Abstract
Objective
The objective of this study was to evaluate the pooled estimate of diabetes prevalence in young (<50 years) versus elderly (>50 years) COVID-19 cohorts.
Methods
Studies published between December-2019 and March-2020 reporting demographic and clinical characteristics of COVID-19 cases were identified. A total of 11 studies included accounting for 2084 COVID-19 patients.
Results
The overall prevalence of diabetes in COVID-19 patients with a mean age>50 years was 13.2%, whereas studies with relatively younger patients (mean age <50 years) had a pooled prevalence of 9.0%
Conclusion
The overall prevalence of diabetes in COVID-19 patients was found to be 13.2% with studies including relatively elderly patients showing higher rates of diabetes. The intermingled effects of diabetes with other cardiovascular comorbidities warrant age-specific outcomes data including the impact of ongoing antidiabetic treatment.
Keywords: COVID-19, Diabetes mellitus, Type-2 diabetes, Prevalence, Antidiabetic treatment, Elderly
1. Introduction
As of April 28, 2020, novel coronavirus disease 2019 (COVID-19) has accounted for the death of around 217,000 people worldwide. Upcoming reports have suggested that patients with COVID-19 infection have a high burden of complications [1], and underlying comorbidities like cardiovascular conditions, diabetes, and hypertension, and cancer [2]. A recent meta-analysis of studies published in China reported a pooled diabetes prevalence of 10.3% among patients infected with Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [3]. Furthermore, COVID-19 patients with adverse outcomes have a diabetes rate ratio of 2.26 (95% CI 1.47–3.49) compared to those with a favorable outcome [3]. Age has been suggested to be one of the important drivers of COVID-19 related mortality with a rate of 7.8% among elderly (>80 years) versus 0.0016% in children (aged ≤ 9 years) [4]. These figures suggest that the presence of diabetes in the elderly COVID-19 population could add-up to the worse outcomes. However, data on age-specific diabetes prevalence in COVID-19 patients remains unknown. Therefore, we sought to evaluate the pooled estimate of diabetes prevalence in young (<50 years) versus elderly (>50 years) COVID-19 cohorts.
2. Methods
From a literature review using PubMed, Scopus and Web of Science until March 2020, all eligible studies reporting frequency of diabetes mellitus were included. Random effects models were obtained, and I2 statistics were used to analyze heterogeneity. I2> 50% was considered moderate heterogeneity. A total of 11 studies included accounting for 2084 COVID-19 patients. Of these, the studies with a mean age of less than 50-years consisted of 1365 patients while cohorts with a mean age of>50-years included 107 patients.
3. Results
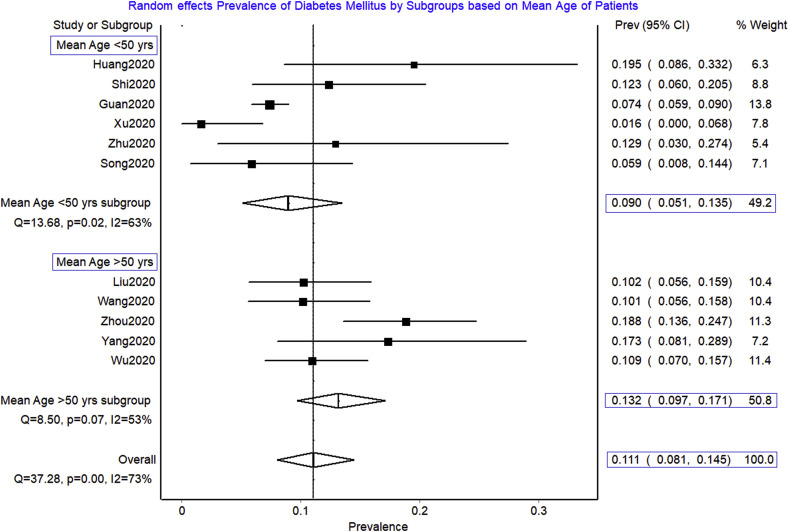
The overall prevalence of diabetes in studies including COVID-19 patients with a mean age >50 years was 13.2% [95% CI 9.7%–17.1%, I2 = 53%], whereas studies with relatively younger patients (mean age <50 years) had pooled prevalence of 9.0% [95% CI 5.1%–13.5%, I2 = 63%] (p < 0.001) ( Fig. 1 ). This meta-analysis revealed that the elderly COVID-19 population had a significantly higher burden of diabetes than the younger cohort (13.2% vs. 9.0%). This rate remains higher than the overall rate earlier studies have estimated (13.2% vs. 10.3%).
Fig. 1.
Pooled prevalence of diabetes mellitus in COVID-19.
4. Discussion
Studies from China and Italy have suggested older age and underlying health conditions to be major risk factors for severe COVID-19 disease. Consistently, a report from the United States also revealed that among 457 intensive care unit admissions, a majority (78%) of them occurred in older patients or patients with pre-existing comorbidities [5]. Previous studies on SARS-CoV reported that the presence of cardiac disease and diabetes could increase the risk of death by two folds as much as other risk factors [6]. Elderly patients with a high burden of diabetes may also have other underlying cardiovascular conditions. A study by Shi et al. suggested that COVID-19 patients with the underlying cardiovascular disease might also be susceptible to acute cardiac injury that could potentially increase the risk of in-hospital mortality [7]. Furthermore, older age is a major risk factor for the occurrence of arrhythmias, which could have an additive worse effect with the presence of diabetes, a chronic inflammatory state.
It has been noted that COVID-19 patients have hyperinflammatory syndrome characterized by fulminant and fatal hypercytokinaemia [8], which could predispose elderly patients with diabetes towards malignant arrhythmias. Elderly with diabetes often have concomitant hypertension which could require Angiotensin-converting enzyme-2 (ACE2) inhibitors (ACEIs) and angiotensin receptor blockers (ARBs). These medications have a debatable role in increasing the susceptibility for COVID-19 infection and related outcomes. ACE2 has been identified as one of the major receptors for SARS-Cov-2, which is also widely expressed in the pancreas [9]. Similarly, Dipeptidyl peptidase-4 (DPP-4) is reported as a primary receptor in MERS-CoV, however, its role in SARS-CoV-2 has not yet established [9]. With such limited knowledge, it is imperative to identify whether patients with diabetes who are on ARBs/ACEIs or any other anti-diabetic drugs exacerbate COVID-19 prognosis.
While we are still searching for drugs to cure COVID-19, one controversial treatment option relevant to patients with diabetes is hydroxychloroquine, which is widely used for malaria and autoimmune diseases. Several trials have shown that hydroxychloroquine decreased HbA1c level in decompensated diabetes patients [10], although, the exact mechanism remains unclear. Given the indirect effect of hydroxychloroquine in diabetes, and the possible role of ACE2 and DPP-4 in SARS-CoV2, caution is warranted when treating COVID-19 patients with diabetes. It is also conceivable that acute decompensated diabetes would severely hinder COVID-19 care and prognosis, especially among the geriatric population.
5. Conclusion
Concisely, it is essential to acknowledge that the prevalence of diabetes in elderly COVID-19 patients remain significantly higher. Considering the intermingled effects of diabetes with other cardiovascular comorbidities, age-specific outcomes data are warranted including the impact of underlying cardiovascular conditions and ongoing antidiabetic treatment on COVID-19 prognosis.
Declaration of competing interest
The authors report no relationships that could be construed as a conflict of interest.
References
- 1.Desai R., Singh S., Parekh T., Sachdeva S., Kumar L., Sachdeva R. COVID-19 and shock: a cautionary tale for elderly patients from a pooled analysis. Ann Emerg Med. 2020 doi: 10.1016/j.annemergmed.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Desai A., Sachdeva S., Parekh T., Desai R. COVID-19 and cancer: lessons from a pooled meta-analysis. JCO Glob Oncol. 2020:557. doi: 10.1200/GO.20.00097. –9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fadini G.P., Morieri M.L., Longato E., Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020 doi: 10.1007/s40618-020-01236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30243-7. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Team C.C.-R. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 — United States, february 12–march 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan J.W.M., Ng C.K., Chan Y.H., Mok T.Y.W., Lee S., Chu S.Y.Y. Short term outcome and risk factors for adverse clinical outcomes in adults with severe acute respiratory syndrome (SARS) Thorax. 2003;58:686–689. doi: 10.1136/thorax.58.8.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020 doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hussain A., Bhowmik B., Cristina do Vale Moreira N. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020 doi: 10.1016/j.diabres.2020.108142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar V., Singh M.P., Singh A.P., Pandey M.S., Kumar S., Kumar S. Efficacy and safety of hydroxychloroquine when added to stable insulin therapy in combination with metformin and glimepiride in patients with type 2 diabetes compare to sitagliptin. Int J Basic Clin Pharmacol. 2018;7:1959. doi: 10.18203/2319-2003.ijbcp20183930. –64. [DOI] [Google Scholar]