Abstract
Aims
The mental health of youth is continually changing and requires reliable monitoring to ensure that adequate social and economic resources are allocated. This study assessed trends in mental health among Canadian youth, 12–24 years old. Specifically, we examined the prevalence of poor/fair perceived mental health, diagnosis of mood and anxiety disorders, suicidality, perceived stress and sleep problems, substance use, and mental health consultations.
Methods
Data were collected from eight cycles of the annual Canadian Community Health Survey (2011–2018). Prevalence of mental health outcomes was calculated from each survey, and meta-regression was used to assess trends over time. In the absence of a significant trend over time, the eight cycles were pooled together using meta-analysis techniques to gain precision. Trends in prevalence were assessed for the overall sample of youth (12–24 years) and separately for male and female adolescents (12–18 years) and young adults (19–24 years).
Results
The prevalence of poor/fair perceived mental health, diagnosed mood and anxiety disorders, and past-year mental health consultations increased from 2011 to 2018, most strongly among young adult females. Past-year suicidality increased among young adult females but did not change for other age and sex groups. Notably, the prevalence of binge drinking decreased by 2.4% per year for young adult males, 1.0% for young adult females and 0.7% per year for adolescent males, while staying relatively stable for adolescent females. Prevalence of cannabis use declined among adolescents before legalisation (2011–2017); however, this trend did not persist in 2018. Instead, the 2018 prevalence was 5.6% higher than the 2017 prevalence (16.3 v. 10.7%). The combined prevalence of other illicit drug use was stable at 4.6%; however, cocaine use and hallucinogens increased by approximately 0.2% per year.
Conclusions
Our findings highlight a growing need for youth mental health services, as indicated by a rise in the prevalence of diagnosed mood and anxiety disorders and past-year mental health consultations. The reason for these observed increases is less apparent – it may represent a true rise in the prevalence of mental illness, or be an artefact of change in diagnostic practices, mental health literacy or diminishing stigma. Nonetheless, the findings indicate a need for the health care system to respond to the rising demand for mental health services among youth.
Key words: Adolescents, mental health, population survey, psychiatric services
Introduction
Mental health is an important dimension of overall health, the absence of which contributes to morbidity and mortality worldwide (Whiteford et al., 2013; Ferrari et al., 2014). Mental disorders are a leading cause of years lived with disability (YLD) and disability-adjusted life years (DALY), of which depression and anxiety are main contributors (Whiteford et al., 2013; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018). Substance use disorders also contribute to the burden of morbidity and mortality, accounting for 17.3% of YLDs, 20.5% of DALYs and 86.1% of years of life lost (Whiteford et al., 2013). While the burden of mental disorders spans the life course, the majority of conditions emerge during adolescence and early adulthood, typically by the age of 24 years old (Kessler et al., 2005).
The transition from adolescence to adulthood is a critical period due to the long-term impacts of unattained academic achievement and lost work productivity throughout the life course (Ratnasingham et al., 2013). Adolescence is afflicted with underlying personal, academic and social pressures that impose additional strain on mental health (Acharya et al., 2018). The inability to handle these stressors can contribute to unhealthy behaviours, including poor sleeping habits, limited physical activity and inadequate diet (Becker et al., 2018; Jao et al., 2018; Murphy et al., 2018; Wattick et al., 2018). Substance use disorders are also common, with 11% of adolescents in the USA (13–18 years old) reporting either an alcohol (6.4%) or drug-related disorder (8.9%) in their lifetime (Merikangas et al., 2010).
To understand the changing state of mental health among youth, it becomes necessary to monitor trends in mental disorders and related symptoms over time. In response to this need, research has examined trends in youth mental health outcomes over recent decades, including symptoms of depression and anxiety, suicidality, substance use and mental health service use. In the following paragraphs, the literature from high-income countries will be summarised over the past decade, most of which was conducted in Europe, Australia, the USA and Canada.
The literature on trends in mental illness has reported conflicting findings. In the UK, the prevalence of self-reported long-standing mental health conditions increased between 2011 and 2014 among 16–24 years old youth in England (2.8–5.9%; OR = 1.25, p < 0.01) and Scotland (5.5–9.7%; OR = 1.19, p = 0.03) (Pitchforth et al., 2018). Similarly, in Wales, the proportion of youth who reported current treatment for a mental illness rose from 5.4% in 2011 to 6.5% in 2014 (OR = 1.14, p < 0.01) (Pitchforth et al., 2018). In Iceland, mean symptom levels of depression and anxiety increased from 2006 to 2016 among female adolescents, with males reporting no change or even reduced symptoms of anxiety over time (Thorisdottir et al., 2017). In contrast, studies from the USA and Australia reported symptom-based measures of depression and anxiety to increase for males and females (Sawyer et al., 2018; Keyes et al., 2019), while Canadian studies reported either an increase for males alone (Comeau et al., 2019) or no change (McMartin et al., 2014; Wiens et al., 2017).
The research on trends in suicidality suggests an increase in suicidality among youth in the USA but not Canada. A 2019 US study reported an increase in the past-year prevalence of suicidality (suicidal ideation, plans and attempts) from 2008 to 2017 among 18–25 years old youth (sex differences were not examined) (Twenge et al., 2019). Of the limited research on sex-specific trends, one study reported a decrease in suicidality for both sexes from 1991 to 2011 (no change in suicide attempts among males) (Lowry et al., 2014), while another reported an increase in the prevalence of suicidality from 2009 to 2015 (no change in suicide attempts among males) (Han et al., 2018). In Canada, the prevalence of self-reported suicidal ideation and attempts decreased among 11–14 years old adolescents from 1998 to 2010 (McMartin et al., 2014). In Ontario, specifically, rates of mental health visits for self-harm decreased for youths aged 13–17 years between 2003 and 2009 but subsequently increased until 2017 (Gardner et al., 2019).
Trends in alcohol use were consistent across studies, with a decline in prevalence reported in Finland (1998–2014) (Mishina et al., 2018), England (2005–2015) (Ng Fat et al., 2018) and the USA (1999–2013) (Johnson et al., 2015). For cannabis use, however, inconsistent findings emerged within the USA. In one study, lifetime cannabis use followed a U-pattern among adolescents between 1999 and 2013. The prevalence was higher among males; however, sex differences narrowed over time (Johnson et al., 2015). In another study, a 2.5% annual decrease in cannabis use disorders was reported from 2003 to 2014 among adolescents 12–17 years old (Grucza et al., 2018). Similarly, in Canada, the prevalence of cannabis use among youth declined over the past decade, with a sudden increase reported in the past year, perhaps due to impending legalisation in 2018 for people aged 18 years and above (Leos-Toro et al., 2019; Zuckermann et al., 2019).
Finally, a rise in the provision of mental health care for youth has been reported in recent decades in the USA and Canada. The proportion of youth 12–17 years old who used outpatient mental health services in the USA increased from 9.0% (1996–1998) to 14.0% (2010–2012) (Olfson et al., 2015). In Canada, mental health-related emergency department visits, hospitalisations and outpatient visits among youth increased from 2006 to 2011 (Gandhi et al., 2016). Moreover, in Ontario, specifically, the rates of mental health emergency department visits among youth increased from 11.7 per 1000 in 2003 to 24.1 per 1000 in 2017 (Gardner et al., 2019). Given the improvements in the treatment of mental disorders (Patten et al., 2016), it is necessary to monitor whether gains in treatment impact trends in youth mental health (Jorm et al., 2017).
The inconsistencies observed in the literature may reflect methodological differences between studies, such as frequency of data collection, age of respondents or incomparable outcomes captured by survey questionnaires. Cross-national differences in the prevalence of mental health outcomes may also explain some of this discrepancy.
Recently, the use of repeated cross-sectional survey data has improved the ability to analyse trends in youth mental health (Thorisdottir et al., 2017; Wiens et al., 2017; Han et al., 2018; Pitchforth et al., 2018; Keyes et al., 2019; Twenge et al., 2019); however, there remains a paucity of research that examines several outcomes simultaneously in a representative sample of Canadian youth. The current study quantifies trends in youth mental health from 2011 to 2018 using nationally representative surveys of the Canadian household population. We assess trends in the prevalence of poor/fair perceived mental health, professionally diagnosed mental illness, perceived stress and sleep problems, suicidality, substance use and mental health service use among Canadian youth 12–24 years old.
Methods
Data source
Data were obtained from eight cycles of the annual Canadian Community Health Survey (CCHS) from 2011 to 2018 (Statistics Canada, 2017). The CCHS is a cross-sectional survey that collects health information from Canadian household residents at least 12 years old. The survey is administered across all provinces and territories, excluding people living on reserves, full-time members of Canadian Armed Forces and residents of institutions and specific remote areas (3% of the Canadian population). Survey respondents were selected using a stratified multistage sampling technique, whereby households were selected from health regions, and an individual was selected from each household. Total (household and respondent) response rates ranged from 58% in 2015 to 70% in 2011. Sampling weights and replicate bootstrap weights were provided by Statistics Canada to account for unequal selection probabilities during sampling. The sampling weights were also adjusted for non-response in order to reduce the risk of selection bias. Participants were eligible for inclusion if they were 12–24 years old (n = 71 700). The annual sample sizes ranged from 7200 in 2018 to 10 700 in 2011 (online Supplementary Table S1).
Demographic measures
Age was dichotomised into adolescents (12–18 years old) and young adults (19–24 years old) to describe the effect of age on the assessment of trends in prevalence. The findings were also stratified by sex (male or female) to quantify any sex differences in mental health trends over time.
Mental health outcomes
The following mental health outcomes were derived from each survey:
Perceived mental health was assessed with the question: ‘In general, would you say your mental health is… excellent, very good, good, fair, or poor?’ The five options were collapsed into two categories: poor/fair v. excellent/very good/good.
Persistent sleep problems were assessed with the question: ‘How often do you have trouble going to sleep or staying asleep… never, rarely, sometimes, all of the time, or most of the time?’ The five options were collapsed into two categories: most/all of the time v. never/rarely/sometimes.
Persistent stress was assessed using a single question ‘Thinking about the amount of stress in your life, would you say that most days are… not at all stressful, not very stressful, a bit stressful, quite a bit stressful, or extremely stressful?’. The five options were collapsed into two categories: quite a bit/extremely stressful v. not at all stressful/not very stressful/a bit stressful.
Mood and anxiety disorders were identified as a self-reported professional diagnosis of each disorder. Participants were asked to report any ‘long-term health conditions which are expected to last or have already lasted 6 months or more and that have been diagnosed by a health professional’. Specifically, they were asked to report if they have ‘a mood disorder such as depression, bipolar disorder, mania or dysthymia’ or ‘an anxiety disorder such as a phobia, obsessive-compulsive disorder or a panic disorder?’
Suicidality was assessed with a set of questions: (i) ‘Have you ever seriously considered committing suicide or taking your own life?’ (ii) ‘Have you ever made a plan to seriously attempt suicide?’ and (iii) ‘Have you ever seriously attempted suicide?’ Each question was followed by: ‘Has this happened in the past 12 months?’ Past-year suicidality was classified as any experience of suicidal ideation, plans or attempts in the past 12 months.
Binge drinking was assessed with the following question: ‘How often in the past 12 months have you had 5 or more drinks on one occasion?’ Past-year binge drinking was identified as five or more drinks consumed in a single occasion at least once a month over the past 12 months.
Drug use was assessed with a set of questions. For example, ‘Have you ever tried marijuana or hashish? Was this in the past 12 months?’ Past-year drug use was divided into two binary variables for the use of cannabis (marijuana or hashish) or other illicit drugs (excluding cannabis) in the past year. Since cannabis was legalised in Canada in 2018, trends in prevalence were examined from 2011–2017 and 2011–2018 to identify whether legalisation altered observed trends. Illicit drug use was further classified by type of drug, including cocaine, amphetamines, ecstasy and hallucinogens.
Consultations were assessed with a single question: ‘In the past 12 months have you seen or talked to a health professional about your emotional or mental health?’ Past-year mental health consultations were classified as at least one visit to a health professional in the past 12 months.
Statistical analysis
Trends in the prevalence of each mental health outcome were examined over time using a two-step meta-analysis approach. First, the prevalence was estimated with 95% confidence intervals (95% CI) from each survey cycle between 2011 and 2018. Sampling weights and bootstrap techniques were applied to account for the complex sampling design. Second, the presence of linear trends in prevalence over time was examined using random-effects meta-regression. Random-effects models were used to account for any heterogeneity between estimates that were not explained by survey year (I2 > 50%; Q-statistic p < 0.05). Random-effects models were applied to all analyses since they are identical to fixed-effects models when heterogeneity is minimal.
While most demographic and mental health variables were included as annual content, certain variables were optional content administered by only some provinces and territories each year (Statistics Canada, 2017). Information on data inclusion and exclusions is provided in online Supplementary Tables S1 and S2. Sensitivity analyses were conducted to ensure inter-provincial differences in prevalence did not drive the observed trends.
All analyses were conducted at the Prairie Regional Data Centre at the University of Calgary using Stata 15 (StataCorp, 2017).
Results
Over the 8-year study period, 71 700 youth participated in the CCHS. Table 1 reports the prevalence estimates, along with meta-regression and meta-analysis output for the total sample of youth 12–24 years old. The prevalence of poor/fair perceived mental health increased from 4.2% in 2011 to 9.9% in 2018, an average increase of 0.8% per year (95% CI 0.5–1.0%). Specifically, there was an increase in the prevalence of poor perceived mental health (Δ = 0.2%; 95% CI 0.0–0.3%; p = 0.036) and fair perceived mental health (Δ = 0.6%; 95% CI 0.4–0.7%; p ≤ 0.001) (online Supplementary Tables S3 and S4). The prevalence of professionally diagnosed mood and anxiety disorders also increased over time, as did past-year suicidality. Diagnosed mood disorders increased from 4.3 to 7.8%, diagnosed anxiety disorder increased from 6.0 to 12.9%, and past-year suicidality increased from 3.0% in 2011 to 5.8% in 2016. Concurrently, the proportion of youth who visited a health care provider for at least one mental health consultation in the past year rose from 11.7% in 2011 to 17.0% in 2018. Over the same period, however, the prevalence of sleep problems and stress remained relatively stable, with nearly 15% of youth reporting persistent sleep problems and 18% of youth reporting persistent stress. Furthermore, the past-year prevalence of binge drinking decreased from 25.5 to 17.6%, representing a decrease of 1% per year (95% CI −1.3 to −0.8%). The prevalence of past-year cannabis use remained stable at a pooled prevalence of 21.4%. Other illicit drug use also appeared stable at 4.6%; however, when separated by drug type, the prevalence increased by 0.2% per year for cocaine use (1.6–3.6%; p = 0.04) and hallucinogen use (1.1–3.1%; p = 0.02). The prevalence of methamphetamine use and ecstasy did not change from 2011 to 2018, with a pooled prevalence of 0.4 and 2.4%, respectively (online Supplementary Tables S5 and S6).
Table 1.
Meta regression and meta-analysis output for the prevalence of poor or fair perceived mental health, professionally diagnosed mental illness, symptoms of stress and sleep problems, suicidality, substance use and mental health service use among youth 12–24 years old from 2011 to 2018 (N = 71 700)
| Prevalence | Meta-regression outputa | Meta-analysis outputb | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | Annual % change (95% CI) | p | Pooled prevalence (95% CI) | I2 | τ2 | |
| Perceived mental health and symptoms of depression | |||||||||||||
| Perceived mental health (poor/fair) | 4.2% | 5.0% | 5.1% | 6.0% | 6.2% | 7.4% | 9.0% | 9.9% | 0.8% (0.5–1.0%) | <0.001 | – | – | – |
| Persistent sleep problems (most/all of the time) | 14.8% | 14.3% | 14.4% | 13.8% | 11.6% | 14.1% | 16.5% | 16.4% | 0.2% (−0.4 to 0.9%) | 0.392 | 14.5% (13.3–15.7%) | 64.3% | 0.0002 |
| Persistent stress (most days are quite a bit/extremely stressful) | 18.4% | 16.8% | 17.1% | 19.1% | 18.1% | 16.0% | 18.3% | 17.6% | 0.0% (−0.6 to 0.5%) | 0.865 | 17.7% (16.9–18.4%) | 58.0% | 0.0001 |
| Mental illness and suicidality | |||||||||||||
| Mood disorder (professional diagnosis) | 4.3% | 5.1% | 5.2% | 5.9% | 7.1% | 7.7% | 7.5% | 7.8% | 0.6% (0.4–0.7%) | <0.001 | – | – | – |
| Anxiety disorder (professional diagnosis) | 6.0% | 6.7% | 7.1% | 8.2% | 10.2% | 11.1% | 10.9% | 12.9% | 1.0% (0.8–1.2%) | <0.001 | – | – | – |
| Suicidality (past 12 months) | 3.0% | 5.7% | 5.1% | 4.6% | 5.3% | 5.8% | – | – | 0.5% (0.1–0.9%) | 0.034 | – | – | – |
| Substance use | |||||||||||||
| Binge drinking (past 12 months) | 25.5% | 22.9% | 23.3% | 21.0% | 20.7% | 19.3% | 19.2% | 17.6% | 1.0% (−1.3 to −0.8%) | <0.001 | – | – | – |
| Cannabis use (past 12 months) | 22.0% | 20.8% | 22.4% | 22.3% | 18.6% | 20.8% | 19.8% | 25.7% | 0.1% (−0.7 to 0.9%) | 0.763 | 21.4% (20.0–22.8%) | 59.3% | 0.0002 |
| Other illicit drug usec (past 12 months) | 4.1% | 4.0% | 5.8% | 4.9% | 4.4% | 5.2% | 4.2% | 6.0% | 0.1% (−0.1 to 0.4%) | 0.249 | 4.6% (4.1–5.0%) | 4.5% | 0.0000 |
| Mental health service use | |||||||||||||
| Mental health consultation (past 12 months) | 11.7% | 11.9% | 11.0% | 11.5% | 14.4% | 15.9% | 17.3% | 17.0% | 0.9% (0.4–1.5%) | 0.004 | – | – | – |
Random-effects meta-regression significance level is α = 0.05 (p < 0.05).
Random-effects meta-analysis significance level is α = 0.05.
Excluding cannabis.
Figures 1–5 display trends in mental health stratified by age and sex groups. The sex- and age-specific prevalence and 95% CIs are reported in online Supplementary Table S7, with meta-regression and meta-analysis output reported in online Supplementary Table S8.
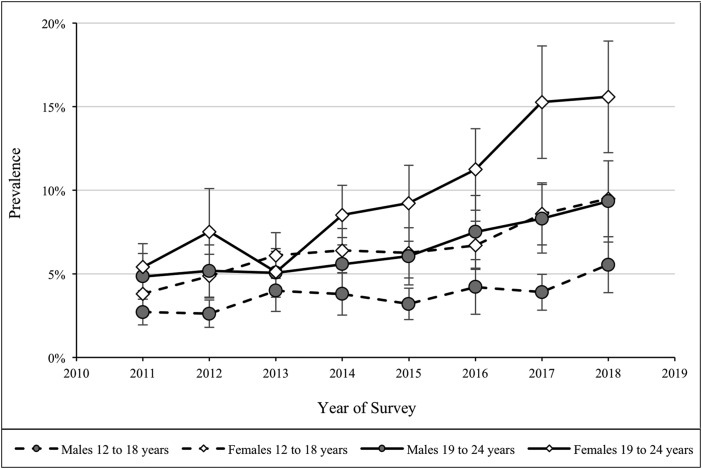
Fig. 1.
Prevalence of perceived poor/fair mental health among youth 12–24 years old, stratified by age and sex groups.
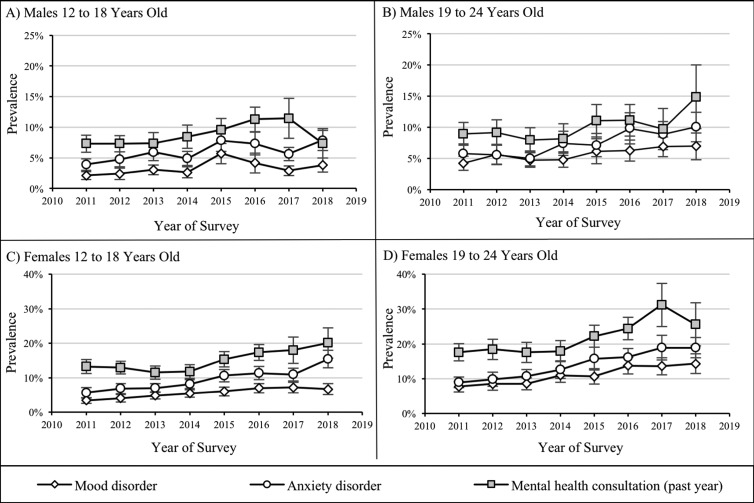
Fig. 2.
Prevalence of professionally diagnosed mood and anxiety disorders and past year prevalence of mental health consultations among youth 12–24 years old, stratified by age and sex groups.
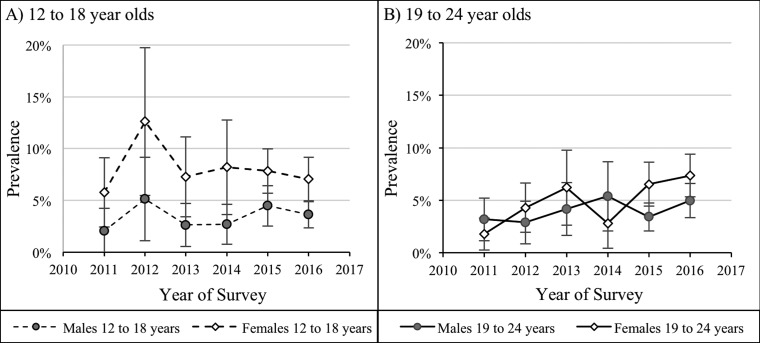
Fig. 3.
Past year prevalence of suicidality among youth 12–24 years old, stratified by age and sex groups.
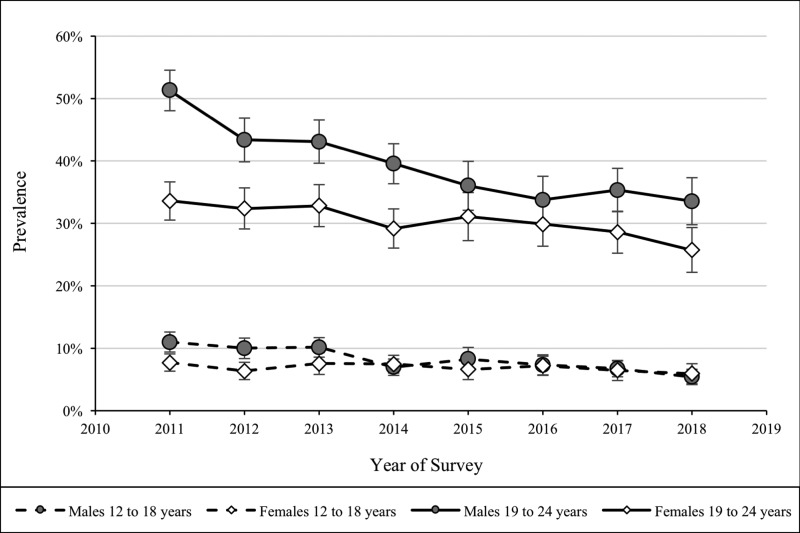
Fig. 4.
Past year prevalence of binge drinking among youth 12–24 years old, stratified by age and sex groups.
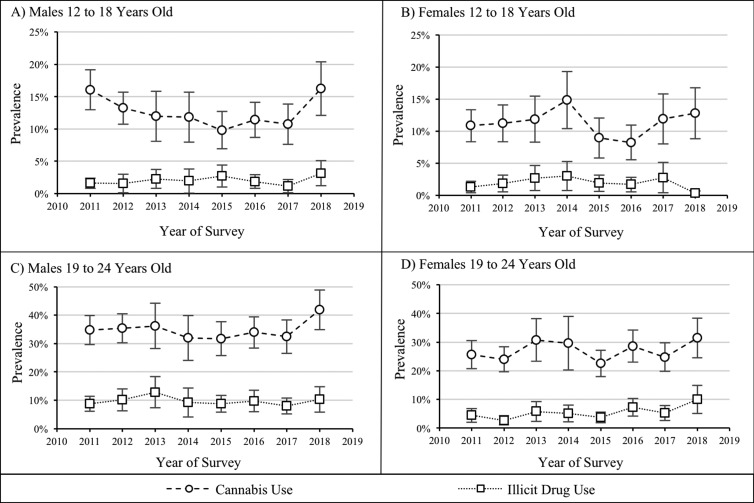
Fig. 5.
Past year prevalence of cannabis use and other illicit drug use among youth 12–24 years old, stratified by age and sex groups.
As shown in Fig. 1, the prevalence of perceived poor/fair mental health increased for all youth between 2011 and 2018, with the largest change among young adult females (5.4–15.6%; p = 0.002), followed by adolescent females (3.8–9.5%; p = 0.001), young adult males (4.8–9.3%; p = 0.006) and adolescent males (2.7–5.5%; p = 0.018). These changes were primarily driven by an increase in fair perceived mental health (online Supplementary Tables S3 and S4).
Figure 2 compares age- and sex-specific trends in the prevalence of professionally diagnosed mood and anxiety disorders with the prevalence of past-year mental health consultations. Over the study period, the prevalence of professionally diagnosed mood disorders and anxiety disorders increased among all age and sex groups (except for mood disorders among adolescent males). The largest rise in prevalence was observed among adolescent females, with increases of 1.0% per year for mood disorders and 1.6% per year for anxiety disorders. The prevalence of past-year mental health consultations also increased over time by 1.0% per year among adolescent females and 1.5% among young adult females; however, trends were not significant for males.
Figure 3 depicts the annual prevalence of suicidality from 2011 to 2016. The prevalence of past-year suicidality among young adult females increased from 1.8% in 2011 to 7.4% in 2016, an increase of approximately 1.0% per year (95% CI 0.1–1.9%). For the remaining age and sex groups, the prevalence remained relatively stable at a pooled prevalence of 3.3% for adolescent males (95% CI 2.5–4.1%), 3.8% for young adult males (95% CI 3.1–4.6%) and 7.4% for adolescent females (95% CI 6.2–8.6%).
Figures 4 and 5 display the trends in the prevalence of binge drinking, cannabis and other illicit drug use over time. For males, there was a significant reduction in binge drinking between 2011 and 2018. The largest reduction in binge drinking from 51.3% (2011) to 35.3% (2018) was among young adult males, a decrease of 2.7% per year (95% CI −3.3 to −1.4%). The change was less pronounced among adolescent males, with a decrease of 0.7% per year from 11.0% (2011) to 6.7% (2018). The prevalence of past-year cannabis and other illicit drug use was relatively stable over time, apart from the pre-legalisation trends among adolescent males. Specifically, from 2011 to 2017, the prevalence decreased by approximately 0.8% per year (p = 0.04). When the post-legalisation 2018 prevalence was included in the analysis, the observed decrease in prevalence did not persist (Δ = −0.3%; 95% CI −1.2 to 0.6%; p = 0.43).
Trends in past year use of cocaine, amphetamines, ecstasy and hallucinogens are reported in online Supplementary Table S5 and S6. The observed increase in cocaine use was driven by young adult females (Δ = 0.33%; 95% CI −0.01 to 0.68%; p = 0.06), while the increase in hallucinogen use was driven by males who were adolescents (Δ = 0.17%; 95% CI 0.01–0.32%; p = 0.04) and young adults (Δ = 0.34%; 95% CI −0.07 to 0.75%; p = 0.09). The pooled prevalence of illicit drug use was highest among young adult males, for cocaine (4.4%), methamphetamines (0.9%), ecstasy (4.2%) and hallucinogens (3.9%).
The sensitivity analyses reported similar trends in prevalence when restricted to the provinces that had data available from 2011 to 2018 (online Supplementary Table S9).
Discussion
This study describes trends in the prevalence of youth mental health outcomes from 2011 to 2018 among Canadian youth 12–24 years old. The main findings report an increase in the prevalence of perceived poor/fair mental health and professionally diagnosed mood and anxiety disorders over the study period. These trends were most pronounced for young adult females, with an annual prevalence of perceived poor/fair mental health, mood disorders and anxiety disorders increasing by 1.4, 1.0 and 1.6%, respectively. Young adult females exhibited the highest prevalence of depression and anxiety, as expected, given that sex differences typically emerge during the transition from adolescence to adulthood (Altemus et al., 2014). The increases in prevalence over time may represent a rise in mental illness among youth during this transitional period. Alternatively, it is possible that other factors, such as mental health literacy programmes in schools, have contributed to reduced levels of stigma, enhanced awareness of mental illness and self-efficacy to seek treatment for mental health concerns (McLuckie et al., 2014; Bjornsen et al., 2018). Irrespective of the underlying cause of increasing prevalence, the impact is a greater demand for mental health services. In fact, mental health consultations increased from nearly 12% in 2011 to 17% in 2018. Again, this increase was primarily driven by females, which is partially explained by the tendency for women to seek help more often than males (Kessler et al., 1981). Given the cross-sectional nature of this study, it is not possible to conclude whether the upsurge of mental health consultations was a result of help-seeking following worsening mental health, or if the worsening mental health was due to ineffective treatment. Future research is required to understand the direction of this relationship.
Another important finding was the increase in the prevalence of past-year suicidality from 1.8% (2011) to 7.4% (2016) among young adult females, with no change observed for other age or sex groups. Rather, pooled prevalence remained relatively stable at 3.3% for adolescent males, 7.4% for adolescent females, and 2.8% for young adult males. In the USA, Han et al. reported a rise in the prevalence of suicidal ideation, plans and attempts among young adult females from 2009 to 2015; however, baseline prevalence was higher at 7.1, 2.3 and 1.3%. In contrast to our findings, they also reported an increase in suicidal ideation and plans among males (Han et al., 2018).
Another important finding was a decrease in the prevalence of binge drinking among males. This was particularly evident among young adult males, with prevalence decreasing by nearly 3% each year from 51.3% in 2011 to 35.3% in 2017. While less pronounced for adolescent males, the prevalence of binge drinking decreased by 0.7% each year from 11.0% in 2011 to 6.7% in 2017. There was no change observed for females, with the pooled prevalence of binge drinking averaging 10.8% for adolescent females and 25.5% for young adult females. Drug use was relatively stable among youth over the study period, except for a decrease in cannabis use among adolescent males prior to legalisation in 2018. Specifically, the prevalence of cannabis use fell from 16.1% in 2011 to 10.7% in 2017, an average decrease of 0.7% per year. This trend did not persist when the 2018 estimate (16.3%) was considered. A recent report using the Canadian Tobacco Alcohol and Drugs Survey also reported a decline in past-year cannabis use among 15–17 years old youth prior to legalisation (Rotermann, 2019). The 2018–2019 prevalence estimates were too unstable to publish, but it is important to point out that cannabis was legalised for persons over the age of 18 in 2018, with legal age varying by province. In the overall sample of adult males (15–64 years old), the 3-month prevalence increased from 16% in the first quarter of 2018 to 22% in the first quarter of 2019 (Rotermann, 2019). The higher prevalence in 2018 could indicate either an increase in cannabis use or a greater willingness to disclose cannabis use because of legalisation. Over the next few years, it will be crucial to monitor trends in the prevalence of cannabis use among youth, as they are most vulnerable to the negative effects of cannabis on brain development (Jacobus et al., 2019).
This study has several strengths. The nationally representative cross-sectional surveys were administered each year with a consistent sampling frame and survey methods, which provided multiple data points to examine prevalence over time. Further, the availability of data on a variety of mental health outcomes allowed us to create a more comprehensive view of the recent trends in youth mental health. Finally, random-effects meta-regression techniques accounted for any differences across surveys that were not attributed to the survey year.
There are also some important limitations to note. First, while the data were taken from large cross-sectional studies, the samples were largely reduced when examining trends stratified by age and sex. As such, some of the age- and sex-specific prevalence estimates had wide confidence intervals that indicate low precision and make it challenging to assess trends. Second, data on optional content (i.e., sleep troubles, depression, drug use, suicidality) were only collected by some provinces each year, which reduced the samples (e.g., 16 800 for past-year suicidality). While optional content reduced the sample size, sensitivity analyses confirmed that the random nature of missing data did not impact trends. Third, due to the nature of survey data, we were unable to describe trends in the mental health of youth who experience homelessness or living on reserves. Further, given the scope of this analysis, trends were not examined by ethnicity; however, these sub-group analyses would further elucidate which groups require additional services. It is important for future research to examine trends by these subgroups.
Conclusion
The rise in the prevalence of professionally diagnosed mood and anxiety disorders was accompanied by an increase in the prevalence of poor/fair perceived health and past-year mental health consultations, especially among young adult females. This may reflect worsening mental health or changes in help-seeking behaviour through mental health literacy. While the declining prevalence of past-year binge drinking among males is promising, the lack of reduction among females has led to a narrowing sex difference for young adults. Trends in the prevalence of cannabis use should be continually monitored after 2018 to examine how legalisation might impact exposure to cannabis among youth. Collectively, these findings highlight a need for continued investment in mental health systems to support the rising need for sex-specific mental health programmes and services.
Acknowledgements
The analysis was conducted at the Prairie Regional Data Centre, which is part of the Canadian Research Data Centre Network (CRDCN). The services and activities provided by the CRDCN are made possible by the financial or in-kind support of the SSHRC, the CIHR, the CFI, Statistics Canada and participating universities whose support is gratefully acknowledged. The views expressed in this paper do not necessarily represent the CRDCN's or that of its partners.
Data
This project used data from a series of Canadian Community Health Survey microdata files available to accredited researchers and federal government employees through Statistics Canada. Additional information is available at https://www.statcan.gc.ca/eng/help/microdata
Financial support
This research was supported by the Cuthbertson and Fischer Chair in Pediatric Mental Health, held by Scott Patten.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796020000281.
click here to view supplementary material
Conflict of interest
None.
References
- Acharya L, Jin L and Collins W (2018) College life is stressful today – emerging stressors and depressive symptoms in college students. Journal of American College Health 66, 655–664. [DOI] [PubMed] [Google Scholar]
- Altemus M, Sarvaiya N and Neill Epperson C (2014) Sex differences in anxiety and depression clinical perspectives. Frontiers in Neuroendocrinology 35, 320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Jarrett MA, Luebbe AM, Garner AA, Burns GL and Kofler MJ (2018) Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 4, 174–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjornsen HN, Ringdal R, Espnes GA, Eilertsen MB and Moksnes UK (2018) Exploring MEST: a new universal teaching strategy for school health services to promote positive mental health literacy and mental wellbeing among Norwegian adolescents. BMC Health Services Research 18, 1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comeau J, Georgiades K, Duncan L, Wang L and Boyle MH (2019) Changes in the prevalence of child and youth mental disorders and perceived need for professional help between 1983 and 2014: evidence from the Ontario Child Health Study. Canadian Journal of Psychiatry 64, 256–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Norman RE, Freedman G, Baxter AJ, Pirkis JE, Harris MG, Page A, Carnahan E, Degenhardt L, Vos T and Whiteford HA (2014) The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study 2010. PLoS ONE 9, e91936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi S, Chiu M, Lam K, Cairney JC, Guttmann A and Kurdyak P (2016) Mental health service use among children and youth in Ontario: population-based trends over time. Canadian Journal of Psychiatry 61, 119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner W, Pajer K, Cloutier P, Zemek R, Currie L, Hatcher S, Colman I, Bell D, Gray C, Cappelli M, Duque DR and Lima I (2019) Changing rates of self-harm and mental disorders by sex in youths presenting to Ontario emergency departments: repeated cross-sectional study. Canadian Journal of Psychiatry 64, 789–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England) 392, 1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Krueger RF, Agrawal A, Plunk AD, Krauss MJ, Bongu J, Cavazos-Rehg PA and Bierut LJ (2018) Declines in prevalence of adolescent substance use disorders and delinquent behaviors in the USA: a unitary trend? Psychological Medicine 48, 1494–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, Colpe L, Huang L and McKeon R (2018) National trends in the prevalence of suicidal ideation and behavior among young adults and receipt of mental health care among suicidal young adults. Journal of the American Academy of Child and Adolescent Psychiatry 57, 20–27, e2. [DOI] [PubMed] [Google Scholar]
- Jacobus J, Courtney KE, Hodgdon EA and Baca R (2019) Cannabis and the developing brain: what does the evidence say? Birth Defects Research 111, 1302–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jao NC, Robinson LD, Kelly PJ, Ciecierski CC and Hitsman B (2018) Unhealthy behavior clustering and mental health status in United States college students. Journal of American College Health 67, 790–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RM, Fairman B, Gilreath T, Xuan Z, Rothman EF, Parnham T and Furr-Holden CD (2015) Past 15-year trends in adolescent marijuana use: differences by race/ethnicity and sex. Drug and Alcohol Dependence 155, 8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF, Patten SB, Brugha TS and Mojtabai R (2017) Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry 16, 90–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Brown RL and Broman CL (1981) Sex differences in psychiatric help-seeking: evidence from four large-scale surveys. Journal of Health and Social Behavior 22, 49–64. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR and Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Gary D, O'Malley PM, Hamilton A and Schulenberg J (2019) Recent increases in depressive symptoms among US adolescents: trends from 1991 to 2018. Social Psychiatry and Psychiatric Epidemiology 54, 987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leos-Toro C, Rynard V, Murnaghan D, MacDonald JA and Hammond D (2019) Trends in cannabis use over time among Canadian youth: 2004–2014. Preventive Medicine 118, 30–37. [DOI] [PubMed] [Google Scholar]
- Lowry R, Crosby AE, Brener ND and Kann L (2014) Suicidal thoughts and attempts among U.S. High school students: trends and associated health-risk behaviors, 1991–2011. The Journal of Adolescent Health 54, 100–108. [DOI] [PubMed] [Google Scholar]
- McLuckie A, Kutcher S, Wei Y and Weaver C (2014) Sustained improvements in students’ mental health literacy with use of a mental health curriculum in Canadian schools. BMC Psychiatry 14, 379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMartin SE, Kingsbury M, Dykxhoorn J and Colman I (2014) Time trends in symptoms of mental illness in children and adolescents in Canada. Canadian Medical Association Journal 186, E672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K and Swendsen J (2010) Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication – Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry 49, 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishina K, Tiiri E, Lempinen L, Sillanmaki L, Kronstrom K and Sourander A (2018) Time trends of Finnish adolescents’ mental health and use of alcohol and cigarettes from 1998 to 2014. European Child & Adolescent Psychiatry 27, 1633–1643. [DOI] [PubMed] [Google Scholar]
- Murphy MH, Carlin A, Woods C, Nevill A, MacDonncha C, Ferguson K and Murphy N (2018) Active students are healthier and happier than their inactive peers: the results of a large representative cross-sectional study of university students in Ireland. Journal of Physical Activity & Health 15, 737–746. [DOI] [PubMed] [Google Scholar]
- Ng Fat L, Shelton N and Cable N (2018) Investigating the growing trend of non-drinking among young people; analysis of repeated cross-sectional surveys in England 2005–2015. BMC Public Health 18, 1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Druss BG and Marcus SC (2015) Trends in mental health care among children and adolescents. New England Journal of Medicine 372, 2029–2038. [DOI] [PubMed] [Google Scholar]
- Patten SB, Williams JV, Lavorato DH, Wang JL, McDonald K and Bulloch AG (2016) Major depression in Canada: what has changed over the past 10 years? Canadian Journal of Psychiatry 61, 80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitchforth J, Fahy K, Ford T, Wolpert M, Viner RM and Hargreaves DS (2018) Mental health and well-being trends among children and young people in the UK, 1995–2014: analysis of repeated cross-sectional national health surveys. Psychological Medicine 49, 1275–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratnasingham S, Cairney J, Manson H, Rehm J, Lin E and Kurdyak P (2013) The burden of mental illness and addiction in Ontario. Canadian Journal of Psychiatry 58, 529–537. [DOI] [PubMed] [Google Scholar]
- Rotermann M (2019) Analysis of trends in the prevalence of cannabis use and related metrics in Canada. Health Reports 30, 3–13. [DOI] [PubMed] [Google Scholar]
- Sawyer MG, Reece CE, Sawyer ACP, Johnson SE and Lawrence D (2018) Has the prevalence of child and adolescent mental disorders in Australia changed between 1998 and 2013 to 2014? Journal of the American Academy of Child and Adolescent Psychiatry 57, 343–350, e5. [DOI] [PubMed] [Google Scholar]
- StataCorp (2017) Stata Statistical Software: Release 15. College Station, TX: StataCorp LP. [Google Scholar]
- Statistics Canada (2017) Canadian Community Health Survey – Annual Component (CCHS). Available at https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=329241 (accessed 1 April 2020).
- Thorisdottir IE, Asgeirsdottir BB, Sigurvinsdottir R, Allegrante JP and Sigfusdottir ID (2017) The increase in symptoms of anxiety and depressed mood among Icelandic adolescents: time trend between 2006 and 2016. European Journal of Public Health 27, 856–861. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Cooper AB, Joiner TE, Duffy ME and Binau SG (2019) Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. Journal of Abnormal Psychology 128, 185–199. [DOI] [PubMed] [Google Scholar]
- Wattick RA, Hagedorn RL and Olfert MD (2018) Relationship between diet and mental health in a young adult Appalachian college population. Nutrients 10, e957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N, Burstein R, Murray CJ and Vos T (2013) Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet (London, England) 382, 1575–1586. [DOI] [PubMed] [Google Scholar]
- Wiens K, Williams JVA, Lavorato DH, Duffy A, Pringsheim TM, Sajobi TT and Patten SB (2017) Is the prevalence of major depression increasing in the Canadian adolescent population? Assessing trends from 2000 to 2014. Journal of Affective Disorders 210, 22–26. [DOI] [PubMed] [Google Scholar]
- Zuckermann AME, Battista K, de Groh M, Jiang Y and Leatherdale ST (2019) Prelegalisation patterns and trends of cannabis use among Canadian youth: results from the COMPASS prospective cohort study. BMJ Open 9, e026515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796020000281.
click here to view supplementary material