Abstract
Introduction:
Migraine is the second leading cause of disability worldwide, yet many patients are unable to tolerate, benefit from, or afford pharmacological treatment options. Non-pharmacological migraine therapies exist, especially to reduce opioid use, which represents a significant unmet need. Mindfulness-based interventions (MBI) have potential as a non-pharmacological treatment for migraine, primarily through the development of flexible attentional capacity across sensory, cognitive, and emotional experiences.
Areas Covered:
We review efficacy and potential mechanisms of MBIs for migraine, including mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT).
Expert Opinion:
While most mindfulness research studies for migraine to date have been pilot trials, which are small and/or lacked rigor, initial evidence suggests there, may be improvements in overall headache-related disability and psychological well-being. Many research questions remain to help target the treatment to patients most likely to benefit, including the ideal dosage, duration, delivery method, responder characteristics, and potential mechanisms and biomarkers. A realistic understanding of these factors is important for patients, providers, and the media. Mindfulness will not “cure” migraine; however, mindfulness may be an important tool as part of a comprehensive treatment approach to help patients “mindfully” engage in valued life activities.
Keywords: Complementary and Alternative Medicine, Integrative Medicine, Mindfulness, Migraine, Meditation, mindfulness-based stress reduction, mindfulness-based cognitive therapy, mind-body medicine, mindfulness-based intervention
1. Introduction
1.1. The Impact of Migraine and the Need for Non-Pharmacological Treatment Options
Migraine is the world’s second leading cause of disability worldwide, with high prevalence and negative social and occupational impact during a person’s peak years of productivity.[1–3] Migraine is a complex neurobiological condition involving attacks of head pain, light and noise sensitivity, nausea and/or vomiting, with clear diagnostic criteria defined by the International Classification of Headache Disorders (ICHD).[4] Over half of patients are so disabled during an attack that they require bedrest.[2] Migraine negatively affects relationships, career, financial stability and achievement, and overall health.[5]
Despite the excitement engendered by the advent of calcitonin gene-related peptide (CGRP) monoclonal antibodies that prevent migraine attacks, this new class of drug’s clinical success is limited by its high cost and unknown long-term risks and side effects. [6–8] Older pharmacological treatment options often lead to side effects and poor response, leading to high levels of unmet treatment needs.[9,10] Approximately 2/3 of all patients who try prescription medications for headache discontinue treatment due to lack of efficacy, untoward side effects, and inadequate relief. [11] Medication discontinuation occurs despite migraines significantly impacting patients’ lives, as 42% of patients who discontinue medications have moderate to severe levels of migraine-related disability.[12] In addition, the recent Migraine in America Symptoms and Treatment (MAST) Study (n=15,133 patients with migraine) demonstrated that 33% of Americans with migraine using acute prescription medications treat acute attacks with opioids.[13] This frequent use of opioids for migraine treatment occurs despite American Headache Society Guidelines against such use, given the risks of a) medication overuse headache; b) migraine progression from an episodic to a chronic state; and c) opioid use disorder.[14] Further, even people with migraine who have effective acute and preventive treatment on-board may experience significant levels of migraine-related interference with valued activities such as occupational and social functioning.[15,16] Thus, a significant need exists for safe non-pharmacological options with few side effects for migraine treatment.[17]
Lifestyle and psychosocial factors often play a role in the development and progression of migraine that pharmacological options often do not address. For example, stress is the most commonly perceived migraine attack trigger.[18] Therefore, treatment options targeting stress reduction may be of particular value for people with migraine. In the field of headache, behavioral treatment options have a long history of evidence supporting their benefit for reduction of attack frequency and headache-related disability.[19,20] Dr. Herb Benson broke new ground in the 1970’s with his research demonstrating that the “Relaxation Response” created a physiological response by decreasing sympathetic nervous system activity, with evidence of its benefit for headache.[21] In 2000, electromyographic (EMG) biofeedback, cognitive behavioral therapy (CBT), thermal biofeedback with relaxation, and relaxation training modalities were given Grade A evidence of benefit by the US Headache Consortium Guidelines for preventive treatment of migraine as they decrease headache frequency by 35–50%, an effect size comparable to pharmacological treatment options.[22]
The use of such behavioral and mind-body treatment options varies widely. Significant overlap exists between treatments labeled as “behavioral” (such as stress management training, biofeedback, and relaxation training) and “mind-body” (such as meditation, yoga, biofeedback, deep breathing, etc.).[17] Despite evidence of its benefit, the National Health Interview Survey (a nationally representative survey) demonstrated that <1% of the US population with headache uses biofeedback.[23] Yet 50% of adults with migraines/severe headaches report using complementary and alternative medicine (CAM), with mind-body treatment approaches used most frequently.[23] This includes deep breathing exercises, meditation, and yoga, all of which comprise the most common mind-body modalities used in adults with neurological conditions.[24] However, these results are limited by the uncertainty of whether these modalities are being used to treat migraine in any guided or specific way. Certain populations, such as pregnant women and children, who often avoid pharmacological treatments for migraine, are especially interested in CAM treatments. [25,26] Many use CAM in conjunction with pharmacological treatments.[27] Unfortunately, more than half of adults who use CAM do not discuss their use with their health care provider.[28] Current interest, availability, and access of treatment options all contribute to the variable uptake of use of these treatment modalities. [17]
1.2. Mindfulness-based Approaches to Treatment
Mindfulness meditation is an evidence-based mind-body intervention that teaches principles of mindfulness and how to apply them in daily life to handle illness and stress. More than two million adults in the US practice mindfulness meditation.[29] Mindfulness is defined as “paying attention in a particular way: on purpose, in the present moment, and non-judgmentally.” [30] Mindfulness is considered a basic human capacity to attend intentionally to sensory experiences, events, perceptions, cognitions, and/or emotions. In mindfulness-based interventions (MBIs), mindfulness meditation is a specific practice that builds one’s attention and awareness by initially focusing on physical bodily sensations, such as the breath, and returning the attention back again whenever the mind wanders away from the intended attentional focus.[31] As the practice progresses, moment-to-moment awareness of body sensations, emotions, and thoughts are enhanced with an attitude of acceptance and non-judgement, with a transition from focused attention to open awareness.[32] At its core, MBIs cultivate the capacity to pay attention to present moment experience with an orientation of openness, curiosity, and acceptance of whatever occurs.[33] Mindfulness meditation is considered separate from relaxation, as it involves a systematic cultivation of flexible attentional capacity for detached observations of one’s sensory, cognitive, and emotional experiences and may help develop experiences of personal “insight.”[34] Through the regular practice of mindfulness meditation, individuals may become more mindful in their day-to-day lives. This may occur during routine, benign activities like brushing one’s teeth; pleasant experiences like savoring and appreciating the usually mindless act of eating; and even “sitting with” and observing unpleasant experiences such as stress, discomfort, and pain.
In 1979, Dr. Jon Kabat-Zinn pioneered the development of a mainstream mindfulness meditation training program called Mindfulness-Based Stress Reduction (MBSR), which was originally developed to treat chronic pain patients.[35] MBSR is a systematic, intensive training in mindfulness meditation and mindful hatha yoga that creates a structured pathway for participants to learn how to practice, integrate, and apply mindfulness in everyday life.[36] The program’s standardized curriculum has been taught to >24,000 participants world-wide.[36] It involves eight weekly 2.5-hour classes on mindfulness meditation through a variety of practices, including body scan (i.e., a deliberate, sequential focus of attention on different body parts, with acceptance of the observed sensations), sitting meditation, walking meditation, and gentle moving meditation (based on Hatha yoga). Over the eight weeks, the meditation develops from a focused attention practice to the practice of open monitoring of one’s experience.[37,38] Participants are also trained to practice lovingkindness meditation, a compassion-oriented practice of mindfully cultivating feelings of goodwill towards oneself and others.[39] Throughout the MBSR course, participants discuss stress and illness, learning how to slow and modify their natural immediate reactions and instead respond wisely through mindful awareness. Dialogue about experiences and observations is encouraged and facilitated in each class to create an experiential inquiry-based learning process.[40] Participants are asked to practice guided meditations at home for 30–45 minutes/day, and to begin incorporating mindfulness into daily activities. Through the regular practice of mindfulness meditation, individuals are taught to become more mindful in their day-to-day lives with routine activities like brushing teeth.
While “second wave” psychological treatment approaches typically aim to modify situations and cognitions to more adaptively manage pain, mindfulness meditation is different as it recommends “turning toward” physical sensations, even painful ones, with a curious, accepting, and non-judgmental attitude.[40] A multitude of studies have been conducted on the benefits of mindfulness meditation for a variety of clinical outcomes, including overall well-being, chronic illness self-management, and improvements in sleep, depression, anxiety, and mild cognitive impairment. [41–51] Mindfulness has especially shown benefit for chronic pain conditions, with preliminary promising evidence in headache. [52–55]
Mindfulness-Based Cognitive Therapy (MBCT) is a mindfulness-based intervention originally developed to treat depression that incorporates features of both cognitive behavioral therapy (CBT) and MBSR.[56] MCBT focuses on changing thought patterns and resulting behaviors by training in mindfulness-based coping skills, problem solving, and psychoeducation. Cognitive restructuring of maladaptive thought processes is taught to improve adaptive cognitive content such as acceptance and to decrease maladaptive content such as pain catastrophizing.[56] MBCT has demonstrated benefit in addressing the cognitive aspects of depression as in CBT, while also positively affecting acceptance, perceived stress, and overall well-being as in MBSR.[57–60]
Although the MBSR program was originally developed to target chronic pain, patients with episodic migraine attacks may also benefit. However, it is important to recognize that many differences exist between chronic pain conditions and migraine that need to be accounted for in research and clinical practice. Unlike most chronic pain conditions, migraine is classified as “episodic” or “Chronic” based on headache frequency, not disease duration, such that those having attacks < 15 days/month are diagnosed as having ‘episodic migraine’ and those with at least 15 days/month are diagnosed as having ‘chronic migraine.’ Therefore, episodic migraine patients may have a life-long history of migraine but are not labeled as “chronic.” Further, while some patients with “chronic migraine” may have constant baseline pain, the majority of people with migraine are pain free most of the time, and intermittently have sudden unexpected and severe attacks that include pain as well as a myriad of other noxious neurologic symptoms. Even people who experience daily headache activity often still experience acute attacks of severe worsening of intensity, change in pain quality, and associated symptoms. Patients with migraine live with a sense of uncertainty and fear of when an attack will occur or be exacerbated, often resulting in significant anticipatory anxiety and pain catastrophizing. While most mindfulness studies in headache were designed to teach mindfulness as a preventive-treatment option, it is uncertain in the studies how often participants used the tools learned as an acute-treatment approach.
1.3. Mindfulness Research in Migraine: Overview, Methods, and Scope of Current Review
With the growth of research on MBIs, [32,40,61] recent evidence is emerging that demonstrates the potential benefit of these interventions in patients with migraine. This paper provides a narrative review of the evidence of MBIs as a non-pharmacological treatment approach for migraine, with an overview of the migraine specific studies provided in Table 1 and quality ratings of the studies in Table 2.
Table 1:
Clinical Research Studies Evaluating Mindfulness-Based Interventions in Migraine
| Article & Location & Yates Quality Rating Scale (YQRS) | Headache Type | Study Characteristics | Results | Strengths Limitations |
|---|---|---|---|---|
| Wells et al.[83] 2014 Boston, MA YQRS=31 |
Episodic Migraine, 4–14 migraine days/ month |
Intervention: MBSR as adjunctive to pharmacological treatments Control group: Wait-list Sample Size: n=19 Average age: 46 |
• Feasible, acceptable • Primary outcome (HA frequency): • Both groups decreased HA frequency, no statistical difference • Positive secondary outcomes-MBSR group improved: • Migraine duration • Disability • Self-efficacy • Mindfulness |
Strengths • Standardized MBSR program • Participants randomized & blinded to control group assignment • HA diaries used • Primary & secondary outcomes clearly defined Limitations • Small sample size (pilot study), underpowered • No active control group |
| Seng et al.[79] 2019 Bronx & Manhattan, NY YQRS=31 |
Migraine, 6–30 headache days/ month |
Intervention: MBCT-Individual therapist Control Group: Waitlist/ Treatment as usual Sample Size:n=60 Average Age: 40 |
• Primary outcome (disability) positive: MBCT group had improvements vs. control: • Migraine related disability • Attack level disability • Secondary outcomes: no improvements in HA frequency or intensity • Both groups had improvements in severe disability ratings |
Strengths • Well-defined primary outcome of disability • Treatment fidelity measures assessed & described • HA diaries used • Primary & secondary outcomes clearly defined Limitations • No active control group • Study stopped prior to reaching recruitment goals • Mixed migraine population of both episodic and chronic migraine |
| Day et al.[85] 2014 Northport & Tuscaloosa, AL YQRS=29 |
Any primary headache (migraine, tension-type, cluster, etc.) |
Intervention: MBCT-group based Control Group: Delayed treatment Sample Size: n=36 Average Age: 42 |
• Feasible, acceptable, tolerable • Primary outcomes (HA frequency, duration, intensity): • Both groups decreased HA frequency, no statistical difference • Secondary outcomes: MBCT group-improved: • Self-efficacy • Chronic pain acceptance |
Strengths • 1st study of MBCT in headache • Primary & secondary outcomes clearly defined Limitations • Un-blinded • Heterogeneous headache population (any primary headache condition) |
| Simshäuser et al.[82] 2019 Freiburg, Germany YQRS=26 |
Episodic migraine, 2–15 migraines/ month |
Intervention: MBSR Control Group: HA education + Behavioral (3 sessions) Sample Size: n=62 Average Age: 44 |
• Primary outcome (HA frequency): • Both groups decreased HA frequency, no statistical difference • Secondary outcomes: MBSR had greater improvements than control group in: • Psychological symptoms • Anxiety • Self-efficacy • Sensory component of pain |
Strengths • Standardized MBSR program • Active control group • HA diaries used • 12 month follow-up • Primary & secondary outcomes clearly defined Limitations • Pilot study • High dropout rates • Control group may have been too active • 19% of MBSR participants had baseline HA frequency <2, no room for improvement |
| Tavallaei et al.[86] 2018 Tehran, Iran YQRS=19 |
Tension-type or migraine headache |
Intervention: MBSR “internet-based bibliotherapy” Control Group: Treatment as usual Sample Size: n=30 Average Age: 34 |
• MBSR group had improvements vs. control: • Pain intensity • Disability • Distress • Mindfulness • Emotional pain |
Strengths • Unique self-guided approach Limitations • Intervention not clearly defined • No HA outcomes measured with daily diaries • Heterogeneous headache population (tension-type & migraine) • Primary & secondary outcomes not clearly defined |
| Bakhshani et al.[87] 2015 Zahedan, Iran YQRS=18 |
Chronic migraine and chronic tension-type headache |
Intervention: MBSR as adjunctive to pharmacological treatments Control Group: Usual care Sample Size: n=40 Average Age:31 |
• MBSR group had improvements vs. control: • Pain intensity • Short form (SF)-36 |
Strengths • Chronic headache patients Limitations • Heterogeneous HA population (migraine & tension-type) • No HA outcomes measured with daily diaries • Primary & secondary outcomes not clearly defined |
| Hess et al. [88] 2015 Salt Lake City, UT YQRS=18 |
“Recurrent headache” 4+/month |
Intervention: adapted MBSR Control Group: No control group Sample Size: n=20 Average Age:14 |
• Primary outcome: Safe, feasible • Secondary outcomes: MBSR participants (without a comparison) had: • Improvements in depression symptoms, pain withdrawal • Parents of participants reported improved quality of life |
Strengths • Study in adolescent females • Primary & secondary outcomes clearly defined Limitations • No control group • Non-randomized • High dropout rates • HA outcomes not analyzed • Heterogeneous headache population (“recurrent headache”) • All females |
| Grazzi et al.[80] 2017 Milan, Italy YQRS=17 |
Chronic migraine-medication overuse headache |
Intervention: Mindfulness training Control Group: Pharmacological treatment Sample Size: n=44 Average Age: 45 |
• Primary outcomes (headache frequency, use of acute medications), both groups had decreases in: • HA frequency • Medication usage • Secondary outcomes, both groups improved: • Disability • Depression |
Strengths • Clinically applicable • Mindfulness compared to pharmacological treatment • HA diaries used • 12 month follow-up Limitations • Non-randomized: participants non-blinded & chose treatment assignment |
Table 2:
Yates Quality Rating Scale (YQRS)[62] of Studies Evaluating Mindfulness for Migraine
| Yates Quality Rating Scale Details | Studies Included | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Items | Options | Wells 2014 [83] | Seng 2019 [79] | Day 2014 [85] | Simshäuser 2019 [82] | Tavallaei 2018 [86] | Bakhshani 2015 [87] | Hesse 2015 [88] | Grazzi 2017 [80] |
| Treatment quality | |||||||||
| Treatment content and setting | 0, 1, 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 |
| Treatment duration | 0, 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 |
| Manualization | 0, 1, 2 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 1 |
| Adherence to manual | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Therapist training | 0, 1, 2 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 1 |
| Patient engagement | 0, 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 |
| Quality of study design and methods | |||||||||
| Sample criteria | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Evidence criteria met | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Attrition | 0, 1, 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 |
| Rates of attrition | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Sample characteristics | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Group equivalence | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| Randomization | 0, 1, 2 | 2 | 2 | 2 | 2 | 1 | 1 | 0 | 0 |
| Allocation bias | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| Measurement bias | 0, 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Treatment expectations | 0, 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| Justification of outcomes | 0, 1, 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 |
| Validity of outcomes for context | 0, 1, 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 |
| Reliability and sensitivity to change | 0, 1, 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 |
| Follow-up | 0, 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 |
| Power calculation | 0, 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sufficient sample size | 0, 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Planned data analysis | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Statistics reporting | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Intention-to-treat analysis | 0, 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| Control group | 0, 1, 2 | 1 | 1 | 2 | 1 | 2 | 1 | 0 | 1 |
| Total score/35 | 31 | 31 | 29 | 26 | 19 | 18 | 18 | 17 | |
The Yates Quality Rating Scale (YQRS) was used to assess study quality and bias, with an assessment of treatment quality and the quality of study design and methods.[62] Two authors (CP and LR) independently assessed study quality, then resolved differences by consensus. Studies ranged in quality from 17–31 (out of 35), with higher scores demonstrating greater quality. Studies will be presented in this review in order of scoring. The potential mechanisms, research and clinical application challenges, and additional research questions are also addressed. Studies evaluating mindfulness specifically for tension-type headache or other primary headache disorders are not discussed given this paper’s focus on migraine.[63–66] Studies with heterogeneous populations (e.g., migraine plus other headache conditions) were included. In addition, this review focuses on mindfulness treatment modalities and excludes studies conducted specifically evaluating other types of integrative or mind-body therapies such as acceptance and commitment therapy, yoga, tai chi, relaxation, supplements, manipulative treatments (massage/acupuncture) and other psychological treatments such as cognitive behavioral therapy, which are reviewed elsewhere.[67–71] Studies evaluating mindfulness meditation plus yoga (such as MBSR), were included. Studies conducted for treatment of migraine using other types of meditation, such as “spiritualized meditation,” [72–75] are not included in this review. One small study assessed a lovingkindness meditation intervention as an acute-treatment option for migraine with promising results, but will not be discussed here as it was not considered an MBI.[76]
Two systematic reviews and meta-analyses evaluating MBIs in headaches were published in 2018 and 2019, [77,78] but several important studies that are described in this narrative review published since 2017 were not included in either of these reviews and may have influenced the results.[79–82] In brief, Gu and colleagues analyzed controlled trials published up to 2016 of structured meditation programs (including both MBSR, MBCT, and other meditation programs) in adults with any type of primary headache, including migraine and tension-type, and included 10 RCTs and 1 controlled clinical trial with a total of 315 patients.[77] Control groups included medication and clinical management, relaxation, education class, delayed treatment, usual pharmacotherapy, and wait-list groups. The studies evaluated in their meta-analysis are all described in detail in our narrative review except for the studies of tension-type headaches. YQRS was used to assess quality and bias; with seven of the publications considered “low risk of bias” and four publications considered “high risk of bias.” Results of their meta-analyses found that when compared to control group data, mindfulness meditation resulted in significant improvements in pain intensity, headache frequency, and self-efficacy. Subgroup analyses showed positive effects of: MBSR interventions (compared to other meditative interventions or other MBIs) and 8-week treatment durations (compared to shorter interventions); patients with migraine headaches (compared to tension-type) and older participants appeared to derive the greatest benefit.
Anheyer and colleagues conducted a similar systematic review and meta-analysis except that it differed from Gu’s review by only including randomized studies specifically evaluating MBSR or MBCT with headache frequency, duration and/or intensity as a primary outcome. This resulted in a meta-analysis of only five of the 11 studies from Gu’s review (n=185 patients; two were exclusively in tension-type headache patients).[78] Risk of bias was assessed with the Cochrane Risk of Bias Tool and most studies had high or unclear risk of bias; only one study had mostly low risk of bias.[83] This meta-analysis demonstrated no significant improvements in headache frequency, duration, or intensity and the authors concluded that the high or unclear risk of bias led to imprecise results. Unfortunately, disability outcomes and other important psychological outcomes of interest (self-efficacy, depression, anxiety, etc.) were not included in Anheyer’s meta-analysis. Our narrative review provides additional details to help understand the studies included in these systematic reviews and includes three additional studies published since these reviews were conducted.[79–82]
2. Mindfulness Based Interventions in Migraine: Current Evidence
The goals of our narrative review are to inform both the patient and provider about the evidence and mechanisms of mindfulness meditation in migraine, to encourage discussion of use and awareness of the potential realistic benefits with treatment. This review focuses on the evidence of MBIs that evaluated migraine with clinical outcomes. The YQRS score provides information to assess study design, methods, bias, and treatment quality. The studies included in this review have YQRS scores ranging from 17–31 (out of 35), with higher scores demonstrating greater quality. Studies are presented in this review from highest to lowest YQRS score.
In the first published randomized controlled pilot study of MBSR specific to adults with episodic migraine with or without aura (YQRS=31), Dr. Wells and colleagues demonstrated the feasibility and acceptability of MBSR with this population and presented initial evidence on its impact on important migraine-related outcomes.[83] Participants (n=19) with 4–14 days/month with migraine (diagnosed by ICHD-II diagnostic criteria through evaluation by a headache specialist) were randomized to either MBSR or usual care in Boston, MA. Participants were able to continue stable dosages of all acute and prophylactic headache medications and were blinded to control group assignment. Both groups received MBSR, but the group that started the program three months ahead of the second group served as the “wait-list” control for the first group. MBSR demonstrated excellent safety (no adverse events reported) and feasibility, with median class attendance of 8/9 (including retreat day) and average MBSR home practice of 34 minutes/day (range 16–50 minutes/day). Headache features were tracked with daily headache logs begun a month prior to randomization and continued for the duration of the study. The primary outcome of headache frequency was not statistically significantly different between groups, although MBSR participants had 1.4 fewer migraines/month after the intervention compared to before and their migraines were less severe (−1.3 points on 0–10 scale, p=0.053). Secondary outcomes demonstrated that MBSR participants reported a statistically significantly shorter migraine duration after intervention compared to the control group (−2.9 hours/headache, p=0.043), as well as reduced disability with Migraine Disability Assessment Scale (MIDAS, −12.6, p=0.017) and Headache Impact Test (HIT)-6,−4.8, p=0.043). Headache management self-efficacy and mindfulness also had statistically significant improvements in MBSR vs. control (13.2 [1.0, 30.0], p=0.035 and 13.1 [3.0, 26.0], p=0.35 respectively). Our study demonstrated the feasibility and acceptability of the intervention in adults with migraines, and showed a clinically meaningful impact of the intervention on headache duration, disability, mindfulness, and self-efficacy. While promising, the study was not powered for efficacy evaluation and did not have an active control group, which should be taken into consideration when interpreting these results.
Seng et al.[79] conducted a two-arm parallel randomized clinical trial (YQRS=31) comparing individualized MBCT for migraine protocol to wait-list/treatment as usual for adults (n=60) with 6–30 days/month of migraine [stratified by episodic migraine (<15 headache days/month) n= 29; and chronic migraine (>=15 days/month) n= 31]; diagnosed with ICHD-3 beta criteria).[79] Participants kept one-month headache diaries during the baseline evaluation period and after the intervention, which involved eight individual 75-minute sessions with a supervised doctoral student therapist over 8–10 weeks. Sessions included education, cognitive exercises, and mindfulness practices, with mindfulness meditation homework assignments modified to be applicable to migraine. Treatment fidelity was assessed and rated as high. The primary outcome was defined a priori as disability (with both MIDAS and Headache Disability Inventory, HDI). Participants in the MBCT group had improvements in the HDI compared to the control group (−14.3/100 vs. −0.2/100, p<0.001), but not for MIDAS when correcting for multiple comparisons (p=0.027). Moderation and subgroup analyses revealed MBCT-related decreases were significant only in the episodic migraine group for both the MIDAS (−40.0% vs. −14.3%; moderation p = 0.013) and the HDI (−14.4/100 vs. −2.0/100; subgroup p=0.011).[84] No changes were seen in headache frequency outcomes. A secondary disability outcome (MIDI, Migraine disability index) also improved in the MBCT group but worsened in the control group (p=0.007 for the comparison of changes across groups). This study demonstrates that MBCT may be an effective treatment to target headache-related disability. The control group was not an active intervention, therefore some of the effects observed may have been nonspecific to any intensive therapeutic relationship. The goal sample size was not reached, which limited power.
Day and Thorn conducted a pilot RCT of a group-based MBCT program (YQRS=27) using a parallel-group design in 36 adults with any primary headache disorder (migraine, tension-type, cluster, etc. as defined by IHS).[85] They demonstrated that MBCT was feasible, tolerable, and acceptable, but group comparisons of primary outcomes (headache frequency, duration, intensity) were negative, as both groups had decreases in headache frequency without statistically significant group differences. Secondary outcomes showed improvements in self-efficacy and pain acceptance in the MBCT group. This was the first study conducted of MBCT in headache, but was limited by its heterogeneous headache sample and lack of headache-specific disability measures.
In 2019, Simshauser and colleagues published a study designed to test feasibility and provide estimations of effect sizes of MBSR vs. an active control intervention (YQRS=26) in 62 adults with 2–15 migraines/month with or without aura (diagnosed by ICD-10 codes by the trial physician) in Freiburg, Germany.[82] The active control condition included instruction on progressive muscle relaxation and psychoeducation, with the information specifically targeting migraine (e.g., migraine pathophysiology, triggers, and prodromal symptoms). Behavioral techniques were also taught, including pacing one’s activities, exercising, keeping consistent sleep cycles, relaxation, and strategies for early migraine identification and treatment. While the MBSR group met weekly, the control group only met three times during the eight-week period of the course; both groups were instructed to practice at home with audio recordings of guided exercises. The dropout rate in the control group was significantly higher compared to the MBSR group (40% vs. 19%, respectively, at initial follow-up) so the authors conducted analyses per-protocol rather than intention-to-treat. The primary outcome, days with migraine/month (tracked with daily headache diaries completed 4 weeks before and 4 weeks after the course), decreased in both groups (MBSR 4.9 to 3.6 days/month and control group 4.2 to 3.2 days/month), but without statistical difference between groups. Secondary outcomes showed that, following treatment, MBSR participants had lower general severity index and anxiety subscale scores of the Brief Symptom Inventory than those in the control group (p<0.01 for both comparisons), and had greater perceived self-efficacy and perception of sensory components of pain but not affective perception of pain (measured with the Pain Perception Scale). Improvements seen on psychological variables were maintained one year after baseline in the MBSR group. Nearly all (96%) of MBSR participants were satisfied or very satisfied with treatment, compared to 79% of control group participants. Homework practice was maintained in 67% of MBSR participants vs. 16% of control participants. A strength of this study includes the use of an active control condition; however, the study was not powered for, or analyzed as, comparative effectiveness therefore the null results observed are challenging to interpret. Limitations include the high control group dropout rate, lack of an intent-to-treat analysis, and inappropriate inclusion criteria that contributed to a floor effect (19% of the MBSR participants had less than two headaches during the baseline period, leaving no room for improvement).
The MBSR program’s eight weekly in-person classes can lead to challenges with participant adherence and availability, leading to the development of program variations. A 2018 study evaluated an eight-session MBSR “Internet-based bibliotherapy” (YQRS=19) for patients (n=30) randomly sampled from 1396 patients from a headache clinic in Tehran, Iran, with tension type or migraine headache (diagnosed by physician using ICHD criteria).[86] Participants were randomized to either treatment as usual (n=15) or the active intervention (n=15), which involved independent reading of a mindfulness text created for this project with eight weekly goals and exercises. Those in the active treatment group had greater improvements than the control group in survey responses of pain intensity (p=0.035, d=0.39), headache-related disability (p<0.0001, d=1.26), distress (p<0.0001, d=0.59) and mindfulness (p<0.0001, d=2.25). The subscales of the pain intensity measures showed improvements in the emotional dimensions of pain (p<0.0001) but not in sensory dimension (p<0.44). This study provided participants with a unique self-guided approach to learning mindfulness and demonstrated meaningful improvements, although headache frequency was not assessed with diaries, the population of headache patients was heterogeneous, and primary and secondary outcomes were not defined a priori. The description of both interventions provided was also limited.
A study conducted in Zahedan, Iran evaluated typical pharmacological treatment under neurologist supervision (including specific and nonspecific drugs) plus either MBSR or usual care (YQRS=18) in patients with either chronic migraine or chronic tension-type headache (n=40) (diagnosed by neurologist using ICHD diagnostic criteria).[87] Participants’ responses on surveys of headache intensity (rated 0–10) and short-form 36 (SF-36) found that pain intensity and SF-36 improved after the MBSR intervention compared to the control group (SF-36 improvements seen on subscales of role limitations on physical health, bodily pain, general health, energy and vitality, affect health, and physical component summary score). This study demonstrated the potential for MBSR to have a positive benefit in a mixed population of chronic headache; however, the lack of headache diaries and additional measures of headache disability with no long-term follow-up limit the study’s full assessment of impact.
Many pediatric patients and their families often want to avoid pharmacological treatments for their headaches, thus mindfulness meditation may be an appealing treatment option. One non-randomized pilot study was conducted in Salt Lake City, Utah of a mindfulness intervention in 11–16 year-old females (n=20) with “recurrent headaches” (4+/month; no diagnostic criteria for migraine specified) as an adjunct to standard pharmacological treatments, (YQRS=18).[88] The mindfulness-based intervention was adapted from the Mindful Schools curriculum for adolescents, was similar to a typical MBSR course (eight weekly two hour classes with a trained MBSR instructor) and was intentionally only minimally tailored to discuss headaches. Participants were instructed to practice at home 10–15 min/day with guided audio recordings. Their primary outcome of safety of feasibility was met, with median class attendance of 7/8 and average home practice sessions 4.69 (SD=1.84) of 6/week. Secondary outcomes of depression and chronic pain acceptance (pain withdrawal subscale) improved, but PedMIDAS scores, anxiety, and quality of life did not change. Parents reported improved quality of life (with Pediatric Quality of Life inventory). Qualitative responses demonstrated that most felt the MBI helped with stress, relaxation, and pain. This small, non-randomized study was limited by attrition (25%), which led the authors to not conduct analyses of headache diaries.
Chronic migraine with medication overuse (CM-MOH) headache is a difficult-to treat headache population often refractory to interventions. A 2016 effectiveness (e.g., non-efficacy) study conducted in Milan, Italy on patients with CM-MOH (diagnosed by headache specialist using ICHD-3 beta) consisted of a structured outpatient medication withdrawal program, followed by the choice (e.g., non-randomized design) of either typical migraine prophylactic medication(s), or mindfulness training alone (YQRS=17).[80,81] Mindfulness training consisted of weekly 30-minute group sessions for 6 weeks. Participants (n=44; 22 in each group) had on average 20.5 baseline headaches/month. Both mindfulness and medication groups had improvement in the primary outcome of headache frequency (~6–8 days reduction/month in both groups) based on daily headache diaries, and both groups had around 50% of patients with 50% reduction of headaches at 12 months, with over 65% of patients no longer meeting chronic migraine criteria by 12 months. Similar improvements in both groups were also seen with a decreased use of acute medication, headache-related disability (MIDAS), and depression (Beck Depression Inventory), [80] with no changes on state and trait anxiety. This externally valid study demonstrates the potential of a mindfulness intervention to treat chronic migraine-medication overuse headache in routine clinical care, with effects comparable to pharmacological interventions. However, it was non-randomized and non-blinded; this is important because those most interested in mindfulness may be highly motivated and more likely to respond than those who are uninterested in mindfulness interventions. On the other hand, patients explicitly uninterested in mindfulness interventions are unlikely to be recommended these interventions as part of their care plan in routine clinical care.
3. Potential Mechanisms of Mindfulness in Migraine
Various mechanisms have been proposed to explain how mindfulness may be helpful for migraine. [89,90] While some mechanistic research has been conducted specific to migraine, many of the hypothesized mechanisms have been generated from research conducted in chronic pain populations and healthy controls administered experimental pain, which limits the interpretation of the results as these populations are distinct from migraine. Despite these limitations, the following section highlights some of the primary mechanisms hypothesized to be of benefit for migraine.
De-Coupling.
A psychological mechanism posits that the systematic cultivation of non-judgmental attention to sensations that is developed in mindfulness may result in an “de-coupling” of the sensory dimension of pain from the affective/evaluative dimension of pain, as the attitude of curiosity and non-attachment to sensations may reduce the experience of suffering via cognitive reappraisal.[35] This process was illuminated in one of the first studies of mindfulness for treatment of chronic pain, in which the authors identified two distinct categories of responders: (A) those that had a reduction or elimination of pain and (B) those that reported the pain was unchanged but their relationship to it had changed. [34] Specifically, the latter group of participants reported that there was less self-pity, less fear of pain, and less willingness to let pain/fear of pain restrict activity, suggesting a changed attitude and approach to coping with pain that resulted in the pain being less problematic and impactful in their lives. Some argue, however, that this model may not be appropriate for episodic migraine patients who do not experience constant pain.
Interoception.
Enhanced body awareness, or interoception, has also been recognized as a key mechanism of change in most mind-body therapies. Mindfulness may specifically promote this sense of unity between “body and self” [91] and such improved interoception may have many clinical benefits.[92,93] Embodied self-awareness and enhanced interceptive attention tendency may enhance patients’ ability to detect subtle changes in migraine symptomatology. Patients who apply mindfulness principles and techniques may learn to recognize early warning signs of migraine (premonitory neurologic symptoms that occur prior to the onset of head pain) which may allow for a meaningful cognitive or timely behavioral response. The resultant opportunity for early intervention may maximize treatment response, as taking a triptan earlier in migraine progression may enhance treatment response, as well as making behavioral changes such as reducing stress or moving to a less stimulating environment.[94] Additional research is needed to fully understand the importance and potential benefit of enhanced interoceptive body awareness in migraine treatment.
Neurological pathways.
For investigations of brain-based mechanisms, human neuroimaging research has investigated the neurobiological underpinnings of mindfulness training.[89,95] For example, in an fMRI study evaluating the impact of learning mindfulness on experimentally induced heat pain in healthy controls, mindfulness decreased pain unpleasantness-the “affective” component of pain, associated with orbitofrontal cortex activation-to a greater degree than pain intensity-the “sensory” component of pain, associated with increased activity in salience processing brain regions, such as anterior cingulate and anterior insula cortices.[96] These neuroimaging findings suggest that mindfulness meditation can engage multiple brain-based mechanisms that modulate the central processing of afferent nociceptive input, highlighting the potential value of MBIs in promoting adaptive reorganization of the brain circuitry that so often becomes dysregulated in the context of pain conditions.[97,98] Additional neuroimaging research has shown that mindfulness-based pain relief may have unique reappraisal mechanisms via higher order regulation (e.g., orbitofrontal cortex and rostral anterior cingulate cortex) of low-level nociceptive neural targets (e.g., thalamus and primary somatosensory cortex).[99] In fact, multiple neuroimaging studies conducted in a multitude of different ways (e.g., cross-sectional studies comparing meditators to non-meditators; longitudinal studies assessing impact of learning mindfulness; active meditating studies evaluating areas of brain activation, etc.) have linked regulation of specific brain regions following mindfulness training with clinical outcomes.[89] Most studies have shown involvement of some or all of these brain regions, including the anterior cingulate cortex (self-regulation of attention and emotion), prefrontal cortex (attention, executive function, and emotion), posterior cingulate cortex (self-awareness), insula (salience, awareness and emotional processing), striatum (regulation of attention and emotion), and amygdala (emotional processing).[89,95] In sum, the functional and structural neuroimaging data suggest that learning mindfulness creates or targets specific brain pathways or networks that may lead to the clinical effects demonstrated. However, the specific function of different brain regions or networks of regions in mediating the clinical effects of mindfulness training is yet to be fully elucidated. clinical effects demonstrated.
Prior mechanistic research proposed several specific neural pathways to explain mindfulness meditation-induced pain relief. Although endogenous opioid pathways may be involved in the cognitive inhibition of pain, endogenous opioids such as endorphins or enkephalins do not appear to be modulated in brief mindfulness meditation-induced pain relief, as a recent study demonstrated that naloxone infusion failed to reverse brief mindfulness mediation-induced analgesia.[100] Yet, mindfulness meditation-induced pain relief may employ different mechanisms than some forms of placebo analgesia. A recent study showed that mindfulness meditation-related pain relief activates brain areas associated with cognitive modulation of pain (orbitofrontal, anterior cingulate, insular cortices) while placebo analgesia (using a placebo cream with conditioning and suggestion) activates dorsolateral prefrontal cortex and deactivation of somatosensory processing regions (secondary somatosensory cortices).[101] Further, “sham mindfulness” (a technique where individuals were deceived into thinking they were engaged in mindfulness) was used to assess nonspecific components of mindfulness training. Subjects were instructed to take a deep breath while sitting in a meditation-like pose. Pain relief following this intervention was not correlated with significant neural activity, but instead with greater reductions in respiration rate.[101] These interesting studies demonstrate the likely existence of several supraspinal cognitively-driven mechanisms underlying the different components (e.g. non-judgmental awareness and reappraisal of sensory sensations, expectancy, deep breathing) of mindfulness meditation training-induced pain relief. Importantly, these studies were performed with evoked heat pain in healthy adults, and how such proposed neural pathways extend to patients experiencing acute migraine attacks is yet to be evaluated.
Biomarkers.
Other proposed biological hypotheses for mindfulness effects on migraine headache include the proposed ability of mindfulness meditation to decrease inflammatory or autonomic dysregulation. In the exploratory non-randomized study that evaluated mindfulness vs. pharmacological prophylaxis for Chronic Migraine Medication Overuse Headache (CM-MOH),[81] participants had blood samples drawn before and after the intervention to assess inflammatory markers, including white blood cell count (WBC), interleukin-6 (IL-6), neutrophils, lymphocytes, CD3, CD4, CD8, and CD19.[102] For all participants across both groups, all markers decreased, although not significantly. Significant changes were only seen for neutrophils and IL-6 in the mindfulness group and CD4 counts in the medication group. It is uncertain if the changes are clinically meaningful, and whether a larger study size would demonstrate a greater effect. In addition, catecholamine levels (noradrenaline, epinephrine, and dopamine), which may be abnormal in those with chronic migraine-medication overuse headache, were also assessed and found to be increased in both the pharmacological and mindfulness treatment groups at 12 months.[103] The authors point out that improvement in headache frequency was accompanied by these changes in blood-based catecholaminergic biomarkers, suggesting that both treatment groups have a similar effect on the regulation of tyrosine metabolism, an important component of pain processing. The authors also noted that mindfulness may be of particular value for the treatment of medication overuse headache, as learning mindfulness may increase patient’s self-efficacy and help them develop non-pharmacological methods for managing pain.[102] This may result in an avoidance of the vicious cycle of increasing medication intake with each headache attack that can be so disabling in medication overuse headache. Although not studied specifically in headache, a recent 2019 systematic review demonstrated that mind-body therapies for treatment of opioid-treated pain conditions are associated with moderate improvements in pain and small reductions of opioid dosages.[104] This review highlights the potential importance of mindfulness meditation training as a complementary therapy for regulating medication overuse in migraine and pain disorders.
Biophysiology.
The role of the autonomic system in migraine-related pain relief has also been explored. Heart rate variability (HRV), a commonly used biomarker of cardiovagal modulation, was previously assessed in patients with self-reported migraine and tension-type headache (n=36) compared to headache-free patients (n=39) before, during, and after a stressful procedure.[105] Participants were randomized to one of two interventions: (A) mindfulness meditation instruction (guided mindfulness practice) or (B) purely a description of mindfulness meditation with historical and scientific information about mindfulness. Self-reported stress ratings were higher after the stressful procedure in those with headache compared to healthy controls (87% vs. 50% rated the experience as inducing “moderate to extreme stress”, respectively). HRV, derived using electrocardiogram recordings and frequency-based HRV metrics, did not recover normally after the stress test in headache patients who were not exposed to the mindfulness instructions, suggesting their perceived stress may have contributed to dysregulation of parasympathetic modulation and recovery from the stressful challenge. Both headache patients and controls responded to the mindfulness instructions with significant improvements in heart rate variability, as expected with the parasympathetic regulation post-stress. The authors concluded that patients with headache may have a stronger physiological response to stressful stimuli compared to healthy controls, and that the sympathetically-oriented heart rate variability response observed in post-stress test patients with headache (but not controls) may be offset by the practice of mindfulness, through its engagement with the parasympathetic nervous system. Patients with headache may have stress vulnerabilities with parasympathetic dysregulation, and mindfulness practice may facilitate effective autonomic regulation, promoting effective recovery after a stressful event. Further, a 2019 study evaluated high frequency HRV (calculated as the natural log of the high-frequency power) before and after experimentally induced pain in participants who had been taught mindfulness meditation compared to sham meditation.[106] During mindfulness meditation (but not sham mindfulness), higher heart rate variability was associated with lower pain unpleasantness ratings. As migraine patients are known to also show autonomic dysfunction, [107,108] mindfulness regulation of autonomic outflow may prove to be an important mediator in how mindfulness meditation training improves clinical outcomes for migraine patients.
Cognitive-Affective Regulation.
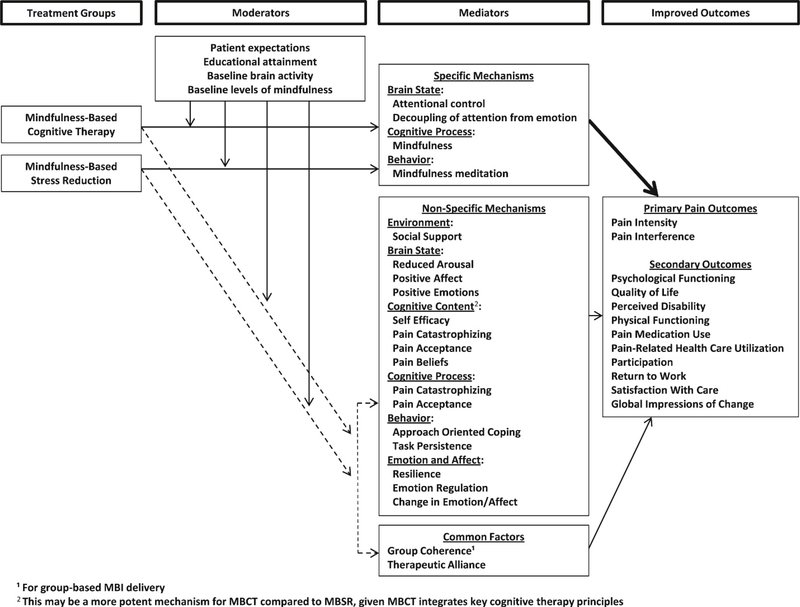
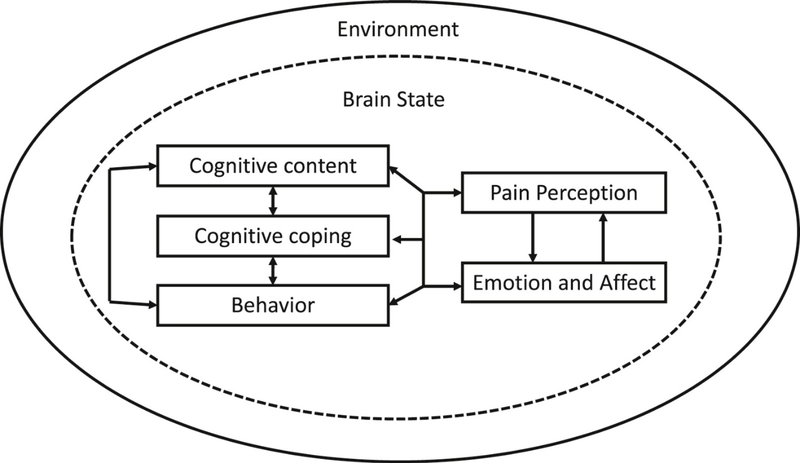
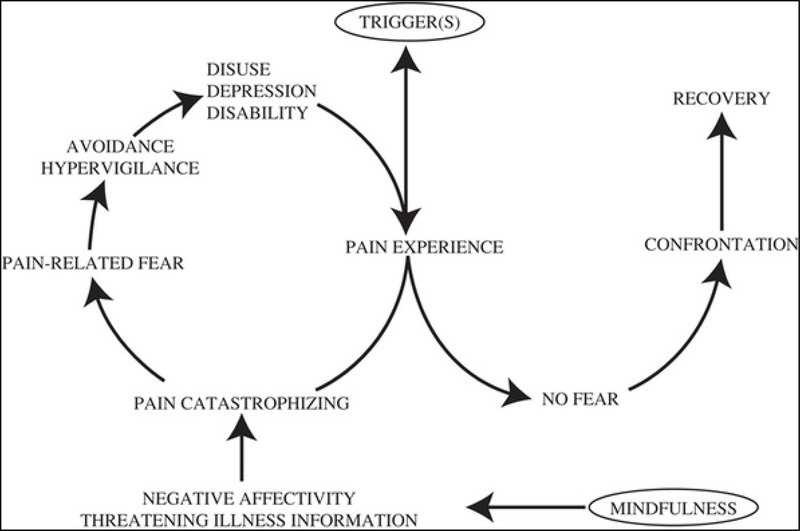
Pain is a multi-dimensional experience with sensory, cognitive, and affective processes involved. Patients with migraine often develop cognitive and affective responses to the recurrent sensory experiences of a migraine attack. For example, patients with migraine may have profound anticipatory anxiety with the uncertainty of when a migraine attack may occur. When a migraine attack begins, pain catastrophizing may develop, as prior episodes of debilitating, bed-ridden attacks lead to fear of such recurrence. Avoidance behaviors are common in patients with migraine, as perceived triggers are often avoided with a sense of hypervigilance. Such maladaptive behaviors may be targeted with mindfulness. The impact of mindfulness on such anticipatory anxiety, pain catastrophizing, pain acceptance, pain coping, and hypervigilance are all important assessments that need to be further investigated. Several psychological models have been developed for chronic pain conditions to understand better how mindfulness-based interventions (MBIs) may target pain processing. Day and colleagues developed a theoretical psychological/behavioral model for mindfulness-based management for chronic pain based on current evidence that addresses treatment groups, moderators, mediators, and improved outcomes (Figure 1). [109]. Specific mechanisms, non-specific mechanisms, and common factors are all included as potential mediators. Although quite thorough, the authors recognized that this model did not specifically delineate the role of emotion and affect, so proposed an updated overarching model framework (Figure 2). These psychological models were based on MBIs in chronic pain populations. Komandur and colleagues published an updated model of the Fear-Avoidance Model of pain (originally published [110]) to help explain mindfulness in chronic headache/migraine that includes the role of triggers and mindfulness (Figure 3). [111] They developed this model based on a cross-sectional survey of the key components of the Fear-Avoidance Model in 217 adults with chronic headache/migraine. They found that mindfulness had significant negative correlations with negative affect, pain catastrophizing, pain-related fear, pain hypervigilance, and functional disability, had no correlation with headache frequency or intensity, and had positive associations with headache duration. All three of these models demonstrate the goal of understanding the roles these important factors may play in understanding how mindfulness may target pain, yet more research needs to be done to fully elucidate these relationships, especially in migraine specific populations.
Figure 1. An evidence-based, specific, testable model of the mechanisms of mindfulness-based interventions for chronic pain management.
Potential moderators, mediators, and improved outcomes of mindfulness-based research are included to inform future research. Reprinted with permission from Elsevier. [1] MBI, mindfulness-based intervention; MBCT, mindfulness-based cognitive therapy; MBSR, mindfulness-based stress reduction.
Figure 2. A revised organizing framework for understanding the six key factors involved and their intertwined relationships in psychosocial pain treatments.
Since decreased pain and suffering are typically desirable endpoints, pain, emotion, and affect are shown as “downstream” factors that are interconnected with (and can also influence) the “upstream” cognitive and behavioral factors, all of which have bidirectional relationships with brain states and environmental/social factors. All factors interact with the others and no factor influences pain and functioning in isolation. Reprinted with permission from Elsevier.[1]
Figure 3. Fear-avoidance model of chronic pain incorporating the suggested role of trigger(s) and mindfulness in individuals with chronic headache/migraine. This model demonstrates how mindfulness may target the experience of pain through its impact on the negative appraisal of the pain (catastrophic thoughts), which often leads to the development of pain-related fear and subsequent maladaptive coping behaviors (escape, avoidance, hypervigilance) with resulting depression/disability and increased pain experience. Triggers may lead to avoidance/escape behaviors and resulting increased sensitivity to the pain experience.
Reprinted with permission from Wolters Kluwers Health [2] Adapted with permission from the version presented by Vlaeyen and Linton, and Schutze and colleagues (2009).[3] In this adjusted version, ‘Trigger(s)’ has replaced ‘Injury’ and ‘Mindfulness’ has been added.
4. Conclusion
Migraine is a disabling condition with recurrent attacks of severe pain, sensitivity to light/noise and nausea/vomiting. Additional treatments are needed, as pharmacological options are often limited by side effects, poor response, and high cost. Medications may not target the multitude of additional factors that play a role in pain processing, as Dr. Morone points out, “top-down regulation is not fully engaged when pain is treated with pharmacotherapy alone.”[112] The concept of “mindfulness-based interventions” was first standardized in the 1970s with the development of the MBSR program to treat chronic pain patients.[35] Since then, many studies have been conducted evaluating mindfulness programs, either the standard MBSR or an adapted MBCT, for headache. Most studies conducted to date have had high risk of bias with significant heterogeneity, with different intervention approaches, populations, and control groups. Despite these limitations, there appears to be some benefit for patients with episodic and chronic migraine. Most studies demonstrate prophylactic benefit, although perhaps more in measures of disability and psychological outcomes (such as self-efficacy and acceptance) over headache frequency measures which are typically the primary outcomes for headache prevention trials. For treatment of chronic migraine-medication overuse, mindfulness was as effective as pharmacological treatment on measures of both headache frequency and disability.[80] Preliminary data suggests MBCT for migraine may produce a larger impact on headache-related disability in people with episodic migraine vs. chronic migraine.[79]
Various underlying mechanisms of mindfulness in migraine have been proposed and detailed in this review. The mechanisms most likely to be playing a role include: changed perception of pain with a decreased affective pain experience; improved emotional and cognitive coping with the anticipation of migraine attacks and perception of migraine attacks; increased interoceptive body awareness and resulting earlier headache treatment and less cognitive and affective reactivity; increased strength of brain pathways that alter the cognitive regulation of nociceptive processing and modify interactions between afferent inputs and executive brain functions; decreased inflammatory responses; increased autonomic control with decreased sympathetic activation and lowered affective reactivity; improved stress coping and stress reactivity. Proposed mechanistic models for migraine must take into account interictal vs. ictal mechanisms and be tested in appropriate clinical research studies. The mechanisms of mindfulness could help explain clinical response and utility. For example, the changes in cognitive processing, pain perception, and cognitions related to the anticipation and management of migraine attacks could help explain why treatment effects are seen even after 12 months.[80,82] Further research is needed to fully elucidate responders vs. non-responders, impact on episodic vs. chronic migraine, comparisons of MBCT vs. MBSR, and mindfulness in the acute setting.
5. Expert Opinion
Many patients with migraine seek “a cure” want “to get to the root cause of the problem” as they want migraines “to go away forever.” This goal has been perpetuated by the natural course of migraines across a life-span, as migraine attacks appear to fluctuate in frequency over time and many male patients may “grow out of them” while female patients often experience near-resolution after menopause. Pharmacological treatments may provide significant benefit for certain patients; yet, they are often limited for many patients by side effects, cost, non-response, or even misalignment with a person’s goals of care. Non-pharmacological treatments such as mindfulness-based interventions have been evaluated as a potential option. This is an exciting time in the field of mindfulness research in migraine, as mindfulness programs are being investigated across the world, including Italy, Germany, Iran, US, India and Australia. This rise in interest is likely due to several factors, including 1) the standardized MBSR and MBCT approaches that can be taught with a high degree of consistency across populations; 2) the internationally-based criteria of headache disorders (ICHD); and 3) the desire for potentially effective treatments with minimal risks, especially in light of the highly-visible opioid epidemic in the U.S.[113] The evaluation of this modality throughout the world powerfully demonstrates the interest of mindfulness meditation across cultures and the need for non-pharmacological treatment options for such a widely prevalent condition.
5.1. Challenges Facing Research
While drug studies have a beautiful matching control in the placebo pill, behavioral interventions are much more challenging to match, with options including a wait-list/treatment as usual group, or an active control group that matches the time/attention of the intervention. Unfortunately, active control groups likely contain ingredients that may also target headache outcomes. Non-pharmacological treatments almost certainly will serve as adjuncts to acute migraine medication; further, the best preventive benefits may be derived from combining pharmacologic and non-pharmacologic approaches.[114,115] Compared to research settings, in most clinical treatment settings, the alternative to behavioral treatments is not an intensive therapeutic relationship with a thoughtful and compassionate provider focused on other topics (e.g., an attention control); it is treatment as usual. Treatment as usual is a more clinically useful control condition, whereas active controls help elucidate specific treatment mechanisms and can be used to understand comparative effectiveness of various active treatment options.
The pharmacological and behavioral guidelines for migraine trials [116,117] recommends headache outcomes as the primary outcome for clinical trials. Mindfulness-based interventions are theoretically more closely related to migraine-related disability than either the most commonly used preventive (headache days/month) or acute (proportion pain free at two hours) migraine treatment outcomes. People with migraine may experience reductions in headache frequency but still experience significant disruptions in their daily lives due to anticipation and management of migraine attacks. Migraine activity does not correlate on a 1:1 basis with migraine-related disability; in fact, mindfulness-based interventions are theoretically incredibly well-suited to explicitly reduce disability in people for whom the level of disability they are experiencing is disproportionate to their migraine symptoms. The FDA has recently recognized the importance of migraine-related disability and has included disability measures in recent approvals. In the MBCT for migraine study. Dr. Seng argued effectively that disability is an equally important outcome, and in her study of MBCT in migraine she powered her study to examine disability outcomes. This is a powerful viewpoint, recognizing that mindfulness interventions may not target frequency, but may change a patient’s relationship to pain and their resulting ability to function in the world. Further, mindfulness enhances body awareness and may actually improve patient’s ability to use medications acutely. Triptans are most effective early when migraine hits, so patients’ earlier awareness of migraine symptoms through mindfulness skills may enhance drug response. Further, many patients have difficulty with adherence to treatments, lack of motivation, poor awareness of triggers, external locus of control, poor self-efficacy, low levels of acceptance, and engagement in maladaptive coping styles, all known contributors to non-adherence.[118] All these factors have been noted to improve with mindfulness, potentially enhancing both pharmacological and non-pharmacological treatment response. These effects of mindfulness suggest the possibility that MBIs may be maximally effective in combination with pharmacologic treatments (whose benefits they could enhance by improving medication timing, adherence, etc.).
5.2. Future Research Questions
There are many unanswered questions about mind-body practices in adults with headaches that are summarized in Table 3.[119] While MBSR and MBCT protocols have been studied, the ideal dose needed for a response is uncertain, as the existing evidence is conflicting [46,75,120–122]. There has been a dramatic rise of meditation-based apps (currently over 1,300) and over 50 million downloads of HeadSpace and Calm, the top two meditation apps.[49,123] Many patients are exploring self-directed meditation as a treatment option, and evaluating the best modality and delivery method to increase access and ease of use for patients is important. MBSR and MBCT programs are directed by a trained instructor, with an opportunity for dialogue, engagement, and questioning, and the additional value of this guidance needs to be assessed. Relatedly, the question of group-based vs. individual delivery of these treatments has not been addressed in comparative trials. Time constraints are one of the most commonly cited barriers for initiating behavioral migraine treatments,[124] so determining how mindfulness can be most efficiently taught and incorporated into a patient’s life is a top priority to increase access and usability. At the same time, we need to understand if a low dose (or dose non-specific to the presenting concern of migraine) can still provide meaningful changes in migraine-related outcomes. Many home-based, therapist facilitated behavioral treatment approaches have been equally effective as clinic-based programs;[125] evaluating minimal therapist contact and telehealth approaches for mindfulness is an important next step to ensuring the treatments we are evaluating have clinical utility. In addition, finding ways to bring this treatment approach to traditionally marginalized groups is also important. With the potential development of variations to increase feasibility and acceptability, it will be important to assess if key principles and aspects of MBSR will be maintained, such as an emphasis on individual effort and motivation, and on regular disciplined practice and time commitment.[126]
Table 3:
Unanswered Questions about Mind-Body Treatments for Adults with Migraine, reprinted with permission from Wiley.[119]
| Content‐Based Research Questions | Development and Dissemination of Interventions |
|---|---|
| 1. Which interventions are most helpful for headache patients? 1A. Which types of patients and headaches are most responsive to these interventions? 2. What is the optimal “dose” of these interventions (e.g., frequency, duration, length of treatment)? 2A. To what extent do patients need to be taught these interventions by a professional, or can they learn them on their own? 3. What are the putative mechanism(s) of action? 3A. What role do these interventions have on headache threshold(s)? 4. What are the side effects and adverse events associated with treatment? |
1. How can standardized protocols be made more accessible to researchers and practitioners? 2. How can these interventions be better integrated into medical practice settings for providers? 3. How can matching of appropriate treatment to patient responders be facilitated? 4. How can these practices be made more accessible and practical for patients? |
The research on underlying mechanisms have yet to determine if mindfulness changes a person’s baseline level of stress reactivity in day-to-day life, making stressful events more manageable and less likely to trigger a migraine, or if tuning into the sensations of stress and pain change a patient’s perception of pain while having a migraine. Further research is needed to assess which mechanisms, or both, may be playing a role. Also understanding if having stress as a trigger for migraines as a prerequisite for response to mindfulness is important.
5.3. The Next Five Years
The next five years will dramatically shape the future of clinical care and research for mindfulness in migraine, as a multitude of ongoing or nearly completed studies will soon be published. The National Center for Complementary and Integrative Health (NCCIH) of the NIH has funded several studies focused on mindfulness’ benefits for migraine, which may guide clinical practice and future research. Given that research to date has been limited by high risk of bias, many of these NIH funded studies have been conducted with a high degree of scientific rigor, increasing the reliability and reproducibility of the results. Hopefully most will meet the goals of future research described in Table 4 and originally described in 2014.[119]
Table 4:
Goals of Future Research in Mind-Body Medicine for Headache, modified and reprinted with permission from Wiley[119]
| Randomized controlled trials |
| Adequate and appropriate controls |
| Intervention upholds therapy integrity and treatment fidelity is assessed |
| Clear specification of primary and secondary outcomes |
| Appropriate handling of treatment dropouts |
| Post‐intervention follow‐up is of sufficient length |
| Assessments of potential mechanisms of action |
| Clear specifications of the intervention protocol |
| Tracking of adverse events |
| Patients of diverse backgrounds |
We have completed a randomized controlled trial (RCT) of MBSR in adults with migraine, building on the results of our pilot data [83] with a larger sample size and an active control group (NCT02695498, results pending). Dr. Seminowicz has completed a study evaluating an enhanced MBSR protocol compared to an active control group in adults with migraines with MRI outcomes (NCT02133209, results pending). Dr. Pressman has published the protocol for an RCT conducted of community-based MBSR classes vs. usual care in adults with migraines [127] and the study is active (NCT02824250). Dr. D’Amico in Italy is building on prior research by conducting another study of a mindfulness-based intervention for adults with chronic migraine-medication overuse headache with fMRI outcomes (NCT03671681). Their group is also conducting a mindfulness meditation study for chronic migraine in pediatric patients.[128] Dr. Napadow is conducting a mechanistic study evaluating mindfulness for episodic migraine patients with MRI and PET data as primary outcomes (NCT03592329).
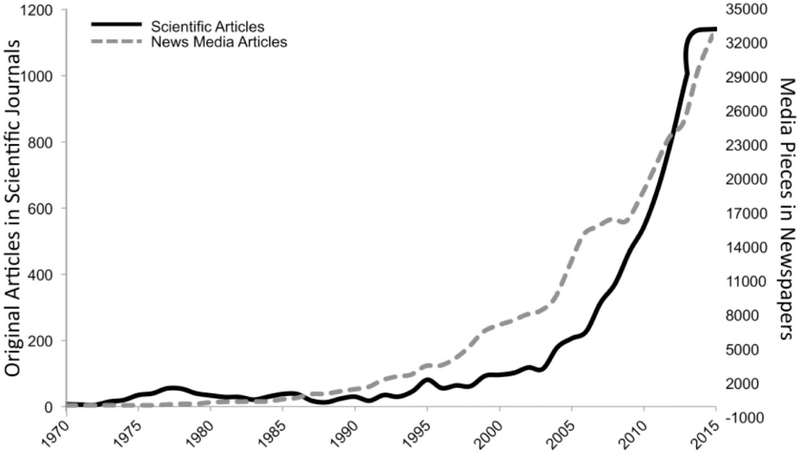
The next few years will also be important for “minding the hype” of mindfulness.[129] As mindfulness has gained scientific attention and has been the focus of significant clinical research, it has also been gaining media attention, resulting in a marked proliferation in meditation-centric news articles touting the physical and emotional benefits of meditation over the last 45 years (Figure 4).[129,130] Given the lack of methodological rigor of many of the mindfulness research studies, the media hype may be especially challenging as it has highlighted studies that need further replication prior to mainstream adoption. Although there is debate on how to address this issue,[129,131,132] future studies need to have both 1) enhanced methodological rigor, and 2) a clear articulation of adverse events, negative effects, and study limitations. Although no major adverse events have been reported in any of the mindfulness for migraine studies, meditation-related challenges exist. [133] As in all aspects of medicine, doing no harm is a key tenet and patients need to be aware of all potential adverse events.[134]
Fig. 4. Scientific and news media articles on mindfulness and/or meditation by year from 1970 to 2015.
Empirical scientific articles (black line) with the term mindfulness or meditation in the abstract, title, or keywords, published between 1970 and 2015 were searched using Scopus. Media pieces (dashed gray line) with the term mindfulness or meditation, published in newspapers, using a similarity filter to minimize double-counting, published between 1970 and 2015 were searched using LexisNexis. Reprinted with permission from SAGE publications.[4]
In summation, despite the challenges of the research evidence to date, mindfulness may be a helpful treatment tool for patients with migraine, with the greatest benefits to date seen in improvements in overall quality of life and disability, self-efficacy and psychological symptoms over headache frequency. Recognizing the role that mindfulness may play in a patient’s life with migraine may help understand potential benefits. Many research questions remain to understand better how, why, and for whom this treatment may be effective, and there is ongoing rigorous research to answer these questions. The evidence presented in the next five years will help guide clinical care and future research directions. This is an exciting time in the field of headache and integrative medicine.
Article highlights:
Key Issues
Migraine is the 2nd leading cause of disability worldwide
Current pharmacological options often fall short in providing effective relief for all patients
There is an unmet need for feasible, available, non-pharmacological approaches
Mindfulness based interventions (MBIs) are a promising option to reduce stress, anxiety, pain and improve patient well-being on the emotional and cognitive level
Current studies have investigated mindfulness-based programs along or in combination with standard of care
Mindfulness-based interventions may not “cure” migraine but may reduce pain severity and improve patients’ quality of life
Highlighted References:
Wells RE, Bertisch SM, Buettner C, et al. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011 2011/08//Jul-undefined;51(7):1087–1097.
This study provides data on the prevalence of complementary and alernative medicine (CAM) use in adults with migraine, particularly mind-body techniques.
Day MA, Thorn BE, Ward LC, et al. Mindfulness-based cognitive therapy for the treatment of headache pain: a pilot study. The Clinical journal of pain. 2014 Feb;30(2):152–61.
This was the first study of MBCT in headache, providing evidence for the feasibility and acceptability of MBCT for headache treatment, and paving the way for future research questions.
Seng EK, Singer AB, Metts C, et al. Does Mindfulness-Based Cognitive Therapy for Migraine Reduce Migraine-Related Disability in People with Episodic and Chronic Migraine? A Phase 2b Pilot Randomized Clinical Trial. Headache. 2019 Oct;59(9):1448–1467.
This study demonstrated MBCT has benefit on headache-related disability.
Grazzi L, Sansone E, Raggi A, et al. Mindfulness and pharmacological prophylaxis after withdrawal from medication overuse in patients with Chronic Migraine: an effectiveness trial with a one-year follow-up. The journal of headache and pain. 2017 Dec;18(1):15.
This study demonstrated that, after withdrawal of the offending medication, participants who choose to participate in a mindfulness intervention may receive as much benefit as those who choose a pharmacological prophylaxis for treatment of chronic migraine-medication overuse headache
Wells RE, Burch R, Paulsen RH, et al. Meditation for Migraines: A Pilot Randomized Controlled Trial. Headache: The Journal of Head and Face Pain. 2014 2014/10/01/;54(9):1484–1495.
This was the first published study of MBSR specific to migraine, providing evidence for the feasibility and acceptability of MBSR for headache treatment, and paving the way for future research questions.
Acknowledgements:
Dr. Wells is supported by the National Center for Complementary & Integrative Health (NCCIH) of the National Institutes of Health under Award Number K23AT008406. Dr. Seng is supported by NIH NINDS (NSK23096107; PI: Seng). Dr. Napadow is funded by US National Institutes for Health (NIH), Office of the Director (OT2-OD023867); National Center for Complementary and Integrative Health (NCCIH), NIH (P01-AT009965, R61-AT009306, R33-AT009306, R01-AT007550); and National Institute for Arthritis and Musculoskeletal and Skin Diseases (NIAMS), NIH (R01-AR064367). Dr. Schuman-Olivier is funded by NIH NCCIH P01AT009965 (PI-Napadow). Dr. Edwards is funded by NIH NCCIH P01AT009965 (PI-Napadow) and PCORI Award OPD-1601–33860. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We also gratefully acknowledge the editorial assistance of Indra M. Newman, PhD at the Wake Forest Clinical and Translational Science Institute, funded by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR001420.
Financial and Competing Interests Disclosure:
See grant support above in Acknowledgements. Dr. Seng has consulted for GlaxoSmithKline, Eli Lilly, and Click Therapeutics. Dr. Seng has received travel funds from the American Psychological Association, the American Academy of Neurology, and the American Association of Pain Medicine Foundation. Vitaly Napadow has a financial interest in Cala Health which is licensing the RAVANS tVNS technology from MGH. Dr. Napadow’s interests were reviewed and are managed by the Massachusetts General Hospital and Partners HealthCare in accordance with their institutional policies.
Contributor Information
Rebecca Erwin Wells, Department of Neurology, Wake Forest Baptist Health, Winston-Salem, NC.
Elizabeth K. Seng, Yeshiva University, Research Associate Professor, Albert Einstein College of Medicine,Bronx, NY.
Robert R Edwards, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham & Women’s Hospital, Boston, MA.
David E Victorson, Department of Medical Social Sciences, Northwestern University Feinberg School of Medicine, Chicago, IL.
Charles R. Pierce, Department of Neurology, Wake Forest Baptist Health, Winston-Salem, NC.
Lauren Rosenberg, Ferkauf Graduate School of Psychology, Yeshiva University, Bronx, NY, USA
Vitaly Napadow, Center for Integrative Pain NeuroImaging (CiPNI), Associate Professor, Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Harvard Medical School, CNY 149-2301, 13th St., Charlestown, MA 02129.
Zev Schuman-Olivier, Center for Mindfulness and Compassion, Medical Director, Addictions, Department of Psychiatry, Cambridge Health Alliance, Harvard Medical School, Cambridge, MA.
REFERENCES:
- 1.Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England). 2018. November 10;392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007. January 30;68(5):343–9. [DOI] [PubMed] [Google Scholar]
- 3.Burch RC, Buse DC, Lipton RB. Migraine: Epidemiology, Burden, and Comorbidity. Neurologic clinics. 2019. Nov;37(4):631–649. [DOI] [PubMed] [Google Scholar]
- 4.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia : an international journal of headache. 2018. January;38(1):1–211. [DOI] [PubMed] [Google Scholar]
- 5.Buse DC, Fanning KM, Reed ML, et al. Life With Migraine: Effects on Relationships, Career, and Finances From the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache. 2019. September;59(8):1286–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loder EW, Burch RC. Who Should Try New Antibody Treatments for Migraine? JAMA neurology. 2018. September 1;75(9):1039–1040. [DOI] [PubMed] [Google Scholar]
- 7.Loder EW, Burch RC. Consideration of Costs and Open-Label Studies of Erenumab-Reply. JAMA neurology. 2019. February 1;76(2):236–237. [DOI] [PubMed] [Google Scholar]
- 8.Robbins L. CGRP Antagonists: Physiologic Effects and Serious Side Effects. Headache. 2018. Oct;58(9):1469–1471. [DOI] [PubMed] [Google Scholar]
- 9.Lipton RB, Hutchinson S, Ailani J, et al. Discontinuation of Acute Prescription Medication for Migraine: Results From the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache. 2019. September 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wells RE, Markowitz SY, Baron EP, et al. Identifying the factors underlying discontinuation of triptans. Headache. 2014. Feb;54(2):278–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Archibald N, Lipscomb J, McCrory DC. AHRQ Technical Reviews. Resource Utilization and Costs of Care for Treatment of Chronic Headache. Rockville (MD): Agency for Health Care Policy and Research (US); 1999. [PubMed] [Google Scholar]
- 12.Lipton RB, Hutchinson S, Ailani J, et al. Discontinuation of Acute Prescription Medication for Migraine: Results From the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache. 2019. November;59(10):1762–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lipton RB, Munjal S, Buse DC, et al. Unmet Acute Treatment Needs From the 2017 Migraine in America Symptoms and Treatment Study. Headache. 2019. September;59(8):1310–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loder E, Weizenbaum E, Frishberg B, et al. Choosing wisely in headache medicine: the American Headache Society’s list of five things physicians and patients should question. Headache. 2013. Nov-Dec;53(10):1651–9. [DOI] [PubMed] [Google Scholar]
- 15.Buse DC, Powers SW, Gelfand AA, et al. Adolescent Perspectives on the Burden of a Parent’s Migraine: Results from the CaMEO Study. Headache. 2018. April;58(4):512–524. [DOI] [PubMed] [Google Scholar]
- 16.Seng EK, Mauser ED, Marzouk M, et al. When Mom Has Migraine: An Observational Study of the Impact of Parental Migraine on Adolescent Children. Headache. 2019. February;59(2):224–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wells RE, Loder E. Mind/Body and behavioral treatments: the evidence and approach. Headache. 2012. 2012/10//;52 Suppl 2:70–75. [DOI] [PubMed] [Google Scholar]
- 18.Pellegrino ABW, Davis-Martin RE, Houle TT, et al. Perceived triggers of primary headache disorders: A meta-analysis. Cephalalgia : an international journal of headache. 2018. May;38(6):1188–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000. September 26;55(6):754–62. [DOI] [PubMed] [Google Scholar]
- 20.Penzien DB, Irby MB, Smitherman TA, et al. Well-Established and Empirically Supported Behavioral Treatments for Migraine. Current pain and headache reports. 2015. July;19(7):34. [DOI] [PubMed] [Google Scholar]
- 21.Benson H, Klemchuk HP, Graham JR. The usefulness of the relaxation response in the therapy of headache. Headache. 1974. 1974/04//;14(1):49–52. [DOI] [PubMed] [Google Scholar]
- 22.Campbell JK, Penzien DB, Wall EM. Evidence-based guidelines for migraine headache: Behavioral and physical treatments. US Headache Consortium; 2000. [Google Scholar]
- 23.Wells RE, Bertisch SM, Buettner C, et al. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011. 2011/08//Jul-undefined;51(7):1087–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Erwin Wells R, Phillips RS, McCarthy EP. Patterns of Mind-Body Therapies in Adults with Common Neurological Conditions. Neuroepidemiology. 2010. 2010/12/22/;36(1):46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dalla Libera D, Colombo B, Pavan G, et al. Complementary and alternative medicine (CAM) use in an Italian cohort of pediatric headache patients: the tip of the iceberg. Neurol Sci. 2014. 2014/05//;35 Suppl 1:145–148. [DOI] [PubMed] [Google Scholar]
- 26.Peng W, Lauche R, Frawley J, et al. Utilization of complementary and alternative medicine and conventional medicine for headache or migraine during pregnancy: A cross-sectional survey of 1,835 pregnant women. Complementary therapies in medicine. 2018. December;41:192–195. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y, Dennis JA, Leach MJ, et al. Complementary and Alternative Medicine Use Among US Adults With Headache or Migraine: Results from the 2012 National Health Interview Survey. Headache. 2017. 2017/09//;57(8):1228–1242. [DOI] [PubMed] [Google Scholar]
- 28.Wells RE, Phillips RS, Schachter SC, et al. Complementary and alternative medicine use among US adults with common neurological conditions. Journal of neurology. 2010. 2010/11//;257(11):1822–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morone NE, Moore CG, Greco CM. Characteristics of Adults Who Used Mindfulness Meditation: United States, 2012. J Altern Complement Med. 2017. July;23(7):545–550. [DOI] [PubMed] [Google Scholar]
- 30.Kabat-Zinn J. Full Catastrophe Living: Using the WIsdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Random House; 1990. [Google Scholar]
- 31.Kerr CE, Sacchet MD, Lazar SW, et al. Mindfulness starts with the body: somatosensory attention and top-down modulation of cortical alpha rhythms in mindfulness meditation. Frontiers in human neuroscience. 2013;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cullen M. Mindfulness-Based Interventions: An Emerging Phenomenon. Mindfulness. 2011;2(3):186–193. [Google Scholar]
- 33.Bishop SR, Lau M, Shapiro S, et al. Mindfulness: A Proposed Operational Definition. Clin Psychol Sci Prac. 2004;11:230–241. [Google Scholar]
- 34.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985. 1985/06//;8(2):163–190. [DOI] [PubMed] [Google Scholar]
- 35.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982. 1982/04//;4(1):33–47. [DOI] [PubMed] [Google Scholar]
- 36.Santorelli S, Meleo-Meyer F, Koerbel L, et al. Mindfulness-Based Stress Reduction (MBSR) Authorized Curriculum Guide Worcester, MA: University of Massachusetts Medical School Center for Mindfulness in Medicine, Health Care, and Society; 2017. [Google Scholar]
- 37.Lutz A, Slagter HA, Dunne JD, et al. Attention regulation and monitoring in meditation. Trends in cognitive sciences. 2008. April;12(4):163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Britton WB, Davis JH, Loucks EB, et al. Dismantling Mindfulness-Based Cognitive Therapy: Creation and validation of 8-week focused attention and open monitoring interventions within a 3-armed randomized controlled trial. Behaviour research and therapy. 2018. February;101:92–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zeng X, Chiu CP, Wang R, et al. The effect of loving-kindness meditation on positive emotions: a meta-analytic review. Frontiers in psychology. 2015;6:1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Crane RS, Brewer J, Feldman C, et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. 2017. April;47(6):990–999. [DOI] [PubMed] [Google Scholar]
- 41.Rusch HL, Rosario M, Levison LM, et al. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Annals of the New York Academy of Sciences. 2019. June;1445(1):5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hilton LG, Marshall NJ, Motala A, et al. Mindfulness meditation for workplace wellness: An evidence map. Work (Reading, Mass). 2019;63(2):205–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Farhang M, Miranda-Castillo C, Rubio M, et al. Impact of mind-body interventions in older adults with mild cognitive impairment: a systematic review. International psychogeriatrics. 2019. May;31(5):643–666. [DOI] [PubMed] [Google Scholar]
- 44.Wells RE, Yeh GY, Kerr CE, et al. Meditation’s impact on default mode network and hippocampus in mild cognitive impairment: a pilot study. Neurosci Lett. 2013. November 27;556:15–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wells RE, Kerr CE, Wolkin J, et al. Meditation for adults with mild cognitive impairment: a pilot randomized trial. J Am Geriatr Soc. 2013. April;61(4):642–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wells RE, Kerr C, Dossett ML, et al. Can Adults with Mild Cognitive Impairment Build Cognitive Reserve and Learn Mindfulness Meditation? Qualitative Theme Analyses from a Small Pilot Study. Journal of Alzheimer’s disease : JAD. 2019;70(3):825–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goldberg SB, Tucker RP, Greene PA, et al. Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical psychology review. 2018. February;59:52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014. March;174(3):357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Creswell JD. Mindfulness Interventions. Annu Rev Psychol. 2017. 2017/01/03/;68:491–516. [DOI] [PubMed] [Google Scholar]
- 50.Gawande R, To MN, Pine E, et al. Mindfulness Training Enhances Self-Regulation and Facilitates Health Behavior Change for Primary Care Patients: a Randomized Controlled Trial. Journal of general internal medicine. 2019. February;34(2):293–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shapero BG, Greenberg J, Pedrelli P, et al. Mindfulness-Based Interventions in Psychiatry. Focus (American Psychiatric Publishing). 2018. Winter;16(1):32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rosenzweig S, Greeson JM, Reibel DK, et al. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. J Psychosom Res. 2010. 2010/01//;68(1):29–36. [DOI] [PubMed] [Google Scholar]
- 53.Hilton L, Hempel S, Ewing BA, et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann Behav Med. 2017. 2017/04//;51(2):199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ngamkham S, Holden JE, Smith EL. A Systematic Review: Mindfulness Intervention for Cancer-Related Pain. Asia-Pacific journal of oncology nursing. 2019. Apr-Jun;6(2):161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ball EF, Nur Shafina Muhammad Sharizan E, Franklin G, et al. Does mindfulness meditation improve chronic pain? A systematic review. Current opinion in obstetrics & gynecology. 2017. December;29(6):359–366. [DOI] [PubMed] [Google Scholar]
- 56.Segal ZV, Williams JM, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. New York: Guilford Press; 2012. [Google Scholar]
- 57.Coelho HF, Canter PH, Ernst E. Mindfulness-based cognitive therapy: evaluating current evidence and informing future research. Journal of consulting and clinical psychology. 2007. December;75(6):1000–5. [DOI] [PubMed] [Google Scholar]
- 58.van der Velden AM, Kuyken W, Wattar U, et al. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical psychology review. 2015. April;37:26–39. [DOI] [PubMed] [Google Scholar]
- 59.Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clinical psychology review. 2011. August;31(6):1032–40. [DOI] [PubMed] [Google Scholar]
- 60.Fjorback LO, Arendt M, Ornbol E, et al. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: a systematic review of randomized controlled trials. Acta psychiatrica Scandinavica. 2011. August;124(2):102–19. [DOI] [PubMed] [Google Scholar]
- 61.Crane RS. Implementing Mindfulness in the Mainstream: Making the Path by Walking IT. Mindfulness 2017;8(3):585–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yates SL, Morley S, Eccleston C, et al. A scale for rating the quality of psychological trials for pain. Pain. 2005. October;117(3):314–25. [DOI] [PubMed] [Google Scholar]
- 63.Cathcart S, Galatis N, Immink M, et al. Brief mindfulness-based therapy for chronic tension-type headache: a randomized controlled pilot study. Behav Cogn Psychother. 2014. 2014/01//;42(1):1–15. [DOI] [PubMed] [Google Scholar]
- 64.Omidi A, Zargar F. Effects of mindfulness-based stress reduction on perceived stress and psychological health in patients with tension headache. J Res Med Sci. 2015. 2015/11//;20(11):1058–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Omidi A, Zargar F. Effect of Mindfulness-Based Stress Reduction on Pain Severity and Mindful Awareness in Patients With Tension Headache: A Randomized Controlled Clinical Trial. Nurs Midwifery Stud. 2014. 2014/09//;3(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kiran n Girgla KK, Chalana H, et al. Effect of rajyoga meditation on chronic tension headache. Indian J Physiol Pharmacol. 2014. 2014/06//April-undefined;58(2):157–161. [PubMed] [Google Scholar]
- 67.Smitherman TA, Wells RE, Ford SG. Emerging behavioral treatments for migraine. Current pain and headache reports. 2015. 2015/04//;19(4):13. [DOI] [PubMed] [Google Scholar]
- 68.Wells RE, Beuthin J, Granetzke L. Complementary and Integrative Medicine for Episodic Migraine: an Update of Evidence from the Last 3 Years. Current pain and headache reports. 2019. February 21;23(2):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wells RE, Baute V, Wahbeh H. Complementary and Integrative Medicine for Neurologic Conditions. Med Clin North Am. 2017. 2017/09//;101(5):881–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Millstine D, Chen CY, Bauer B. Complementary and integrative medicine in the management of headache. BMJ. 2017. 2017/05/16/;357:j1805. [DOI] [PubMed] [Google Scholar]
- 71.Wahbeh H, Elsas S-M, Oken BS. Mind–body interventions Applications in neurology. Neurology. 2008. 2008/06/10/;70(24):2321–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wachholtz AB, Pargament KI. Migraines and meditation: does spirituality matter? J Behav Med. 2008. 2008/08/01/;31(4):351–366. [DOI] [PubMed] [Google Scholar]
- 73.Wachholtz AB, Pargament KI. Is spirituality a critical ingredient of meditation? Comparing the effects of spiritual meditation, secular meditation, and relaxation on spiritual, psychological, cardiac, and pain outcomes. J Behav Med. 2005. 2005/08//;28(4):369–384. [DOI] [PubMed] [Google Scholar]
- 74.Wachholtz AB, Malone CD, Pargament KI. Effect of Different Meditation Types on Migraine Headache Medication Use. Behav Med. 2017. 2017/03//January-undefined;43(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wachholtz A, Vohra R, Metzger A. A reanalysis of a randomized trial on meditation for migraine headaches: Distraction is not enough but meditation takes time. Complementary therapies in medicine. 2019. October;46:136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tonelli ME, Wachholtz AB. Meditation-Based Treatment Yielding Immediate Relief for Meditation-Naïve Migraineurs. Pain Manag Nurs. 2014. 2014/03//;15(1):36–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gu Q, Hou J-C, Fang X-M. Mindfulness Meditation for Primary Headache Pain: A Meta-Analysis. Chin Med J. 2018. 2018/04/05/;131(7):829–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Anheyer D, Leach MJ, Klose P, et al. Mindfulness-based stress reduction for treating chronic headache: A systematic review and meta-analysis. Cephalalgia : an international journal of headache. 2019. April;39(4):544–555. [DOI] [PubMed] [Google Scholar]
- 79.Seng EK, Singer AB, Metts C, et al. Does Mindfulness-Based Cognitive Therapy for Migraine Reduce Migraine-Related Disability in People with Episodic and Chronic Migraine? A Phase 2b Pilot Randomized Clinical Trial. Headache. 2019. October;59(9):1448–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Grazzi L, Sansone E, Raggi A, et al. Mindfulness and pharmacological prophylaxis after withdrawal from medication overuse in patients with Chronic Migraine: an effectiveness trial with a one-year follow-up. The journal of headache and pain. 2017. December;18(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Andrasik F, Grazzi L, D’Amico D, et al. Mindfulness and headache: A “new” old treatment, with new findings. Cephalalgia: An International Journal of Headache. 2016. 2016/09/30/. [DOI] [PubMed] [Google Scholar]
- 82.Simshauser K, Luking M, Kaube H, et al. Is Mindfulness-Based Stress Reduction a Promising and Feasible Intervention for Patients Suffering from Migraine? A Randomized Controlled Pilot Trial. Complementary medicine research. 2019. August 7:1–12. [DOI] [PubMed] [Google Scholar]
- 83.Wells RE, Burch R, Paulsen RH, et al. Meditation for Migraines: A Pilot Randomized Controlled Trial. Headache: The Journal of Head and Face Pain. 2014. 2014/10/01/;54(9):1484–1495. [DOI] [PubMed] [Google Scholar]
- 84.E.K. S, Singer. A, MEtts C, et al. Response to Mindfulness-Based Cognitive Therapy for Migraine in Chronic and Episodic Migraine: Planned Secondary Analyses of a Randomized Clinical Trial. Headache. 2019;59:206–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Day MA, Thorn BE, Ward LC, et al. Mindfulness-based cognitive therapy for the treatment of headache pain: a pilot study. The Clinical journal of pain. 2014. February;30(2):152–61. [DOI] [PubMed] [Google Scholar]
- 86.Tavallaei V, Rezapour-Mirsaleh Y, Rezaiemaram P, et al. Mindfulness for female outpatients with chronic primary headaches: an internet-based bibliotherapy. Eur J Transl Myol. 2018. 2018/04/24/;28(2):7380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bakhshani NM, Amirani A, Amirifard H, et al. The Effectiveness of Mindfulness-Based Stress Reduction on Perceived Pain Intensity and Quality of Life in Patients With Chronic Headache. Glob J Health Sci. 2015. 2015/08/06/;8(4):142–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hesse T, Holmes LG, Kennedy-Overfelt V, et al. Mindfulness-Based Intervention for Adolescents with Recurrent Headaches: A Pilot Feasibility Study. Evidence-Based Complementary and Alternative Medicine. 2015. 2015/12/22/;2015:e508958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Holzel BK, Lazar SW, Gard T, et al. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspectives on psychological science : a journal of the Association for Psychological Science. 2011. November;6(6):537–59. [DOI] [PubMed] [Google Scholar]
- 90.Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. Jama. 2008. September 17;300(11):1350–2. [DOI] [PubMed] [Google Scholar]
- 91.Mehling WE, Wrubel J, Daubenmier JJ, et al. Body Awareness: a phenomenological inquiry into the common ground of mind-body therapies. Philosophy, ethics, and humanities in medicine : PEHM. 2011. April 7;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Farb N, Daubenmier J, Price CJ, et al. Interoception, contemplative practice, and health. Frontiers in psychology. 2015;6:763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Khalsa SS, Adolphs R, Cameron OG, et al. Interoception and Mental Health: A Roadmap. Biological psychiatry Cognitive neuroscience and neuroimaging. 2018. June;3(6):501–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sinclair AJ, Sturrock A, Davies B, et al. Headache management: pharmacological approaches. Practical neurology. 2015. December;15(6):411–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tang Y-Y, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015. 2015/04//;16(4):213–225. [DOI] [PubMed] [Google Scholar]
- 96.Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011. 2011/04/06/;31(14):5540–5548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Necka EA, Lee IS, Kucyi A, et al. Applications of dynamic functional connectivity to pain and its modulation. Pain reports. 2019. Jul-Aug;4(4):e752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.van der Miesen MM, Lindquist MA, Wager TD. Neuroimaging-based biomarkers for pain: state of the field and current directions. Pain reports. 2019. Jul-Aug;4(4):e751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zeidan F, Baumgartner JN, Coghill RC. The neural mechanisms of mindfulness-based pain relief: a functional magnetic resonance imaging-based review and primer. Pain reports. 2019. Jul-Aug;4(4):e759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zeidan F, Adler-Neal AL, Wells RE, et al. Mindfulness-Meditation-Based Pain Relief Is Not Mediated by Endogenous Opioids. J Neurosci. 2016. 2016/03/16/;36(11):3391–3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zeidan F, Emerson NM, Farris SR, et al. Mindfulness Meditation-Based Pain Relief Employs Different Neural Mechanisms Than Placebo and Sham Mindfulness Meditation-Induced Analgesia. J Neurosci. 2015. 2015/11/18/;35(46):15307–15325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Grazzi L, D’Amico D, Raggi A, et al. Mindfulness and pharmacological prophylaxis have comparable effect on biomarkers of inflammation and clinical indexes in chronic migraine with medication overuse: results at 12 months after withdrawal. Neurol Sci. 2017. 2017/05//;38(Suppl 1):173–175. [DOI] [PubMed] [Google Scholar]
- 103.Grazzi L, Raggi A, D’Amico D, et al. A prospective pilot study of the effect on catecholamines of mindfulness training vs pharmacological prophylaxis in patients with chronic migraine and medication overuse headache. Cephalalgia : an international journal of headache. 2019. April;39(5):655–664. [DOI] [PubMed] [Google Scholar]
- 104.Garland EL, Brintz CE, Hanley AW, et al. Mind-Body Therapies for Opioid-Treated Pain: A Systematic Review and Meta-analysis. JAMA Intern Med. 2019. November 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Azam MA, Katz J, Mohabir V, et al. Individuals with tension and migraine headaches exhibit increased heart rate variability during post-stress mindfulness meditation practice but a decrease during a post-stress control condition-A randomized, controlled experiment. Int J Psychophysiol. 2016. 2016//12/;110:66–74. [DOI] [PubMed] [Google Scholar]
- 106.Adler-Neal AL, Waugh CE, Garland EL, et al. The Role of Heart Rate Variability in Mindfulness-Based Pain Relief. J Pain. 2019. August 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Miglis MG. Migraine and Autonomic Dysfunction: Which Is the Horse and Which Is the Jockey? Current pain and headache reports. 2018. February 23;22(3):19. [DOI] [PubMed] [Google Scholar]
- 108.Gazerani P, Cairns BE. Dysautonomia in the pathogenesis of migraine. Expert review of neurotherapeutics. 2018. Feb;18(2):153–165. [DOI] [PubMed] [Google Scholar]
- 109.Day MA, Jensen MP, Ehde DM, et al. Toward a theoretical model for mindfulness-based pain management. J Pain. 2014. 2014/07//;15(7):691–703. [DOI] [PubMed] [Google Scholar]
- 110.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000. April;85(3):317–32. [DOI] [PubMed] [Google Scholar]
- 111.Komandur B, Martin PR, Bandarian-Balooch S. Mindfulness and Chronic Headache/Migraine: Mechanisms Explored Through the Fear-Avoidance Model of Chronic Pain. The Clinical journal of pain. 2018. 2018/07//;34(7):638–649. [DOI] [PubMed] [Google Scholar]
- 112.Morone NE. Not Just Mind Over Matter: Reviewing With Patients How Mindfulness Relieves Chronic Low Back Pain. Journal of evidence-based integrative medicine. 2019. Jan-Dec;24:2515690×19838490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Blendon RJ, Benson JM. The Public and the Opioid-Abuse Epidemic. The New England journal of medicine. 2018. February 1;378(5):407–411. [DOI] [PubMed] [Google Scholar]
- 114.Powers SW, Kashikar-Zuck SM, Allen JR, et al. Cognitive behavioral therapy plus amitriptyline for chronic migraine in children and adolescents: a randomized clinical trial. Jama. 2013. December 25;310(24):2622–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Holroyd KA, Cottrell CK, O’Donnell FJ, et al. Effect of preventive (beta blocker) treatment, behavioural migraine management, or their combination on outcomes of optimised acute treatment in frequent migraine: randomised controlled trial. BMJ. 2010. September 29;341:c4871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tfelt-Hansen P, Pascual J, Ramadan N, et al. Guidelines for controlled trials of drugs in migraine: third edition. A guide for investigators. Cephalalgia : an international journal of headache. 2012. January;32(1):6–38. [DOI] [PubMed] [Google Scholar]
- 117.Penzien DB, Andrasik F, Freidenberg BM, et al. Guidelines for trials of behavioral treatments for recurrent headache, first edition: American Headache Society Behavioral Clinical Trials Workgroup. Headache. 2005. May;45 Suppl 2:S110–32. [DOI] [PubMed] [Google Scholar]
- 118.Matsuzawa Y, Lee YSC, Fraser F, et al. Barriers to Behavioral Treatment Adherence for Headache: An Examination of Attitudes, Beliefs, and Psychiatric Factors. Headache. 2019. January;59(1):19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wells RE, Smitherman TA, Seng EK, et al. Behavioral and mind/body interventions in headache: unanswered questions and future research directions. Headache. 2014. 2014/06//;54(6):1107–1113. [DOI] [PubMed] [Google Scholar]
- 120.Zeng X, Chio FH, Oei TP, et al. A Systematic Review of Associations between Amount of Meditation Practice and Outcomes in Interventions Using the Four Immeasurables Meditations. Frontiers in psychology. 2017;8:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Prasad K, Wahner-Roedler DL, Cha SS, et al. Effect of a single-session meditation training to reduce stress and improve quality of life among health care professionals: a “dose-ranging” feasibility study. Alternative therapies in health and medicine. 2011. May-Jun;17(3):46–9. [PubMed] [Google Scholar]
- 122.Parsons CE, Crane C, Parsons LJ, et al. Home practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behaviour research and therapy. 2017. August;95:29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mani M, Kavanagh DJ, Hides L, et al. Review and Evaluation of Mindfulness-Based iPhone Apps. JMIR mHealth and uHealth. 2015. August 19;3(3):e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Minen MT, Azarchi S, Sobolev R, et al. Factors Related to Migraine Patients’ Decisions to Initiate Behavioral Migraine Treatment Following a Headache Specialist’s Recommendation: A Prospective Observational Study. Pain medicine (Malden, Mass). 2018. November 1;19(11):2274–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Blanchard EB, Andrasik F, Appelbaum KA, et al. The efficacy and cost-effectiveness of minimal-therapist-contact, non-drug treatments of chronic migraine and tension headache. Headache. 1985. June;25(4):214–20. [DOI] [PubMed] [Google Scholar]
- 126.Santorelli SF. Mindfulness-Based Stress Reduction (MBSR): Standards of Practice. Worcester, MA: University of Massachusetts Medical School Center for Mindfulness in Medicine, Health Care, and Society; 2014. [Google Scholar]
- 127.Pressman A, Law H, Stahl R, et al. Conducting a pilot randomized controlled trial of community-based mindfulness-based stress reduction versus usual care for moderate-to-severe migraine: protocol for the Mindfulness and Migraine Study (M&M). Trials. 2019. May 6;20(1):257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sansone E, Raggi A, Grignani E, et al. Mindfulness meditation for chronic migraine in pediatric population: a pilot study. Neurol Sci. 2018. 2018/06//;39(Suppl 1):111–113. [DOI] [PubMed] [Google Scholar]
- 129.Van Dam NT, van Vugt MK, Vago DR, et al. Mind the Hype: A Critical Evaluation and Prescriptive Agenda for Research on Mindfulness and Meditation. Perspectives on psychological science : a journal of the Association for Psychological Science. 2018. January;13(1):36–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lauricella S. The Ancient-Turned-New Concept of “Spiritual Hygiene”: An Investigation of Media Coverage of Meditation from 1979 to 2014. Journal of religion and health. 2016. October;55(5):1748–62. [DOI] [PubMed] [Google Scholar]
- 131.Van Dam NT, van Vugt MK, Vago DR, et al. Reiterated Concerns and Further Challenges for Mindfulness and Meditation Research: A Reply to Davidson and Dahl. Perspectives on psychological science : a journal of the Association for Psychological Science. 2018. January;13(1):66–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Davidson RJ, Dahl CJ. Outstanding Challenges in Scientific Research on Mindfulness and Meditation. Perspectives on psychological science : a journal of the Association for Psychological Science. 2018. January;13(1):62–65. [DOI] [PubMed] [Google Scholar]
- 133.Lindahl JR, Fisher NE, Cooper DJ, et al. The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PloS one. 2017;12(5):e0176239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Baer R, Crane C, Miller E, et al. Doing no harm in mindfulness-based programs: Conceptual issues and empirical findings. Clinical psychology review. 2019. July;71:101–114. [DOI] [PMC free article] [PubMed] [Google Scholar]