Abstract
Osteomas are one of the most common benign fibro-osseous lesions affecting the sinonasal tract. Rarely osteomas have osteoblastoma-like areas histologically, which are often misdiagnosed radiologically and pathologically as osteoblastomas. We report the CT and MR imaging findings of 3 cases of osteoma with osteoblastomas-like features in pediatric patients, 1 initially diagnosed as an osteoblastoma. Only 5 case reports of osteoma with osteoblastoma-like features within the paranasal sinuses have been reported in the English literature to date using the PubMed search engine, none of which include pediatric patients. We review the typical zonal imaging characteristics of this rare presentation of osteoma and propose a distinct “sclerotic cap” sign to aide radiologists in differentiating osteomas with osteoblastoma-like features from the more common benign fibro-osseous lesions. Additionally, we address some radiologic-pathologic discrepancies in diagnosis between osteoblastoma and osteoma with osteoblatoma-like features.
Keywords: Sinus, Osteoma, Osteoblastoma, Sclerotic cap
Introduction
The most common benign fibro-osseous lesions affecting the sinonasal tract are osteomas, fibrous dysplasia and ossifying fibromas [1,2]. These entities often can reliably be distinguished radiologically, but sinonasal osteomas can rarely contain osteoblastomas-like areas, which can lead to misdiagnosis both on imaging and histologically as a paranasal osteoblastoma [2]. Osteoblastoma is a rare benign, bone forming tumor that most commonly occurs in the vertebrae and long bones [3]. When osteoblastoma occurs in the head and neck area, it is most commonly seen in cervical vertebrae or the mandible [4]. It rarely occurs in the paranasal sinuses as reported in a small collection of case reports. The first paranasal sinus osteoblastoma was reported by Fu and Perzin in 1974 [4], and subsequent reported cases are few. However, there has been differing terminology in the literature leading to confusion between osteoblastoma, reportedly rare in the paranasal sinuses, and variants of osteoma of the paranasal sinus, such as osteoma with osteoid-osteoma like features and osteoma with osteoblastoma-like features. Upon literature review, we believe many previously reported cases of sinus osteoblastoma likely falls into the category of osteoma with osteoblastoma-like features. Sinonasal osteomas with osteoblastoma-like features demonstrate distinct radiologic features, as our 3 cases demonstrate, allowing for potential prospective identification by radiologist.
Case 1
A 14-year-old female with no significant past medical history presented with a 2 year history of a slowly growing forehead mass. She had intermittent imaging at an outside institution following the size of the mass, which had been asymptomatic. She came to our medical center with 6-7 months of intermittent headaches, about 1 per week that resolved with sleep, and no exacerbating factors. The mass also had over time become cosmetically distressing. Physical exam demonstrated a 2 × 3 cm, noncompressible protrusion over the left forehead. Imaging was performed for further evaluation.
A noncontrast CT of the head demonstrated a well-defined, polypoid mixed density mass within an expanded, remodeled left frontal sinus (Fig. 1). The mass arose from the inferior frontal wall of the frontal sinus and/or frontoethmoidal recess with a ground glass base and/or central component and a dense, sclerotic cap along the superior and posterior borders. The fibrous component measured 2.2 × 3.1 cm in maximum transaxial dimensions. The mass was associated with focal dehiscence in the posterior wall of the frontal bone and adjacent mucocele formation (Fig. 1).
Fig. 1.
(A) Coronal noncontrast CT of the head demonstrates an expansile, lobular mass in the left frontal sinus with thick sclerotic superior and posterior margins (white arrow) and a large central low density, fibrous component arising from the frontoethmoidal recess (black arrow). (B) In the axial plane, the focal dehiscence in the posterior wall of the frontal bone and adjacent mucocele formation are visible.
A follow up MRI of the brain with and without contrast showed a well-defined, polypoid lesion within the left frontal sinus measuring 2.7 × 3.7 × 2.8 cm (anterior-posterior by transverse by craniocaudal) (Fig. 2). There was thickened, confluent marked T1 and T2 hypointense signal along the superior and posterior borders correlating to the dense sclerotic cap on CT which demonstrated no enhancement on post contrast sequences. The fibrous component at the base of the mass was iso to hypointense on T1 and T2 weighted sequences and showed avid homogenous enhancement. Homogenous T2 hyperintense material surrounded the mass within the expanded left frontal sinus with thin peripheral enhancement, consistent with suspected mucocele formation. Primary imaging differential was that of an osteoblastoma with associated mucocele formation.
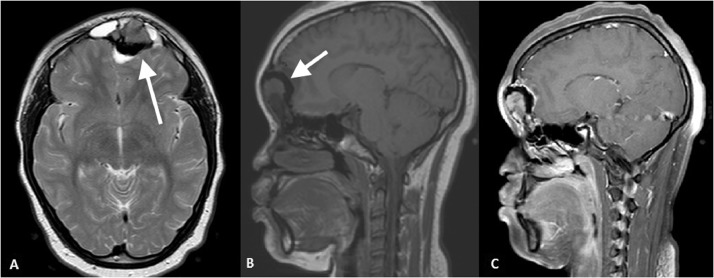
Fig. 2.
(A) Axial T2 weighted sequence demonstrates low signal “void” corresponding to the dense sclerotic cap seen on the CT (white arrow) and intermediate to low signal central fibrous component anteriorly. T2 hyperintense mucocele formation along the lateral borders is present. (B and C) Pre- and postcontrast sagittal T1 weighted sequences demonstrates avid enhancement of the anterior fibrous component at the base of the mass. The sclerotic cap does not enhance.
Percutaneous US guided core biopsy preliminarily revealed a benign osteoblastic lesion, favoring an osteoblastoma based on size on imaging. The patient underwent surgical excision with cranioplasty, supraorbital bar reconstruction with titanium mesh and hydroxyappetite as well as bone grafting to the epidural space behind the frontal sinus with cranialization of the frontal sinuses. She tolerated the surgery well without complication. Final pathology was read as craniofacial osteoma with osteoid osteoma-like features, which was later changed to osteoma with osteoblastoma-like features solely based on size criteria.
Case 2
A 16-year-old male with no past medical history presented to the emergency room with right eye pain and swelling for 4 days. He initially noted swelling and erythema, and as it progressed he noted intermittent fevers. After 4 days the pain was severe so he decided to come to the hospital. Physical exam revealed erythematous right periorbital soft tissues. A CT was ordered for further evaluation.
CT of the orbits with contrast demonstrated a large, expansile mass centered within the right frontoethmoidal recess measuring 1.7 × 2.5 × 2.5 cm (transverse x anterior-posterior x craniocaudal) (Fig. 3). The mass had a ground glass narrow base attached to the superior wall of the medial right frontal sinus, with apparent polypoid growth inferiorly transitioning into a dense, sclerotic cap along its most inferior aspect. The mass obstructed the right frontal drainage pathway with resultant complete opacification of the sinus. Laterally, the lesion extended through an eroded lamina papyracea into the right medial extraconal orbit. Inflammatory changes were present within the medial and superior extraconal post-septal orbit, immediately adjacent to the lesion. The medial rectus, inferior rectus and superior oblique muscles were enlarged and demonstrated enhancement.
Fig. 3.
(A) Sagittal and (B) coronal CT of the face without contrast reveals a large, expansile mass centered within the right frontoethmoidal recess with a ground glass, narrow base attached to the superior wall of the medial right frontal sinus (white arrow), with apparent polypoid growth inferiorly transitioning into a dense, sclerotic cap along its most inferior aspect (black arrow). The mass obstructs the right frontal drainage pathway with resultant complete opacification of the frontal sinus. The mass extends through an eroded lamina papyracea into the right medial extraconal orbit.
A MRI of the brain and orbits with and without contrast was then performed for further evaluation, which once again demonstrated a well-fined, polypoid mass within the right frontoethmoidal recess (Fig. 4). The ground glass base on CT was iso-hypointense on T1 and T2 weighted sequences and demonstrated avid homogenous enhancement. The sclerotic rim along the inferior aspect of the mass was markedly hypointense on all sequences and did not enhance. The mass obstructed the right frontal sinus, which was occupied by purulent material that showed restricted diffusion on diffusion weighted imaging. As seen on the CT, findings of associated orbital cellulitis was present. The mass was interpreted as a likely benign fibro-osseous lesion, such as an ossifying fibroma, complicated by sinusitis and orbital cellulitis.
Fig. 4.
MRI of the brain and orbits with and without contrast. (A) Coronal Short Tau Inversion Recovery (STIR) sequence demonstrates a well-fined, polypoid mass within the right frontoethmoidal recess with a fibrous T2 iso-hypointense base attached to the superior wall of the medial right frontal sinus (white arrow) and a markedly hypointense signal along it's inferior margins. On (B) Pre- and (C) postcontrast T1 weighted sequences the fibrous base demonstrates avid homogenous enhancement, while the sclerotic cap remains hypointense (black arrow). Enhancing inflammatory phlegmon is present within the medial and superior extraconal postseptal orbit, immediately adjacent to the lesion. The medial rectus, inferior rectus and superior oblique muscles are enlarged and enhance.
A percutaneous core biopsy was performed of the mass which revealed dense, compact mature bone with Haversian system, broad trabeculae and paucicellular fibrous stroma consistent with an osteoma. However, the pathologist noted that the sampling was limited and the biopsy appeared to spare the more central fibrous component of the tumor, where osteoblastoma-like features are typically found. As such, taking the radiologic appearance of the mass into account, osteoma with osteoblastoma-like features was determined to be the presumptive diagnosis.
The patient was treated for sinusitis and orbital cellulitis, with plans on resection of the mass at a later date after treatment of infection. However, the mass was not resected as the patient decided against surgery and elected serial radiologic monitoring.
Case 3
A 9-year-old female with reported history of paranasal osteoma was referred to our institution for second opinion of imaging. No further history or final pathology was obtainable, however the imaging findings are presented here given the characteristic features similar to our other cases and presumed diagnosis of osteoma with osteoblastoma-like features.
CT of the head without contrast demonstrates a lobular, expansile mass centered within the right frontoethmoidal recess (Fig. 5A). The mass has a fibrous/ground glass component along the medial aspect within right anterior ethmoid air cells which measured 1.6 × 0.9 × 1.6 cm (craniocaudal by transverse by anterior posterior). The lateral aspect of the mass was densely sclerotic and measured 1.8 × 0.8 × 1.6 cm (craniocaudal by transverse by anterior posterior). The sclerotic cap projected into the superior medial orbit, displacing the superior oblique muscle as well as the globe. Mild proptosis was present. A follow up MRI of the brain with and without contrast was performed for further characterization (Fig. 5B-D). MRI demonstrated marked T1 and T2 hypointense signal correlating to the sclerotic cap seen on CT. The fibrous component was heterogeneous on T1 and T2 and demonstrated heterogeneous enhancement.
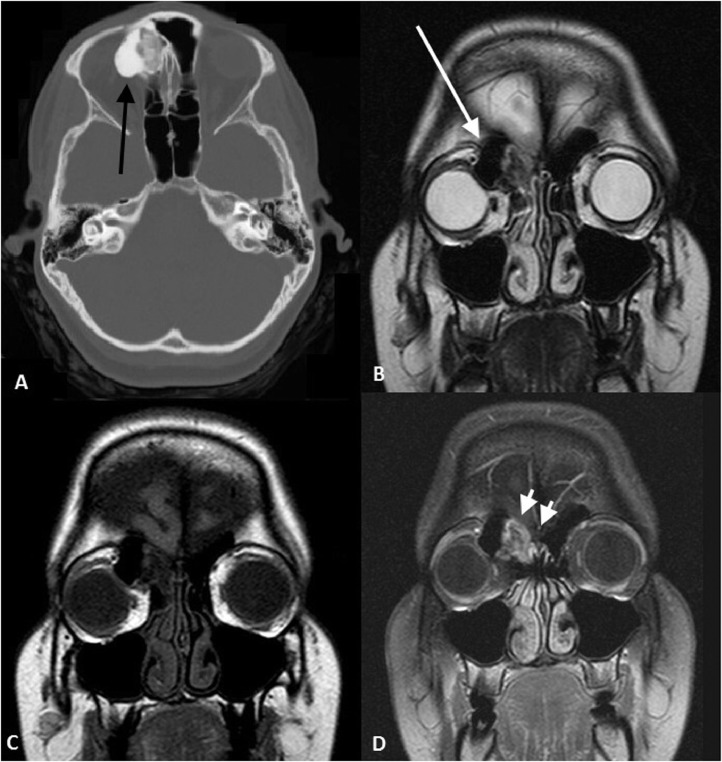
Fig. 5.
(A) Axial noncontrast CT of the head demonstrates a lobular, expansile mass centered within the right frontoethmoidal recess. The mass has a fibrous and/or ground glass component along the medial aspect within right anterior ethmoid air cells and a dense sclerotic cap laterally (black arrow). The sclerotic cap projects into the superior medial orbit. (B) MRI of the brain with and without contrast shows hypointense signal “void” along the lateral margins corresponding to the sclerotic cap on CT (white arrow). The mass projects into the superior medial orbit, displacing the superior oblique muscle as well as the globe. On (C) pre- and (D) postcontrast T1 weighted sequences the fibrous component heterogeneously enhances (double short white arrows).
Discussion
Osteomas are the most common tumor of the paranasal sinuses [2]. Osteomas are benign, slow growing tumors that almost exclusively arise within the sinuses and mandible [2]. Generally, these are asymptomatic until mass effect results in obstruction, at which time patients can present with facial pain, headache, or facial distortion. Obstruction of the sinus drainage pathways, commonly the nasofrontal duct, can also lead to mucocele formation and infection, as demonstrated in our cases. Osteomas can also erode into the cranial vault resulting in cerebrospinal fluid leaks or meningitis. They are classified into 3 categories based on the proportion of bone and stromal components; ivory, mature, and mixed [2]. The ivory osteoma is the most common, and presents as an exophytically growing, well circumscribed mass of dense cortical bone on CT. The mature osteoma is often less dense and can have regions that appear similar to normal marrow. On MRI, the dense ivory osteomas are low signal on all sequences, while the mature osteomas may demonstrate marrow signal internally.
In McHugh et al's histological examination of 45 surgically excised paranasal osteomas, 38% had interanastomosing trabeculae of woven bone rimmed by enlarged osteoblasts and osteoclasts. These regions of enlarged osteoblasts in loose fibrovascular stroma are histologically indistinguishable from osteoblastomas if taken out of context, and osteomas that demonstrate these findings have been designated as osteomas with osteoblastoma-like features by Dorfman and Czerniak. Some diagnostic confusion has arisen due to discrepancy between what has been called osteoblastoma of the paranasal sinuses based on imaging and possible overlap with what has been termed osteoma with osteoblastoma-like features between different sources [2]. Only 27 cases of osteoblastoma of the paranasal sinuses have been reported as case reports [4,5,6]. Osteoblastomas are found most commonly in the posterior elements of the spine (42%) and have a nonaggressive appearance. Osteoblastomas tend to be mildly expansile and can range in appearance from sclerotic to lytic [3]. Most commonly, they present with both sclerotic bony and heterogeneous fibrous components [5]. Osteoblastomas are pathologically indistinguishable from osteoid osteomas and are separated by size criteria, with osteoid osteomas having a fibrous nidus that measures <1.5 cm whereas osteoblastomas measure 2 or more cm [3].
Comparing available CT imaging of these 27 previously reported paranasal sinus osteoblastomas with our cases of osteomas with osteoblastoma-like features shows very similar radiologic findings [4,5,7]. In each case, there is an exophytic, polypoid mass with a low density fibrous-like component at the base and a dense, sclerotic cap. On MRI, the sclerotic portion is low signal on all sequences and the fibrous component enhances. These imaging findings are also very similar to those shown by McHugh et al in their review of the 45 surgical cases of resected paranasal osteomas with a focus on osteomas with osteoblastoma-like features. Additionally, this distinct zonal pattern of a less dense base with a sclerotic peripheral cap seen on our cases as well as the reviewed “paranasal osteoblastoma” literature are also quite similar to 3 other case reports of osteoma with osteoblastoma-like features by Yazici et al [8]. As McHugh stated in his article and our literature review suggests, these previous case reports of osteoblastoma of the paranasal sinuses were likely misdiagnosed osteomas with osteoblastoma-like features, given the rarity of true osteoblastomas and the characteristic zonal imaging findings these “osteoblastomas” demonstrated. The size of pathology specimens can be variable depending on factors such as the surgical technique, the ability to fully excise a specimen and the postprocessing changes. What the pathologist actually receives to evaluate may not represent the full size of the mass, which might make it difficult to distinguish between osteoblastomas or osteomas with osteoblastoma-like features.
Therefore, we propose the use of a “sclerotic cap” sign to aide both radiologist and pathologist in the diagnosis of osteoma with osteoblastoma-like features. The “sclerotic cap” sign and the distinct zonal pattern allows a radiologist to prospectively suggest the diagnosis of osteoma with osteoblastoma-like features, reliably differentiating it from other benign fibro-osseous lesions such as ivory osteomas, ossifying fibromas, and fibrous dysplasia. For pathologist, concurrent review of imaging and knowledge of the “sclerotic cap” sign can direct the diagnosis towards osteoma with osteoblastoma-like features rather than osteoblastoma, as isolated histologic review of these masses can be misleading depending on pathologic sampling technique.
References
- 1.Ciniglio Appiani M., Verillaud B., Bresson D., Sauvaget E., Blancal J.-P., Guichard J.-P. Ossifying fibromas of the paranasal sinuses: diagnosis and management. Acta Otorhinolaryngol Ital. 2015;35(5):355–361. doi: 10.14639/0392-100X-533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McHugh J., Mukherji S., Lucas D. Sino-orbital osteoma. A clinicopathologic study of 45 surgically treated cases with emphasis on tumors with osteoblastoma-like features. Arch Pathol Lab Med. 2009;133:1587–1593. doi: 10.5858/133.10.1587. [DOI] [PubMed] [Google Scholar]
- 3.Manaster B.J., May D.A., Disler D.G. 3rd ed. Mosby; Philadelphia, PA: 2007. Musculoskeletal imaging; the requisites; pp. 420–425. [Google Scholar]
- 4.Ruske D., Fields M., Blennerhassett J. Benign osteoblastoma of the sinonasal tract. Aust J Otolaryngol. 2001;4(2):123–126. [Google Scholar]
- 5.Sidani C.A., Karam A.R., Bruce J.H., Sklar E. Osteoblastoma of the frontal sinuses presenting with headache and blurred vision: case report and review of the literature. J Radiol Case Rep. 2010;4(6):1–7. doi: 10.3941/jrcr.v4i6.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paradi M., Iustulin D., Isola V. Partial ablation of benign osteoblastoma: a case report. Metab Pediatr Syst Ophthalmoly. 1993;16:43–45. [PubMed] [Google Scholar]
- 7.Caltabiano R., Serra A., Bonfiglio M., Platania N., Albanese V., Lanzafame S. A rare location of benign osteoblastoma: case study and a review of the literature. Eur Rev Med Pharmacol Sci. 2012;16:1891–1894. [PubMed] [Google Scholar]
- 8.Yazici Z., Yazici B., Yalcinkaya U., Gokalp G. Sino-Orbital osteoma with osteoblastoma-like features: case reports. Neuroradiology. 2012;54:765–769. doi: 10.1007/s00234-011-0973-9. [DOI] [PubMed] [Google Scholar]