Abstract
Objective:
Stafne’s bone cyst (SBC) is an asymptomatic, round or oval-shaped, well-defined, uniform radiolucent lesion, usually incidentally observed in the posterior aspects of the mandible. Radiographical appearance may be confusing though. This study aimed to review the literature on SBCs and to map the SBC as shown in their respective papers.
Methods:
A Pubmed® search (1/9/2018 till 31/5/2019), mentioning SBC, was carried out. Included papers had to contain: patient’s age, gender and radiographs.
Results:
In total, 114 papers were found, but only 64 papers were retained, which contained 109 cases (95 males, 14 females). The patients’ ages ranged between 14 and 89 years old (mean age being 52 years). Male patients’ ages (N = 95) ranged from 14 to 89 years (mean age 52.3 years), whereas the females (N = 14) ages ranged between 22 and 68 (mean age 50.2 years). 28 combinations of locations of SBC were recorded. Only three lesions were located at the symphysis, six were bilateral, 55 appeared on the left hand side and 45 on the right hand side of the mandible.The literature mentioned that these cavities could contain salivary gland tissue, muscular tissue, lymphoid tissue, blood vessels, fat tissue or connective tissue.
Discussion/Conclusion:
This study illustrates the wide variation of SBC locations across the mandible and leads us to conclude that the differential diagnosis of every asymptomatic, oval or round, well-defined, uniform radiolucent lesion on two-dimensional radiographs of the mandible should include “a benign mandibular concavity”, formerly known as SBC.
Keywords: Stafne's bone cyst mandibular concavity
Introduction
A clinically justified diagnostic panoramic radiograph is common grounds in dentistry and provides an overview of the dentomaxillofacial complex and its adjacent anatomy. Dental clinicians are trained to recognize normal anatomical boundaries and landmarks, besides identifying pathology in the jaws. However, aberrant anatomy and its radiographical appearance can be confusing and may be misinterpreted as pathology.1 The latter can lead to unnecessary additional imaging (e.g., CBCT or multi-slice CT (MSCT)) which results in an increased cost and radiation burden for the patient. Moreover this can also result in unnecessary surgical interventions, which also have a cost, a potential risk of complications and it contradicts the Hippocratic oath (primum non-nocere). This can all be avoided if clinicians can be trained better by providing evidence, by publications, for these aberrant anatomical presentations appearing in radiographs.
Panoramic and intraoral radiographs of the mandible can reveal incidental findings, like a unilocular round or oval cystic appearing, uniform radiolucent, lesion with well-defined borders, which can be confusing for interpretation, especially if it occurs superior of or seems to be encroaching on the inferior alveolar nerve canal or on the inferior cortical border of the mandible, or if projected on a tooth’s apex, or if observed in the ramus of the mandible.2–4 It is important that clinicians think of a differential diagnosis when assessing their diagnostic images.
In 1942 Edward Stafne described for the first time, 35 asymptomatic, radiographically radiolucent cavities, unilaterally located in the posterior region of the mandible, between the mandibular angle and the third molar, and below the inferior dental canal and slightly above the inferior cortical border of the mandible. He described the following phenomenon as Stafne’s bone cyst (SBC).5–10 While at the time Stafne did not analyse the contents of these cavities on a microscopic level, what triggered his interest was fuelled by a multitude of factors. These included the similarity in the appearance of these cavities and a somewhat consistent location in oblique lateral and lateral radiographs. This congruence across the 35 cases that he observed suggested a common aetiological factor, which continued to be reported in the literature over time.6 The aetiology remains unclear, but assumptions such as hypertrophy of a lobe of a salivary gland, bony erosion caused by vascular compression, or an incomplete Meckel cartilage calcification during ossification, have been proposed. According to Hisatomi et al. (2019),6 the incidence of SBC is less than 0.5% for the posterior lingual variant, and differences in prevalence have been reported to vary between 0.10 and 0.48% and in a cadaver study a prevalence as high as 6.06% was reported.11,12 The anterior lingual variant appears to be seven times less prevalent than the posterior one and can be expected between the incisors and the premolar area, superior to the insertion of the mylohyoid muscle.13,14 According to the literature, the age range is quite wide, with a predilection for males over 50 years of age.7,8,15 The size of the lesion was studied by Adisen et al. (2015) and they found that the mean volume of the defect was 361.7 mm3.16 This also explains the confusion it can cause when visible on radiographs.
Different definitions can be found in various radiology text books:
a bone cavity or depression on the lingual aspect of the mandible near the lower border;17
a well-defined round or ovoid or occasionally lobulated radiolucency that ranges in diameter from 1 to 3 cm, below the inferior alveolar canal and anterior to the angle of the mandible, in the region of the antegonial notch and the submandibular gland fossa;18
a corticated unilocular radiolucency below the mandibular canal, between the first molar and a the angle of the mandible, with rare location in the ramus of the mandible (buccal or lingual);19
a developmental depression along the mesial aspect of the mandible most commonly near the angle but sometimes along the body more anteriorly;20
a not always corticated, well-defined round or oval defect or pseudocyst in the lingual surface of the mandible, usually at the mandibular angle caudally to the mandibular canal, seldom in the anterior part of the mandible.21,22
The SBC is also known under a myriad of synonyms: Stafne bone cavity, lingual salivary gland depression, lingual mandibular bone depression, developmental salivary gland defect, Stafne defect, static bone cavity, latent bone cyst, mandibular salivary gland defect and idiopathic bone cavity.1–22
The aim of the present narrative review was to investigate, verify and map the different locations of a SBC from publications that actually showed the radiographs with the exact location of the lesion. Knowledge of the possible locations of this lesion helps clinicians establish a differential diagnosis when a round or oval, uniform radiolucent, well-defined, lesion is observed on a radiographic image of the mandible.
Methods and materials
A Pubmed® search for “SBC” was conducted between 1 September 2018 and 31 May 2019. Inclusion criteria for the review were: English, Dutch, French or German language, full papers available (some with the help of the library of the University of Western Australia and by emailing authors), radiographic image of the lesion available in the publication, and finally patient gender and age clearly mentioned. A hand search was also performed through dental and medical handbooks available to the authors. A check was done using different search terms, such as aberrant salivary gland, Stafne bone cavity, Stafne’s bone cavity and static bone cavity, in order to identify more papers, but that did not result in any additional manuscripts. Therefore, the authors considered their search as comprehensive and complete enough for the purpose of this narrative review.
Results
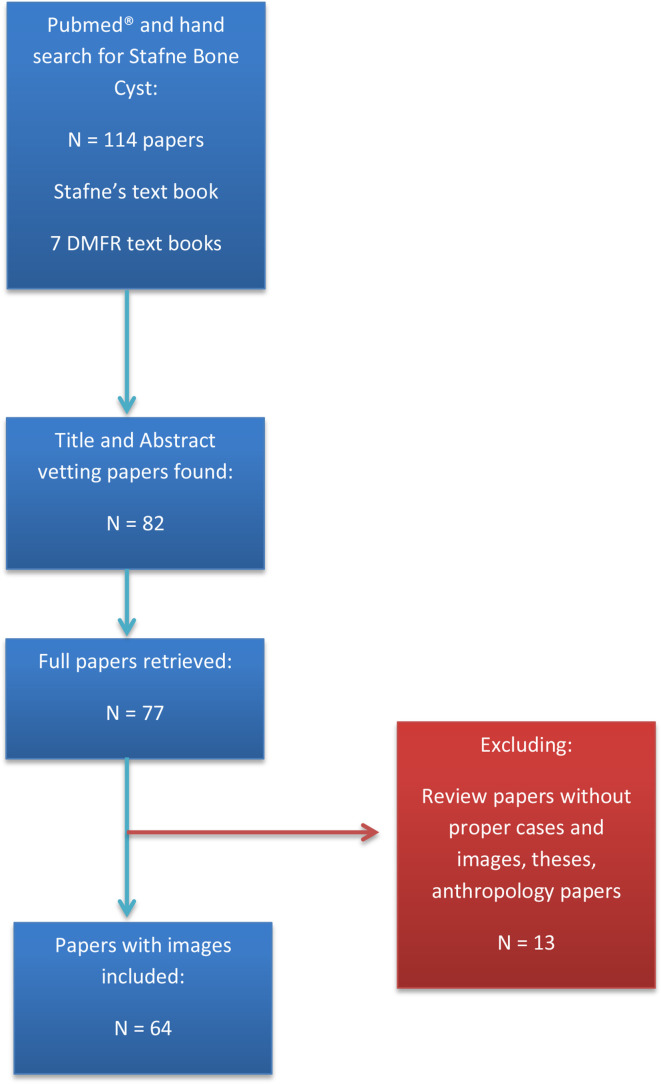
Figure 1 provides an overview of the search methodology in a typical PRISMA flow chart model.23 A total of 114 papers were found on Pubmed®, of which 82 were deemed eligible for the purpose of this review. Only 77 papers were available as full paper. After thorough selection and vetting by the three authors, a final selection of 64 papers was deemed eligible for the final assessment, as they contained enough detailed imaging and patient information to be used for mapping the lesions. This resulted in 109 patient cases with SBC. The 13 papers that were excluded contained anthropomorphic studies, a PhD thesis, letters to the editor, general papers about incidental findings on radiographs and papers regarding other types of lesions mimicking SBC and finally papers covering classification of SBCs. The hand search resulted in retrieving Edward Stafne’s 1963 text book and six other text books on dental and maxillofacial radiology which had a section dedicated to SBC.
Figure 1.
PRISMA flow chart for Stafne Bone Cyst narrative review (1 September 2018 – 31 May 2019)
Table 1 provides an overview of the publications per year, the authors and the country of origin of these papers. The period covers 1980 to 2019. There seems to be a trend, namely that the number of reports published per year has increased after 2009, compared to the period before. The majority of papers came from Turkey, Japan and the UK.
Table 1.
Publications on Stafne’s Bone Cyst found on Pubmed® in the period 1980–2019, which contained images that were eligible for this narrative review
| Year of Publication | Authors | Country of Origin |
|---|---|---|
| 1980 | Adra et al.24 | Lebanon |
| 1984 | Chen and Ohba25 | Japan |
| 1985 | Smith et al.26 | United Kingdom |
| 1986 | Wolf et al.27 | Finland |
| 1988 | Barker28 | United Kingdom |
| 1989 | Tominaga et al.29 | Japan |
| 1990 | Grellner et al.30 | USA |
| 1993 | Ariji et al.31 Shigematsu et al.9 |
Japan Japan |
| 1994 | Tsui and Chan32 | Hong Kong |
| 1997 | Graham et al.33 | United Kingdom |
| 1998 | Reuter34 | Germany |
| 1999 | Apruzzese and Longini35 Branstetter et al.36 Junquera et al.37 |
Italy USA Spain |
| 2000 | Boyle et al.38 | United Kingdom |
| 2001 | Katz et al.14 | Israel |
| 2002 | de Courten et al.39 Dorman and Pierse40 Philipsen et al.7 |
Switzerland United Kingdom Japan |
| 2003 | Longo et al.41 | Italy |
| 2004 | Campos et al.42 Guedes Queiroz et al.43 Phillips and Yates44 |
Brazil Brazil United Kingdom |
| 2006 | Minowa et al.45 Quesada-Gomez et al.8 Segev et al.46 |
Japan and USA Spain Israel |
| 2009 | Bornstein et al.47 | Switzerland |
| 2010 | Kao et al.48 Kopp et al.49 Krafft et al.50 Sisman et al.13 Turkoglu and Orhan51 Flores Campos et al.52 |
Taiwan Germany Germany Turkey Turkey Brazil |
| 2011 | Vieira Aguiar et al.53 Li et al.54 |
Brazil China |
| 2012 | Dereci and Duran55 Etoz et al.56 Friedrich et al.57 Munevveroglu and Aydin58 Sisman et al.12 |
Turkey Turkey Germany Turkey Turkey |
| 2013 | Boffano et al.59 Prechtl et al.60 Saglam et al.61 |
Italy Germany Turkey |
| 2014 | Assaf et al.11 Herranz-Aparicio et al.62 Kim et al.63 Miloglu et al.64 Probst et al.65 Schneider et al.66 Taysi et al.67 |
Switzerland Spain Korea Turkey Germany Switzerland Turkey |
| 2015 | Adisen et al.16 Lee et al.68 Mauprivez et al.69 More et al.70 Ozaki et al.71 Venkatesh72 |
Turkey Australia and United Kingdom France India Japan Kingdom of Saudi Arabia |
| 2016 | Atil et al.73 Chen et al.74 Deyhimi et al.75 Lee et al.76 |
Turkey USA Iran Korea |
| 2017 | Hisatomi et al.77 | Japan and Brazil |
| 2018 | da Silva et al.78 Kaya et al.79 Nishimura et al.80 |
Brazil Turkey Japan |
| 2019 | Lee et al.81 Bayrak82 |
USA Turkey |
In Table 2, one can find the distribution of imaging modalities that were used in the 64 manuscripts. Panoramic radiography, only, was used in 36.7% of the reports, with a combination of panoramic radiography and CBCT being used in 17.4% of cases and a combination of panoramic radiography and multi-slice CT being used in 16.5% of cases. The table shows the prevalence of imaging combinations used in the different papers. Panoramic imaging was involved in 14 of the 18 found imaging combinations in these papers (77.7%), as was expected as SBC is an incidental finding after all. Table 2 also shows which imaging modalities or combinations of modalities were used in the respective papers.
Table 2.
Distribution of imaging modalities used in the papers used for this narrative review about Stafne’s bone cyst (N is the number of cases per imaging modality or combination of imaging modalities)
| Type of Imaging | Publications | N | % |
|---|---|---|---|
| PANO | Chen and Ohba 198425 Sisman et al. 201212 Philipsen et al. 20027 Shigematsu et al. 19939 Adra et al. 198024 Assaf et al. 201411 Smith et al. 198526 de Courten et al. 200239 Apruzzese and Longoni 199935 Barker 198828 Prechtl et al. 201360 Friedrich et al. 201257 Kim et al. 20144 Miloglu et al. 201464 |
40 | 36.70% |
| PANO + MSCT | da Silva et al. 201878 Minowa et al. 200645 Ariji et al. 199331 Boyle et al. 200038 Grellner et al. 199030 Phillips and Yates 200444 Kao et al. 201048 Katz et al. 200114 Bayrak 201982 Campos et al. 200442 Etoz et al. 201256 Reuter 199834 Junquera et al. 199937 Nishimura et al. 201880 Vieira Aguiar et al. 201153 |
18 | 16.50% |
| PANO + CBCT | More et al. 201570 Ozaki et al. 201571 Atil et al. 201673 Bornstein et al. 200947 Sisman et al. 201013 Boffano et al. 201359 Muenevveroglu and Aydin 201258 Venkatesh 201572 Kopp et al. 201049 Taysi et al. 201467 Krafft et al. 201050 Lee et al. 201981 |
19 | 17.40% |
| CBCT | Assaf et al. 201411 | 1 | 0.90% |
| PANO + CBCT+MRI | Schneider et al. 201466 Probst et al. 201465 Bornstein et al. 200947 |
3 | 2.80% |
| PANO + MSCT+MRI | Branstetter et al. 199936 Herranz-Aparicio et al. 201462 Segev et al. 200646 Saglam et al. 201361 |
4 | 3.70% |
| MSCT | Dereci and Duran 201255 | 1 | 0.90% |
| PANO + IO | Deyhimi et al. 201675 Dorman and Pierse 200240 Guedes Queiroz et al. 200443 |
3 | 2.80% |
| PANO + MSCT+ SCINTIGRAPHY |
Flores Campos et al. 201052 | 1 | 0.90% |
| PANO + MRI | Graham et al. 199733 Lee et al. 201568 Hisatomi et al. 201777 Kaya et al. 201879 Mauprivez et al. 201569 |
5 | 4.60% |
| PANO + IO+MSCT | Turkoglu and Orhan 201051 Grellner et al. 199030 |
2 | 1.80% |
| IO + MSCT | Minowa et al. 200645 | 1 | 0.90% |
| PANO + MSCT+ SIALOGRAPHY |
Li et al. 201154 Tominaga et al. 198929 |
2 | 1.80% |
| PANO + OCCL | Tsui and Chan 199432 | 1 | 0.90% |
| PANO + SIALOGRAPHY | Wolf et al. 198627 | 1 | 0.90% |
| CEPH + CBCT | Lee et al. 201676 | 1 | 0.90% |
| PANO + CEPH+CBCT | Longo et al. 200341 | 1 | 0.90% |
| PANO + CBCT+MSCT | Sisman et al. 201212 | 5 | 4.60% |
| 109 | 100.00% |
CBCT, cone beam computed tomography; CEPH, cephalometric radiography; IO, intraoral radiography; MRI, magnetic resonance imaging; MSCT, multi-slice computed tomography; OCCL, occlusal radiography; PANO, panoramic radiography.
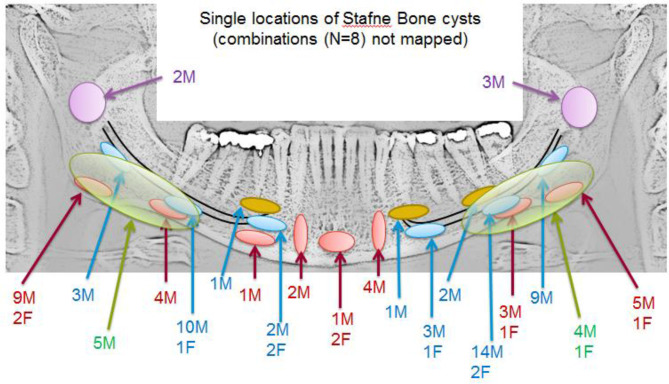
Table 3 summarises the different locations of SBC as recorded from the radiographic images found in the included papers of this review. The table also shows the anatomical locations per gender for the 109 cases in total. Only three lesions were located at the symphysis, six were bilateral, 55 appeared on the left hand side and 45 on the right hand side of the mandible.
Table 3.
Summary of the locations of Stafne’s bone cysts, for the entire sample (N) and per gender (M,F), as checked in the radiographs included in the manuscripts used for this narrative review. The abbreviations used in this table are: RHS = right hand side, PM = premolar, M = molar, IANC = inferior alveolar nerve canal
| Location of Stafne’s Bone Cyst | Publications | N | M | F |
|---|---|---|---|---|
| RHS PM inferior to IANC | Shigematsu et al.19939 | 1 | 1 | |
| RHS PM superior to IANC | Phillips and Yates 200444 | 1 | 1 | |
| LHS PM superior to IANC | Krafft et al. 201050 | 1 | 1 | |
| Bilateral M to angle area, inferior to IANC but encroaching | Junquera et al. 199937 | 1 | 1 | |
| Bilateral angle of mandible | Mauprivez et al. 201569 | 1 | 1 | |
| LHS angle to M area inferior to IANC - double lesion | Miloglu et al. 201464 | 1 | 1 | |
| RHS ramus and LHS M area inferior to IANC and encroaching | Nishimura et al. 201880 | 1 | 1 | |
| RHS angle and RHS anterior mandible | Ozaki et al. 201571 | 1 | 1 | |
| RHS M inferior to IANC + RHS PM inferior IANC + LHS PM inferior IANC | Vieira Aguiar et al. 201153 | 1 | 1 | |
| LHS M superior to IANC | de Courten et al. 200239 Kopp et al. 201049 |
2 | 2 | |
| RHS anterior mandible | Tominaga et al. 198929 Turkoglu and Orhan 201051 |
2 | 2 | |
| RHS ramus | Campos et al. 200442 Lee et al. 201568 |
2 | 2 | |
| Bilateral PM area | Grellner et al. 199030 Kim et al. 201463 |
2 | 1 | 1 |
| RHS angle of mandible and encroaching IANC | Chen and Ohba 198425 Ozaki et al. 201571 Philipsen et al. 20027 |
3 | 3 | |
| LHS ramus | Barker 198828 Hisatomi et al. 201777 Lee et al. 201981 |
3 | 3 | |
| Midline mandible | Dorman and Pierse 200240 Grellner et al. 199030 Guedes Queiroz et al. 200443 |
3 | 1 | 2 |
| RHS M inferior to IANC | Minowa et al. 200645 Shigematsu et al. 19939 Sisman et al. 201212 |
4 | 4 | |
| RHS PM inferior to IANC and encroaching | Bornstein et al. 200947 Shigematsu et al. 19939 Sisman et al. 201013 Sisman et al. 201212 |
4 | 2 | 2 |
| LHS M inferior to IANC | Assaf et al. 201411 More et al. 201570 Sisman et al. 201212 |
4 | 3 | 1 |
| LHS PM inferior to IANC and encroaching | Apruzzese and Longoni 199935 Bornstein et al. 200947 Katz et al. 200114 Taysi et al. 201467 |
4 | 3 | 1 |
| LHS anterior mandible | Bayrak 201982 Dereci and Duran 201255 Deyhimi et al. 201675 Minowa et al. 200645 |
4 | 4 | |
| LHS angle to M area inferior to IANC and encroaching | Etoz et al. 201256 Flores Campos et al. 201052 Lee et al. 201676 Prechtl et al. 201360 Reuter 199834 |
5 | 4 | 1 |
| RHS angle to M area inferior to IANC and encroaching | Friedrich et al. 201257 Kaya et al. 201879 Longo et al. 200341 Muenevveroglu and Aydin 201258 Saglam et al. 201361 |
5 | 5 | |
| LHS angle of mandible | Philipsen et al. 20027 Shigematsu et al. 19939 Sisman et al. 201212 |
6 | 5 | 1 |
| LHS angle of mandible and encroaching IANC | Adra et al. 198024 Assaf et al. 201411 Chen and Ohba 198425 da Silva et al. 201878 Herranz-Aparicio et al. 201462 Sisman et al. 201212 |
9 | 9 | |
| RHS angle of mandible | Branstetter et al. 199936 Chen and Ohba 198425 More et al. 201570 Sisman et al. 201212 |
11 | 9 | 2 |
| RHS M inferior to IANC and encroaching | Ariji et al. 199331 Atil et al. 201673 Boyle et al. 200038 Grellner et al. 199030 More et al. 201570 Schneider et al. 201466 Shigematsu et al. 19939 Smith et al. 198526 Tsui and Chan 199432 |
11 | 10 | 1 |
| LHS M inferior to IANC and encroaching | Adra et al. 198024 Ariji et al. 199331 Boffano et al. 201359 Graham et al. 199733 Kao et al. 201048 Li et al. 201154 More et al. 201570 Muenevveroglu and Aydin 201258 Probst et al. 201465 Segev et al. 200646 Sisman et al. 201212 Smith et al. 198526 Venkatesh 201572 Wolf et al. 198627 |
16 | 14 | 2 |
| Total | 109 | 95 | 14 |
IANC, inferior alveolar nerve canal; LHS, left hand side; M, molar; PM, premolar; RHS, right hand side.
With regard to patient age range, our analysis showed that patients’ ages ranged from 14 to 89 years old, with the mean age being 52 years. Male patients’ ages (N = 95) ranged from 14 to 89 years (mean age 52.3 years), whereas the females (N = 14) ages ranged from 22 to 68 (mean age 50.2 years).
In Figure 2, the different anatomical locations of SBCs are mapped on a panoramic radiograph of a mandible. This figure shows graphically what Table 3 summarised. In red are the ones that did not encroach on the mandibular canal, whereas the blue ovals are. The orange ovals involve locations where the SBC was close to the apex of a tooth, mimicking a radicular lesion. In green are the lesions that covered a larger area of the jaw and in purple are the lesions located in the rami of the mandible. Eight cases were not graphically shown in this figure as these were patients in whom multiple SBCs were observed in different locations. The information about these can be retrieved from Table 3 (the white boxes in the prevalence column).
Figure 2.
The mappings of the different locations of Stafne Bone Cysts as retrieved from the 64 papers which were included in this narrative review. M stands for male, F stands for female and the number indicates how many cases were identified. Eight cases in which multiple locations were present are not shown in this figure, as it would clutter the figure.
Discussion
The current study can be considered an inventory of published radiographically illustrated cases, which has resulted in an evidence-based map of SBC locations, which can now be used for teaching purposes. This study did not question and/or investigate the aetiology of the SBC or the age range in which one can expect this asymptomatic, incidental, radiographic finding to be observed. Therefore, the information regarding prevalence, age and gender is nothing new.
What is new, is however, what is illustrated in Figure 2: the mapping of possible locations of SBCs. The latter shows that radiographic interpretation of radiolucent lesions in the mandible can be complicated, as for instance SBCs can mimic other radiolucent lesions, as they can occur anywhere in the mandible. Occurrence of an SBC superior of the inferior alveolar canal and/or close to the apex of a tooth, complicates differential diagnosis of radiolucent lesions.1–4,38,39,50,70,78 It is therefore the authors’ opinion that all asymptomatic well-defined, round or oval, uniform radiolucent lesions, in the mandible should be considered as possible SBC. That being said, the definition of SBC as mentioned in text books and by Edward Stafne in 1942 is no longer accurate and we think these lesions should be called “benign mandibular concavities”, as their content may be salivary gland tissue, but also lymphoid, muscular, adipose or vascular tissue, as mentioned in several publications.5,10,17–22,31,33,36,46,47,54,57,63,69,70,80
We are aware that several classifications have been proposed to identify the depth of the concavity and its actual content, but as this was not within the scope of the current review, we refer the interested reader to the relevant literature on this.9,10,17–22,31,70 We were purely interested in the anatomical mapping of the lesions in order to illustrate to clinicians that a benign concavity in the mandible should always be considered with the incidental identification of an asymptomatic, round or oval-shaped, well-defined, uniform radiolucent lesion, anywhere in the mandible.
As mentioned above, the aetiology is unknown and it seems interesting to the authors that, despite the fact that millions of teenagers receive orthodontic treatment, and therefore undergo panoramic and other diagnostic imaging, there is no information available on the presence or emergence of these benign mandibular concavities in teenagers. Does that support the hypotheses that it is a developmental lesion? This calls for a longitudinal or retrospective study in which panoramic radiographs, taken for the right reasons, from patients are studied from childhood into adulthood.
It should be emphasized that this narrative review did not investigate the validity or accuracy of the imaging techniques to identify mandibular concavities. However, this could be an interesting topic for a future review.
Conclusion
SBC is an asymptomatic, incidental radiographic finding in the mandible. The current review study has mapped the locations of these lesions as mentioned in their respective publications. The conclusion is that these lesions can occur anywhere in the mandible and that they can mimic any asymptomatic round or oval-shaped, well-defined, uniform radiolucent lesion on a two-dimensional radiograph of the mandible. Therefore we suggest to leave the name SBC and to rename the entity as “benign mandibular concavity”.
REFERENCES
- 1.Sirotheau Corrêa Pontes F, Paiva Fonseca F, Souza de Jesus A, Garcia Alves AC, Marques Araújo L, Silva do Nascimento L, et al. Nonendodontic lesions misdiagnosed as apical periodontitis lesions: series of case reports and review of literature. J Endod 2014; 40: 16–27. doi: 10.1016/j.joen.2013.08.021 [DOI] [PubMed] [Google Scholar]
- 2.Lam EW, Ruprecht A, Dolan KD, Frank JA. Osteomyelitis of the mandible simulating a Stafne mandibular cortical defect. Ann Otol Rhinol Laryngol 1994; 103: 490–4. doi: 10.1177/000348949410300612 [DOI] [PubMed] [Google Scholar]
- 3.Parvizi F, Rout PG. An ossifying fibroma presenting as Stafne's idiopathic bone cavity. Dentomaxillofac Radiol 1997; 26: 361–3. doi: 10.1038/sj.dmfr.4600294 [DOI] [PubMed] [Google Scholar]
- 4.Togan B, Gander T, Lanzer M, Martin R, Lübbers H-T. Incidence and frequency of nondental incidental findings on cone-beam computed tomography. J Craniomaxillofac Surg 2016; 44: 1373–80. doi: 10.1016/j.jcms.2016.06.026 [DOI] [PubMed] [Google Scholar]
- 5.Stafne EC. Congenital defect of the mandible containing salivary gland tissue : Stafne E. C, Oral Roentgenographic Diagnosis. 2nd Ed. Philadelphia and London: WB Saunders Company; 1963. 43–6. [Google Scholar]
- 6.Hisatomi M, Munhoz L, Asaumi J, Arita E-S. Stafne bone defects radiographic features in panoramic radiographs: assessment of 91 cases. Med Oral Patol Oral Cir Bucal 2019; 24: e12–19. doi: 10.4317/medoral.22592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Philipsen HP, Takata T, Reichart PA, Sato S, Suei Y. Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol 2002; 31: 281–90. doi: 10.1038/sj.dmfr.4600718 [DOI] [PubMed] [Google Scholar]
- 8.Quesada-Gómez C, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Stafne bone cavity: a retrospective study of 11 cases. Med Oral Patol Oral Cir Bucal 2006; 11: e277–80. [PubMed] [Google Scholar]
- 9.Shigematsu H, Suzuki S, Osuga T, Okumura Y, Fujita K. A radiographical classification of Stafne's bone cavity. Oral Radiol 1993; 9: 13–18. doi: 10.1007/BF02351544 [DOI] [Google Scholar]
- 10.Shimizu M, Osa N, Okamura K, Yoshiura K. Ct analysis of the Stafne's bone defects of the mandible. Dentomaxillofac Radiol 2006; 35: 95–102. doi: 10.1259/dmfr/71115878 [DOI] [PubMed] [Google Scholar]
- 11.Assaf AT, Solaty M, Zrnc TA, Fuhrmann AW, Scheuer H, Heiland M, et al. Prevalence of Stafne's bone cavity--retrospective analysis of 14,005 panoramic views. In Vivo 2014; 28: 1159–64. [PubMed] [Google Scholar]
- 12.Sisman Y, Miloglu O, Sekerci AE, Yilmaz AB, Demirtas O, Tokmak TT. Radiographic evaluation on prevalence of Stafne bone defect: a study from two centres in turkey. Dentomaxillofac Radiol 2012; 41: 152–8. doi: 10.1259/dmfr/10586700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sisman Y, Etöz OA, Mavili E, Sahman H, Tarim Ertas E. Anterior Stafne bone defect mimicking a residual cyst: a case report. Dentomaxillofac Radiol 2010; 39: 124–6. doi: 10.1259/dmfr/49320253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katz J, Chaushu G, Rotstein I. Stafne's bone cavity in the anterior mandible: a possible diagnostic challenge. J Endod 2001; 27: 304–7. doi: 10.1097/00004770-200104000-00020 [DOI] [PubMed] [Google Scholar]
- 15.Correll RW, Jensen JL, Rhyne RR. Lingual cortical mandibular defects: a radiographic incidence study. Oral Surg Oral Med Oral Pathol 1980; 50: 287–91. doi: 10.1016/0030-4220(80)90386-2 [DOI] [PubMed] [Google Scholar]
- 16.Adisen MZ, Yilmaz S, Misirlioglu M, Atil F. Evaluation of volumetric measurements on CBCT images using stafne bone cavities as an example. Med Oral 2015; 20: e580–6. doi: 10.4317/medoral.20633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whaites E. Differential diagnosis of radiolucent lesions of the jaws In: Whaites E, Drage N, eds. Essentials of dental radiography and radiology. Churchill Livingstone Edinburgh. 5th Ed; 2013. pp 333–58. [Google Scholar]
- 18.Murdoch-Kinch CA. Craniofacial Anomalies : White S. C, Pharoah M. J, Oral radiology. Principles and interpretation. 7th Ed. Canada: Elsevier; 2014. 612–29. [Google Scholar]
- 19.Koenig L. Mandible and Maxilla. Section 3 : Koenig L, Diagnostic imaging. Oral and maxillofacial. 1st ed: Amirsys; 2012. [Google Scholar]
- 20.Mancuso AA, Pettigrew JC, Nair MK. Mandible: introduction and general principles : Mancuso A. A, Hanafee W. N, Head and neck radiology. 1 Philadelphia: Wolters Kluwer Lippincott Williams & Wilkins; 2011. 508–18. [Google Scholar]
- 21.Larheim TA, Westesson P-LA. Jaw cysts and cyst-like conditions In: Larheim T. A, Westesson P. -L. A, eds. Maxillofacial imaging. Springer. 2nd Ed.; 2018. pp 23–56. [Google Scholar]
- 22.MacDonald D. Radiolucencies : MacDonald D, Oral and maxillofacial radiology. A diagnostic approach: Wiley-Blackwell West Sussex; 2011. 93–150. [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG, .PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adra NA, Barakat N, Melhem RE. Salivary gland inclusions in the mandible: Stafne's idiopathic bone cavity. AJR Am J Roentgenol 1980; 134: 1082–3. doi: 10.2214/ajr.134.5.1082 [DOI] [PubMed] [Google Scholar]
- 25.Chen CY, Ohba T. An analysis of radiological findings of Stafne's idiopathic bone cavity. Dentomaxillofac Radiol 1981; 10: 18–23. doi: 10.1259/dmfr.1981.0004 [DOI] [PubMed] [Google Scholar]
- 26.Smith NJ, Looh FC, Todd JM, Whaites EJ. Stafne's bone cavity: a review of the literature and report of two cases. Clin Radiol 1985; 36: 297–9. doi: 10.1016/S0009-9260(85)80068-4 [DOI] [PubMed] [Google Scholar]
- 27.Wolf J, Mattila K, Ankkuriniemi O. Development of a Stafne mandibular bone cavity. Report of a case. Oral Surg Oral Med Oral Pathol 1986; 61: 519–21. doi: 10.1016/0030-4220(86)90398-1 [DOI] [PubMed] [Google Scholar]
- 28.Barker GR. A radiolucency of the ascending ramus of the mandible associated with invested parotid salivary gland material and analogous with a Stafne bone cavity. Br J Oral Maxillofac Surg 1988; 26: 81–4. doi: 10.1016/0266-4356(88)90155-6 [DOI] [PubMed] [Google Scholar]
- 29.Tominaga K, Kuga Y, Kubota K, Ohba T. Stafne's bone cavity in the anterior mandible: report of a case. Dentomaxillofac Radiol 1990; 19: 28–30. doi: 10.1259/dmfr.19.1.2387472 [DOI] [PubMed] [Google Scholar]
- 30.Grellner TJ, Frost DE, Brannon RB. Lingual mandibular bone defect: report of three cases. J Oral Maxillofac Surg 1990; 48: 288–96. doi: 10.1016/0278-2391(90)90396-J [DOI] [PubMed] [Google Scholar]
- 31.Ariji E, Fujiwara N, Tabata O, Nakayama E, Kanda S, Shiratsuchi Y, et al. Stafne's bone cavity. classification based on outline and content determined by computed tomography. Oral Surg Oral Med Oral Pathol 1993; 76: 375–80. doi: 10.1016/0030-4220(93)90271-5 [DOI] [PubMed] [Google Scholar]
- 32.Tsui SH, Chan FF. Lingual mandibular bone defect. Case report and review of the literature. Aust Dent J 1994; 39: 368–71. doi: 10.1111/j.1834-7819.1994.tb03108.x [DOI] [PubMed] [Google Scholar]
- 33.Graham RM, Duncan KA, Needham G. The appearance of Stafne's idiopathic bone cavity on magnetic resonance imaging. Dentomaxillofac Radiol 1997; 26: 74–5. doi: 10.1038/sj.dmfr.4600224 [DOI] [PubMed] [Google Scholar]
- 34.Reuter I. An unusual case of Stafne bone cavity with extra-osseous course of the mandibular neurovascular bundle. Dentomaxillofac Radiol 1998; 27: 189–91. doi: 10.1038/sj.dmfr.4600349 [DOI] [PubMed] [Google Scholar]
- 35.Apruzzese D, Longoni S. Stafne cyst in an anterior location. J Oral Maxillofac Surg 1999; 57: 333–8. doi: 10.1016/S0278-2391(99)90684-5 [DOI] [PubMed] [Google Scholar]
- 36.Branstetter BF, Weissman JL, Kaplan SB. Imaging of a Stafne bone cavity: what Mr adds and why a new name is needed. AJNR Am J Neuroradiol 1999; 20: 587–9. [PMC free article] [PubMed] [Google Scholar]
- 37.Junquera LM, Albertos JM, Ferreras J, Baladron J. Stafne bone cyst. revision of four cases, one of them with bilateral affectation. Ann Otolaryngol Chir Cervicofac 1999; 116: 295–8. [PubMed] [Google Scholar]
- 38.Boyle CA, Horner K, Coulthard P, Fleming GJ. Multiple Stafne bone cavities: a diagnostic dilemma. Dent Update 2000; 27: 494–7. doi: 10.12968/denu.2000.27.10.494 [DOI] [PubMed] [Google Scholar]
- 39.de Courten A, Küffer R, Samson J, Lombardi T. Anterior lingual mandibular salivary gland defect (Stafne defect) presenting as a residual cyst. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2002; 94: 460–4. doi: 10.1067/moe.2002.125196 [DOI] [PubMed] [Google Scholar]
- 40.Dorman M, Pierse D. Ectopic salivary gland tissue in the anterior mandible: a case report. Br Dent J 2002; 193: 571–2. doi: 10.1038/sj.bdj.4801629 [DOI] [PubMed] [Google Scholar]
- 41.Longo F, Piombino P, Califano L. Stafne's bone cyst. Plast Reconstr Surg 2003; 111: 1369–70. doi: 10.1097/00006534-200303000-00080 [DOI] [PubMed] [Google Scholar]
- 42.Campos PSF, Panella J, Crusoé-Rebello IM, Azevedo RA, Pena N, Cunha T. Mandibular ramus-related Stafne's bone cavity. Dentomaxillofac Radiol 2004; 33: 63–6. doi: 10.1259/dmfr/39682286 [DOI] [PubMed] [Google Scholar]
- 43.Queiroz LMG, Rocha RS, de Medeiros KB, da Silveira EJD, Lins RDAU, Guedes Queiroz LM. Anterior bilateral presentation of Stafne defect: an unusual case report. J Oral Maxillofac Surg 2004; 62: 613–5. doi: 10.1016/j.joms.2003.04.019 [DOI] [PubMed] [Google Scholar]
- 44.Phillips A, Yates C. Case report: anterior lingual mandibular cortical bone concavity. Dent Update 2004; 31: 175–6. doi: 10.12968/denu.2004.31.3.175 [DOI] [PubMed] [Google Scholar]
- 45.Minowa K, Inoue N, Izumiyama Y, Ashikaga Y, Chu B, Maravilla KR, et al. Static bone cavity of the mandible: computed tomography findings with histopathologic correlation. Acta Radiol 2006; 47: 705–9. doi: 10.1080/02841850600796517 [DOI] [PubMed] [Google Scholar]
- 46.Segev Y, Puterman M, Bodner L. Stafne bone cavity--magnetic resonance imaging. Med Oral Patol Oral Cir Bucal 2006; 11: e345–7. [PubMed] [Google Scholar]
- 47.Bornstein MM, Wiest R, Balsiger R, Reichart PA. Anterior Stafne's bone cavity mimicking a periapical lesion of endodontic origin: report of two cases. J Endod 2009; 35: 1598–602. doi: 10.1016/j.joen.2009.08.008 [DOI] [PubMed] [Google Scholar]
- 48.Kao Y-H, Huang I-YE, Chen C-M, Wu C-W, Hsu K-J, Chen C-M. Late mandibular fracture after lower third molar extraction in a patient with Stafne bone cavity: a case report. J Oral Maxillofac Surg 2010; 68: 1698–700. doi: 10.1016/j.joms.2009.06.019 [DOI] [PubMed] [Google Scholar]
- 49.Kopp S, Ihde S, Bienengraber V. Differential diagnosis of stafne idiopathic bone cyst with digital volume tomography (DVT. J Maxillofac Oral Surg 2010; 9: 80–1. doi: 10.1007/s12663-010-0023-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Krafft T, Eggert J, Karl M. A Stafne bone defect in the anterior mandible--a diagnostic dilemma. Quintessence Int 2010; 41: 391–3. [PubMed] [Google Scholar]
- 51.Turkoglu K, Orhan K. Stafne bone cavity in the anterior mandible. J Craniofac Surg 2010; 21: 1769–75. doi: 10.1097/SCS.0b013e3181f40347 [DOI] [PubMed] [Google Scholar]
- 52.Flores Campos PS, Oliveira JAC, Dantas JA, de Melo DP, Pena N, Santos LAN, et al. Stafne's defect with buccal cortical expansion: a case report. Int J Dent 2010; 2010: 1–3. doi: 10.1155/2010/515931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vieira Aguiar LB, Sampaio neves F, Costa Bastos L, Crusoe-Rebello I, Bovi Ambrosano GM, Flores Campos PS. Multiple Stafne bone defects: a rare entity. ISNR Dentistry 2011; 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li B, Long X, Cheng Y, Wang S. Cone beam CT sialography of Stafne bone cavity. Dentomaxillofac Radiol 2011; 40: 519–23. doi: 10.1259/dmfr/84472023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dereci O, Duran S. Intraorally exposed anterior Stafne bone defect: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: e1–3. doi: 10.1016/j.tripleo.2011.07.029 [DOI] [PubMed] [Google Scholar]
- 56.Etöz M, Etöz OA, Şahman H, Şekerci AE, Polat HB. An unusual case of multilocular Stafne bone cavity. Dentomaxillofac Radiol 2012; 41: 75–8. doi: 10.1259/dmfr/34731967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Friedrich RE, Zustin J, Scheuer HA, Assaf AT, Gröbe A. An unilateral basal bone defect of the mandible occupied by fatty tissue: Stafne's cavity. In Vivo 2012; 26: 1045–8. [PubMed] [Google Scholar]
- 58.Münevveroğlu AP, Aydın KC. Stafne bone defect: report of two cases. Case Rep Dent 2012; 2012: 1–5. doi: 10.1155/2012/654839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Boffano P, Gallesio C, Daniele D, Roccia F. An unusual trilobate Stafne bone cavity. Surg Radiol Anat 2013; 35: 351–3. doi: 10.1007/s00276-012-1043-7 [DOI] [PubMed] [Google Scholar]
- 60.Prechtl C, Stockmann P, Neukam FW, Schlegel KA. Enlargement of a Stafne cyst as an indication for surgical treatment - a case report. J Craniomaxillofac Surg 2013; 41: 270–3. doi: 10.1016/j.jcms.2012.10.013 [DOI] [PubMed] [Google Scholar]
- 61.Saglam M, Salihoglu M, Sivrioglu AK, Kara K. Multimodality imaging of Stafne bone defect. BMJ Case Rep 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Herranz-Aparicio J, Figueiredo R, Gay-Escoda C. Stafne's bone cavity: an unusual case with involvement of the buccal and lingual mandibular plates. J Clin Exp Dent 2014; 6: e96–9. doi: 10.4317/jced.51229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim H, Seok JY, Lee S, An J, Kim NR, Chung DH, et al. Bilateral stafne bone cavity in the anterior mandible with heterotopic salivary gland tissue: a case report. Korean J Pathol 2014; 48: 248–9. doi: 10.4132/KoreanJPathol.2014.48.3.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Miloğlu Özkan, Sekerci AE, Yasa Y, Dagistan S. Unilateral bone cavities situated near the angle of the mandibula. J Craniofac Surg 2015; 26: e27–8. doi: 10.1097/SCS.0000000000001262 [DOI] [PubMed] [Google Scholar]
- 65.Probst FA, Probst M, Maistreli I-Z, Otto S, Troeltzsch M. Imaging characteristics of a Stafne bone cavity--panoramic radiography, computed tomography and magnetic resonance imaging. Oral Maxillofac Surg 2014; 18: 351–3. doi: 10.1007/s10006-014-0454-5 [DOI] [PubMed] [Google Scholar]
- 66.Schneider T, Filo K, Stadlinger B, Locher M, Kruse AL, Luebbers H-T. Eine ungewoenliche Stafne-kavitaet. Swiss Dental J 2014; 124: 545–50. [DOI] [PubMed] [Google Scholar]
- 67.Taysi M, Ozden C, Cankaya B, Olgac V, Yıldırım S. Stafne bone defect in the anterior mandible. Dentomaxillofac Radiol 2014; 43: 20140075. doi: 10.1259/dmfr.20140075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lee KH, Thiruchelvam JK, McDermott P. An unusual presentation of Stafne bone cyst. J Maxillofac Oral Surg 2015; 14: 841–4. doi: 10.1007/s12663-014-0737-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mauprivez C, Sahli Amor M, Khonsari RH. Magnetic resonance sialography of bilateral Stafne bone cavities. Journal of Oral and Maxillofacial Surgery 2015; 73: 934.e1–934.e7. doi: 10.1016/j.joms.2015.01.034 [DOI] [PubMed] [Google Scholar]
- 70.More CB, Das S, Gupta S, Patel P, Saha N. Stafne's bone cavity: a diagnostic challenge. J Clin Diagn Res 2015; 9: ZD16–19. doi: 10.7860/JCDR/2015/14273.6772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ozaki H, Ishikawa S, Kitabatake K, Yusa K, Tachibana H, Iino M. A case of simultaneous unilateral anterior and posterior Stafne bone defects. Case Rep Dent 2015; 2015: 1–5. doi: 10.1155/2015/983956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Venkatesh E. Stafne bone cavity and cone-beam computed tomography: a report of two cases. J Korean Assoc Oral Maxillofac Surg 2015; 41: 145–8. doi: 10.5125/jkaoms.2015.41.3.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Atil F, Adisen MZ, Misirlioglu M, Suer BT. Atafne bone cavity complicated by periapical infection. J Coll Phys Surg Pakistan 2016; 26: S109–10. [PubMed] [Google Scholar]
- 74.Chen CA, Ahn Y, Odell S, Mupparapu M, Graham DM. Developmental salivary gland depression in the ascending mandibular ramus: a cone-beam computed tomography study. Imaging Sci Dent 2016; 46: 223–7. doi: 10.5624/isd.2016.46.3.223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Deyhimi P, Darisavi S, Khalesi S. Stafne bone cavity with ectopic salivary gland tissue in the anterior of mandible. Dent Res J 2016; 13: 454–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee JI, Kang SJ, Jeon SP, Sun H, Sum H. Stafne bone cavity of the mandible. Arch Craniofac Surg 2016; 17: 162–4. doi: 10.7181/acfs.2016.17.3.162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hisatomi M, Munhoz L, Asaumi J, Arita ES. Parotid mandibular bone defect: a case report emphasizing imaging features in plain radiographs and magnetic resonance imaging. Imaging Sci Dent 2017; 47: 269–73. doi: 10.5624/isd.2017.47.4.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.da Silva W-G, Kemp A-T, Dos Santos-Silva A-R, Diz MDP-E, Brandão T-B. Stafne's bone defect in a metastatic prostate cancer patient: a diagnostic conundrum. J Clin Exp Dent 2018; 10: e88–91. doi: 10.4317/jced.53656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kaya M, Ugur KS, Dagli E, Kurtaran H, Gunduz M. Stafne bone cavity containing ectopic parotid gland. Braz J Otorhinolaryngol 2018; 84: 669–72. doi: 10.1016/j.bjorl.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nishimura S, Osawa K, Tanaka T, Imamura Y, Kokuryo S, Habu M, et al. Multiple mandibular static bone depressions attached to the three major salivary glands. Oral Radiol 2018; 34: 277–80. doi: 10.1007/s11282-017-0304-x [DOI] [PubMed] [Google Scholar]
- 81.Lee KC, Yoon AJ, Philipone EM, Peters SM. Stafne bone defect involving the ascending ramus. J Craniofac Surg 2019; 30: e301–3. doi: 10.1097/SCS.0000000000005252 [DOI] [PubMed] [Google Scholar]
- 82.Bayrak NB. A rare presentation of stafne bone cyst. J Stomatol Oral Maxillofac Surg 2019;12 Feb 2019. doi: 10.1016/j.jormas.2019.02.006 [DOI] [PubMed] [Google Scholar]