Capsule Summary
Early sensitization is ~50% higher in children with atopic dermatitis compared to children from a high-risk allergy cohort with comparable rates of parental atopy. AD may increase sensitization risk over heredity alone.
Keywords: sensitization, atopic dermatitis, pediatric, high-risk, cohort
To the Editor:
Birth cohort studies have yielded important information regarding sensitization profiles in early life and their associations with the development of subsequent allergic disease. The design of these cohorts differs and these differences are critical to the interpretation of the data. Higher rates of sensitization have been established in high-risk cohorts of children who have a family history of allergies and asthma compared to unselected population cohorts. Indeed, the sensitization rate in children aged one year in the high-risk Cincinnati Childhood Air Pollution Study (CCAAPS) was 28% compared to just 8% reported in children aged 1.5 years in unselected birth cohorts1. Epidemiologic studies consistently show an association between atopy and asthma. Atopic dermatitis (AD) is an established risk factor for asthma development and it has been estimated that one-third to half of patients with AD will develop asthma2. However, the sensitization rates and profiles in a cohort of children with AD are not established. We sought to compare the sensitization rates and profiles of children in CCAAPS, a high risk asthma cohort based on parental atopy, and the Mechanisms of Progression of Atopic Dermatitis to Asthma in Children (MPAACH), a high risk asthma cohort based on the presence of AD.
MPAACH is the first US-based prospective early life cohort of children with AD and the first mechanistic AD cohort designed to elucidate endotypes of AD that progress to asthma and identify biomarkers of disease progression. Inclusion criteria were: 1) aged 1–2 years upon enrollment; 2) gestation of ≥36 weeks AND 3) a diagnosis of AD (based on the Hanifin and Rajka Criteria for Atopic Dermatitis3), OR the parent(s)/legal authorized representative (LAR) indicates a positive response to each of the 3 questions from the Children’s Eczema Questionnaire4. CCAAPS is a high-risk birth cohort of infants with at least one atopic parent, defined as symptoms of allergy and/or asthma diagnosis, and a positive skin prick test (SPT) to at least one allergen5. CCAAPS inclusion criteria also included a gestational age of ≥35 weeks. In CCAAPS, the definition of AD was adapted from a validated questionnaire (International Study of Asthma and Allergies in Childhood) and included a parental report of the child’s scratching and redness, “raised bumps,” or dry skin/scaling for at least 6 of the last 12 months6.
Participants in both cohorts had SPTs to aero and food allergens performed as part of the study protocol. Herein we compared the SPT results at age one in both cohorts as age may affect sensitization rates. The CCAAPS cohort was skin tested to a panel of 15 aeroallergens, milk and egg as previously reported5. SPTs in the MPAACH cohort include 11 aeroallergens and 13 food allergens. In this analysis, we directly compare sensitization rates to dog, mold, tree, cat, grass, dust mite, ragweed, egg and milk, which were performed using the same method in both cohorts. Sensitization patterns in MPAACH (n=128) were compared to the overall CCAAPS cohort (n=712), the subset with AD (n=222), and those without AD (n=490). All data and sensitization results were analyzed via Chi squared/Fishers Exact tests using SAS.
Demographic comparisons highlight the distinct recruitment techniques and populations of each high-risk cohort. MPAACH recruitment is conducted at an urban hospital and is comprised of 53% black race participants and 54% public insurance. In contrast, the CCAAPS cohort is a population-based cohort and includes 21% black participants (p<0.01) and 24% public insurance (p< 0.01).
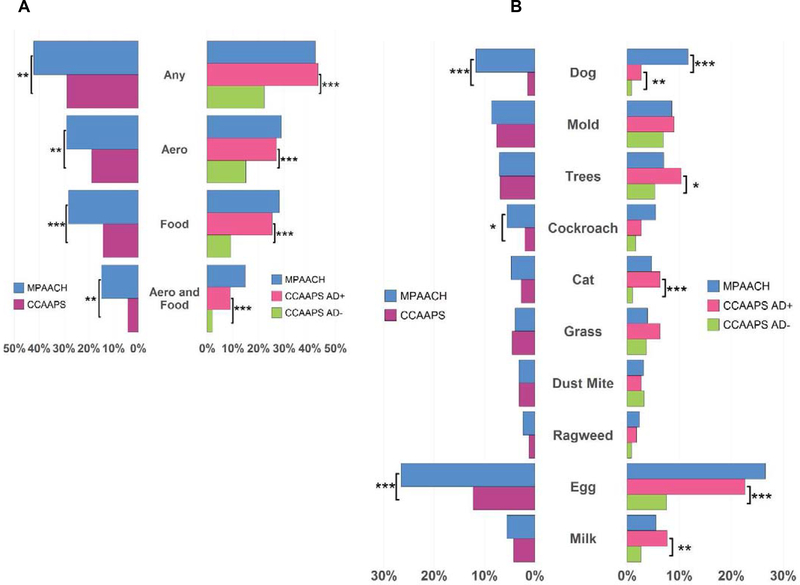
When compared to the CCAAPS cohort, MPAACH children were significantly more likely to be sensitized to any allergen (42.2% vs 28.8%, p = 0.003), co-sensitized to both food and aero allergens (14.8% vs 4.2%, p=0.009), sensitized to food allergens only (28.1% vs 14.2%, p<0.001), and sensitized to aero allergens only (28.9% vs 18.8%, p=0.009, Figure 1A). At the individual allergen level, MPAACH children were also significantly more likely to be sensitized to dog (11.7% vs 1.4%, p<0.001), cockroach (5.5% vs 2.0%, p=0.029), and egg (26.6% vs 12.3%, p=0.001, Figure 1B), highlighting that children with AD are at much higher risk for developing atopy than children in a high-risk asthma cohort based on parental atopy.
Fig 1.
Sensitization rates in the Mechanisms of Progression of Atopic Dermatitis to Asthma in Children (MPAACH) cohort and Cincinnati Childhood Air Pollution Study (CCAAPS). A) Overall rates and aeroallergen and food allergen rates in MPAACH, CCAAPS Atopic Dermatitis (AD)+ and CCAAPS AD−. B) Individual allergen sensitization rates in MPAACH, CCAAPS AD+ and CCAAPS AD−.
In order to determine if AD was indeed driving the higher sensitization rates in MPAACH, we compared sensitization rates in children in CCAAPS with AD (AD+) to those without AD (AD−). As in MPAACH, the CCAAPS AD+ group had higher sensitization rates to any allergen (43.2% vs 22.2%, p<0.001), co-sensitization (9.0% vs 2.0%, p<0.001), food only (25.3% vs 9.2%, p<0.001), and aero only (27.0% vs 15.1%, p<0.001, Figure 1A) compared to the AD− group. The AD+ group had higher rates of sensitization to trees (10.4% vs 5.3%, p=0.014), cats (6.3% vs 1.9%, p<0.001), egg (22.6% vs 7.6%, p<0.001), and milk (7.7% vs 2.7%, p=0.002, Figure 1B). Dog sensitization was also higher in the AD+ group (2.7% vs 0.8%, p=0.048), however, it was significantly lower than the prevalence in MPAACH (11.7%, p = 0.001, Figure 1B).
Herein we show that the sensitization rate in the cohort of pediatric AD is almost 1.5 fold higher than the rate for a high risk asthma and allergy cohort, even though the rate of parental history of allergic disease was highly comparable. These results suggest AD further increases the risk of sensitization over heredity alone. Children from MPAACH and AD+ children from CCAAPS are almost twice as likely to be sensitized to any allergens and almost four times more likely to be co-sensitized to food and aero allergens. Both cohorts had increased sensitization rates when compared to the general population7. The MPAACH children and the CCAAPS children with AD had similar sensitization profiles despite stark demographic differences, supporting that AD independently contributes to increased sensitization risk. While it has been reported that children with AD may develop peanut and egg sensitizations through epidermal allergen exposure,8, 9 our findings suggest cutaneous sensitization of aeroallergens as well. Future analyses of sensitization patterns in the MPAACH cohort will determine which phenotypes of AD are associated with early persistent, early transient, and late transient sensitization in children, and ultimately establish which AD phenotypes and sensitization profiles are most predictive of asthma and clinical allergy development in children.
Acknowledgements
We thank the research participants and their families for participation in the study and the Schubert Research Clinic of the Cincinnati Children’s Hospital Medical Center for assistance with research participants.
Funding: This work was supported by National Institutes of Health grants U19AI070235 and R01ES011170.
Footnotes
COI: The authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Nissen SP, Kjaer HF, Host A, Nielsen J, Halken S. The natural course of sensitization and allergic diseases from childhood to adulthood. Pediatr Allergy Immunol 2013; 24:549–55. [DOI] [PubMed] [Google Scholar]
- 2.Amat F, Saint-Pierre P, Bourrat E, Nemni A, Couderc R, Boutmy-Deslandes E, et al. Early-Onset Atopic Dermatitis in Children: Which Are the Phenotypes at Risk of Asthma? Results from the ORCA Cohort. PLoS One 2015; 10:e0131369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol 1980; 92 (suppl):44–7. [Google Scholar]
- 4.von Kobyletzki LB, Berner A, Carlstedt F, Hasselgren M, Bornehag CG, Svensson A. Validation of a parental questionnaire to identify atopic dermatitis in a population-based sample of children up to 2 years of age. Dermatology 2013; 226:222–6. [DOI] [PubMed] [Google Scholar]
- 5.LeMasters GK, Wilson K, Levin L, Biagini J, Ryan P, Lockey JE, et al. High prevalence of aeroallergen sensitization among infants of atopic parents. J Pediatr 2006; 149:505–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Epstein TG, LeMasters GK, Bernstein DI, Ericksen MB, Martin LJ, Ryan PH, et al. Genetic variation in small proline rich protein 2B as a predictor for asthma among children with eczema. Ann Allergy Asthma Immunol 2012; 108:145–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dharma C, Lefebvre DL, Tran MM, Lou WYW, Subbarao P, Becker AB, et al. Patterns of allergic sensitization and atopic dermatitis from 1 to 3 years: Effects on allergic diseases. Clin Exp Allergy 2018; 48:48–59. [DOI] [PubMed] [Google Scholar]
- 8.Flohr C, Perkin M, Logan K, Marrs T, Radulovic S, Campbell LE, et al. Atopic dermatitis and disease severity are the main risk factors for food sensitization in exclusively breastfed infants. J Invest Dermatol 2014; 134:345–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan SM, Turcanu V, Stephens AC, Fox AT, Grieve AP, Lack G. Cutaneous lymphocyte antigen and alpha4beta7 T-lymphocyte responses are associated with peanut allergy and tolerance in children. Allergy 2012; 67:336–42. [DOI] [PubMed] [Google Scholar]