Abstract
Despite expectations that Medicare accountable care organizations (ACOs) would curb healthcare spending, their effect has been modest. One possible explanation is that ACOs cannot prohibit out-of-network care, limiting control over spending. To examine this possibility, we examined the association between out-of-network care and per beneficiary spending using national Medicare data, 2012–2015. While there was no association between out-of-network specialty care and ACO spending, each percentage point increase in receipt of out-of-network primary care was associated with a $10.79 increase in quarterly ACO per beneficiary total spending. When we broke down total spending by place of service, we found that out-of-network primary care was associated with higher spending in outpatient, skilled nursing, and emergency settings, but not inpatient settings. Our findings suggest an opportunity for the Medicare program to realize substantial savings, if policymakers developed explicit incentives for beneficiaries to seek more of their primary care within network.
Introduction
In an effort to curb healthcare spending growth and improve quality, the Centers for Medicare & Medicaid Services (CMS) launched the Shared Savings Program (SSP) in 2012. This program uses collective incentives to motivate providers participating in an accountable care organization (ACO) to collaborate with each other. Despite great fanfare, SSP evaluations have demonstrated only modest spending reductions (1), with significant variation across ACOs in performance (2, 3). One reason for such variation may be differences in the level of out-of-network care that ACO beneficiaries receive. Unlike health maintenance organizations that are allowed to implement explicit mechanisms to incentivize patients to stay in network (e.g., requiring referrals, charging higher fees for out-of-network care), ACO-aligned beneficiaries are free to seek care from whomever they want. In fact, prior to the Bipartisan Budget Act of 2018, SSP beneficiaries were assigned to ACOs after they had already received care (based on where they received the plurality of primary care services that year), even though participating organizations were responsible for all costs of care received. While preserving patient choice is laudable, it may hinder ACOs from lowering healthcare spending.
Specifically, ACOs have few sight lines into and even less control over care delivered outside their boundaries, making it difficult for ACOs with higher proportions of out-of-network care to reduce spending (4–6). Recognizing this, ACO leaders are paying increasing attention to out-of-network specialty care given specialists’ outsized contribution to spending (7). However, out-of-network primary care may also be important because of the critical role that primary care providers (PCPs) play in gate-keeping and care coordination, which could have salutary effects on spending. Previous studies demonstrate that patients in managed care systems receive more coordinated care and have lower inpatient utilization than those whose care is delivered on a fee-for-service basis (8, 9). This may be attributable to the ability of managed care systems to keep primary care visits within network. Although variation in out-of-network specialty care across ACOs has been described, little is known about out-of-network primary care and its effects on spending (4, 10).
Furthermore, little is known about how patient, organizational, and regional characteristics may influence beneficiary choice or ACOs’ ability to limit care sought outside their networks. It may be that ACOs with sicker patients, fewer participating providers, or those in underserved communities may face additional challenges to keeping patient care inside the network, leading to higher spending. Indeed, there are compelling data to suggest that ACOs are more likely to reduce spending in areas with lower poverty rates, smaller populations of marginalized communities, and more educated patients (11–13).
To address these knowledge gaps, we analyzed national Medicare data. For each SSP ACO, we calculated the amount of primary and specialty care delivered outside its network by year. We then assessed whether the level of out-of-network care is associated with ACO characteristics. Finally, we assessed whether the level of out-of-network primary and specialty care was associated with per beneficiary spending, both total and by setting (inpatient, outpatient, skilled nursing facility, and emergency department).
Methods
Data Sources and Study Population
For our study, we used a random 20% sample of Medicare beneficiaries over years 2012 to 2015. Among those enrolled in fee-for-service, we analyzed their claims from the Medicare Provider and Analysis Review, Outpatient, and Carrier Research Identifiable Files (RIFs). Through the SSP Beneficiary-level RIF, we were able to determine which beneficiaries were attributed to a SSP ACO during a given year. We included only beneficiaries that have continuous Parts A and B coverage that year. We excluded those under age 65 and those with end-stage renal disease. To identify and characterize ACO participating providers, we used the SSP Provider-level RIF and the Leavitt-Partners ACO Database (14). We also gathered county-level data from the Area Health Resource File.
Calculating Out-of-Network Care
For each ACO-year observation, we calculated the proportion of outpatient primary care and specialty care visits delivered out-of-network using a two-step process (4). We first abstracted preventive visits, annual wellness visits, and other outpatient visits from beneficiaries’ claims using Current Procedural Terminology. We classified outpatient visits as primary care or specialty care based on Medicare Provider Specialty codes. PCPs were identified as providers with a specialty of general practice, family practice, internal medicine, or geriatric medicine. Specialist providers were identified as non-PCPs [for a full list of specialty codes, see (15)].
For each ACO, we then calculated the proportion of out-of-network primary care as the number of outpatient visits provided to the ACO’s beneficiaries by PCPs not in its contracting network, divided by the total number of outpatient visits provided to its beneficiaries by any PCP. We calculated the proportion of out-of-network specialty care, dividing the number of outpatient visits made by an ACO’s beneficiaries to specialists not in its contracting network by the total number of outpatient visits provided to its beneficiaries by any specialist.
Measuring Per Beneficiary Spending
Our primary outcome was per beneficiary total spending. We calculated this by summing all price-standardized and inflation-adjusted payments from Parts A and B claims at the quarter level for each beneficiary. CMS uses total spending to calculate the amount of “shared savings” that participating ACOs receive as incentive for reducing their costs. Specifically, ACOs are given a portion of the difference between actual total spending and a benchmark (which is based on historical performance), provided that specific quality metrics are met. Therefore, our primary outcome parallels processes used by CMS to assess individual ACO performance.
We focused on per beneficiary spending instead of other performance measures like shared savings or clinical quality for multiple reasons. First, we wanted our results to be directly comparable to existing studies. To date, the bulk of the literature on ACO performance, as well as many CMS evaluations, use per beneficiary spending as a main outcome (1, 16). Second, our research question was to understand whether ACO spending varies with out-of-network care among ACOs. To do this, we needed a measure of healthcare spending that could be compared across all ACOs. The way that shared savings are calculated is problematic for our purposes because they are based on ACO- and population-specific factors that could systematically bias our results (17). Third, as previously described, the dollar amount of the SSP incentive award is directly related to healthcare spending for a given ACO’s beneficiaries. Thus, once specific quality metrics are met, SSP ACOs may be more likely to focus on cost reduction efforts rather than further quality improvement. Fourth, data suggest that efforts to improve clinical quality in ACOs are still maturing. In particular, SSP ACOs have made only small quality gains, especially in the early years of ACO implementation from which our study draws its data (18). Finally, while studies have demonstrated significant spending reductions in ACOs over time (18), the exact mechanism through which these reductions occur is unknown. By focusing on spending, our study attempts to address this knowledge gap.
To understand how patterns of spending change with level of out-of-network care, we broke down total spending by place of service (i.e., inpatient, outpatient, skilled nursing, and emergency department settings). We chose to examine these specific categories based on prior ACO and managed care literature (9, 19, 20), which suggests that ACOs may be reducing costs by shifting utilization from one care setting to another. For example, if out-of-network care is associated with increased outpatient and decreased inpatient spending, this would imply that ACO providers may be shifting expensive inpatient procedures to less costly ambulatory venues. We identified place of service using Medicare place of service codes.
Statistical Analysis
For our initial analytic step, we examined the median and interquartile range (IQR) of percent of out-of-network primary and specialty care, as well as yearly percent and percentage point changes in out-of-network primary and specialty care. We also evaluated the extent to which an organization’s level of out-of-network primary care correlated with its level of out-of-network specialty care.
We then sought to understand how ACOs with high versus low levels of out-of-network care differ. We conducted bivariate analyses, examining characteristics at the patient, organizational, and regional level that we hypothesized were related to beneficiary choice and ability to seek care outside their ACO’s network. In particular, we compared ACOs in the highest quartile of out-of-network primary and specialty care with ACOs in the three lower quartiles in 2015. We examined differences in their aligned beneficiaries with respect to age, gender, race/ethnicity, comorbidity [assessed by Hierarchical condition categories (HCCs) ((21, 22))], and dual eligibility distributions. We also examined organizational differences [percent of PCPs, leadership (i.e., physician-led, hospital-led, or physician-hospital partnership), risk-bearing status, size (number of beneficiaries and providers in the ACO), and whether the ACO included a critical access hospital, federally qualified health center, or acute care hospital] and regional differences (population, urban/rural, income, percent of families living in poverty, percent of adults with less than a high school education, supply of medical doctors and PCPs, and number of skilled nursing facilities and hospitals).
Finally, we assessed the association between percent out-of-network care and per beneficiary spending adjusting for patient, ACO, and regional characteristics, using two-part multivariable regression models on our beneficiary-quarter level data set (Q1 2012-Q4 2015) (23). Compared to linear regression, two-part models are more appropriate for our analysis given the high proportion of patients with $0 spending per quarter. The first part of our two-part model predicted whether a patient had any Medicare spending using a logistic regression. The second part used a generalized linear model to predict the amount of spending conditional on any spending. We present our results from these models as marginal effects across both parts to make inferences about the entire study population.
Our models included ACO fixed effects to account for non-time varying ACO-specific effects, quarter-year fixed effects, the beneficiary characteristics described above to control for beneficiary-level factors that may simultaneously influence out-of-network care and costs (e.g. comorbidity), the organizational characteristics described above (e.g. number of providers, risk-bearing status, size), and selected regional characteristics. In addition to controlling for seasonal effects, quarter-year fixed effects allowed us to account for differences in the way beneficiaries were attributed to ACOs in 2012 compared to the other years (2012 attribution was based on 2013 primary care utilization, resulting in higher levels of out-of-network primary care for 2012). To make our results more interpretable, we used our models to predict the annual change in spending across all ACOs if every ACO decreased out-of-network primary care by one tenth of a percentage point (which represents 1% of the median 2015 level). Eleven ACOs in the 2014 Medicare Provider RIF and SSP PUF had no aligned NPIs at the time of this analysis. Therefore, beneficiaries aligned to these ACOs were dropped (0.5% or n=56,024 beneficiary-quarter observations).
Sensitivity Analyses
We conducted several sensitivity analyses. Because more complex patients are also more likely to seek care outside the network and have higher spending, ACOs with more complex patients may have higher out-of-network care and spending. Although our main analysis controlled for beneficiary comorbidity, endogeneity may still introduce bias. To examine the size of this potential issue we ran the models without controls. We also tested the sensitivity of our main results to this issue by calculating out-of-network care using a random 50% “holdout” sample of beneficiaries in each ACO-year and predicting spending for the remaining 50% of beneficiaries. Our next sensitivity analysis included a measure of whether or not a health information organization was present in the HRR in which the majority of ACO beneficiaries reside, as health information organizations may facilitate lower healthcare costs and greater care continuity. Our next three sensitivity analyses tested the robustness of our results to outliers in out-of-network primary care. Outliers may exist due to differences in how patients are attributed to ACOs in 2012, and because some patients are attributed to ACOs despite having a very low number of primary care visits. Finally, our last sensitivity analysis used lagged levels of out-of-network care to assess the robustness of our main analysis to learning effects. Full details of our methodology can be found in Appendix Exhibit A1 (24).
Limitations
Our study has several limitations. First, because we used a retrospective observational design, the potential for omitted variable bias exists. We addressed this using the sensitivity analyses described above. Second, the findings of our study may not apply to ACOs outside the study sample, such as commercial ACOs, Medicare Next Generation ACOs, and ESRD Seamless Care Organizations. Nonetheless, given that the vast majority of Medicare ACOs participate in the SSP and Medicare is the main driver of the ACO model, our findings are still critically important to understand how ACO design can influence spending. Finally, it is important to note that we did not examine the association between out-of-network care and other measures of ACO performance (e.g. processes and outcomes). Therefore, we cannot provide insight into the relationship between out-of-network care and quality. Future research will need to examine this relationship, especially in light of our finding that ACOs that serve disadvantaged populations have higher out-of-network care. If out-of-network care is also associated with poorer quality, these ACOs may also struggle to meet the required benchmarks, further exacerbating existing disparities.
Results
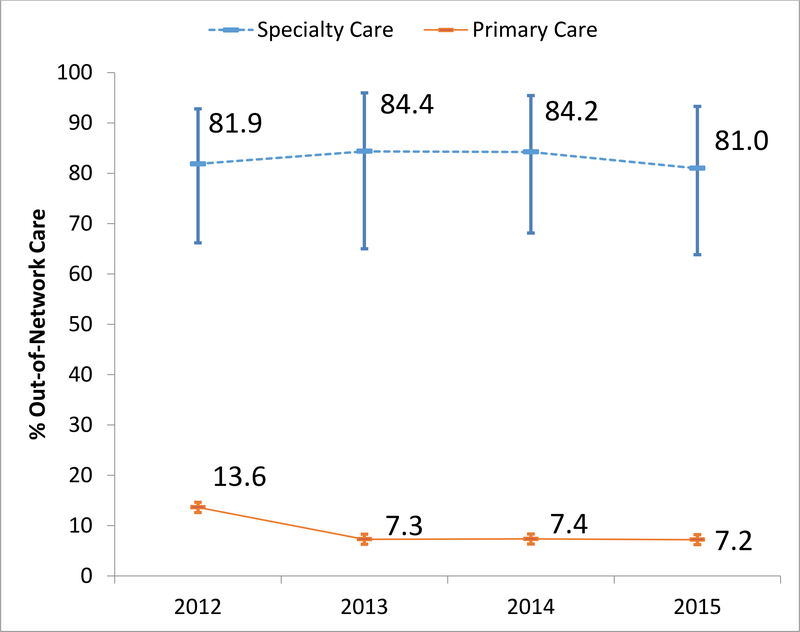
Our sample included 1,604,809 unique beneficiaries. The number of SSP ACOs from which these beneficiaries received care grew from 114 in 2012 to 392 in 2015. Overall, the median level of out-of-network primary care was 8% [interquartile range (IQR): 6%, 10%] and the median level of out-of-network specialty care was 82% (IQR: 66%, 95%). While overall levels remained constant across study years (Exhibit 1), we observed variation in yearly change in out-of-network care at the ACO level. Across all study years, the median yearly percentage point change in out-of-network care was −0.27 percentage points (IQR: −1.77, 0.59) for primary care and 0.00 percentage points (IQR: −1.84, 1.31) for specialty care; representing a −3.54% (IQR: −19.72%, 8.43%) and 0.00% (IQR: −2.40%, 1.75%) change, respectively. Levels of out-of-network primary care and out-of-network specialty care were not highly correlated in any year (average correlation: 0.23). Quarterly spending per beneficiary ranged from $0 to $391,937 for total spending, $0 to $379,498 for inpatient spending, $0 to $330,645 for outpatient spending, $0 to $117,135 for skilled nursing facility spending, and $0 to $350,531 for emergency department spending; the distribution of spending was left skewed for all spending categories, with many beneficiaries spending $0.
Exhibit 1.
Median and Interquartile Range of Percent of Primary Care and Specialty Care Delivered Out of Network for Medicare Shared Savings Program Accountable Care Organizations by Year (2012–2015)
Source: Authors’ analysis of 2012–2015 Medicare Claims
Relationship between ACO Characteristics and Out-of-Network Care
ACOs in the highest quartile of out-of-network primary care and ACOs in the highest quartile of specialty care shared common characteristics. Compared to ACOs in the lower three quartiles, these ACOs had significantly different patient, organizational, and regional characteristics (Exhibit 2). These ACOs cared for beneficiaries who had more comorbidities, were older, were more likely to be dual eligible, and were more likely to be black or Hispanic. These ACOs also had fewer beneficiaries and providers, were more likely to be physician-led, were less likely to have an acute care hospital, and had a larger proportion of PCPs. They were also more likely to be located in rural areas and in areas with higher poverty levels and less educated populations.
Exhibit 2.
Characteristics of ACOs in the Top versus Lower 3 Quartiles of Out-of-Network Care in 2015
| Out-of-Network Primary Care | Out-of-Network Specialty Care | |||||
|---|---|---|---|---|---|---|
| Lower 3 Quartiles | Top Quartile | Difference | Lower 3 Quartiles | Top Quartile | Difference | |
| Number of ACOs (n) | 294 | 98 | 294 | 98 | ||
|
Patient Characteristics (mean) | ||||||
| Mean No. Comorbidities | 1.6 | 1.8 | 0.2**** | 1.6 | 1.7 | 0.1** |
| Mean Age | 76.1 | 76.3 | 0.2** | 76.1 | 76.2 | 0.1 |
| % Dual Eligible | 10.9 | 19.1 | 8.2**** | 12.0 | 16.0 | 4.0*** |
| % Black | 7.2 | 10.1 | 2.9** | 7.4 | 9.6 | 2.2** |
| % Hispanic | 4.6 | 9.3 | 4.7**** | 4.7 | 9.1 | 4.4**** |
| % White | 83.8 | 74.6 | −9.2**** | 82.8 | 77.5 | −5.3** |
| % Other Race/Ethnicity | 4.4 | 6.0 | 1.6 | 5.2 | 3.8 | −1.4 |
| % Female | 58.5 | 58.5 | 0.0 | 58.3 | 59.1 | 0.8** |
|
ACO Organizational Characteristics (%) | ||||||
| Leadership | ||||||
| Physician Led | 40.8 | 54.1 | 13.3** | 36.4 | 67.4 | 31.0**** |
| Hospital Led | 22.5 | 13.3 | −9.2** | 23.1 | 11.2 | −11.9**** |
| Joint Led | 36.7 | 32.7 | −4.0** | 40.5 | 21.4 | −19.1**** |
| Risk Model | ||||||
| 1-Sided Riska | 99.0 | 100.0 | 1.0 | 99.3 | 99.0 | −0.3 |
| 2-Sided Riskb | 1.0 | 0.0 | −1.0 | 0.7 | 1.0 | 0.3 |
| Participating Organizations | ||||||
| Acute care hospital | 54.8 | 29.6 | −25.2**** | 60.2 | 13.3 | −46.9*** |
| Critical access hospital | 15.7 | 10.2 | −5.5 | 17.4 | 5.1 | −12.3** |
| Federally qualified health center | 15.3 | 31.6 | 16.3**** | 19.1 | 20.4 | 1.3 |
| Rural | 0.7 | 5.1 | 4.4** | 1.0 | 4.1 | 3.1** |
|
Regional Characteristics (mean) | ||||||
| Number of Primary Care Doctors | 853.8 | 1281.7 | 427.9** | 1039.7 | 724.0 | −315.7 |
| Number of Total MDs (in Hundreds) | 31.4 | 48.3 | 16.9*** | 38.5 | 26.7 | −11.8 |
| Number of SNFs | 39.2 | 51.8 | 12.6 | 46.3 | 30.6 | −15.7 |
| Number of Hospitals | 13.6 | 19.4 | 5.8** | 16.0 | 11.9 | −4.1 |
| Median Per Capita Income (in Thousands) | 57.9 | 57.4 | −0.5 | 58.7 | 54.8 | −3.9** |
| % Families at or below poverty level | 11.1 | 12.5 | 1.4** | 11.1 | 12.6 | 1.5** |
| % Adults 25 years or older with less than a high school education | 12.2 | 14.6 | 2.4**** | 12.4 | 14.1 | 1.7*** |
Source: Authors’ analysis of 2015 Medicare Claims, Leavitt Partners ACO Database, and 2015 data from the Area Health Resource Filea
Notes: Statistical significance compares ACOs in highest quartile of out-of-network care with ACOs in lower 3 quartiles; significance based on ANOVA for continuous variables and Chi-squared test for categorical variables
p<0.10
p<0.05
p<0.01
p<0.001
1-Sided Risk ACOs receive incentives for spending below benchmarks and are not penalized for spending above benchmarks
2-Sided Risk ACOs receive larger incentives for spending below benchmarks than 1-Sided Risk ACOs, but are penalized for spending above benchmarks
Relationship between Out-of-Network Care and Spending
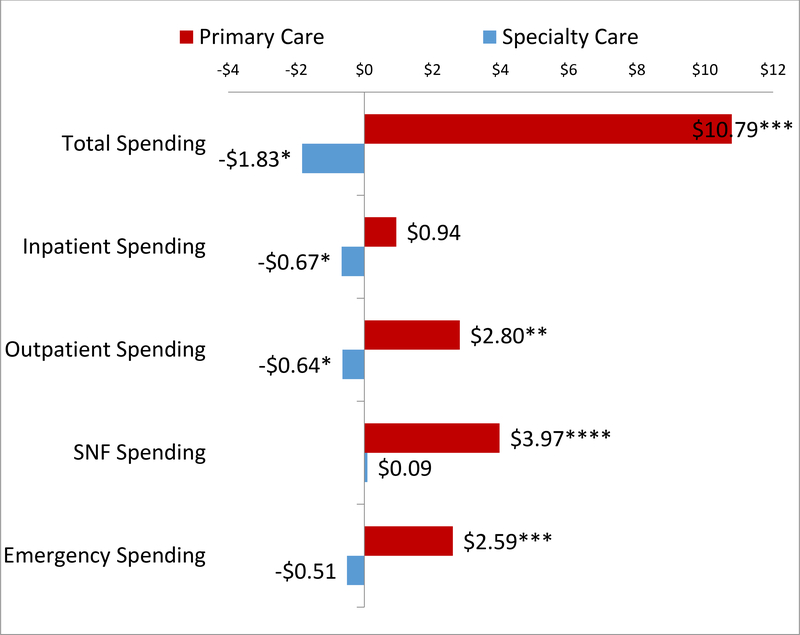
The median level of total per beneficiary spending for ACO beneficiaries was $401 per quarter (IQR: $140, $1131). Holding control characteristics constant, increasing levels of out-of-network primary care was associated with higher per-beneficiary spending (Exhibit 3). Each percentage point increase in out-of-network primary care was associated with a $10.79 increase in per quarter total spending for each beneficiary (p-value=0.001). When we examined the relationship between out-of-network primary care and spending by setting, we found that out-of-network primary care was associated with increases in outpatient, skilled nursing facility, and emergency department settings; each percentage point increase in out-of-network primary care was associated with a $2.80 increase in outpatient spending (p-value=0.015), a $3.97 increase in skilled nursing facility spending (p-value<0.001), and a $2.59 increase in emergency spending (p-value=0.008). However, the same was not true for specialty care; changes in out-of-network specialty care were not significantly associated with total spending or spending in any specific setting (Exhibit 3). To put these numbers in context at the national level, our results suggest that at an estimated quarterly savings of $10.79 per percentage point increase in out-of-network primary care, if all SSP ACO’s decreased the level of out-of-network primary care by one tenth of a percentage point for all 10.5 million of its beneficiaries (based on 2018 enrollment), national ACO spending would decrease by an estimated $11.3 million a quarter, or approximately $45 million a year.
Exhibit 3.
Association between Percentage Point Increase in Out-of-Network Primary Care and Specialty Care and Per-Beneficiary-Per-Quarter Spending, by Spending Category
Source: Authors’ analysis of 2012–2015 Medicare Claims
Notes: Bars indicate marginal effect of percentage point increase in out-of-network care on spending category. One model was run for each spending category. Models include ACO and quarter-year fixed effects and the following controls (not shown): sex, race, age, Medicare/Medicaid dual eligibility, Hierarchical Condition Categories (HCC), whether the beneficiary was a new Medicare enrollee, percent of ACO providers that were primary care providers, number of beneficiaries (based on number of beneficiaries in sample), number of providers, ACO leadership (hospital, physician, or joint), whether the ACO included a critical access hospital, federally qualified health center, and/or acute care hospital, ACO risk-bearing status (1-sided or 2-sided), number of Primary Care Providers, MDs, and skilled nursing facilities in county, county population, and county median per capita income; *p<0.10, **p<0.05; ***p<0.01, ****p<0.001
Sensitivity Analysis
When we ran the analyses without time-varying controls to assess the potential size of selection bias, we found that out-of-network primary care was still significantly associated with higher total, outpatient, and skilled nursing facility spending (Appendix Exhibit A3 (24)); the model predicting emergency department spending did not converge. Additionally, results from our second sensitivity analysis, which used the level of out-of-network care for a random 50% subsample to predict spending on the remaining 50% of beneficiaries, were also consistent with our main finding that out-of-network primary care is associated with total spending (Appendix Exhibit A4 (24)). Results from our third sensitivity analysis, where we controlled for the presence of Health Information Organizations, were also consistent with our main findings (Appendix Exhibit A5 (24)). In addition, results from our sensitivity analyses which removed outliers were also consistent with our main results (Appendix Exhibit A6–A8 (24)). Our final sensitivity analysis, which used one-year lags, suggests the level of out-of-network care does not significantly predict the next year’s level of spending (Appendix Exhibit A9 (24)).
Discussion
In a national study of Medicare ACOs, we found that higher out-of-network primary care was associated with higher total spending. When we broke this relationship down into spending by place of service, out-of-network primary care was associated with higher spending in outpatient, skilled nursing, and emergency settings. We observed that ACOs that serve poorer and sicker patients and those from underserved backgrounds were more likely to have high levels of out-of-network primary care. Collectively, our findings suggest that reducing out-of-network primary care could yield substantial savings for SSP ACOs.
The existing literature on out-of-network care in Medicare ACOs has focused primarily on specialty care (4, 10). However, we found that out-of-network specialty care was not associated with an organization’s performance. The lack of an association may explain why early SSP evaluations reveal only modest ACO effects on spending with most gains occurring in regions with high pre-ACO spending (1, 25). Taken together, our study suggests that ACO administrators may have focused too much attention on reducing specialty care usage, while overlooking the importance of out-of-network primary care (26).
Our study also suggests that SSP ACOs with high out-of-network primary care may have difficulty achieving shared savings. However, even small changes in out-of-network primary care could have large effects on performance. Indeed, lowering out-of-network primary care across all SSP ACOs by one tenth of a percentage point could save Medicare an estimated $45 million annually. This finding is most relevant for ACOs with high shares of beneficiaries from underserved backgrounds, who are more likely to receive out-of-network primary care.
One possible explanation for the association between out-of-network primary care and healthcare spending relates to churn. Specifically, higher spending ACOs may also have substantial beneficiary and provider turnover year-to-year, leading to both higher levels of out-of-network care and poorer organizational performance (27). However, if this were the case, we would not expect differential effects of out-of-network primary care by place of service as we observed.
There are at least two plausible reasons for why out-of-network primary care was associated with healthcare spending in outpatient, skilled nursing, and emergency settings. First, ACO-participating PCPs may be acting as “gate keepers,” reducing the provision of unnecessary or lower value services, which are often delivered in these settings. For example, PCPs may limit access to specialists who deliver lower value care, or they may refer patients to home health agencies instead of skilled nursing facilities. Previous studies, showing that cost savings in ACOs are driven by decreases in utilization of unnecessary and lower value services in skilled nursing facilities (16, 28), provide support for this possibility. Second, ACO-participating PCPs may be acting as “care coordinators,” ensuring that patients are not receiving duplicative care in outpatient and emergency settings. Prior research, revealing that care coordination is associated with less redundant imaging in emergency departments and fewer emergency department visits (20, 29–31), supports this possibility.
Our finding that-of-network primary care is not associated with differences in inpatient spending is not surprising given that the bulk of ACO savings results from reductions in overused skilled nursing services, outpatient departments, and home health care (1, 28, 32). This is likely due to the fact that ACO-participating PCPs have limited control over the utilization of inpatient services, or that interventions at the primary care level need more time to mature before we see meaningful effects on inpatient spending.
Policy Implications
In light of the recent SSP overhaul (“Pathways to Success”) that will require ACOs to assume downside risk more quickly, our findings suggest that controlling the level of out-of-network primary care may be one mechanism to lower spending. Our findings also suggest that Medicare may realize more savings if all its ACO initiatives created explicit incentives for beneficiaries to seek primary care within network. For instance, co-pays could be lowered for in-network primary care services. The ACO Beneficiary Incentive Program, which allows certain ACOs to pay beneficiaries a monetary incentive to receive primary care in-network, could also be expanded (33). Of course, incentives like these must be balanced with preservation of patient choice—a defining characteristic of SSP ACOs.
We also found that ACOs with a high level of out-of-network primary care serve poorer and sicker patients and those from underserved backgrounds. Perhaps these patients lack the mobility necessary to maintain continuity of care (34). Such an explanation is supported by prior work, showing that ACOs with higher proportions of disadvantaged populations are less likely to achieve shared savings than those with more affluent ones (12). Without additional support, it is less likely that these ACOs will be able to thrive under current Medicare policies, leading to further bifurcation of an already two-tiered healthcare system (35). To avoid exacerbating existing disparities, policymakers should consider providing data on out-of-network care to these ACOs to help identify reasons why their patients are seeking primary care services elsewhere. They could also provide training and resources to encourage these ACOs to offer telehealth services in line with those covered under the Bipartisan Budget Act of 2018 (36).
Conclusion
In this study, we found that higher out-of-network primary care is associated with higher healthcare spending for ACO beneficiaries, especially in outpatient, skilled nursing, and emergency settings. These findings highlight the critical role of primary care physicians and suggest that ACOs that are not able to keep primary care services in-network are less likely to succeed under current ACO policies. Relatedly, we also found that ACOs with higher levels of out-of-network primary care were also more likely to serve disadvantaged patients, suggesting that current Medicare ACO design may inadvertently exacerbate existing healthcare disparities. Consequently, policymakers may want to consider explicit incentives for beneficiaries to seek primary care within their assigned ACOs.
Supplementary Material
References
- 1.McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early Performance of Accountable Care Organizations in Medicare. N Engl J Med. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McClellan M, Kocot SL, White R. Early evidence on medicare acos and next steps for the medicare aco program (updated). Health Affairs Blog. 2015. [Google Scholar]
- 3.Muhlestein D, Hall C. ACO quality results: good but not great. Health Affairs Blog. 2014. [Google Scholar]
- 4.McWilliams J, Chernew ME, Dalton JB, Landon BE. Outpatient care patterns and organizational accountability in medicare. JAMA Internal Medicine. 2014;174(6):938–45. [DOI] [PubMed] [Google Scholar]
- 5.Han MA, Clarke R, Ettner SL, Steers WN, Leng M, Mangione CM. Predictors of out-of-ACO care in the medicare shared savings program. Med Care. 2016;54(7):679–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McWilliams JM. Cost containment and the tale of care coordination. N Engl J Med. 2016;375(23):2218–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Medicare Payment Advisory Commission. Healthcare Spending and the Medicare Program. In: Commission MPA, editor. Washington, DC: 2016. [Google Scholar]
- 8.Safran DG, Tarlov AR, Rogers WH. Primary Care Performance in Fee-for-Service and Prepaid Health Care Systems: Results From the Medical Outcomes Study. JAMA. 1994;271(20):1579–86. [PubMed] [Google Scholar]
- 9.Miller RH, Luft HS. Managed Care Plan Performance Since 1980: A Literature Analysis. JAMA. 1994;271(19):1512–9. [PubMed] [Google Scholar]
- 10.Barnett ML, McWilliams JM. Changes in specialty care use and leakage in Medicare accountable care organizations. The American journal of managed care. 2018;24(5):e141–e9. [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis VA, Colla CH, Carluzzo KL, Kler SE, Fisher ES. Accountable Care Organizations in the United States: Market and Demographic Factors Associated with Formation. Health Serv Res. 2013;48(6pt1):1840–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lewis VA, Fraze T, Fisher ES, Shortell SM, Colla CH. ACOs Serving High Proportions Of Racial And Ethnic Minorities Lag In Quality Performance. Health Aff (Millwood). 2017;36(1):57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yasaitis LC, Pajerowski W, Polsky D, Werner RM. Physicians’ Participation In ACOs Is Lower In Places With Vulnerable Populations Than In More Affluent Communities. Health Aff (Millwood). 2016;35(8):1382–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colla CH, Lewis VA, Tierney E, Muhlestein DB. Hospitals Participating In ACOs Tend To Be Large And Urban, Allowing Access To Capital And Data. Health Aff (Millwood). 2016;35(3):431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Medicare Shared Savings Program: shared savings and losses and assignment methodology: specifications. Version 3: Centers for Medicare and Medicaid Services; 2014. [Google Scholar]
- 16.Nyweide DJ, Lee W, Cuerdon TT, Pham HH, Cox M, Rajkumar R, et al. Association of Pioneer Accountable Care Organizations vs Traditional Medicare Fee for Service With Spending, Utilization, and Patient Experience. JAMA. 2015;313(21):2152. [DOI] [PubMed] [Google Scholar]
- 17.Savings Reported By CMS Do Not Measure True ACO Savings. Health Affairs Blog. [Google Scholar]
- 18.Kaufman BG, Spivack BS, Stearns SC, Song PH, O’Brien EC. Impact of Accountable Care Organizations on Utilization, Care, and Outcomes: A Systematic Review. Med Care Res Rev. 2017:1077558717745916. [DOI] [PubMed] [Google Scholar]
- 19.Hsu J, Price M, Vogeli C, Brand R, Chernew ME, Chaguturu SK, et al. Bending The Spending Curve By Altering Care Delivery Patterns: The Role Of Care Management Within A Pioneer ACO. Health Aff (Millwood). 2017;36(5):876–84. [DOI] [PubMed] [Google Scholar]
- 20.Larson BK, Van Citters AD, Kreindler SA, Carluzzo KL, Gbemudu JN, Wu FM, et al. Insights from transformations under way at four Brookings-Dartmouth accountable care organization pilot sites. Health Aff (Millwood). 2012;31(11):2395–406. [DOI] [PubMed] [Google Scholar]
- 21.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998:8–27. [DOI] [PubMed] [Google Scholar]
- 22.Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004:355–60. [DOI] [PubMed] [Google Scholar]
- 23.Deb P, Norton EC. Modeling health care expenditures and use. Annu Rev Public Health. 2018;39:489–505. [DOI] [PubMed] [Google Scholar]
- 24. To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 25.Epstein AM, Jha AK, Orav EJ, Liebman DL, Audet A-MJ, Zezza MA, et al. Analysis Of Early Accountable Care Organizations Defines Patient, Structural, Cost, And Quality-Of-Care Characteristics. Health Aff (Millwood). 2014;33(1):95–102. [DOI] [PubMed] [Google Scholar]
- 26.Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care—two essential elements of delivery-system reform. N Engl J Med. 2009;361(24):2301–3. [DOI] [PubMed] [Google Scholar]
- 27.Hsu J, Vogeli C, Price M, Brand R, Chernew ME, Mohta N, et al. Substantial Physician Turnover And Beneficiary ‘Churn’ In A Large Medicare Pioneer ACO. Health Aff (Millwood). 2017;36(4):640–8. [DOI] [PubMed] [Google Scholar]
- 28.McWilliams JM, Gilstrap LG, Stevenson DG, Chernew ME, Huskamp HA, Grabowski DC. Changes in postacute care in the Medicare Shared Savings Program. JAMA internal medicine. 2017;177(4):518–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cabana MD, Jee SH. Does continuity of care improve patient outcomes? The Journal of Family Practice. 2004;53(12):974–80. [PubMed] [Google Scholar]
- 30.Van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review: Association between continuity of care and outcomes. J Eval Clin Pract. 2010;16(5):947–56. [DOI] [PubMed] [Google Scholar]
- 31.Lammers EJ, Adler-Milstein J, Kocher KE. Does health information exchange reduce redundant imaging? Evidence from emergency departments. Med Care. 2014;52(3):227–34. [DOI] [PubMed] [Google Scholar]
- 32.McWilliams JM, Chernew ME, Landon BE. Medicare ACO program savings not tied to preventable hospitalizations or concentrated among high-risk patients. Health Aff (Millwood). 2017;36(12):2085–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schulz J, DeCamp M, Berkowitz SA. Medicare Shared Savings Program: public reporting and shared savings distributions. Am J Manag Care. 2015;21(8):546. [PMC free article] [PubMed] [Google Scholar]
- 34.Nutting PA, Goodwin MA, Flocke SA, Zyzanski SJ, Stange KC. Continuity of primary care: to whom does it matter and when? The Annals of Family Medicine. 2003;1(3):149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lewis VA, Larson BK, McClurg AB, Boswell RG, Fisher ES. The Promise And Peril Of Accountable Care For Vulnerable Populations: A Framework For Overcoming Obstacles. Health Aff (Millwood). 2012;31(8):1777–85. [DOI] [PubMed] [Google Scholar]
- 36.H.R. 1892—Bipartisan Budget Act of 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.