To the Editor:
In the midst of the worldwide coronavirus disease 2019 (COVID-19) pandemic, health care is seeing an increasing number of COVID-19-positive patients, with cases ranging from mild to fatal. Emerging data indicate that myocardial dysfunction can be detected presumably earlier than clinical decompensation using transthoracic echocardiography. However, the use of echocardiography needs to be balanced against the risk to frontline sonographers of contracting COVID-19. A group of five American Registry for Diagnostic Medical Sonography–certified sonographers volunteered to form a focused cardiac imaging protocol using high-end cardiac ultrasound machines (Table 1 ). Their goal was to answer to the call of critically ill COVID-19-positive patients while preserving protection for sonographers as this pandemic evolves.
Table 1.
Focused cardiac imaging protocol for COVID-19-positive patients
| 2D image | Corresponding measurements | Post-processing |
|---|---|---|
| Parasternal long-axis | LV wall thickness LV internal diastolic diameter |
|
| Parasternal short-axis mid | ||
| Parasternal short-axis apex | ||
| Apical four-chamber | Simpson's biplane | LV longitudinal strain |
| Apical two-chamber | Simpson's biplane | LV longitudinal strain |
| Apical long-axis | LV longitudinal strain | |
| Apical RV-focused view | RV longitudinal strain | |
| RV annular tissue Doppler | RV systolic tissue velocity (S′) | |
| Tricuspid valve color Doppler | TR | |
| Tricuspid valve CW Doppler | TR peak velocity for PASP calculation | |
| IVC | RAP for PASP calculation |
2D, Two-dimensional; CW, continuous wave; IVC, inferior vena cava; PASP, pulmonary artery systolic pressure; RAP, right atrial pressure; TR, tricuspid regurgitation.
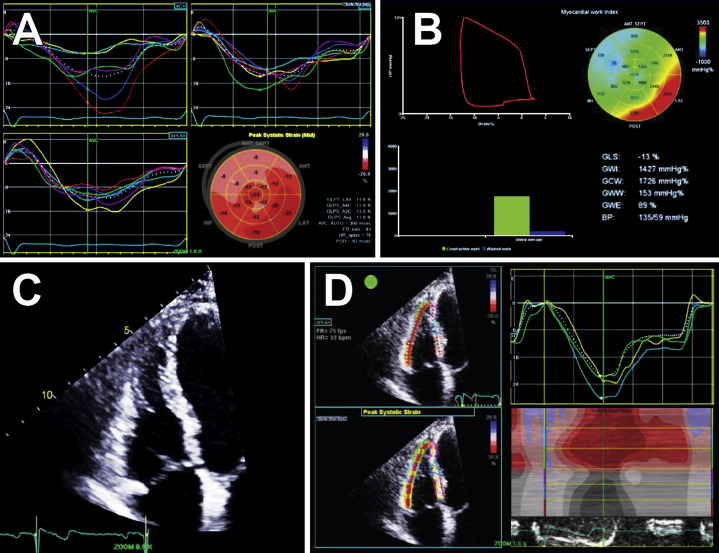
It is essential for intensivists caring for patients with COVID-19 in the intensive care unit to use echocardiography to thoroughly monitor biventricular systolic function as the inflammatory process takes effect. Strain imaging using speckle-tracking has a proven ability to detect a decrease in systolic function before a decline in ejection fraction if image quality facilitates accuracy (Figures 1 A and 1B).1 After pertinent images have been acquired, left ventricular (LV) global longitudinal strain and myocardial work evaluation should be completed outside of the patient room to limit the sonographer's exposure. With regard to more technically difficult patients, contrast imaging may be used to better visualize the endocardial definition.
Figure 1.
Transthoracic echocardiography. Focused-protocol transthoracic echocardiograms for COVID-19-positive patients with (A) LV strain speckle-tracking imaging and (B) myocardial work index performed. (C) Focused RV view from the apical window for (D) RV strain imaging, omitting the septal segments.
Similar to LV function, there are key parameters to the proper investigation of right ventricular (RV) systolic function. It is important to obtain an RV-focused view from an elongated apical four-chamber view (slide more laterally on the patient's chest). Obtaining this image will improve RV free wall endocardial definition, avoid foreshortening, and aid in lengthening the right ventricle from base to apex. Additional RV parameters should include pulmonary artery systolic pressure as well as annular mobility (Doppler tissue imaging) for an overall comprehensive assessment of RV systolic function. In conjunction with the LV evaluation, RV longitudinal strain should be assessed from the acquired RV-focused view after the sonographer leaves the patient room. On the basis of the most recent American Society of Echocardiography and European Association of Cardiovascular Imaging guidelines, the septum should be omitted, and only the free wall segments should be analyzed in the strain calculation (Figures 1C and 1D).2 , 3
The five sonographers limited their exposure while scanning patients who were positive for COVID-19 by following a condensed and focused protocol to determine LV and RV function and evaluate pulmonary artery systolic pressure and using postprocessing techniques. Implementing these recommendations for 38 COVID-19-positive intensive care unit patients, a mean scan time of 15 ± 5.6 min was documented. Decreasing scan times and amount of exposure to the sonographer allowed ample time between patients to don and doff appropriate personal protective equipment and maintain a sonographer rotation to prevent fatigue. Focused cardiac imaging can answer to the call of critically ill COVID-19 patients while minimizing frontline sonographers' exposure. Both sonographer protection and detection of cardiac involvement in life-threatening COVID-19-positive cases are significant components of the evolution of treatment of patients with COVID-19.
Footnotes
Conflicts of interest: None.
References
- 1.Wen H., Liang Z., Zhao Y., Yang K. Feasibility of detecting early left ventricular systolic dysfunction using global area strain: a novel index derived from three-dimensional speckle-tracking echocardiography. Eur J Echocardiogr. 2011;12:910–916. doi: 10.1093/ejechocard/jer162. [DOI] [PubMed] [Google Scholar]
- 2.Lang R.M., Badano L.P., Mor-Avi V., Afilalo J., Armstrong A., Ernande L. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Rudski L.G., Lai W.W., Afilalo J., Hua L., Handschumacher M.D., Chandrasekaran K. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]