Abstract
Background
The 2019 Coronavirus Disease (COVID-19) pandemic has become a global health emergency. The extreme actions aimed to reduce virus diffusion have profoundly changed the lifestyles of the Italian population. Moreover, fear of contracting the infection has generated high levels of anxiety. This study aimed to understand the psychological impact of the COVID-19 outbreak on sleep quality, general anxiety symptomatology, and psychological distress.
Methods
An online survey collected information on socio-demographic data and additional information concerning the COVID-19 pandemic. Furthermore, sleep quality, sleep disorders, generalized anxiety symptoms, psychological distress, and post-traumatic stress disorder (PTSD) symptomatology related to COVID-19 were assessed.
Results
This study included 2291 respondents. The results revealed that 57.1% of participants reported poor sleep quality, 32.1% high anxiety, 41.8% high distress, and 7.6% reported PTSD symptomatology linked to COVID-19. Youth and women, those uncertain regarding possible COVID-19 infection, and greater fear of direct contact with those infected by COVID-19 had an increased risk of developing sleep disturbances, as well as higher levels of anxiety and distress. Finally, a significant relationship between sleep quality, generalized anxiety, and psychological distress with PTSD symptoms related to COVID-19 was evidenced.
Conclusions
Our findings indicate that the COVID-19 pandemic appears to be a risk factor for sleep disorders and psychological diseases in the Italian population, as previously reported in China. These results should be used as a starting point for further studies aimed to develop psychological interventions to minimize the brief and long-term consequences of the COVID-19 pandemic.
Keywords: COVID-19, Generalized anxiety, Psychological well-being, Post-traumatic stress disorder, PTSD, Sleep quality
Highlights
-
•
The COVID-19 pandemic is a risk factor for sleep disorders and psychological diseases.
-
•
Low sleep quality, anxiety, and distress are associated with COVID-19-related PTSD.
-
•
Youth and women have a greater risk of developing COVID-19-related sleep disorders and distress.
1. Introduction
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), known as Coronavirus disease 2019 (COVID-19), was first identified in December 2019 in the city of Wuhan, located in central China [1]. At the end of December 2019, COVID-19 began to spread rapidly on a global scale. At the beginning of February 2020, a massive outbreak of the infection was reported in Italy. Moreover, Italy quickly became one of the countries with the highest COVID-19 infection and victim rates. As of April 8th 2020, more than 139.442 Italians have been infected by COVID-19, and approximately 17.669 have died [2].
On March 8th, the Italian Government implemented extraordinary measures to limit viral transmission and to minimize contact with people infected by COVID-19. The Italian population has been subjected to a substantial period of social isolation with a restriction of movements, in some cases characterized by a formal mandatory quarantine. Social distancing measures have also been imposed. Many people have been detained at home, allowing them to go to work only if their physical presence was deemed essential. Leaving home is only allowed if strictly necessary.
These extreme rules profoundly changed lifestyles and social relationships and, together with the fear of contracting the infection, have probably generated profound levels of anxiety. Therefore, it is reasonable to speculate that psychological conditions may be compromised during the COVID-19 outbreak, not only in the population directly affected by the virus but also in the general population. Unpleasant experiences and their related psychological distress would strictly connect with the perception of constrained freedom as a consequence of the quarantine [3]. Although the measures adopted have been fundamental to reduce the outbreak of the virus, they may have a high psychological cost for the population that should be noted [4].
Previous studies reported a negative impact on the mental health of those who underwent unexpected events, which could culminate in post-traumatic symptomatology [5]. Traumatic events, such as those related to the global spread of unknown epidemics [3,6], generate psychological distress and anxiety symptoms, which impact sleep quality [7]. These diseases may represent the first signs of the development of more severe symptoms, which could culminate in the onset of post-traumatic stress disorder (PTSD).
Researches on the COVID-19 pandemic are still absent in the Italian population. However, several studies conducted in China on the COVID-19 epidemic confirmed the role of both medical impacts of the infection and restrained measures on psychological dimensions, sleep quality, well-being, as well as more complex syndromes (eg, PTSD) [8,9]. Accordingly, this study is aimed to take a brief look into the psychological cost of the COVID-19 emergency on the Italian population forced to isolation and social distancing. Specifically, sleep quality, generalized anxiety, psychological distress, and the risk of PTSD have been investigated.
2. Material and methods
2.1. Study design and participants
A web-based cross-sectional survey, broadcasted through different platforms and mainstream social-media, was used to collect data in the Italian population. The survey was enabled from March 18th to April 2nd. A brief presentation informed the participants about the aims of the study, and electronic informed consent was requested from each participant before starting the investigation. The survey took approximately 30 min to complete. A short questionnaire collected information on some demographic and COVID-19 related information. Standardized questionnaires to evaluate psychological dimensions were administered. To guarantee anonymity, no personal data, which could allow the identification of participants, was collected. Due to the aim of the current research, having at least 18 years was the only inclusion criterion adopted. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Department of Dynamic and Clinical Psychology, “Sapienza” University of Rome (protocol number: 0000266). Participants could withdraw from the survey at any moment without providing any justification, and no data were saved. Only data from questionnaires that had a complete set of participant responses were considered. In sum, 98% of respondents (2.291 participants out of 2.332) that started the questionnaires completed the whole survey and were considered for the statistical analyses.
2.2. Outcomes
Demographic COVID related information: to collect data on gender, age, education, occupation, and region of origin, a questionnaire including demographic information was administered. A section aimed to evaluate contact on COVID-19 infection was included.
Generalized Anxiety Symptoms: the General Anxiety Disorder questionnaire (GAD-7) [10] was administered. The GAD includes 7 items on a 4-point Likert scale ranging from 0 (never) to 3 (nearly every day). The total score ranges from 0 to 21, with higher scores indicating more severe functional impairments as a result of anxiety. For this study, we defined a GAD-7 total score of 10 points or higher as an index of the presence of generalized anxiety symptoms [11].
Psychological Well-Being: to measure general psychological well-being or distress, the Psychological General Well-Being questionnaire (PGWB) was adopted [12]. The PGWB consists of 22 items, divided into six dimensions: Anxiety, Depressed mood, Positive well-being, Self-control, General health, and Vitality. Responses are given on a 6-point Likert scale ranging from 0 to 5. The total score ranges from 0 to 110. A global score and measures for each dimension are calculated, with higher scores indicating greater well-being. In our study, PGWB scores lower than 60 indicated a higher level of distress according to Chassany et al. [13].
Sleep Quality: sleep characteristics have been assessed through the Pittsburgh Sleep Quality Index (PSQI) [14], an 18-item questionnaire used to measure sleep quality. The PSQI includes items evaluating sleep quality, sleep duration, sleep latency, habitual sleep efficiency, sleep disorders, the use of sleeping medications, and daytime dysfunctions. Each dimension scored between 0 and 3, with a total score ranging from 0 to 21. Higher scores indicate lower sleep quality. A global PSQI score higher than 5 points indicates poor sleep quality [14]. Moreover, to analyze variables not considered by the PSQI, we included in the survey some items focused on assessing sleep fragmentation (interruptions of sleep during the night), nap duration, the percentage of sleep efficiency and the total sleep time in minutes.
COVID-19 as a risk factor for PTSD occurrence: PTSD related to COVID-19 (COVID-19-PTSD; a modified version of PTSD Checklist for DSM-5; PCL-5) [15] is a self-reported questionnaire designed ad hoc to assess specific symptoms concerning the COVID-19 emergency, similar to PTSD symptoms, according to DSM-5 criteria. The questionnaire includes 19 items structured on a 5-point Likert scale (from 0 = not at all to 4 = extremely). The psychometric qualities of this questionnaire indicate a monofactorial structure, explaining 49% of the variance and a Cronbach's α equal to 0.94 [16].
2.3. Statistical analysis
Descriptive analyses were conducted to describe the demographic characteristics, as well as COVID-19 related aspects in the Italian population, considering the different Italian territorial areas involved in the emergency (North, Centre, South).
The Student's t-test was used to compare our data on sleep quality, generalized anxiety, and psychological distress with data from the general population, considering previous studies. Specifically, our data on sleep quality were compared with Curcio et al. [14], results on PSQI, scores of GAD-7 were compared with the data reported by Lowe et al. [11], and PGWB indices were confronted with those reported by Chassany et al., [13].
Analyses of Variance (ANOVAs) were performed to explore the different potential degree of the impact of the COVID-19 among the Italian territorial areas. The differences among the North Italy, Centre Italy, and South Italy were evaluated by considering the sleep quality (PSQI indices, sleep fragmentation, nap duration, sleep efficiency percentage, and total sleep time), the general anxiety symptomatology (GAD-7), and psychological distress (Anxiety, Depressed mood, Positive well-being, Self-control, General health, Vitality, General Well-Being by the PGWB).
The prevalence of low sleep quality, generalized anxiety, and psychological distress were reported, and logistic regressions were performed to explore the influence of demographic factors and contact with COVID-19 in determining risk for sleep quality, anxiety, and distress in our sample.
A regression model was performed to explore the role of sleep quality, general anxiety, and psychological distress on the COVID-19 post-traumatic symptomatology assessed by the COVID-19-PTSD questionnaire. All data were analyzed using Statistical Package for Social Sciences (SPSS) version 24.0 and Statistica 10.0.
P-values of less than 0.05 were considered statistically significant.
3. Results
3.1. Demographic characteristics
The characteristics of participants are shown in Table 1 .
Table 1.
Demographic characteristics of the sample and their distribution in the Italian territorial areas.
| Overall Sample (N = 2.291) | North Italy (N = 541) | Centre Italy (N = 574) | South Italy (N = 1.176) | |
|---|---|---|---|---|
| Sex, n (%) | ||||
| Man | 580 (25.3) | 107 (18.4) | 121 (20.9) | 352 (60.7) |
| Woman | 1.708 (74.6) | 434 (25.4) | 451 (26.4) | 823 (48.2) |
| Other | 3 (0.1) | – | 2 (66.7) | 1 (33.3) |
| Age, n (%) | ||||
| 18–29 years old | 1.571 (68.6) | 342 (21.8) | 374 (23.8) | 855 (54.4) |
| 30–49 years old | 485 (21.2) | 156 (32.2) | 130 (26.8) | 199 (41.0) |
| >50 years old | 235 (10.3) | 43 (18.3) | 70 (29.8) | 122 (51.9) |
| Education, n (%) | ||||
| Until middle School | 99 (4.4) | 22 (22.2) | 18 (18.2) | 59 (59.6) |
| High School | 1.136 (49.6) | 265 (23.3) | 242 (21.3) | 629 (55.4) |
| Undergraduate | ||||
| Health care | 246 (10.7) | 49 (19.9) | 80 (32.5) | 117 (47.6) |
| Other | 660 (28.8) | 174 (26.4) | 165 (25.0) | 321 (48.6) |
| Post-graduated | ||||
| Health care | 63 (2.7) | 10 (15.9) | 28 (44.4) | 25 (39.7) |
| Other | 87 (3.8) | 21 (24.1) | 41 (47.1) | 25 (28.7) |
| Occupation, n (%) | ||||
| Student | 1.073 (46.8) | 207 (19.3) | 272 (25.3) | 594 (55.4) |
| Employed | 688 (30.0) | 227 (33.0) | 162 (23.5) | 299 (43.5) |
| Unemployed | 279 (12.2) | 52 (18.6) | 61 (21.9) | 166 (59.5) |
| Self-Employed | 222 (9.7) | 50 (22.5) | 64 (28.9) | 108 (48.6) |
| Retired | 29 (1.3) | 5 (17.2) | 15 (51.7) | 9 (31.1) |
| Number of inhabitants in own city, n (%) | ||||
| <2.000 | 124 (5.4) | 28 (22.6) | 17 (13.7) | 79 (63.7) |
| 2.000–10.000 | 453 (19.8) | 130 (28.7) | 81 (17.9) | 242 (53.4) |
| 10.000–100.000 | 937 (40.9) | 199 (21.2) | 174 (18.6) | 564 (60.2) |
| >100.000 | 777 (33.9) | 184 (23.7) | 302 (38.9) | 291 (37.5) |
| Quarantine Experience, n (%) | ||||
| Alone | 234 (10.2) | 74 (31.6) | 59 (25.2) | 101 (43.2) |
| Others | 2.057 (89.8) | 467 (22.7) | 515 (25.0) | 1.075 (52.3) |
| Infection by the virus | ||||
| Yes | 9 (0.4) | 2 (22.2) | 2 (22.2) | 5 (55.6) |
| No | 1.707 (74.5) | 374 (21.6) | 409 (23.6) | 951 (54.8) |
| Do not know | 575 (25.1) | 192 (33.4) | 163 (28.4) | 220 (38.3) |
| Direct contact with people infected by COVID-19 | ||||
| Yes | 40 (1.7) | 28 (70.0) | 6 (15.0) | 6 (15.0) |
| No | 1.441 (62.9) | 274 (19.0) | 337 (23.4) | 830 (58.6) |
| Do not know | 810 (35.4) | 239 (29.5) | 231 (28.5) | 340 (42.0) |
| Knowledge of people infected by COVID-19 | ||||
| Yes | 550 (24.0) | 237 (43.1) | 126 (22.9) | 187 (30.4) |
| No | 1.741 (76.0) | 304 (17.5) | 448 (25.7) | 989 (56.8) |
| Knowledge of people in ICU for COVID-19 | ||||
| Yes | 177 (7.7) | 87 (49.2) | 39 (22.0) | 51 (28.8) |
| No | 2.114 (92.3) | 454 (21.5) | 535 (25.3) | 1.125 (53.2) |
| Knowledge of people died for COVID-19 | ||||
| Yes | 112 (4.9) | 66 (58.9) | 21 (18.8) | 25 (22.3) |
| No | 2.179 (95.1) | 475 (21.8) | 553 (25.4) | 1.151 (58.2) |
In sum, 2.291 individuals completed the questionnaires, 580 (25.3%) were men, and 1.708 (74.6%) were women and the mean age of the participants was 30.0 years (SD: 11.5 years; age range: 18–89). The most represented age range was 18–29 years (68.6%). Most of the participants (1.136; 49.6%) received a high school education and were students (1.073; 46.8%) or employees (688; 30.0%). The respondents’ current locations were sorted considering territorial area: North (23.6%), Centre (25.1%), and South (51.3%) of Italy. Most of the participants live in urban areas (937; 40.9%) with a number of inhabitants between 10.000 and 100.000.
Among all respondents, only 9 (0.4%) were infected with COVID-19, and 40 (1.7%) were certain that they had had close contact with individuals suspected to have contracted a COVID-19 infection (see Table 1). Of the overall sample, 112 respondents (4.9%) and 177 (7.7%) respectively knew people dead and inpatients in intensive care units (ICU) because of COVID-19.
3.2. Comparisons with data from the general population of sleep quality, generalized anxiety symptoms, and psychological distress during the COVID-19 epidemic
The comparisons of sleep quality, generalized anxiety symptoms, and psychological distress during the COVID-19 epidemic in the Italian population are presented in Table 2 .
Table 2.
Mean and SD of sleep quality, general anxiety symptomatology, psychological distress, and COVID-19-PTSD outcomes in the overall sample and comparison with data from general population.
| Respondents' Data | General Data | t student | p | |
|---|---|---|---|---|
| Sleep Quality | ||||
| PSQ indicesa | ||||
| Self-reported sleep quality | 1.13 (0.73) | 0.70 (0.26) | 1.86 | 0.06 |
| Sleep Latency | 1.15 (1.01) | 0.40 (0.22) | 2.34 | <0.05 |
| Sleep Duration | 0.62 (0.72) | 0.20 (0.13) | 1.84 | 0.06 |
| Habitual Sleep Efficiency | 1.00 (1.08) | 0.90 (0.46) | <1 | 0.77 |
| Sleep Disturbance | 1.03 (0.55) | 0.80 (0.13) | 1.32 | 0.18 |
| Use of Sleeping Medication | 0.17 (0.60) | 0.00 (0.00) | <1 | 0.37 |
| Daytime dysfunctions | 0.60 (0.64) | 1.00 (0.00) | 1.97 | <0.05 |
| PSQ total score | 5.69 (3.40) | 4.00 (0.42) | 1.57 | 0.11 |
| Symptom of Anxiety (GAD)b | ||||
| Total | 7.61 (5.23) | 2.95 (3.41) | 45.4 | 0.0001 |
| Psychological Well-Being (PGWB)c | ||||
| Anxiety | 62.50 (21.51) | 72.80 (19.18) | 14.98 | <0.0001 |
| Depressed Mood | 78.88 (16.46) | 83.35 (16.43) | 8.35 | <0.0001 |
| Positive well-being | 44.74 (17.58) | 62.67 (18.65) | 30.39 | <0.0001 |
| Self-Control | 69.83 (19.30) | 80.27 (18.80) | 16.70 | <0.0001 |
| General Health | 71.06 (15.94) | 75.87 (18.47) | 8.52 | <0.0001 |
| Vitality | 58.13 (19.45) | 68.48 (18.32) | 16.64 | <0.0001 |
| Total Well-being | 62.88 (15.69) | 72.86 (15.56) | 18.49 | <0.0001 |
| Post-Traumatic Stress Disorder Symptomatology (COIVD-19-PTSD) | ||||
| Total | 19.88 (15.88) | N/A | ||
PSQ general data from Curcio et al., 2013.
GAD data from Lowe et al., 2008.
PGWB data from Chassany et al., 2004.
Considering PSQI indices, sleep latency (t = 2.34; p < 0.05) significantly differs from of the general population [14], indicating greater difficulty in sleep onset in our sample.
GAD-7 scores appear to be higher in our sample compared to data from the general population (t = 45.4; p < 0.0001) of Lowe et al. [11], as well as psychological distress assessed by the PGWB indices (t > 8.35; p < 0.0001) compared to Chassany et al.'s data [13].
3.3. Differences in sleep quality, generalized anxiety symptoms, and psychological distress among north, centre, and South Italy
Table 3 presents the group differences in sleep characteristics and psychological dimensions, considering North, Centre and South Italy.
Table 3.
Mean and SD of sleep quality, general anxiety symptomatology, psychological distress, and COVID-19-PTSD outcomes in the different Italian territorial areas, and ANOVA's results.
| North Italy | Center Italy | South Italy | F | p | |
|---|---|---|---|---|---|
| Sleep Quality | |||||
| Sleep Disorders (PSQ) | |||||
| Self-reported sleep quality | 1.17 (0.75) | 1.13 (0.73) | 1.10 (0.70) | 1.90 | 0.14 |
| Sleep Latency | 1.16 (1.01) | 1.20 (1.05) | 1.12 (0.98) | 1.35 | 0.25 |
| Sleep Duration | 0.68 (0.75) | 0.60 (0.69) | 0.61 (0.72) | 2.3 | 0.07 |
| Habitual Sleep Efficiency | 1.07 (1.11) | 1.04 (1.09) | 0.94 (1.06) | 3.55 | <0.05 |
| Sleep Disturbance | 1.04 (0.54) | 1.06 (0.53) | 1.01 (0.56) | 2.24 | 0.10 |
| Use of Sleeping Medication | 0.21 (0.70) | 0.20 (0.67) | 0.12 (0.50) | 6.00 | <0.01 |
| Daytime dysfunction | 0.60 (0.64) | 0.65 (0.65) | 0.58 (0.64) | 2.29 | 0.10 |
| PSQ total score | 5.94 (3.55) | 5.88 (3.45) | 5.47 (3.29) | 4.84 | <0.01 |
| Low sleep quality (%) | 60.3 | 58.5 | 54.9 | ||
| Sleep Quality Items | |||||
| Sleep Fragmentation index % | 1.74 (3.19) | 1.42 (2.72) | 1.26 (2.48) | 5.88 | <0.01 |
| Sleep Efficiency (%) | 78.42 (15.18) | 79.50 (13.85) | 80.35 (14.18) | 3.41 | <0.05 |
| Total Sleep Time (minutes) | 388.96 (95.59) | 398.34 (88.17) | 399.08 (87.97) | 2.51 | 0.08 |
| Diurnal nap (minutes) | 10.67 (25.05) | 9.09 (23.6) | 14.28 (28.59) | 8.38 | <0.001 |
| Symptom of Anxiety (GAD) | |||||
| Total | 7.78 (5.39) | 7.49 (5.13) | 7.60 (5.20) | <1 | 0.64 |
| High general anxiety symptomatology (n%) | 33.4 | 31.8 | 31.8 | ||
| Psychological Well-Being (PGWB) | |||||
| Anxiety | 61.3 (22.10) | 62.74 (20.44) | 62.79 (21.75) | <1 | 0.56 |
| Depressed Mood | 78.82 (16.13) | 78.85 (15.58) | 78.92 (17.03) | <1 | 0.99 |
| Positive well-being | 44.94 (17.41) | 44.31 (17.85) | 44.85 (17.54) | <1 | 0.79 |
| Self-Control | 69.08 (19.35) | 70.63 (18.61) | 69.79 (19.62) | <1 | 0.41 |
| General Health | 69.89 (16.56) | 70.60 (15.21) | 71.82 (15.98) | 3.04 | 0.05 |
| Vitality | 54.54 (19.16) | 57.44 (19.44) | 58.73 (19.59) | 1.17 | 0.31 |
| Total Well-being | 62.34 (15.63) | 62.77 (15.07) | 63.17 (16.01) | <1 | 0.58 |
| High Distress (%) | 42.1 | 43.2 | 41.0 | ||
| Post-Traumatic Stress Disorder Symptomatology (COIVD-19-PTSD) | |||||
| Total | 20.89 (16.26) | 19.44 (15.13) | 19.63 (16.04) | 1.47 | 0.22 |
| Higher PTSD COVID-19 related symptomatology (%) | 9.2 | 6.3 | 7.4 | ||
Considering Sleep Quality assessed by the PSQI, significant differences were reported in habitual sleep efficiency (F2,2288 = 3.55; p < 0.05; η2 = 0.003), use of sleep medication (F2,2288 = 6.00; p < 0.01; pη2 = 0.01) and PSQI total score (F2,2288 = 4.84; p < 0.01; pη2 = 0.004). Moreover, significant differences were highlighted in sleep fragmentation (F2,2288 = 5.88; p < 0.003; η2 = 0.01), percentage of sleep efficiency (F2,2288 = 3.41; p < 0.05; pη2 = 0.004) and diurnal naps (F2,2288 = 8.38; p < 0.0001; pη2 = 0.01).
Generally, people from North Italy reported the worst sleep quality compared to people from South Italy, specifically considering habitual sleep efficiency (p < 0.05), use of sleep medication (p < 0.01), PSQI total score (p < 0.01). Furthermore, a higher sleep fragmentation index (p < 0.001), a low percentage of sleep efficiency (p < 0.01), and shorter nap times (p < 0.01) were reported in respondents from North Italy compared to respondents from South Italy.
People from Centre Italy reported low sleep quality (p < 0.05), higher use of medication (p < 0.01), and lower naps time (p < 0.0001) compared to those who live in the South of Italy. No differences were reported between people from North and Centre Italy, except for sleep fragmentation (p < 0.05) with the worst condition in North Italy.
Significant differences were reported between individuals from North, Centre, and South Italy considering the General Health subscale of PGWB (F2,2288 = 3.04; p < 0.05; pη2 = 0.003). In particular, North Italian respondents showed the worst perception of general health compared to South Italian respondents (p < 0.01), no other differences were significant.
Considering GAD (F < 1; p = 0.64) and PTSD (F2,2288 = 1.47; p < 0.22) no significant differences were found (see Table 3).
3.4. Prevalence and risk factors of sleep disorders, generalized anxiety symptoms, and psychological distress during the COVID-19 epidemic
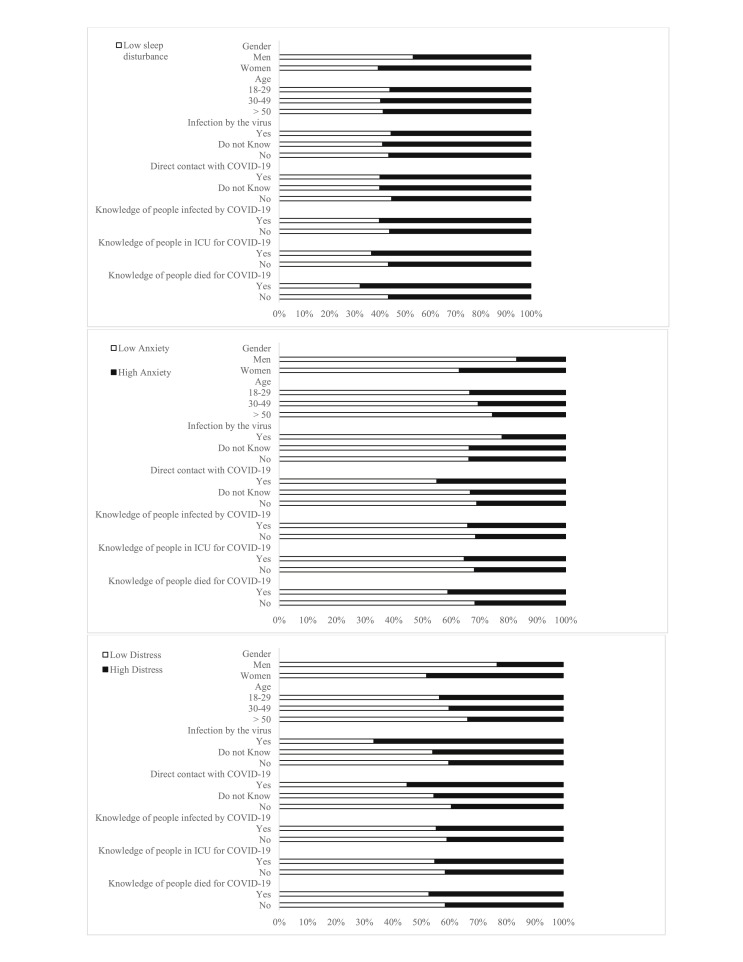
The prevalence of poor sleep quality, generalized anxiety symptoms, and psychological distress stratified by gender, age, territorial areas, knowledge of people affected by COVID-19, and loneliness in social isolation experience are shown in Fig. 1 .
Fig. 1.
Prevalence of poor sleep quality, generalized anxiety symptoms and psychological distress.
The overall prevalence of low sleep quality, high generalized anxiety symptoms, and psychological distress were 57.1%, 32.1%, and 41.8%, respectively.
Logistic regressions showed that the risk of sleep disorders was higher in women (OR = 1.75; 95% CI = 1.45–2.13), those unemployed (OR = 1.34; 95% CI = 1.02–1.70), those living in North Italy (OR = 1.24; 95% CI = 1.01–1.53), those uncertain regarding direct contact with individuals infected by COVID-19 (OR = 1.21; 95% CI = 1.02–1.45), and those who knew people that died because of COVID-19 (OR = 1.62; 95% CI = 1.08–2.43). Considering generalized anxiety symptomatology, being female (OR = 2.87; 95% CI = 2.27–3.64), younger than 30 years (OR = 1.47; 95% CI = 1.08–2.01), having a post graduate title in a health care profession (OR = 3.00; 95% CI = 1.22–7.39), and knowing people who died because of COVID-19 (OR = 1.51; 95% CI = 1.02–2.22) appeared to be risk factors. Higher risk of psychological distress was linked to being female (OR = 3.05; 95% CI = 2.46-3-79), a range age between 18 and 30 years (OR = 1.52; 95% CI = 1.14–2.03), uncertainty regarding possible COVID-19 infection (OR = 1.26; 95% CI = 1.04–1.52) and uncertainty (OR = 1.28; 95% CI = 1.07–1.52) or certainty about direct contact with people infected by COVID-19 (OR = 1.88; 95% CI = 1.00–3.53) (See Table 4 ).
Table 4.
Results of logistic regression analysis.
| Low Sleep Quality | High Anxiety Symptoms | High Psychological Distress | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Prevalences in overall sample, n (% | 1309 (57.1) | 735 (32.1) | 958 (41.8) | ||||||
| B | OR (95% CI) | p | B | OR (95% CI) | p | B | OR (95% CI) | p | |
| Gender, n (%) | |||||||||
| Man | Reference | Reference | Reference | ||||||
| Woman | 0.56 | 1.75 (1.45–2.13) | <0.0001 | 1.06 | 2.87 (2.27–3.64) | <0.0001 | 1.12 | 3.05 (2.46–3.79) | <0.0001 |
| Age, n (%) | |||||||||
| 18–29 years old | −0.11 | 0.89 (0.68–1.18) | 0.44 | 0.39 | 1.47 (1.08–2.01) | <0.01 | 0.42 | 1.52 (1.14–2.03) | <0.01 |
| 30–49 years old | 0.04 | 1.04 (0.76–1.43) | 0.78 | 0.25 | 1.28 (0.90–1.82) | 0.17 | 0.28 | 1.33 (0.96–1.84) | 0.08 |
| >50 years old | Reference | Reference | Reference | ||||||
| Education, n (%) | |||||||||
| Until middle School | Reference | Reference | Reference | ||||||
| High School | 0.38 | 1.47 (0.97–2.21) | 0.06 | −0.32 | 0.73 (0.46–1.15) | 0.17 | 0.31 | 1.37 (0.89–2.10) | 0.15 |
| Undergraduate | |||||||||
| Other | 0.31 | 1.36 (0.89–2.07) | 0.15 | −0.27 | 0.77 (0.48–1.23) | 0.27 | 0.25 | 1.28 (0.83–1.99) | 0.27 |
| Health Care | 0.13 | 1.14 (0.72–1.82) | 0.57 | 0.01 | 1.00 (0.59–1.69) | 0.99 | −0.06 | 0.94 (0.58–1.53) | 0.81 |
| Post-graduated | |||||||||
| Other | 0.18 | 1.20 (0.67–2.13) | 0.54 | −0.34 | 0.71 (0.38–1.33) | 0.29 | 0.31 | 1.36 (0.75–2.45) | 0.31 |
| Health Care | 0.31 | 1.36 (0.72–2.57) | 0.34 | 1.10 | 3.00 (1.22–7.39) | <0.05 | −0.21 | 0.81 (0.42–1.59) | 0.55 |
| Occupation, n (%) | |||||||||
| Student | Reference | Reference | Reference | ||||||
| Employed | −0.01 | 0.98 (0.81–1.19) | 0.88 | −0.26 | 0.77 (0.63–0.95) | <0.05 | −0.29 | 0.75 (0.62–0.91) | <0.01 |
| Unemployed | 0.29 | 1.34 (1.02–1.7) | <0.05 | 0.17 | 1.18 (0.89–1.5) | 0.23 | −0.08 | 0.92 (0.70–1.20) | 0.53 |
| Self-Employed | −0.08 | 0.92 (0.69–1.23) | 0.59 | −0.28 | 0.76 (0.55–1.04) | 0.09 | −0.34 | 0.71 (0.53–0.96) | <0.05 |
| Retired | 0.38 | 1.46 (0.67–3.18) | 0.33 | 0.03 | 1.03 (0.47–2.24) | 0.94 | −0.45 | 0.64 (0.29–1.39) | 0.26 |
| Territorial Area | |||||||||
| North Italy | 0.22 | 1.24 (1.01–1.53) | <0.05 | 0.02 | 0.97 (0.78–1.20) | 0.79 | 0.05 | 1.05 (0.85–1.29) | 0.65 |
| Center Italy | 0.15 | 1.17 (0.95–1.43) | 0.13 | 0.08 | 1.09 (0.88–1.35) | 0.45 | 0.09 | 1.09 (0.89–1.34) | 0.38 |
| South Italy | Reference | Reference | Reference | ||||||
| Number of inhabitants, n (%) | |||||||||
| <2.000 | Reference | Reference | Reference | ||||||
| 2.000–10.000 | −0.02 | 0.98 (0.65–1.47) | 0.93 | 0.26 | 1.30 (0.84–2.00) | 0.24 | 0.24 | 1.27 (0.85–1.90) | 0.24 |
| 10.000–100.000 | −0.17 | 0.84 (0.57–1.23) | 0.37 | 0.20 | 1.22 (0.81–1.84) | 0.34 | 0.01 | 0.99 (0.68–1.45) | 0.96 |
| >100.000 | −0.18 | 0.83 (0.56–1.22) | 0.35 | 0.03 | 1.03 (0.68–1.56) | 0.90 | 0.04 | 0.95 (0.65–1.40) | 0.82 |
| Quarantine Experience, n (%) | |||||||||
| Alone | 0.05 | 0.95 (0.72–1.25) | 0.71 | 0.14 | 1.14 (0.85–1.54) | 0.37 | 0.04 | 1.04 (0.79–1.37) | 0.76 |
| Others | Reference | Reference | Reference | ||||||
| Infection by the virus | |||||||||
| Yes | 0.04 | 0.96 (0.26–3.59) | 0.95 | 0.48 | 1.62 (0.33–7.80) | 0.55 | 1.09 | 2.96 (0.74–11.88) | 0.12 |
| Do not Know | 0.10 | 1.10 (0.91–1.34) | 0.31 | 0.10 | 1.10 (0.90–1.35) | 0.34 | 0.23 | 1.26 (1.04–1.52) | <0.05 |
| No | Reference | Reference | Reference | ||||||
| Direct contact with people infected by COVID-19 | |||||||||
| Yes | 0.19 | 1.21 (0.64–2.29) | 0.56 | 0.60 | 1.82 (0.97–3.43) | 0.06 | 0.63 | 1.88 (1.00–3.53) | <0.05 |
| Do not Know | 0.20 | 1.21 (1.02–1.45) | 0.03 | 0.11 | 1.11 (0.93–1.34) | 0.26 | 0.25 | 1.28 (1.07–1.52) | <0.01 |
| No | Reference | Reference | Reference | ||||||
| Knowledge of people infected by COVID-19 | |||||||||
| Yes | 0.17 | 1.18 (0.97–1.43) | 0.09 | 0.13 | 1.13 (0.92–1.29) | 0.23 | 0.16 | 1.17 (0.96–1.42) | 0.11 |
| No | Reference | Reference | Reference | ||||||
| Knowledge of people in ICU for COVID-19 | |||||||||
| Yes | 0.28 | 1.32 (0.96–1.81) | 0.08 | 0.14 | 1.15 (0.84–1.59) | 0.38 | 0.15 | 1.16 (0.85–1.58) | 0.34 |
| No | Reference | Reference | Reference | ||||||
| Knowledge of people died for COVID-19 | |||||||||
| Yes | 0.48 | 1.62 (1.08–2.43) | <0.05 | 0.41 | 1.51 (1.02–2.22) | <0.05 | 0.24 | 1.26 (0.86–1.85) | 0.22 |
| No | Reference | Reference | Reference | ||||||
3.5. Prevalence and variables associated with PTSD COVID-related symptoms
Considering all respondents enrolled in this study, 173 reported a high level of PTSD COVID-related, with a score higher than 1.5 standard deviations from the mean scores, indicating a prevalence of PTSD symptomatology in this sample of 7.6%.
The linear regression analysis, adjusted for gender, age and the mean of the days spent in quarantine by the respondents revealed a significant predictive role (F6,2290 = 806.76; p < 0.0001; R2 = 0.68; Adjusted R2 = 0.68) of sleep quality, generalized anxiety and psychological distress toward COVID-19-PTSD scores (see Table 5 ).
Table 5.
Regression model considering sleep quality (PSQI total score), general anxiety symptomatology (GAD-7 total score) and psychological distress (PGWB total score) as predictor of COVID-19-PTSD.
| Model | B | Std.Err | Beta | T | Sign (p<) | 95% CI lower | 95% CI upper |
|---|---|---|---|---|---|---|---|
| PSQI global score | 0.63 | 0.07 | 0.14 | 9.36 | 0.0001 | 0.50 | 0.76 |
| GAD-7 global score | 1.25 | 0.06 | 0.41 | 20.82 | 0.0001 | 1.14 | 1.37 |
| PGWB global score | −0.37 | 0.02 | −0.36 | −17.37 | 0.0001 | −0.41 | −0.33 |
4. Discussion
The rapid human-to-human transmission of COVID-19 has greatly influenced national and international policies. To the best of our knowledge, our study is the first to report the psychological effects of the COVID-19 emergency in Italy, approximately two months after the Sars-COVID-2 outbreak and one month after mandatory strict isolation and social distancing dispositions of the Italian Government. These severe measures were taken to avoid further spread of the COVID-19 epidemic, including the request to isolation at home for both people infected by the virus and people without infection, prohibiting all gathering activities, and mandating the wearing of surgical masks in public places. As this is the first instance in Italy that such contention measures were adopted, this study aimed to document the well-being of the Italian population forced to quarantine through the context of sleep quality, generalized anxiety symptoms, and psychological distress.
The results revealed that 57.1% of the respondents experienced poor sleep quality, 32.1% had high levels of generalized anxiety symptoms, 41.8% experienced psychological distress, and 7.6% reported relevant PTSD symptomatology linked to the COVID-19 diffusion. Studies on the Italian population underlined a 30% prevalence of sleep problems [17], with 10.3% anxiety disorders [18], and 29.3% experiencing psychological distress [19]. However, the use of various questionnaires to assess these psychological dimensions and the different samples in the studies made a statistical comparison impossible. However, it is possible to observe that our results showed a substantially worse psychological condition during the actual emergency. Finally, it is impossible to differentiate whether the results are attributable to the fear of the epidemic or the restrictive measures imposed by the Italian government.
Characteristics of the sample (eg, younger age, being female, having uncertainty about the possibility of contracting the infection by COVID-19, or having had direct contacts with people infected by COVID-19) appear to relate with wore psychological conditions. Individuals with these characteristics are more likely to develop sleep problems, anxiety symptomatology, and psychological distress, similar to what has been reported in previous studies on the COVID-19 or the SARS outbreak [20,21].
The results of the present study have shown that two out of three Italians had disturbed sleep during the COVID-19 outbreak, although the comparison with previous data from the general population underlined significant differences only in sleep latency and daytime dysfunctions. However, significant differences were reported in sleep quality considering Italian territorial areas with a worse status in North Italy, according to the most widespread and the highest number of deaths due to COVID-19 in this Italian territorial area. Extensive research has documented the importance of sleep in restoring neurobehavioral functions and many psychological aspects, including emotion regulation, depression, and anxiety [22]. Moreover, other psychological conditions, such as PTSD and other stress-related disorders, are significantly associated with an impairment of sleep quality [7,22]. Reduced sleep quality negatively affects life satisfaction, health status, social, and emotional domains [23,24]. Additionally, studies have reported an association between poor sleep quality and high risk of falls, infections, or the cold virus as a consequence of a reduction of the immune response [25]. Therefore, investigating sleep quality during the COVID-19 pandemic became critical to estimate the psychological well-being of the Italian population. Although it should be noted that further studies are needed.
Considering other psychological variables, one out of three Italians showed higher generalized anxiety symptoms, and two out of five Italians perceived psychological distress and lower well-being during the COVID-19 pandemic. As reported by studies on natural disasters, war crisis, and other epidemic emergencies [[26], [27], [28]], these situations are associated with high levels of anxiety and distress, which represent some of the precursors of the PTSD onset. In our sample, these results have been confirmed. Sleep quality, generalized anxiety, and psychological distress were associated with PTSD symptomatology. Our findings confirmed the results of previous studies on the priority role of disturbed sleep in contributing to the development of PTSD symptoms [29]. Moreover, we confirmed the results of preceding studies on the Chinese population who reported high concomitance of sleep disturbance, psychological distress, and anxiety in the general population during the COVID-19 outbreak, with an increased risk of PTSD occurrence [20,30]. Although further longitudinal studies are necessary, the present findings make us worry about the possible development of PTSD in the Italian population consequent to the COVID-19 emergency.
To better understand the current Italian status, one aim of this study was to compare our data with previous ones reported by researches on the general population and collected under usual conditions [11,13,14]. Our results, as expected, indicated poor sleep quality, higher levels of generalized anxiety, and higher psychological distress in the Italian population involved in the COVID-19 emergency. Although these results should be considered with caution, given some characteristics of the samples considered, they further confirm the stressful impact of the COVID-19 pandemic on the well-being of the Italian population. The uncertainty of the epidemic progression, together with the restrictive measures adopted by the Italian Government, is causing higher psychological pressure due to the fear that the epidemic is hard to control. In the first few weeks alone, the COVID-19 pandemic has already had dangerous effects on the Italian population. Our findings suggest that symptoms highlighted above can be a potent risk factor for the development of psychological diseases as previously reported for the Chinese population and accordingly with other studies on epidemic and quarantine conditions [3,[31], [32], [33]].
Considering the perception and the effects of the COVID-19 epidemic in the different territorial areas, people who reside in North Italy, considered the principal Italian core of the emergency, characterized by the highest number of infections and deaths [2], compared to Centre and South Italy, reported the worst sleep quality and psychological symptomatology. These results are consistent with a study about the psychological impact of the SARS, which demonstrated that residents in the region with the high prevalence of SARS cases have shown higher psychological consequences and were prone to develop PTSD symptomology [34]. People living in high infection-prevalent locations perceive themselves to be at higher risk of infection, as confirmed by the low general health perception reported in the PGWB. Conversely, the lockdown of the transport hub and the overload of the public health system in most cities of North Italy could have led to a detrimental psychological impact on residents impacting on sleep quality and psychological symptomatology. Yet, this relationship has not been clarified. Some studies suggested that people who were repeatedly exposed to traumatic events were prone to suffering from many psychological problems [35]. Other researchers found no relationship between the prolonged exposure to critical events and the gravity of psychological symptoms [36] considering exposure to epidemics [37]. As stated previously, further studies are needed to explore the psychological distress associated with the exposure history of epidemics, considering the restrictive measures adopted to contain the contagion.
Although the findings of the current study appear relevant in the current COVID-19 emergency, some limitations need to be considered. First, the data and results were derived from a cross-sectional design, making causal inferences challenging. In addition, the adoption of the online survey limits the generalizability of the results, although it currently represents the best solution for data collection in times of social distancing. Accordingly, a recruitment bias emerged in our sample, which is characterized by a high number of young adults, mainly students, and women. This aspect should be considered in the interpretation of the results. Especially those variables that were compared with previous data collected on the general population, because these characteristics could be associated with an increased risk of psychopathological conditions. The risk factors analyses have also suggested it. Moreover, some aspects (eg, younger age or being female) could have affected the individual responses to the actual emergency. Considering the statistical comparisons with the general population data, the absence of percentage data on the considered dimensions in the general population did not allow us to compare our percentages in the investigated diseases with the prevalence of sleep disturbance, generalized anxiety, and psychological distress in the general population.
5. Conclusion
Previous studies have shown that the epidemic diffusion of viral diseases (eg, SARS, Ebola) can be related to anxiety, depression, distress, sleep disorders, and post-traumatic stress disorders, not only for the medical impact of the infection but also for the impact of quarantine measures aimed to reduce the outbreak [3]. Accordingly, studies conducted in China on the effect of the COVID-19 diffusion on psychological dimensions and well-being highlighted similar results [8,9]. This study, for the first time, confirmed similar results considering the Italian population, and investigates some aspects of the role of extreme situations on the variables under investigation.
Generally, there is still a lack of relevant research on the targeted intervention on psychological aspects during the COVID-19 epidemic. However, it should be essential to increase the number of these studies, not only in the Italian population but also in the other countries in which the COVID-19 emergency is spreading. These results appear relevant to predispose effective psychological interventions focused on the improvement of the psychological well-being and in the reduction of risk of occurrence of stress-related disorders. Interventions of this kind are recommended, especially considering vulnerable populations.
Role of the funding source
There was no funding source for this study. The authors have full access to all the data of the study, and they take responsibility for the integrity and accuracy of the data analyses and the submission of the manuscript. Declaration of interests.We declare no competing interests.
CRediT authorship contribution statement
Maria Casagrande: Conceptualization, Methodology, Investigation, Resources, Writing - original draft, Writing - review & editing, Supervision. Francesca Favieri: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft, Writing - review & editing. Renata Tambelli: Conceptualization, Investigation, Resources, Writing - review & editing, Supervision. Giuseppe Forte: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft, Writing - review & editing.
Acknowledgments
There is no funding support for this survey. We want to thank Gianluca Pistore and all the other people who helped in the data collection by sharing our survey on the various social network.
Footnotes
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2020.05.011.
Conflict of interest
The following is the Supplementary data to this article:
References
- 1.World Health Organization . 2020. Coronavirus disease (COVID-2019) situation reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ Consulted on April 1st. [Google Scholar]
- 2.Istituto Superiore di Sanità. 2020. Epicentro. Coronavirus.https://www.epicentro.iss.it/coronavirus/ Consulted on April 8th. [Google Scholar]
- 3.Brooks S.K., Webster R.K., Smith L.E. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubin G.J., Wessely S. The psychological effects of quarantining a city. BMJ. 2020:368. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 5.Mak I.W.C., Chu C.M., Pan P.C. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen Hosp Psychiatr. 2010;32(6):590–598. doi: 10.1016/j.genhosppsych.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hossain M.M., Sultana A., Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. SSRN. 2020:3561265. doi: 10.4178/epih.e2020038. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen S., Kaplan Z., Zohar J. Preventing sleep on the first resting phase following a traumatic event attenuates anxiety-related responses. Behvior brain res. 2017;320:450–456. doi: 10.1016/j.bbr.2016.10.039. [DOI] [PubMed] [Google Scholar]
- 8.Xiao H., Zhang Y., Kong D. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Mon Int Med J Exp Clin Res. 2020;26:e923549. doi: 10.12659/MSM.923549. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu S., Yang L., Zhang C. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiat. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spitzer R.L., Kroenke K., Williams J.B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch int med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 11.Löwe B., Decker O., Müller S. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. 2008:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 12.Dupuy H.J. The psychological general well-being (PGWB) index. In: Wenger N.K., Mattson M.E., Fuberg C.P., editors. Assessment of quality of life in clinical trials of cardiovascular therapies. Le Jacq; New York: 1984. [DOI] [PubMed] [Google Scholar]
- 13.Chassany O., Dimenas E., Dubois D. MAPI Research Institute; Lyon, France: 2004. The psychological general well-being index (PGWBI) user manual. [Google Scholar]
- 14.Curcio G., Tempesta D., Scarlata S. Validity of the Italian version of the Pittsburgh sleep quality index (PSQI) Neurol Sci. 2013;34(4):511–519. doi: 10.1007/s10072-012-1085-y. [DOI] [PubMed] [Google Scholar]
- 15.Blevins C.A., Weathers F.W., Davis M.T. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 16.Favieri F., Forte G., Tambelli R. 2020. The Italians in the time of coronavirus: psychosocial aspects of unexpected COVID-19 pandemic. Available at SSRN 3576804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leger D., Poursain B., Neubauer D. An international survey of sleeping problems in the general population. Curr Med Res Opin. 2008;24(1):307–317. doi: 10.1185/030079907x253771. [DOI] [PubMed] [Google Scholar]
- 18.de Girolamo G., Polidori G., Morosini P. Prevalence of common mental disorders in Italy. Soc Psychiatr Psychiatr Epidemiol. 2006;41(11):853–861. doi: 10.1007/s00127-006-0097-4. [DOI] [PubMed] [Google Scholar]
- 19.Eskin M., Sun J.M., Abuidhail J. Suicidal behavior and psychological distress in university students: a 12-nation study. Arch Suicide Res. 2016;20(3):369–388. doi: 10.1080/13811118.2015.1054055. [DOI] [PubMed] [Google Scholar]
- 20.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;112954 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su T.P., Lien T.C., Yang C.Y. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychol Res. 2007;41(1–2):119–130. doi: 10.1016/j.jpsychires.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baglioni C., Spiegelhalder K., Lombardo C. Sleep and emotions: a focus on insomnia. Sleep Med Rev. 2010;14(4):227–238. doi: 10.1016/j.smrv.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Zhi T.F., Sun X.M., Li S.J. Associations of sleep duration and sleep quality with life satisfaction in elderly Chinese: the mediating role of depression. Arch Gerontol Geriatr. 2016;65:211–217. doi: 10.1016/j.archger.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 24.Becker N.B., de Jesus S.N., Viseu J.N. Depression and quality of life in older adults: mediation effect of sleep quality. Int J clinic and health psychology. 2018;18(1):8–17. doi: 10.1016/j.ijchp.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prather A.A., Janicki-Deverts D., Hall M.H. Behaviorally assessed sleep and susceptibility to the common cold. Sleep. 2015;38(9):1353–1359. doi: 10.5665/sleep.4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beaglehole B., Mulder R.T., Frampton C.M. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychol. 2018;213(6):716–722. doi: 10.1192/bjp.2018.210. [DOI] [PubMed] [Google Scholar]
- 27.Comtesse H., Powell S., Soldo A. Long-term psychological distress of Bosnian war survivors: an 11-year follow-up of former displaced persons, returnees, and stayers. BMC Psychiatr. 2019;19(1):1. doi: 10.1186/s12888-018-1996-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.James P.B., Wardle J., Steel A. Post-Ebola psychosocial experiences and coping mechanisms among Ebola survivors: a systematic review. Trop Med Int Health. 2019;24(6):671–691. doi: 10.1111/tmi.13226. [DOI] [PubMed] [Google Scholar]
- 29.Mantua J., Helms S.M., Weymann K.B. Behav neurol; 2018. Sleep quality and emotion regulation interact to predict anxiety in veterans with PTSD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun L., Sun Z., Wu L. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in wuhan, China. MedRxiv. 2020 [Google Scholar]
- 31.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cao W., Fang Z., Hou G. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatr Res. 2020:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Publ Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee T.M.C., Chi I., Chung L.M. Ageing and psychological response during the post-SARS period. Aging Ment Health. 2006;10(3):303–311. doi: 10.1080/13607860600638545. [DOI] [PubMed] [Google Scholar]
- 35.Alexander D.A., Klein S. Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. Br J Psychiatry. 2001;178(1):76–81. doi: 10.1192/bjp.178.1.76. [DOI] [PubMed] [Google Scholar]
- 36.Declercq F., Meganck R., Deheegher J. Frequency of and subjective response to critical incidents in the prediction of PTSD in emergency personnel. J traum stress. 2011;24(1):133–136. doi: 10.1002/jts.20609. [DOI] [PubMed] [Google Scholar]
- 37.Xu J., Song X. Posttraumatic stress disorder among survivors of the Wenchuan earthquake 1 year after: prevalence and risk factors. Compr psych. 2011;52(4):431–437. doi: 10.1016/j.comppsych.2010.08.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.