Abstract
Over the past decade several developments have lead to an increased interest in lower extremity PNBs including transient neurologic symptoms associated with spinal anesthesia, increased risk of epidural hematoma with the introduction of new antithromboembolic prophylaxis regimens, and evidence of improved rehabilitation outcome with continuous lower extremity PNBs. Simultaneously, the field of lower extremity blockade has been revolutionized through our better understanding of functional regional anesthesia anatomy, introduction of new drugs, better and more sophisticated equipment and wider teaching of lower extremity nerve block techniques. This review focuses on techniques and applications of lower extremity nerve blocks in patients having orthopedic surgery or trauma of the lower extremity, as well as potential complications and means to avoid them.
Keywords: regional anesthesia, nerve block, trauma, neurologic complications
LOWER EXTREMITY NERVE BLOCK TECHNIQUES
PSOAS COMPARTMENT BLOCK (LUMBAR PLEXUS BLOCK)
The psoas compartment block (PCB) is a deep block of the lumbar plexus approached posteriorly, and can be performed either as a single injection or as a continuous technique with catheter placement for prolonged analgesia. The PCB block provides anesthesia for thigh surgery and hip fracture repair in combination with a parasacral nerve block.1 The PCB is successfully used for analgesia following total hip arthroplasty (THA)2-4, total knee arthroplasty (TKA)5 and in the treatment of chronic hip pain.2 At the level of L4-L5 the following anatomic structures would be encountered from posterior to anterior; posterior lumbar fascia, paraspinous muscles, anterior lumbar fascia, quadratus lumborum, and the psoas muscle. The common iliac artery and vein lie anterior to the psoas muscle, which is located inside a fascial sheath, the psoas compartment. The most consistent approach to block the entire lumbar plexus with a single injection is via the posterior approach, since the lumbar plexus travels through the body of the psoas muscle. The PCB provides consistent anesthesia in the distributions of the femoral, lateral cutaneous nerve of the thigh, and the obturator nerves. Several descriptions of the needle entry site for the PCB have been described.1-3,6,7 (Figure 1). was significant (p<0.05). There was no statistically significant difference in the expression of HER-2 protein in cases with and without signs of vascular invasion. In cases with no metastases in axillary lymph nodes, expression of the HER-2 protein was significantly (p<0.05) higher in comparison to cases with no metastases. Most descriptions rely on bony contact with the transverse process as a guide to depth of needle placement. The distance from the skin to the lumbar plexus ranges from 6.1-10.1 cm in men and 5.7-9.3 cm in women and this distance correlates with gender and body mass index (BMI). The distance from the transverse process to the lumbar plexus is typically less than 2 cm, and this is independent of BMI or gender. Contact with the transverse process provides a consistent landmark to avoid excessive needle penetration during PCB.8 The depth of needle insertion is emphasized because of the complications associated with deep needle penetration including renal hematoma, pneumocele, total spinal anesthesia, and unintended intraabdominal and intervertebral disk catheter placement.8-11 Epidural spread of local anesthetic is a common side effect of PCB occurring in 9 -16% of adult patients.12,13 In children, Dalens reported a greater than 90% incidence of epidural spread when using the original landmarks of Chayen compared to no epidural spread when using the landmarks as modified by Win-nie.14 The epidural spread is attributed to diffusion of the local anesthetic into the epidural space when large volumes of local anesthetic (greater than 20 mL) are used. In most cases of epidural spread, residual lumbar plexus blockade is apparent after resolution of the contralateral block. However, there are case reports of total spinal anesthesia occurring during PCB and vigilance must be maintained during the management of this block.10,15
FIGURE 1.

Lumbar Plexus Block: A10 cm long needle is inserted at L3/4 level and 3-4 cm lateral to the midline.
(Reproduced with Permission from: HadZicA., Vhka J. Peripheral Nerve Blocks: Principles and Practice. McGrawHiH New York, NY, 2003.).
CONTINUOUS PSOAS COMPARTMENT BLOCKS
Continuous PCB techniques have been described to provide analgesia following a variety of operations including THA, TKA, open reduction and internal fixation (ORIF) of acetabular fractures, ORIF of femur fractures and anterior cruciate ligament (ACL) reconstruction.4,8,16-20 Interest in this block developed as practitioners sought alternatives to central neuraxial techniques that could provide consistent analgesia following hip, femur and knee surgery. One advantage of PCB over other continuous approaches to the lumbar plexus is the decreased likelihood of catheter dislodgement because of the large muscle mass that must be traversed to reach the lumbar plexus. Continuous infusion of local anesthetic should be started after an initial bolus is given through the catheter. Care must be taken to watch for local anesthetic toxicity, intravascular injection, and the unilateral sympathetic blockade that accompanies a PCB.
FEMORAL NERVE BLOCK
Indications for single injection femoral nerve block (FNB) include anesthesia for knee arthroscopy in combination with intraarticular local anesthesia and analgesia for femoral shaft fractures, ACL reconstruction, and TKA in multimodal regimens.21-27 The femoral nerve divides into the posterior and anterior divisions shortly after it emerges from under the inguinal ligament and undergoes extensive arborization. Commonly the anterior branch of the femoral nerve, which innervates the sartorius muscle, will be identified first. Vloka and Hadžić reported this to be a common first motor re-sponse.28 Stimulation of this branch leads to contraction of the sartorius muscle on the medial aspect of the thigh and should not be accepted, as the articular and muscular branches arise from the posterior part of the femoral nerve. The needle should be redirected slightly laterally and deeper to encounter the posterior branch of the femoral nerve. Stimulation of this branch is identified by patellar ascension as the quadriceps contract (Figure 2).
FIGURE 2.

Femoral Nerve Block: A 5 cm needle is inserted at the femoral crease and immediately laterally to the pulse of the femoral artery The nerve is typically stimulated at a depth of 1-3 cm.
(Reproduced with Permission from: HadiuiA., Vhka J. Peripheral Nerve Blocks: Principles and Practice. McGrawHUL New York, NY.2003.).
A 3-IN-1 BLOCK
During FNB, it has been advocated to use a higher volume of local anesthetic and apply firm pressure just distal to the needle during and a few minutes after injection to block the femoral, lateral femoral cutaneous, and obturator nerves, the so named 3-in-1 block.29 However, despite many efforts to consistently produce a 3-in-1 block, the efficiency of these maneuvers has not been demonstrated. In most reports, the femoral nerve is the only nerve consistently blocked with this approach.30-32 Occasional blockade of the lateral femoral cutaneous (LFC) nerve occurs through lateral diffusion of local anesthetic and not through proximal spread to the lumbar plexus.31 The obturator nerve is less frequently anesthetized during 3-in-1 block than the LFC nerve, which is not surprising given the number of fascial barriers between these structures at the level of the inguinal ligament.
CONTINUOUS FEMORAL NERVE BLOCK
Continuous FNB has been shown to improve surgical outcome following major knee and vascular surgery of the lower extremity compared to intravenous narcotic therapy or continuous intraarticular infusions of analgesics.33-36 Two prospective randomized studies examined three different modes of analgesia, continuous FNB, epidural analgesia, and intravenous narcotic therapy following TKA.33,34 These studies demonstrated improvement in perioperative rehabilitation scores and a decreased duration of stay in a rehabilitation center for patients receiving the regional anesthesia techniques. Continuous FNB was shown to have equivalent analgesia with fewer side effects than epidural analgesia in both of these studies.33,34 However, not all investigators have been able to demonstrate these improvements in outcome with continuous FNBs. Lang found no difference between patients receiving a single injection FNB and patients receiving a continuous FNB after TKA.32 The accuracy of catheter placement may play a role in these conflicting findings. In a prospective study, Capdevila showed that continuous FNB using a standard approach led to unpredictable catheter placement. In the Capdevila study, a vastus intermedius muscle response was elicited at 0.5mA, the sheath was distended with 5 mL of saline, a catheter was inserted 16-20 cm, then a bolus of local anesthetic was given through the catheter.37 Most of the catheters tended to course medially in the direction of the psoas muscle or laterally in the direction of the iliacus muscle. The accuracy of final catheter placement correlated well with the quality of analgesia following proximal lower limb surgery, although VAS values were generally low in all groups.37
LATERAL FEMORAL CUTANEOUS NERVE BLOCK
The LFC nerve of the thigh is a sensory nerve that supplies the cutaneous sensation to a large but variable area from the inguinal ligament to the knee on the lateral aspect of the thigh.38 LFC nerve block is most commonly used as the sole anesthetic during diagnostic muscle biopsy and harvesting of split thickness skin grafts.39,40 It has also been used to provide analgesia in elderly patients undergoing hip fracture repair.41 However, in a study comparing LFC nerve block, FNB, and patients receiving no block following femoral neck repair, LFC nerve block was not as effective at controlling postoperative pain as FNB.42 Typically this block is done as a blind, “fan” technique with a variable success rate. This may be due to variability in the innervation of the nerve or imprecise localization of the nerve. Shannon compared the traditional fan technique for LFC nerve block to the use of a nerve stimulator technique seeking tingling in the distribution of the nerve.43 A 40% success rate with the “fanning” technique was reported compared to 100% with the nerve stimulating technique. There was no difference in the extent of the blockade in successful blocks. FNB has been reported following LFC block,44 which is not surprising given the fact that most FNB literature reports that FNB results in anesthetic spread to the LFC nerve.
SAPHENOUS NERVE BLOCK
The saphenous nerve follows the saphenous vein to the medial malleolus and supplies the cutaneous area of the medial aspect of the calf and foot to the level of the midfoot. The saphenous nerve block is often combined with a sciatic block to provide anesthesia and analgesia for surgery involving the medial aspect of the lower leg and foot. The saphenous nerve is a sensory nerve and does not contribute to the bony innervation of the foot. Approaches to the saphenous nerve along its entire course, from the adductor canal to the ankle, have been described. Success rates vary widely between techniques. For example, successful block is reported in 33-65% of cases with a field infiltration performed medially at the level of the tibial plateau,45,46 70-80% of cases with the transsartorial approach,45,47 95-100% of cases with femoral paracondylar approach,47 and nearly 100% of cases with the paravenous ap-proach.46 The saphenous nerve has been reported to be selectively blocked, sparing of the quadriceps musculature, in the adductor canal.48 However, this finding has not been confirmed in a large series of patients receiving this approach for a saphenous nerve block.
PSOAS COMPARTMENT BLOCK VERSUS FEMORAL NERVE BLOCK
Parkinson compared the extent of blockade following FNB and the posterior approach to the lumbar plexus.13 They compared the extent of blockade of the lumbar plexus with four different methods: posterior approach at L3 (posterior approach of Dekrey) and L4-5 (Chayen’s approach) with a nerve stimulator using noninsulated needles, and anterior FNB (approach of Winnie) with a paresthesia technique and nerve stimulation technique.13 The FNB had a 100% success rate, while the LFC nerve block success rate was 85-95%. The obturator nerve, as assessed by thigh adduction, was blocked 100% of the time with the posterior approaches and never with the anterior approaches. Limitations of this report include lack of details regarding the type of nerve stimulation, the small sample size, and exclusion of patients in whom FNB failed to develop. A more recent comparison has been made between PCB and FNB.49 In this study, patients receiving a PCB developed a sensory block of the femoral, LFC, and obturator nerves in 100, 97, and 77% of patients versus 93, 63 and 47% of the patients receiving a FNB.
CONTINUOUS PSOAS COMPARTMENT BLOCKS VERSUS EPIDURAL ANALGESIA
Advantages of continuous PCB compared to epidural block include unilateral analgesia and motor block, lack of impairment of bladder function, and improved risk/benefit ratio in patients receiving anticoagulation medications following surgery. These advantages must be weighed against the disadvantages of incomplete blockade for anesthesia, and the need for supplementation in a balanced analgesic regimen for effective analgesia. Türker recently compared continuous PCB with epidural block for analgesia following THA under combined general/regional technique and demonstrated that continuous PCB provided excellent intra-and postoperative analgesia with a low incidence of complications.4 Epidural block took longer to perform and had a significantly higher incidence of hypotension, while the analgesia and patient satisfaction provided by the two blocks were similar. Epidural block also provided more motor blockade, longer time to ambulation, and significantly more complications.
CONTINUOUS PSOAS COMPARTMENT BLOCKS VERSUS CONTINUOUS FEMORAL BLOCKS
Following TKA, continuous FNB and continuous PCB reduce narcotic consumption and pain scores compared to intravenous morphine usage alone.34 However, no differences in outcome were observed between the two peripheral nerve block groups despite a more consistent presence of obturator nerve block in the psoas compartment group. Both the continuous FNB and continuous PCB can be effective for pain control after a TKA and the choice of which continuous nerve block to choose should be based on patient profile and preference, comfort of the anesthesiologist in placing the block and catheter, and preference of the surgeon.
PARASACRAL BLOCK
The parasacral nerve block (PSNB) described by Man-sour in 1993 has been described as more than an isolated sciatic nerve block.50,51 It has been used to provide analgesia following major foot and ankle reconstruction. PSNB will consistently block both components of the sciatic nerve and the posterior cutaneous nerve of the thigh. Spread of local anesthetic may also anesthetize other branches of the sacral plexus including the superior and inferior gluteal, and pudendal nerves. The pelvic splanchnic nerves, the terminal portion of the sympathetic trunk, the inferior hypogastric plexus, and the obturator nerve all lie in close proximity to the elements of the sacral plexus and may all be anesthetized with this approach. For procedures around the knee this may be advantageous over more distal approaches to the sciatic nerve.51,52 For procedures below the knee, the adductor weakness from the obturator and superior gluteal nerve block may actually be disadvantageous for mobilization of the patient following blockade. The sympathetic nerve supply to the bladder is in close proximity to the sacral plexus, but problems with voiding and the need for bladder catheterization after PSNB have not been reported.52 A notable difference from other approaches to the sciatic nerve is the type of muscle response deemed acceptable as an endpoint for injection. Mansour described contraction of the hamstring muscles (biceps femoris, semitendinous) above the knee as the endpoint for PSNB with consistent success.50
CONTINUOUS PARASACRAL BLOCKS
Continuous PSNBs have been used in combination with PCBs to provide lower extremity anesthesia for TKA, above the knee amputation, ACL repair and a variety of other lower extremity procedures.53 Gaertner reported successful catheter placement, as confirmed by radiographic contrast dye, in 86 out of 87 consecutive patients undergoing lower extremity surgery. All patients developed analgesia in the distribution of the tibial, peroneal and cutaneous nerve of thigh.
SCIATIC NERVE BLOCK: AT THE LEVEL OF THE GLUTEUS MAXIMUS
The sciatic nerve, the largest nerve derived from the sacral plexus, innervates the posterior thigh and almost the entire leg below the knee. The most common indications for sciatic nerve block (SNB) are anesthesia and analgesia for foot and ankle surgery. Gaston Labat first described the approach to the SNB, now referred to as the Classic Approach of Labat, at the beginning of the 20th century. This approach is based on the bony relationship of the posterior superior iliac spine (PSIS) and the greater trochanter with the patient positioned in a modified Sims position (Figure 3). Winnie was the first to modify the original description by adding another landmark, the sacral hiatus, to more precisely account for varying body habitus.54 The reported success rate of this approach is ranges from 33% to 95%.54-57 More recently, Franco described a simplified approach to the SNB in the prone position. The needle entry site is perpendicular to the floor 10-cm lateral from the middle of the intragluteal sulcus regardless of the patient’s gender or body mass index.58 The sciatic nerve was found by trainees in three passes or less in 85% of the cases reported. Whether the success of this simple approach will be replicated in a larger sample size remains to be seen.
FIGURE 3.
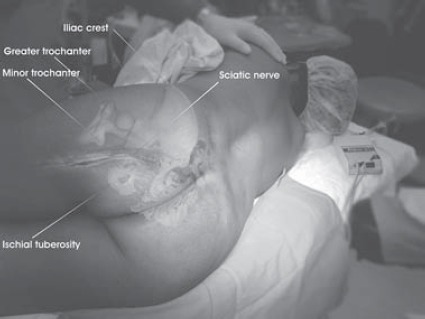
Sciatic Nerve Block: Anatomical relationships of importance to the technique.
(Reproduced with Permission from: Hadžić A., Vloka J. Peripheral Nerve Blocks: Principles and Practice. McGrawHill, New York, NY, 2003.).
SUBGLUTEAL APPROACHES TO THE SCIATIC NERVE
Raj described a supine approach to the sciatic nerve in the flexed hip position initiating the block at the midpoint between the greater trochanter of the femur and the ischial tuberosity.55 The positioning of the patient was thought to be advantageous compared to the classic approach of Labat by “thinning the gluteus maximus muscles, making the sciatic nerve more superficial”. However identifying these bony landmarks in very obese patients is sometimes difficult and maintaining this position requires additional personnel to assist the patient. A lateral subgluteal approach to the sciatic nerve using the greater trochanter of the femur as a landmark was first described by Ichniyanagi in 1959. Other investigators have described a high success rate using this high lateral approach with a slightly more caudal entry point.57 When using this approach, the success rate of the blockade of the posterior cutaneous nerve of the thigh was 83%. Although theoretically this nerve should reliably be blocked in most proximal approaches to the sciatic nerve, the success rate of blockade of the posterior cutaneous nerve of the thigh is not usually reported. The anterior approach to the sciatic nerve has the appeal of supine positioning and one skin prep when performing a combined femoral and sciatic nerve block. However, its clinical utility has been limited by its complexity, patient discomfort, and low success rate.59,60 Numerous variations of the original Beck’s technique description have been described.61,62 In separate studies, Vloka and Hadžić, and Moore described the importance of internal rotation of the leg if the path to the sciatic nerve is obstructed by the lesser trochanter.63,64 An MRI study of the anatomy of this area found that in 65% of patients the sciatic nerve is inaccessible from the anterior approach at the level of the lesser trochanter.65 These authors suggested needle placement 4 centimeters lower, where obstruction to the sciatic nerve occurred in only 5% of the patients. Dalens compared the success rate of the posterior, lateral and anterior approaches to the sciatic nerve in children.66 Although a success rate of 90% with all approaches was reported, fewer manipulations were required to perform either a lateral or posterior approach compared to the anterior approach. Recently, a medial approach to the sciatic nerve at the level of the lesser trochanter was reported in series of 10 children.67 Advantages of this approach are the lack of obstruction from the femur and no muscle mass to transverse. The authors reported a 70% rate of blockade of the posterior cutaneous nerve of the thigh with this medial approach. di Bendetto recently described results from 135 consecutive patients using a posterior subgluteal approach to the sciatic nerve.68 The time to perform the block was 41 ± 25 s (mean ± SD), with an average of 2 needle redirections. The degree of discomfort reported was very low and only 16 patients (12%) reported severe pain during placement of the block. In contrast to this, Fanelli reported patient discomfort in 88% of patients receiving a classic Labat approach to the sciatic nerve.69
SCIATIC NERVE BLOCK AT THE LEVEL OF THE POPLITEAL FOSSA
Popliteal block is typically used for foot and ankle sur-gery.70-72 This technique offers advantages over spinal anesthesia in patients having short saphenous vein stripping.73 The block has also been successfully utilized in the pediatric population.74 As opposed to an ankle block, popliteal block anesthetizes the musculature of the lower leg which likely improves tolerance for a calf tourniquet and provides an immobile foot for surgery. Performance of popliteal fossa block in patients with previous TKA or vascular bypass (femoral-popliteal) should be done with care even though there are no reported cases of joint infections or graft disruption relating to needle placement in these patients. The components of the sciatic nerve may be blocked at the level of the popliteal fossa via a posterior or lateral approach. Access to the sciatic nerve may also occur with the patient in the lithotomy position.75 Continuous techniques have been described using both the poste-rior76-78 and lateral79 approaches. The posterior approach to the popliteal fossa is accomplished with a patient in the prone position.64 In order to block the sciatic nerve before it divides, injection of local anesthetic is given 7-10 cm above the popliteal crease (Figure 4).58,71,72,80-82 With a single injection technique, inversion may be best predictor of complete neural block of the foot.83 A lateral approach to blockade of the sciatic nerve in the popliteal fossa has recently been described.83-86 Success rate with all approaches to the popliteal sciatic nerve block is typically 90-95%, with approximately 5% of patients requiring supplemental general anesthesia. It is believed that incomplete block is the result of poor diffusion (due to the size of the sciatic nerve), separate fascial coverings of the tibial and peroneal nerves, or blockade of only a single component of the sciatic nerve. This has lead some practitioners to endorse the practice of dual stimulation to improve success rate.85
FIGURE 4.
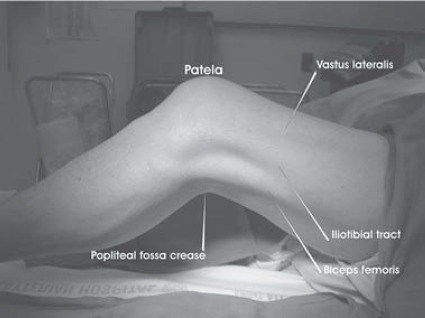
Popliteal Sciatic Block Through the Lateral Approach: Surface landmarks.
(Reproduced with Permission from: HadZidA., Vhka J. Peripheral Nerve Blocks: Principles and Practice. McGrawHill, New York, NY, 2003.).
CONTINUOUS SCIATIC NERVE BLOCKS
Continuous PNBs can theoretically be achieved at any place along the course of the sciatic nerve. Continuous SNBs have been used for analgesia following major foot and ankle reconstruction, ankle fracture fixation, and below the knee amputation.52,77,81,87,88 Three studies have been published on the use of continuous popliteal blocks for analgesia after extensive foot and ankle surgery.76,77,79 All three studies reported excellent analgesia with few side effects. Compared to intravenous analgesia or placebo infusion, a continuous infusion of local anesthetic via a popliteal catheter reduces pain scores, opioid consumption, and sleep disturbances.76,77 Successful catheter placement has been reported with both the lateral and posterior approach. The only consistent problem reported with popliteal catheters is a high incidence, 15-25%, of kinking or dislodgement.76,77 di Benedetto compared the subgluteal approach to the posterior popliteal approach for continuous infusions in a prospective study.87 In the 24-hour observation period following surgery 13,3% of the catheters in the popliteal group were either occluded or dislodged compared to 6,6% of the catheters in the subgluteal group. This difference did not reach statistical difference.
ANKLE AND FOOT BLOCK
The main indication for blockade of the lumbosacral plexus distally, at the ankle and midtarsal levels, is anesthesia for surgery to the foot.89,90 A diagnostic ankle block for sympathetically mediated ankle pain has also been described.91 The peripheral nerves blocked at the ankle are the terminal branches of both the sciatic (posterior tibial, superficial peroneal, deep peroneal, and sural) and femoral (saphenous) nerves. The five peripheral nerves that supply the foot are relatively easy to block at the ankle. There are no important variants in the innervation of the distal musculature. However, there is considerable variation in the branching and distribution of the sensory nerves of the foot. For this reason, blockade of all five nerves has been advocated.92 Neural blockade of the posterior tibial nerve has been described at the supramalleolar,92-94 midmalleolar89 subcalcaneal,95,96 and midtarsal97 levels with no evidence of superiority of one technique. The three superficial nerves are consistently blocked with simple field infiltration. Few studies evaluating perioperative outcomes with ankle block exist98 although the technique has been in clinical practice for decades. Rather, most publications describe variations to improve success rate. Peak blood levels of local anesthetic occur around 90 minutes after blockade and are very low even after bilateral ankle block.99
PHARMACOLOGIC CONSIDERATIONS
Complete unilateral lower extremity blockade involves multiple nerve blocks and a large volume of local anesthetics. Attention must be given to total local anesthetic dose; the concentration should be adjusted to accommodate the volume required for initial blockade as well as the ongoing local anesthetic administered as part of a continuous postoperative infusion. The concentration must also take into account the degree of sensory and/or motor block desired. Residual blockade may impede the ability of the patient to ambulate or actively participate in physical therapy. Thus, it is critical for the anesthesiologist to be aware of the postoperative rehabilitation program. Finally, the efficacy of adjuvants such as clonidine, opioids and ketorolac in improving the quality or duration of blockade has not been consistently demonstrated. Relatively few randomized studies have compared local anesthetics for lower extremity block. Casati evaluated the onset and duration of combined femoral-sciatic block performed with 0,5%, 0,75%, or 1% ropivacaine versus 2% mepivacaine.100 0,75% and 1% ropivacaine had an onset similar to that of mepivacaine, but with a duration of analgesia longer than mepivacaine. These results are similar to those involving upper extremity blocks, which suggest that 0.75% ropivacaine and 0,5% bupivacaine produce similar block quality and duration. In a single comparative study of SNB, levobupivacaine has block characteristics similar to ropivacaine. Although 0,5% ropivacaine took a longer time to onset than 2% mepi-vacaine, the duration of analgesia with 0,5% ropivacaine was much longer (mean of 12 hours versus 5 hours).
EPINEPHRINE
Epinephrine prolongs the duration and quality of most local anesthetics used for lower extremity peripheral nerve blocks. The effects are the result of vasoconstriction of the perineural vessels, which decreases uptake and increases the neural exposure time to the local anesthetic. The difference in effect is only somewhat dose-dependent. For example, the addition of epinephrine 5μg/mL (1:200,000 dilution) significantly increases the duration of lidocaine from 186 minutes to 264 minutes. Epinephrine 2μg/mL (1:400,000 dilution) prolongs the block to nearly the same extent (240 minutes) without any effect on nerve blood flow.101,102 The addition of epinephrine to local anesthetics with vasoconstrictive properties, such as ropivacaine, may not significantly increase block duration, but may facilitate detection of intravascular injection.103 The decision to add epinephrine and the dose of epinephrine added is based on the concerns related to cardiac or neural ischemia versus the ability to discern an intravascular injection. In general, since seizures related to intravascular injection are highest in patients undergoing PNB,104 the benefits of adding epinephrine may outweigh the risks. However, the nearly equivalent effects on block quality and duration reported with epinephrine 2μg/mL when compared to 5μg/mL, suggest that the lower concentration is sufficient. It is a personal bias of this author that epinephrine should not be used for sciatic blocks, in particularly the anterior SNB, due to the long duration of sciatic blockade and risks of nerve ischemia compounded by vasoconstriction, the possibility of arterial puncture, pressure on the anesthetized sciatic nerve, and application of the tourniquet over the upper thigh.
BICARBONATE
The addition of bicarbonate has been recommended to increase the speed of onset of peripheral and plexus blockade. However, most studies that have demonstrated a statistically significant difference utilized commercially prepared epinephrine-containing solutions of local anesthetics (which have a much lower pH due to the addition of antioxidants) compared to plain local anesthetic solutions. A recent review of the literature involving brachial plexus block concluded that there was little reason to add sodium bicarbonate with plain local anesthetics or those with freshly added epinephrine.105 These results were substantiated in a study by Candi-do,106 which reported no difference in the onset or duration of combined lumbar plexus-sciatic block in patients that received 0,5% bupivacaine with bicarbonate compared to those who received a non-alkalinized solution.
COMPLICATIONS OF LOWER EXTREMITY PERIPHERAL NERVE BLOCKS
Auroy prospectively evaluated serious complications following 21,278 PNBs in a 5-month period in France.104 Using a 95% confidence interval, the potential for serious complications was estimated per 10,000 PNBs to be 0 to 2,6 deaths, 0,3 to 4,1 cardiac arrests, 0,5 to 4,8 neurologic injuries, and 3,9 to 11,2 seizures. There is a paucity of reports of complications specifically associated with lower extremity PNBs as compared to upper extremity PNBs. This is most likely related to decreased use rather than inherent safety of the techniques. Complications can occur with lower extremity PNBs and it is up to the anesthesiologist performing the block to be aware of these complications and be vigilant in preventing them.
LOCAL ANESTHETIC SYSTEMIC TOXICITY
The potential for systemic local anesthetic toxicity would seem to be very high for lower extremity PNBs. Relatively large doses of local anesthetic are employed for combined femoral and sciatic nerve blocks to anesthetize the entire lower extremity, but there are only a few case reports of local anesthetic toxicity associated with lower extremity PNBs. For instance, Fanelli reported a series of 2175 patients undergoing femoral sciatic combined blocks in which there were no systemic adverse local anesthetic reactions reported (69). The apparent margin of safety seems to vary with individual block techniques. For instance, there are no case reports of toxicity after popliteal sciatic blockade, whereas there are several case reports of severe toxicity following lumbar plexus and sciatic nerve blocks.107-110 Differences in anatomy, primarily in the vasculature and presence of deep muscle beds in the area blocked, are the most likely explanation for this discrepancy. Interestingly, severe toxic reactions typically occur during or immediately after the injection. This suggests that the mechanism of these events is most commonly an unintentional intravascular injection of local anesthetic into the circulation, rather than absorption.12,111-115 A forceful, rapid injection of local anesthetic carries a much higher risk of local anesthetic toxicity than a slow, gentle injection.116 This is because the mean dose of local anesthetic that elicits the signs of CNS toxicity is much less during rapid intravascular injection as compared to that associated with slower absorption after appropriate deposition of the local anesthetic. After a lower extremity PNB, local anesthetic levels peak at approximately 60 minutes following injection. Perhaps this slow time-to-peak level in the bloodstream offers an explanation for the low incidence of toxic complications associated with absorption of local anesthetics after PNB. Important measures to decrease the risk of severe toxicity include the use of epinephrine as an intravascular marker, slow and methodical injection while avoiding high-injection pressures, frequent aspiration and constant assessment of the patient and vital signs, and prudent selection of local anesthetic concentration and volume.
PROXIMAL SPREAD (NEURAXIAL BLOCK)
Another potential needle misadventure is intrafascicu-lar spread of the local anesthetic proximally toward the spinal cord, resulting in central neuraxial blockade (10,117). This is of particular concern with block techniques that involve needle placement at the level of the nerve roots or spinal nerves, such as paravertebral and PCBs. Forceful, fast injections under high pressures into dural cuffs or perineurium can result in unintentional spinal or epidural anesthesia (15,118,119). In a large series of severe complications associated with regional anesthesia, Auroy found that the posterior approach to the lumbar plexus has the highest incidence of complications of the lower extremity PNBs (120). Of the 394 posterior lumbar plexus blocks reported, there were 5 serious complications reported. Three of these complications, 1 cardiac arrest and 2 respiratory arrests, were directly attributed to cephalad diffusion of the local anesthetic to the epidural or intrathecal space. Managing this block with the same degree of vigilance as for a neuraxial block is essential to detect and treat these complications early if they should occur.
HEMORRHAGIC COMPLICATIONS
Several approaches for PNBs of the lower extremity involve deep needle insertion, including the PCB, the obturator nerve block, and the parasacral and classical approaches to the sciatic nerve. Despite the proximity to vascular and hollow viscous structures of these deep nerves, there are relatively few reports of needle misadventures in published reports. Retroperitoneal hematoma formation following PCB has been re-ported(9). In order to reach the lumbar plexus, the needle must transverse multiple muscle and other tissue layers. The combination of deep location and inability to apply direct pressure after an inadvertent puncture of deep blood vessels makes this block less suitable in the setting of anticoagulation as compared to other, more superficial lower extremity PNBs.
INFECTIOUS COMPLICATIONS
There are no case reports of infection following single injection, lower extremity PNBs. However, Cuvillon reported incidences of bacterial complications associated with the use of continuous FNBs.121 In a cohort of 208 patients, 57% had positive bacterial colonization of the catheter at 48 hours postoperatively. Three patients had transitory symptoms of bacteremia that resolved after removal of the catheter. There were no long-term sequelae related to these positive catheter cultures. Two case reports of psoas abscess requiring drainage and intravenous antibiotic therapy has been reported in patients who received a continuous FNB. This stresses the importance of keeping a sterile field when performing a continuous catheter placement.
NEUROLOGIC COMPLICATIONS
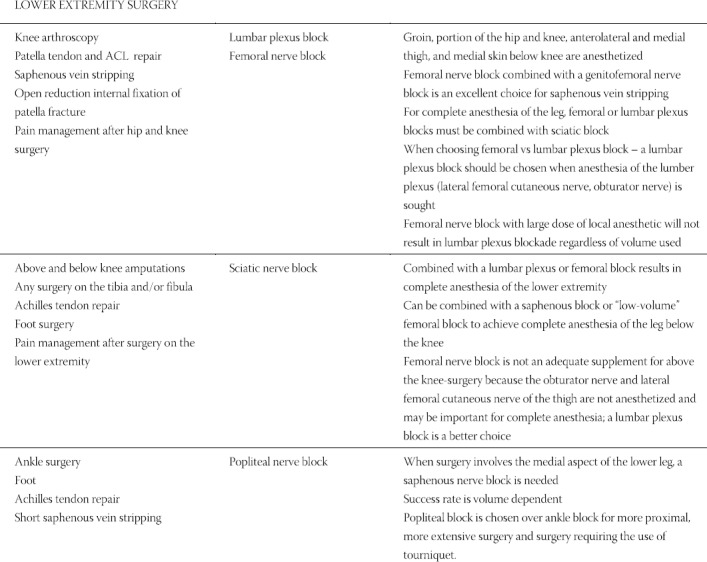
Neurologic injury is an infrequent but often-feared comall nerve block procedures.69,104,120 Most reports of neurologic complications after PNBs are related to upper extremity nerve blocks, a fact that more likely reflects the higher use of upper extremity blocks rather than an unique sensitivity to nerve injury in the upper extremity. The symptoms of nerve injury after PNB usually manifest shortly after block resolution. The perception and presentation of symptoms are typically influenced by the origin of the nerve lesion and other confounding factors, such as postoperative pain, immobility, effects of surgery, operative position, and the application of casts, dressings, and bandages. Intensity and duration of symptoms also vary with the severity of the injury, from light, intermittent tingling and numbness lasting a few weeks, to persistent and painful paresthe-sias, neuropathic pain, and sensory and/or motor deficits that can last for several months or years.122,123 Some nerve injuries result in a permanent neurologic deficit or evolve into severe reflex sympathetic dystrophies.124 Unfortunately, current understanding of the factors that lead to neurologic complications after PNBs is limited. This is partly the result of our inability to conduct meaningful retrospective studies owing to a lack of standard and objective documentation procedures for PNBs. In the absence of objective data, published discussions of the factors that lead to nerve injury, as well as medico-legal reviews, are often speculative at best. Intraneural injection is a well-known mechanism of neurologic injury associated with PNBs.125-138 However, in current clinical practice, there is no consensus on the techniques or methods that can reduce the risk of intraneural injection. Much of the debate has focused on methods of nerve localization (i.e., paresthesia versus nerve stimulation). However, there is still no evidence that one method is safer than the other, and neurologic injury can occur even with experienced practitioners using either technique.139 Recent reports have also suggested that nerve-stimulator assisted nerve localization may not eliminate the risk of intraneural needle placement. These reports document that par-esthesia (presumably caused by needle-nerve contact or intraneural placement of the needle) may be present without a motor response to nerve stimulation even with current intensity as high as 1,5 mA.140,141 In addition, there are currently no manufacturing standards for nerve stimulators, and older models may be inaccurate.142 Use of short-bevel needles and a nerve stimulator is generally believed to result in a lower risk of nerve trauma.143 Still, the advantages of short-bevel over sharper, long-bevel needles remain controversial.144 Educational material in regional anesthesia suggests that lancinating pain and high injection pressure may portend intraneural injection of local anesthetic, thus increasing the potential for nerve injury.145-148 However, a number of case reports suggest that pain is not a reliable warning sign of impending nerve injury.146,149-151 Because greater force required to perform an injection may be associated with intraneural injection, anesthesiologists often rely on a subjective evaluation of injection pressure during PNB to detect abnormal resistance to injection and prevent intraneural injection.108,116,117,152,153 Indeed, an earlier study performed in rabbits suggested that a intraneural injections result in higher injection pressures than perineural (“normal”) injections.149 More recently, studies in large animal models documented that high injection pressures (>20 psi) with intraneural needle placement lead to nerve injury.154 Unfortunately, clinical perception of an abnormally high resistance and pressure required to inject is impossible to verify because clinicians vary widely in what they perceive as appropriate force and rate of injection during PNB.153 Since current clinical practice does not allow for meaningful assessment, monitoring, and documentation of the injection technique, objective monitoring of injection pressures may prove beneficial to avoid pressures known to be capable of injuring the nerve fascicles.153 Neuronal ischemia can occur from a variety of sources including disruption of the neuronal microvasculature, high endoneurial pressures, addition of vasoconstrict-ing agents, and exogenous compression from tour-niquets,155 although a combination of these events is most likely required for development of nerve injury. The perineurium is a tough and resistant tissue layer. An injection into this compartment or into a fascicle can cause a prolonged increase in endoneurial pressure, exceeding the capillary perfusion pressure, which can result in endoneural ischemia.150 Addition of vaso-constricting agents theoretically can enhance ischemia because of the resultant reduction in blood flow. Addition of epinephrine has been shown in vitro to decrease blood supply to intact nerves, however this has not been shown to be a risk factor for development of post block nerve dysfunction in patients having lower extremity PNBs.69,149 An additional source of ischemia may be the application of a tourniquet, particularly over the site of a nerve block. Post-tourniquet palsy (“tourniquet paralysis”) has been reported to occur in 1 in 8,000 operations.155 However, the paucity of reported severe complications, despite the widespread use of tourniquets, suggests that peripheral nerves are relatively resistant to ischemia of limited duration and magnitude.156 The potential for neurotoxicity with a local anesthetic is a function of its potency, concentration, and the length of exposure of the neuronal tissue to the agent. Local anesthetics are used in concentrations that, under normal clinical conditions, do not cause irreversible nerve damage. Under normal circumstances, the concentration of local anesthetic at the injection site decreases quickly because of dilution by interstitial fluids and absorption in the blood. For this reason, local anesthetic solutions used in vivo are of a higher concentration than what is needed for nerve block in vitro. Nonetheless, exposure of the endoneurium (as may occur during intraneuronal injection) to a very high concentration of local anesthetic, particularly when coupled with intraneural pressure and ischemia, may contribute to the increased vulnerability of the nerve to neurologic injury.114,157 While neurologic complications of PNBs are uncommon, they can and do occur even in the hands of experienced practitio-ners139 and may result in significant patient suffering, distress to the practitioner, and medico-legal consequences. In summary, recent developments in the field of regional anesthesia have lead to an increased interest in lower extremity PNBs. These include reports of transient neurologic symptoms associated with spinal anesthesia, increased risk of epidural hematoma with the introduction of new anti-thromboembolic prophylaxis regimens, and evidence of improved rehabilitation outcome with continuous lower extremity PNBs. Research and focus on functional regional anesthesia anatomy have significantly contributed to the ease and success rate of lower extremity nerve blocks. More widespread acceptance of nerve blocks in clinical practice will depend on our ability to complete the transformation of this subspe-cialty field of anesthesiology to a more objective, standardized and reproducible practice with more clearly defined indications (Table 1) both to improve their clinical utility and to reduce the risk of complications.
TABLE 1.
Choice of peripheral nerve block technique for common surgical procedures of the lower extremity Reproduced with Permission from: New York School of Regional Anesthesia (NYSORA), http://www.nysora.com. (December 29,2004).
REFERENCES
- 1.Ho A, Karmakar M. Combinedparavertebral lumbar plexus and parasacral sciatic nerve block for reduction of hip fracture in a patient with severe aortic stenosis. Can J Anaesth. 2002;49:946–950. doi: 10.1007/BF03016880. [DOI] [PubMed] [Google Scholar]
- 2.Goroszeniuk T, di Vadi P. Repeatedpsoas compartment blocks for the management of long-standing hip pain. Reg Anesth Pain Med. 2001;26:376–378. doi: 10.1053/rapm.2001.25068. [DOI] [PubMed] [Google Scholar]
- 3.Chudinov A, Berkenstadt H, Salai M, et al. Continuous psoas compartment block for anesthesia and perioperative analgesia in patients with hip fractures. Reg Anesth Pain Med. 1999;24:563568. doi: 10.1016/s1098-7339(99)90050-0. [DOI] [PubMed] [Google Scholar]
- 4.Turker G, Uckunkaya N, Yavascaoglu B, et al. Comparison of the catheter-technique psoas compartment block and the epidural block for analgesia in partial hip replacement surgery. Acta An-aesthesiol Scand. 2003;47:30–36. doi: 10.1034/j.1399-6576.2003.470106.x. [DOI] [PubMed] [Google Scholar]
- 5.Luber M, Greengrass R, Vail T. Patientsatisfaction and effectiveness of lumbar plexus and sciatic nerve block for total knee arthroplasty. J Arthroplasty. 2001;16:17–21. doi: 10.1054/arth.2001.16488. [DOI] [PubMed] [Google Scholar]
- 6.Bridenbaugh P, Wedel D. In: Thelower extremity Somatic blockade, Neural blockade in clinical anesthesia and management of pain. 3 Edition. Cousins M, Bridenbaugh P, editors. Philadelphia: Lippincott; 1998. pp. 374–376. [Google Scholar]
- 7.Solanski D. In: Posterior lumbar plexus (psoas) block, Peripheral nerve blocks A color atlas. 1 Edition. JE C, editor. Philadelphia: Lippincott; 1999. pp. 90–92. [Google Scholar]
- 8.Capdevila X, Macaire P, Dadure C, et al. Continuous psoas compartment block for postoperative analgesia after total hip arthroplasty:new landmarks, technical guidelines and clinical evaluation. Anesth Analg. 2002;94:1606–1613. doi: 10.1097/00000539-200206000-00045. [DOI] [PubMed] [Google Scholar]
- 9.Aida S, Takahashi H, Shimoji K. Renalsubcapsular hematoma after lumbar plexus block. Anesthesiology. 1996;84:452–455. doi: 10.1097/00000542-199602000-00027. [DOI] [PubMed] [Google Scholar]
- 10.Pousman R, Mansoor Z, Sciard D. Totalspinal anesthetic after continuous posterior lumbar plexus block. Anesthesiology. 2003;98:1281–1282. doi: 10.1097/00000542-200305000-00034. [DOI] [PubMed] [Google Scholar]
- 11.Reddy M. Pneumocoele following psoas compartment block. Anaesthesia. 2002;57:938–939. doi: 10.1046/j.1365-2044.2002.279316.x. [DOI] [PubMed] [Google Scholar]
- 12.Farny J, Girard M, Drolet P. Posteriorapproach to the lumbar plexus combined with a sciatic nerve block using lidocaine. Can J Anaesth. 1994;41:486–491. doi: 10.1007/BF03011542. [DOI] [PubMed] [Google Scholar]
- 13.Parkinson S, Mueller J, Little W, et al. Extent of blockade with various approaches to the lumbar plexus. Anesth Analg. 1989;68:243–8. [PubMed] [Google Scholar]
- 14.Dalens B, Tanguy A, Vanneuville G. Lumbar plexus block in children:a comparison of two procedures in 50 patients. Anesth Analg. 1988;67:750–758. [PubMed] [Google Scholar]
- 15.Muravchick S, Owens W. Anunusual complication of lumbar plexus block a case report. Anesth Analg. 1976;55:350–352. doi: 10.1213/00000539-197605000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Chelly J, Greger J, Gebhard R, et al. Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplasty. 2001;16:436–445. doi: 10.1054/arth.2001.23622. [DOI] [PubMed] [Google Scholar]
- 17.Singelyn F, Gouverneur J. Extended “three-in-one” block after total knee arthroplasty:continuous versus patient-controlled techniques. Anesth Analg. 2000;91:176–180. doi: 10.1097/00000539-200007000-00033. [DOI] [PubMed] [Google Scholar]
- 18.Singelyn F, Vanderelst P, Gouverneur J. Extendedfemoral nerve sheath block after total hip arthroplasty continuous versus patient-controlled techniques. Anesth Analg. 2001;92:455–459. doi: 10.1097/00000539-200102000-00033. [DOI] [PubMed] [Google Scholar]
- 19.Matheny J, Hanks G, Rung G, et al. A comparison of patient-controlled analgesia and continuous lumbar plexus block after anterior cruciate ligament reconstruction. Arthroscopy. 1993;9:87–90. doi: 10.1016/s0749-8063(05)80350-0. [DOI] [PubMed] [Google Scholar]
- 20.Pandin P, Vandesteene A, d'Hollander A. Lumbarplexus posterior approach a catheter placement description using electrical nerve stimulation. Anesth Analg. 2002;95:1428–1431. doi: 10.1097/00000539-200211000-00060. [DOI] [PubMed] [Google Scholar]
- 21.Goranson B, Lang S, Cassidy J, et al. A comparison of three regional anaesthesia techniques for outpatient knee arthroscopy. Can J Anaesth. 1997;44:371–376. doi: 10.1007/BF03014456. [DOI] [PubMed] [Google Scholar]
- 22.Lopez S, Gros T, Bernard N, et al. Fascia iliaca compartment block for femoral bone fractures in prehospital care. Reg Anesth Pain Med. 2003;28:203–207. doi: 10.1053/rapm.2003.50134. [DOI] [PubMed] [Google Scholar]
- 23.Fletcher A, Rigby A, Heyes F. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department a randomized, controlled trial. Ann Emerg Med. 2003;41:227–233. doi: 10.1067/mem.2003.51. [DOI] [PubMed] [Google Scholar]
- 24.Mulroy M, Larkin K, Batra M, et al. Femoral nerve block with 0.25% or 0.5% bupivacaine improves postoperative analgesia following outpatient arthroscopic anterior cruciate ligament repair. Reg Anesth Pain Med. 2001;26:24–29. doi: 10.1053/rapm.2001.20773. [DOI] [PubMed] [Google Scholar]
- 25.McCarty E, Spindler K, Tingstad E, et al. Does intraarticular morphine improve pain control with femoral nerve block after anterior cruciate ligament reconstruction? Am J Sports Med. 2001;29:327–332. doi: 10.1177/03635465010290031301. [DOI] [PubMed] [Google Scholar]
- 26.Wang H, Boctor B, Verner J. Theeffect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med. 2002;27:139–144. doi: 10.1053/rapm.2002.29253. [DOI] [PubMed] [Google Scholar]
- 27.Frost S, Grossfeld S, Kirkley A, et al. The efficacy of femoral nerve block in pain reduction for outpatient hamstring anterior cruciate ligament reconstruction:a double-blind, prospective, randomized trial. Arthroscopy. 2000;16:243–248. doi: 10.1016/s0749-8063(00)90047-1. [DOI] [PubMed] [Google Scholar]
- 28.Vloka J, Hadžić A, Drobnik L, et al. Anatomic landmarks for femoral nerve block:a comparison of four needle insertion sites. Anesth Analg. 1999;89:1467–1470. doi: 10.1097/00000539-199912000-00028. [DOI] [PubMed] [Google Scholar]
- 29.Winnie A, Ramamurthy S, Durrani Z. Theinguinal paravascular technic of lumbar plexus anesthesia the “3-in-1 block”. Anesth Analg. 1973;52:989–996. [PubMed] [Google Scholar]
- 30.Cauhepe C, Oliver M, Colombani R, Railhac N. The“3-in-1” block myth or reality. Ann Fr Anesth Reanim. 1989;8:376–378. doi: 10.1016/s0750-7658(89)80084-x. [DOI] [PubMed] [Google Scholar]
- 31.Marhofer P, Nasel C, Sitzwohl C, Kapral S. Magneticresonance imaging of the distribution of local anesthetic during the three-in-one block. Anesth Analg. 2000;90:119–124. doi: 10.1097/00000539-200001000-00027. [DOI] [PubMed] [Google Scholar]
- 32.Lang S, Yip R, Chang P, Gerard M. Thefemoral 3-in-1 block revisited. J Clin Anesth. 1993;5:292–296. doi: 10.1016/0952-8180(93)90121-t. [DOI] [PubMed] [Google Scholar]
- 33.Capdevila X, Barthelet Y, Biboulet P, et al. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91:8–15. doi: 10.1097/00000542-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Singelyn F, Deyaert M, Joris D, et al. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthro-plasty. Anesth Analg. 1998;87:88–92. doi: 10.1097/00000539-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 35.Griffith J, Whiteley S, Gough M. Prospectiverandomized study of a new method of providing postoperative pain relief following femoropopliteal bypass. Br J Surg. 1996;83:1735–1738. doi: 10.1002/bjs.1800831223. [DOI] [PubMed] [Google Scholar]
- 36.Dauri M, Polzoni M, Fabbi E, et al. Comparison of epidural, continuous femoral block and intraarticular analgesia after anterior cruciate ligament reconstruction. Acta Anaesthesiol Scand. 2003;47:20–25. doi: 10.1034/j.1399-6576.2003.470104.x. [DOI] [PubMed] [Google Scholar]
- 37.Capdevila X, Biboulet P, Morau D, et al. Continuous three-in-one block for postoperative pain after lower limb orthopedic surgery:where do the catheters go? Anesth Analg. 2002;94:1001–6. doi: 10.1097/00000539-200204000-00042. [DOI] [PubMed] [Google Scholar]
- 38.Hopkins P, Ellis F, Halsall P. Evaluation of local anaesthetic blockade of the lateral femoral cutaneous nerve. Anaesthesia. 1991;46:95–96. doi: 10.1111/j.1365-2044.1991.tb09347.x. [DOI] [PubMed] [Google Scholar]
- 39.Karacalar A, Karacalar S, Uckunkaya N, et al. Combined use of axillary block and lateral femoral cutaneous nerve block in upper-extremity injuries requiring large skin grafts. J Hand Surg Am. 1998;23:1100–1105. doi: 10.1016/S0363-5023(98)80023-3. [DOI] [PubMed] [Google Scholar]
- 40.Maccani R, Wedel D, Melton A, Gronert G. Femoraland lateral femoral cutaneous nerve block for muscle biopsies in children. Paediatr Anaesth. 1995;5:223–227. doi: 10.1111/j.1460-9592.1995.tb00287.x. [DOI] [PubMed] [Google Scholar]
- 41.Jones S, White A. Analgesiafollowing femoral neck surgery. Lateral cutaneous nerve block as an alternative to narcotics in the elderly. Anaesthesia. 1985;40:682–685. doi: 10.1111/j.1365-2044.1985.tb10952.x. [DOI] [PubMed] [Google Scholar]
- 42.Coad N. Post-operative analgesia following femoral-neck surgery-a comparison between 3 in 1 femoral nerve block and lateral cutaneous nerve block. Eur J Anaesthesio. 1991;l(8):287–290. [PubMed] [Google Scholar]
- 43.Shannon J, Lang S, Yip R, Gerard M. Lateralfemoral cutaneous nerve block revisited. A nerve stimulator technique. Reg Anesth Pain Med. 1995;20:100–104. [PubMed] [Google Scholar]
- 44.Sharrock N. Inadvertent“3-in-1 block” following injection of the lateral cutaneous nerve of the thigh. Anesth Analg. 1980;59:887–888. [PubMed] [Google Scholar]
- 45.van der Wal M, Lang S, Yip R. Transsartorialapproach for sa-phenous nerve block. Can J Anaesth. 1993;40:542–6. doi: 10.1007/BF03009739. [DOI] [PubMed] [Google Scholar]
- 46.De Mey J, Deruyck L, Cammu G, et al. A paravenous approach for the saphenous nerve block. Reg Anesth Pain Med. 2001;26:504–506. doi: 10.1053/rapm.2001.25925. [DOI] [PubMed] [Google Scholar]
- 47.Comfort V, Lang S, Yip R. Saphenousnerve anaesthesia--a nerve stimulator technique. Can J Anaesth. 1996;43:852–857. doi: 10.1007/BF03013038. [DOI] [PubMed] [Google Scholar]
- 48.Bouaziz H, Benhamou D, Narchi P. A. new approach for saphe-nous nerve block. Reg Anesth Pain Med. 1996;21:490. [PubMed] [Google Scholar]
- 49.Tokat O, Turker Y, Uckunkaya N, Yilmazlar A. A clinical comparison of psoas compartment and inguinal paravascular blocks combined with sciatic nerve block. J Int Med Res. 2002;30:161–167. doi: 10.1177/147323000203000208. [DOI] [PubMed] [Google Scholar]
- 50.Mansour N. Sub-sartorial saphenous nerve block with the aid of nerve stimulator. Reg Anesth Pain Med. 1993;18:266–268. [PubMed] [Google Scholar]
- 51.Morris G, Lang S, Dust W, Van der Wal M. Theparasacral sciatic nerve block. Reg Anesth Pain Med. 1997;22:223–228. doi: 10.1016/s1098-7339(06)80005-2. [DOI] [PubMed] [Google Scholar]
- 52.Morris G, Lang S. Continuousparasacral sciatic nerve block two case reports. Reg Anesth Pain Med. 1997;22:469–472. doi: 10.1016/s1098-7339(97)80036-3. [DOI] [PubMed] [Google Scholar]
- 53.Gaertner E, Lascurian P, Venet C, et al. Continuous parasacral sciatic block:a radiographic study. Anesth Analg. 2004;98:831834. doi: 10.1213/01.ane.0000099368.62200.01. [DOI] [PubMed] [Google Scholar]
- 54.Winnie A. RegionalAnesthesia. Surg Clin North Am. 1975;55:861–892. doi: 10.1016/s0039-6109(16)40687-0. [DOI] [PubMed] [Google Scholar]
- 55.Raj P, Parks R, Watson T, Jenkins M. A. New single-position supine approach to sciatic-femoral nerve block. Anesth Analg. 1975;54:489–493. doi: 10.1213/00000539-197507000-00020. [DOI] [PubMed] [Google Scholar]
- 56.McNichol L. Sciaticnerve block for children. Sciatic nerve block by anterior approach for postoperative pain relief. Anaesthesia. 1985;40:410–414. [PubMed] [Google Scholar]
- 57.Guardini R, Waldron B, Wallace W. Sciaticnerve block. A new lateral approach. Acta Anaesthesiol Scand. 1985;29:515–519. doi: 10.1111/j.1399-6576.1985.tb02245.x. [DOI] [PubMed] [Google Scholar]
- 58.Franco C. Posteriorapproach to the sciatic nerve in adults:is euclidean geometry still necessary? Anesthesiology. 2003;98:723728. doi: 10.1097/00000542-200303000-00022. [DOI] [PubMed] [Google Scholar]
- 59.Beck G. Anteriorapproach to sciatic nerve block. Anesthesiol-ogy. 1963;24:222–4. doi: 10.1097/00000542-196303000-00011. [DOI] [PubMed] [Google Scholar]
- 60.Magora F, Rozin R, Ben-Menachem Y, Magora A. Obturatornerve block an evaluation of technique. Br J Anaesth. 1969;41:695–698. doi: 10.1093/bja/41.8.695. [DOI] [PubMed] [Google Scholar]
- 61.Chelly J, Delaunay L. A new anterior approach to the sciatic nerve block. Anesthesiology. 1999;91:1655–1660. doi: 10.1097/00000542-199912000-00017. [DOI] [PubMed] [Google Scholar]
- 62.Hadžić A, Vloka J. In: Sciatic nerve block anterior approach, Peripheral nerve blocks:principles and practice. 1 Edition. Hadžić A, Vloka J, editors. New York: McGraw-Hill; 2003. pp. 252–265. [Google Scholar]
- 63.Vloka J, Hadžić A, April E, Thys D. Anteriorapproach to the sciatic nerve block the effects of leg rotation. Anesth Analg. 2001;92:460–462. doi: 10.1097/00000539-200102000-00034. [DOI] [PubMed] [Google Scholar]
- 64.Moore C, Sheppard D, Wildsmith J. Thighrotation and the anterior approach to the sciatic nerve a magnetic resonance imaging study. Reg Anesth Pain Med. 2004;29:32–35. doi: 10.1016/j.rapm.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 65.Ericksen M, Swenson J, Pace N. Theanatomic relationship of the sciatic nerve to the lesser trochanter implications for anterior sciatic nerve block. Anesth Analg. 2002;95:1071–1074. doi: 10.1097/00000539-200210000-00052. [DOI] [PubMed] [Google Scholar]
- 66.Dalens B, Tanguy A, Vanneuville G. Sciaticnerve blocks in children comparison of the posterior, anterior, and lateral approaches in 180 pediatric patients. Anesth Analg. 1990;70:131–137. doi: 10.1213/00000539-199002000-00001. [DOI] [PubMed] [Google Scholar]
- 67.Pandin P, Vandesteene A, D'Hollander A. Sciaticnerve blockade in the supine position a novel approach. Can J Anaesth. 2003;50:52–56. doi: 10.1007/BF03020187. [DOI] [PubMed] [Google Scholar]
- 68.di Benedetto P, Casati A, Bertini L, Fanelli G. Posteriorsubglu-teal approach to block the sciatic nerve description of the technique and initial clinical experiences. Eur J Anaesthesiol. 2002;19:682–686. doi: 10.1017/s0265021502001126. [DOI] [PubMed] [Google Scholar]
- 69.Fanelli G, Casati A, Garancini P, Torri G. Nervestimulator and multiple injection technique for upper and lower limb blockade failure rate, patient acceptance, and neurologic complications. Anesth Analg. 1999;88:847–852. doi: 10.1097/00000539-199904000-00031. [DOI] [PubMed] [Google Scholar]
- 70.Rorie D, Byer D, Nelson D, et al. Assessment of block of the sciatic nerve in the popliteal fossa. Anesth Analg. 1980;59:371–376. [PubMed] [Google Scholar]
- 71.Hansen E, Eshelman M, Cracchiolo A. Poplitealfossa neural blockade as the sole anesthetic technique for outpatient foot and ankle surgery. Foot Ankle Int. 2000;21:38–44. doi: 10.1177/107110070002100107. [DOI] [PubMed] [Google Scholar]
- 72.Rongstad K, Mann R, Prieskorn D, et al. Popliteal sciatic nerve block for postoperative analgesia. Foot Ankle Int. 1996;17:378–382. doi: 10.1177/107110079601700704. [DOI] [PubMed] [Google Scholar]
- 73.Vloka J, Hadžić A, Mulcare R, et al. Combined popliteal and posterior cutaneous nerve of the thigh blocks for short saphe-nous vein stripping in outpatients:an alternative to spinal anesthesia. J Clin Anesth. 1997;9:618–622. doi: 10.1016/s0952-8180(97)00150-5. [DOI] [PubMed] [Google Scholar]
- 74.Tobias J, Mencio G. Poplitealfossa block for postoperative analgesia after foot surgery in infants and children. J Pediatr Orthop. 1999;19:511–514. doi: 10.1097/00004694-199907000-00017. [DOI] [PubMed] [Google Scholar]
- 75.Vloka J, Hadžić A, Koorn R, Thys D. Supineapproach to the sciatic nerve in the popliteal fossa. Can J Anaesth. 1996;43:964967. doi: 10.1007/BF03011812. [DOI] [PubMed] [Google Scholar]
- 76.Singelyn F, Aye F, Gouverneur J. Continuous popliteal sciatic nerve block:an original technique to provide postoperative analgesia after foot surgery. Anesth Analg. 1997;84:383–386. doi: 10.1097/00000539-199702000-00027. [DOI] [PubMed] [Google Scholar]
- 77.Ilfeld B, Morey T, Wang R, Enneking F. Continuouspopliteal sciatic nerve block for postoperative pain control at home a randomized, double-blinded, placebo-controlled study. Anesthesi-ology. 2002;97:959–965. doi: 10.1097/00000542-200210000-00031. [DOI] [PubMed] [Google Scholar]
- 78.Schimek F, Deusch H. Newtechnique of sciatic nerve block in the popliteal fossa. Eur J Anaesthesiol. 1995;12:163–169. [PubMed] [Google Scholar]
- 79.Levecque J, Borne M, Saissy J. Analgesiawith continuous lateral posterior tibial nerve block. Reg Anesth Pain Med. 1999;24:191192. doi: 10.1016/s1098-7339(99)90095-0. [DOI] [PubMed] [Google Scholar]
- 80.Gouverneur J. Sciaticnerve block in the popliteal fossa with atraumatic needles and nerve stimulation. Acta Anaesthesiolog Belg. 1985;36:391–399. [PubMed] [Google Scholar]
- 81.Singelyn F, Gouverneur J, Gribomont B. Poplitealsciatic nerve block aided by a nerve stimulator a reliable technique for foot and ankle surgery. Reg Anesth Pain Med. 1991;16:278–281. [PubMed] [Google Scholar]
- 82.Hadžić A, Volka J, Singson R, et al. A comparison of interten-dinous and classical approaches to popliteal nerve block using magnetic resonance imaging simulation. Anesth Analg. 2002;94:1321–1324. doi: 10.1097/00000539-200205000-00051. [DOI] [PubMed] [Google Scholar]
- 83.Benzon H, Kim C, Benzon H, et al. Correlation between evoked motor response of the sciatic nerve and sensory blockade. Anes-thesiology. 1997;87:547–552. doi: 10.1097/00000542-199709000-00014. [DOI] [PubMed] [Google Scholar]
- 84.Paqueron X, Bouaziz H, Macalou D, et al. The lateral approach to the sciatic nerve at the popliteal fossa:one or two injections? Anesth Analg. 1999;89:1221–1225. [PubMed] [Google Scholar]
- 85.Zetlaoui P, Bouaziz H. Lateralapproach to the sciatic nerve in the popliteal fossa. Anesth Analg. 1998;87:79–82. doi: 10.1097/00000539-199807000-00017. [DOI] [PubMed] [Google Scholar]
- 86.Vloka J, Hadžić A, Kitain E, et al. Anatomic considerations for sciatic nerve block in the popliteal fossa through the lateral approach. Reg Anesth Pain Med. 1996;21:414–418. [PubMed] [Google Scholar]
- 87.di Benedetto P, Casati A, Bertini L, et al. Postoperative analgesia with continuous sciatic nerve block after foot surgery:a prospective, randomized comparison between the popliteal and sublglueal approaches. Anesth Analg. 2002;94:996–1000. doi: 10.1097/00000539-200204000-00041. [DOI] [PubMed] [Google Scholar]
- 88.Chelly J, Greger J, Casati A, et al. Continuous lateral sciatic blocks for acute postoperative pain management after major ankle and foot surgery. Foot Ankle Int. 2002;23:749–752. doi: 10.1177/107110070202300812. [DOI] [PubMed] [Google Scholar]
- 89.Schurman D. Ankle-block anesthesia for foot surgery. Anesthe-siology. 1976;44:348–352. [PubMed] [Google Scholar]
- 90.Pinzur M, Morrison C, Sage R, et al. Syme's two-stage amputation in insulin-requiring diabetics with gangrene of the forefoot. Foot Ankle Int. 1991;11:394–396. doi: 10.1177/107110079101100610. [DOI] [PubMed] [Google Scholar]
- 91.Harvey C. Dilute lidocaine ankle blocks in the diagnosis of sympathetically maintained pain. J Am Podiatr Med Assoc. 1997;87:473–477. doi: 10.7547/87507315-87-10-473. [DOI] [PubMed] [Google Scholar]
- 92.Delgado-Martinez A, Marchal-Escalona J. Supramalleolarankle block anesthesia and ankle tourniquet for foot surgery. Foot Ankle Int. 2001;22:836–838. doi: 10.1177/107110070102201011. [DOI] [PubMed] [Google Scholar]
- 93.Gerbert J. The location of the terminal branching of the posterior tibial nerve and its effect on administering a posterior tibial nerve block. J Am Podiatry Assoc. 1971;61:8–11. doi: 10.7547/87507315-61-1-8. [DOI] [PubMed] [Google Scholar]
- 94.Lichtenfeld N. The pneumatic ankle tourniquet with ankle block anesthesia for foot surgery. Foot Ankle Int. 1992;13:344–9. doi: 10.1177/107110079201300609. [DOI] [PubMed] [Google Scholar]
- 95.Colgrove R. Posterior tibial nerve block. Foot Ankle Int. 2001;22:839–840. doi: 10.1177/107110070102201012. [DOI] [PubMed] [Google Scholar]
- 96.Wassef M. Posterior tibial nerve block. A new approach using the bony landmark of the sustentaculum tali. Anaesthesia. 1991;46:841–844. doi: 10.1111/j.1365-2044.1991.tb09597.x. [DOI] [PubMed] [Google Scholar]
- 97.Sharrock N, Waller J, Fierro L. Midtarsalblock for surgery of the forefoot. Br J Anaesth. 1986;58:37–40. doi: 10.1093/bja/58.1.37. [DOI] [PubMed] [Google Scholar]
- 98.NeedoffM Radford P, Costigan P. Localanesthesia for postoperative pain relief after foot surgery a prospective clinical trial. Foot Ankle Int. 1995;16:11–13. doi: 10.1177/107110079501600103. [DOI] [PubMed] [Google Scholar]
- 99.Mineo R, Sharrock N. Venouslevels of lidocaine and bupivacaine after midtarsal ankle block. Reg Anesth Pain Med. 1992;17:47–49. [PubMed] [Google Scholar]
- 100.Casati A, Fanelli G, Borghi B, Torri G. Ropivacaineof 2% mepi-vacaine for lower limb peripheral nerve blocks. Anesthesiology. 1999;90:1047–1052. doi: 10.1097/00000542-199904000-00018. [DOI] [PubMed] [Google Scholar]
- 101.Kennedy W, Jr, Bonica J, Ward R, et al. Cardiorespiratory effects of epinephrine when used in regional anesthesia. Acta An-aesthesiol Scand Suppl. 1966;23:320–333. doi: 10.1111/j.1399-6576.1966.tb01030.x. [DOI] [PubMed] [Google Scholar]
- 102.DiFazio C, Rowlingson J. In: Additiveto local anesthetic solutions, Regional anesthesia and analgesia. 1 Edition. Brown D, editor. Philadelphia: WB Saunders; 1996. pp. 232–239. [Google Scholar]
- 103.Weber A, Fournier R, Van Gessel E, et al. Epinephrine does not prolong the analgesia of 20 mL ropivacaine 0.5% or 0.2% in a femoral three-in-one block. Anesth Analg. 2001;93:1327–1331. doi: 10.1097/00000539-200111000-00060. [DOI] [PubMed] [Google Scholar]
- 104.Auroy Y, Narchi P, Messiah A, et al. Serious complications related to regional anesthesia:results of a prospective survey in France. Anesthesiology. 1997;87:479–486. doi: 10.1097/00000542-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 105.Neal J, Hebl J, Gerancher J, Hogan Q. Brachialplexus anesthesia essentials of our current understanding. Reg Anesth Pain Med. 2002;27:402–428. doi: 10.1053/rapm.2002.34377. [DOI] [PubMed] [Google Scholar]
- 106.Candido K, Winnie A, Covino B, et al. Addition of bicarbonate to plain bupivacaine does not significantly alter the onset or duration of plexus anesthesia. Reg Anesth Pain Med. 1995;20:133–138. [PubMed] [Google Scholar]
- 107.Pham-Dang C, Beaumont S, Floch H, et al. Acute toxic accident following lumbar plexus block with bupivacaine. Ann Fr Anesth Reanim. 2000;19:356–359. [PubMed] [Google Scholar]
- 108.Breslin D, Martin G, Macleod D, et al. Central nervous system toxicity following the administration of levobupivacaine for lumbar plexus block:a report of two cases. Reg Anesth Pain Med. 2003;28:144–147. doi: 10.1053/rapm.2003.50127. [DOI] [PubMed] [Google Scholar]
- 109.Mullanu C, Gaillat F, Scemama F, et al. Acute toxicity of local anesthetic ropivacaine and mepivacaine during a combined lumbar plexus and sciatic block for hip surgery. Acta Anaesthe-siol Belg. 2002;53:221–223. [PubMed] [Google Scholar]
- 110.Petitjeans F, Mion G, Puidupin M, et al. Tachycardia and convulsions induced by accidental intravascular ropivacaine injection during sciatic block. Acta Anaesthesiol Scand. 2002;46:616617. doi: 10.1034/j.1399-6576.2002.460524.x. [DOI] [PubMed] [Google Scholar]
- 111.Odoom J, Zuurmond W, Sih I, et al. Plasma bupivacaine concentrations following psoas compartment block. Anaesthesia. 1986;41:155–158. doi: 10.1111/j.1365-2044.1986.tb13171.x. [DOI] [PubMed] [Google Scholar]
- 112.Elmas C, Atanassoff P. Combinedinguinal paravascular (3-in-1) and sciatic nerve blocks for lower limb surgery. Reg Anesth Pain Med. 1993;18:88–92. [PubMed] [Google Scholar]
- 113.Misra U, Pridie A, McClymont C, Bower S. Plasmaconcentrations of bupivacaine following combined sciatic and femoral 3 in 1 nerve blocks in open knee surgery. Br J Anaesth. 1991;66:310–313. doi: 10.1093/bja/66.3.310. [DOI] [PubMed] [Google Scholar]
- 114.Simon M, Gielen M, Lagerwerf A, Vree T. Plasmaconcentrations after high doses of mepivacaine with epinephrine in the combined psoas compartment/sciatic nerve block. Reg Anesth Pain Med. 1990;15:256–60. [PubMed] [Google Scholar]
- 115.Edkin B, Spindler K, Flanagan J. Femoralnerve block as an alternative to parenteral narcotics for pain control after anterior cruciate ligament reconstruction. Arthroscopy. 1995;11:404–409. doi: 10.1016/0749-8063(95)90191-4. [DOI] [PubMed] [Google Scholar]
- 116.Liu P, Feldman H, Giasi R, et al. Comparative CNS toxicity of lidocaine, etidocaine, bupivacaine, and tetracaine in awake dogs following rapid intravenous administration. Anesth Analg. 1983;62:375–379. [PubMed] [Google Scholar]
- 117.Selander D, Sjostrand J. Longitudinalspread of intraneurally injected local anesthetics. An experimental study of the initial distribution following intraneural injections. Acta Anaesthesiol Scand. 1978;22:622–634. doi: 10.1111/j.1399-6576.1978.tb01346.x. [DOI] [PubMed] [Google Scholar]
- 118.Singelyn F, Contreras V, Gouverneur J. Epiduralanesthesia complicating continuous 3-in-1 lumbar plexus blockade. Anes-thesiology. 1995;83:217–220. doi: 10.1097/00000542-199507000-00029. [DOI] [PubMed] [Google Scholar]
- 119.Gentili M, Aveline C, Bonnet F. Totalspinal anesthesia after posterior lumbar plexus block. Ann Fr Anesth Reanim. 1998;17:740–742. doi: 10.1016/s0750-7658(98)80112-3. [DOI] [PubMed] [Google Scholar]
- 120.Auroy Y, Benhamou D, Bargues L, et al. Major complications of regional anesthesia in France:the SOS regional anesthesia hotline service. Anesthesiology. 2002;97:1274–1280. doi: 10.1097/00000542-200211000-00034. [DOI] [PubMed] [Google Scholar]
- 121.Cuvillon P, Ripart J, Lalourcey L, et al. The continuous femoral nerve block catheter for postoperative analgesia:bacterial colonization, infectious rate and adverse effects. Anesth Analg. 2001;93:1045–1049. doi: 10.1097/00000539-200110000-00050. [DOI] [PubMed] [Google Scholar]
- 122.Lim E, Pereira R. Brachialplexus injury following brachial plexus block. Anaesthesia. 1984;39:691–694. doi: 10.1111/j.1365-2044.1984.tb06478.x. [DOI] [PubMed] [Google Scholar]
- 123.Bashein G, Robertson H, Kennedy W.J. Persistent phrenic nerve paresis following interscalene brachial plexus block. Anesthesiology. 1985;63:102–104. doi: 10.1097/00000542-198507000-00017. [DOI] [PubMed] [Google Scholar]
- 124.Gillespie J, Menk E, Middaugh R. Reflexsympathetic dystrophy a complication of interscalene block. Anesth Analg. 1987;66:1316–1317. [PubMed] [Google Scholar]
- 125.Fremling M, Mackinnon S. Injectioninjury to the median nerve. Ann Plast Surg. 1996;37:561–567. doi: 10.1097/00000637-199611000-00019. [DOI] [PubMed] [Google Scholar]
- 126.Curtiss P.J, Tucker H. Sciaticpalsy in premature infants a report and follow-up study of ten cases. JAMA. 1960;174:1586–1588. doi: 10.1001/jama.1960.03030120026005. [DOI] [PubMed] [Google Scholar]
- 127.Gilles F, French J. Postinjectionsciatic nerve palsies in infants and children. J Pediatr Orthop. 1961;58:195–204. doi: 10.1016/s0022-3476(61)80158-3. [DOI] [PubMed] [Google Scholar]
- 128.Ling C, Loong S. Injectioninjury of the radial nerve. Injury. 1976;8:60–62. doi: 10.1016/0020-1383(76)90012-7. [DOI] [PubMed] [Google Scholar]
- 129.Hudson A, Kline D, Gentili F. Management of peripheral nerve problems. 1 Edition. Philadelphia: Saunders; 1980. [Google Scholar]
- 130.Burkel W, McPhee M. Effectof phenol injection into peripheral nerve of rat electron microscope studies. Arch Phys Med Reha-bil. 1970;51:391–397. [PubMed] [Google Scholar]
- 131.Holbrook T, Pilsher C. Theeffects of injection of penicillin;peanut oil and beeswax, separately and in combination, upon nerve and muscle;an experimental study. Surg Gynecol Obstet. 1950;90:39–44. [PubMed] [Google Scholar]
- 132.Shapiro S, Norman D. Neurologicalcomplications following the use of efocaine;report of three cases. JAMA. 1953;152:608–609. doi: 10.1001/jama.1953.63690070004010c. [DOI] [PubMed] [Google Scholar]
- 133.Gentili F, Hudson A, Kline D, Hunter D. Peripheralnerve injection injury an experimental study. Neurosurgery. 1979;4:244–253. doi: 10.1227/00006123-197903000-00009. [DOI] [PubMed] [Google Scholar]
- 134.Gentili F, Hudson A, Hunter D, Kline D. Nerveinjury with local anesthetic agents a light and electron microscopic, fluorescent microscopic, and horseradish peroxidase study. Neurosur-gery. 1980;6:263–272. [PubMed] [Google Scholar]
- 135.Gentili F, Hudson A, Kline D, Hunter D. Earlychanges following injection injury of peripheral nerves. Can J Surg. 1980;23:177–182. [PubMed] [Google Scholar]
- 136.Allensworth M, Scheinberg L. Sciaticneuropathy in infants related to antibiotic injections. Pediatrics. 1957;19:261–265. [PubMed] [Google Scholar]
- 137.Selander D, Dhuner K, Lundborg G. Peripheralnerve injury due to injection needles used for regional anesthesia. An experimental study of the acute effects of needle point trauma. Acta Anaesthesiol Scand. 1977;21:182–188. doi: 10.1111/j.1399-6576.1977.tb01208.x. [DOI] [PubMed] [Google Scholar]
- 138.Selander D, Brattsand R, Lundborg G, et al. Local anesthetics. importance of mode of application, concentration and adrenaline for the appearance of nerve lesions. An experimental study of axonal degeneration and barrier damage after intrafascicular injection or topical application of bupivacaine (marcain) Acta Anaesthesiol Scand. 1979;23:127–136. doi: 10.1111/j.1399-6576.1979.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 139.Kent K, Moscucci M, Mansour K, et al. Retroperitoneal hematoma after cardiac catheterization:prevalence, risk factors, and optimal management. J Vasc Surg. 1994;20:905–910. doi: 10.1016/0741-5214(94)90227-5. [DOI] [PubMed] [Google Scholar]
- 140.Mulroy M, Mitchell B. Unsolicitedparesthesias with nerve stimulator case reports of four patients. Anesth Analg. 2002;95:762–763. doi: 10.1097/00000539-200209000-00043. [DOI] [PubMed] [Google Scholar]
- 141.Urmey W, Stanton J. Inabilityto consistently elicit a motor response following sensory paresthesia during interscalene block administration. Anesthesiology. 2002;96:552–554. doi: 10.1097/00000542-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 142.Hadžić A, Vloka J, Hadžić N, et al. Nerve stimulators used for peripheral nerve blocks vary in their electrical characteristics. Anesthesiology. 2003;98:969–974. doi: 10.1097/00000542-200304000-00026. [DOI] [PubMed] [Google Scholar]
- 143.Barber F, Click J, Britt B. Complicationsof ankle arthroscopy. Foot Ankle Int. 1990;10:263–266. doi: 10.1177/107110079001000504. [DOI] [PubMed] [Google Scholar]
- 144.Rice A, McMahon S. Peripheral nerve injury caused by injection needles used in regional anaesthesia:influence of bevel configuration, studied in a rat model. Br J Anaesth. 1992;69:433–438. doi: 10.1093/bja/69.5.433. [DOI] [PubMed] [Google Scholar]
- 145.Weaver M, Tandatnick C, Hahn M. In: Peripheral Nerve Blockade Textbook of Regional Anesthesia. 3 Edition. Raj P, editor. Philadelphia: Churchill Livingston; 2002. pp. 857–870. [Google Scholar]
- 146.Selander D. Peripheralnerve injury after regional anesthesia, Complications of Regional. In: Fi-nucane B, Ross A, editors. Anesthesia. 1 Edition. Churchill Livingstone: Philadelphia; 1999. pp. 105–115. [Google Scholar]
- 147.Jankovic D, Wells C. In: Brachialplexus, Regional nerve blocks textbook and color atlas. 2 Edition. Jankovic D, Wells C, editors. Berlin: Blackwell; 2000. pp. 76–77. [Google Scholar]
- 148.Adriani J. Labat's regional anesthesia techniques and clinical applications. 4 Edition. St. Louis: Warren H. Green; 1985. [Google Scholar]
- 149.Selander D, Mansson L, Karlsson L, Svanvik J. Adrenergicvasoconstriction in peripheral nerves of the rabbit. Anesthesiology. 1985;62:6–10. doi: 10.1097/00000542-198501000-00002. [DOI] [PubMed] [Google Scholar]
- 150.Myers R, Kalichman M, Reisner L, Powell C. Neurotoxicityof local anesthetics altered perineurial permeability, edema, and nerve fiber injury. Anesthesiology. 1986;64:29–35. [PubMed] [Google Scholar]
- 151.Bonner S, Pridie A. Sciaticnerve palsy following uneventful sciatic nerve block. Anaesthesia. 1997;52:1205–1207. doi: 10.1111/j.1365-2044.1997.258-az0396.x. [DOI] [PubMed] [Google Scholar]
- 152.Kent K, Moscucci M, Gallagher S, et al. Neuropathy after cardiac catheterization:incidence, clinical patterns, and long-term outcome. J Vasc Surg. 1994;19:1008–1013. doi: 10.1016/s0741-5214(94)70212-8. [DOI] [PubMed] [Google Scholar]
- 153.Claudio R, Hadžić A, Shih H, et al. Injection pressures by anesthesiologists during simulated peripheral nerve block. Reg Anesth Pain Med. 2004;29:201–205. doi: 10.1016/j.rapm.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 154.Hadžić A, Dilberović F, Shah S, et al. Combination of intraneural injection and high injection pressure leads to severe fascicular injury and neurologic deficits in dogs. Reg Anesth Pain Med. 2004;29:417–423. doi: 10.1016/j.rapm.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 155.Middleton R, Varian J. Tourniquet paralysis. Aust N Z J Surg. 1974;44:124–128. doi: 10.1111/j.1445-2197.1974.tb06402.x. [DOI] [PubMed] [Google Scholar]
- 156.Shrarock N, Savarese J. In: Anesthesia for Orthopedic Surgery, Anesthesia. 5 Edition. RD M, editor. Philadelphia: Churchill Livingston; 1998. pp. 2118–2139. [Google Scholar]
- 157.Selander D. In: Nerve toxicity of local anesthetics, Local anesthesia and regional blockade. Lofstrom J, Sjostrand U, editors. Amsterdam: Elsevier Science Publisher B. V; 1988. p. 77. [Google Scholar]


