2005. Plain Language: a Promising Strategy for Clearly Communicating Health Information and Improving Health Literacy. Retrieve from. https://health.gov/communication/literacy/plainlanguage/IssueBrief.pdf.
- Walcott FL, Dunn BK, DeShields M, Baquet C, 2014. The affordable care act and genetic testing for inheritable cancer syndromes: impact on high-risk underserved minorities. J. Health Care Poor Underserved 25 (1), 46–62. 10.1353/hpu.2014.0070. [DOI] [PubMed] [Google Scholar]
- Weil J, 2003. Psychosocial genetic counseling in the post-nondirective era: a point of view. J. Genet. Counsel. 12 (3), 199–211. 10.1023/A:1023234802124. [DOI] [PubMed] [Google Scholar]
- Weiss BD, 2007. Health Literacy and Patient Safety: help Patients Understand Manual for clinicians, second ed. AHRQ Patient Safety Network. American Medical Association Foundation. [Google Scholar]
- Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. , 2005. Quick assessment of literacy in primary care: the newest vital sign. Ann. Fam. Med 3 (6), 514–522. 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White M, Garbez R, Carroll M, Brinker E, Howie-Esquivel J, 2013. Is “Teach-Back” associated with knowledge retention and hospital readmission in hospitalized heart failure patients? J. Cardiovasc. Nurs 28 (2), 137–146. 10.1097/JCN.0b013e31824987bd. [DOI] [PubMed] [Google Scholar]