Abstract
The Coronavirus (COVID-19) pandemic has resulted in over 4.5 million confirmed cases and over 300,000 deaths. The impact of COVID-19 on surgical practice is widespread, ranging from workforce and staffing issues, procedural prioritisation, viral transmission risk intraoperatively, changes to perioperative practice and ways of working alongside the impact on surgical education and training. Whilst there has been a growing literature base describing the early clinical course of COVID-19 and on aspects of critical care related to treating these patients, there has been a dearth of evidence on how this pandemic will affect surgical practice.
This paper seeks to review the current evidence and offers recommendations for changes to surgical practice to minimise the effect of the COVID-19 pandemic.
Keywords: Novel coronavirus, COVID-19, Surgery
Highlights
-
•
COVID-19 has a broad impact on surgical practice including in case prioritisation, operative technique and workforce planning.
-
•
Telemedicine virtual clinics are to be encouraged where possible.
-
•
Elective and non-urgent surgeries must be postponed.
-
•
Consider safe non-surgical management of patients.
1. Introduction
Following a number of cases of pneumonia of unknown origin in Hubei Province in China, Severe Acute Respiratory Syndrome Coronavirus-type 2 (SARS-CoV-2) was identified as the RNA virus causing ‘Coronavirus Disease 2019’ (COVID-19). This virus rapidly spread throughout the world and was recently declared a pandemic by the World Health Organisation (WHO) on March 11, 2020 [[1], [2], [3], [4]], impacting many sectors as well as leading to global socio-economic implications [5].
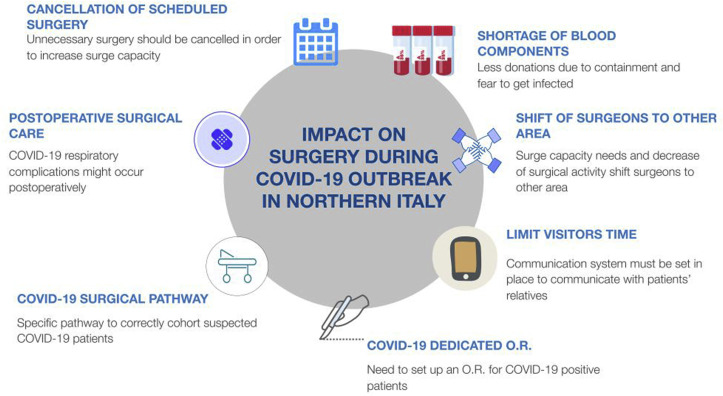
The impact of COVID-19 on surgical practice is widespread ranging from workforce and staffing issues, procedural prioritisation, viral transmission risk intraoperatively as well as impact on surgical education (Fig. 1 ).
Fig. 1.
Impact on surgical practice. Reprinted by permission from Wolters Kluwer [6] Copyright (2020).
Whilst there has been a growing literature base describing the early clinical course of COVID-19 [7] and on aspects of critical care related to treating these patients, there has been a dearth of evidence on how this pandemic will affect surgical practice.
Both Brindle et al. [8] and the COVIDSurg Collaborative [9] have identified key areas where practice should be altered during the COVID-19 pandemic for safe global surgical care. These include:
-
1.
Preparing a surgical pandemic response plan for this rapidly evolving situation to include postponing elective operations, repurposing operating rooms (OR) as critical care areas and operative workflow
-
2.
Develop a clear team-based plan for providing an essential emergency surgical service during the pandemic
-
3.
Staff education on personal protective equipment (PPE) and COVID-19 management to deliver surgery safely during the pandemic
-
4.
Recognising and managing COVID-19 infections whilst decreasing exposure of health care staff
-
5.
Develop a dedicated COVID-19 operating space as part of a wider hospital response
This paper seeks to review the current evidence and offers recommendations for practice in the implementation of these areas.
There are different considerations for each speciality with regards to the prioritisation of surgical services and delivery of surgical practice. These have been outlined in part 2.
2. Changes to surgical systems
2.1. Usage of surgical facilities
The critical care bed capacity in the United Kingdom (UK) compares poorly with other countries in Europe. For example, a comparison between the UK and Germany shows a difference in Intensive Care Unit (ICU) bed numbers of 7.5 versus 31.8 per 100,000 population, respectively [10]. Moreover, predictions made by the Imperial College COVID-19 Response Team indicate a critical care bed demand of more than 30 times the UK capacity [11].
Consequently, the UK National Health Service (NHS) hospitals have been reconfigured in order to provide more space for critically-ill patients in anticipation of greater surges of COVID-19 cases. To date, 33,000 hospital beds have been freed up and 1,200 ventilators have been provided by the private sector. Elective and other routine operations have been cancelled or postponed, allowing access to the OR and the recovery rooms to be used as critical care units [12,13] with a potential model being set up by a commercial team, COVIDvent [14].
2.2. Redeploying staff
Considering the large numbers of anticipated critically ill patients, pressure has also been put on increasing the number of appropriately trained medical staff to care for these patients. Guidelines have been published by the NHS with recommendations on staffing frameworks for critical care of patients and on the deployment of medical staff to meet the critical care capacity surge [15].
Elective and non-urgent surgery cancellations mean that surgeons can play a key role and contribute to the critical care of these patients. Specifically, surgeons can carry out line insertions and proning of patients while ensuring safety of the airway and management of infusions and lines [15]. Other healthcare staff with OR experience such as nurses and allied healthcare workers can provide critical care nursing [16].
The Royal College of Surgeons of England (RCS) has set a number of priorities for adapting the surgical workforce [17]. It is of primary importance to maintain other non-COVID emergency surgery pathways with competent surgical staff and virtual support with teleconferencing from specialists for the generic surgeon and virtual outpatient clinics to minimise exposure. Secondary priority is to protect and preserve the surgical workforce with the appropriate use of PPE, alongside adequate rest and psychological support where necessary. A lower importance has been set for fulfilling alternate surgical and non-surgical roles. The adapting roles of individual surgeons can be divided into current practice, “on the edge” practice, and “beyond the edge” practice (Fig. 2 ).
Fig. 2.
The adapting role of individual surgeons during the COVID-19 pandemic [17].
For surgical staff who need to work beyond their competencies, the RCS has recommended that their extended scope of practice should depend on the specific local needs identified. The recommendations emphasise the need for appropriate training, support and collaboration with appropriately trained colleagues to allow best possible patient care. The same recommendations apply for retired surgeons and trainees who temporarily return to practice [18].
A strategy to minimise the risk of acquiring COVID-19 infection while managing the critical care of patients is to reorganise the surgical team into two groups. One that is active within hospitals, and one that works remotely in isolation, both groups alternating with each other at 2-week intervals. This will ensure that any symptoms are identified within the incubation period of COVID-19 [19].
An alternative strategy is to consolidate the surgical teams in each day into two teams working long (e.g. 12 h) shifts using each available operating room in turn (rather than to complete the whole day's list in a single OR) to allow maximum time for deep cleaning of each OR and minimise the amount of staff in a department who could be potentially exposed [20].
2.3. Oncological work
During the COVID-19 pandemic elective operating services will be greatly restricted, with the exception of cancer cases requiring surgical management.
Stratification of patients into groups is crucial in order to prioritise the workload and offer the best available treatment under the circumstances while simultaneously preserving resources to enable the battle against the deadly virus. NHS England recommends patients be classified into priorities 1–3 based on clinical need [21]:
Priority 1 patients should be further divided into 1a and 1b.
1a being patients requiring an emergency operation within 24 h in order to preserve life; and 1b to include patients with acute conditions secondary to their underlying issue which may cause irreversible harm if not operated on urgently i.e. within 72 h. Situations included in the 1b classification may include gastrointestinal obstructions, bleeding or spinal cord compression among others.
Priority 2 patients should include patients aimed to be operated on within 4 weeks with the intention of cure and prevention of progression of the disease to an inoperable stage. These patients should be stratified based on clinical urgency, expected secondary complications and the specific growth rate of the specific cancer. The NHS also recommends that complications be controlled utilising interventional radiological or gastroenterological procedures (e.g. stents) in cases where operative intervention has been postponed.
Priority 3 patients are classified as those whose operations can be deferred for 10–12 weeks without negative consequences.
The American College of Surgeons also stresses the importance of cancer care coordination. It recommends the establishment of triage criteria based on prevalence of the disease in the area as well as the availability of non-surgical alternatives [22].
The College has classified the cancer workload into 3 phases based on hospital COVID-19 status (Table 1).
Table 1.
American College of Surgeons hospital phases.
| Phase One: Semi-Urgent Setting (Preparation Phase) |
Hospital status:
|
|
Aim: Surgery to be prioritised for patients whose survival will be affected if they don't receive an operation within 3 months. |
| Phase Two: Urgent Setting (Preparation Phase) |
Hospital status:
|
Aim:
|
| Phase Three |
Hospital status:
|
Aim:
|
2.4. Outpatient clinics and telemedicine
During the COVID-19 pandemic, face-to-face outpatient appointments should be avoided where possible. This is because it increases the risk of infection for both the patient as well as the medical professional conducting the clinic.
Where face-to-face appointments are still essential, the recommendation is to follow a one-patient one-room policy to minimise risk of infection. However, telephone and video appointments are preferred where possible. Virtual clinics have run successfully for many years [[23], [24], [25]], but during the COVID-19 pandemic regulations have been eased to allow greater usage [26].
There are a number of methods in use in the UK such as NHS Attend Anywhere as well as those conforming to USA HIPAA regulations such as Zoom, Microsoft Teams and Doxy. However where this is not available, it is also acceptable to use video conferencing tools such as Skype, WhatsApp, Viber and Apple FaceTime [27].
Conor et al. [26] suggest that the stages of setting up a telemedicine clinic are:
-
1.
Identifying patients who are suitable for a telemedicine clinic
-
2.
Informing patients and giving instructions on access. A locally modified patient information sheet is recommended, such as the sheet set up in Norwich and Norfolk University Hospitals in the UK [28].
-
3.
Choosing an appropriate platform
-
4.
Documentation and coding for appropriate remuneration [29].
As many clinicians are uncomfortable with the use of telemedicine clinics, some recommendations for setting up a service are outlined in Table 2 .
Table 2.
| Internal simulation of different platforms to find what works for your service. Have a dedicated technology facilitator in the department to set up the service |
| Consent patients adequately and ensure telephone numbers are up to date as a backup to video clinics |
| Create a personalised link to your ‘room’ rather a numbered ID or code |
| Set up a virtual waiting room that informs patients where they are in the queue |
Physical room:
|
| Load any documents or imaging prior to starting the consultation to avoid disruption |
| Set up a ‘Virtual Background’ such as an image of the hospital or of your usual clinic room. This provides the patient with continuity and reassurance as well privacy for your surroundings. |
Starting a consultation:
|
During the consultation:
|
After the consultation:
|
| Complete documentation in the normal way and record that the consultation was performed over a virtual platform |
3. Procedural considerations
The COVID-19 outbreak has also necessitated global surgical workforce repurposing and reconfiguration [36]. Alongside hospitals being advised to urgently discharge all medically fit patients, authority institutions such as NHS England have instructed the suspension of all non-urgent elective surgeries for at least 3 months [37]. Similar measures have been invoked in other affected countries. These measures are intended to maximise critical care capacity, in order to mitigate the anticipated sharp increase of cases [38]. In England, this is predicted to increase capacity of general and acute beds from 100,000 to 130,000 [12].
Indeed, modelling by the Imperial College COVID-19 Response Team predicted an 8-fold overwhelmed critical care system notwithstanding the most drastic protective measures (i.e. case isolation, home quarantine, and social distancing of over 70s) [11]. Thus, the UK government is taking further measures to increase capacity such as acquiring up to 8,000 beds from independent hospitals and building multiple field hospitals capable of housing up to 4,000 beds each [39,40].
The first surgical priority of healthcare systems is the maintenance of emergency capabilities, including major trauma [12]. As staffing deficiencies are likely due to the self-isolation of clinicians, the protection and preservation of the surgical workforce is critical for upholding the provision of emergency services.
The considerations for optimal protection of the surgeon can be compartmentalised into five domains: (1) the use of PPE, (2) pre-operative risks such as during intubation, (3) specific operative risk issues, (4) post-operative risks, and (5) keeping others safe.
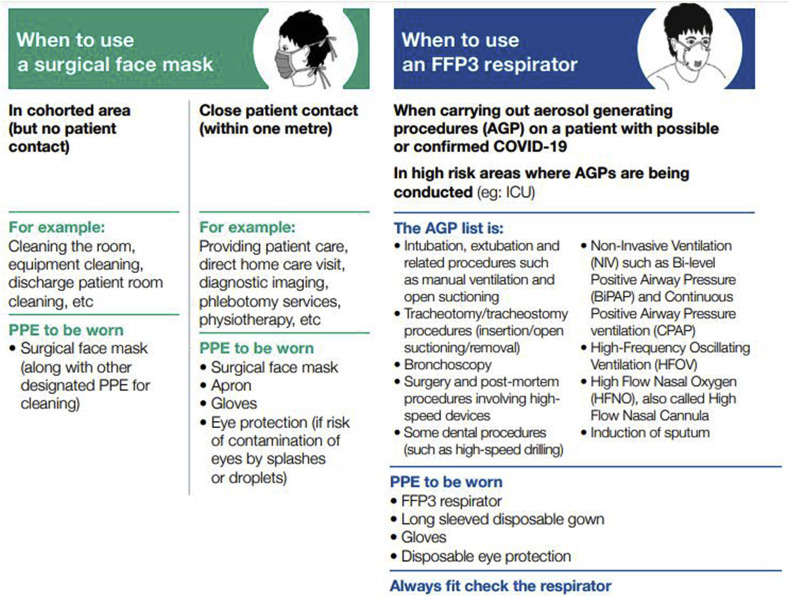
3.1. Personal protective equipment
There are four identified modes of transmission for the COVID-19 virus: contact, droplet, airborne, and faeco-oral [18].
Thus, advisory bodies such as the United States of America (USA) Centres for Disease Control (CDC) and Public Health England (PHE) have recommended the utilisation of PPE for all procedures involving a patient with confirmed or suspected COVID-19 infection [41]. For procedures involving an aerosol-generating procedure (e.g. intubation and extubation) a higher level of protection such as N95 respirators are advised with a paramount emphasis on fit testing (Fig. 3 ) [42]. This is supported by a number of studies suggesting a relationship between viral dose and severity of disease [43]. The specific method of discarding disposable equipment should be in accordance with local policy, followed by hand hygiene [44]. In order to minimise human error, the CDC has advised a trained observer, with the sole responsibility of ensuring adherence to correct procedure, to supervise the donning process. This involves verbally walking through the procedural checklist, concluded by visual confirmation and official documentation.
Fig. 3.
PHE guidance on appropriate use of PPE [42].
3.2. Pre-operative risks
The risk of COVID-19 transmission through aerolisation and droplets are important considerations for surgical personnel. This was highlighted during the 2003 SARS-CoV outbreak which resulted in a preponderance of frontline healthcare workers demonstrating significantly increased risk of contraction and thus illness and death [45]. Additionally, the COVID-19 outbreak also has reported cases emerging in the medical staff population with 29% of nosocomial infections in the Wuhan University Central South Hospital being in staff [46]. Procedures which are believed to generate aerosol include: bronchoscopy, endotracheal intubation, tracheostomy procedures, cardiopulmonary resuscitation, and diagnostic sputum induction [47,48]. Surgical personnel are at an increased risk when conducting procedures which involve the aspiration of body fluids [49] and this is highlighted in the algorithm developed by Forrester et al. [50] for institutional protection of surgical staff.
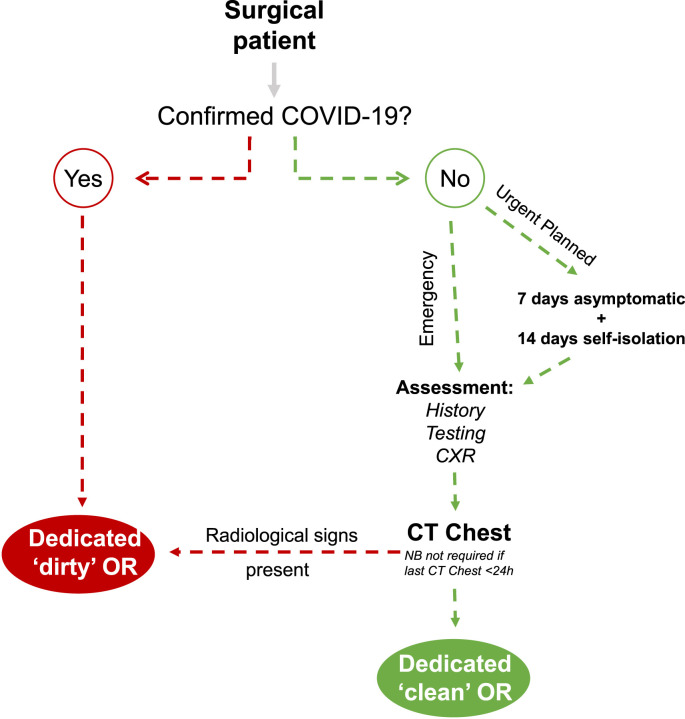
The UK Royal Surgical Colleges advise that any patients for prioritised planned surgery must have been asymptomatic for 7 days, self-isolated for 14 days and then have a negative swab within 48 h prior to planned admission as well as to be assessed for COVID-19 (Fig. 4 ). Furthermore, where the patient is likely to require level 2 or 3 critical care post cancer surgery (High Dependency Unit or ICU), they should be assessed with a CT chest [51].
Fig. 4.
Any patients presenting to hospital requiring urgent or emergency surgery should be assessed for COVID-19 using history, RT-PCR COVID-19 testing and chest x-ray. Any patient receiving an emergency abdominal CT scan for acute pain, should also receive a High resolution CT chest (unless a previous scan performed in the past 24 h) at the same time to exclude COVID-19.
In order to minimise the risk of transmission, the CDC advises removal of non-essential surgeons and personnel from the operating room during aerosol generating procedures [53]. For example, when dealing with a confirmed or suspected COVID-19 case, non-essential personnel should wait outside the OR whilst anaesthesia induction and intubation are completed. Additionally, even essential staff should be screened for temperature before entry into the OR [54]. For quick and safe induction of anaesthesia during Caesarean section, Chen et al. [55] used 5 min of preoxygenation with 100% oxygen, rapid inhalation of sevoflurane (8% in 100% oxygen) concurrent with cricoid pressure followed by 2–3 min of ventilation and intravenous 2% lidocaine (1–1.5 mg/kg), remifentanil (1–2 mg/kg) and succinylcholine (1–2 mg/kg).
Ergonomics are also crucial to infection control. Amongst other evidence-based perioperative guidelines, Dexter et al. [20] suggesting double gloving during induction and placing alcohol or chlorhexidine hand rub on the IV pole to the left of the anaesthetist and a wire basket lined with a zip closure plastic bag to the IV pole on their right as a designated dirty area to place contaminated instruments such as laryngoscopes. Moreover, they suggest using nasal povidone iodine and oral chlorhexidine decolonisation [56].
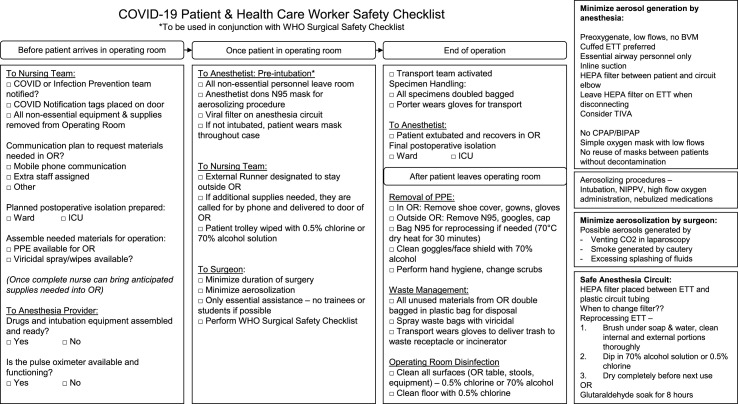
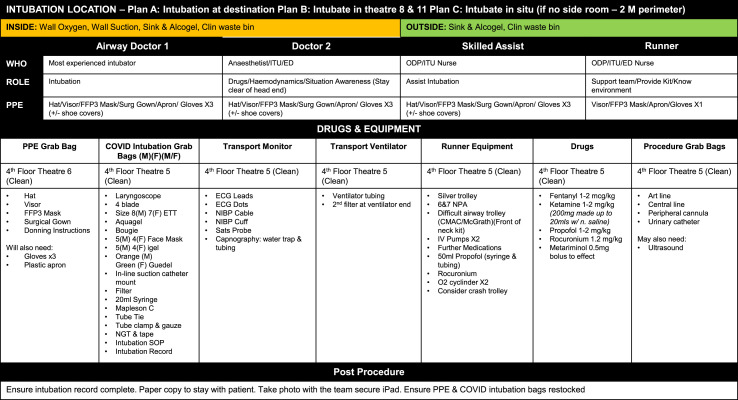
It is also recommended that a COVID-19 modified version of the WHO Safety Surgery Checklist should be used (Fig. 5 ) as well as intubation checklists of which there is a multitude [57,58]. Furthermore, the designation of dedicated PPE donning and doffing areas can reduce cross-contamination and many editable templates are available for local modification [59,60].
Fig. 5.
COVID-19 patient and health care worker safety checklist [61].
Furthermore, one recommendation is to produce pre-prepared bags of equipment (Fig. 6 ) to avoid contaminating general equipment stores [59]. These can include intubation sets (such as laryngoscopes and airway devices), intravenous access sets, transportation monitoring sets (such as blood pressure and ECG equipment) and regularly used drug sets (such as muscle relaxants and sedatives).
Fig. 6.
COVID-19 Surgical unit equipment list in the Royal London Hospital [62].
Finally, Wong et al. [59] also wrapped all ‘high-touch’ equipment such as monitors, nursing station and anaesthetic workstation to avoid repeated contamination.
Furthemore, changes can be made to the OR ventilation system to minimise risk. Advancements in computational fluid dynamics have enabled evaluation of OR ventilation design and monitoring procedures [63] and this in turn has established several principles relating to the design of ORs.
Firstly, ventilation applies a dilution effect which minimises the concentration of contaminants, including viruses and thus it is recommended that in patients with COVID-19, the OR is set to have a high frequency of air flow changes (≥25 per hour) to maximise this effect on reduction of viral load [59].
Secondly, contaminant diffusion is further minimised by introducing low-velocity airflow directed towards the exhaust outlets. Moreover, personnel in adjacent areas will benefit from negative pressurisation in ORs as this functions as a filtration barrier and so negative pressurisation ORs is now an official recommendation of the CDC.
3.3. Intra-operative risks
There are a number of measures that must be undertaken to protect essential members of the operating team during an operation.
Surgical teams managing the early wave of infection in China produced comprehensive guides to the intraoperative management of surgical patients including the recommendation that if electrocautery is used, to use on the lowest power setting with a smoke evacuator to minimise the exposure to surgical smoke and any potential aerosolised virus particles [54,64]. Furthermore, surgical practitioners should pay extra attention to any needlestick injuries or damage to PPE during the procedure.
PHE [65] have also suggested using well-known protocols for infectious patients undergoing surgical procedures and modifying for those suspect of suffering from COVID-19 to include:
-
•
Placing a surgical mask on the patient during transfer to and from the OR
-
•
The patient being anaesthetised and recovered in the OR rather than an anaesthetic room. This should also be undertaken by staff wearing FFP3 respirators and full gowns if this will involve aerosol-generating procedures (AGPs) such as intubation
-
•
Single-use instruments wherever possible
-
•
Surgical instruments to be decontaminated in the normal method
-
•
Staff to be reduced to only the minimum required with no unnecessary visitors
-
•
To place all operations on patients with confirmed or suspected COVID-19 at the end of the list where possible
3.4. Laparoscopy/endoscopy
There is a theoretical risk of transmission of SARS-CoV-2 during laparoscopy as it is an aerosol generating procedure and that other viruses have been detected in surgical smoke [67,68]. Additionally, it has been suggested by Tao et al. [69] that laparoscopy should be avoided due to artificial pneumoperitoneum potentially causing increased airway pressure, CO2 retention, and decreased lung compliance in patients with reduced lung volume, which is not conducive to postoperative functional lung recovery however it is possible to mitigate the risk from laparoscopy [70].
Zheng et al. [71] report their experiences of minimally invasive surgery in China and Italy and recommend using minimally-feasible insufflation pressures and liberal intraperitoneal suction usage as well as to minimise use of the Trendelenburg position to further minimise the risk of pulmonary complications of the pneumoperitoneum.
Furthermore, the Royal Surgical Colleges of Great Britain advise that laparoscopy should only be performed in select cases where it can be clinically justified considering the risk of viral transmission to surgical staff [52].
The Society of American Gastrointestinal and Endoscopic Surgeons recommend that incisions be made as small as possible to minimise leakage, that insufflation pressures are kept to a minimum and that smoke evacuation systems should be utilised [72], and that CO2 insufflation must be turned off and vented through a filter before the removal of specimens, trocars or port closure [73,74]. Considerations are similar during endoscopic procedures for the use of ‘clean’ ORs and filtration devices as well as for only to be performed where urgent. Additionally, in endourological surgeries, irrigation fluid should be collected in a closed system.
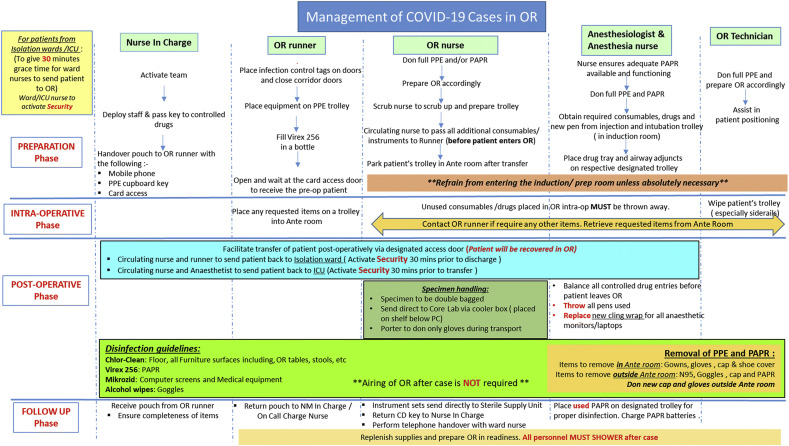
3.5. Post-operative risks
Patients should be recovered in the OR as part of an alteration of the usual patient flow, both to minimise risk of spread as well as due to the repurposing of the usual surgical recovery area (Fig. 7 ). Patients should also be given a single dose of 5-HT3 antagonist (such as ondansetron or metoclopramide) to minimise postoperative nausea and vomiting which could lead to further spread [75].
Fig. 7.
OR anaesthesiologist workflow for COVID-19 cases. Reprinted by permission from Springer [66], Copyright (2020).
Surgical specimens must be labelled as suspected COVID-19 and sealed in the OR in addition to all body fluids, disposable equipment, tubing, gowns and PPE should be double-bagged, labelled with a sign designating as from an OR with confirmed/suspected COVID-19 patient and disposed of according to local infectious waste guidelines.
Following this, the OR must be disinfected according to local protocols which may include the disinfection of high-touch surfaces such as the operating table and anaesthetic machine with a minimum of 75% alcohol or chlorine-based disinfectant. Furthermore, other surfaces in the OR are to be thoroughly cleaned after each operation with a neutral detergent followed by a chlorine-based solution with a minimum strength of no less than 1000 ppm of chlorine. This is especially important as without proper decontamination, the virus can survive on surfaces for a long time [76]. Conventionally ventilated ORs are not to be used for 20 min post-procedure, or 5 min if ultraclean ventilation is used [65,75]. This is due to the fact that one ventilation system air exchange is thought to reduce viral load by 63% and after 5 air changes, less than 1% of airborne contaminant remains [65].
Furthermore, personnel involved in the transportation of confirmed or suspected COVID patients should be minimised to essentials as well as the provision of a dedicated route for the transfer of suspected COVID-19 patients. Then, all members of the transportation team should wear different PPE to what was donned during the procedure as well as for the patient to wear a respirator or surgical mask during transfer, according to local protocols.
Patients should be monitored carefully in the post-operative phase as there are indications that previously undiagnosed COVID-19 may complicate post-operative recovery [77]. Postoperative pulmonary complications are not uncommon and it is important to consider COVID-19 as part of the differential diagnoses alongside aspiration pneumonia or pulmonary emboli and to perform the appropriate diagnostic workup.
Additionally, it is common in many surgical systems for patients after major surgery to be electively admitted to critical care routinely to monitor for post-operative complications. Typically, these patients have short lengths of stay, with one large study showing median length of stay of 0.9 days (IQR 0.8–1.5) and low mortality [78] and there is some evidence that additional critical care support may be harmful or futile [79]. With severe strain on the capacity of critical care units, it would be prudent to carefully rationalise elective planned ICU admissions and whether it is required.
Finally, at the time of writing, large-scale cohort studies on post-operative patients during the COVID-19 pandemic have not yet been published, however Lei et al. [80] report on the clinical characteristics and outcomes in 34 surgical patients in Wuhan City, Hubei Province, China, who were operated on in the early incubation period of the COVID-19 pandemic in January 2020.
Of those, the majority were oncological cases as well as five caesarean sections but none of the patients demonstrated COVID-19 symptoms prior to surgery.
The median time from surgery to first sign or symptom was 2.5 days and seven days from surgery to dyspnoea, 32.4% later developed ARDS and 2/34 patients developed an acute kidney injury. 7 patients later died following admission to critical care units post surgery. Furthermore, the authors demonstrated that the proportion of patients requiring critical care support (44.1%) was higher than the general population of patients hospitalised with COVID-19 (26.1%) indicated the possibility that surgery may accelerate or exacerbate previously undiagnosed COVID-19. This was a small study but does demonstrate the need for close monitoring in the postoperative period of all patients during this pandemic.
3.6. Keeping others safe
Many workers on the frontline share their places of residence (e.g. family or individuals residing within the same flat or apartment) thus there exists an understandable anxiety about passing the infection on. Exact policies regarding post-operative actions for personnel involved in the surgical procedure differs from hospital to hospital. However, it is generally advisable to seal your clothes in a bag upon arriving at the hospital and having a shower before putting them back on to go home.
Although hospitals and healthcare institutions may offer accommodation to workers who live with vulnerable individuals (e.g. the elderly and immunocompromised), this is not a feasible option for all. Alongside the previous measures mentioned (i.e. hand hygiene, changing clothes) workers must be aware that they are exposed more frequently to other possibly contaminated surfaces (e.g. ATM, petrol pumps) compared to persons in self-isolation. It is thus important to have a heightened sense of caution regarding hygiene methods. (e.g. frequency of hand hygiene, wiping phones, minimising non-essential travel). Furthermore, the absolute reduction of physical contact with family and friends should be considered.
If healthcare workers are at all concerned about possible exposure to SARS-CoV-2, they should contact their occupational health service as well as to begin to log their temperature or any symptoms [81,82].
4. Impact on surgical education and training
The pandemic is expected to cause an unprecedented disruption to the provision of surgical education. Undoubtedly undergraduate medical education and the training of surgical residents will suffer with the suspension of normal training rotations as highlighted in the UK, Singapore and many other countries [83,84]. The Association of Surgeons in Training and the 15 surgical speciality associations in the UK have specifically warned of a profound impact to surgical training. On March 13, 2020, the Royal College of Surgeons of Edinburgh announced that all examinations, courses, and other educational events would be postponed until further notice [85]. This was a move swiftly seconded internationally across many healthcare institutions [[86], [87], [88]].
Many surgical educational conferences have also been cancelled or delayed, decreasing the number of learning opportunities for surgical trainees. The deceleration of training is expected to increase the capacity of emergency and critical care units by enabling the redeployment of trainees and attendings to clinical areas not usually occupying their daily practice or grade [89]. In the USA, hospitals have been enrolling surgical residents into critical care nursing workshops enabling them to support key allies [90]. There has been a strong emphasis on deployed trainees receiving appropriate induction and supervision before they begin unfamiliar roles, ensuring safe practise [18]. For those surgical trainees in academic surgical training, a huge emphasis is on ensuring an easy and safe transition to clinical surgical service delivery.
This experience has borne out in Italy where urological residents have adapted and used smart learning technologies to replace traditional training methods [91]. These include a pre-recorded video library featuring taught classes and expert tips and tricks, live webinars with expert commentary and discussion of clinical cases, social media journal clubs, and ‘virtual’ rounds.
The four governing surgical bodies of the UK have assured their trainees that COVID-19 will be taken into consideration during the Annual Review of Competency Progression (ARCP), where their yearly progress is reviewed [92]. For surgical trainees requiring revalidation before September 2020, extensions have been granted. As an alternative option, funding for online and distance learning during COVID-19 as described above is being considered. The Health Education England will need to discuss strategies for the smooth transition of surgeons to return to their surgical training for times past the pandemic [[93], [94], [95]].
The American Board of Medical Specialities has also developed similar guidelines for recertification as well as the American Board of Surgery modifying certification requirements such as not including self-isolation into the 6 weeks of allowed leave, reducing minimum case-logs by 10% as well as recognising time spent treating COVID-19 patients as part of training time requirements [96,97].
5. Research
Surgical research, both laboratory and clinically based, has been suspended due to the COVID-19 pandemic with many surgeons in academia being re-deployed to the clinical setting to help treat patients with COVID-19 [98]. Moreover, many clinical and scientific conferences have been cancelled which are valuable sources of scientific communication, with some transferring to a virtual model instead [99].
However, many academic institutions have realigned their research goals to tackle COVID-19 and surgeons are no exception [100].
The University of Birmingham and the National Institute for Health Research (NIHR) Global Surgery Unit are using real world collaborative international data as part of a project called CovidSurg with the RCSEng encouraging members to contribute to it [101]. This international, multicentre, pan-speciality project will determine multiple end-points, including 30 day mortality in patients with COVID-19, the impact on safety in cancer surgery patients and impact of delayed pathways, as well as the impact on the surgical workforce and on emergency surgical services [102].
The United States are scaling back the work of many of the basic science based laboratories to prioritise work on the COVID-19 pandemic and thus with many surgical researchers being away from their laboratories, many researchers have been forced to postpone and abandon experiments, leading to severe implications for the pace of scientific discoveries [100,103].
6. Recovery of surgical services
The postponement of non-urgent surgical services will inevitably lead to a significant backlog. This has a significant impact, both on the capacity of the surgical system as well as at a personal level, causing extreme stress and anxiety for patients. One study showed that 30% of patients who had operations cancelled during winter pressures complained of extreme stress and frustration as well as 59% reporting moderate or severe concern about a deterioration in their condition [104], in addition to the impact on a patient's family as well.
The Royal College of Ophthalmology have outlined a framework for resumption of normal services to include: a preliminary period of gradual resumption of operations whilst maintaining a surge capacity in case of further COVID-19 peaks (Recovery phase 1 - ‘interim period’) and a longer period (Recovery Phase 2 - ‘the new normal’) during the next 12–18 months [105]. They stressed the need to consider repeated cycles of ‘switching on and off’ peak COVID-19 demand as well as the need for adoption of clear patient pathways during looser social distancing measures.
Furthermore, the importance of not returning to ‘business as usual’ and the benefits of embedding the transformative ways of working developed during the pandemic such as increased efficiency, regional workload sharing, and digital outpatient services.
Additionally, the RCS have developed nine key elements to the short-term recovery of surgical services [106].
-
•Key considerations before resuming elective services
-
oEstablishment of declining numbers, adequate testing capacity and PPE
-
o
-
•Developing cohesive leadership and process of frequent communication
-
oDedicated local recovery management team with daily clinical input
-
o
-
•Assessing surgical workload and patient populations
-
oAssessment of baseline demand and patient prioritisation
-
o
-
•Ensuring adequate hospital capacity and facilities
-
oTemporary field hospitals and private sector facilities
-
oClinician job planning to reduce administrative demands
-
oAdjustment of case list length to allow for longer operations
-
o
-
•Enhancing workforce capacity
-
oMaintenance of temporary redeployment
-
o
-
•Reconfiguring services
-
o‘Cold’ COVID-19 free sites
-
oCOVID-19 patient testing protocol
-
oTriaging protocols
-
oUse of virtual clinics and patient-initiated reviews
-
o
-
•Supporting the surgical workforce
-
oAdequate PPE and testing
-
oMonitoring surgical workforce burnout and wellbeing
-
o
-
•
Patient communication
-
•Supporting training
-
oTrainee development
-
oCross-speciality learning from deployed staff
-
o
7. Conclusion
The impact of COVID-19 on a surgeon's daily practice and the education of surgeons have been profound. Elective and non-urgent surgery cancellations have enabled surgeons to become a critical staff resource for the health systems to treat the COVID-19 pandemic. Surgeons are considering safe non-surgical alternative options to treat their patients during COVID-19.
This is a fast-moving pandemic with the academic literature base growing exponentially on a daily basis. This paper is a comprehensive general overview of the most current guidelines issued by speciality bodies and learned societies as of date of publication. However, these guidelines are responsive to emerging research and subject to change.
Additionally, whilst surgical services vary widely across the world in response to local and regional variation in budgetary restraints, healthcare system configurations and patient demographics, this leads to differing and often contradictory guidelines issued by different bodies. This paper does not seek to offer specialised local guidelines, but instead points of principle that are generally applicable, with room for local variation.
While COVID-19 continues to make its presence felt in healthcare all over the world, surgeons will no doubt adapt to non-surgical roles in the crucial fight against the COVID-19 pandemic.
Finally, it is imperative that in this time of crisis, as Yong et al. [107] remind us:
‘All medical staff and patients [must] face this together to construct the Great Wall of Epidemic Prevention’
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. Lond. Engl. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation WHO Director-General’s opening remarks at the media briefing on COVID-19. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 accessed March 29, 2020.
- 4.Nicola M., O'Neill N., Sohrabi C., Khan M., Agha M., Agha R. Evidence based management guideline for the COVID-19 pandemic - review article. Int. J. Surg. Lond. Engl. 2020 doi: 10.1016/j.ijsu.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kurihara H., Bisagni P., Faccincani R., Zago M. COVID-19 outbreak IN northern Italy: viewpoint OF the milan area surgical community. J. Trauma Acute Care Surg. 2020;1 doi: 10.1097/TA.0000000000002695. [DOI] [PubMed] [Google Scholar]
- 7.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., Liu L., Shan H., Lei C., Hui D.S.C., Du B., Li L., Zeng G., Yuen K.-Y., Chen R., Tang C., Wang T., Chen P., Xiang J., Li S., Wang J., Liang Z., Peng Y., Wei L., Liu Y., Hu Y., Peng P., Wang J., Liu J., Chen Z., Li G., Zheng Z., Qiu S., Luo J., Ye C., Zhu S., Zhong N. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2002032. NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brindle M., Gawande A. Managing COVID-19 in surgical systems. Ann. Surg. 2020;1 doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVIDSurg Collaborative Global guidance for surgical care during the COVID-19 pandemic: surgical care during the COVID-19 pandemic. Br. J. Surg. 2020 doi: 10.1002/bjs.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monitor International comparisons of selected service lines in seven health systems. Annex 3 – review of service lines: critical Care. 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/382845/Annex_3_Critical_Care1.pdf accessed February 4, 2020.
- 11.Ferguson N., Laydon D., Nedjati Gilani G., Imai N., Ainslie K., Baguelin M., Bhatia S., Boonyasiri A., Cucunuba Perez Z., Cuomo-Dannenburg G., Dighe A., Dorigatti I., Fu H., Gaythorpe K., Green W., Hamlet A., Hinsley W., Okell L., Van Elsland S., Thompson H., Verity R., Volz E., Wang H., Wang Y., Walker P., Winskill P., Whittaker C., Donnelly C., Riley S., Ghani A. Report 9: impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. 2020. [DOI]
- 12.Stevens S. Next steps on NHS response to COVID-19. 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf
- 13.Ziser A., Alkobi M., Markovits R., Rozenberg B. The recovery room as an intensive care unit. Crit. Care. 1998;2:P165. doi: 10.1186/cc294. [DOI] [Google Scholar]
- 14.COVIDvent COVIDvent, COVIDvent. 2020. https://www.covidvent.com accessed April 13, 2020.
- 15.NHS England Clinical guide to adult critical care during the coronavirus pandemic: staffing framework. 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0087-specialty-guide-critical-care-standard-operating-procedure-and-coronavirus-v1-28-march.pdf accessed April 2, 2020.
- 16.NHS England Coronavirus: principles for increasing the nursing workforce in response to exceptional increased demand in adult critical care. 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-critical-care-workforce-v1-25-march-2020.pdf accessed February 4, 2020.
- 17.Royal College of Surgeons of England Guidance for surgeons working during the COVID-19 pandemic. 2020. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v1/ accessed April 2, 2020.
- 18.Royal College of Surgeons of England COVID-19: good practice for surgeons and surgical teams. 2020. https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/coronavirus/covid-19-good-practice-for-surgeons-and-surgical-teams/ accessed April 2, 2020.
- 19.Schwartz A.M., Wilson J., Boden S.D., Moore T.J., Bradbury T.L., Fletcher N.D. J. Bone Jt. Surg.; 2020. Managing resident workforce and education during the COVID-19 pandemic.https://journals.lww.com/jbjsjournal/Documents/Schwartz.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dexter F., Parra M.C., Brown J.R., Loftus R.W. Perioperative COVID-19 defense: an evidence-based approach for optimization of infection control and operating room management. Anesth. Analg. 2020 doi: 10.1213/ANE.0000000000004829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NHS England Clinical guide for the management of noncoronavirus patients requiring acute treatment: Cancer. 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-acute-treatment-cancer-23-march-2020.pdf accessed April 2, 2020.
- 22.American College of Surgeons COVID-19 guidelines for triage of cancer surgery patients. 2020. https://www.facs.org/covid-19/clinical-guidance/elective-case/cancer-surgery accessed April 2, 2020.
- 23.Browne C., Davis N.F., Mac Craith E.D., Lennon G.M., Galvin D.J., Mulvin D.W. Prospective evaluation of a virtual urology outpatient clinic. Ir. J. Med. Sci. 2018;187:251–254. doi: 10.1007/s11845-017-1615-y. [DOI] [PubMed] [Google Scholar]
- 24.Evans D., Hardman J., Middleton S.D., Anakwe R.E. Developing a virtual fracture clinic for hand and wrist injuries. J. Hand Surg. Eur. 2018;43:893–894. doi: 10.1177/1753193418778472. [DOI] [PubMed] [Google Scholar]
- 25.Sultan A.A., Acuña A.J., Samuel L.T., Rabin J.M., Grits D., Gurd D.P., Kuivila T.E., Goodwin R.C. Utilization of telemedicine virtual visits in pediatric spinal deformity patients: a comparison of feasibility and patient satisfaction at a large academic center. J. Pediatr. Orthop. 2020 doi: 10.1097/BPO.0000000000001553. [DOI] [PubMed] [Google Scholar]
- 26.Connor M.J., Winkler M., Miah S. COVID-19 Pandemic - is Virtual Urology Clinic the answer to keeping the cancer pathway moving? BJU Int. 2020 doi: 10.1111/bju.15061. [DOI] [PubMed] [Google Scholar]
- 27.The Royal College of Ophthalmologists Telemedicine applications for opthalmology consultations during a pandemic emergency. 2020. https://www.rcophth.ac.uk/wp-content/uploads/2020/03/Telemedicine-Options-for-Ophthalmology-Consultations-COVID19.pdf accessed April 2, 2020.
- 28.Norfolk, Norwich University Hospitals NHS Foundation Trust Telehealth Video Consultation patient information sheet. 2020. http://www.nnuh.nhs.uk/publication/download/telehealth-video-consultation-v4 accessed April 8, 2020.
- 29.Centers for Medicare & Medicaid Services Medicare telemedicine health care provider fact sheet. 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet accessed April 8, 2020.
- 30.Greenhalgh T., Shaw S., Wherton J., Vijayaraghavan S., Morris J., Bhattacharya S., Hanson P., Campbell-Richards D., Ramoutar S., Collard A., Hodkinson I. Real-world implementation of video outpatient consultations at macro, meso, and micro levels: mixed-method study. J. Med. Internet Res. 2018;20 doi: 10.2196/jmir.9897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greenhalgh T., Wherton J., Shaw S., Morrison C. Video consultations for covid-19. BMJ. 2020;368 doi: 10.1136/bmj.m998. [DOI] [PubMed] [Google Scholar]
- 32.NHS England Clinical guide for the management of remote consulations and remote working in secondary care during the Coronavirus pandemic. 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0044-Specialty-Guide-Virtual-Working-and-Coronavirus-27-March-20.pdf accessed April 2, 2020.
- 33.UCLPartners How-to guide: non face-to-face clinics. 2019. https://uclpartners.com/non-face-to-face-clinics-resource/ accessed April 8, 2020.
- 34.Royal College of Surgeons of England Running and setting up virtual surgical outpatients clinics. 2020. https://www.rcseng.ac.uk/news-and-events/events/calendar/running-and-setting-up-virtual-surgical-outpatients-clinics/ accessed April 8, 2020.
- 35.Barts Health NHS Trust Video consultations. 2017. https://www.bartshealth.nhs.uk/video-consultations accessed April 8, 2020.
- 36.General Medical Council How we will continue to regulate in light of novel coronavirus (Covid-19) https://www.gmc-uk.org/news/news-archive/how-we-will-continue-to-regulate-in-light-of-novel-coronavirus (n.d.) accessed April 2, 2020.
- 37.Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020:m1106. doi: 10.1136/bmj.m1106. [DOI] [PubMed] [Google Scholar]
- 38.World Health Organisation Coronavirus disease 2019. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (n.d.) accessed April 2, 2020.
- 39.Schraer R. BBC News; 2020. ExCeL Centre to Be Used as Coronavirus Hospital.https://www.bbc.com/news/health-52018477 accessed April 2, 2020. [Google Scholar]
- 40.BBC News; 2020. NHS Deal Will Provide Thousands of Extra Beds.https://www.bbc.com/news/uk-51989183 accessed April 2, 2020. [Google Scholar]
- 41.Centres for Disease Control and Prevention Donning PPE. 2019. https://www.cdc.gov/vhf/ebola/hcp/ppe-training/n95respirator_gown/donning_01.html accessed April 2, 2020.
- 42.Public Health England When to use a surgical face mask or FFP3 respirator. 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control accessed February 4, 2020.
- 43.Heneghan C., Brassey J., Jefferson T. Oxford Centre for Evidence-Based Medicine; 2020. SARS-CoV-2 Viral Load and the Severity of COVID-19.https://www.cebm.net/covid-19/sars-cov-2-viral-load-and-the-severity-of-covid-19/ accessed April 2, 2020. [Google Scholar]
- 44.European Centre for Disease Prevention and Control (ECDC) Infection prevention and control and preparedness for COVID-19 in healthcare settings. 2020. https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings accessed April 2, 2020.
- 45.Lim W.S., Anderson S.R., Read R.C. SARS guidelines committee of the British thoracic society, British infection society, health protection agency, hospital management of adults with severe acute respiratory syndrome (SARS) if SARS re-emerges. J. Infect. 2004;49:1–7. doi: 10.1016/j.jinf.2004.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in wuhan, China. J. Am. Med. Assoc. 2020;323:1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organisation . Aide Memoire); Geneva: 2008. Epidemic- and Pandemic-Prone Acute Respiratory Diseases Infection Prevention and Control in Health Care.https://www.who.int/csr/resources/publications/EPR_AM3_E3.pdf accessed April 2, 2020. [PubMed] [Google Scholar]
- 48.Srinivasan A., Jernign D.B., Liedtke L., Strausbaugh L. Hospital preparedness for severe acute respiratory syndrome in the United States: views from a national survey of infectious diseases consultants. Clin. Infect. Dis. 2004;39:272–274. doi: 10.1086/421777. [DOI] [PubMed] [Google Scholar]
- 49.American College of Surgeons . Am. Coll. Surg.; 2020. COVID-19: considerations for optimum surgeon protection before, during, and after operation.https://www.facs.org/covid-19/clinical-guidance/surgeon-protection accessed April 2, 2020. [Google Scholar]
- 50.Forrester J.D., Nassar A.K., Maggio P.M., Hawn M.T. Precautions for operating room team members during the COVID-19 pandemic. J. Am. Coll. Surg. 2020 doi: 10.1016/j.jamcollsurg.2020.03.030. S1072751520303033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Royal College of Surgeons of Edinburgh Intercollegiate guidance for pre-operative chest CT imaging for elective cancer surgery during the COVID-19 pandemic. 2020. https://www.rcsed.ac.uk/news-public-affairs/news/2020/april/intercollegiate-guidance-for-pre-operative-chest-ct-imaging-for-elective-cancer-surgery-during-the-covid-19-pandemic accessed April 15, 2020.
- 52.Association of Surgeons of Great Britain & Ireland Association of coloproctology of Great Britain & Ireland, association of upper gastrointestinal surgeons, royal College of surgeons of Edinburgh, royal College of surgeons of England, royal College of physicians and surgeons of glasgow, royal College of surgeons in Ireland, updated general surgery guidance on COVID-19, 2nd revision. 2020. https://www.rcsed.ac.uk/news-public-affairs/news/2020/april/updated-general-surgery-guidance-on-covid-19-2nd-revision-7th-april-2020 accessed April 9, 2020.
- 53.Brat G.A., Hersey S.P., Chhabra K., Gupta A., Scott J. Protecting surgical teams during the COVID-19 outbreak: a narrative review and clinical considerations. Ann. Surg. 2020 doi: 10.1097/SLA.0000000000003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kaixiong T., Bixiang Z., Peng Z., Peng Z., Guobin W., Xiaoping C., G.S.B. of H.M. Association. G.S.B. of W.M. Association [Recommendations for general surgery clinical practice in novel coronavirus pneumonia situation] Chin. J. Surg. 2020;58:E001. doi: 10.3760/cma.j.issn.0529-5815.2020.0001. [DOI] [PubMed] [Google Scholar]
- 55.Chen R., Zhang Y., Huang L., Cheng B., Xia Z., Meng Q. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: a case series of 17 patients. Can. J. Anesth. Can. Anesth. 2020 doi: 10.1007/s12630-020-01630-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kirk-Bayley J., Combes J., Sunkaraneni S., Challacombe S. Social Science Research Network; Rochester, NY: 2020. The Use of Povidone Iodine Nasal Spray and Mouthwash during the Current COVID-19 Pandemic May Reduce Cross Infection and Protect Healthcare Workers. [DOI] [Google Scholar]
- 57.Royal Hospital for Children Glasgow Intubation checklist for suspected or confirmed COVID-19 patient. 2020. https://www.clinicalguidelines.scot.nhs.uk/media/2206/covid-19-intubation-checklist-v22.pdf accessed April 8, 2020.
- 58.Brighton and Sussex University Hospitals NHS Trust Anaesthetic ‘COVID sequence induction’ CSI. 2020. https://www.bsuh.nhs.uk/library/wp-content/uploads/sites/8/2020/03/Covid-Intubation-Checklist-VX1-1.pdf accessed April 8, 2020.
- 59.Wong J., Goh Q.Y., Tan Z., Lie S.A., Tay Y.C., Ng S.Y., Soh C.R. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can. J. Anesth. Can. Anesth. 2020 doi: 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lyness D. Hospital warning sign infographs. 2020. https://www.propofology.com/infographs/hospital-warning-signs accessed April 8, 2020.
- 61.Ademuyiwa A.O., Bekele A., Berhea A.B., Borgstein E., Capo-Chichi N., Derbew M., Evans F.M., Feyssa M.D., Galukande M., Gawande A.A., Gueye S.M., Harrison E., Jani P., Kaseje N., Litswa L., Mammo T.N., Mellin-Olsen J., Muguti G., Nabukenya M.T., Ngoga E., Ntirenganya F., Rulisa S., Starr N., Tabiri S., Tadesse M., Walker I., Weiser T.G., Wren S.M. COVID-19 preparedness within the surgical, obstetric, and anaesthetic ecosystem in sub-Saharan Africa, East Cent. Afr. J. Surg. 2020;25 doi: 10.4314/ecajs.v25i1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barts Health NHS Trust . 2020. Royal London Hospital COVID Intubation SOP. [Google Scholar]
- 63.Chow T.T., Yang X.Y. Ventilation performance in operating theatres against airborne infection: review of research activities and practical guidance. J. Hosp. Infect. 2004;56:85–92. doi: 10.1016/j.jhin.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 64.Chen Y., Zhang S., Zhang Z., Sun Z., Zhao H., Zhang Y., Li H., Yin D. J. Xi’an Jiaotong Univ. Med.; 2020. Management Strategies and Recommendations for New-type Coronavirus Pneumonia Patients in Emergency Surgery.http://yxxb.xjtu.edu.cn//oa/darticle.aspx?type=view&id=2020004&utm_source=TrendMD&utm_medium=cpc&utm_campaign=Journal_of_Xi%27an_Jiaotong_University_(Medical_Sciences)_TrendMD_1 accessed April 8, 2020. [Google Scholar]
- 65.Public Health England Reducing the risk of transmission of COVID-19 in the hospital setting. 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/reducing-the-risk-of-transmission-of-covid-19-in-the-hospital-setting accessed April 8, 2020.
- 66.Ti L.K., Ang L.S., Foong T.W., Ng B.S.W. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can. J. Anesth. Can. Anesth. 2020 doi: 10.1007/s12630-020-01617-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.DesCoteaux J.G., Picard P., Poulin E.C., Baril M. Preliminary study of electrocautery smoke particles produced in vitro and during laparoscopic procedures. Surg. Endosc. 1996;10:152–158. doi: 10.1007/bf00188362. [DOI] [PubMed] [Google Scholar]
- 68.Kwak H.D., Kim S.-H., Seo Y.S., Song K.-J. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery, Occup. Environ. Med. 2016;73:857–863. doi: 10.1136/oemed-2016-103724. [DOI] [PubMed] [Google Scholar]
- 69.Tao K.X., Zhang B.X., Zhang P., Zhu P., Wang G.B., Chen X.P. General surgery branch of Hubei medical association, general surgery branch of wuhan medical association, [recommendations for general surgery clinical practice in 2019 coronavirus disease situation] Zhonghua Wai Ke Za Zhi. 2020;58:170–177. doi: 10.3760/cma.j.issn.0529-5815.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 70.Morris S.N., Fader A.N., Milad M.P., Dionisi H.J. Understanding the “scope” of the problem: why laparoscopy is considered safe during the COVID-19 pandemic. J. Minim. Invasive Gynecol. 2020 doi: 10.1016/j.jmig.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zheng M.H., Boni L., Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann. Surg. 2020;1 doi: 10.1097/SLA.0000000000003924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schultz L. Can efficient smoke evacuation limit aerosolization of bacteria? AORN J. 2015;102:7–14. doi: 10.1016/j.aorn.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 73.SAGES SAGES and EAES recommendations regarding surgical response to COVID-19 crisis. 2020. https://www.sages.org/recommendations-surgical-response-covid-19/ accessed April 9, 2020.
- 74.SAGES, Resources for Smoke & Gas Evacuation During Open Laparoscopic, and endoscopic procedures. 2020. https://www.sages.org/resources-smoke-gas-evacuation-during-open-laparoscopic-endoscopic-procedures/ accessed April 9, 2020.
- 75.He Y., Wei J., Bian J., Guo K., Lu J., Mei W., Ma J., Xia Z., Xu M., Yan F., Yu C., Wang E., Wang W., Zeng N., Wang S., Xu J., Huang Y., Huang J. Chinese society of anesthesiology expert consensus on anesthetic management of cardiac surgical patients with suspected or confirmed coronavirus disease 2019. J. Cardiothorac. Vasc. Anesth. 2020 doi: 10.1053/j.jvca.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Aminian A., Safari S., Razeghian-Jahromi A., Ghorbani M., Delaney C.P. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann. Surg. 2020;1 doi: 10.1097/SLA.0000000000003925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bos M.M.E.M., Bakhshi-Raiez F., Dekker J.W.T., de Keizer N.F., de Jonge E. Outcomes of intensive care unit admissions after elective cancer surgery. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2013;39:584–592. doi: 10.1016/j.ejso.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 79.Zampieri F.G. Elective ICU admission after major surgery: can too much support be futile? J. Thorac. Dis. 2018;10:S1992–S1994. doi: 10.21037/jtd.2018.05.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lei S., Jiang F., Su W., Chen C., Chen J., Mei W., Zhan L.-Y., Jia Y., Zhang L., Liu D., Xia Z.-Y., Xia Z. EClinicalMedicine; 2020. Clinical Characteristics and Outcomes of Patients Undergoing Surgeries during the Incubation Period of COVID-19 Infection. 100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Christopher Newport University Coronavirus (COVID-19) self-monitoring sheet. 2020. http://cnu.edu/public/_pdf/covid-19%20-%2014%20day%20symptom%20self%20monitoring%20sheet.pdf accessed April 12, 2020.
- 82.North Carolina Department of Health and Human Services 2019-nCoV symptom self-monitoring log. 2020. https://epi.ncpublichealth.info/cd/lhds/manuals/cd/coronavirus/2_PUM_Symptom%20Self-monitoring%20Log.pdf?ver=1.2&fbclid=IwAR19gFJ7CEaaMWq3rZdHVITrQgOGy-4-oHe6daogjN4jw8jLcG4j8LwTp0Y accessed April 12, 2020.
- 83.Chan M.-C., Yeo S.E.K., Chong Y.-L., Lee Y.-M. Stepping forward: urologists' efforts during the COVID-19 outbreak in Singapore. Eur. Urol. 2020 doi: 10.1016/j.eururo.2020.03.004. S0302283820301457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Alsafi Z., Abbas A.-R., Hassan A., Ali M.A. The coronavirus pandemic: adaptations in medical education. Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.03.083. S1743919120303101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Riding D. Statement on COVID-19 and its effect on surgical training. 2020. https://www.rcsed.ac.uk/news-public-affairs/news/2020/march/statement-on-covid-19-and-its-effect-on-surgical-training accessed April 10, 2020.
- 86.Royal College of Physicians MRCP(UK) and other exams cancelled – new advice on trainee progression in 2020. 2020. https://www.rcplondon.ac.uk/news/mrcpuk-and-other-exams-cancelled-new-advice-trainee-progression-2020 accessed April 10, 2020.
- 87.Siddique H. The Guardian; 2020. Final-year Medical Students Graduate Early to Fight Covid-19.https://www.theguardian.com/world/2020/mar/20/final-year-medical-students-graduate-early-fight-coronavirus-covid-19 accessed April 10, 2020. [Google Scholar]
- 88.Association of American Medical Colleges Coronavirus (COVID-19) and the MCAT exam. 2020. https://students-residents.aamc.org/applying-medical-school/article/coronavirus-mcat-faqs/ accessed April 10, 2020.
- 89.Association of Surgeons in Training ASiT and the 15 Speciality Associations Joint Letter to Surgical Trainees on COVID-19: the implications for surgical trainees in the delivery of care and training. 2020. https://www.asit.org/news/asit-and-the-15-speciality-associations-joint-letter-to-surgical-trainees-on-covid-19-the-implications-for-surgical-tra/nwc11195 accessed April 10, 2020.
- 90.Davis L. USC News; 2020. Surgeons-in-training Learn Important Skills to Back up Key Allies during the Coronavirus Pandemic — Nurses.https://news.usc.eduhttps://news.usc.edu/167632/surgical-residents-nurses-critical-care-covid-19/ accessed April 10, 2020. [Google Scholar]
- 91.Porpiglia F., Checcucci E., Amparore D., Verri P., Campi R., Claps F., Esperto F., Fiori C., Carrieri G., Ficarra V., Scarpa R.M., Dasgupta P. European society of residents in urology (ESRU) of European association of urology (EAU), slowdown of urology residents' learning curve during COVID-19 emergency. BJU Int. 2020 doi: 10.1111/bju.15076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Health Education England, NHS Education for Scotland Northern Ireland medical and dental training agency, health education and improvement wales, letter and ARCP update from the four statutory education bodies to all trainees. 2020. https://www.nimdta.gov.uk/download/supporting-the-covid-19-response/ accessed April 9, 2020.
- 93.London, South East Postgraduate Medical and Dental Education COVID-19 study leave update. 2020. https://www.lpmde.ac.uk/training-programme/covid-19-response-updates/study-leave-update accessed April 12, 2020.
- 94.London, South East Postgraduate Medical and Dental Education COVID-19 Letter to all medical trainees. 2020. https://www.lpmde.ac.uk/training-programme/covid-19-response-updates/covid-19-letter-to-all-medical-trainees accessed April 12, 2020.
- 95.Conference of Postgraduate Medical Deans of the United Kingdom Guidance on managing revalidation arrangements for doctors in postgraduate training during the GMC's 6-month deferral of revalidation recommendations. 2020. https://www.copmed.org.uk/images/docs/revalidation/COPMeD_guidance_on_trainee_revalidation_during_COVID-19.pdf accessed April 12, 2020.
- 96.American Board of Medical Specialities ABMS and ACGME joint principles: physician training during the COVID-2019 pandemic. 2020. https://www.abms.org/news-events/abms-and-acgme-joint-principles-physician-training-during-the-covid-2019-pandemic/ accessed April 12, 2020.
- 97.American Board of Surgery Modifications to training requirements - COVID-19 update. 2020. http://www.absurgery.org/default.jsp?news_covid19_trainingreq accessed April 12, 2020.
- 98.American College of Surgeons COVID-19 and surgery. 2020. https://www.facs.org/covid-19 accessed April 13, 2020.
- 99.Porpiglia F., Amparore D., Autorino R., Checcucci E., Cooperberg M.R., Ficarra V., Novara G. Traditional and virtual congress meetings during the COVID-19 pandemic and the post-COVID-19 era: is it time to change the paradigm? Eur. Urol. 2020 doi: 10.1016/j.eururo.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Basken P. Times High. Educ.; 2020. US Research Labs Closing Down for Everything but Coronavirus.https://www.timeshighereducation.com/news/us-research-labs-closing-down-everything-coronavirus accessed April 15, 2020. [Google Scholar]
- 101.NIHR Global Surgery Unit, CovidSurg, Globalsurg 2020. https://globalsurg.org/covidsurg/ accessed April 15, 2020.
- 102.ClinicalTrialsgov . CovidSurg); 2020. Outcomes of Surgery in COVID-19 Infection: International Cohort Study.https://clinicaltrials.gov/ct2/show/NCT04323644 accessed April 15, 2020. [Google Scholar]
- 103.Joseph A. STAT; 2020. Coronavirus Pandemic Forces Some Research Labs to Shut Down.https://www.statnews.com/2020/03/14/coronavirus-pandemic-forces-research-labs-shut-down/ accessed April 15, 2020. [Google Scholar]
- 104.Herrod P.J.J., Adiamah A., Boyd-Carson H., Daliya P., El-Sharkawy A.M., Sarmah P.B., Hossain T., Couch J., Sian T.S., Wragg A., Andrew D.R., Parsons S.L., Lobo D.N. Winter cancellations of elective surgical procedures in the UK: a questionnaire survey of patients on the economic and psychological impact. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-028753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Royal College of Ophthalmology Reopening and redeveloping ophthalmology services during Covid recovery – interim guidance. 2020. https://rcophth.ac.uk/2020/05/covid-19-update-and-resources-for-ophthalmologists/ accessed May 5, 2020.
- 106.Royal College of Surgeons of England Recovery of surgical services during and after COVID-19. 2020. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/ accessed May 6, 2020.
- 107.Yong L., Jianjun Q., Zhen W., Yuan Y., Yongyao W., Xiankai C., Weixin L., Yin L. Surgical treatment for esophageal cancer during the outbreak of COVID-19, Chin. J. Oncol. 2020;42 doi: 10.3760/cma.j.cn112152-20200226-00128. E003–E003. [DOI] [PubMed] [Google Scholar]