Abstract
Background
There is emerging evidence that patients with Latent Tuberculosis Infection(LTBI) and Tuberculosis(TB) disease have an increased risk of the SARS-CoV-2 infection and predisposition towards developing severe COVID-19 pneumonia. In this study we attempted to estimate the number of TB patients infected with SARS-CoV-2 and have severe disease during the COVID-19 epidemic in Delhi, India.
Methods
Susceptible-Exposed-Infectious-Recovered (SEIR) model was used to estimate the number of COVID-19 cases in Delhi. Assuming the prevalence of TB in Delhi to be 0.55%, 53% of SARS-CoV2 infected TB cases to present with severe disease we estimated the number of SARS-CoV2 infected TB cases and the number of severe patients. The modelling used estimated R0 for two scenarios, without any intervention and with public health interventions.
Results
We observed that the peak of SARS-CoV-2-TB co-infected patients would occur on the 94th day in absence of public health interventions and on 138th day in presence of interventions. There could be 20,880 SARS-CoV-2 infected TB cases on peak day of epidemic when interventions are implemented and 27,968 cases in the absence of intervention. Among them, there could be 14,823 patients with severe disease when no interventions are implemented and 11,066 patients with severe disease in the presence of intervention.
Conclusion
The importance of primary prevention measures needs to be emphasized especially in TB patients. The TB treatment centres and hospitals needs to be prepared for early diagnosis and management of severe COVID-19 in TB patients.
Keywords: COVID-19, Epidemic, Mathematical modelling, SARS-CoV-2
Highlights
-
•
Study of its kind estimating the number of SARS-CoV2 infected TB cases during the COVID-19 epidemic in Delhi.
-
•
A mathematical modelling study which used Susceptible-Exposed-Infectious-Recovered (SEIR) model to estimate the number of patients infected with COVID-19.
-
•
The modelling used the estimated R0 for two scenarios, (i) without any intervention and (ii) with public health interventions like lockdown, social distancing, contacts quarantine and case isolation.
-
•
The model estimated that there could be 20,880 SARS-CoV-2 infected TB cases on peak day of epidemic when interventions are implemented and 27,968 cases in the absence of interventions.
-
•
Assuming 53% of the SARS-CoV-2 infected TB cases present with severe disease, it is estimated that there could be 14,823 patients with severe disease when no interventions are implemented.
-
•
With implementation of public health interventions, there could be 11,066 TB patients severe COVID-19 disease.
1. Introduction
The on-going pandemic of COVID-19, a viral pneumonia like illness, emerged in Wuhan, China in December and has since spread across 210 nations.1 Till date (21.4.2020), there have been 2 397 216 confirmed cases and 162 956 deaths due to the disease.2 Most cases SARS-CoV-2 infection has minimal symptoms and are self-limiting. However, it is also well-established that patients with underlying comorbidities especially diabetes, hypertension, coronary heart disease, tuberculosis (TB) and the elderly are at significantly increased risk of complications and death due to COVID-19.3 , 4
Tuberculosis is a bacterial disease predominantly affecting the lung. During 2017, an estimated 10 million new TB disease cases occurred globally,5 while 2.8 million cases were registered in India, the highest in the world.6 Although, TB-related mortality declined from 56/100000/year in 2000 to 32/100000/year but still caused an estimated 1.7 million deaths in 2016 in India.6 Furthermore, the prevalence of latent mycobacterium tuberculosis infection (LTBI) is also very high (40%) in India.7
Even though the portal of entry is upper respiratory tract for both TB and COVID-19, the association between co-infection of severe influenza and pulmonary TB disease remain inconclusive.8 , 9 However, there is emerging evidence that patients with LTBI and TB disease have an increased risk of the SARS-CoV-2 infection and predisposition towards developing severe COVID-19 pneumonia.4 Any relationship of COVID-19 and TB is particularly relevant for the public health system in India since India is one of the major contributors in burden due to TB with highest number of TB cases in the world.5 Also, isolation of cases and contacts for controlling COVID-19 can be problematic in low socioeconomic TB households.10
Under these circumstances and considering the large burden of active tuberculosis patients in India along with localized, hotspot and community transmission of COVID-19, estimation of the infection and morbidity due to COVID-19 epidemic among TB patients in India is warranted. This would also enable allocation of resources towards the development and implementation of effective public health interventions in such vulnerable populations. With this background in this study we attempted to estimate the number of TB patients infected with SARS-CoV-2 and have severe disease during the COVID-19 epidemic in Delhi, India.
2. Materials and methods
The estimations in this study are based on Susceptible-Exposed-Infectious-Recovered (SEIR) model.11 This is a compartmental model which is used to predict the infectious disease epidemic. The model is summarized with the following chart and equations.12
where N is the total population S is the number of susceptible population in the community, E is the number of exposed people, I is the number of infected people, R is the number of recovered people, β is the transmission coefficient, γ is the recovery coefficient. The R0 for COVID-19 was calculated for Delhi by multiplying the population density ratio of Delhi and Wuhan with R0 for Wuhan.12 The Markov's probability model was used to estimate the number of mild/moderate and severe disease.13
Two scenarios were considered to estimate the number of infected COVID-19 cases, (i). Without any public health intervention, (i) With public health interventions like lock down, social distancing and isolation of cases and contacts. The proportion contributed to case pool was 48.5% for household contact, 30.5% for workplace contact, 20.8% for community contact.14 The assumed reduction achieved by the intervention lockdown, social distancing, case and contact isolation was 25% for household contacts, 96% for workplace contacts, and 70% for community contacts. Case isolation was done from day zero in Delhi, lock down was implemented from 20th day of reporting of reporting of the index case till 3rd May 2020 (62nd day). We also assumed that the effect of lockdown and social distancing interventions may be shown after 7 days which is half of maximum incubation period. The effective reproductive rate (Rt) under public health interventions was calculated by multiplying the reduction fractions assumed for the intervention with R0. The parameters used for modelling are provided in Table 1 . The number of notified cases of tuberculosis in 2018 for Delhi was obtained from India Tuberculosis report 2019 and was considered as the estimated prevalence of tuberculosis case in Delhi. The proportion of SARS-CoV-2 infected TB cases with severe disease was considered as 53% as per the results of a study in China.10
Table 1.
Parameters used in SEIR model for COVID-19 outbreak in Delhi.
| Parameters | Value |
|---|---|
| Delhi populationa | 1.9 crore19,20 |
| Date of reporting of index case | 02.03.2020 |
| Incubation period | 5 days8,21,22 |
| Time to recovery | 7 days (mild disease) and 15 days (severe disease)22 |
| Average infectious period | 10 days23 |
| Proportion of asymptomatic cases | 30%24 |
| Proportion of mild/moderate disease among symptomatic cases | 80%22 |
| Proportion of severe disease among symptomatic cases | 20%22 |
| Case fatality rate | 3.8%25 |
| Basic reproductive rate (R0) for Wuhan | 3.2826 |
| Population density of Delhi | 11,32027 |
| Population density of Wuhan | 600012 |
| Estimated R0 for Delhib | 6.18 |
| Notification of tuberculosis cases in Delhi | 505 per 100,000 population6 |
| Proportion of COVID-19 infected TB patients who had severe disease | 53%4 |
Ethics: There are no ethical concerns related to the study since all the data are taken from the official public domains of respective institutions.
3. Results
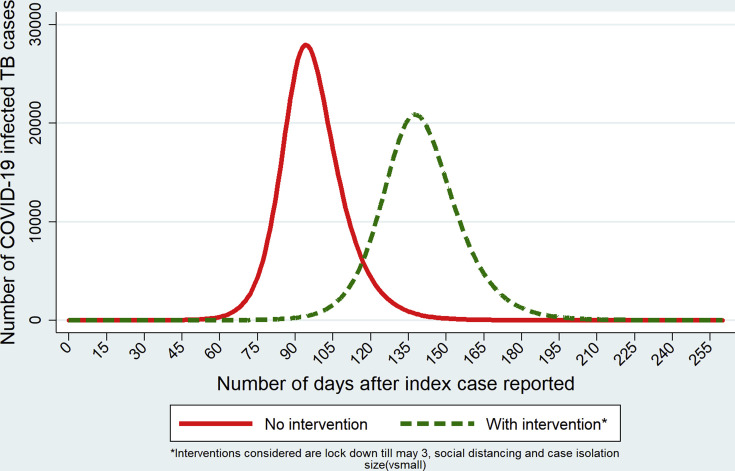
Our study estimated the number of SARS-CoV-2 infected active TB cases during COVID-19 epidemic in Delhi. It was observed that the implementation of public health interventions would delay the peak and leads to flattening of the epidemic curve. We found that the peak of SARS-CoV-2-TB co-infected patients would occur on the 94th day in absence of public health interventions. In presence of effective interventions like lockdown for a period 42 days, social distancing, contact tracing and case isolation, the peak would be delayed by 44 days and occur on the 138th day. The estimated number of SARS-CoV-2 infected TB patients during the epidemic in Delhi is depicted in Fig. 1 . It is estimated that there could be 20,880 SARS-CoV-2 infected TB cases on peak day of epidemic when interventions are implemented and 27,968 SARS-CoV-2 infected TB cases if no interventions were implemented.
Fig. 1.
Estimated COVID-19 infected Tuberculosis patients during the outbreak in Delhi.
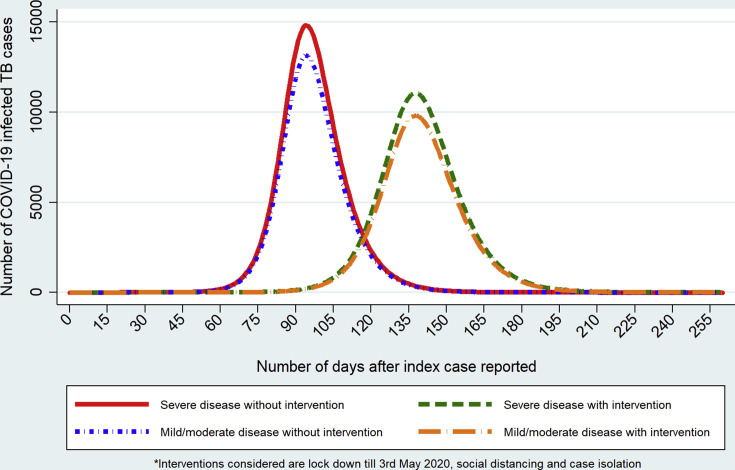
We also observed that on peak day there could be 14,823 patients with severe disease when no interventions are implemented and 11,066 patient with severe disease when the above mentioned public health interventions are implemented (Fig. 2 ). There could be 13,145 SARS-CoV-2 infected TB cases with mild to moderate disease on peak day in the absence of any intervention and 9813 SARS-CoV-2 infected TB cases with mild to moderate disease on peak day on implementing the necessary interventions mentioned above.
Fig. 2.
Estimated COVID-19 infected Tuberculosis patients with severe disease in Delhi.
4. Discussion
The present study estimated the probable peak count of COVID-19 cases among TB patients using SEIR compartmental model. We also estimated the SARS-CoV-2 infected TB patients with mild-moderate disease and severe disease, both in event of public health interventions and their absence respectively. TB patients in developing countries are likely to be undernourished (low BMI) with a weakened immune system which might predispose to superadded infections even in those patients initiated on DOTS but in the early treatment stages.15
The TB patients with COVID-19 are at higher risk of developing severe disease and may become critically ill requiring mechanical ventilation.4 Even with the implementation of public health interventions, we observed there could be 11,066 SARS-CoV-2 infected TB patients with severe disease. There are evidences that 62% of the critically ill patients and 81% of the patients requiring mechanical ventilation had succumbed to death.16
Our results have few implications for the National Tuberculosis Elimination Program (NTEP) of India. First, since the rate of severe COVID-19 is higher among TB patients, the program needs to focus of primary prevention measures like adequate ventilation, queuing with physical distancing of at-least 1 meters and preferable airborne control measures needs to be maintained in all TB care centres to reduce the risk of transmission of SARS-CoV2 infection. Second, the TB patients and their family members needs to be educated on measures to protect against COVID-19 including respiratory hygiene, regular hand washing with soap water, social distancing and avoid touching of the face, mouth and eyes. Third, there is an urgent need for surveillance of TB patients on DOTS anti-tubercular therapy reporting for symptoms of flu-like illness that could be suggestive of COVID-19 disease. Particular attention is required for TB cases reporting with acute breathlessness which can be symptomatic of severe COVID-19 disease. Furthermore, ensuring continuing of DOTS by provision of timely refills to patients with TB to fulfil obligations under the universal health care requirements is required. This would also potentially reduce their susceptibility to SARS-CoV2.17 Resolution of any TB drug related stock-outs or associated procurement challenges warrant urgent prioritization.17
The strength of our study is that we used SEIR model to estimate the number of infected patients with COVID-19 which will help the policy makers to design effective public health strategies to control the epidemic. SEIR model is a compartmental model and assumes closed population which might be violated in the actual scenario.18 However, because of lockdown the migration is effectively controlled in Delhi. The results of the study needs to be interpreted with caution since the estimation of excess risk of severe disease of COVID-19 in TB patients was based on a study in China having a small sample size.4 However, due to lack of other studies from high burden TB countries we used the results of this study.
The prevalence of TB in general population might not be the same as the prevalence of TB in COVID-19 patients. However because of the limited evidences related to the increased risk of COVID-19 among tuberculosis patients, the study used the above assumption.
In conclusion, our study estimated that even with implementation of public health interventions, 20,880 SARS-CoV2 infected TB cases and among them, 11,066 patients might present with severe disease during peak days of the epidemic curve and have high risk of mortality. So, the importance of primary prevention measures needs to be emphasized especially in TB patients. The TB treatment centres and hospitals needs to be prepared for early identification and management of COVID-19 in TB patients.
Conflicts of interest
The authors have none to declare.
References
- 1.Coronavirus Resource Center. 2020. https://coronavirus.jhu.edu/map.html [Internet] [cited 2020 Apr 25]. Available from: [Google Scholar]
- 2.World Health Organization . 2020 Apr. Coronavirus Disease 2019 (COVID-19) Situation Report – 92.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200421-sitrep-92-covid-19.pdf?sfvrsn=38e6b06d_4 [Internet]. Geneva [cited 2020 Apr 22]. Available from: [Google Scholar]
- 3.Guan W., Liang W., Zhao Y. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020 Mar 26:2000547. doi: 10.1183/13993003.00547-2020. https://erj.ersjournals.com/content/early/2020/03/17/13993003.00547-2020 [Internet] [cited 2020 Apr 25] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Y., Bi L., Chen Y. Active or latent tuberculosis increases susceptibility to COVID-19 and disease severity. medRxiv. 2020 Mar 16 2020.03.10.20033795. [Google Scholar]
- 5.World Health Organization . 2019. Global Tuberculosis Report-2019.https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1 [Internet]. Geneva [cited 2020 Apr 26]. Available from: [Google Scholar]
- 6.Central TB Division . 2019 Jun. India TB Report 2019.https://tbcindia.gov.in/WriteReadData/India-TB-Report 2019.pdf [Internet]. New Delhi [cited 2020 Apr 17]. Available from: [Google Scholar]
- 7.Chadha V.K. vol. 9. 2005. Tuberculosis epidemiology in India: a review; pp. 1072–1082. (International Journal of Tuberculosis and Lung Disease). [PubMed] [Google Scholar]
- 8.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Jan 29;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walaza S., Cohen C., Tempia S. Influenza and tuberculosis co-infection: a systematic review. Influenza Other Respi Viruses. 2020 Jan 1;14(1):77–91. doi: 10.1111/irv.12670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hellewell J., Abbott S., Gimma A. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020 Apr 1;8(4):e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mandal S., Bhatnagar T., Arinaminpathy N. Prudent public health intervention strategies to control the coronavirus disease 2019 transmission in India: a mathematical model-based approach. Indian J Med Res. 2020 Mar 23 doi: 10.4103/ijmr.IJMR_504_20. http://www.ncbi.nlm.nih.gov/pubmed/32202261 [Internet] [cited 2020 Apr 23]. [Epub ahead of print]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rocklöv J., Sjödin H., Wilder-Smith A. COVID-19 outbreak on the Diamond Princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures. J Trav Med. 2020 Feb 28:aaa030. doi: 10.1093/jtm/taaa030. https://academic.oup.com/jtm/article/doi/10.1093/jtm/taaa030/5766334 [Internet] [cited 2020 Apr 16] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yaesoubi R., Cohen T. Generalized Markov models of infectious disease spread: a novel framework for developing dynamic health policies. Eur J Oper Res. 2011 Dec 16;215(3):679–687. doi: 10.1016/j.ejor.2011.07.016. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3182455/ [Internet] [cited 2020 Apr 16] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Milne G.J., Baskaran P., Halder N., Karl S., Kelso J. Pandemic influenza in Papua New Guinea: a modelling study comparison with pandemic spread in a developed country. BMJ Open. 2013;3(3):1–10. doi: 10.1136/bmjopen-2012-002518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.John Waitt Catriona, Peter N., Banda K. Early deaths during tuberculosis treatment are associated with depressed innate responses, bacterial infection, and tuberculosis progression. J Infect Dis. 2011 Aug 1;204(3):358–362. doi: 10.1093/infdis/jir265. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3132140/ [Internet] [cited 2020 Apr 24] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Resp Med. 2020 May;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30079-5/fulltext [Internet] [cited 2020 Apr 26]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO . 2020 Apr. World Health Organization (WHO) Information Note Tuberculosis and COVID-19 COVID-19: Considerations for Tuberculosis (TB) Care.https://www.who.int/tb/COVID_19considerations_tuberculosis_services.pdf [Internet] [cited 2020 Apr 19]. Available from: [Google Scholar]
- 18.Vynnycky E., White R.G. 1st ed. Oxford University Press; 2010. An Introduction to Infectious Disease Modelling; p. 370. [Google Scholar]
- 19.Census of India 2011 . 2011. Provisional Population Totals NCT of Delhi.http://censusindia.gov.in/2011-prov-results/data_files/delhi/3_PDFC-Paper-1-tables_60_81.pdf [Internet]. Mumbai [cited 2020 Apr 16]. Available from: [Google Scholar]
- 20.Census of India . 2019. Sample Registration System Statistical Report 2019.http://censusindia.gov.in/vital_statistics/SRS_Bulletins/SRS_Bulletin-Rate-2017-_May_2019.pdf [Internet] Available from: [Google Scholar]
- 21.WHO . 2020 Apr. Coronavirus Disease 2019 (COVID-19) Situation Report-73.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200402-sitrep-73-covid-19.pdf?sfvrsn=5ae25bc7_6 [Internet]. Geneva [cited 2020 Apr 16]. Available from: [Google Scholar]
- 22.Adhikari S.P., Meng S., Wu Y.-J. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Pov. 2020 Mar 17;9:29. doi: 10.1186/s40249-020-00646-x. http://www.ncbi.nlm.nih.gov/pubmed/32183901 [Internet] [cited 2020 Mar 26]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Y., Yan L.-M., Wan L. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30232-2. https://www.thelancet.com/action/showPdf?pii=S1473-3099%2820%2930232-2 [Internet] Mar 19 [cited 2020 Apr 16]. [Epub ahead of print]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nishiura H., Kobayashi T., Suzuki A. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020 Mar 14;94:154–155. doi: 10.1016/j.ijid.2020.03.020. doi: 10.1016/j.ijid.2020.03.020. [Internet] [cited 2020 Apr 16]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.WHO . 2020 Feb. Coronavirus Disease 2019 (COVID-19) Situation Report-30.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200219-sitrep-30-covid-19.pdf?sfvrsn=3346b04f_2 [Internet] Geneva [cited 2020 Apr 16]. Available from: [Google Scholar]
- 26.Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Trav Med. 2020;27(2):1–4. doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Census of India 2011 . 2011. 7. Density of Population.http://censusindia.gov.in/2011-prov-results/data_files/india/Final_PPT_2011chapter7.pdf [Internet] [cited 2020 Apr 20]. Available from: [Google Scholar]