Abstract
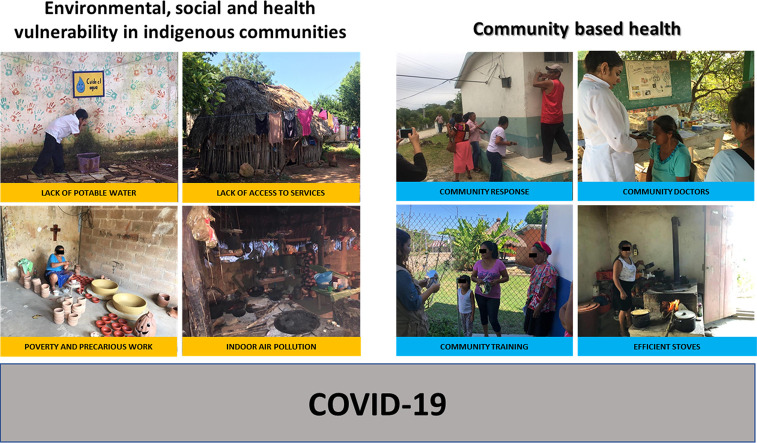
The objective of this study was to conduct a critical analysis of the social, environmental and health risk factors in the Mexican indigenous population in the context of the COVID-19 disease pandemic, and to propose strategies to mitigate the impacts on these communities. Regarding social factors, we identified the return of indigenous people to their communities, poor access to water, language barriers, and limited access to the Internet, as factors that will not allow them to take the minimum preventive measures against the disease. Additionally, environmental risk factors associated with pollutants from biomass burning were identified. In health, the lack of coverage in these areas and comorbidities such as diabetes mellitus, hypertension, respiratory tract infections, and chronic pulmonary diseases were identified. Some existing government programmes were identified that could be supported to address these social, environmental and health gaps. We believe that the best way to address these issues is to strengthen the health system with a community-based approach.
Health is the best element of cohesion for inserting development and progress proposals in indigenous communities, given the vulnerability to which they are exposed in the face of the COVID-19 pandemic. In this review, all information is provided (as possible) on risk factors and potential solutions in indigenous communities in the hope of providing solutions to this pandemic and providing a reference for future studies.
Keywords: COVID-19; Indigenous people; Mexico; Vulnerability; Social, environmental and health risk factors
Graphical abstract
Highlights
-
•
Covid-19 is a pandemic disease
-
•
Indigenous populations are more vulnerable to COVID-19 due to social, environmental and health factors.
-
•
A health system with a community-based scheme must be strengthened.
-
•
Mexico has government programmes that could be reorganized to meet the needs of the indigenous population.
1. Introduction
The epidemic of the new SARSCoV-2 coronavirus causing COVID-19 disease originating in Wuhan, China, has spread globally with more than 1.9 million infected and more than 142,000 deaths (information up to April 16, 2020). Disease control efforts include counting infected cases, controlling transmission, clinical severity, research in drug treatments, and social isolation. The overall mortality rate varies between 5.5 and 5.9%, but could be as high as 20% in Wuhan where the epicenter of the outbreak occurred (Baud et al., 2020). In Mexico the reported mortality rate is 9.7% as of June 6, 2020 (https://coronavirus.gob.mx/datos/).
The World Health Organization has accomplished an excellent job in establishing the guidelines to face this pandemic, it has marked the protocols of action of the health authorities of all the countries given the magnitude of the event that goes from the most basic prevention such as constant hand washing, hygiene habits, social distancing to detection tests, patient care inside the housing, epidemiological surveillance, among many others (https://www.who.int/es/emergencies/diseases/novel-coronavirus-2019).
Although all population groups may be at risk of contracting SARSCoV-2, the risk of mortality associated with COVID-19 is higher in people over 60 years of age, and in population groups with chronic diseases such as cardiovascular disease, diabetes, chronic respiratory disease and kidney disease (Caramelo et al., 2020; Cheng et al., 2020; Fu et al., 2020; Jordan et al., 2020; Lippi and Henry, 2020).
The COVID-19 pandemic could have serious effects on the well-being, quality of life, livelihoods and health of all populations, but most significantly on those who are most vulnerable.
From the perspective of human health risk assessment, risk must be understood as the vulnerability of a population and its capacity to respond to new conditions in order to mitigate potential effects.
The vulnerability has several definitions, all of them including the degree to which individuals are susceptible or unable to cope with adverse effects. Thus, the vulnerability in human health is a function of i) -vulnerable individuals- which includes factors such as the sensitivity of the population at greatest risk (exposure-response relationship), ii) -exposure factors- which includes the pathways and points of exposure to an agent that causes harm, and iii) measures and actions implemented to mitigate the burden of an adverse health outcome, whose effectiveness is the result of managing the exposure-response relationship.
In general, the vulnerability of a population depends on its local environment, the level of material resources, the effectiveness of governance and institutions, the quality of public health infrastructure and access to local information (Cutter, 1996). Clearly, these factors are not uniform and differ according to geography, demographics and socio-economic factors. Effectively targeting prevention strategies requires an understanding of demographic subpopulations, therefore individual, community and geographic factors determine vulnerability.
To build health, the factors that are related to the origin of the disease and those that affect the well-being of the population must be addressed. Its study should be analyzed from a perspective that includes the scenario of risks (COVID-19) in a context of vulnerability (poverty, marginalization, violence, social security, among others) for human health and the environment.
In this review, the main objective was to identify the vulnerabilities of indigenous peoples in the context of Mexico, from an environmental, social and health perspective and thus approach proposals for tools to increase the capacity to adapt to the COVID-19.
2. Identification of socio-economic vulnerabilities in the context of the indigenous population in Mexico
2.1. Population size and people at risk
The National Commission for the Development of Indigenous Communities in Mexico, now the National Institute of Indigenous Communities, states that of the 119,530,753 inhabitants in Mexico, there is an indigenous population of 12,025,947 (10.1%), distributed in 64,172 communities (INPI, 2017).
In Mexico, 8 (Chiapas, Hidalgo, San Luis Potosí, Oaxaca, Yucatán, Veracruz, Durango, and Guerrero) of the 32 entities concentrate between 66 and 85% of the indigenous population. The largest populations are: Nahuatl, (24%); Maya, (13.7%); Mixteco, (6.8%); Zapoteco, (6.8%); Tseltal, (5.7%); Paipai, (5.5%); Otomi, (5.5%); Tsotsil, (5.1%); Totonaco (3.6%); and Mazahua (3.0%). These 10 towns of the 68 that exist in our country, concentrate 80% of the indigenous population (INPI, 2017).
In 2015, it was recorded that 51.1% of the indigenous population were women and 48.9% men, the demographic distribution of the indigenous population under 15 years of age represented 31.8%, the group of 15–64 years represented 60.7% and 7.4% of people were over 65 years (INPI, 2017). Until 2015, 10.4% of the indigenous population was over 60 years old (INPI, 2017), but in addition 4 out of 5 older adults who speak an indigenous language are monolingual and only 18% also speak Spanish, therefore, the transmission of prevention messages, symptoms, and any intervention measure for COVID-19 disease must contemplate language to achieve effective communication. In view of this, Mexico must implement measures planned from an intercultural perspective. Among these initial efforts are the actions carried out by the National Institute of Indigenous Peoples in Mexico, which has translated information from the health sector for the prevention of COVID-19 virus infection into 35 indigenous languages, focusing on the WHO recommendations (https://www.gob.mx/inpi/documentos/coronavirus-en-lenguas-indigenas?idiom=es).
2.2. Socio-economic indicators
The efforts to prevent and mitigate COVID-19 disease in indigenous peoples in Mexico have been the same as those implemented in the general population. They are based so far on the transmission of information, such as the “Stay at Home” campaign, messages about proper handwashing and hygiene measures, social distancing, among others, this in a precarious socio-economic context.
In 2018, the National Council for the Evaluation of Social Development Policy stated that 11.8 million indigenous people in Mexico are in situations of poverty and extreme poverty. Social deprivation indicators show that 3.7 million are lagging in education, 1.9 million in access to health services, 9.4 million in access to social security, 3.8 million in food, 3.4 million in housing quality and space and 6.9 million in basic housing services, of which 12.8% lack piped water, 26.9% do not have sanitation services, 13.9% of homes have dirt floors and 58.8% cook with wood or charcoal (CONEVAL, 2019).
These inequities are factors that will not allow the COVID-19 to be confronted in indigenous communities. Although preventive actions such as constant handwashing have worked in mainly urban contexts (WHO, 2020), the barriers to the marginalization that include limited access to piped water, soap, and drainage (the use of dry or wet toilets is common in these areas but lacks adequate maintenance arrangements), make these solutions unprovable in all indigenous communities.
Achieving permanent access in these populations to piped water 24 h a day at the moment is not feasible, the long-term goal is slow and costly. To address this problem in the short and medium-term there are successful community programmes such as the hand-washing stations in rural Kenya, the cost per station was US$ 14.35 (Freedman et al., 2017). So investing in this program at present could be an alternative to mitigate contagion in indigenous communities.
2.3. Migration and return to communities
Another phenomenon that has contributed to the spread of the infection is the return of the indigenous population from work sites to their communities of origin. Migration is a social determinant of indigenous health. The phenomenon of migration has a negative impact on the health of indigenous migrants (León-Pérez, 2019), While improvements in their living conditions are sought, indigenous migrants are the most vulnerable as they are paid less than their non-indigenous counterparts, occupy precarious jobs where discrimination, poor access to benefits and health care are a reality (Montenegro and Stephens, 2006).
By recognizing this group and taking into account their social characteristics (work within informality) we are faced with a scenario where they have difficulty accessing health services. Now, it may be an important indicator of potentially contagious infected people returning to their communities, in the absence of a key coordinated response in public health planning and public health system response (Liem et al., 2020). There is a continuous flow of indigenous migration to urban destinations, where they are employed mainly in jobs such as construction, domestic work or informal sector sales (Pérez Campuzano and Santos Cerquera, 2013).
Data from 2015 indicate high national mobility among the indigenous population and show the states of Baja California Sur, Nuevo León, Colima, Mexico City, Aguascalientes, Sinaloa, and Baja California as a pole of attraction, recruiting more than 70% of migrants (INPI, 2017). Within these national migratory movements, there is evidence that the population of indigenous peoples within cities is concentrated in the periphery where there are scenarios with marked social inequalities (Durin et al., 2007). Concerning international mobility, the main destination is the United States. For example, the transnational circuit of indigenous Triqui immigrants from the mountains of Oaxaca to northeastern Washington state and central California has been documented (Holmes, 2012); from the P'urépechas of Michoacán to North Carolina, the Nahuas of Tlaxcala to New York (Asad and Hwang, 2019) and the Mixtecs and Zapotecas of Oaxaca whose main destination is California (Kearney, 2000).
In response to the pandemic, many indigenous leaders have taken protection into their own hands, in some cases shielding their borders, which can lead to stigmatization of the disease and undermine social cohesion, causing social isolation of population groups. To this end, WHO has designed programmes to reduce this type of action (https://www.paho.org/es/documentos/estigmatizacion-social-asociada-covid-19), in which it recommends that communication with indigenous peoples about the disease should take into account these recommendations to avoid social conflict. For example, in Colombia, a Latin American country with about 2000 of the more than 30,000 confirmed cases of COVID-19 in the region, indigenous leaders in the mountainous department of Cauca were threatened by drug trafficking groups after they closed their borders by establishing 69 checkpoints protected by 1200 guards (Julie, 2020). Some indigenous leaders in Peru decided to close their borders to people outside their communities until COVID-19 is under control (Zavaleta, 2020).
COVID-19 disease could potentially have serious effects on the well-being, livelihoods, and health of all peoples. The strict public health policy measures of quarantine and isolation implemented by China in Wuhan showed a reduction in the effective number of propagation (Dandekar and Barbastathis, 2020) and 76 days later they ended the closure of their borders. The United Nations Permanent Forum on Indigenous Issues mentions that several Indigenous Peoples' communities have self-imposed quarantine and have established controls to limit access to their communities. These mechanisms should be respected and strengthened whenever requested.
2.4. The indigenous digital breach
Global culture brings with it certain “ideal” lifestyles which are difficult to achieve within the reality of indigenous populations. This global culture is generally mediated by exposure to the media and the expansion of the use of Information and Communication Technologies. This refers to the creation, distribution, and use of information, relegating indigenous communities to the role of recipients and not as generators of health information.
In Mexico, there are 80.6 million internet users, but internet use is an urban phenomenon as 76% of users are in cities compared to 47% in rural areas (INEGI, 2019). Despite the limitations that indigenous populations confront in relation to technological areas (lack of infrastructure and low purchasing power), we can consider that within the users, young people have greater access to the Internet and that they have more schooling than their parents and older adults (Sunkel and Ullmann, 2019). This is an important point in the design of intervention strategies, as we already highlighted, local indigenous communities do not often have a complete command of the main languages. The UN Permanent Forum on Indigenous Issues recommends that to avoid communication breaks that will spread the disease, all key messages on hygiene, quarantine, and containment should be shared with traditional leaders and youth leaders and translated into local indigenous languages. Faced with this pandemic situation, the Mexican government has the program “Youth Building the Future” and has a census of more than 678 thousand young people between 18 and 29 years old, who during one year are linked to institutions, companies, workshops or businesses where they develop or strengthen work habits and technical skills to increase their employment opportunities in the future. This is where an opportunity is found to establish a strategy for the formation of local human capital. If only 10% of these young people were in indigenous localities, all the indigenous communities in Mexico would be covered, with training in the surveillance and prevention systems for COVID-19, support for telemedicine in strategic communities, and so could be covered even more and vulnerabilities due to lack of access to information could be reduced.
3. Identification of environmental vulnerability in the indigenous population
Environmental factors associated with chemical contamination are a vulnerability factor in the indigenous population to the effects of the present pandemic. In general, pollution is related to the premature death of 9 million people per year worldwide and 268 million disability-adjusted life-years (DALYs), which represents about 16% of all deaths on the planet, three times more than those caused by HIV-AIDS, tuberculosis, and malaria combined and 15 times more than those caused by violence (Landrigan et al., 2018).
But well-being is not only related to the environment through the risks of exposure to pollutants but also to mental health, nutrition, culture and the generation of natural resources, these are some of the health factors that can be affected by the quality of ecosystems. These new interactions are now defined as the ecological determinants of health (Hancock et al., 2016). If the ecosystem becomes ill, man, being part of the ecosystem, also becomes ill. Therefore, climate change with floods, droughts, temperature increases, acidification of the oceans, and so on, affects health in the full extent of the concept.
Our research group has reported exposure to different toxics in indigenous communities in Mexico, identifying exposure to lead from the use of glazed clay (Flores-Ramirez et al., 2012), organochlorine insecticides such as DDT that were used for malaria vector control (Flores-Ramirez et al., 2017), polycyclic aromatic hydrocarbons and particulate matter from the use of wood for cooking (Estevez-Garcia et al., 2020; Flores-Ramirez et al., 2016), volatile organic compounds (Pérez-Herrera et al., 2019), mining areas (Silva and Lizardi-Jiménez, 2020), water contaminated with carcinogenic hydrocarbons (Lizardi-Jiménez and Aguirre-García, 2018; Valdivia-Rivera et al., 2018) and contaminants of biological origin such as aflatoxins from the consumption of contaminated maize (Díaz de León-Martínez et al., 2019). In other words, the indigenous population is exposed to various chemical mixtures and, therefore, we can assume the maximum risk and, consequently, conclude that due to exposure to chemical mixtures they are in a high vulnerability.
Since the pandemic is unfortunately in progress, there are limited data on the environment and the progress of the disease, research is currently focused on climate variations such as temperature and humidity associated with the increase in cases of COVID-19 (Ma et al., 2020). In this regard, one hypothesis we raise in indigenous communities is that indoor air pollution (IAP) has an association with the severity of COVID-19. This, supported by studies on factors such as smoking which is associated with the adverse prognosis of the disease, because of the negative impact it has on the lung and the immune system (Vardavas and Nikitara, 2020).
Solid fuel smoke, burned in inefficient devices, possesses most of the toxins found in tobacco smoke and has also been associated with a variety of diseases, including chronic obstructive pulmonary disease and lung cancer in women and acute respiratory infection in children (Perez-Padilla et al., 2010). Notably, the child population exposed to IAP increases the risk of childhood pneumonia two-fold and is associated with 45% of pneumonia deaths in children under 5 years (WHO, 2018).
In our country, 23 million people use wood in their homes (INEGI, 2012), which mainly inhabit rural and marginalized urban areas (Berrueta et al., 2017). Our research group has identified different areas with IAP scenarios in indigenous populations (Flores-Ramirez et al., 2016; Martínez-Salinas et al., 2010; Martinez-Salinas et al., 2011), in whose prevalence of respiratory diseases is 39% compared to 22% in non-indigenous communities among people with similar demographic characteristics (PNUD, 2010).
On the other hand, despite the fact that smoke is composed of several toxic and even carcinogenic pollutants (Naeher et al., 2007), particulate matter (PM) that has a diameter of less than 2.5 μm are the best indicator for assessing health risks from IAP (Northcross et al., 2015). This is because they have been associated with different health effects, mainly with respiratory and cardiovascular diseases (Wyzga and Rohr, 2015). The effects on the respiratory system include: increased incidence and severity of asthma, decreased lung function, increased chronic respiratory disease, exacerbation of bronchitis symptoms, and an increase in acute respiratory infections mainly from viral or bacterial origin (Gordon, 2007).
The particles present different size and physical form, which allows PM2.5 to pass through the respiratory system, depositing mainly in the tracheobronchial region and reaching the alveoli (Hsu et al., 2011). Studies in rural communities of Michoacán indicate average PM2.5 concentrations in households from 51 to 319 μg/m3 (Schilmann et al., 2019), en San Luis Potosí, 155.2 μg/m3 (Estevez-Garcia et al., 2020). In Mexico, the Official Mexican Norm NOM-025-SSA1–2014, establishes that the maximum concentration must be 45 μg/m3 (SSA, 2014); meanwhile, the WHO has published a maximum permissible limit of 25 μg/m3 as an average of 24 h (OMS, 2006).
The main factors that increase the proportion of these pollutants are the size of the dwelling, the ventilation of the kitchen, the relative humidity, the temperature, but also the use of a stove inside the home. To this end, efficient stove programmes have been designed, which have managed to reduce PM2.5 (Zuk et al., 2007) y furthermore, it has been shown to reduce the effects mainly in terms of reducing the duration of the respiratory infection (Schilmann et al., 2015). This program has been implemented in some states and extensively in indigenous areas, however, it has not had the continuity and follow-up, now during the COVID-19 pandemic, there is an excellent area of opportunity to implement programs to transition to cleaner energy that achieves adoption and sustained use.
For all the above reasons, a contaminated environment must be considered as a factor of vulnerability to the serious effects of COVID-19. We are aware that this review is based on studies of environmental contamination carried out in indigenous communities in Mexico, and that no conclusive evidence has been shown about environmental contamination and the severity of COVID-19. Nevertheless, the Precautionary Principle must be used in this case even though there are considerable scientific uncertainties about the probability, causality, magnitude and nature of the damage of a certain disease (Aven and Bouder, 2020): this is exactly the case of COVID-19 in the indigenous regions of Mexico.
4. Identification of the health vulnerability of the indigenous population
The unfavorable health and quality of life conditions that have historically prevailed among the indigenous people of Mexico are well known. Because of the COVID-19, we can identify two main vulnerabilities for health in indigenous peoples, i) health coverage and ii) development of the disease.
The Health System in Mexico is a segmented system consisting of a social security system that serves the population with a formal job and covers 50% of the population and the other social protection model (Popular Insurance now the Health Institute for Welfare) created to serve the rest of the population.
In the indigenous areas, social security coverage is only 11%, with a predominance of 70.6% affiliation to the Popular Insurance and 15.1% with no health coverage at all (Freyermuth, 2018).
The distribution of health resources also presents an enormous difference. While in the municipalities without an indigenous presence there are 377 clinics and 336 beds, the municipalities with high indigenous presence have only 63 clinics and 31 beds per 100 thousand inhabitants. The distribution of human resources for health is also unequal. In municipalities where there is no indigenous presence, the rate of doctors (general and specialists) is 670 per 100,000 inhabitants, compared to 86 doctors in municipalities with a high indigenous presence (Freyermuth, 2018). Their most common access to health services is through a medical intern. This intern, the only doctor in the community, is responsible for attending to all illnesses as well as generating all the preventive health programs that should be implemented in the community (Palacios-Ramirez et al., 2018). Other challenges associated with health coverage are the geographical distribution of staff at the subnational level and the areas of care that must be addressed (WHO, 2016).
In Mexico, almost 20 million people lack access to health services, many of whom are indigenous people (CONEVAL, 2017). Therefore, it is not enough just to have human resources, but programmes should be promoted to facilitate their mobility to territories with greater health inequality.
The United Nations Department of Economic and Social Affairs of Indigenous People, mentions that all indigenous populations have much more precarious health, are more likely to become disabled and to have their quality of life diminished, and ultimately die younger than other populations.
One of the greatest problems faced by indigenous people, particularly women, is the fact that they have the worst health indicators in the whole country: high general mortality, high infant mortality, high maternal mortality and high prevalence of malnutrition. It is also a population with high fertility rates and short intergenesic periods (SSA, 2012).
Within the 20 leading causes of death in the indigenous Mexican population, non-communicable diseases such as heart disease, malignant tumors, diabetes mellitus type 2 (DM2), chronic obstructive pulmonary disease and two infectious diseases remain among the leading causes of death, intestinal infections, influenza, and pneumonia (SSA, 2012).
Chronic diseases in our country, Diabetes mellitus type 2, hypertension and obesity are present at alarming rates. In the Mexican indigenous population, it has been indicated that there is a prevalence of metabolic syndrome of up to 50.3%, with a prevalence of 42.7% of high blood pressure (Mendoza-Caamal et al., 2020).
There is increasing evidence from national health systems that a higher burden of chronic kidney disease occurs in indigenous populations driven by social disadvantage, greater loss of kidney function, and increased progression among indigenous people with diabetes (Dyck et al., 2014; Yeates and Tonelli, 2006).
On the other hand, some states in Mexico are dengue and zika endemic areas, the rainy season in Mexico is typically between the months of July–October, and historically cases of dengue and dengue hemorrhagic fever infection are increasing (Hernández-Gaytán et al., 2017). So we will have a high probability of co-infections of both viruses in indigenous areas, with mixed symptoms, which may worsen the epidemiological situation of diagnosis, control, and treatment.
The scenario recorded in this article is one of very high health risk in a context of lack of adequate information for better decision-making, which cannot be ignored by public health authorities.
It is clear then that health must be approached from another horizon and with non-conventional health tools. In the face of this pandemic, it reflects that not only clinical care and the construction of hospitals are necessary to fight it, but it extends to a wide range of factors that make it possible to build a healthy life, such as access to drinking water, food security, housing, living and working in healthy environments, health education, and information, and gender equity.
5. Tools to increase adaptive capacity
At this time the health system is based on disease. But the World Health Assembly, since 2016, has called for a shift in strategy towards a framework on people-centered health services, which could be achieved by applying five strategies (OMS, 2016). The five interdependent strategies are i) making people and communities responsible and involved; ii) strengthening participatory governance and common responsibility; iii) re-orienting the care model, strengthening primary care and re-evaluating advocacy and prevention efforts; (iv) coordinating services between and within sectors, not only in the health sector but also in other sectors, such as social services, finance, education, employment, housing, and the environment; and (v) creating conditions for achieving integrated attention, people-centered care, which requires the implementation of complex innovations in processes and services.
A community-based health system that could be achieved by applying for protection, prevention, promotion, and preparedness, building inter-institutional alliances to promote health as the axis of environmental, health, educational and food interventions, at different levels and in multiple and simultaneous directions. Starting with participatory schemes, local networks with health personnel, health promoters and families (Frenk and Gómez-Dantés, 2016). Through common structures and the development of its relational, contextual, anticipatory, strategic and innovative components, community-based health is built, which allows for the orientation of collective efforts towards health promotion and prevention of COVID-19. Among the actions to be developed are participatory community diagnoses, the formation of local multidisciplinary teams, mobile brigades and campaigns, participatory workshops, multilevel evaluation, and early warning systems, among others.
The health risk in the most vulnerable population within the context must be determined through a combination of participatory techniques that allow us to understand the population's perception of risk. Its main lines of action should focus on monitoring the disease, timely detection of cases and community strategies to prevent transmission. Communities must have the right to propose contextualized intervention strategies based on reliable information, respecting at all times the interests and priorities of the community.
6. Conclusion
The contaminated community, besides suffering the environmental threats, are areas of high poverty and, therefore, the domestic activities are precarious and of the informal economic sector, with no health control and no economic support to improve working conditions. Poverty has been associated with greater social disadvantage, lack of access to health services, poor quality of education services, lack of nutritional education (obesity) and/or lack of food (malnutrition), lack of drinking water, addictions, domestic violence and finally, the migration of human capital. (WHO, 2010). In rural areas, this includes mismanagement of natural resources in the environment, leading to problems with biodiversity and ecosystems' environmental services.
One element of cohesion, perhaps the first in importance, is health. Health is a priority for society. Health is closely related to education and the economy. When someone in the family falls ill, individual and family well-being is affected. The lack of access to health services to which the indigenous population is exposed causes health expenses, which, tied to the situation of poverty in which they are immersed, leads to catastrophic and/or impoverishing expenses that put at risk the subsequent growth of individuals and their family environment. In other terms, health is the best element of cohesion for inserting proposals for development and progress in contaminated communities, given the vulnerability to which they are exposed in the presence of the COVID-19 pandemic.
CRediT authorship contribution statement
Lorena Díaz de León-Martínez:Conceptualization, Writing - original draft, Writing - review & editing, Methodology.Luz de la Sierra-de la Vega:Writing - original draft.Andrés Palacios-Ramírez:Writing - original draft.Maribel Rodriguez-Aguilar:Writing - original draft.Rogelio Flores-Ramírez:Conceptualization, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Asad A.L., Hwang J. Migration to the United States from indigenous communities in Mexico. The ANNALS of the American Academy of Political and Social Science. 2019;684:120–145. [Google Scholar]
- Aven T., Bouder F. The COVID-19 pandemic: how can risk science help? J. Risk Res. 2020:1–6. [Google Scholar]
- Baud D., Qi X., Nielsen-Saines K., Musso D., Pomar L., Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30195-X. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrueta V.M., Serrano-Medrano M., Garcia-Bustamante C., Astier M., Masera O.R. Promoting sustainable local development of rural communities and mitigating climate change: the case of Mexico's Patsari improved cookstove project. Clim. Chang. 2017;140:63–77. [Google Scholar]
- Caramelo F., Ferreira N., Oliveiros B. 2020. Estimation of Risk Factors for COVID-19 Mortality - Preliminary Results. medRxiv. (2020.02.24.20027268) [Google Scholar]
- Cheng Y., Luo R., Wang K., Zhang M., Wang Z., Dong L. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CONEVAL . Consejo Nacional de Evaluación de la Política de Desarrollo Social; 2017. Coneval informa la evolución de la pobreza 2010–2016. [Google Scholar]
- CONEVAL . Consejo Nacional de Evaluación de la Política de Desarrollo Social; Ciudad de México: 2019. La pobreza en la población indígena de México, 2008–2018. [Google Scholar]
- Cutter S.L. Vulnerability to environmental hazards. Prog. Hum. Geogr. 1996;20:529–539. [Google Scholar]
- Dandekar R., Barbastathis G. 2020. Neural Network Aided Quarantine Control Model Estimation of COVID Spread in Wuhan, China. arXiv preprint arXiv:2003.09403. [Google Scholar]
- Díaz de León-Martínez L., Solis-Mercado J., Rodríguez-Aguilar M., Díaz-Barriga F., Guzmán Ortíz D., Flores-Ramírez R. Assessment of aflatoxin B1-lysine adduct in serum of infant population of the Huasteca Potosina, México – a pilot study. World Mycotoxin J. 2019;12:421–429. [Google Scholar]
- Durin S., Moreno R., Sheridan C. Rostros desconocidos. Perfil sociodemográfico de las indígenas en Monterrey. Trayectorias. 2007;9:29–42. [Google Scholar]
- Dyck R.F., Jiang Y., Osgood N.D. The long-term risks of end stage renal disease and mortality among first nations and non-first nations people with youth-onset diabetes. Can. J. Diabetes. 2014;38:237–243. doi: 10.1016/j.jcjd.2014.03.005. [DOI] [PubMed] [Google Scholar]
- Estevez-Garcia J.A., Schilmann A., Riojas-Rodriguez H., Berrueta V., Blanco S., Villasenor-Lozano C.G. Women exposure to household air pollution after an improved cookstove program in rural San Luis Potosi, Mexico. Sci. Total Environ. 2020;702:134456. doi: 10.1016/j.scitotenv.2019.134456. [DOI] [PubMed] [Google Scholar]
- Flores-Ramirez R., Rico-Escobar E., Nunez-Monreal J.E., Garcia-Nieto E., Carrizales L., Ilizaliturri-Hernandez C. Children exposure to lead in contaminated sites. Salud Publica Mex. 2012;54:383–392. doi: 10.1590/s0036-36342012000400008. [DOI] [PubMed] [Google Scholar]
- Flores-Ramirez R., Perez-Vazquez F.J., Cilia-Lopez V.G., Zuki-Orozco B.A., Carrizales L., Batres-Esquivel L.E. Assessment of exposure to mixture pollutants in Mexican indigenous children. Environ. Sci. Pollut. Res. Int. 2016;23:8577–8588. doi: 10.1007/s11356-016-6101-y. [DOI] [PubMed] [Google Scholar]
- Flores-Ramirez R., Perez-Vazquez F.J., Rodriguez-Aguilar M., Medellin-Garibay S.E., Van Brussel E., Cubillas-Tejeda A.C. Biomonitoring of persistent organic pollutants (POPs) in child populations living near contaminated sites in Mexico. Sci. Total Environ. 2017;579:1120–1126. doi: 10.1016/j.scitotenv.2016.11.087. [DOI] [PubMed] [Google Scholar]
- Freedman M., Bennett S.D., Rainey R., Otieno R., Quick R. Cost analysis of the implementation of portable handwashing and drinking water stations in rural Kenyan health facilities. J. Water Sanit. Hyg. Dev. 2017;7:659–664. [Google Scholar]
- Frenk J., Gómez-Dantés O. ¿ Atención a la salud o la enfermedad? Restableciendo el equilibrio. Salud Publica Mex. 2016;58:84b–88b. [Google Scholar]
- Freyermuth G. Mortalidad en poblaciones indígenas desde los determinantes sociales y violencia estructural. In: CIESAS, editor. El derecho a la protección de la salud en las mujeres indígenas en México. Análisis nacional y de casos desde una perspectiva de Derechos Humanos, Ciudad de México. 2018. [Google Scholar]
- Fu L., Fei J., Xiang H.-X., Xiang Y., Tan Z.-X., Li M.-D. Fang-Fang and Liu, Hong-Yan and Zheng, Ling and Li, Ying and Zhao, Hui and Xu, De-Xiang, Analysis of Death Risk Factors among. 2020. Analysis of death risk factors among 200 COVID-19 patients in Wuhan, China: A hospital-based case-cohort study; p. 200. [Google Scholar]
- Gordon T. Linking health effects to PM components, size, and sources. Inhal. Toxicol. 2007;19(Suppl. 1):3–6. doi: 10.1080/08958370701490312. [DOI] [PubMed] [Google Scholar]
- Hancock T., Spady D.W., Soskolne C.L. Canadian Public Health Association; 2016. Global Change and Public Health: Addressing the Ecological Determinants of Health. [Google Scholar]
- Hernández-Gaytán S.I., Díaz-Vásquez F.J., Duran-Arenas L.G., López Cervantes M., Rothenberg S.J. 20 years spatial-temporal analysis of dengue fever and hemorrhagic fever in Mexico. Arch. Med. Res. 2017;48:653–662. doi: 10.1016/j.arcmed.2018.01.003. [DOI] [PubMed] [Google Scholar]
- Holmes S.M. The clinical gaze in the practice of migrant health: Mexican migrants in the United States. Soc. Sci. Med. 2012;74:873–881. doi: 10.1016/j.socscimed.2011.06.067. [DOI] [PubMed] [Google Scholar]
- Hsu S.O., Ito K., Lippmann M. Effects of thoracic and fine PM and their components on heart rate and pulmonary function in COPD patients. J. Expo. Sci. Environ. Epidemiol. 2011;21:464–472. doi: 10.1038/jes.2011.7. [DOI] [PubMed] [Google Scholar]
- INEGI . 2012. Censo de Población y Vivienda 2010: Tabulados del Cuestionario Básico, México. [Google Scholar]
- INEGI, editor. Encuesta Nacional sobre Disponibilidad y Uso de Tecnologías de la Información en los Hogares (ENDUTIH) 2019. Instituto Nacional de Estadística y Geografía. Instituto Nacional de Estadística y Geografía México; 2019. [Google Scholar]
- INPI . Instituto Nacional de los Pueblos Indígenas; 2017. Indicadores Socioeconómicos de los Pueblos Indígenas de México, 2015. [Google Scholar]
- Jordan R.E., Adab P., Cheng K.K. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- Julie Turkewitz. The New York Times; 2020. Indigenous Groups Isolated by Coronavirus Face another Threat: Hunger. [Google Scholar]
- Kearney M. Transnational Oaxacan indigenous identity: the case of Mixtecs and Zapotecs. Identities. 2000;7:173–195. [Google Scholar]
- Landrigan P.J., Fuller R., Acosta N.J.R., Adeyi O., Arnold R., Basu N.N. The lancet commission on pollution and health. Lancet. 2018;391:462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- León-Pérez G. Internal migration and the health of indigenous Mexicans: a longitudinal study. SSM - population health. 2019;8:100407. doi: 10.1016/j.ssmph.2019.100407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liem A., Wang C., Wariyanti Y., Latkin C.A., Hall B.J. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e20. doi: 10.1016/S2215-0366(20)30076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G., Henry B.M. Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19) Respir. Med. 2020 doi: 10.1016/j.rmed.2020.105941. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lizardi-Jiménez M.A., Aguirre-García G.J. Carcinogenic hydrocarbon pollution in Quintana Roo's sinkholes: biotechnology for remediation and social participation for prevention. 2018;16:20170245. [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Salinas R., Elena Leal M., Batres-Esquivel L., Domínguez-Cortinas G., Calderón J., Díaz-Barriga F. Exposure of children to polycyclic aromatic hydrocarbons in Mexico: assessment of multiple sources. Int. Arch. Occup. Environ. Health. 2010;83:617–623. doi: 10.1007/s00420-009-0482-x. [DOI] [PubMed] [Google Scholar]
- Martinez-Salinas R.I., Perez-Maldonado I.N., Batres-Esquivel L.E., Flores-Ramirez R., Diaz-Barriga F. Assessment of DDT, DDE, and 1-hydroxypyrene levels in blood and urine samples in children from Chiapas Mexico. Environ. Sci. Pollut. Res. Int. 2011;19:2658–2666. doi: 10.1007/s11356-012-0758-7. [DOI] [PubMed] [Google Scholar]
- Mendoza-Caamal E.C., Barajas-Olmos F., García-Ortiz H., Cicerón-Arellano I., Martínez-Hernández A., Córdova E.J. Metabolic syndrome in indigenous communities in Mexico: a descriptive and cross-sectional study. BMC Public Health. 2020;20:339. doi: 10.1186/s12889-020-8378-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montenegro R.A., Stephens C. Indigenous health in Latin America and the Caribbean. Lancet. 2006;367:1859–1869. doi: 10.1016/S0140-6736(06)68808-9. [DOI] [PubMed] [Google Scholar]
- Naeher L.P., Brauer M., Lipsett M., Zelikoff J.T., Simpson C.D., Koenig J.Q. Woodsmoke health effects: a review. Inhal. Toxicol. 2007;19:67–106. doi: 10.1080/08958370600985875. [DOI] [PubMed] [Google Scholar]
- Northcross A.L., Hwang N., Balakrishnan K., Mehta S. Assessing exposures to household air pollution in public health research and program evaluation. Ecohealth. 2015;12:57–67. doi: 10.1007/s10393-014-0990-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OMS . 2006. Guías de calidad del aire de la OMS relativas al material particulado, el ozono, el dióxido de nitrógeno y el dióxido de azufre. Actualización mundial 2005. Ginebra, Suiza. [Google Scholar]
- OMS . Organización Mundial de la Salud; 2016. Marco sobre servicios de salud integrados y centrados en la persona: Informe de la Secretaría. [Google Scholar]
- Palacios-Ramirez A., Flores Ramirez R., Javier Perez-Vazquez F., Rodriguez-Aguilar M., Schilmann A., Riojas-Rodriguez H. Assessment of exposure to polycyclic aromatic hydrocarbons (PAHs) and suspended particles (PM2. 5) generated by the burning of biomass in an indigenous area in the state of San Luis Potosi, Mexico. Revista De Salud Ambiental. 2018;18:29–36. [Google Scholar]
- Pérez Campuzano E., Santos Cerquera C. Tendencias recientes de la migración interna en México. Papeles de población. 2013;19:53–88. [Google Scholar]
- Pérez-Herrera N., Díaz de León-Martínez L., Flores-Ramírez R., Barbier O., Ortega-Romero M., May-Euán F. Evaluation of benzene exposure and early biomarkers of kidney damage in children exposed to solvents due to precarious work in Ticul, Yucatán, México. Annals of global health. 2019;85:94. doi: 10.5334/aogh.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Padilla R., Schilmann A., Riojas-Rodriguez H. Respiratory health effects of indoor air pollution. Int. J. Tuberc. Lung Dis. 2010;14:1079–1086. [PubMed] [Google Scholar]
- PNUD . La verdadera riqueza de las naciones: caminos al desarrollo humano, Programa de las Naciones Unidas para el Desarrollo. 2010. Informe sobre Desarrollo Humano 2010. [Google Scholar]
- Schilmann A., Riojas-Rodriguez H., Ramirez-Sedeno K., Berrueta V.M., Perez-Padilla R., Romieu I. Children's respiratory health after an efficient biomass stove (Patsari) intervention. Ecohealth. 2015;12:68–76. doi: 10.1007/s10393-014-0965-4. [DOI] [PubMed] [Google Scholar]
- Schilmann A., Riojas-Rodríguez H., Catalán-Vázquez M., Estevez-García J.A., Masera O., Berrueta-Soriano V. A follow-up study after an improved cookstove intervention in rural Mexico: estimation of household energy use and chronic PM2.5 exposure. Environ. Int. 2019;131 doi: 10.1016/j.envint.2019.105013. [DOI] [PubMed] [Google Scholar]
- Silva V.M., Lizardi-Jiménez M.A. 2020. Environmental Problems and the State of Compliance with the Right to a Healthy Environment in a Mining Region of México; p. 20190179. [Google Scholar]
- SSA . Secretaría de Salud; México, Ciudad de México: 2012. Perfil Epidemiológico de los Municipios Indígenas en México. [Google Scholar]
- SSA . In: NORMA Oficial Mexicana NOM-025-SSA1–2014, Salud ambiental. Valores límite permisibles para la concentración de partículas suspendidas PM10 y PM2.5 en el aire ambiente y criterios para su evaluación. COFEPRIS, editor. DOF; México: 2014. [Google Scholar]
- Sunkel G., Ullmann H. Las tecnologías de la información y las comunicaciones (TIC): una clave para la inclusión de las personas mayores en América Latina. Revista de la CEPAL. 2019;127 [Google Scholar]
- Valdivia-Rivera S., Martínez-Cano A.K., Aguirre-García G., Lizardi-Jiménez M.A. Hydrocarbon water-pollution related to chronic kidney disease in Tierra Blanca, a perfect storm. Environ. Int. 2018;121:1204–1209. doi: 10.1016/j.envint.2018.10.036. [DOI] [PubMed] [Google Scholar]
- Vardavas C.I., Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob. Induc. Dis. 2020;18:20. doi: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2010. Hidden Cities: Unmasking and Overcoming Health Inequities in Urban Settings. [Google Scholar]
- WHO . World Health Organization; 2016. Global Strategy on Human Resources for Health: Workforce 2030. [Google Scholar]
- WHO . World Health Organization; Geneva, Switzerland: 2018. Household Air Pollution and Health. [Google Scholar]
- WHO . WHO Regional Office for Europe. WHO Regional Office for Europe; Denmark: 2020. World Water Day 2020 Highlights the Essential Role of Handwashing. [Google Scholar]
- Wyzga R.E., Rohr A.C. Long-term particulate matter exposure: attributing health effects to individual PM components. J. Air Waste Manag. Assoc. 2015;65:523–543. doi: 10.1080/10962247.2015.1020396. [DOI] [PubMed] [Google Scholar]
- Yeates K., Tonelli M. Indigenous health: update on the impact of diabetes and chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 2006;15:588–592. doi: 10.1097/01.mnh.0000247495.54882.e4. [DOI] [PubMed] [Google Scholar]
- Zavaleta C. COVID-19: review indigenous peoples' data. Nature. 2020;580:185. doi: 10.1038/d41586-020-01032-1. [DOI] [PubMed] [Google Scholar]
- Zuk M., Rojas L., Blanco S., Serrano P., Cruz J., Angeles F. The impact of improved wood-burning stoves on fine particulate matter concentrations in rural Mexican homes. J. Expo. Sci. Environ. Epidemiol. 2007;17:224–232. doi: 10.1038/sj.jes.7500499. [DOI] [PubMed] [Google Scholar]