Highlights
-
•
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
-
•
Some COVID-19 patients have exhibited widespread neurological manifestations including stroke.
-
•
Acute ischemic stroke, intracerebral hemorrhage, and cerebral venous sinus thrombosis have been reported in patients with COVID-19.
-
•
COVID-19-associated coagulopathy is likely caused by inflammation.
-
•
Resultant ACE2 down-regulation causes RAS imbalance, which may lead to stroke.
Keywords: COVID-19, SARS-CoV-2, Stroke, Endothelial damage, ACE2, Renin-angiotensin system, Pandemic
Abstract
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a global health threat. Some COVID-19 patients have exhibited widespread neurological manifestations including stroke. Acute ischemic stroke, intracerebral hemorrhage, and cerebral venous sinus thrombosis have been reported in patients with COVID-19. COVID-19-associated coagulopathy is increasingly recognized as a result of acute infection and is likely caused by inflammation, including inflammatory cytokine storm. Recent studies suggest that axonal transport of SARS-CoV-2 to the brain can occur via the cribriform plate adjacent to the olfactory bulb that may lead to symptomatic anosmia. The internalization of SARS-CoV-2 is mediated by the binding of the spike glycoprotein of the virus to the angiotensin-converting enzyme 2 (ACE2) on cellular membranes. ACE2 is expressed in several tissues including lung alveolar cells, gastrointestinal tissue, and brain. The aim of this review is to provide insights into the clinical manifestations and pathophysiological mechanisms of stroke in COVID-19 patients. SARS-CoV-2 can down-regulate ACE2 and, in turn, overactivate the classical renin-angiotensin system (RAS) axis and decrease the activation of the alternative RAS pathway in the brain. The consequent imbalance in vasodilation, neuroinflammation, oxidative stress, and thrombotic response may contribute to the pathophysiology of stroke during SARS-CoV-2 infection.
Introduction
An outbreak of an acute respiratory illness of unknown cause started in Wuhan, Hubei province, China on December 12, 2019.1 , 2 A new strain of coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified in these patients. Subsequently, the identified acute respiratory illness was named coronavirus disease 2019 (COVID-19). Soon thereafter, the COVID-19 epidemic in China became a pandemic with a significant burden on healthcare and the worldwide economy. SARS-CoV-2 has been shown to be a distinct class of the beta coronaviruses (Beta-CoVs) with a 79.5% gene sequence homology to the severe acute respiratory syndrome coronavirus (SARS-CoV),3 and the 50% homology to Middle East respiratory syndrome coronavirus (MERS-CoV).4 Moreover, the genome sequence of SARS-CoV-2 is 96.2% identical to RaTG13, a short RNA-dependent RNA polymerase (RdRp) region from a bat coronavirus.3 The amino acid sequences of the seven conserved replicase domains of Open Reading Frame 1ab (ORF1ab) used to classify coronavirus species are 94.4% identical between SARS-CoV and SARS-CoV-2.1 Coronaviruses, which include non-segmented enveloped positive-sense RNA viruses from the Coronaviridae family of Nidovirales order, are widely distributed in mammals, including humans. Although most cases of coronavirus infections are mild, the epidemics of the SARS-CoV and MERS-CoV affected more than 10,000 people in the past two decades with mortality rates of 9.6% and 34%, respectively.5 , 6 The mortality rate of COVID-19 has been reported to be as high as 4.3%7 and as of May 18, 2020, the number of confirmed cases and deaths worldwide have been 4,628,903 and 312,009, respectively.8 SARS-CoV-2 is primarily transmitted between humans via exposure of mucosae or conjunctiva to infected respiratory droplets or contact routes such as fomites in the immediate environment around an infected person.9, 10, 11, 12, 13 SARS-CoV-2 has also been detected in tears, similar to SARS-CoV.14 Fever, cough, shortness of breath, fatigue, anosmia, and hypogeusia are the main symptoms of COVID-19. Anorexia, myalgia, dyspnea, chest tightness, sputum production, hemoptysis, sore throat, diarrhea, nausea, vomiting, and abdominal/back pain are other signs and symptoms.15
Epithelial cells of the respiratory and gastrointestinal tracts are the primary target of SARS-CoV-2. Nevertheless, its effect is not restricted to these cells, and the nervous system can also be involved. Remarkably, SARS-CoV infection has been found in the cerebrospinal fluid.16 Encephalitis, seizures, refractory status epilepticus, acute disseminated encephalomyelitis (ADEM), Guillain-Barré syndrome (GBS), leukoencephalopathy, myopathy, and critical illness neuromyopathy have been observed among COVID-19 patients.17 Helms et al.18 reported neurologic signs in about 84% of the patients with COVID-19. Headache, dizziness, and altered level of consciousness were also seen in 11%, 8%, and 9% of the patients with COVID-19, respectively.15 A less common neurological symptom is characterized by acute confusion.4 A GBS-like phenotype has also been noted in patients with COVID-19.19 , 20 Impaired taste and smell have been found to be strong predictors of COVID-19. In one study, among 59 patients with COVID-19, 20 (33.9%) had at least one taste or olfactory disorder and 11 (18.6%) had both.21 In another study, loss of smell and taste was found in 59% of 1702 patients with COVID-19.22
Recent evidence suggests that COVID-19 can also affect the cardiovascular and cerebrovascular systems.23 A study which investigated 41 patients with COVID-19 in Wuhan, observed arterial hypertension and cardiovascular disease in six (15%) patients.12 Some patients with SARS-CoV-2 have been reported to have a stroke due to cardioembolism and large vessel atherosclerosis. Furthermore, it has been postulated that inflammatory and hypercoagulable mechanisms, including the presence of antiphospholipid antibodies, contribute to the occurrence of thrombotic events.24 , 25 COVID-19 increases pro-inflammatory molecules including interleukin (IL)-1 and IL-6.26 The systemic inflammatory response may also result in rupture or erosion of atherosclerotic plaque and destabilize previously asymptomatic cardiovascular conditions such as myocardial infarction (MI), heart failure, acute cardiac injury, and myocarditis.27 , 28 The aim of this article is to review recent research about the clinical manifestations and underlying potential pathophysiological stroke mechanisms in SARS-CoV-2 infection.
Thrombosis and thromboembolic events in patients with COVID-19
Markedly elevated D-dimer levels and fibrin degradation products have been associated with high mortality rates among COVID-19 patients.29 Early case reports have described both acute pulmonary embolism and disseminated pulmonary microthrombi in patients with COVID-19.30 , 31 In a study of 198 patients with COVID-19 (37% of those whom were admitted to the intensive care unit, ICU), the overall incidence of venous thromboembolism (VTE) was 17%, with 11% of cases being symptomatic. VTE was associated with death and its cumulative incidence was higher in the ICU than in other locations.32 In three Dutch hospitals, 184 ICU patients with COVID-19 were studied.33 Despite standard thromboprophylaxis measures, VTE was found in 27%, and arterial thrombotic events in 3.7%, and pulmonary embolism was the most common thrombotic complication among patients.33 At the Tongi hospital in Wuhan, 449 patients with severe COVID-19 were studied.34 Heparin (mainly low molecular weight) for 7 days or longer was administered to 99 patients. There was a positive correlation between D-dimer level, prothrombin time (PT), and age. However, platelet count and 28-day mortality were negatively correlated. Moreover, there was no difference in the 28-day mortality rate among heparin users and nonusers (30.3% vs 29.7%, P = 0.910). Nonetheless, the 28-day mortality rate of heparin users was lower than that of nonusers in patients with D-dimer levels > 6 fold of the upper limit of normal (32.8% vs 52.4%, P = 0.017) or with a sepsis-induced coagulopathy (SIC) score ≥ 4 (40.0% vs 64.2%, P = 0.029). Furthermore, COVID-19 patients can develop a more severe coagulopathy defined as COVID-19-associated coagulopathy (CAC) that is induced by the acute systemic inflammatory response presumably mediated by the infectious agent or its products. CAC is characterized by an elevation of several blood coagulation markers (e.g., D-dimer, fibrin or fibrinogen degradation product, and fibrinogen), a concomitant rise of peripheral inflammatory markers (e.g., C-reactive protein, CRP) and a mild thrombocytopenia. The degree of activated partial thromboplastin time (aPTT) elevation is often less than PT, mainly due to increased factor VIII level concentrations secondary to the concomitant inflammatory status. Finally, some severe COVID-19 patients exhibit a coagulopathy similar to disseminated intravascular coagulation (DIC) defined according to the International Society on Thrombosis and Haemostasis (ISTH) criteria,35 or a fulminant coagulation activation and coagulation factors’ consumption. This coagulopathy is characterized by moderate to severe thrombocytopenia with platelet count < 50 × 109/L, PT and aPTT prolongation together with a considerable rise of D-dimer levels, and low fibrinogen levels (< 1.0 g/L).7 , 12 , 36 , 37
Histological and immunohistochemistry studies have also defined a pathological pattern characterized by microvascular injury and thrombosis, consistent with activation of the alternative pathway and the lectin pathway of complement. This suggests that at least in this subgroup of patients, COVID-19 infection involves a complement-mediated thrombotic microvascular injury syndrome with sustained activation of both complement cascades.38 Investigating critical biomarkers consistent with complement-mediated microvascular injury and thrombosis in COVID-19 patients should be part of clinical practice.
Inflammatory responses due to COVID-19
SARS-CoV-2 can lead to severe inflammation, including an inflammatory cytokine storm which in turn leads to CAC or thrombosis.39 This is of particular concern for patients with chronic immune-mediated inflammatory diseases.40 SARS-CoV-2 can bind to Toll-like receptors, which leads to the synthesis and liberation of IL-1.26 , 41 This receptor activation triggers a biochemical cascade beginning with the generation of pro-IL-1 cleaved by caspase-1, followed by inflammasome activation. In SARS-CoV-2 infection, Type I interferon (IFN), which exerts an influence upon innate and acquired immunity, and most importantly against viral infections, is released.26 Nevertheless, IFN release can give rise to inflammation and immune system suppression.42 A significant difference in IL-6 concentrations between COVID-19 survivors and non-survivors has been observed, where non-survivors had up to 1.7-times higher levels of IL-6. Moreover, a cytokine profile similar to that of secondary hemophagocytic lymphohistiocytosis (hyperinflammatory syndrome) is associated with the severity of COVID-19.12 This cytokine storm is explained by IL-2, IL-7, interferon-γ inducible protein 10, granulocyte-colony stimulating factor, monocyte chemo-attractant protein 1, tumor necrosis factor-α (TNF-α), and macrophage inflammatory protein 1-α.12 Therefore, blocking inflammation and IL-6 is the rationale for ongoing clinical trials that are examining the use of IL-6 receptor blocker such as Tocilizumab (clinicaltrials.gov trials NCT04317092, NCT04320615, and NCT04335071) where elevated IL-6 level is strongly associated with the need for mechanical ventilation.43
In the past, acute infections have been linked to stroke44 mainly among younger adults. Therefore, it is also likely that in the case of COVID-19 the systemic inflammatory response in the host, rather than the viral invasion per se, could be responsible for an elevated stroke risk. However, at present all studies on COVID-19 related stroke are observational and retrospective. Studies evaluating the stroke risk after COVID-19 have not been performed thus far. Furthermore, study results may be biased by low numbers, absence of appropriate control subjects with recent infection, and multiple selection biases, so the data is inconclusive. There is preliminary evidence for an association between COVID-19 and stroke, but causality has not been established. The preliminary observed association could be explained by residual confounding, incomplete ascertainment, and insufficiently controlled studies. Before assuming causality (Koch postulates) a specific link between SARS-Cov-2 and stroke should be fully established. Thus at the moment no changes in the routine stroke care should be implemented as an adjunct to antiplatelets/antithrombotics and statin therapies that are already practiced in clinical settings.
The immune response to acute cerebral ischemia plays an important role in the pathophysiology and outcome of stroke. The inflammatory cascade, heightening the risk of stroke, can be activated by acute infections.45 Systemic inflammation and inflammatory biomarkers are associated with ischemic stroke risk. Serum IL-6 level has been shown to be a reliable prognostic factor of ischemic stroke.46 Therefore, together with the appropriate blood coagulation markers (including antiphospholipid antibodies) and an inflammatory biomarker panel including CRP, pro-inflammatory cytokines (i.e., IL-1, IL-6, and TNF-α), circulating complement proteins such as C3, C4, C5b, C6, C7, C8, C9, and Bb (where "b" denotes the larger fragment) should be part of routine laboratory tests.
SARS-CoV-2 spike glycoprotein and binding to angiotensin-converting enzyme 2
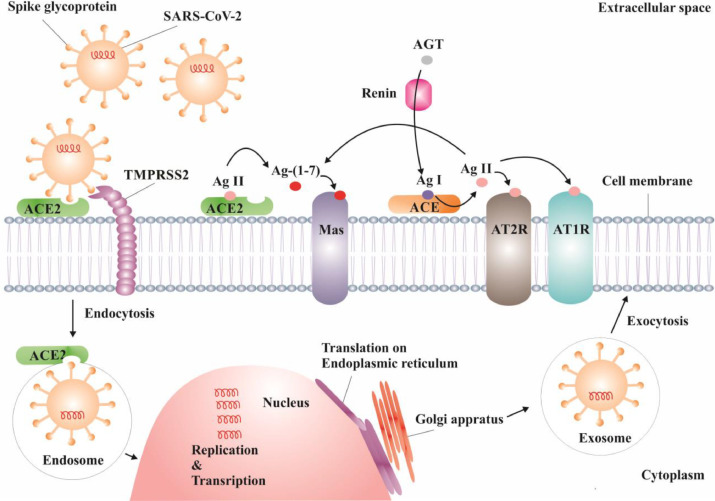
SARS-CoV-2 RNA expresses at least 27 proteins including 15 non-structural, 4 structural, and 8 auxiliary proteins.2 The spike (S) glycoprotein is a structural protein on the outer envelope of SARS-CoV-2 that is primed by transmembrane protease, serine 2 (TMPRSS2), to allow SARS-CoV-2 to bind to angiotensin-converting enzyme 2 (ACE2) as the host cell receptor (see Fig. 1 ). The S glycoprotein may also be primed by cathepsin B and L (CatB and L), which are endosomal serine proteases.47
Fig. 1.
Schematic process of endocytosis of SARS-COV-2, proliferation of the virus inside the cell, and effect of virus upon RAS. Having been primed by TMPRSS2, SARS-COV-2’s spike glycoprotein binds to ACE2. The virus enters the cell and is proliferated. SARS-COV-2 downregulates ACE2, which in turn under-activates the RAS alternative axis (ACE2-Ang-(1-7)-Mas). Under-activation of the alternative axis gives rise to over-activation of the classical RAS axis (ACE-Ang II-AT1R). The consequent imbalance in vasodilation, neuroinflammation, oxidative stress, and thrombotic response can contribute to the pathophysiology of stroke during SARS-CoV-2 infection.
Abbreviations: SARS-COV-2: severe acute respiratory syndrome coronavirus 2, RAS: renin-angiotensin system, ACE2: angiotensin-converting enzyme 2, TMPRSS2: Transmembrane protease, serine 2, Ang: angiotensin, Mas: Mas receptor, AT1R: angiotensin 1 receptor.
Even though the S glycoprotein of SARS-CoV-2 is very similar to those of SARS-CoV and MERS-CoV, differences exist. Amplification of SARS-CoV-2 protein demonstrated a functional polybasic (furin) cleavage site at the S1–S2 boundary through the insertion of 12 nucleotides.48 This difference may explain why the S glycoprotein of SARS-CoV-2 has a higher affinity to ACE2 than SARS-CoV and MERS-CoV that may lead to a higher contagious rate. The S glycoprotein of SARS-CoV-2 contains 1,273 amino acids and has S1 and S2 subunits.48 The receptor-binding domain (RBD) of SARS-CoV-2 in the S1 subunit binds to ACE2 of the host cell.49 This mechanism is shared with SARS-CoV and MERS-CoV.
The abundant expression of ACE2 on the epithelium of the respiratory system may explain the involvement of the lung in COVID-19. ACE2 is expressed in type I and type II alveolar epithelial, bronchiolar epithelial, endothelial, and arterial smooth muscle cells of the lung.27 Moreover, it has been detected on the oral mucosa, especially on the epithelial cells of the tongue.50 The number and proportion of cells expressing ACE2 in nasal and oral tissues are comparable to those in the lungs and colon.51 , 52 ACE2 is also present on endothelial cells and the gastrointestinal tract. Neurons and glial cells express ACE2 as well where can be invaded by SARS-CoV-2.53
Neurotropism of SARS-CoV-2
Neurotropism is the ability of a pathogen to invade and survive in the nervous system. Coronaviruses are neurotropic in several of their hosts, including humans.16 The blood-brain barrier (BBB), the anatomical gateway essential for the maintenance of homeostasis and physiological environment of the central nervous system (CNS), serves an important role in the protection against pathogens. Endothelial cells of the capillaries, pericytes, and astrocyte end-feet constitute the BBB. Inflammation and vascular damage can increase BBB permeability and potentiates unwanted CNS effects.16 Viruses can cross the BBB through several ways including transcellular, paracellular, and retrograde axonal transport along sensory and olfactory nerves.54 Viremia is the viral mechanism for migration. Viral transcellular migration occurs when the virus invades the host cells or macrophages to overcome the BBB. Paracellular migration occurs when the virus attacks the tight junctions in BBB.54 Axonal transport is provided via adherence of the virus to proteins of peripheral or cranial nerves, which allows retrograde neuronal transport.55
Recent studies suggest axonal transport of SARS-CoV-2 via the cribriform plate, adjacent to the olfactory bulb, to the brain. The loss of smell, which can be an early symptom of COVID-19,56 favors this mechanism. Moreover, it has been postulated that SARS-CoV-2 can cause viremia reaching the cerebral circulation via systemic spread. The slow microcirculation at the capillary level may also facilitate the interaction of the S glycoprotein of SARS-CoV-2 with the ACE2 expressed on endothelial cells.
Brain renin angiotensin system in pathogenesis of stroke
The renin-angiotensin system (RAS) plays several physiological roles, including electrolyte homeostasis, cardiovascular control, and regulation of body fluid volume.57 RAS includes angiotensinogen (AGT), renin, angiotensin I (Ang I), angiotensin II (Ang II), ACE, ACE2, angiotensin type-1 receptor (AT1R), angiotensin type-2 receptor (AT2R), and Mas receptor (MAS). Brain RAS has similar components to that of the peripheral RAS. The BBB insulates the brain from the peripheral RAS preventing the diffusion of Ang II from blood circulation into the brain.58 The brain also has the ability to synthesize its own Ang II,59 which is involved in central brain RAS activities.60 However, peripheral angiotensins may interact with brain RAS at the circumventricular organs that lack BBB.61 In many areas of the brain, AGT and renin are co-expressed.62 Most of AGT is expressed in the astrocytes.63, 64, 65 ACE is expressed in the endothelium of cerebral vasculature; it is also highly expressed in choroid plexus, organum vasculosum of the lamina terminalis, area postrema, and subfornical organ.66
In the classical axis (ACE-Ang II-AT1R), renin first cleaves AGT to Ang I. Having been hydrolyzed by ACE, Ang I is converted to Ang II that in turns simulate AT1R and AT2R. Ang II has a higher affinity to AT1R where it exerts its main physiological effects by mediating vasoconstriction, neuroinflammation, oxidative stress, apoptosis, and cellular proliferation,67 see Fig. 1. In the alternative axis (ACE2-Ang (1–7)-Mas), ACE2 cleaves Ang II to Ang (1–7), which is a ligand for the Mas receptor. Activation of this axis results in vasodilation, angiogenesis, anti-inflammatory, antioxidant, and anti-apoptotic responses.67 Over-activation of the ACE/Ang II/AT1R axis can serve an important role in the pathogenesis of acute ischemic stroke through its vasoconstrictor effects upon cerebral vessels, in addition to pro-fibrotic, pro-inflammatory, and increased oxidative stress impact upon the brain parenchyma.68 Conversely, brain ACE2-Ang-(1-7)-MAS axis is an important regulator of blood pressure that counteracts the pressor effect of ACE-Ang II-AT1R axis in the brain.69
A larger metabolic penumbra volume and higher cerebral blood flow (CBF) in the core and penumbra were observed in AT1R knockout mice with a permanent middle cerebral artery (MCA) occlusion, compared to wild-type controls; mice with overexpression of human renin and AGT genes had large infarcts.70 , 71 Ang II has been shown to increase contractile response in isolated MCAs subsequent to MCA occlusion through AT1R72 and impair cerebral perfusion post occlusion.67
Antihypertensive effect of RAS alternative axis
Activation of ACE2-Ang-(1-7)-Mas may have protective effects against stroke by blunting the ACE-Ang II-AT1R axis. ACE2-Ang-(1-7)-Mas pathway also exerts antihypertensive property by directly affecting the classical RAS system in the CNS. In catecholaminergic neurons, ACE2 overexpression has been demonstrated to lessen the Ang II-induced upregulation of AT1R.73 In the brain, ACE2 overexpression normalizes baroreflex dysfunction, improves parasympathetic tone, and attenuates sympathetic activity.74 In a mouse neuroblastoma cell line treated with Ang II, overexpression of ACE2 has been associated with a reduction in reactive oxygen species (ROS) levels.75
Vascular effect and angiogenesis role of RAS alternative axis
Improvement of angiogenesis arising from the activity of the alternative RAS axis is a protective mechanism against cerebral ischemia. After ischemic stroke, the priming of endothelial progenitor cells with ACE2 improves angiogenesis in the peri-infarct region of the cerebral cortex in mice.76 Intraventricular infusion of Ang-(1-7) markedly improved brain capillary density,77 while ACE2 overexpression in neurons increased angiogenic cytokine level and augment CBF in stroke.78
Antithrombotic effect of RAS alternative axis
Activation of ACE2-Ang-(1-7)-Mas axis induces antithrombotic activity. It has been shown that ACE2 activation inhibited thrombus formation and platelet adhesion to the vessel walls among spontaneously hypertensive rats.79 Infusion of Ang-(1-7) (1, 10, or 100 pmol/kg/min for 2 hours) in rats with venous thrombosis resulted in a 50-70% decrease in the amount of thrombus.80 This was reversed in a dose-dependent manner by co-treatment with a selective Ang-(1-7) receptor antagonist (A-779) or AT1R antagonist (EXP 3174) but not by AT2R antagonist (PD 123,319). Additionally, the antithrombotic effect of captopril (an ACE inhibitor) and losartan (an AT1R blocker) were dose-dependently weakened by administering A-779. Concomitant treatment of N G-nitro-l-arginine methyl ester (NO synthase inhibitor) and indomethacin (prostacyclin synthesis inhibitor) annulled the effect of Ang-(1-7).80 In Mas+/+ mice, Ang-(1-7) was seen to inhibit thrombus formation, which was annulled in Mas-knockout mice; NO release stimulated by Ang-(1–7) was blocked in platelets of Mas-knockout mice; and Mas deficiency significantly decreased bleeding time.81
Antiatherosclerotic effect of the RAS alternative axis
Recent evidence has shown that Ang-(1-7) inhibits atherosclerosis and increases stability of atherosclerotic plaques by decreasing smooth muscle cell proliferation and migration, as well as regulating lipid metabolism. By suppressing P38 mitogen-activated protein kinase (MAPK) phosphorylation and attenuating nuclear translocation of NF- кB, Ang-(1-7) downregulates Ang-II-induced intercellular adhesion molecule 1 (ICAM-1) and vascular cell adhesion molecule 1 (VCAM-1).82 , 83 These findings suggest a role for Ang-(1-7) in modulating endothelial cell adhesion molecules. ACE2-Ang-(1-7)-Mas axis activation can decrease atherosclerosis development and progression through the inhibition of vascular smooth muscle cell proliferation and restoration of endothelial function, and lower the risk of ischemic stroke.84 In the abdominal aorta of rabbits, ACE2 overexpression has been found to give rise to more stable plaques with less lipid deposition, fewer macrophages, and more collagen content.85
Neuroprotective and antioxidant effects of RAS alternative axis
ACE2-Ang-(1-7)-Mas axis has neuroprotective properties following ischemia. Ang-(1-7) infusion considerably lowered the ischemia-induced rise in malondialdehyde, a biomarker of oxidative stress that is markedly elevated following ischemic stroke, and improved superoxide dismutase activity in peri-infarct tissue of rat brain.84 These effects were reversed by A-779, indicating that Mas receptor plays a role in the antioxidative action of Ang-(1-7).84 Activation of the alternative RAS axis restricts neuronal cell death by diminishing oxidative stress. Ang-(1-7) can decrease the levels of inducible NO synthase (iNOS), a pro-oxidant molecule, which is increased in patients with stroke.86 Moreover, the infusion of Ang-(1-7) resulted in a marked reduction in NF-кB activity and a decrease in expression of TNF-α, IL-1β and COX-2 in peri-infarct tissue. These data overall suggest that Ang-(1-7) may have neuroprotective effects during the early phase of cerebral ischemia through the suppression of the inflammatory response.
COVID-19 and RAS
The degree of ACE2 expression is associated with the extent of infectivity by SARS-CoV and SARS-CoV-2.87 , 88 Endogenous Ang II is suggested to prevent COVID-19 infection. Ang II binds to ACE2 during its conversion to Ang-(1-7),89 competing with the SARS-CoV-2 for ACE2. Ang II binds to AT1R and triggers ACE2 internalization and downregulation via an ERK1/2 and p38 MAP kinase pathway both in vitro and in vivo,90 , 91 and Ang II leads to AT1R-dependent destruction of ACE2 via ubiquitination and transport into lysosomes.9
In SARS-CoV-2 infection, binding of the S glycoprotein to ACE2 may lead to ACE2 downregulation,93 which in turn results in a higher formation of Ang II by ACE, with less ACE2 to convert to Ang-(1-7).94 Greater availability of ACE due to the infection activates the classical RAS axis, which can have an important role in promoting ischemia through its vasoconstrictor effect on cerebral arteries, in addition to pro-fibrotic, pro-inflammatory, and increased oxidative stress impact on brain parenchyma. Overactivation of the classical RAS pathway underactivates alternative RAS signaling and results in lower vasodilation, angiogenesis, anti-inflammatory, antioxidant, and anti-apoptotic responses, as well as lower antithrombotic, antiatherosclerotic, and neuroprotective effects.
ACE inhibitors (ACEI), AT1R blockers (ARB) such as thiazolidinediones, and mineralocorticoid receptor blockers (MRB) such as pioglitazone and ibuprofen induce ACE2 expression that is in contrast with the inhibitory effects on the ACE2-Ang-(1-7)-axis by gluco-corticoids.95 Moreover, diabetic patients overexpress ACE2.96 The above-mentioned hypothesis has raised some preliminary concerns regarding the use of these drugs in patients with diabetes mellitus (DM) and cardiovascular diseases, which may be affected by COVID19. However, in a retrospective, multi-center study of 1128 adult patients with hypertension diagnosed with COVID-19, 188 patient taking ACEI/ARB had a lower all-cause mortality than non-ACEI/ARB group (adjusted HR = 0.42; 95% CI: 0.19–0.92; P = 0.03).97 This study suggests, although with its conceptual limitations (as ACEI and ARB treatment were not evaluated dependably), that the interaction between SARS-CoV-2 and the ACE2 receptor is more complex than we can actually realize. Based on currently available data, ACEI and ARB therapy should be maintained or initiated in patients with heart failure, hypertension, and/or MI according to current guidelines, irrespective of SARS-CoV-2 status.
Recombinant ACE2 a potential therapy for COVID-19
ACE overactivation and ACE2 underactivition is involved in lung injury. Therefore, ACE2 treatment may itself slow down viral entry into cells88 , 98, hence viral spread, and protect the lung from injury99, 100, 101, 102. Intravenous recombinant human ACE2 (rhACE2; APN01, GSK2586881) was given to healthy subjects in a randomized clinical trial (RCT) in order to assess pharmacodynamics, pharmacokinetics, safety, and tolerability of rhACE2.103 Consequently, it was demonstrated that the therapy was well-tolerated. Although considerable changes were observed in RAS peptide concentrations, cardiovascular effects were not seen.103 Administration of the rhACE2 was also evaluated in patients with respiratory distress syndrome in an RCT.104 However, the study was not adequately powered to determine changes in acute physiology or clinical outcomes.
COVID-19 and stroke epidemiology
Some COVID-19 patients develop strokes, seizures, confusion, and brain inflammation.105 Early case reports described a Chinese patient with COVID-19 with left hemiparesis due to acute cerebral infarction and large blood vessel occlusion,106 as well as a patient with COVID-19 with massive intracerebral hemorrhage (ICH) without prior history of arterial hypertension or anticoagulant use.107 Guan et al.36 showed that cerebrovascular morbidity was seen in 1.4% and headache in 13.6% of patients with COVID-19. In another study, cerebrovascular morbidity, dizziness, and headache have been noted in 5.1%, 9.4%, and 6.5%, respectively, among COVID-19 patients.7 In a further study, among 214 patients with COVID-19, acute cerebrovascular disease was found in 6 (2.8%).25 Comparing severe and moderate COVID-19 patients, neurologic symptoms (45.5% vs 30.2%) such as acute cerebrovascular diseases (5.7% vs 0.8%) and impaired consciousness (14.8% vs 2.4%) were observed more often among severe COVID-19 patients.24 Helms et al.18 studied 58 patients with COVID-19 of which 13 had brain MRI. The authors reported ischemic strokes in 3 of the 13 patients (23%). Table 1 summarizes the evidence of cerebrovascular disease in patients with COVID-19. Needless to say, the reported rate of neurological symptoms among COVID-19 patients is probably a gross underestimate as many of these patients are sedated and on ventilators.105
Table 1.
Evidence of cerebrovascular disease in patients with COVID-19
| Authors | Study design | Results |
|---|---|---|
| Zhao et al., 2020106 | Case report | Acute cerebral infarction and large blood vessel occlusion |
| Sharifi-Razavi et al., 2020107 | Case report | Massive intracerebral hemorrhage |
| Wang et al., 20207 | Retrospective study | Cerebrovascular morbidity in 7 out of 138 patients (5.1%) with COVID-19. |
| Helms et al., 202018 | Retrospective study | Ischemic stroke in 23% of patients with COVID-19 with MRI. |
| Mao et al., 202024 | Retrospective study | Acute cerebrovascular disease in 6 (2.8%) out of 214 patients with COVID-19. The acute cerebrovascular disease was seen more frequently in patients with severe patients with COVID-19, compared to non-severe patients with COVID-19 (5.7% vs 0.8%). |
| Guan et al., 202036 | Retrospective study | Cerebrovascular morbidity in 1.4% of COVID-19 patients. |
The epidemiological data on stroke incidence during the COVID-19 pandemic are not published yet, but anecdotal observations and single-center experiences suggest an increase of thromboembolic stroke among younger adults,33 a reduction of stroke admissions to Emergency Departments (EDs)108 of both mild and severe strokes. Reasons for these observations can be multifactorial, and any attempt to explain this phenomenon is highly speculative at the moment. Only a well-designed worldwide epidemiological study can shed a light on the true incidence of COVID-19 related stroke and the underlying causes.
Fig. 2 presents a non-contrast head CT showing posterior fossa ICH with acute obstructive hydrocephalus in a hospitalized COVID-19 positive 54-year old patient with history of asthma, DM, supraventricular tachycardia, sickle cell trait, and obstructive sleep apnea. The patient had been anticoagulated with low-molecular weight heparin and then switch to unfractionated heparin due to elevated D-dimer levels.
Fig. 2.
Non-contrast head CT showing posterior fossa ICH with acute obstructive hydrocephalus in a COVID-19 positive patient.
Possible impact of COVID-19 on the clinical stroke practice
A peculiar observation has been noted worldwide during the COVID-19 pandemic. Stroke presentations (as well as other acute emergencies) to EDs have declined, with some areas reporting a significant decline.108 The reasons for these observations are not fully clear, as yet. Some have speculated a decline in incidence, perhaps related a decrease of other respiratory infections. This may be attributed to improved hand-washing frequency and social distancing practices, which would also limit the spread of other infections linked to strokes. Another plausible explanation may reflect patients’ reluctance to come to EDs (particularly with mild non-disabling strokes) due to fear of exposure to the SARS-CoV-2 virus or the perception that EDs are crowded and overwhelmed that cannot provide proper care. In this regard, it is of the utmost importance to educate patients and the public at large, that this is not the case, as EDs have taken precautions to ensure patients and caregivers are protected and hospitals remain the best place to receive timely and appropriate care for time-sensitive acute emergencies such as acute ischemic strokes. Hospital administrations should also ensure patients safety through appropriate preventive measures and the use of personal protective equipment (PPE). Many important aspects of patient evaluation and care can be performed via telemedicine. Early supported discharge services should be organized for patients suffering from acute strokes with or without confirmed COVID-19.
In areas with COVID-19 case surges, stroke rates do appear to be elevated as well. Estimates from Wuhan stated that 5% of COVID-19 patients had a concomitant stroke.24 Reports from New York suggest that numbers of emergent large vessel occlusion (ELVO) strokes were significantly elevated, occurring in younger patients without vascular risk factors.109 At-risk areas should have plans in place to handle these potential increased volumes, as well as ensure treating teams have adequate training and PPE to handle SARS-CoV-2 positive stroke patients.
Concluding remarks
COVID-19 is a ferocious global health threat. It is apparent that some patients with COVID-19 manifest neurological symptoms, including strokes. CAC, a crucial condition of this disease, is likely caused by inflammation, including an inflammatory cytokine storm. Recent studies have also suggested axonal transport of SARS-CoV-2 via the cribriform plate to the olfactory bulb to the brain. The process of internalization of SARS-CoV-2 occurs when S glycoprotein of the virus binds to ACE2 on cellular membranes. ACE2 is expressed in several tissues and organs, including the respiratory system, gastrointestinal tract, and brain. SARS-CoV-2 induces downregulation of ACE2. This can overactivate the classical RAS axis, as well as underactivate the alternative RAS signaling in the brain. The consequent imbalance in vasodilation, neuroinflammation, oxidative stress, and thrombogenesis can contribute to stroke pathophysiology during SARS-CoV-2 infection. Anecdotal observations highlight the challenges of treating COVID-19 patients who have strokes that further complicate the care for these severely ill patients. Although the lungs are ground zero in COVID-19 patients, SARS-CoV-2 can also affect other organs such as the brain, heart, vascular system, and kidneys.105 Unlike our earlier understanding that COVID-19 was similar to a “regular flu”, we now know that SARS-CoV-2 acts like no other pathogen scientists and clinicians have previously experienced, as it can attack several organs, causing significant and permanent damage. Standing orders and protocols should be modified to provide better individualized care for stroke patients vis-à-vis COVID-19.
Declaration of Competing Interest
The authors declare no conflict of interest with regard to this paper.
References
- 1.Zhou P., Yang X.-L., Wang X.-G. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu A., Peng Y., Huang B. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27:325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He F., Deng Y., Li W. Coronavirus disease 2019: What we know? J Med Virol. 2020 doi: 10.1002/jmv.25766. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y., Wang Y., Chen Y. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92:568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. https://www.who.int/csr/sars/country/table2004_04_21/en/. Published Dec 31, 2003. Accessed April 28, 2020.
- 6.WHO. Middle East respiratory syndrome coronavirus (MERS-CoV). https://www.who.int/emergencies/mers-cov/en/. Accessed May 18, 2020.
- 7.Wang D., Hu B., Hu C. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Coronavirus (COVID-19). https://covid19.who.int/. Published 2020. Accessed April 28, 2020.
- 9.Liu J., Liao X., Qian S. Community transmission of severe acute respiratory syndrome Coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2606.200239. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan J.F.-W., Yuan S., Kok K.-H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Eng J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/s0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ong S.W.X., Tan Y.K., Chia P.Y. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020 doi: 10.1001/jama.2020.3227. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xia J., Tong J., Liu M. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92:589–594. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen T., Wu D., Chen H. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bohmwald K., Gálvez N.M.S., Ríos M. Neurologic alterations due to respiratory virus infections. Front Cell Neurosci. 2018;12:386. doi: 10.3389/fncel.2018.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robinson C.P., Busl K.M. Neurologic manifestations of severe respiratory viral contagions. Crit Care Explor. 2020;2:e0107. doi: 10.1097/CCE.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Helms J., Kremer S., Merdji H. Neurologic features in severe SARS-CoV-2 Infection. N Eng J Med. 2020 doi: 10.1056/NEJMc2008597. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toscano G., Palmerini F., Ravaglia S. Guillain–Barré syndrome associated with SARS-CoV-2. N Eng J Med. 2020 doi: 10.1056/NEJMc2009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao H., Shen D., Zhou H. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19:383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Giacomelli A., Pezzati L., Conti F. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis. 2020;70 doi: 10.1093/cid/ciaa330. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menni C, Valdes A, Freydin MB, et al. Loss of smell and taste in combination with other symptoms is a strong predictor of COVID-19 infection. medRxiv2020:2020.2004.2005.20048421. doi: 10.1101/2020.04.05.20048421. [DOI]
- 23.Madjid M., Safavi-Naeini P., Solomon S.D. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1286. [ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Mao L., Jin H., Wang M. Neurologic manifestations of hospitalized patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y., Xiao M., Zhang S. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Eng J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conti P., Ronconi G., Caraffa A. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents. 2020;34 doi: 10.23812/CONTI-E. [ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Hamming I., Timens W., Bulthuis M.L. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arabi Y.M., Balkhy H.H., Hayden F.G. Middle east respiratory syndrome. N Eng J Med. 2017;376:584–594. doi: 10.1056/NEJMsr1408795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tang N., Li D., Wang X. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xie Y., Wang X., Yang P. COVID-19 complicated by acute pulmonary embolism. Radiol Cardiothorac Imaging. 2020;2 doi: 10.1148/ryct.2020200067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ullah W., Saeed R., Sarwar U. COVID-19 complicated by acute pulmonary embolism and right-sided heart failure. JACC Case Rep. 2020 doi: 10.1016/j.jaccas.2020.04.008. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Middeldorp S., Coppens M., van Haaps T.F. Incidence of venous thromboembolism in hospitalized patients with COVID-19. Preprints. 2020;2020040345 doi: 10.20944/preprints202004.0345.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klok F.A., Kruip M., van der Meer N.J.M. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.013. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tang N., Bai H., Chen X. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 doi: 10.1111/jth.14817. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levi M., Toh C.H., Thachil J. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol. 2009;145:24–33. doi: 10.1111/j.1365-2141.2009.07600.x. [DOI] [PubMed] [Google Scholar]
- 36.Guan W.J., Ni Z.Y., Hu Y. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Han H., Yang L., Liu R. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 2020 doi: 10.1515/cclm-2020-0188. [ahead of print] [DOI] [PubMed] [Google Scholar]
- 38.Magro C., Mulvey J.J., Berlin D. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020 doi: 10.1016/j.trsl.2020.04.007. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vaninov N. In the eye of the COVID-19 cytokine storm. Nat Rev Immunol. 2020 doi: 10.1038/s41577-020-0305-6. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schett G., Sticherling M., Neurath M.F. COVID-19: risk for cytokine targeting in chronic inflammatory diseases? Nat Rev Immunol. 2020 doi: 10.1038/s41577-020-0312-7. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marchetti C., Swartzwelter B., Koenders M.I. NLRP3 inflammasome inhibitor OLT1177 suppresses joint inflammation in murine models of acute arthritis. Arthritis Res Ther. 2018;20:169. doi: 10.1186/s13075-018-1664-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McNab F., Mayer-Barber K., Sher A. Type I interferons in infectious disease. Nat Rev Immunol. 2015;15:87–103. doi: 10.1038/nri3787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Herold T, Jurinovic V, Arnreich C, et al. Level of IL-6 predicts respiratory failure in hospitalized symptomatic COVID-19 patients. medRxiv2020:2020.2004.2001.20047381. doi: 10.1101/2020.04.01.20047381. [DOI]
- 44.Elkind M.S.V., Ramakrishnan P., Moon Y.P. Infectious burden and risk of stroke: the northern Manhattan study. Arch Neurol. 2010;67:33–38. doi: 10.1001/archneurol.2009.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Esenwa C.C., Elkind M.S. Inflammatory risk factors, biomarkers and associated therapy in ischaemic stroke. Nat Rev Neurol. 2016;12:594–604. doi: 10.1038/nrneurol.2016.125. [DOI] [PubMed] [Google Scholar]
- 46.Shaafi S., Sharifipour E., Rahmanifar R. Interleukin-6, a reliable prognostic factor for ischemic stroke. Iran J Neurol. 2014;13:70–76. [PMC free article] [PubMed] [Google Scholar]
- 47.Hoffmann M., Kleine-Weber H., Schroeder S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. .e278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wrapp D., Wang N., Corbett K.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Letko M., Marzi A., Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xu H., Zhong L., Deng J. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu C, Zheng S, Chen Y, et al. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCoV, in the nasal tissue. medRxiv2020:2020.2002.2011.20022228. doi: 10.1101/2020.02.11.20022228. [DOI]
- 52.Wu C., Zheng M. Single-cell RNA expression profiling shows that ACE2, the putative receptor of COVID-2019, has significant expression in nasal and mouth tissue, and is co-expressed with TMPRSS2 and not co-expressed with SLC6A19 in the tissues. BMC Infect Dis. 2020 doi: 10.21203/rs.3.rs-16992/v1. Preprints. [DOI] [Google Scholar]
- 53.Baig A.M., Khaleeq A., Ali U. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11:995–998. doi: 10.1021/acschemneuro.0c00122. [DOI] [PubMed] [Google Scholar]
- 54.Dahm T., Rudolph H., Schwerk C. Neuroinvasion and inflammation in viral central nervous system infections. Mediators Inflamm. 2016;2016 doi: 10.1155/2016/8562805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Swanson P.A., II, McGavern D.B. Portals of viral entry into the central nervous system. In: Dorovini-Zis K., editor. The Blood-Brain Barrier in Health and Disease, Volume Two: Pathophysiology and Pathology. CRC Press; Cleveland, OH: 2015. [Google Scholar]
- 56.Eliezer M., Hautefort C., Hamel A.L. Sudden and complete olfactory loss function as a possible symptom of COVID-19. JAMA Otolaryngol Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0832. [ahead of print] [DOI] [PubMed] [Google Scholar]
- 57.Abiodun O.A., Ola M.S. Role of brain renin angiotensin system in neurodegeneration: an update. Saudi J Biol Sci. 2020;27:905–912. doi: 10.1016/j.sjbs.2020.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schelling P., Hutchinson J.S., Ganten U. Impermeability of the blood-cerebrospinal fluid barrier for angiotensin II in rats. Clin Sci Mol Med Suppl. 1976;3:399s–402s. doi: 10.1042/cs051399s. [DOI] [PubMed] [Google Scholar]
- 59.Harding J.W., Sullivan M.J., Hanesworth J.M. Inability of [125I]Sar1, Ile8-Angiotensin II to move between the blood and cerebrospinal fluid compartments. J Neurochem. 1988;50:554–557. doi: 10.1111/j.1471-4159.1988.tb02946.x. [DOI] [PubMed] [Google Scholar]
- 60.Ferguson A.V., Washburn D.L.S., Latchford K.J. Hormonal and neurotransmitter roles for angiotensin in the regulation of central autonomic function. Exp Biol Med. 2001;226:85–96. doi: 10.1177/153537020122600205. [DOI] [PubMed] [Google Scholar]
- 61.Fry M., Ferguson A.V. The sensory circumventricular organs: Brain targets for circulating signals controlling ingestive behavior. Physiol Behav. 2007;91:413–423. doi: 10.1016/j.physbeh.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 62.Lavoie J.L., Cassell M.D., Gross K.W. Adjacent expression of renin and angiotensinogen in the rostral ventrolateral medulla using a dual-reporter transgenic model. Hypertension. 2004;43:1116–1119. doi: 10.1161/01.hyp.0000125143.73301.94. [DOI] [PubMed] [Google Scholar]
- 63.Grobe J.L., Buehrer B.A., Hilzendeger A.M. Angiotensinergic signaling in the brain mediates metabolic effects of deoxycorticosterone (DOCA)-salt in C57 mice. Hypertension. 2011;57:600–607. doi: 10.1161/hypertensionaha.110.165829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Milsted A., Barna B.P., Ransohoff R.M. Astrocyte cultures derived from human brain tissue express angiotensinogen mRNA. Proc Natl Acad Sci USA. 1990;87:5720–5723. doi: 10.1073/pnas.87.15.5720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sherrod M., Liu X., Zhang X. Nuclear localization of angiotensinogen in astrocytes. Am J Physiol Regul Integr Comp Physiol. 2005;288:R539–R546. doi: 10.1152/ajpregu.00594.2004. [DOI] [PubMed] [Google Scholar]
- 66.Bodiga V.L., Bodiga S. Renin angiotensin system in cognitive function and dementia. Asian J Neurosci. 2013;2013 doi: 10.1155/2013/102602. [DOI] [Google Scholar]
- 67.Arroja M.M.C., Reid E., McCabe C. Therapeutic potential of the renin angiotensin system in ischaemic stroke. Exp Transl Stroke Med. 2016;8:8. doi: 10.1186/s13231-016-0022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wright J.W., Harding J.W. The brain renin-angiotensin system: a diversity of functions and implications for CNS diseases. Pflugers Arch. 2013;465:133–151. doi: 10.1007/s00424-012-1102-2. [DOI] [PubMed] [Google Scholar]
- 69.Feng Y., Xia H., Santos R.A. Angiotensin-converting enzyme 2: a new target for neurogenic hypertension. Exp Physiol. 2010;95:601–606. doi: 10.1113/expphysiol.2009.047407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Walther T., Olah L., Harms C. Ischemic injury in experimental stroke depends on angiotensin II. FASEB J. 2002;16:169–176. doi: 10.1096/fj.01-0601com. [DOI] [PubMed] [Google Scholar]
- 71.Inaba S., Iwai M., Tomono Y. Exaggeration of focal cerebral ischemia in transgenic mice carrying human renin and human angiotensinogen genes. Stroke. 2009;40:597–603. doi: 10.1161/STROKEAHA.108.519801. [DOI] [PubMed] [Google Scholar]
- 72.Stenman E., Edvinsson L. Cerebral ischemia enhances vascular angiotensin AT1 receptor-mediated contraction in rats. Stroke. 2004;35:970–974. doi: 10.1161/01.STR.0000121642.53822.58. [DOI] [PubMed] [Google Scholar]
- 73.Xiao L., Gao L., Zucker I.H. Angiotensin-converting enzyme 2 attenuates the angiotensin II-induced upregulation of angiotensin II type 1 receptor in CATH. A neurons. Hypertension. 2009:E70–E71. Lippincott Williams & WilkinsI 530 Walnut St, Philadelphia, PA 19106-3621 USA. [Google Scholar]
- 74.Xia H., Feng Y., Obr T.D. Angiotensin II Type 1 Receptor–mediated reduction of angiotensin-converting enzyme 2 activity in the brain impairs baroreflex function in hypertensive mice. Hypertension. 2009;53:210–216. doi: 10.1161/HYPERTENSIONAHA.108.123844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xia H., Suda S., Bindom S. ACE2-mediated reduction of oxidative stress in the central nervous system is associated with improvement of autonomic function. PloS One. 2011;6:e22682. doi: 10.1371/journal.pone.0022682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen J., Xiao X., Chen S. Angiotensin-converting enzyme 2 priming enhances the function of endothelial progenitor cells and their therapeutic efficacy. Hypertension. 2013;61:681–689. doi: 10.1161/HYPERTENSIONAHA.111.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jiang T., Yu J.T., Zhu X.C. Angiotensin-(1–7) induces cerebral ischaemic tolerance by promoting brain angiogenesis in a Mas/eNOS-dependent pathway. Br J Pharmacol. 2014;171:4222–4232. doi: 10.1111/bph.12770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen J., Zhao Y., Chen S. Neuronal over-expression of ACE2 protects brain from ischemia-induced damage. Neuropharmacology. 2014;79:550–558. doi: 10.1016/j.neuropharm.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fraga-Silva R.A., Sorg B.S., Wankhede M. ACE2 activation promotes antithrombotic activity. Mol Med. 2010;16:210–215. doi: 10.2119/molmed.2009.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kucharewicz I., Pawlak R., Matys T. Antithrombotic effect of captopril and losartan is mediated by Angiotensin-(1-7) Hypertension. 2002;40:774–779. doi: 10.1161/01.HYP.0000035396.27909.40. [DOI] [PubMed] [Google Scholar]
- 81.Fraga-Silva R.A., Pinheiro S.V.B., Gonçalves A.C.C. The antithrombotic effect of angiotensin-(1-7) involves mas-mediated NO release from platelets. Mol Med. 2008;14:28–35. doi: 10.2119/2007-00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang F., Ren J., Chan K. Angiotensin-(1–7) regulates Angiotensin II-induced VCAM-1 expression on vascular endothelial cells. Biochem Biophys Res Commun. 2013;430:642–646. doi: 10.1016/j.bbrc.2012.11.098. [DOI] [PubMed] [Google Scholar]
- 83.Liang B., Wang X., Zhang N. Angiotensin-(1-7) attenuates angiotensin II-induced ICAM-1, VCAM-1, and MCP-1 expression via the MAS receptor through suppression of P38 and NF-κB pathways in HUVECs. Cell Physiol Biochem. 2015;35:2472–2482. doi: 10.1159/000374047. [DOI] [PubMed] [Google Scholar]
- 84.Jiang T., Gao L., Lu J. ACE2-Ang-(1-7)-Mas axis in brain: a potential target for prevention and treatment of ischemic stroke. Curr Neuropharmacol. 2013;11:209–217. doi: 10.2174/1570159×11311020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dong B., Zhang C., Feng J.B. Overexpression of ACE2 enhances plaque stability in a rabbit model of atherosclerosis. Arterioscler Thromb Vasc Biol. 2008;28:1270–1276. doi: 10.1161/ATVBAHA.108.164715. [DOI] [PubMed] [Google Scholar]
- 86.Bennion D.M., Haltigan E., Regenhardt R.W. Neuroprotective mechanisms of the ACE2-angiotensin-(1-7)-Mas axis in stroke. Curr Hypertens Rep. 2015;17:3. doi: 10.1007/s11906-014-0512-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hofmann H., Geier M., Marzi A. Susceptibility to SARS coronavirus S protein-driven infection correlates with expression of angiotensin converting enzyme 2 and infection can be blocked by soluble receptor. Biochem Biophys Res Commun. 2004;319:1216–1221. doi: 10.1016/j.bbrc.2004.05.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Li W., Moore M.J., Vasilieva N. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chawla L.S., Chen S., Bellomo R. Angiotensin converting enzyme defects in shock: implications for future therapy. Crit Care. 2018;22:274. doi: 10.1186/s13054-018-2202-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Koka V., Huang X.R., Chung A.C. Angiotensin II up-regulates angiotensin I-converting enzyme (ACE), but down-regulates ACE2 via the AT1-ERK/p38 MAP kinase pathway. Am J Pathol. 2008;172:1174–1183. doi: 10.2353/ajpath.2008.070762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fernandes T., Hashimoto N.Y., Magalhães F.C. Aerobic exercise training–induced left ventricular hypertrophy involves regulatory MicroRNAs, decreased angiotensin-converting enzyme-angiotensin II, and synergistic regulation of angiotensin-converting enzyme 2-angiotensin (1-7) Hypertension. 2011;58:182–189. doi: 10.1161/HYPERTENSIONAHA.110.168252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Busse L.W., Chow J.H., McCurdy M.T. COVID-19 and the RAAS—a potential role for angiotensin II? Crit Care. 2020;24:136. doi: 10.1186/s13054-020-02862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang H., Penninger J.M., Li Y. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020 doi: 10.1002/ddr.21656. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ghadhanfar E., Alsalem A., Al-Kandari S. The role of ACE2, angiotensin-(1-7) and Mas1 receptor axis in glucocorticoid-induced intrauterine growth restriction. Reprod Biol Endocrinol. 2017;15:97. doi: 10.1186/s12958-017-0316-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8:e2. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang P., Zhu L., Cai J. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020 doi: 10.1161/CIRCRESAHA.120.317134. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Li F., Li W., Farzan M. Structure of SARS coronavirus spike receptor-binding domain complexed with receptor. Science. 2005;309:1864–1868. doi: 10.1126/science.1116480. [DOI] [PubMed] [Google Scholar]
- 99.Kuba K., Imai Y., Rao S. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus–induced lung injury. Nat Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Imai Y., Kuba K., Rao S. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhang R., Pan Y., Fanelli V. Mechanical stress and the induction of lung fibrosis via the midkine signaling pathway. Am J Respir Crit Care Med. 2015;192:315–323. doi: 10.1164/rccm.201412-2326OC. [DOI] [PubMed] [Google Scholar]
- 102.Wösten-van Asperen R.M., Lutter R., Specht P.A. Acute respiratory distress syndrome leads to reduced ratio of ACE/ACE2 activities and is prevented by angiotensin-(1–7) or an angiotensin II receptor antagonist. J Pathol. 2011;225:618–627. doi: 10.1002/path.2987. [DOI] [PubMed] [Google Scholar]
- 103.Haschke M., Schuster M., Poglitsch M. Pharmacokinetics and pharmacodynamics of recombinant human angiotensin-converting enzyme 2 in healthy human subjects. Clin Pharmacokinet. 2013;52:783–792. doi: 10.1007/s40262-013-0072-7. [DOI] [PubMed] [Google Scholar]
- 104.Khan A., Benthin C., Zeno B. A pilot clinical trial of recombinant human angiotensin-converting enzyme 2 in acute respiratory distress syndrome. Crit Care. 2017;21:234. doi: 10.1186/s13054-017-1823-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wadman M., Couzin-Frankel J., Kaiser J. A rampage through the body. Science. 2020;368:356–360. doi: 10.1126/science.368.6489.356. [DOI] [PubMed] [Google Scholar]
- 106.Zhao J., Rudd A., Liu R. Challenges and potential solutions of stroke care during the Coronavirus Disease 2019 (COVID-19) outbreak. Stroke. 2020 doi: 10.1161/strokeaha.120.029701. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sharifi-Razavi A., Karimi N., Rouhani N. COVID 19 and Intra cerebral hemorrhage: causative or coincidental. New Microbes New Infect. 2020;35 doi: 10.1016/j.nmni.2020.100669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Morelli N., Rota E., Terracciano C. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020 doi: 10.1159/000507666. [ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, et al. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382:e60 [DOI] [PMC free article] [PubMed]