Supplemental Digital Content is available in the text.
Background.
Patients that have undergone successful simultaneous pancreas/kidney (SPK) transplantation attain normoglycemia and are free from dialysis. However, only a minor improvement in quality of life (QOL) has been demonstrated. Here, we evaluated the role of psychological symptoms in QOL after SPK transplantation.
Methods.
We assessed patients with type 1 diabetes and end-stage renal disease waitlisted for SPK transplantation (pre-SPK, n = 47), and recipients of an SPK transplant (post-SPK, n = 72). Matched patients with type 1 diabetes without end-stage renal disease were included as reference group (type 1 diabetes [T1D] reference group, n = 42). The brief symptom inventory (BSI) was used to measure psychological symptoms. The Short Form-36 (SF-36) was used to determine QOL.
Results.
Post-SPK patients scored slightly better on the SF-36 than pre-SPK patients (“General health” 47.2 ± 23.1 versus 37.5 ± 18.1 [P = 0.017]). In the T1D reference group, this score was 60.6 ± 22.3. Post- and pre-SPK patients had similar BSI scores (0.54 ± 0.55 and 0.45 ± 0.42, respectively [P = 0.34]). This score was better in the T1D reference group (BSI score 0.32 ± 0.33). The BSI score inversely correlated with the SF-36 (r = −0.61, P < 0.001).
Conclusions.
Psychological symptoms are prevalent in both pre-SPK and post-SPK patients and could play an important role in the reduced QOL observed in these groups.
Type 1 diabetes is caused by destruction of beta cells in the pancreas, leading to an absolute insulin deficiency. Exogenous insulin is life-saving but does not prevent long-term diabetes-related complications such as retinopathy, neuropathy, vascular disease, nephropathy, and increased mortality.1 As a result, type 1 diabetes is associated with a reduction in quality of life (QOL).2 Type 1 diabetes and end-stage renal disease (ESRD) are good indications for a simultaneous pancreas and kidney (SPK) transplantation, resulting in insulin independence in 70%–80% of patients after 5 y.3 Importantly, SPK transplantation has been shown to halt the progression of or to improve secondary complications due to diabetes such as vascular disease, neuropathy, or nephropathy.3
QOL among SPK transplant recipients compared to waitlisted patients has been studied by different groups.4-7 Although diabetes-related QOL improves significantly,8,9 several studies show a minor increase in overall QOL,4-6,8,9 whereas only 1 study indicates a more profound increase.7 The reason for the lack of a substantial increase in general QOL after SPK transplantation is unknown.
Several determinants of QOL in SPK transplant recipients have been identified, such as age, diabetes-related complications, and long-term transplantation-related complications.4-9 However, the presence of psychological symptoms, which evidently can have a detrimental effect on QOL, has not been studied in SPK transplant recipients.10,11 Both chronic illnesses in general and type 1 diabetes in particular have been associated with increased psychopathology.12,13
Therefore, we aimed to determine the prevalence of psychological symptoms in pre- and post-SPK transplantation patients and to assess whether these symptoms are associated with QOL.
MATERIALS AND METHODS
Study Population
The main study population consisted of patients who underwent SPK transplantation at the Leiden University Medical Center, a national referral center for SPK transplantation in The Netherlands (post-SPK group). SPK transplantation was performed between 1991 and 2007. Assessment took place at least 1 y after transplantation. The post-SPK group was compared to patients with type 1 diabetes and ESRD due to diabetic nephropathy who were placed on the SPK waiting list (pre-SPK group) between 2007 and 2009. To provide a background reference value for questionnaire outcomes, patients with type 1 diabetes without ESRD, who were matched with the post-SPK group for age and sex and had a minimal duration of diabetes of 10 y, were asked to fill out the same questionnaires (type 1 diabetes [T1D] reference group). Patients who were unable to adequately fill out the questionnaires were excluded. Questionnaires were filled out between 2007 and 2010
Baseline variables included creatinin clearance, retinopathy requiring laser coagulation, vascular events defined by either an arterial thromboembolic event such as stroke or myocardial infarction or arterial vascular disease requiring hospitalization or intervention, diabetic foot defined as amputation, nonmelanoma skin cancer, other cancers, dialysis dependency, HbA1c, and insulin usage.
Questionnaires
All questionnaires used in this study were self-report instruments and were part of a computerized program QuestManager.14 To minimize bias problems, we specifically instructed patients to fill the questionnaires out by themselves. The same questionnaires with the same instructions were administered digitally or on paper.
The Brief symptom inventory (BSI) is a frequently used instrument to screen for psychological symptoms.15 The BSI is a shortened version of the Symptom Checklist, which measures psychological symptoms in several domains. The BSI has shown a good internal consistency, reliability, and validity.15 The 9 subscales of the BSI consist of “Somatization,” “Obsessive-compulsive/cognitive functions,” “Interpersonal sensitivity,” “Depression,” “Anxiety,” “Hostility,” “Phobic anxiety,” “Paranoid ideation,” and “Psychoticism.” In addition, “Miscellaneous items” reflect multiple dimensions, such as questions about sleeping problems. Each item reflects the extent to which a certain symptom troubled the patient during the previous week on a 5-point Likert scale ranging from 0 (absolutely not) to 4 (very much).15 The “BSI total score” (an average of all the answers, scale 0–4) has been validated as a general indicator of psychopathology, defined as a psychological or psychiatric disorder classified by the Diagnostic and Statistical Manual of Mental Disorders.16,17 In our study, an average score for each scale was calculated. A higher score indicates more psychological symptoms. Reference values were derived from a recent Dutch study.18
The Short Form 36 (SF-36 or RAND36) is a well-known and validated questionnaire for multidimensional assessment of QOL that has been used in previous studies on QOL in transplant patients.4-6,8,9,19,20 It consists of 36 items and measures the health-related QOL in the previous 30 d. The question type varies from yes/no answers to 3-, 5-, and 6-point scale answers. The 8 subscales of the SF-36 questionnaire are: “Bodily pain,” “Vitality,” “General health,” “Physical function,” “Mental health,” “Social function,” “Role physical,” and “Role emotional” and can yield a score from 0 to 100.20 A total QOL score was made by adding all the items into an SF-36 total score (range 0–800). A higher score corresponds to a higher QOL and/or less impairment.
The Dimensional Assessment of Personality Pathology- short form (DAPP-sf) was used to assess personality traits. The DAPP-sf is a validated shortened version (eg, consists of 136 items rather than 290) of the DAPP-BQ.21-23 This instrument measures 18 subscales of personality: “Submissiveness,” “Cognitive distortion,” “Identity problems,” “Affective lability,” “Stimulus seeking,” “Compulsivity,” “Restricted expression,” “Oppositionality,” “Callousness,” “Intimacy problems,” “Rejection,” “Anxiousness,” “Conduct problems,” “Suspiciousness,” “Social avoidance,” “Narcissism,” “Insecure attachment,” and “Self-harm,”21-23 The items on the DAPP-sf were rated on a 5-point Likert scale, ranging from 1 (“not applicable to me”) to 5 (“applicable to me”). For each subscale, an average score of the items was calculated. A higher score on a specific subscale reflects the presence of a specific personality trait. Reference values were derived from a recent Dutch study.18
Questionnaires were filled out at home (paper version) or at the outpatient clinic (computer version).
This study was exempt from ethical board approval under Dutch law.
Statistical Analyses
QuestManager was used to enter the questionnaire data.14 The post-SPK and pre-SPK groups were compared by unpaired T-tests for continuous variables and Χ2-tests for categorical variables. The Wilcoxon rank-sum test was used for data that were not normally distributed. Subgroup analysis was performed in patients who had undergone the transplantation either <7 y or ≥7 y previously. This time period was chosen as it is the median time period after transplantation in the post-SPK group.
To assess correlations between the BSI and SF-36 tests, Spearman’s rank correlation coefficient was calculated.
To assess the relative impact of the measured variables on QOL, a linear regression model was used including somatic and baseline variables as covariates. The outcome measure was QOL total score or physical QOL sum score (bodily pain, vitality, physical function, and role physical). Variables in the initial univariate model included gender, ethnicity, marital status, age, level of education, dialysis dependency, retinopathy, past vascular event, amputation due to diabetic foot, nonmelanoma skin cancer, malignancy, BSI total score, and DAPP-sf scores. Variables that had a low level of significance (P > 0.25) were left out in the final multivariate model.
A 2-tailed P < 0.05 was considered statistically significant. The statistical software was SPSS 21.0. Data are reported as average ± SD.
RESULTS
A total of 80 post-SPK transplantation patients were approached. One patient refused and 1 patient had a psychotic episode at the time. Of the 49 post-SPK transplantation patients who chose to fill out the questionnaires at home, 43 returned a completed questionnaire, which was a response rate of 87.8%. In addition, 29 post-SPK transplantation patients completed the questionnaires at the outpatient clinic. Thus, 72 post-SPK transplantation patients were included. Forty-seven pre-SPK transplantation patients participated and filled out the questionnaires at the outpatient clinic.
For the T1D reference group, 72 patients with type 1 diabetes without ESRD matched for age and gender with the post-SPK group were asked to participate. Six patients refused and 3 patients were unable to take part in the study. Ten patients completed the questionnaires at the outpatient clinic, whereas 53 patients chose to fill them out at home. A total of 42 patients filled out the questionnaires. Thirty-two questionnaires were returned to the outpatient clinic (response rate 58.3%). Thus, the complete data were available for 42 patients in the T1D reference group.
Patient Characteristics
The pre-SPK patients were significantly younger than the patients in the post-SPK group (43.3 ± 9.5 versus 47.9 ± 8.3 y, P = 0.001). The T1D reference patients were matched for age and sex with the post-SPK patients and were 49.7 ± 7.1 y old (Table 1).
TABLE 1.
Baseline characteristics of post-SPK, pre-SPK, and T1D reference patients
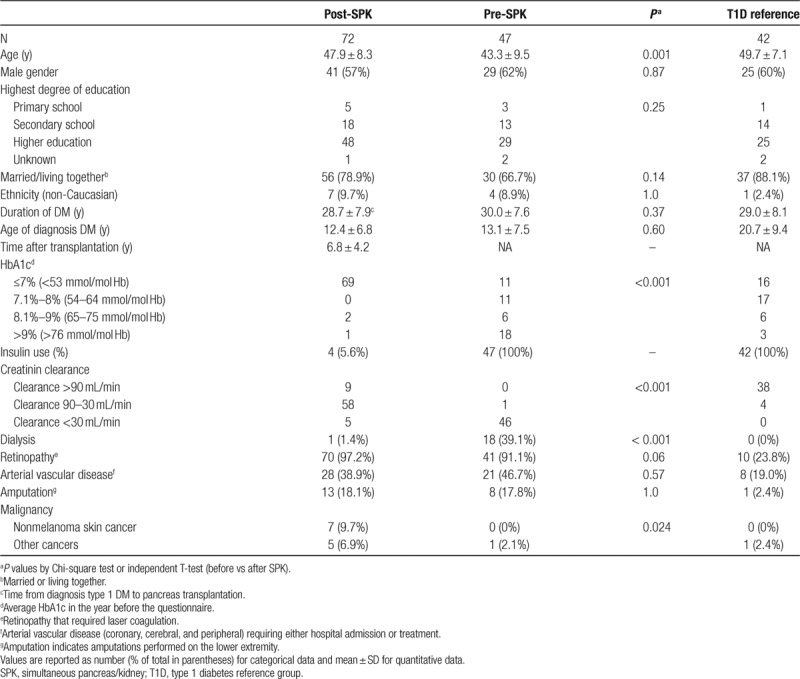
The age of diagnosis was similar between the post-SPK and pre-SPK patients (12.4 ± 6.8 and 13.1 ± 7.5 y, respectively (P = 0.60)). The age of diagnosis in the T1D reference patients was significantly later at 20.7 ± 9.4 y (Table 1) (P < 0.001).
In the post-SPK group, 4 patients used exogenous insulin (5.6%) due to failure of the pancreas graft. All these patients were <7 y after transplantation. One patient was on dialysis. The HbA1c was significantly higher in the pre-SPK group than in the post-SPK group (P < 0.001) (Table 1).
Of note, in the post-SPK group more malignancies were diagnosed in the previous 5 y compared to the pre-SPK group (P = 0.024). This included both nonmelanoma skin cancers such as basal and squamous cell carcinoma as well as other cancers such as malignant lymphoma.
Subgroup analysis showed that patients who were 7 y or longer after SPK transplantation had more vascular events (51% versus 26%, P = 0.026) and malignancy (30% versus 3%, P = 0.007) compared to patients who were <7 y after SPK transplantation (Table S1, SDC, http://links.lww.com/TXD/A251).
Psychological Symptoms: the BSI Questionnaire
No significant differences were found in the BSI total score or any of the BSI subscales between the post- and pre-SPK patients (Figure 1) or between post-SPK subgroups more or less than 7 y after transplantation (Table S1, SDC, http://links.lww.com/TXD/A251). Higher scores (indicating more psychological symptoms) were observed in the post-SPK and pre-SPK patients as compared to the T1D reference patients (Table S2, SDC, http://links.lww.com/TXD/A251).
FIGURE 1.
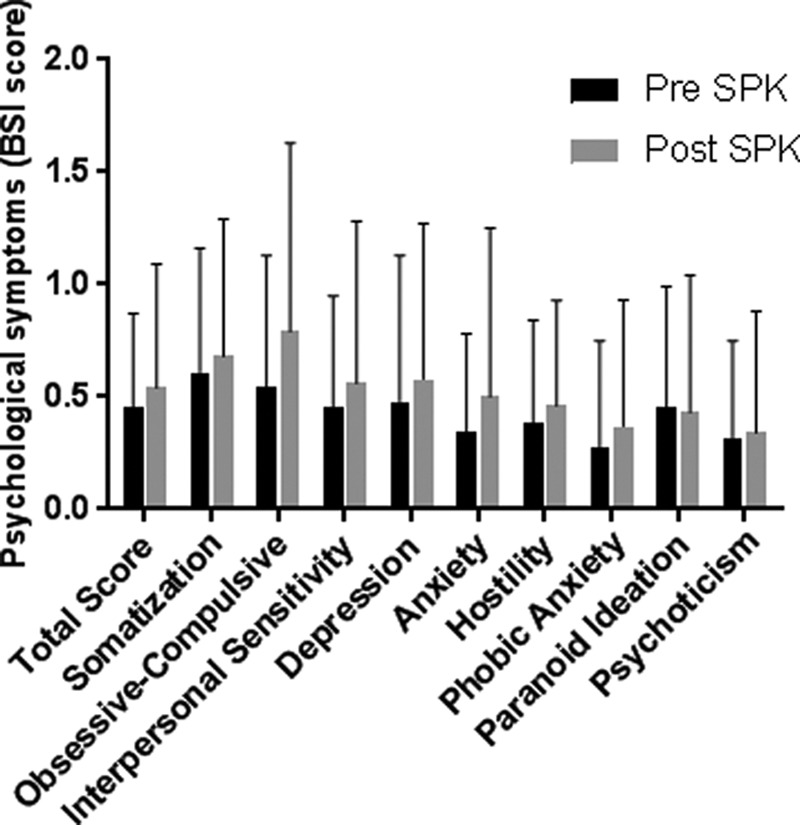
Psychological symptoms in pre-SPK and post-SPK patients. *P < 0.05. BSI, brief symptom inventory; SPK, simultaneous pancreas/kidney.
QOL: the SF-36 Questionnaire
Total scores on physical and mental QOL did not differ between the post- and pre-SPK patients (Figure 2) (Table S3, SDC, http://links.lww.com/TXD/A251). The post-SPK patients scored higher on “general health” compared to the pre-SPK patients (47.2 versus 37.5, P = 0.017). Compared to the T1D reference patients, the post-SPK patients had lower scores on the SF-36 for almost all subscales except for “mental health” and “role emotional.”
FIGURE 2.
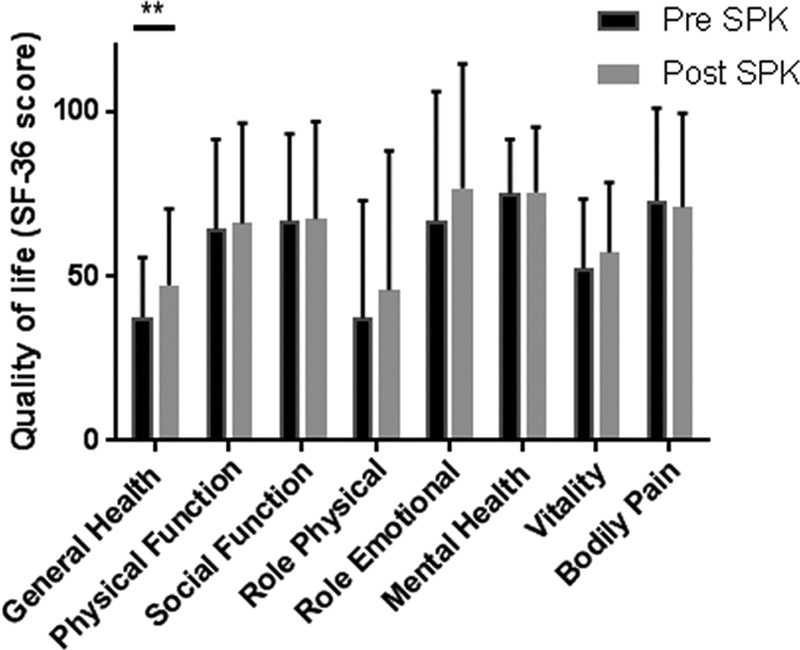
QOL in pre-SPK and post-SPK patients. **P < 0.001. QOL, quality of life; SF-36, short form-36; SPK, simultaneous pancreas/kidney.
Post-SPK patients who were ≥7 y after SPK transplantation did not have a higher score on “general health” when compared to pre-SPK patients (P = 0.087. General health score 45.5, confidence interval 37.7-53.3). In contrast, the patients that were <7 y post-SPK transplantation scored higher on “physical function” compared to the pre-SPK group (P = 0.05, score 73.1, confidence interval 64.1-82.1). No differences were found in the other SF-36 and BSI subscales in the post-SPK subgroup analysis (data not shown).
No significant differences were found on the SF-36 subscales between patients filling out the questionnaires at the outpatient clinic or at home.
Personality Traits: the DAPP-sf Questionnaire
No differences were found between the post- and pre-SPK patients. Both groups scored lower than the national reference values on the subscales “Submissiveness,” “Narcissism,” and “Oppositionality” (P < 0.026) (Table S4, SDC, http://links.lww.com/TXD/A251), but there were no differences between the pre- and post-SPK groups on these subscales.
Relationship Between QOL and Psychological Symptoms
The BSI total score (a general indicator of psychopathology) correlated significantly with the SF-36 total score (QOL) when subjects of all 3 groups were included (r = −0.62, P < 0.001) (Figure 3A). In both the post- and pre-SPK groups, the correlation remained significant (Figure 3B). There was also a significant correlation between BSI total score and physical QOL sum score when subjects of both the post- and pre-SPK groups were included (r = −0.47, P < 0.001) and of each separate group (pre-SPK r = −0.52, post-SPK r = −0.43, T1D r = −0.46; P < 0.001 for each group).
FIGURE 3.
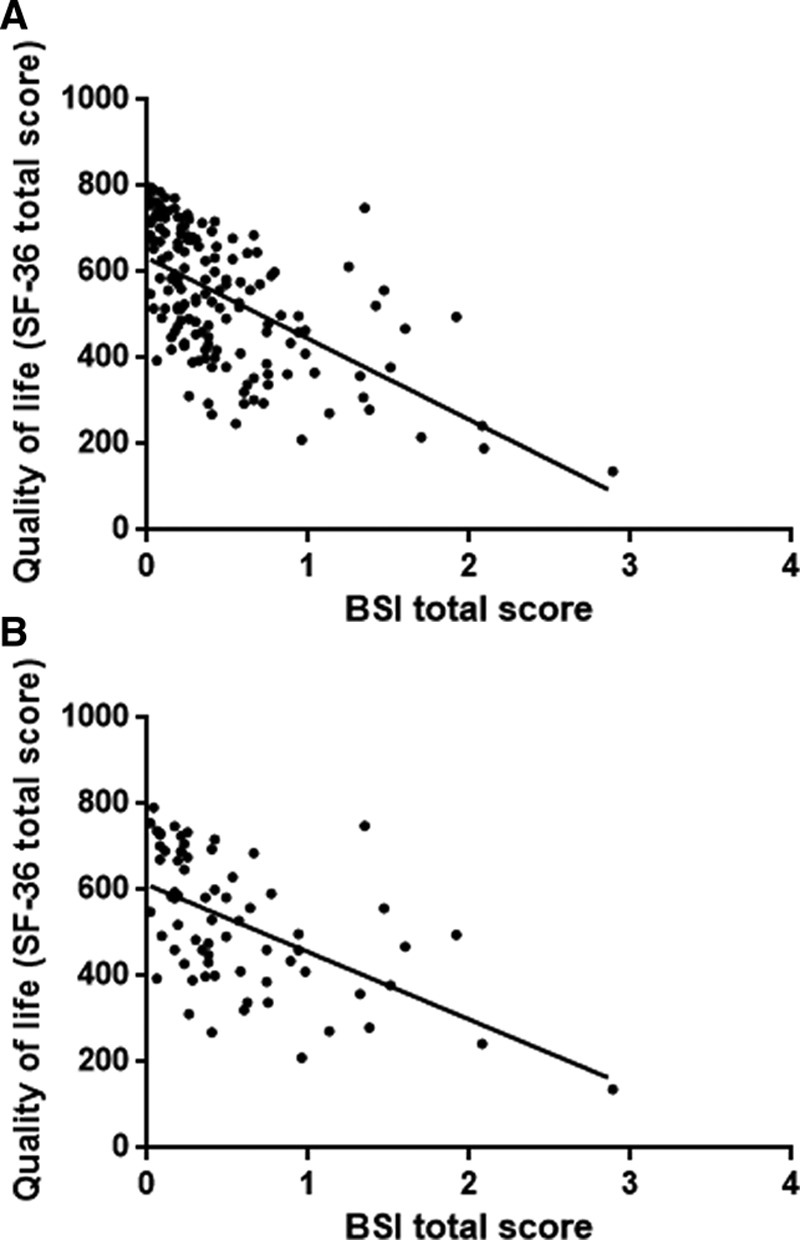
Scatter diagrams and correlation between SF-36 total score and BSI total score. A, Pre-SPK, post–SPK, and T1D reference patients (r = 0.62, P < 0.001). B, Only post-SPK group (r = 0.59, P < 0.001). BSI, brief symptom inventory; SF-36, short form-36; SPK, simultaneous pancreas/kidney; T1D, type 1 diabetes reference group.
In order to determine the contribution of potential confounding somatic variables on QOL, a linear regression model was used. The initial model included all covariates that are likely to affect QOL and psychological well-being. The following factors did not have a significant influence on the outcome in the model: amputation, DAPP-sf scores, age, age of diagnosis T1DM, sex, ethnicity, marital status, and level of education. The final linear regression analysis resulted in 6 variables that had a significant impact on QOL (P < 0.05), and these consisted of: the BSI total score (as a general indicator of psychopathology), nonmelanoma skin cancer, other malignancies, dialysis dependency, retinopathy, or a previous vascular event. The relative detrimental effect of the different variables on QOL could be rendered into a model with the following result:
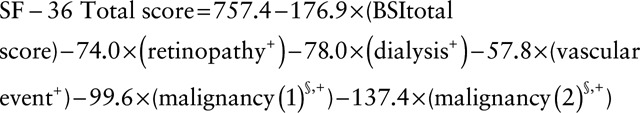 |
where + indicates if the variable is not present, it is 0 in this model, and if it is present, it is 1. § indicates Malignancy (1): nonmelanoma skin cancer. Malignancy (2): malignancy other than nonmelanoma skin cancer.
Residual plots of “SF-36 total score” after modeling did not show a gross violation of the normal distribution.
The considerable weighed contribution of the BSI total score was also present when only physical subscales of the SF-36 were used as outcome (Supplementary data 5, SDC, http://links.lww.com/TXD/A251). Analyses with the BSI total score as outcome demonstrated retinopathy, gender, level of education, and non-Caucasian ethnicity as significant correlating factors (Data S1, SDC, http://links.lww.com/TXD/A251).
DISCUSSION
The main results of our study show that there is an increased prevalence of psychological symptoms in post-SPK patients and that these symptoms are strongly correlated with QOL. Although QOL was slightly higher in patients who have been transplanted compared to patients who were on the SPK waiting list, a worse psychological symptom score was significantly associated with reduced QOL in both post-SPK and pre-SPK patients.
QOL has previously been studied in post-SPK versus pre-SPK transplantation recipients.4-9,24 These studies showed that SPK transplantation is in general associated with a modest improvement of QOL in patients who suffer from both diabetes and ESRD. However, many of these studies suffer from methodological shortcomings, such as using recall to measure baseline QOL. Also, different and sometimes nonvalidated questionnaires are used. These studies and our current study also show that a considerable reduction in QOL remains, which may be counterintuitive to many healthcare providers considering the remission of diabetes in combination with freedom from dialysis. We observed that QOL after SPK transplantation does not reach the level observed in the T1D reference group. Furthermore, we found that the benefit in QOL is not observed in patients who are >7 y after SPK transplantation. This may be related to an increased prevalence of vascular disease and malignancy in this group.
Different factors have been attributed to low QOL in post-SPK transplantation patients, such as malignancy and long-term complications of diabetes.6 We also confirm their association with QOL but additionally show the importance of psychological symptoms in understanding the limited QOL after transplantation, even after correction for possible confounders. These findings are in line with studies in the general population, showing a negative correlation between QOL and psychopathology.10,11 In our study, both the post-SPK and pre-SPK transplantation groups had higher scores on the BSI psychological symptoms questionnaire compared to the T1D reference group. Therefore, we conclude that both the post- and pre-SPK patients are more likely to suffer from psychological symptoms, in comparison with patients with type 1 diabetes without ESRD. Since many of the factors that correlated to the BSI total score (such as retinopathy, ethnicity, education, and gender) were present before SPK transplantation, it is likely that the increased psychological symptoms were already present before transplantation. Possibly the complicated course of the underlying illness in these patients explains the increased psychological symptomatology. It is important to note that the BSI questionnaire can only be used to estimate general psychopathology, and firm conclusions on subdomains cannot be drawn from these results. This would require more rigorous testing with specific questionnaires and structured psychiatric interviewing. Furthermore, the T1D reference group was different in several aspects compared to the pre- and post-SPK groups. This group had a shorter duration of diabetes, fewer diabetes-related and atherosclerotic complications, and fewer malignancies. Also the small sample size limits the power of the study to draw strong conclusions.
No previous studies have been performed on the prevalence of psychological symptoms and its effect on somatic outcomes or QOL in SPK transplant patients. Psychopathology in relation to general QOL was studied in patients after kidney transplantation alone (KTA) by Sayin et al,19 who found that increased psychopathology leads to reduced QOL in patients on dialysis, but not in patients after kidney transplantation. Noohi et al25 found a relationship between decreased mental health and psychopathology in KTA recipients. An important difference between our study group and the KTA patients previously studied is the fact that SPK transplantation patients are known to have more long-term complications (eg, retinopathy sometimes leading to blindness, [painful] neuropathy, and macrovascular disease), which may have an adverse effect on both QOL and psychopathology. Taking this into account, multivariate analysis was performed to assess the relationship between the psychological symptom score and QOL. We incorporated long-term complications such as retinopathy, dialysis dependency, vascular disease, and malignancy. The results support the added contribution of psychological symptoms in the reduced QOL observed in post-SPK transplantation patients. However, the cross-sectional study design excludes determination of causality.
Personality pathology could be a possible confounding factor for the relationship between QOL and psychopathology. Also, it could have in itself a detrimental effect on QOL.26 Previous research has not shown a relationship between either age of diagnosis of diabetes or diabetes-related complications and personality disorders, but certain personality traits have been found to relate to self-management and glycemic control.27 In our study, we found that the pre-SPK and post-SPK transplantation patients had a lower score on the subscale “submissiveness” than patients with type 1 diabetes, which may also be related to worse self-management and glycemic control. Because of the lack of other relevant findings on the personality trait screening, we conclude that it is unlikely that personality traits are a confounding factor for the relationship between QOL and psychological symptoms.
In conclusion, we found that psychological symptoms contribute to the limited QOL observed in post-SPK transplantation patients compared to patients with type 1 diabetes without ESRD. Our study underscores the importance of increased awareness of the presence of psychological symptoms in post-SPK patients. Prospective studies on changes in QOL in relation to changes in psychological symptoms could provide more insight in this relationship. Research to establish whether interventions focused on psychological symptoms improve QOL in SPK transplantation patients is needed.
Supplementary Material
Footnotes
Published online 27 April, 2020.
The authors declare no funding or conflicts of interest.
M.F.N. analyzed data, set up the study protocol, included patients, and wrote/revised the manuscript. J.G.F.M.H. set up the study protocol and reviewed/edited the manuscript. S.D.H. contributed to the discussion and revised the manuscript. J.R., T.A.J.R., and H.J.W.F. reviewed/edited the manuscript. P.J.M.B. included patients, set up the study protocol, and reviewed/edited the manuscript. E.J.P.K. included patients, set up the study protocol, and wrote/revised the manuscript.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
REFERENCES
- 1.Lind M, Svensson AM, Kosiborod M, et al. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med. 2014; 371:1972–1982. doi:10.1056/NEJMoa1408214 [DOI] [PubMed] [Google Scholar]
- 2.Jacobson AM, Braffett BH, Cleary PA, et al. ; DCCT/EDIC Research Group The long-term effects of type 1 diabetes treatment and complications on health-related quality of life: a 23-year follow-up of the Diabetes Control and Complications/Epidemiology of Diabetes Interventions and Complications cohort. Diabetes Care. 2013; 36:3131–3138. doi:10.2337/dc12-2109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindahl JP, Jenssen T, Hartmann A. Long-term outcomes after organ transplantation in diabetic end-stage renal disease. Diabetes Res Clin Pract. 2014; 105:14–21. doi:10.1016/j.diabres.2014.03.004 [DOI] [PubMed] [Google Scholar]
- 4.Piehlmeier W, Bullinger M, Kirchberger I, et al. Evaluation of the quality of life of patients with insulin-dependent diabetes mellitus before and after organ transplantation with the SF 36 health survey. Eur J Surg. 1996; 162:933–940 [PubMed] [Google Scholar]
- 5.Matas AJ, McHugh L, Payne WD, et al. Long-term quality of life after kidney and simultaneous pancreas-kidney transplantation. Clin Transplant. 1998; 12:233–242 [PubMed] [Google Scholar]
- 6.Gross CR, Limwattananon C, Matthees BJ. Quality of life after pancreas transplantation: a review. Clin Transplant. 1998; 12:351–361 [PubMed] [Google Scholar]
- 7.Martins LS, Outerelo C, Malheiro J, et al. Health-related quality of life may improve after transplantation in pancreas-kidney recipients. Clin Transplant. 2015; 29:242–251. doi:10.1111/ctr.12511 [DOI] [PubMed] [Google Scholar]
- 8.Sureshkumar KK, Mubin T, Mikhael N, et al. Assessment of quality of life after simultaneous pancreas-kidney transplantation. Am J Kidney Dis. 2002; 39:1300–1306. doi:10.1053/ajkd.2002.33408 [DOI] [PubMed] [Google Scholar]
- 9.Sureshkumar KK, Patel BM, Markatos A, et al. Quality of life after organ transplantation in type 1 diabetics with end-stage renal disease. Clin Transplant. 2006; 20:19–25. doi:10.1111/j.1399-0012.2005.00433.x [DOI] [PubMed] [Google Scholar]
- 10.Rapaport MH, Clary C, Fayyad R, et al. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005; 162:1171–1178. doi:10.1176/appi.ajp.162.6.1171 [DOI] [PubMed] [Google Scholar]
- 11.Spinhoven P, Elzinga BM, Giltay E, et al. Anxious or depressed and still happy? PLoS One. 2015; 10:e0139912.doi:10.1371/journal.pone.0139912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maia AC, Braga Ade A, Paes F, et al. Psychiatric comorbidity in diabetes type 1: a cross-sectional observational study. Rev Assoc Med Bras (1992). 2014; 60:59–62. doi:10.1590/1806-9282.60.01.013 [DOI] [PubMed] [Google Scholar]
- 13.Popkin MK, Callies AL, Lentz RD, et al. Prevalence of major depression, simple phobia, and other psychiatric disorders in patients with long-standing type I diabetes mellitus. Arch Gen Psychiatry. 1988; 45:64–68. doi:10.1001/archpsyc.1988.01800250078010 [DOI] [PubMed] [Google Scholar]
- 14.Philips. Philips VitalHealth QuestManager. Philips; Available at http://www.vitalhealthsoftware.nl/oplossingen/vitalhealth-questmanager. Accessed April 2019. [Google Scholar]
- 15.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983; 13:595–605 [PubMed] [Google Scholar]
- 16.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 19944th edWashington, DC: American Psychiatric Association [Google Scholar]
- 17.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 20135th edWashington, DC: American Psychiatric Association [Google Scholar]
- 18.Schulte-van Maaren YW, Carlier IV, Zitman FG, et al. Reference values for generic instruments used in routine outcome monitoring: the Leiden Routine Outcome Monitoring Study. BMC Psychiatry. 2012; 12:203.doi:10.1186/1471-244X-12-203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sayin A, Mutluay R, Sindel S. Quality of life in hemodialysis, peritoneal dialysis, and transplantation patients. Transplant Proc. 2007; 39:3047–3053. doi:10.1016/j.transproceed.2007.09.030 [DOI] [PubMed] [Google Scholar]
- 20.Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992; 305:160–164. doi:10.1136/bmj.305.6846.160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Kampen D, de Beurs E, Andrea H. A short form of the Dimensional Assessment of Personality Pathology-Basic Questionnaire (DAPP-BQ): the DAPP-SF. Psychiatry Res. 2008; 160:115–128. doi:10.1016/j.psychres.2007.05.002 [DOI] [PubMed] [Google Scholar]
- 22.Tromp NB, Koot HM. Dimensions of personality pathology in adolescents: psychometric properties of the DAPP-BQ-A. J Pers Disord. 2008; 22:623–638. doi:10.1521/pedi.2008.22.6.623 [DOI] [PubMed] [Google Scholar]
- 23.Tromp NB, Koot HM. Dimensions of personality pathology in adolescents: relations to DSM-IV personality disorder symptoms. J Pers Disord. 2009; 23:514–527. doi:10.1521/pedi.2009.23.5.514 [DOI] [PubMed] [Google Scholar]
- 24.Hanlon M, Cooper M, Abrams P. Quality of life after pancreas transplantation: time to look again. Curr Opin Organ Transplant. 2019; 24:451–455. doi:10.1097/MOT.0000000000000676 [DOI] [PubMed] [Google Scholar]
- 25.Noohi S, Khaghani-Zadeh M, Javadipour M, et al. Anxiety and depression are correlated with higher morbidity after kidney transplantation. Transplant Proc. 2007; 39:1074–1078. doi:10.1016/j.transproceed.2007.04.002 [DOI] [PubMed] [Google Scholar]
- 26.Larivière N, Denis C, Payeur A, et al. Comparison of objective and subjective life balance between women with and without a personality disorder. Psychiatr Q. 2016; 87:663–673. doi:10.1007/s11126-016-9417-3 [DOI] [PubMed] [Google Scholar]
- 27.Waller D, Johnston C, Molyneaux L, et al. Glycemic control and blood glucose monitoring over time in a sample of young Australians with type 1 diabetes: the role of personality. Diabetes Care. 2013; 36:2968–2973. doi:10.2337/dc12-1743 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


