Abstract
Although some information on the epidemiology of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and a few selected cases has been reported, data on the clinical characteristics and outcomes of patients hospitalized therewith in South Korea are lacking. We conducted a retrospective single-center study of 98 consecutive hospitalized patients with confirmed SARS-CoV-2 infection at Yeungnam University Medical Center in Daegu, South Korea. Sixty patients were women (61.2%), and the mean age was 55.4±17.1 years. Thirteen patients (13.3%) were treated in the intensive care unit (ICU). The mean interval from symptom onset to hospitalization was 7.7±4.5 days. Patients who received ICU care were significantly older and were more likely to have diabetes mellitus. The National Early Warning Score on the day of admission was significantly higher in patients requiring ICU care. Acute respiratory distress syndrome (13/13 patients; 100%), septic shock (9/13; 69.2%), acute cardiac injury (9/13; 69.2%), and acute kidney injury (8/13; 61.5%) were more common in patients who received ICU care. All patients received antibiotic therapy, and most (97/98 patients; 99.0%) received antiviral therapy (lopinavir/ritonavir). Hydroxychloroquine was used in 79 patients (80.6%), and glucocorticoid therapy was used in 18 patients (18.4%). In complete blood counts, lymphopenia was the most common finding (40/98 patients; 40.8%). Levels of all proinflammatory cytokines were significantly higher in ICU patients. As of March 29, 2020, the mortality rate was 5.1%. Here, we report the clinical characteristics and laboratory findings of SARS-CoV-2 patients in South Korea up to March 29, 2020.
Keywords: Coronavirus, SARS-CoV-2, COVID-19, Korea, clinical characteristics
In December 2019, a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic causing pneumonia began in Wuhan, China. By March 29, 2020, 9583 cases of coronavirus disease 2019 (COVID-19) had been diagnosed in South Korea. Although several Chinese studies have described the clinical characteristics of COVID-19,1,2,3 there are no such studies for Korea. As patient-, disease-, physician-, and healthcare systemrelated factors can be associated with mortality from COVID-19, we sought to describe the clinical and radiological characteristics of SARS-CoV-2 patients admitted to Yeungnam University Medical Center in Daegu, South Korea up to March 29, 2020, as well as laboratory findings.
This study was conducted in accordance with the tenets of the Declaration of Helsinki, and was reviewed and approved by the Institutional Review Board of Yeungnam University Hospital (YUH IRB 2020-03-057). The requirement for informed consent was waived because of the retrospective study design. The final date of follow-up was March 29, 2020.
Patient electronic medical records were reviewed. Clinical data included age, sex, exposure history, comorbidities, symptoms, vital signs, radiologic findings, complications, treatment, clinical outcomes, and laboratory findings. Blood samples of some suspected cases were collected for proinflammatory cytokine analysis. The concentrations of cytokines in COVID-19 were determined using commercial enzyme-linked immunosorbent assays.
The National Early Warning Score (NEWS) is an early warning score facilitating the early detection of and responses to patient deterioration.4 NEWS encompasses seven physiological parameters: pulse oximetry, oxygen, pulse, systolic blood pressure, respiration rate, temperature, and central nervous system status. Each parameter is assigned a score of 0 to 3 points. The score reflects the extent to which the parameter differs from the standard.
Acute respiratory distress syndrome (ARDS) was defined according to the Berlin definition.5 Septic shock was defined according to the third international consensus definitions for sepsis and septic shock (Sepsis-3).6 Acute cardiac injury was defined as a serum troponin I level above the 99th percentile upper reference limit or new abnormal electrocardiography and echocardiography findings.2 Acute kidney injury was defined according to the Kidney Disease Improving Global Guidelines (KDIGO) for acute kidney injury.7
The Acute Physiology and Chronic Health Evaluation II (APACHE II), a severity of disease classification system,8 is widely used as an index of illness severity and as a predictor of outcomes.9 APACHE II score is based on age, previous health status, and the initial values of 12 physiological measurements. The Sequential Organ Failure Assessment (SOFA) scale is a scoring system deigned to evaluate complications in critically ill patients.10 The SOFA scale assigns a score of 0 to 4 to each of six parameters related to organ function (respiration, coagulation, liver, cardiovascular, central nervous system, and renal).
Continuous variables are expressed as means±standard deviations (SDs) and were compared using Student's t-test or the Mann-Whitney U test. Categorical variables were compared using the chisquared test or Fisher's exact test. In all analyses, a two-tailed p value<0.05 was considered to indicate statistical significance. All statistical analyses were performed using SPSS software (ver. 24.0; IBM Corp., Armonk, NY, USA).
Table 1 shows the baseline clinical characteristics and radiological findings of patients hospitalized with SARS-CoV-2 infection. This study included 98 patients with SARS-CoV-2, 13 (13.3%) of whom were treated in the intensive care unit (ICU). Sixty patients were women (61.2%) and their mean age was 55.4±17.1 years, similar to recently released national epidemiological data for Korea.11 The mean interval from symptom onset to hospitalization was 7.7 days. Similar to the national epidemiological data,11 the largest group in our study with a history of exposure was the Shincheonji religious group, which comprised 47 patients (48.0%). In our study, the proportion of patients over 50 years of age was 70.4%, compared to 44% in China. The large proportion of women over 50 years of age in our research is thought to be related to the outbreak in the Shincheonji religious group whose followers comprise a female majority.
Table 1. Baseline Characteristics and Radiological Findings of Patients Admitted to Yeungnam University Medical Center with SARS-CoV-2 Infection.
| Characteristics | All patients (n=98) | ICU (n=13) | Non-ICU (n=85) | p value |
|---|---|---|---|---|
| Age (yr) | 55.4±17.1 | 63.2±10.1 | 54.2±17.7 | 0.014 |
| 21–49 | 29 (29.6) | 1 (7.7) | 28 (32.9) | 0.054 |
| 50–64 | 40 (40.8) | 6 (46.2) | 34 (40.0) | |
| ≥65 | 29 (29.6) | 6 (46.2) | 23 (27.1) | |
| Sex | 0.558 | |||
| Male | 38 (38.8) | 6 (46.2) | 32 (37.6) | |
| Female | 60 (61.2) | 7 (53.8) | 53 (62.4) | |
| Interval from symptom onset to hospital admission (day) | 7.7±4.5 | 4.7±3.1 | 8.2±4.6 | 0.009 |
| Exposure history | ||||
| Shincheonji follower | 47 (48.0) | 2 (15.4) | 45 (52.9) | 0.012 |
| Comorbidities | 38 (38.8) | 5 (38.5) | 33 (38.8) | 0.980 |
| Cardiovascular disease | 11 (11.2) | 0 (0) | 11 (12.9) | 0.350 |
| Cerebrovascular disease | 2 (2.0) | 0 (0)) | 2 (2.4) | 1.000 |
| Chronic lung disease | 3 (3.1) | 0 (0) | 3 (3.5) | 1.000 |
| Dementia | 3 (3.1) | 0 (0) | 3 (3.5) | 1.000 |
| Diabetes mellitus | 9 (9.2) | 3 (23.1) | 6 (7.1) | 0.096 |
| Hypertension | 30 (30.6) | 5 (38.5) | 25 (29.4) | 0.529 |
| Liver disease | 1 (1.0) | 0 (0) | 1 (1.2) | 1.000 |
| Malignancy | 4 (4.1) | 1 (7.7) | 3 (3.5) | 0.439 |
| Parkinson’s disease | 1 (1.0) | 1 (7.7) | 0 (0) | 0.133 |
| Symptoms on admission | ||||
| Fever | 62 (63.3) | 8 (61.5) | 54 (63.5) | 1.000 |
| Cough | 58 (59.2) | 6 (46.2) | 52 (61.2) | 0.305 |
| Sputum | 39 (39.8) | 2 (15.4) | 37 (43.5) | 0.054 |
| Myalgia | 37 (37.8) | 3 (23.1) | 34 (40.0) | 0.359 |
| Dyspnea | 32 (32.7) | 8 (61.5) | 24 (28.2) | 0.026 |
| Vital signs on admission | ||||
| Body temperature, ℃ | 37.3±0.7 | 37.5±0.9 | 37.3±0.7 | 0.321 |
| Heart rate, beats/min | 84.7±16.1 | 83.5±20.4 | 84.9±15.5 | 0.321 |
| Respiratory rate | 22.3±9.5 | 30.0±18.6 | 21.2±6.7 | 0.115 |
| Systolic BP, mm Hg | 127.9±18.4 | 135.5±20.3 | 126.7±18.0 | 0.109 |
| Diastolic BP, mm Hg | 80.2±12.4 | 84.4±11.6 | 79.6±12.5 | 0.199 |
| Mean arterial BP, mm Hg | 96.1±12.9 | 101.4±14.1 | 84.4±11.6 | 0.111 |
| NEWS | 2.6±3.0 | 7.8±2.9 | 1.8±2.2 | <0.001 |
| Respiratory rate | 0.4±0.8 | 1.3±1.3 | 0.2±0.6 | 0.011 |
| Peripheral oxygen saturation | 0.7±1.1 | 2.5±1.0 | 0.4±0.8 | <0.001 |
| Supplemental oxygen | 0.5±0.9 | 1.8±0.6 | 0.3±0.7 | <0.001 |
| Body temperature | 0.1±0.3 | 0.1±0.3 | 0.1±0.4 | 0.530 |
| Systolic BP | 0.5±0.9 | 0.9±1.1 | 0.4±0.8 | 0.039 |
| Heart rate | 0.3±0.6 | 0.8±1.0 | 0.3±0.4 | 0.055 |
| Level of consciousness | 0.1±0.5 | 0.2±0.8 | 0.1±0.5 | 0.509 |
| Radiological findings | 0.657 | |||
| Chest X-ray only | 34 (34.7) | 6 (46.2) | 28 (32.9) | |
| Chest X-ray and CT | 64 (65.3) | 7 (53.8) | 57 (67.1) | |
| Unilateral pneumonia | 14 (14.3) | 1 (7.7) | 13 (15.3) | |
| Bilateral pneumonia | 34 (34.7) | 8 (61.5) | 26 (30.6) | |
| Multiple ground-glass opacity | 42 (42.9) | 4 (30.8) | 38 (44.7) |
BP, blood pressure; CT, computed tomography; ICU, intensive care unit; NEWS, National Early Warning Score; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Data are presented as a mean±SD or number (percentage).
More than one comorbidity was present in 38 patients (38.8%), of whom 30 (30.6%) had hypertension; this was the most prevalent comorbidity. A recent study in China revealed that patients who required ICU care were more likely to have hypertension, diabetes, cardiovascular disease, and cerebrovascular disease than patients who did not receive ICU care.2 In our study, diabetes mellitus tended to be more common in ICU patients (23.1% vs. 7.1%, p=0.096). It was difficult to detect meaningful differences in comorbidities between patients treated in the ICU and those who were not due to the relatively small number of patients.
On admission, about 60% of the patients had a fever and cough, and one-third had sputum, myalgia, and dyspnea. Interestingly, vital signs recorded on the day of admission did not differ between patients who did and did not require ICU care. NEWS values on the day of admission was significantly higher in patients requiring ICU care (7.8±2.9 vs. 1.8±2.2, p<0.001). Of the NEWS parameters, body temperature, heart rate, and level of consciousness were not associated with ICU care. The Royal College of Physicians recommend the use of NEWS to identify patients at risk of cardiac arrest, unanticipated ICU admission, or death. The area under receiver operating characteristic curves of NEWS for predicting unanticipated ICU admission was 0.857 ([95% confidence interval (CI), 0.847–0.868] in a previous study.4 Our study demonstrated that NEWS was more useful than initial vital signs in predicting ICU admission in patients with COVID-19.
Table 2 shows the complications, treatment patterns, and clinical outcomes of the patients hospitalized with SARS-CoV-2 infection. As previously reported in a Chinese study,2 our patients who required ICU care had many complications, such as multiple organ failure. ARDS (18/98 patients; 18.4%), septic shock (9/98; 9.2%), acute cardiac injury (11/98; 11.2%), and acute kidney injury (9/98; 9.2%) were more frequent in our study than in other Chinese studies.1,2,3,12 It is estimated that the severity of disease in the COVID-19 patients enrolled in this study was higher than that of the patients in Chinese studies. The greater disease severity may account for higher rates of use of invasive mechanical ventilation (11.2%), extracorporeal membrane oxygenation (4.1%), and continuous renal replacement therapy (3.1%) than reported in the aforementioned Chinese studies.
Table 2. Complications, Treatment, and Clinical Outcomes of Patients with SARS-CoV-2 Infection.
| All patients (n=98) | ICU (n=13) | Non-ICU (n=85) | p value | |
|---|---|---|---|---|
| Complications | ||||
| ARDS | 18 (18.4) | 13 (100) | 5 (5.9) | <0.001 |
| Septic shock | 9 (9.2) | 9 (69.2) | 0 (0) | <0.001 |
| Acute cardiac injury | 11 (11.2) | 9 (69.2) | 2 (2.4) | <0.001 |
| Acute kidney injury | 9 (9.2) | 8 (61.5) | 1 (1.2) | <0.001 |
| Treatment | ||||
| Oxygen | 37 (37.8) | 12 (92.3) | 25 (29.4) | <0.001 |
| HFNC | 12 (12.2) | 7 (53.8) | 5 (5.9) | <0.001 |
| IMV | 11 (11.2) | 11 (84.6) | 0 (0) | <0.001 |
| CRRT | 3 (3.1) | 3 (23.1) | 0 (0) | 0.002 |
| ECMO | 4 (4.1) | 4 (30.8) | 0 (0) | <0.001 |
| Antibiotics | 98 (100) | 13 (100) | 85 (100) | |
| Lopinavir/ritonavir | 97 (99.0) | 13 (100) | 84 (98.8) | 1.000 |
| Hydroxychloroquine | 79 (80.6) | 13 (100) | 66 (77.6) | 0.067 |
| Glucocorticoid | 18 (18.4) | 10 (76.9) | 8 (9.4) | <0.001 |
| Clinical outcomes | 0.004 | |||
| Remains in hospital | 57 (58.2) | 7 (53.8) | 50 (58.8) | |
| Discharged | 30 (30.6) | 1 (7.7) | 29 (34.1) | |
| Died | 5 (5.1) | 4 (30.8) | 1 (1.2) | |
| Transferred | 6 (6.1) | 1 (7.7) | 5 (5.9) |
ARDS, acute respiratory distress syndrome; CRRT, continuous renal replacement therapy; ECMO, extracorporeal membrane oxygenation; HFNC, high-flow nasal cannula; ICU, intensive care unit; IMV, invasive mechanical ventilation; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Data are presented as a number (percentage).
All patients received antibiotic therapy, and most (99.0%) received antiviral therapy (lopinavir/ritonavir). Hydroxychloroquine was used in 79 (80.6%) patients. Glucocorticoid therapy was used in 18 patients (18.4%); this therapy was used more frequently in patients who required ICU care (76.9% vs. 9.4%, p<0.001). According to a study involving 1099 patients in 552 hospitals,3 18.6% received systemic glucocorticoids, and 44.5% of patients with severe COVID-19 received systemic glucocorticoids. In our study, 18.4% of all patients received systemic glucocorticoids, and 76.9% of patients in the ICU received systemic glucocorticoids. Because “severity” was not clearly defined in the Chinese study, it is difficult to compare findings. However, the high rate of use of glucocorticoids in our study can be explained by the fact that 84% of our ICU patients received invasive mechanical ventilation versus just 35.7% of the severe COVID-19 patients in the Chinese study. Wu, et al.13 reported that treatment with methylprednisolone decreased the risk of death (hazard ratio, 0.38; 95% CI, 0.20–0.72) in patients with COVID-19 pneumonia who developed ARDS. The use of glucocorticoids for COVID-19 is beneficial in certain groups of patients, although further investigation is needed to identify the subgroups that can benefit the most.
As of March 29, 30 patients (30.6%) had been discharged, and 5 (5.1%) had died. Six patients (one ICU and five general ward patients) were transferred to other tertiary care hospitals because our medical resources were exhausted. All of the other patients are still in the hospital. Because our hospital is a tertiary care university hospital, with many patients requiring intensive care, the fatality rate is likely higher than the overall mortality rate in Korea. However, the fatality rate in our study was much lower than rates reported in three single-center studies of hospitalized COVID-19 patients in Wuhan, China.1,2,12 Since there will be additional deaths among patients who remain in the hospital, the final fatality rate is expected to increase.
Table 3 shows the laboratory findings of the patients on admission to hospital. In the complete blood counts, lymphopenia (40.8%) was the most common finding, followed by anemia (24.5%), neutrophilia (20.4%), and thrombocytopenia (13.3%). In blood chemistry analyses, increased lactate dehydrogenase (50.5%) was common.
Table 3. Laboratory Findings of Patients with SARS-CoV-2 Infection on Admission to Hospital.
| All patients (n=98) | ICU (n=13) | Non-ICU (n=85) | p value | |
|---|---|---|---|---|
| Complete blood count | ||||
| White blood cell count, ×109/L | 6.5±3.4 | 8.9±3.3 | 6.1±3.2 | 0.005 |
| Increased | 9 (9.2) | 4 (30.8) | 5 (5.9) | 0.003 |
| Decreased | 18 (18.4) | 0 (0) | 18 (21.2) | |
| Neutrophil count, ×109/L | 4.6±3.4 | 7.7±3.3 | 4.1±3.2 | <0.001 |
| Increased | 20 (20.4) | 9 (69.2) | 11 (12.9) | <0.001 |
| Lymphocyte count, ×109/L | 1.4±0.7 | 0.8±0.3 | 1.5±0.7 | <0.001 |
| Decreased | 40 (40.8) | 11 (84.6) | 29 (34.1) | 0.001 |
| Hemoglobin, g/dL | 13.0±1.6 | 13.5±1.7 | 13.0±1.6 | 0.253 |
| Decreased | 24 (24.5) | 3 (23.1) | 21 (24.7) | 1.000 |
| Platelets, ×109/L | 237.3±104.9 | 186.7±64.9 | 245.0±107.9 | 0.061 |
| Increased | 4 (4.1) | 0 (0) | 4 (4.7) | 0.188 |
| Decreased | 13 (13.3) | 3 (23.1) | 10 (11.8) | |
| Blood chemistry | ||||
| Albumin, g/dL | 3.7±0.5 | 3.0±0.3 | 3.9±0.5 | <0.001 |
| Decreased | 33 (34.4) | 12 (92.3) | 21 (25.3) | <0.001 |
| Alanine aminotransferase, IU/L | 33.9±42.1 | 58.8±93.6 | 30.1±26.3 | 0.294 |
| Increased | 19 (19.4) | 3 (23.1) | 16 (18.8) | 0.712 |
| Aspartate aminotransferase, IU/L | 45.9±47.2 | 100.3±97.0 | 37.5±26.6 | 0.038 |
| Increased | 42 (42.9) | 11 (84.6) | 31 (36.5) | 0.001 |
| Total bilirubin, mg/dL | 0.9±0.4 | 1.1±0.6 | 0.8±0.4 | 0.071 |
| Increased | 16 (16.3) | 4 (30.8) | 12 (14.1) | 0.218 |
| Blood urea nitrogen, mg/dL | 15.3±9.5 | 20.0±11.4 | 14.6±9.0 | 0.057 |
| Increased | 12 (12.2) | 4 (30.8) | 8 (9.4) | 0.051 |
| Creatinine, mg/dL | 0.9±0.5 | 1.0±0.3 | 0.8±0.5 | 0.467 |
| Increased | 29 (29.6) | 6 (46.2) | 23 (27.1) | 0.196 |
| Creatinine phosphokinase, IU/L | 105.4±153.9 | 131.9±122.0 | 100.7±159.1 | 0.504 |
| Increased | 11 (12.6) | 2 (15.4) | 9 (12.2) | 0.667 |
| Lactate dehydrogenase, IU/L | 648.0±350.7 | 1272.6±542.1 | 555.5±184.0 | <0.001 |
| Increased | 47 (50.5) | 12 (100) | 35 (43.2) | <0.001 |
| Infection biomarkers | ||||
| C-reactive protein, mg/dL | 6.0±8.4 | 17.7±9.5 | 4.2±6.7 | <0.001 |
| Increased | 61 (67.8) | 12 (100) | 49 (62.8) | 0.008 |
| Procalcitonin, ng/mL | 0.5±2.8 | 2.7±7.0 | 0.2±1.3 | 0.248 |
| Increased | 6 (6.2) | 4 (33.3) | 2 (2.4) | 0.002 |
ICU, intensive care unit; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Data are presented as a mean±SD or number (percentage).
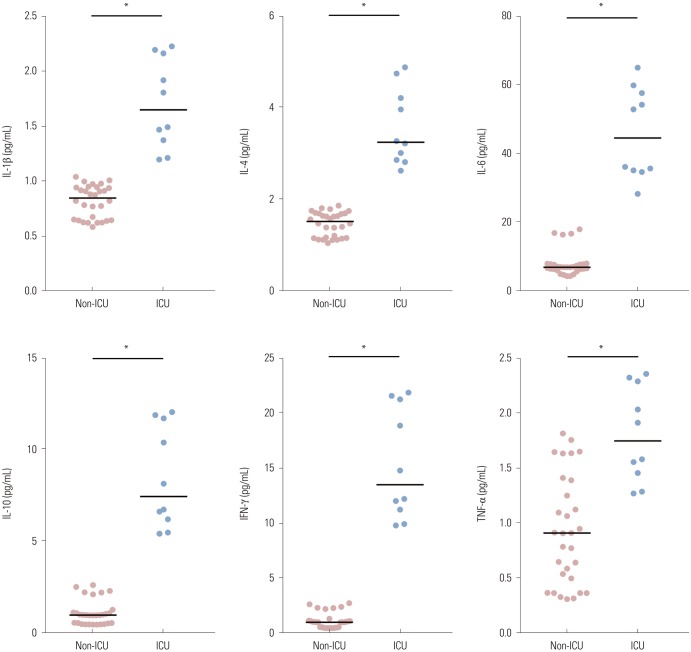
Among infection-related biomarkers, C-reactive protein was elevated in 61 (67.8%) patients, while procalcitonin was increased only in 6 (6.2%). Fig. 1 shows the concentrations of the proinflammatory cytokines interleukin-1β (IL-1β), IL-4, IL-6, IL-10, interferon-γ (IFN-γ), and tumor necrosis factor-α (TNF-α) in the SARS-CoV-2-infected patients [n=40 (ICU, n=10)]. Levels of all proinflammatory cytokines were significantly higher in ICU patients than in non-ICU patients in our study. Previous studies have demonstrated that increases in proinflammatory cytokine levels are associated with more severe disease in Middle East respiratory syndrome and severe acute respiratory syndrome patients. In patients with Middle East respiratory syndrome in South Korea, IL-6 and CXCL-10 levels were significantly higher in the severe disease group than in the mild group.14 In severe acute respiratory syndrome patients, the levels of inflammatory cytokines IL-1, IL-6, IL-12, and IFN-γ were elevated.15 To prevent organ damage from cytokine release syndrome, it is imperative to develop a drug that targets these cytokines.
Fig. 1. Concentrations of proinflammatory cytokines in the plasma of SARS-CoV-2 patients. Plasma levels of the proinflammatory cytokines IL-1β, IL-4, IL-6, IL-10, IFN-γ, and TNF-α in SARS-CoV-2-infected non-ICU (n=30) and ICU (n=10) patients. Data are presented as a mean±standard error of the mean. *p<0.001 vs. non-ICU (one-way ANOVA). IL, interleukin; ICU, intensive care unit; IFN, interferon; TNF, tumor necrosis factor; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; ANOVA, analysis of variance.
The severity of respiratory illness and results of arterial blood gas analyses of 13 ICU patients on the day of ICU admission were also measured. The mean interval from hospital admission to ICU admission was 1.2±1.5 days. On the day of ICU admission, the mean APACHE II score was 19.6±7.1, and the mean SOFA score was 7.4±3.2. The mean pH, lactate level, mean partial pressure of oxygen/fraction of inspired oxygen ratio, and mean partial pressure of carbon dioxide were 7.4±0.1, 1.7±0.8 mmol/L, 174.5±44.9, and 39.8±9.5, respectively.
A limitation of this study was that it was conducted at a single medical center and included a small number of patients. However, this study identified many predictors of the likely requirement for ICU care. We also found that proinflammatory cytokine levels were higher in patients with severe disease. A second limitation was the fact that this study did not include the patients' final clinical outcomes. Further analysis will be needed when the COVID-19 pandemic ends and final outcome data are available.
This is the first study to describe the clinical characteristics of hospitalized patients with SARS-CoV-2 in South Korea. In this single-center descriptive study of 98 patients hospitalized with SARS-CoV-2 in Daegu, South Korea, 13.3% of the patients received ICU care. As of March 29, 2020, the mortality rate was 5.1%.
ACKNOWLEDGEMENTS
We thank all of the staff who have helped to care for COVID-19 patients at Yeungnam University Medical Center in Daegu, South Korea. This study was supported by a research grant from Daegu Medical Association COVID-19 scientific committee.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kyung Soo Hong, Kwan Ho Lee, and June Hong Ahn.
- Data curation: Kyung Soo Hong, Jong Geol Jang, Wonhwa Lee, and June Hong Ahn.
- Formal analysis: June Hong Ahn and Wonhwa Lee.
- Funding acquisition: June Hong Ahn.
- Investigation: Kyung Soo Hong, Jong Geol Jang, and June Hong Ahn.
- Methodology: Kyung Soo Hong, Jong Geol Jang, Eun Young Choi, and June Hong Ahn.
- Project administration: June Hong Ahn.
- Resources: Kyung Soo Hong, Eun Young Choi, and Jong Geol Jang.
- Software: June Hong Ahn.
- Supervision: Kwan Ho Lee, Jin Hong Chung, Kyeong-Cheol Shin, Eun Young Choi, and Hyun Jung Jin.
- Validation: June Hong Ahn.
- Visualization: June Hong Ahn.
- Writing—original draft: June Hong Ahn.
- Writing—review & editing: June Hong Ahn.
- Approval of final manuscript: all authors.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirusinfected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Feb 28; doi: 10.1056/NEJMoa2002032. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation. 2013;84:465–470. doi: 10.1016/j.resuscitation.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 5.ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 6.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179–c184. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 8.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 9.Polderman KH, Girbes AR, Thijs LG, Strack van Schijndel RJ. Accuracy and reliability of APACHE II scoring in two intensive care units problems and pitfalls in the use of APACHE II and suggestions for improvement. Anaesthesia. 2001;56:47–50. doi: 10.1046/j.1365-2044.2001.01763.x. [DOI] [PubMed] [Google Scholar]
- 10.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 11.Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020;35:e112. doi: 10.3346/jkms.2020.35.e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 Mar 13; doi: 10.1001/jamainternmed.2020.0994. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim ES, Choe PG, Park WB, Oh HS, Kim EJ, Nam EY, et al. Clinical progression and cytokine profiles of middle east respiratory syndrome coronavirus infection. J Korean Med Sci. 2016;31:1717–1725. doi: 10.3346/jkms.2016.31.11.1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong CK, Lam CW, Wu AK, Ip WK, Lee NL, Chan IH, et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136:95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]