Abstract
Purpose
For patients with time-critical acute coronary syndrome, reporting electrocardiogram (ECG) findings is the most important component of the treatment process. We aimed to develop and validate an automated Fast Healthcare Interoperability Resources (FHIR)-based 12-lead ECG mobile alert system for use in an emergency department (ED).
Materials and Methods
An automated FHIR-based 12-lead ECG alert system was developed in the ED of an academic tertiary care hospital. The system was aimed at generating an alert for patients with suspected acute coronary syndrome based on interpretation by the legacy device. The alert is transmitted to physicians both via a mobile application and the patient's electronic medical record (EMR). The automated FHIR-based 12-lead ECG alert system processing interval was defined as the time from ED arrival and 12-lead ECG capture to the time when the FHIR-based notification was transmitted.
Results
During the study period, 3812 emergency visits and 1581 12-lead ECGs were recorded. The FHIR system generated 155 alerts for 116 patients. The alerted patients were significantly older [mean (standard deviation): 68.1 (12.4) years vs. 59.6 (16.8) years, p<0.001], and the cardiac-related symptom rate was higher (34.5% vs. 19%, p<0.001). Among the 155 alerts, 146 (94%) were transmitted successfully within 5 minutes. The median interval from 12-lead ECG capture to FHIR notification was 2.7 min [interquartile range (IQR) 2.2–3.1 min] for the group with cardiac-related symptoms and 3.0 min (IQR 2.5–3.4 min) for the group with non-cardiac-related symptoms.
Conclusion
An automated FHIR-based 12-lead ECG mobile alert system was successfully implemented in an ED.
Keywords: Health information interoperability, electrocardiogram, ST elevation myocardial infarction, workflow, health information exchange
INTRODUCTION
Accurate and timely transfer of medical information plays an essential role in clinical settings.1 When carried out appropriately, information transfer can improve the effectiveness of care, reduce medical errors, and decrease medical costs.2,3 However, even with the use of up-to-date electronic medical record (EMR) systems, relevant information among providers is often difficult to distribute clinically.4,5,6
Health information exchange faces several obstacles.7,8,9 Although interoperability, privacy, and security are critical issues, the lack of standards is reportedly the most important issue.10,11,12 The Health Level 7 Fast Healthcare Interoperability Resources (FHIR) system is the new standard for exchanging electronic health records.10,13 The FHIR system is fast and easy to implement and is more suitable for mobile phone and tablet devices.14,15 These features hold more importance when applied to time-critical conditions in complex clinical settings, such as the emergency department (ED).
Acute coronary syndrome is one of the most targeted conditions in acute healthcare systems, owing to its time-dependent and multidisciplinary aspects. Although 12-lead electrocardiogram (ECG) has been emphasized as the most important component of the treatment process,16,17 delivering and sharing 12-lead ECG findings are still challenging under complex circumstances.18 An FHIR-based mobile alert system can deliver relevant information effectively and can improve clinical outcomes, just as often as with other automatic alert systems. Also, shortening process times can contribute to door-to-balloon time.
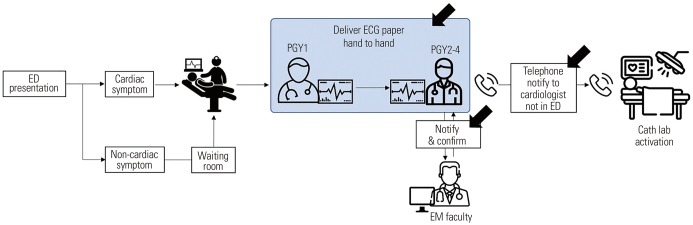
The usual process of obtaining a 12-lead ECG report in the ED is as follows: a postgraduate year 1 (PGY1) visits the patient with an ECG machine capable of printing a paper version of the 12-lead ECG on-site. The device also wirelessly transmits the ECG image to the EMR, which stores it in the PDF format. After printing, the printed ECG result is handed over to a supervising emergency medicine resident PGY2-4, who consults the on-call cardiologist for cardiac catheterization laboratory activation when a significant problem, such as ST-elevation myocardial infarction (STEMI), is observed. The overall process is illustrated in Fig. 1.
Fig. 1. The ED process of obtaining and sharing a 12-lead ECG information. The black arrow indicates factors that could delay information transmission. ED, emergency department; ECG, electrocardiogram; PGY, postgraduate year; EM, emergency medicine.
This study aimed to develop and validate an automated FHIR-based 12-lead ECG mobile alert system in an ED. The primary outcome was successful transmission of 12-lead ECG information via the FHIR system within 5 minutes.
MATERIALS AND METHODS
Study setting
This study was conducted in an ED of an academic tertiary care hospital in Seoul. The hospital has approximately 2000 inpatient beds and 2 million annual outpatient visits.19 The number of annual ED visits is approximately 80000. The number of 12-lead ECGs is approximately 2500/month in the ED. This was a single-center retrospective study conducted between November 14 and December 7, 2018. This study included patients aged >18 years who visited the ED and underwent a 12-lead ECG.
Database (DARWIN-C)
The Data Analytics and Research Window for Integrated kNowledge (DARWIN) project was initiated in 2011. The system was aimed at developing concepts for future generations of hospital information systems, such as data-driven and precision medicine. The system was rolled out in July 2016.
The clinical data warehouse system was initiated in January 2014 as part of the DARWIN project and named DARWIN-C. The Clinical Data Warehouse is a research database of clinical information obtained from the hospital information system. Data from diverse legacy databases, such as patient-side monitoring devices and EMRs, are integrated into a single database for research use. DARWIN-C is a research database, does not include any patient-identifying information, and is not based on FHIR.
Variables of importance
Data were extracted from the DARWIN-C database of Samsung Medical Center and the National Emergency Department Information System for this study. Patient demographic and clinical information included sex, age, type of medical insurance, Korean Triage and Acuity Scale (KTAS) score,20 mode of presentation, information about arrival and discharge times, and disposition after the ED visit: the KTAS is a triage tool based on the Canadian Triage and Acuity Scale. We also extracted vital signs, laboratory results, and final diagnosis. Information from the FHIR database included 12-lead ECG transmission and response times after notification, ECG readings, automatic 12-lead ECG diagnosis, and 12-lead ECG capture time. Twelve-lead ECG capture was defined as the examination time shown in the ECG header during 12-lead ECG.
Development concept
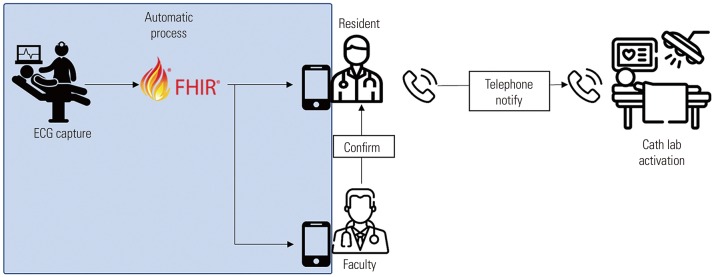
Fig. 2 shows the architecture of the FHIR-based transfer system in comparison with that of a conventional system. In the new system, a PGY1 visits the patient with a 12-lead ECG machine and transmits the data to the FHIR server. The FHIR server transmits the ECG image to the EMR as a PDF document, and when STEMI is observed, it sends a mobile notification to the resident and attending physician. The new system did not involve adding providers or communication lines, but rather removing the unnecessary gateways that could be bottlenecks with increased workload.
Fig. 2. New process using an FHIR-based 12-lead ECG. ECG, electrocardiogram; FHIR, Fast Healthcare Interoperability Resources.
Study participants
The study included patients who visited the ED between November 14 and December 7, 2018 and underwent a 12-lead ECG. Patients aged <18 years were excluded.
Primary outcome
The primary outcome was the successful transmission of 12-lead ECG information via the FHIR system. Successful transmission was defined as the process from ECG capture to alert transmission within 5 minutes. The automated FHIR-based 12-lead ECG alert system processing interval was defined as the time from ED arrival and 12-lead ECG capture to the time when the FHIR-based notification was transmitted.
Statistical analysis
On the basis or the cardiac-related symptoms, we analyzed successful transmission intervals from ED arrival to ECG capture and ECG capture to FHIR transmission in an automated FHIR-based 12-lead ECG alarm system. Continuous variables are expressed as means, standard deviations (SD), and medians (interquartile range, IQR). Categorical variables are expressed as frequencies and percentages. R version 3.5.2 (R Core Team, Vienna, Austria)21 was used for the statistical analysis.22 In the study, we used the t test, chi-square test, Fisher exact test, and Wilcoxon rank-sum test.
Ethics approval statement
This study was approved by our Institutional Review Board (IRB File No: SMC 2019-01-010).
RESULTS
System development
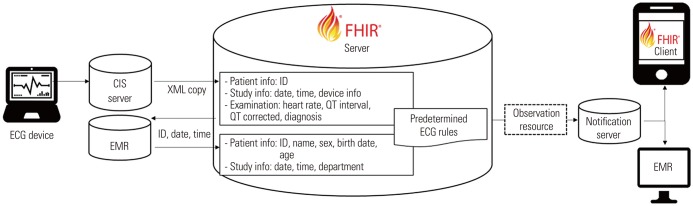
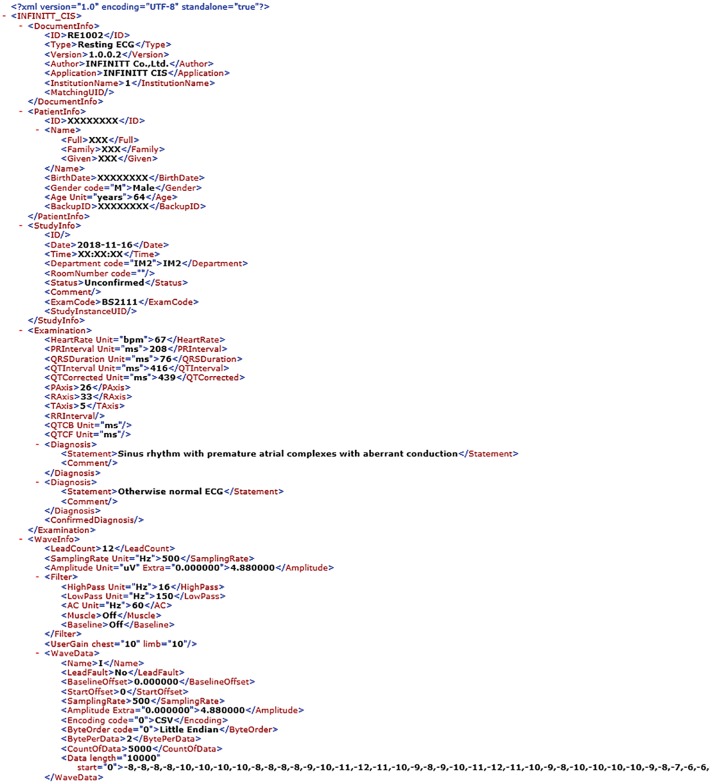
The automated FHIR-based 12-lead ECG alert transmission system was developed and activated in June 2016. As intended, the new system collected 12-lead ECG information as XML files stored in the clinical information system server. The FHIR server copied the XML file and activated the notification in accordance with the predetermined rules based on expert opinions to identify potential acute coronary syndrome cases and comprised 81 expressions, such as “ACUTE MI” and “ST elevation, consider anterior injury or acute infarct.” The full list is provided in Supplementary Table 1 (only online). Then, a notification was sent via FHIR transfer to a notification server, delivered through a mobile application and EMR. Fig. 3 shows the overall FHIR system. The FHIR-based 12-lead ECG system used the “Observation” FHIR resource, in which patient information was included as an identifier, and numerical information from the 12-lead ECG device was included as the value. The reference of its infrastructure is the XML structure of 10.1.3 Resource content, where an observation XML is generated and transmitted using HTTP POST methods. Once data are received, they are validated through the FHIR restful application programming interface (POST) and stored. The response message contains information on the success or failure of the transmission. The observation XML format and success or failure of the response messages are shown in Supplementary Fig. 1 (only online). Fig. 4 shows an FHIR-based 12-lead ECG XML sample. The file includes the identifier, name, sex, and findings, such as heart rate, QT interval, QTc, and diagnosis.
Fig. 3. Automated FHIR-based 12-lead ECG mobile alert system architecture. ECG, electrocardiogram; EMR, electronic medical record; CIS, clinical information system; FHIR, Fast Healthcare Interoperability Resources.
Fig. 4. Fast Healthcare Interoperability Resources message sample XML.
Patient enrollment
Of 5140 ED visits during the study period, 1328 were excluded because the patients were <18 years of age. Among 3812 cases, 1581 received 12-lead ECG. For 116 patients, 155 alerts were generated. The basic patient characteristics are shown in Table 1. The patients in the alerted group were significantly older and had more cardiac-related symptoms as the chief complaint. The chief complaint of cardiac-related symptoms included chest pain, chest discomfort, dyspnea, and palpitations.
Table 1. Basic Patient Characteristics.
| Alert group (n=116) | Non-alert group (n=1465) | p value | |
|---|---|---|---|
| Age | 68.1±12.4 | 59.6±16.8 | <0.001 |
| Sex | 0.529 | ||
| Male | 64 (55.2) | 757 (51.7) | |
| Female | 52 (44.8) | 708 (48.3) | |
| KTAS | 0.267 | ||
| 1 | 4 (3.4) | 21 (1.4) | |
| 2 | 14 (12.1) | 157 (10.7) | |
| 3 | 70 (60.3) | 881 (60.1) | |
| 4 | 25 (21.6) | 387 (26.4) | |
| 5 | 3 (2.6) | 19 (1.3) | |
| Chief complaint | <0.001 | ||
| Cardiac-related | 40 (34.5) | 279 (19.0) | |
| Non-cardiac-related | 76 (65.5) | 1186 (81.0) | |
| Trauma | 0.024 | ||
| Non-injury | 115 (99.1) | 1369 (93.4) | |
| Injury | 1 (0.9) | 96 (6.6) | |
| Visit | 0.259 | ||
| Direct visit | 82 (70.7) | 1111 (75.8) | |
| Non-direct visit | 34 (29.3) | 354 (24.2) | |
| Disposition | 0.011 | ||
| Discharge | 57 (49.1) | 879 (60.0) | |
| Death | 0 (0) | 13 (0.9) | |
| Admission | 46 (39.7) | 497 (33.9) | |
| Transfer to other institution | 13 (11.2) | 76 (5.2) | |
| Final diagnosis | <0.001 | ||
| Non-ACS | 101 (87.1) | 1405 (95.9) | |
| ACS except STEMI | 15 (12.9) | 58 (4.0) | |
| STEMI | 0 (0) | 2 (0.1) |
KTAS, Korean Triage and Acuity Scale; STEMI, ST-elevation myocardial infarction; ACS, Acute Coronary Syndrome.
Data are presented as number (%) or mean±SD.
Main results
The processing intervals are shown in Table 2. A total of 109 FHIR-based alerts (94%) were successfully activated, and 7 (6%) were delayed. In the group with cardiac-related symptoms, the overall median time was 26.3 min (IQR 15.4–109.0 min); the median time from arrival in the ED to 12-lead ECG capture was 21.9 min (IQR 11.1–86.7 min). In the group with cardiac-related symptoms, 39 patients received successfully transmitted FHIR-based alerts, and the median time elapsed from 12-lead ECG capture to alert transmission was 2.7 min (IQR 2.2–3.1 min). The median interval in the unsuccessful case was 1 patient, and the median time was 132 min. In the group with non-cardiac-related symptoms, the overall median time was 82.1 min (IQR 20.1–185.0 min). The median interval was 78.5 min (IQR 17.6–181.0 min) from arrival in the ED to 12-lead ECG capture. In the successful transmission, the median interval was 3.0 min (IQR 2.5–3.4 min). The median interval in the unsuccessful cases was 17.7 min (IQR 8.5–23.1 min) in the noncardiac- related symptom group.
Table 2. Processing Intervals.
| Interval, median (IQR) | Chief complaint | p value | |
|---|---|---|---|
| Cardiac-related (n=40) | Non-cardiac related (n=76) | ||
| From ED arrival to FHIR transmission | 26.3 (15.4–109.0) | 82.1 (20.1–185.0) | 0.077 |
| From ED arrival to ECG capture | 21.9 (11.1–86.7) | 78.5 (17.6–181.0) | 0.048 |
| From ECG capture to FHIR transmission | |||
| Successful transmission | 2.7 (2.2–3.1) | 3.0 (2.5–3.4) | 0.043 |
| Unsuccessful transmission | 132 (132–132) | 17.7 (8.5–23.1) | 0.286 |
IQR, interquartile range; ED, emergency department; FHIR, Fast Healthcare Interoperability Resources; ECG, electrocardiogram.
Among 81 rule expressions, 29 were used to alert generation. From 155 12-lead ECGs, 195 automatic 12-lead ECG diagnoses were generated. The top 10 most frequent activated automatic 12-lead ECG diagnoses based on the predetermined rules are shown in Table 3. The most frequent automatic 12-lead ECG diagnosis that activated the transmission was “PROBABLE INFERIOR INFARCT, AGE INDETERMINATE,” followed by “PROBABLE INFERIOR INFARCT, OLD.”
Table 3. The Top 10 Most Frequent Activated Automatic 12-Lead ECG Diagnoses Based on Predetermined Rules.
| No. | Automatic 12-lead ECG diagnosis | Frequency, n (%) |
|---|---|---|
| 1 | PROBABLE INFERIOR INFARCT, AGE INDETERMINATE | 20 (12.9) |
| 2 | PROBABLE INFERIOR INFARCT, OLD | 17 (11.0) |
| 3 | ANTERIOR INFARCT, AGE INDETERMINATE | 13 (8.4) |
| 4 | LATERAL INFARCT, AGE INDETERMINATE | 13 (8.4) |
| 5 | CONSIDER ANTERIOR INFARCT | 12 (7.7) |
| 6 | CONSIDER RVH OR POSTERIOR INFARCT | 12 (7.7) |
| 7 | CONSIDER ANTEROSEPTAL INFARCT | 9 (5.8) |
| 8 | PROBABLE POSTERIOR INFARCT | 9 (5.8) |
| 9 | CONSIDER INFERIOR INFARCT | 8 (5.1) |
| 10 | INFERIOR INFARCT, AGE INDETERMINATE | 8 (5.1) |
ECG, electrocardiogram.
DISCUSSION
This study described the development of an automated FHIR-based 12-lead ECG alert system applied to a real clinical setting. The system was successfully developed, and alerts were successfully generated in 109 (94%) cases. The alert group showed higher rates of admission and cardiac-related diagnosis. However, the system failed to detect two STEMI cases.
To our knowledge, this is the first study to apply the FHIR system in the ED environment. An automated algorithm-based alert system can play an important role in the ED, especially when the ED is overcrowded. Our alert system is comparable to that described in previous studies related to FHIR, which had been primarily used for outpatients.23,24,25 This study focused on the time-sensitive conditions that may most benefit from the FHIR system.
In the automated FHIR-based alert group, the process interval for the patients with cardiac-related disease was shorter than that for the patients with non-cardiac-related diagnosis. The system successfully transmitted FHIR-based alerts, although seven alerts (6%) were delayed. For the unsuccessful cases, the reason was likely synchronization failure: synchronization failure encompasses failure to connect to WIFI, failure to save the FHIR message, and failure to trigger alert modules. To confirm the cause of the error, detailed transmission logs should be archived for surveillance of each transmission process. The most frequent automatic 12-lead ECG diagnosis that activated transmission was “PROBABLE INFERIOR INFARCT, AGE INDETERMINATE.” Although we included 81 rules for STEMI detection, they failed to capture two STEMI cases during the study period. Improving alert accuracy will be critical in system implementation. To develop a more intelligent ECG interpretation, clinical data, such as vital signs, cardiac enzymes, and machine learning on waveform, will be required. This implies that this system and an “ECG diagnostic algorithm for acute coronary syndrome” should not completely replace a physician's clinical acumen, which includes comprehensive medical history taking, physical examination, and communication skills. The system should be used to complement a physician's abilities.
There are several limitations to our study. First, system notification was not directly transmitted to on-call cardiologists or the catheterization laboratory team, which limited the effectiveness of the system in shortening the door-to-balloon interval. Direct activation was not performed because the system was not fully developed enough to be implemented in full scale. The plan was to implement a full-scale alert system after the completion of this study, which was postponed because of the high rate of false alerts. Second, a well-known clinical outcome, namely door-to-balloon time, was not measured in this study. We also did not measure catheterization laboratory activation of door-to-balloon time. The FHIR activation rules were based solely on automatic ECG diagnosis of the ECG devices, whose accuracy is not sufficient for automated activation. Owing to these pitfalls, the FHIR-based system missed two true STEMI cases during the study period. In the two 12-lead ECGs (Supplementary Fig. 2, only online), the 12-lead ECG report failed to read the ECG findings, and the other automatic 12-lead ECG diagnosis did not include our predetermined rules. Enhancing the diagnostic algorithm is critical for expanding the application of the system. Moreover, this study did not include clinical outcomes, such as mortality or morbidity. A trial with clinical outcomes can be carried out when the diagnostic accuracy and alerting network are further improved. Third, only STEMI patients were targeted as study subjects. The impact of this study could have been more significant if the alert triggering rules included various cardiac emergency conditions, such as paroxysmal supraventricular tachycardia. This is because the study aimed at developing and testing the feasibility of the system described herein. Fourth, this study took a longer time interval between system development and validation than initially expected. This could pose bias since the initial design could have been altered during the long waiting time. Finally, this study was retrospective in nature; therefore, a well-designed prospective study is needed for future work. Also, we plan to create an algorithm that analyzes the ECG header to link the results to clinical findings.
We found that our automated FHIR-based 12-lead ECG mobile alert system is applicable in the ED. With vigorous optimization and workflow adoption, the system is expected to show better effects in the future.
ACKNOWLEDGEMENTS
The authors acknowledge J.Y. for the statistical assistance.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI19C0275).
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Won Chul Cha and Dong Kyung Chang.
- Data curation: Won Chul Cha and Sujeong Hur.
- Formal analysis: Sujeong Hur and Jeanhyoung Lee.
- Funding acquisition: Won Chul Cha.
- Investigation: Mira Kang.
- Methodology: Won Chul Cha and Dong Kyung Chang.
- Project administration: Won Chul Cha.
- Resources: Jeanhyoung Lee.
- Software: Jeanhyoung Lee and Jong Soo Choi.
- Supervision: Won Chul Cha and Dong Kyung Chang.
- Validation: Taerim Kim.
- Visualization: Taerim Kim.
- Writing—original draft: Sujeong Hur, Jeanhyoung Lee, and Won Chul Cha.
- Writing—review & editing: all authors.
- Approval of final manuscript: all authors.
SUPPLEMENTARY MATERIALS
Predetermined Rules Based on Expert Opinions to Identify Potential Acute Coronary Syndrome Cases
Observation XML format and success or failure response message.
Two true STEMI cases missed during the study period.
References
- 1.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79:186–194. doi: 10.1097/00001888-200402000-00019. [DOI] [PubMed] [Google Scholar]
- 2.Aspden P, Corrigan JM, Wolcott J, Erickson SM, editors. Institute of Medicine, Board on Health Care Services, Committee on Data Standards for Patient Safety. Patient safety: achieving a new standard for care. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 3.Shapiro JS, Kannry J, Lipton M, Goldberg E, Conocenti P, Stuard S, et al. Approaches to patient health information exchange and their impact on emergency medicine. Ann Emerg Med. 2006;48:426–432. doi: 10.1016/j.annemergmed.2006.03.032. [DOI] [PubMed] [Google Scholar]
- 4.Zahabi M, Kaber DB, Swangnetr M. Usability and safety in electronic medical records interface design: a review of recent literature and guideline formulation. Hum Factors. 2015;57:805–834. doi: 10.1177/0018720815576827. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman S, Podgurski A. Meaningful use and certification of health information technology: what about safety? J Law Med Ethics. 2011;39 Suppl 1:77–80. doi: 10.1111/j.1748-720X.2011.00572.x. [DOI] [PubMed] [Google Scholar]
- 6.Sittig DF, Singh H. Defining health information technology-related errors: new developments since to err is human. Arch Intern Med. 2011;171:1281–1284. doi: 10.1001/archinternmed.2011.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kellermann AL, Jones SS. What it will take to achieve the as-yetunfulfilled promises of health information technology. Health Aff (Millwood) 2013;32:63–68. doi: 10.1377/hlthaff.2012.0693. [DOI] [PubMed] [Google Scholar]
- 8.Akhlaq A, Sheikh A, Pagliari C. Defining health information exchange: scoping review of published definitions. J Innov Health Inform. 2017;23:838. doi: 10.14236/jhi.v23i4.838. [DOI] [PubMed] [Google Scholar]
- 9.Edwards A, Hollin I, Barry J, Kachnowski S. Barriers to cross--institutional health information exchange: a literature review. J Healthc Inf Manag. 2010;24:22–34. [PubMed] [Google Scholar]
- 10.Walker J, Pan E, Johnston D, Adler-Milstein J, Bates DW, Middleton B. The value of health care information exchange and interoperability. Health Aff (Millwood) 2005;Suppl Web Exclusives:W5-10–W5-18. doi: 10.1377/hlthaff.w5.10. [DOI] [PubMed] [Google Scholar]
- 11.Mead CN. Data interchange standards in healthcare IT--computable semantic interoperability: now possible but still difficult, do we really need a better mousetrap? J Healthc Inf Manag. 2006;20:71–78. [PubMed] [Google Scholar]
- 12.Hammond WE. The making and adoption of health data standards. Health Aff (Millwood) 2005;24:1205–1213. doi: 10.1377/hlthaff.24.5.1205. [DOI] [PubMed] [Google Scholar]
- 13.Helman G, Shah I, Williams AJ, Edwards J, Dunne J, Patlewicz G. Generalized Read-Across (GenRA): a workflow implemented into the EPA CompTox Chemicals Dashboard. ALTEX. 2019;36:462–465. doi: 10.14573/altex.1811292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehta AY, Cummings RD. GLAD: GLycan Array Dashboard, a visual analytics tool for glycan microarrays. Bioinformatics. 2019;35:3536–3537. doi: 10.1093/bioinformatics/btz075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khalilia M, Choi M, Henderson A, Iyengar S, Braunstein M, Sun J. Clinical predictive modeling development and deployment through FHIR Web services. AMIA Annu Symp Proc. 2015;2015:717–726. [PMC free article] [PubMed] [Google Scholar]
- 16.Yiadom MY, Baugh CW, McWade CM, Liu X, Song KJ, Patterson BW, et al. Performance of Emergency Department Screening Criteria for an Early ECG to Identify ST-Segment Elevation Myocardial Infarction. J Am Heart Assoc. 2017;6:e003528. doi: 10.1161/JAHA.116.003528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 18.Choi IK, Choi HJ, Oh SB, Kang TS. Effect of establishing an ECG transmission system on time required for patients with ST-segment elevation myocardial infarction to receive reperfusion therapy. J Korean Soc Emerg Med. 2011;22:591–598. [Google Scholar]
- 19.Cha WC, Ahn KO, Shin SD, Park JH, Cho JS. Emergency department crowding disparity: a nationwide cross-sectional study. J Korean Med Sci. 2016;31:1331–1336. doi: 10.3346/jkms.2016.31.8.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim JH, Kim JW, Kim SY, Hong DY, Park SO, Baek KJ, et al. Validation of the Korean triage and acuity scale compare to triage by emergency severity index for emergency adult patient: preliminary study in a tertiary hospital emergency medical center. J Korean Soc Emerg Med. 2016;27:436–441. [Google Scholar]
- 21.R Core Team. R: A Language and Environment for Statistical Computing. 3.5.2 ed. Vienna, Austria: R Foundation for Statistical Computing; 2018. [Google Scholar]
- 22.Opsahl A, Horton-Deutsch S. A nursing dashboard to communicate the evaluation of program outcomes. Nurse Educ. 2019;44:326–329. doi: 10.1097/NNE.0000000000000632. [DOI] [PubMed] [Google Scholar]
- 23.Lee J, Hulse NC, Wood GM, Oniki TA, Huff SM. Profiling Fast Healthcare Interoperability Resources (FHIR) of family health history based on the clinical element models. AMIA Annu Symp Proc. 2017;2016:753–762. [PMC free article] [PubMed] [Google Scholar]
- 24.Pandya ST, Chakravarthy K, Vemareddy A. Obstetric anaesthesia practice: dashboard as a dynamic audit tool. Indian J Anaesth. 2018;62:838–843. doi: 10.4103/ija.IJA_346_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yoo J, Jung KY, Kim T, Lee T, Hwang SY, Yoon H, et al. A real-time autonomous dashboard for the emergency department: 5-year case study. JMIR Mhealth Uhealth. 2018;6:e10666. doi: 10.2196/10666. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Predetermined Rules Based on Expert Opinions to Identify Potential Acute Coronary Syndrome Cases
Observation XML format and success or failure response message.
Two true STEMI cases missed during the study period.