Graphical abstract
Keywords: Dapoxetine hydrochloride, Microenvironmental pH, Hydroxypropyl methyl cellulose E5, Maltodextrin, In vivo mouth dissolving time, Mechanical properties
Abstract
Instantly dissolving buccal films have gained attention owing to their easy administration and capability to surmount the hepatic first pass effect of drugs. Dapoxetine hydrochloride (DPX) has a low oral bioavailability due to significant hepatic first pass metabolism. In addition, DPX is a weakly basic drug with a pH dependent solubility that could limit its dissolution in the body neutral fluids. In order to surpass these challenges, this work aimed at enhancing DPX bioavailability via the formulation of instantly dissolving buccal films comprising a pH modifier and a hydrophilic cyclodextrin. Tartaric acid and hydroxypropyl beta-cyclodextrin were selected as dual solubilizing agents based on the screening study. 32 factorial design was employed for the formulation and optimization of DPX films. Statistical analysis revealed that hydroxypropyl methyl cellulose E5: maltodextrin ratio and propylene glycol concentrations have significant effects on mechanical properties, percent DPX dissolved after 5 min, and in vivo mouth dissolving time at P < 0.05. The optimized film [HPMC E5: MDX, 1:1 and 1% PG] showed no significant change of properties or drug dissolution upon storage at 40 °C/75% RH for a period of 3 months. In addition, the optimized film showed significantly enhanced absorption relative to the oral reference tablet. Therefore, the optimized film could be considered a promising delivery system for DPX with expected improved patient compliance and enhanced pharmacokinetic performance.
Introduction
Intraoral delivery systems (IODSs) have been used as a promising substitute to surmount the problems associated with oral drug administration. These dosage forms offer the advantages of easy administration and rapid action as they disintegrate or dissolve rapidly in the mouth. In addition, direct absorption of drugs into the systemic circulation could be achieved via the buccal mucosa, thus bypassing hepatic first pass [1]. Instantly disintegrating or dissolving tablets (IDT) have been introduced as the first IODSs for patients who suffer from dysphagia. They are characterized by their rapid disintegration and/or dissolution; however, they have some drawbacks such as difficult handling owing to their fragility. Accordingly, instantly dissolving buccal films have been introduced recently as an alternative to surpass the limitations associated with instantly dissolving tablets [2], [3], [4].
Instantly dissolving buccal films (IDBFs) are hydrocolloid based films that readily dissolve upon contact with the salivary fluid. They have recently gained attention due to enhanced patient compliance and capability of surmounting the problem of hepatic first pass of many drugs [5], [6]. However, intraoral administration of poorly soluble drugs poses a great challenge for their buccal absorption. Several approaches have been utilized for enhancing the dissolution of drugs including solid dispersion with water soluble polymers, binary systems with cyclodextrins [7], use of surfactants [8] and pH modifiers [9].
The use of pH modifiers has been reported as a worthwhile strategy for improving the dissolution and bioavailability of drugs characterized by pH-dependent solubility [10], [11]. A pH modifier could alter the microenvironmental pH of the drug particles to a pH that allows easy dissolution of the drug [12], [13], [14]. Organic acids have been extensively used as pH modifiers in the pharmaceutical field to increase the dissolution of weakly basic drugs [9], [15], [16], [17], [18], [19].
Cyclodextrins (CDs) oligomers of d-glucopyranose that have been widely used for drugs’ solubilization. Their solubilizing action is achieved via the formation of partial or complete inclusion complexes, in addition, to their surfactant-like properties that could promote wetting and dissolution of poorly soluble drugs. CDs, being biodegradable, non-toxic, and biocompatible, possess an advantage over surfactants and many other hydrophilic solubilizing agents [20], [21].
Dapoxetine hydrochloride (DPX) is a selective serotonin reuptake inhibitor for depression treatment. It was recently approved as an oral treatment for premature ejaculation (PE) to be the first selective serotonin reuptake inhibitor approved for this function [22], [23], however, DPX has an oral bioavailability of 42% owing to the drug significant hepatic first pass metabolism [24]. DPX presystemic metabolism represents a challenging limitation for oral administration of the drug and foreshadows the potential of utilizing transmucosal route for enhancing the drug’s bioavailability [25]. However, DPX is a weakly basic drug with a pH dependent solubility that could limit its dissolution in the body’s neutral fluids and subsequent absorption via mucosal barriers [26].
Transmucosal delivery of DPX via sublingual and intranasal mucosa has been investigated by Fouad et al. [26], [27] who developed DPX loaded instantly-soluble matrix and instantly-dispersible nanocarrier powder systems. In addition, buccal delivery of DPX has been investigated by Liew and Peh [28] who developed DPX orally disintegrating tablets and El-Refai et al. [29] who developed vardenafil hydrochloride/DPX hydrochloride orodispersible tablets. However, no attempts were reported for the formulation of dissolvable buccal films of DPX. Thus, this work was done with the objective of improving DPX bioavailability and providing rapid onset of action via the formulation of hydrophilic polymer-based instantly dissolving buccal films (IDBFs). Tartaric acid (as a pH modifier) and hydroxypropyl beta-cyclodextrin (as a hydrophilic solubilizer) were incorporated to improve the drug dissolution in the salivary pH. A 32 factorial design was employed to explore the effect of hydroxypropyl methyl cellulose E5 (HPMC E5; film former) to maltodextrin (MDX; film modifier) ratio and propylene glycol concentration (PG %; plasticizer) on the films’ characteristics and dissolution of DPX. In addition, DPX pharmacokinetic behavior was studied after buccal administration of the selected optimal formulation to rats in comparison to an oral reference product.
Material and methods
Material
Dapoxetine hydrochloride (DPX) was a gift from Spimaco (Riyadh, Saudi Arabia). Hydroxypropyl methyl cellulose E5 (HPMC E5), maltodextrin (MDX, dextrose equivalent 16.5–19.5), propylene glycol (PG), ethanol, citric acid (CA), malic acid (MA), L-tartaric acid (TA), saccharin, beta-cyclodextrin (β-CD, MW = 1135 Da), hydroxypropyl beta-cyclodextrin (HP-β-CD, average degree of substitution = 0.8 and MW = 1460 Da) and orange oil were purchased from Sigma Aldrich (St. Louis, Missouri, USA). High-performance liquid chromatography (HPLC) grade acetonitrile were purchased from Merck (Darmstadt, Germany). All other reagents and chemicals were of analytical grade.
Screening of organic acids and cyclodextrins for enhancing dissolution of DPX
Various organic acids (CA, MA, and TA) and cyclodextrins (β-CD and HP-β-CD) were assessed as acidifiers and hydrophilic solubilizers to enhance the dissolution of DPX. Equivalent amounts of DPX and each of the studied excipients were thoroughly mixed for 5 min. The dissolution behavior of specified quantity of each mixture equivalent to 30 mg DPX was done in 900 mL phosphate buffer (pH 6.8) using USP Dissolution Tester, apparatus II (DT 720, Erweka, Germany) operating at 50 rpm at 37 ± 0.5 °C [26]. Aliquot samples were withdrawn after 2 and 15 min and replaced with equal volume of fresh buffer. Samples were filtered through a 0.22 µm Millipore filter, and the concentration of DPX was quantified spectrophotometrically at 292 nm (UV-2600 PC; Shimadzu, Kyoto, Japan). The dissolution study was done in triplicate.
Preparation of DPX instantly dissolving buccal films (IDBFs)
Solvent casting technique was utilized to prepare IDBFs containing 30 mg DPX per dosage unit. In all formulations, TA and HP-β-CD were used as acidifier and hydrophilic solubilizer, respectively. Orange oil and saccharin were used as flavoring and sweetening agents, respectively, at a concentration of 0.2% each. The total concentration of HPMC and MDX was kept constant at 16%. In addition, ethanol was added at a concentration of 15% to all formulations. All percentages are expressed relative to the total dispersion. Briefly, specified quantities of HPMC, MDX, PG, and saccharin were dispersed in specified volume of distilled water (8 mL) with added ethanol (2.25 mL), and the volume was then completed to 15 mL. The prepared mixture was stirred at 70 °C for 45 min, and then cooled down to 40 °C. Subsequently, a mixture of equal amounts of DPX, HP-β-CD, and TA were stirred into the polymer solution, and then orange oil alcoholic solution was added. 10 mL of the mixture was poured into glass Petri dish (d = 7.5 cm) and left to dry in thermal oven adjusted to 40 °C overnight. The dried films were split into 1 × 3 cm strips (3 cm2), each containing 30 mg drug. The strips were placed individually in air-tight containers and stored in desiccators over CaCl2 at ambient temperature until further studies.
32Factorial design for formulation and optimization of DPX instantly dissolving buccal films
Preliminary studies were conducted to assess the effect of using various ratios of the film-forming polymer (HPMC E5) and the film modifier (MDX) on the IDBFs properties. The use of different concentrations of either glycerin or PG as a plasticizer was also investigated. The preliminary films were inspected for ability to peel, stickiness, surface perfection, and in vivo disintegration. According to the results, a 32 factorial design was utilized to explore the effect of the independent variables; HPMC E5: MDX ratio (X1) and PG percentage (X2). Each factor was studied at three levels and a total of nine formulations were prepared, Table 1, Table 2.
Table 1.
Independent variables and responses used in 32 full factorial experimental design for the formulation and optimization of dapoxetine hydrochloride instantly dissolving buccal films.
| Independent variables | Levels |
||
|---|---|---|---|
| (−1) | (0) | (+1) | |
| X1: HPMC E5: MDX (w/w) | 1:3 | 1:1 | 3:1 |
| X2: PG % | 1.00 | 3.00 | 5.00 |
| Responses | Desirability constraints | ||
| Y1: TS (MPa) | Minimize | ||
| Y2: % E (%) | Maximize | ||
| Y3: EM (MPa) | Minimize | ||
| Y3: % D5min (%) | Maximize | ||
| Y3: In vivo MDT (sec) | Minimize | ||
HPMC E5; Hydroxypropyl methyl cellulose E5, PG; Propylene glycol.
TS; Tensile strength, % E; Percent elongation at break, EM; Elastic (Young’s) modulus, % D5min; Percent drug dissolved after 5 min, In vivo MDT; In vivo mouth dissolving time
Table 2.
Composition and responses of dapoxetine hydrochloride instantly dissolving buccal films prepared according 32 full factorial design.
| Run | Independent Variables |
Responses (Dependent Variable) |
|||||
|---|---|---|---|---|---|---|---|
| HPMC E5: MDX (w/w, X1)* | PG (%, X2) | TS$ (MPa, Y1) | % E$ (%, Y2) | EM$ (MPa, Y3) | D5 min# (%, Y4) | MDT# (sec, Y5) | |
| F1 | 1:3 | 1.00 | 0.217 ± 0.014 | 147.97 ± 2.56 | 0.146 ± 0.009 | 84.76 ± 3.98 | 9.67 ± 0.56 |
| F2 | 1:3 | 3.00 | 0.434 ± 0.038 | 235.68 ± 5.14 | 0.184 ± 0.019 | 75.97 ± 4.23 | 14.32 ± 1.78 |
| F3 | 1:3 | 5.00 | 0.567 ± 0.043 | 273.88 ± 2.14 | 0.207 ± 0.031 | 71.21 ± 2.11 | 12.89 ± 0.78 |
| F4 | 1:1 | 1.00 | 0.811 ± 0.077 | 115.34 ± 1.56 | 0.703 ± 0.065 | 66.91 ± 2.45 | 13.15 ± 1.77 |
| F5 | 1:1 | 3.00 | 1.330 ± 0.098 | 144.56 ± 1.98 | 0.920 ± 0.087 | 72.12 ± 1.33 | 14.98 ± 0.81 |
| F6 | 1:1 | 5.00 | 1.934 ± 0.145 | 216.31 ± 3.87 | 0.894 ± 0.091 | 46.54 ± 0.98 | 19.12 ± 1.44 |
| F7 | 3:1 | 1.00 | 1.16 ± 0.156 | 92.35 ± 1.19 | 2.338 ± 0.134 | 52.98 ± 0.99 | 22.67 ± 1.65 |
| F8 | 3:1 | 3.00 | 4.22 ± 0.257 | 57.05 ± 0.99 | 7.397 ± 0.219 | 38.41 ± 1.14 | 23.54 ± 1.98 |
| F9 | 3:1 | 5.00 | 6.45 ± 0.549 | 39.52 ± 1.88 | 16.321 ± 0.341 | 37.08 ± 2.13 | 25.12 ± 2.12 |
HPMC E5; Hydroxypropyl methyl cellulose E5, MDX; maltodextrin, PG; Propylene glycol.
TS; tensile strength, %E; percentage elongation, EM; Elastic (Young’s) modulus, % D5min; Percent drug dissolved after 5 min, MDT; In vivo mouth- dissolving time, Values are expressed as mean ± SD; # n = 3, $n = 6.
The dependent variables (responses) including tensile strength (TS, Y1), percentage elongation (%E, Y2,), Elastic modulus (EM, Y3), in-vivo mouth dissolving time (MDT, Y4), and percentage DPX dissolved after 5 min (% DPX, Y5) were subjected to statistical analysis using Design-Expert® Software Version 11 (Stat-Ease Inc, Minneapolis, Minnesota, USA). ANOVA test was utilized to evaluate the impact of the variables on the studied responses at 95% level of significance. Mathematical equations corresponding to linear, two-factor interaction, and quadratic models were applied to relate the variables to the responses. The model maximizing the adjusted and predicted determination coefficients (R2) was selected for each response.
The desirability function that integrates all the studies responses to predict the optimum levels of the studied variables was computed to select the optimal formulation. The desired goals were maximizing the elongation percentage and percent DPX dissolved after 5 min., in addition to, minimizing in vivo mouth dissolving time, tensile strength, and elastic modulus, Table 1.
Dosage units’ uniformity
The prepared IDBFs were split into 1 × 1 cm strips. Ten strips were weighed individually and the average mass of each film was recorded in milligrams. Films’ thickness was measured using Vernier caliper micrometer (Shanghai, China); each film’s thickness was measured at six positions (two points in the center and four corners). To assess the uniformity of drug content, ten units of each of formulation were used. Each strip was dissolved in specified volume of distilled water (20 mL) and DPX content was detected spectrophotometrically at 292 nm (UV-2600 PC; Shimadzu, Kyoto, Japan). The determined drug content of the films was compared to the United States Pharmacopeial standards [30]. The acceptance value (AV) was also computed as follows:
Where M is label claim (100%), X is the mean DPX content (%), K is the acceptability constant (2.4 for n = 10), and SD is the standard deviation.
Moisture uptake
Before conducting the study, three strips (1 × 3 cm) from each formulation were placed in desiccator over CaCl2 for 48 h to ensure complete dryness. The strips were then accurately weighed and directly exposed to 75% relative humidity (RH) at 25 ± 1 °C for 7 days. The films were reweighed daily and the moisture uptake was computed as percent increase in the film’s weight [31].
Mechanical properties
The IDBFs were cut into 1 × 1.5 cm strips and allowed to equilibrate over CaCl2 at room temperature for 7 days, then the mechanical properties were determined using Tensile Tester Machine (EZ-X, Shimadzu Co., Koyoto, Japan). Each strip was held between the two clamps of the machine and pulled at a specified rate of 5 mm/min. The force required for film breakage was recorded. Each measurement was done six times and the average determination was recorded. Tensile strength (TS) was computed by dividing the maximum load recorded at breakage by the sample cross-sectional area [32]. Percent elongation at breakage (% E) and elastic (Young’s) modulus (EM) were calculated as follows:
Where L0 and L are the length of the sample at the beginning of the experiment and its length at maximum elongation (mm), respectively. F is the maximum load at breakage (N), and A is the cross-sectional area of the film (mm2) [33], [34].
In-vitro dissolution
In vitro dissolution was performed for the prepared IDBFs using USP II dissolution test apparatus (DT 720 Series, Erweka GmbH, Germany) at 37 ± 0.5 °C and a rotation speed of 50 rpm. A strip measuring 1 × 3 cm (≡ 30 mg DPX) was placed in 900 mL phosphate buffer (pH 6.8). Specified aliquots were withdrawn at preset time intervals for a period of 45 min and replaced with equal volume of fresh buffer. The samples were filtered through Millipore filter (0.45 μm) and % DPX dissolved was quantified spectrophotometrically (UV-2600 PC; Shimadzu, Kyoto, Japan) at 292 nm. Each experiment is done in triplicate.
In-vivo mouth-dissolving time (MDT) and taste assessment
The palatability and the time needed for the films to dissolve completely in the buccal cavity were evaluated in six healthy human volunteers. Each volunteer administered three individual strips at a 0.5 h time intervals. The study was performed according to the ethical principles in the Declaration of Helsinki and followed the ICH GCP guidelines (Directive 75/318/EEC-1996). Every subject signed a written consent prior to starting the study. A strip of 3 cm2 was placed in the volunteers’ oral cavity and the time required for the films to completely dissolve was recorded. Moreover, all the participating subjects were instructed to assess the films according to taste, convenience of administration, and mouth feel using a scoring system as follows: 0 (highly satisfied), 1 (satisfied), and 2 (dissatisfied). Mouth feel and sensation was evaluated based on the residues remained in the buccal cavity following administration [32].
Effect of storage on the optimized DPX instantly dissolving buccal film
The selected IDBF (F4) was subjected accelerated storage conditions according to ICH guidelines. Individual strips were wrapped in aluminum foil and subjected to storage at 40 °C/ 75% RH for 3 months. Samples were re-evaluated for appearance, DPX content, mechanical properties, in vivo mouth dissolving time and in-vitro drug dissolution after 1 and 3 months [35]. Paired student t test was utilized to test the difference between the determined parameters before and after storage at P < 0.05.
Pharmacokinetic assessment of the optimized DPX instantly dissolving buccal film
Study design
In vivo performance of the selected DPX instantly dissolving buccal film, F4, was evaluated in male Wistar rats (n = 24), weighing ≈250 g each, compared to DPX oral market tablet Priligy® containing DPX dose of 30 mg [26]. The experiment design was approved by the Research Ethics Committee, Faculty of Pharmacy, King Abdulaziz University, KSA (Reference number PH-118-41). The committee confirms that animal use is in compliance with the Interdisciplinary Principles and Guidelines for the Use of Animals in Research, Testing, and Education issued by the New York Academy of Sciences [36]. Rats were fasted overnight (with free access to water) prior to administration of the treatment. They were divided equally between two groups (I&II). For group I, the optimized IDBF (1 × 3 cm2) containing 30 mg DPX were split into two halves (1 × 1.5 cm2) then the two parts were applied to the two sides of the buccal cavity. Before application, the rats were subjected to short-term anesthesia (3 min) with ether to ensure that the films were maintained in the mouth cavity without passing to the gastrointestinal tract. For group II, the oral market tablets were orally administered to the rats via gastric tubing. Blood specimens were withdrawn via the tail vein in a heparinized glass tubes at 0, 0.25, 0.5, 1, 2, 3, 4, 6, 8, 12, and 24 h after administration of either of the two treatments. Blood samples were centrifuged at 3000 rpm for 10 min, and the separated plasma was stored at −80 °C until analysis.
DPX assay in plasma
Modified method of Kim et al. [37] was adopted for the quantification of DPX concentration in rat plasma using liquid chromatography-tandem mass spectrometry with diode array detector (LC-MS/MS-DAD) analysis. An Agilent 6320 liquid chromatography-ion trap mass spectrometer (LC-IT-MS) was used for the detection of DPX. The MS system was connected to an HPLC system (Agilent 1200, Agilent Technologies, CA, USA) equipped with an autosampler and a quaternary pump. Separation was conducted on Agilent Eclipse XDB-C18 column (150 mm × 4.6 mm, 5 μ). The elution was performed using isocratic mobile phase comprising acetonitrile/0.1% formic acid mixture (80: 20, v/v) at a flow rate of 0.5 mL.min−1. Single positive molar ion mode was applied for detection of DPX (0–4.5 min, m/z 306.2) and the internal standard; valsartan (4.5–10 min, m/z 436.3). Calibration curve was constructed in the range of 1–1000 ng.mL−1.
Specified volume of each of the withdrawn plasma samples was transferred to screw-capped test tube, mixed with specified volume of acetonitrile and internal standard solution. The mixture was vortexed for 1 min, and then centrifuged at 5300 rpm for 7 min. An aliquot of the clear supernatant was transferred to a total recovery autosampler vial, and a specified volume was injected for LC-MS/MS-DAD analysis. Concentrations of DPX in the samples were computed based on the developed calibration curve.
Pharmacokinetic and Statistical analysis
Non compartmental analysis was applied using PK-SOLVER. Maximum plasma concentrations (Cmax, ng.mL−1) and their corresponding time (Tmax, h) were obtained from the individual plasma concentration versus time plots. The zero pharmacokinetic moment (AUC, ng. h.mL−1) was computed as the area under the plasma concentration versus time plot. Both Cmax and AUC were expressed as mean ± standard deviation, while Tmax was presented as median.
Statistical analysis was performed using Prism® (version 8.2.1, GraphPad Software Inc., La Jolla, CA, USA) at 95% level of significance. Two-way ANOVA followed by Sidak’s multiple comparisons test was applied to statistically analyze the determined plasma concentrations. The determined Cmax and AUC were statistically analyzed using unpaired t test with Welch’s correction, while Tmax was analyzed using the nonparametric Mann-Whitney U test (Wilcoxon rank sum test).
Results and discussion
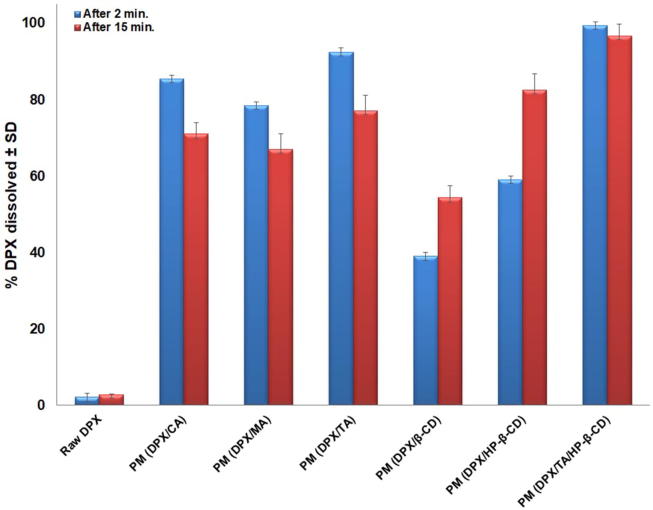
Screening of organic acids and cyclodextrins
DPX is characterized by pH dependent solubility that decreases as pH increases. It is reported that DPX has very low solubility in phosphate buffer pH 6.8 (0.26 µg.mL−1), and consequently poor and slow dissolution at salivary pH [26]. Thus, physical mixtures with different organic acids and cyclodextrins were investigated for DPX dissolution enhancement in phosphate buffer pH 6.8, Fig. 1. It was evident that in absence of excipients, the drug showed very slow dissolution with percent dissolved of 2.13 ± 0.09 and 2.89 ± 0.06% after 2 and 15 min, respectively.
Fig. 1.
Percent DPX dissolved from physical mixtures with organic acids and native cyclodextrins in comparison to raw DPX powder in phosphate buffer pH 6.8 at 37 ± 0.5 °C (Results are presented as mean ± SD, n = 3).
Enhanced dissolution was observed for all the physical mixtures compared to pure drug. Regarding organic acids, the enhancement could be explained on the basis of lowering the microenvironmental pH around DPX particles. The order of enhancing drug release was as follows: TA > CA > MA. This could be interpreted on the basis of pKa values and the acidity of the used pH modifiers. The pH modifiers with lower pka values have higher acidity, and consequently, they could have stronger modulation effect on the pH of the microenvironment around drug particles [10]. The observed order of dissolution enhancement agrees with the reported pKa values of the used pH modifiers, where TA has the lowest pKa values (2.98, 4.34), followed by CA (3.12, 4.76, 6.39) then malic acid (3.4, 5.13) [9], [16].
On the other hand, the enhancement in case of cyclodextrins could be credited to their surfactant-like characteristics that lowers the interfacial tension between DPX particles and the dissolution medium, thus promoting the wetting and dissolution of the poorly soluble drug [38], [39]. Moreover, the CDs rapid dissolution might result in local solubilizing action in the hydrodynamic layer surrounding drug particles in the early stages of the dissolution via the formation of drug-CD in situ inclusion complex [39]. It was observed that HP-β-CD had a greater impact on DPX dissolution compared to β-CD owing to its higher aqueous solubility and better wetting promoting effect.
It is worthy to note that although dissolution enhancement was more pronounced in case of organic acids compared to cyclodextrins after 2 min, an observed reduction in the percent dissolved was observed after 15 min. This could be attributed to the gradual rise in the pH of the drug particles microenvironment by the dilution effect of the buffered dissolution medium with consequent possible precipitation of DPX [26], [5]. Thus, in an attempt to benefit from both mechanisms of dissolution, physical mixture of the drug with both TA and HP-β-CD was prepared showing significant enhancement and maintenance of drug dissolution.
Design and preparation of DPX instantly dissolving buccal films (IDBFs)
The selection of the polymer(s) to be used in the films’ development and their amounts are crucial as they represent the main component in the formulation. Polymers are responsible for imparting adequate mechanical properties to the films, and they affect the film dissolution and/or disintegration within the buccal cavity, and consequently the liberation of the drug. MDXs are mixtures of poly- and oligo-saccharides produced by starch hydrolysis that vary in their dextrose equivalent value. In this study, MDX with relatively high DE value (16.5–19.5) was selected to yield films with high solubility and low viscosity [31]. In addition, HPMC E5 is previously reported as a film forming agent for fast dissolving films [35]. Accordingly, a mixture of HPMC E5 and MDX was chosen for film development aiming at combining the advantages of the film forming ability of HPMC and the enhanced dissolution property of MDX. The mixtures were investigated in the ratios 1:3, 1:1, and 3:1 according to the results of the preliminary trials (results provided as supplementary, S1).
Choosing the adequate plasticizer that is capable of imparting elasticity and good mechanical characteristics to buccal films is a crucial step in their development. The satisfactory performance of plasticizers containing hydroxyl groups with cellulose based polymers and their compatibility with MDX are previously reported [40], thus in this study, both glycerol and PG were investigated as plasticizers at a concentration range of 0 to 15%. The films prepared with propylene glycol showed appreciable flexibility at concentrations up to 5% compared to glycerin that resulted in stickier films. Concentrations of PG higher than 5% led to the formation of sticky films. The stickiness observed at higher concentrations could be credited to the oozing of excess plasticizer towards upper and lower surfaces of the film [2]; in addition, the hygroscopic nature of the plasticizer could also contribute to the observed stickiness. According to these results, PG was studied as a plasticizer in a concentration range of 1–5%. In addition, the range for the ratio of HPMC E5 (film former) to MDX (film modifier) was selected to be 1:3 to 3:1, w/w based on the physical characteristics of the preliminary films.
Based on the screening study, TA and HP-β-CD were selected to be incorporated in the prepared formulations as a pH modifier and hydrophilic solubilizer, respectively. The selected dissolution enhancing agents were incorporated at a 1:1:1 wt ratio (drug: TA: HP-β-CD) in all the prepared films.
Uniformity of dosage units
Mean weight and thickness of the films ranged from 65.43 ± 4.33 to 82.63 ± 7.13 mg and 0.24 ± 0.02 to 0.42 ± 0.05 mm, respectively, Table 3. The observed variability in the individual strips could be owing to the difference in ratios of HPMC E5 and MDX in the prepared films.
Table 3.
Characterization and equilibrium moisture uptake of dapoxetine hydrochloride instantly dissolving buccal films prepared according 32 full factorial design.
| Run | Weight& (mg) | Thickness$ (mm) | Drug content (%)& | Moisture uptake* (%)# |
|---|---|---|---|---|
| F1 | 76.81 ± 6.11 | 0.24 ± 0.02 | 96.21 ± 1.58 | 8.68 ± 0.56 |
| F2 | 78.12 ± 5.45 | 0.29 ± 0.04 | 98.33 ± 4.12 | 12.46 ± 0.98 |
| F3 | 65.15 ± 4.33 | 0.26 ± 0.04 | 106.27 ± 2.74 | 14.90 ± 1.21 |
| F4 | 68.34 ± 6.21 | 0.30 ± 0.11 | 104.73 ± 2.91 | 8.82 ± 0.87 |
| F5 | 82.43 ± 7.13 | 0.35 ± 0.07 | 97.12 ± 1.79 | 10.17 ± 0.91 |
| F6 | 75.32 ± 6.98 | 0.32 ± 0.06 | 102.34 ± 1.52 | 11.68 ± 1.34 |
| F7 | 68.12 ± 5.87 | 0.42 ± 0.05 | 94.56 ± 3.81 | 9.61 ± 1.12 |
| F8 | 65.43 ± 5.13 | 0.39 ± 0.04 | 101.41 ± 3.14 | 12.91 ± 0.94 |
| F9 | 66.98 ± 6.09 | 0.38 ± 0.02 | 96.47 ± 1.47 | 13.67 ± 1.29 |
Values are expressed as mean ± SD; $n = 6, &n = 10.
Equilibrium moisture uptake (after 3 days).
Regarding the content uniformity, all the prepared films complied with the compendial standards, i.e. within 90% to 110% with a relative standard deviation of ≤6% [30]. Mean DPX percent computed from six films of each formulation was in the range of 94.56 ± 3.81 to 106.79 ± 2.74. The relatively low standard deviations highlights the precision and the reproducibility of the casting method. In addition, the computed acceptance values were less than the Japanese Pharmacopeial (JP) accepted value of 15% (data provided as supplementary, S2) [30].
Moisture uptake
Adequate moisture percentage is required to protect the films against drying and brittleness on storage by the virtue of the plasticizing action of water. Moisture uptake studies revealed that all DPX films exhibited maximum moisture sorption after 3 days, after which no change or slight decrease in moisture uptake was recorded. The maximum moisture uptake ranged from 8.68 ± 0.56 to 14.90 ± 1.21%, Table 3. The moisture sorption could be credited to the presence of HPMC E5 and MDX with high DE value, where both polymers are reported to possess hygroscopic character. An overall pattern of increasing moisture sorption with increasing PG concentrations was also observed. This effect could be due to the increase in the polymers chains mobility by the virtue of insertion of the plasticizer between these chains, and consequently increasing their exposure to moisture absorption [31], [32].
Statistical analysis of the factorial design
Pointing out the formulation factors that might influence the drug delivery system characteristics is necessary. Factorial design has an advantage in this issue as they are able to analyze the impact of various factors synchronously. In this study, the factors and their corresponding levels were selected according to the preliminary trials as previously stated. For each response, the predicted R2 of the selected model reasonably agreed with the corresponding adjusted R2 (Table 4). In all responses, adequate precision with value greater than 4 confirmed that the selected model is appropriate for exploring the design space [41].
Table 4.
Output data of the analysis of 32 factorial design used for the formulation of DPX instantly dissolving buccal films.
| Response | Model | P-value | R2 | Adjusted R2 | Predicted R2 | Adequate precision | Significant factors and interactions |
|---|---|---|---|---|---|---|---|
| Y1: TS (MPa) | 2FI | 0.0026 | 0.9295 | 0.8873 | 0.7176 | 12.5912 | X1, X2, X1X2 |
| Y2: % E (%) | 2FI | 0.0013 | 0.9471 | 0.9154 | 0.7514 | 15.6532 | X1, X2, X1X2 |
| Y3: EM (MPa) | 2FI | 0.0287 | 0.813 | 0.7008 | 0.5006 | 7.8320 | X1, X1X2 |
| Y4: % D5min (%) | Linear | 0.0006 | 0.9144 | 0.8859 | 0.8652 | 15.1142 | X1, X2 |
| Y5: In vivo MDT (sec) | Linear | 0.0006 | 0.9173 | 0.8897 | 0.8424 | 14.7436 | X1, X2 |
TS; Tensile strength, % E; Percent elongation at break, EM; Elastic (Young’s modulus), % D5min; Percent drug dissolved after 5 min, MDT; In vivo mouth dissolving time
Effect of variables on mechanical properties
Adequate mechanical properties are essential for the successful development of the films and their ease of handling by the patients [42]. In this study, tensile strength (TS, Y1), percent elongation at break (%E, Y2) and elastic modulus (EM, Y3) were evaluated as indices for film’ brittleness, elasticity (ductility), and stiffness, respectively [43]. The results are compiled in Table 2.
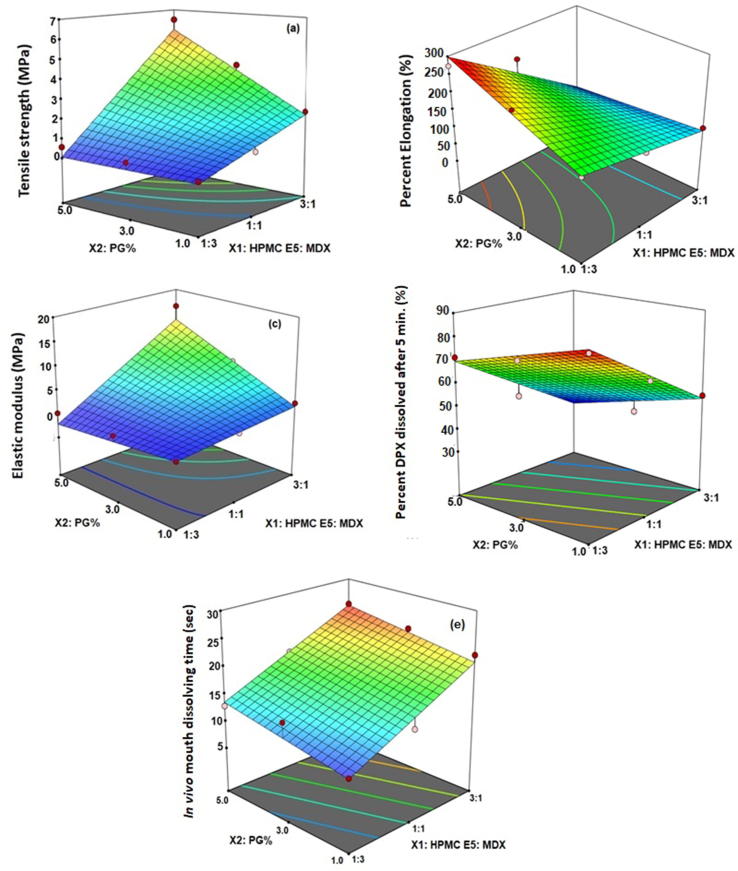
The response 3D-surface plots showing the influence of HPMC E5: MDX ratio (X1) and PG % (X2) on the films’ mechanical properties are shown in Fig. 2(a-c). The sequential model relating each of the three responses to the explored variables was suggested to be 2-factor interaction (2FI) indicating the significance of the main effects and the interactions between variables, Table 4. F-values of 21.99, 29.86, and 7.25 for Y1, Y2, and Y3, respectively confirms the significance of the model. The equations representing the selected sequential model for each response in terms of coded factors were computed as follows:
Fig. 2.
Response 3D surface plot for the effect of HPMC E5: MDX ratio (X1) and PG % (X2) on the (a) tensile strength (Y1), (b) percentage elongation (Y2) at break, (c) elastic modulus (Y3), percent DPX dissolved after 5 min (Y4), and in vivo mouth dissolving time of DPX instantly-dissolving buccal films.
ANOVA revealed that the HPMC E5: MDX ratio has significant effect on all the studied mechanical properties (P = 0.0010, 0.0005, and 0.0170 for TS, %E, and EM, respectively), while PG% exhibits a significant effect on both TS and %E (P = 0.0196 and 0.0295, respectively). In addition, the interaction between both factors was statistically significant on the three responses (P = 0.0365, 0.0127, and 0.0456 for TS, %E, and EM, respectively); detailed analysis is provided in supplementary S3, S4, and S5.
Fig. 2 illustrates that increasing HPMC: MDX ratio led to significant increase in TS and EM accompanied by marked decrease in %E and vice-versa. This results agrees with previous work that reported hard and brittle nature for films made with HPMC alone. On the other hand, the simultaneous increase in MDX (with high DE value) concentration with decreasing HPMC concentration could result in higher flexibility and ductility to the films [31], [44].
In contrast, increasing PG % was accompanied by significant reduction in the TS and increase in the %E of the prepared films. This could be explained on the basis of the plasticizing action of PG. Plasticizers are reported to embed themselves among the polymer chains, and thus, cause the disruption of polymer chains interaction leading to increase in their mobility [31]. This action is expected to impart increased ductility and decreased stiffness for the films with increasing plasticizer concentration [32], [42].
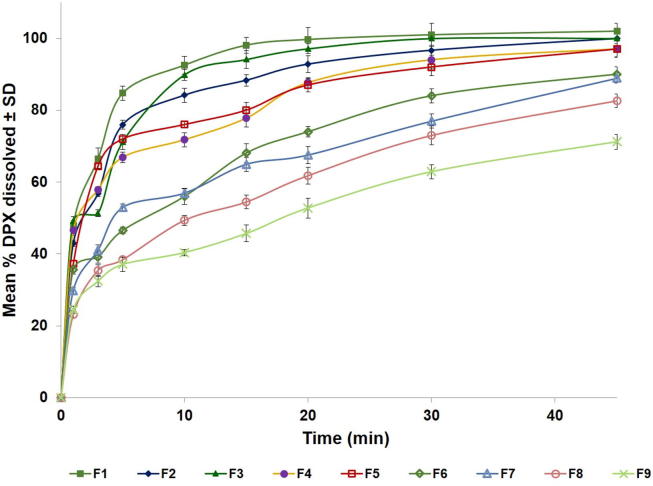
Effect of variables on in vitro dissolution
In-vitro dissolution profiles of DPX instantly dissolving buccal films in phosphate buffer pH 6.8 exhibited remarkable differences among formulations as depicted in Fig. 3. Percent drug dissolved after 5 min ranged from 37.08 ± 2.13 to 84.76 ± 3.98%. For further evaluation for the source of this variation, statistical analysis for percent DPX dissolved after 5 min was performed using ANOVA. F-value of 32.06 affirms the significance of the model, where there is only a 0.06% chance that this value could be large due to noise. Fig. 2d illustrates the response 3D-surface plot of the effect of HPMC E5: MDX (X1) and PG % (X2) on the percentage DPX dissolved after 5 min (D5min, Y4). The suggested sequential model was the linear model indicating the significance of the main effects only. The mathematical equation that relates percent DPX dissolved after 5 min to the studied factors in terms of coded factors was computed as follows:
Fig. 3.
In vitro dissolution profiles of DPX instantly-dissolving buccal films in phosphate buffer pH 6.8 at 37 ± 0.5 °C (Results are presented as mean ± SD, n = 3).
ANOVA revealed that both HPMC E5: MDX and PG% had significant impact of on DPX dissolution from the films (P = 0.0004 and 0.0133, respectively). The effect of polymers ratio on drug dissolution was more pronounced than that of plasticizer concentration as evident by the lower P-value and the higher coefficient of X1 compared to X2 (detailed analysis is provided in supplementary S6). Fig. 2d shows that D5min significantly decreases with increasing both HPMC E5: MDX ratio and PG %. The effect of polymers ratio could be explained on the basis of varying concentrations of both HPMC E5 and MDX simultaneously. At higher HPMC levels, viscous gel layer formation surrounding drug particles due to the closer contact of the polymer chains could result in reduced mobility of the drug within the formed gel layer, and consequently reduced dissolution rate [45]. Similar effect for increasing HPMC concentration was previously reported by Abdelbary et al. [35]. On the other hand, increasing MDX resulted in increased drug dissolution owing to its high aqueous solubility that contributes to enhancing DPX dissolution from the prepared films [31].
Effect of variables on in-vivo mouth-dissolving time (MDT) and palatability studies
All the prepared formulations showed short dissolving time in the saliva of less than 30 s, however, marked variations of MDT were observed among formulations ranging from 9.67 ± 0.56 to 25.12 ± 2.12 s, Table 2. The effects of HPMC E5: MDX (X1) and PG % (X2) on the in-vivo MDT (Y5) is displayed in the response 3D-surface plot, Fig. 2e. The suggested sequential model was linear rather than 2FI indicating the insignificance of the interaction between polymers ratio and PG % on MDT. F-value of 33.26 affirms the significance of the model indicating there is only a 0.06% chance that this value could be large owing to noise. The linear equation depicting the relation between in and vivo MDT (Y5) and the investigated variables was computed as:
Statistical treatment of the data using ANOVA showed a significant influence for both polymers ratio and PG % on in vivo MDT (P = 0.0003 and 0.0335, respectively). The impact of polymers ratio was more obvious than that of plasticizer concentration as evident by the lower P-value and the higher coefficient of X1 compared to X2 (detailed analysis is provided in supplementary S7). It was evident that MDT increases with increasing HPMC E5: MDX. This could be ascribed to viscous gel layer formation upon contacting saliva at higher HPMC concentration with consequent hindrance of further fluids penetration and retardation of the films’ dissolution in the oral cavity. Similar effect for increasing HPMC concentration on the films’ disintegration time was reported in previous studies [35], [46]. In addition, the increase in MDX concentration at lower HPMC E5: MDX ratios could contribute to decreasing the MDT by the virtue of the high aqueous solubility of MDX that could facilitate the fluid penetration into the films [31], [32]. Furthermore, the observed significant decreased MDT with increasing plasticizer concentration has been previously reported and was related to the reduced tensile strength of the films [44], [47].
Regarding the in-vivo palatability study, all the formulations showed satisfactory results for with a score ranging from 0 (highly satisfied) to 1 (satisfied) for the taste and a score of 0 (highly satisfied) for the convenience of administration and mouth feel. Although PG is reported to have a bitter taste, all the films were satisfactory with respect to taste owing to the added sweetener, saccharin, and the flavoring agent, orange oil. In addition, the presence of MDX might contribute to improving the films’ palatability due to its sweetening action [2], [32]. The satisfactory results with respect to mouth feel of all films assures complete and rapid dissolution in the mouth.
Selection of the optimized DPX instantly dissolving buccal film
Desirability function was applied for selection of the optimized DPX instantly dissolving buccal film from the prepared films according to the 32 factorial design. The criteria set for selection were attaining maximum flexibility and in vitro dissolution, in addition to minimum in vivo mouth dissolving duration as presented in Table 1. It was found that DPX film F4 prepared at a ratio of 1:1, w/w HPMC E5: MDX and 1% PG fulfilled the required criteria with a desirability value of 0.802. Thus this formulation was selected for further stability studies and in vivo assessment. It is worthy to note that although the formulation F1-F3 prepared at a ratio of 1:3, w/w HPMC E5: MDX exhibited better desirability values, yet, they were excluded from further investigations due to their high stickiness that could result from the relatively low concentration of the film former HPMC E5.
Effect of storage on the optimized DPX IDBF
Upon storage of the selected DPX film, F4, at the specified conditions, the stored films showed no appreciable changes in the physical appearance or characteristics. The results are compiled in Table 5. Paired student t test revealed no significant difference between the parameters of the fresh films and the stored ones at P < 0.05.
Table 5.
Effect of storage on the characteristics of the selected optimized DPX instantly dissolving buccal film (F4) at 40 °C/75% RH for 3 months.
| Fresh Films | After 1 month | After 3 months | |
|---|---|---|---|
| Weight& (mg) | 68.34 ± 6.21 | 69.11 ± 4.65 | 70.14 ± 5.87 |
| Thickness$ (mm) | 0.30 ± 0.11 | 0.31 ± 0.14 | 0.31 ± 0.37 |
| Drug content (%)& | 104.73 ± 2.91 | 99.43 ± 4.11 | 98.32 ± 2.89 |
| TS $ (MPa) | 0.811 ± 0.077 | 0.823 ± 0.091 | 0.834 ± 0.106 |
| % E $ (%) | 115.34 ± 1.56 | 113.45 ± 1.59 | 112.67 ± 2.21 |
| EM $ (MPa) | 0.703 ± 0.065 | 0.725 ± 0.073 | 0.740 ± 0.098 |
| D5 min# (%) | 66.91 ± 2.45 | 65.14 ± 3.27 | 64.99 ± 3.19 |
| MDT$ (sec) | 13.15 ± 1.77 | 13.99 ± 2.11 | 14.65 ± 1.98 |
TS; Tensile strength, % E; Percent elongation at break, EM; Elastic (Young’s) modulus, % D5min; Percent drug dissolved after 5 min, In vivo MDT; In vivo mouth dissolving time
*Values are expressed as mean ± SD; # n = 3, $n = 6, &n = 10.
In addition, there was also no significant change in the dissolution profile in phosphate buffer pH 6.8 (data not shown) as evidenced by the computed similarity factor f2 between the fresh and the stored films’ dissolution profiles [48]. The computed f2 values of 69.04 and 62.52 after 1 and 3 months, respectively, could indicate adequate relative stability of the formulations.
Pharmacokinetic assessment of the optimized DPX instantly dissolving buccal film
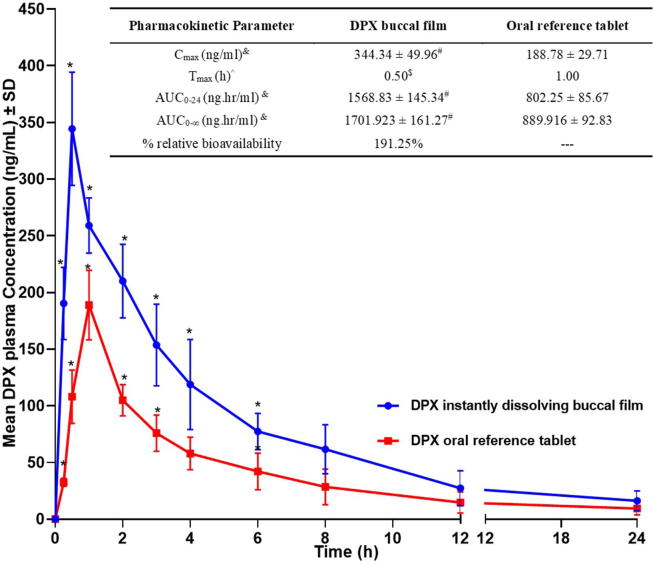
The relationship between DPX concentrations spiked in plasma and peak area ratios (DPX/IS) showed good linearity with determination coefficient (R2) of 0.9984. The assay showed acceptable intra- and inter-day precision with CV% of <9% and <13%, respectively. The assay accuracy was also acceptable with % relative error ranging from 3.38 to 12.89%. Mean DPX concentrations in rats’ plasma versus time following buccal administration of the optimized DPX IDBF (F4) compared to oral reference product are graphically plotted in Fig. 4.
Fig. 4.
Mean DPX plasma concentration versus time following buccal administration of optimized instantly dissolving film compared to oral reference tablet in rats and computed in vivo pharmacokinetic parameters (Inset table). &Data represent the mean value ± standard deviation (SD), n = 12. ^ Data represent the median, n = 12 * Significant at P < 0.05, test of significance using Two-way ANOVA, Sidak's multiple comparisons test # Significant at p < 0.05, test of significance using unpaired t test (two-tailed) with Welch’s correction $ Significant at p < 0.05, test of significance using Mann-Whitney test.
Compared to the oral reference tablet, the optimized DPX film demonstrated a significantly higher Cmax and AUC (P = 0.0125 and 0.0231, respectively) and a relative bioavailability of 191.25%, Fig. 4 (Inset table). The significant enhanced absorption of DPX following buccal administration of the optimized IDBF could be credited to the dual solubilizing action of both the pH modifier (TA) and the hydrophilic solubilizer (HP-β-CD) that was previously discussed under section 3.1. In addition, avoiding the hepatic first pass effect of the drug via the buccal route could significantly contribute to increasing the drug’s absorption. In addition, the film demonstrated a significantly shorter Tmax (P = 0.0317) than the oral market tablets that could be explained on the basis of rapid dissolution of the film in the oral cavity with consequent rapid absorption via the highly vascular oral mucosa.
Based on these results, the optimized DPX instantly dissolving buccal film could be considered a promising delivery system for the drug, with expected enhanced bioavailability and improved patient compliance.
Conclusion
Being a patient-friendly substitute, the pharmaceutical industry is mostly switching many of their buccal products to the dissolvable oral films. Thus, objective of this work was to improve the bioavailability of DPX hydrochloride via the formulation of instantly dissolving buccal film with dual mechanism for enhancement of drug dissolution (the use of both acidic pH modifier and hydrophilic cyclodextrin). TA and HP-β-CD were selected for the drug solubilization based on the screening study. 32 full factorial design was successfully applied for the development and optimization of the films. The film prepared utilizing HPMC E5: MDX (1:1, w/w) and 1% PG was selected as the optimum film based on the desirability function. The selected film showed satisfactory physical and mechanical properties, high in-vivo dissolution, and rapid in vivo mouth dissolution. In addition, it exhibits significantly higher and more rapid drug absorption compared to the oral reference product in rats. Therefore, the selected formulation could be a promising delivery system for the drug with expected enhanced patient compliance and improved bioavailability owing to drug dissolution enhancement and avoidance of first pass effect.
Compliance with Ethics requirements
All Institutional and National Guidelines for the care and use of animals (fisheries) were followed.
Funding Source
Deanship of Scientific Research (DSR), King Abdulaziz University, Jeddah, Saudia Arabia.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This project was funded by the Deanship of Scientific Research (DSR), King Abdulaziz University, Jeddah, under grant No. (G-392-249-38). The authors, therefore, gratefully acknowledge DSR technical and financial support.
Footnotes
Peer review under responsibility of Cairo University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jare.2020.04.019.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Kathpalia H., Gupte A. An introduction to fast dissolving oral thin film drug delivery systems: a review. Curr Drug Deliv. 2013;10:667–684. doi: 10.2174/156720181006131125150249. [DOI] [PubMed] [Google Scholar]
- 2.Fahmy R.H., Badr-Eldin S.M. Novel delivery approach for ketotifen fumarate: Dissofilms formulation using 32 experimental design: In vitro/in vivo evaluation. Pharm Dev Technol. 2014:19. doi: 10.3109/10837450.2013.800108. [DOI] [PubMed] [Google Scholar]
- 3.Hosny K.M., El-Say K.M., Ahmed O.A. Optimized sildenafil citrate fast orodissolvable film: A promising formula for overcoming the barriers hindering erectile dysfunction treatment. Drug Deliv. 2016;23:355–361. doi: 10.3109/10717544.2014.916763. [DOI] [PubMed] [Google Scholar]
- 4.Shimoda H., Taniguchi K., Nishimura M., Matsuura K., Tsukioka T., Yamashita H. Preparation of a fast dissolving oral thin film containing dexamethasone: a possible application to antiemesis during cancer chemotherapy. Eur J Pharm Biopharm. 2009;73:361–365. doi: 10.1016/j.ejpb.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 5.Senta-Loys Z., Bourgeois S., Valour J.P., Briançon S., Fessi H. Orodispersible films based on amorphous solid dispersions of tetrabenazine. Int J Pharm. 2017;518:242–252. doi: 10.1016/j.ijpharm.2016.12.036. [DOI] [PubMed] [Google Scholar]
- 6.Dixit R.P., Nagarsenker M.S. Self-nanoemulsifying granules of ezetimibe: design, optimization and evaluation. Eur J Pharm Sci. 2008;35:183–192. doi: 10.1016/j.ejps.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 7.Badr-Eldin S.M., Ahmed T.A., Ismail H.R. Aripiprazole-cyclodextrin binary systems for dissolution enhancement: Effect of preparation technique, cyclodextrin type and molar ratio. Iran J Basic. Med Sci. 2013:16. [PMC free article] [PubMed] [Google Scholar]
- 8.Kwon H., Heo E.-J., Kim Y.-H., Kim S., Hwang Y.-H., Byun J.-M. Development and evaluation of poorly water-soluble celecoxib as solid dispersions containing nonionic surfactants using fluidized-bed granulation. Pharmaceutics. 2019;11:136. doi: 10.3390/pharmaceutics11030136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adachi M., Hinatsu Y., Kusamori K., Katsumi H., Sakane T., Nakatani M. Improved dissolution and absorption of ketoconazole in the presence of organic acids as pH-modifiers. Eur J Pharm Sci. 2015;76:225–230. doi: 10.1016/j.ejps.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Kojo Y., Matsunaga S., Suzuki H., Taniguchi C., Kawabata Y., Wada K. Improved dissolution of dipyridamole with the combination of ph-modifier and solid dispersion technology. Chem Pharm Bull Pharm Bull. 2017;65:426–431. doi: 10.1248/cpb.c16-00714. [DOI] [PubMed] [Google Scholar]
- 11.Onoue S., Inoue R., Taniguchi C., Kawabata Y., Yamashita K., Wada K. Improved dissolution and pharmacokinetic behavior of dipyridamole formulation with microenvironmental pH-modifier under hypochlorhydria. Int J Pharm. 2012;426:61–66. doi: 10.1016/j.ijpharm.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 12.Bi M., Kyad A., Alvarez-Nunez F., Alvarez F. Enhancing and sustaining AMG 009 dissolution from a bilayer oral solid dosage form via microenvironmental pH modulation and supersaturation. AAPS PharmSciTech. 2011;12:1401–1406. doi: 10.1208/s12249-011-9710-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bassi P., Kaur G. pH modulation: a mechanism to obtain pH-independent drug release. Expert Opin Drug Deliv. 2010;7:845–857. doi: 10.1517/17425247.2010.491508. [DOI] [PubMed] [Google Scholar]
- 14.Taniguchi C., Kawabata Y., Wada K., Yamada S., Onoue S. Microenvironmental pH-modification to improve dissolution behavior and oral absorption for drugs with pH-dependent solubility. Expert Opin Drug Deliv. 2014;11:505–516. doi: 10.1517/17425247.2014.881798. [DOI] [PubMed] [Google Scholar]
- 15.Ploen J., Andersch J., Heschel M., Leopold C.S. Citric acid as a pH-modifying additive in an extended release pellet formulation containing a weakly basic drug. Drug Dev Ind Pharm. 2009;35:1210–1218. doi: 10.1080/03639040902882256. [DOI] [PubMed] [Google Scholar]
- 16.Choi J.S., Kwon S.H., Lee S.E., Jang W.S., Byeon J.C., Jeong H.M. Use of acidifier and solubilizer in tadalafil solid dispersion to enhance the in vitro dissolution and oral bioavailability in rats. Int J Pharm. 2017;526:77–87. doi: 10.1016/j.ijpharm.2017.04.056. [DOI] [PubMed] [Google Scholar]
- 17.Singh S., Parikh T., Sandhu H.K., Shah N.H., Malick A.W., Singhal D. Supersolubilization and amorphization of a model basic drug, haloperidol, by interaction with weak acids. Pharm Res. 2013;30:1561–1573. doi: 10.1007/s11095-013-0994-7. [DOI] [PubMed] [Google Scholar]
- 18.Shah A., Serajuddin A.T.M. Conversion of solid dispersion prepared by acid-base interaction into free-flowing and tabletable powder by using Neusilin® US2. Int J Pharm. 2015;484:172–180. doi: 10.1016/j.ijpharm.2015.02.060. [DOI] [PubMed] [Google Scholar]
- 19.Parikh T., Sandhu H.K., Talele T.T., Serajuddin A.T.M. Characterization of solid dispersion of itraconazole prepared by solubilization in concentrated aqueous solutions of weak organic acids and drying. Pharm Res. 2016;33:1456–1471. doi: 10.1007/s11095-016-1890-8. [DOI] [PubMed] [Google Scholar]
- 20.Loftsson T., Duchêne D. Cyclodextrins and their pharmaceutical applications. Int J Pharm. 2007;329:1–11. doi: 10.1016/j.ijpharm.2006.10.044. [DOI] [PubMed] [Google Scholar]
- 21.Sharma N., Baldi A. Exploring versatile applications of cyclodextrins: an overview. Drug Deliv. 2014:1–19. doi: 10.3109/10717544.2014.938839. [DOI] [PubMed] [Google Scholar]
- 22.Russo A., Capogrosso P., Ventimiglia E., La Croce G., Boeri L., Montorsi F. Efficacy and safety of dapoxetine in treatment of premature ejaculation: An evidence-based review. Int J Clin Pract. 2016;70:723–733. doi: 10.1111/ijcp.12843. [DOI] [PubMed] [Google Scholar]
- 23.Waldinger M.D. Drug treatment options for premature ejaculation. Expert Opin Pharmacother. 2018;19:1077–1085. doi: 10.1080/14656566.2018.1494725. [DOI] [PubMed] [Google Scholar]
- 24.McMahon C.G. Dapoxetine: a new option in the medical management of premature ejaculation. Ther Adv Urol. 2012;4:233–251. doi: 10.1177/1756287212453866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersson K.E., Mulhall J.P., Wyllie M.G. Pharmacokinetic and pharmacodynamic features of dapoxetine, a novel drug for “on-demand” treatment of premature ejaculation. BJU Int. 2006;97:311–315. doi: 10.1111/j.1464-410X.2006.05911.x. [DOI] [PubMed] [Google Scholar]
- 26.Fouad S.A., Shamma R.N., Basalious E.B., El-Nabarawi M.A., Tayel S.A. Novel instantly-soluble transmucosal matrix (ISTM) using dual mechanism solubilizer for sublingual and nasal delivery of dapoxetine hydrochloride: In-vitro/in-vivo evaluation. Int J Pharm. 2016;505:212–222. doi: 10.1016/j.ijpharm.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 27.Fouad S.A., Shamma R.N., Basalious E.B., El-Nabarawi M.M., Tayel S.A. Novel instantly-dispersible nanocarrier powder system (IDNPs) for intranasal delivery of dapoxetine hydrochloride: in-vitro optimization, ex-vivo permeation studies, and in-vivo evaluation. Drug Dev Ind Pharm. 2018;44:1443–1450. doi: 10.1080/03639045.2018.1459675. [DOI] [PubMed] [Google Scholar]
- 28.Bin Liew K., Peh K.K. Investigation on the effect of polymer and starch on the tablet properties of lyophilized orally disintegrating tablet. Arch Pharm Res. 2015 doi: 10.1007/s12272-014-0542-y. [DOI] [PubMed] [Google Scholar]
- 29.El-Refai K., Teaima M.H., El-Nabarawi M.A. Dual-purpose vardenafil hydrochloride/dapoxetine hydrochloride orodispersible tablets: in vitro formulation/evaluation, stability study and in vivo comparative pharmacokinetic study in healthy human subjects. Drug Dev Ind Pharm. 2018;44:988–1000. doi: 10.1080/03639045.2018.1427761. [DOI] [PubMed] [Google Scholar]
- 30.USP 41-NF36. 〈905〉 Uniformity of Dosage Units. United States Pharmacop. Natl. Formul., Rockville, MD: The united States Pharmacopeial Convention, United Book Press, Inc.; 2018, p. 6637.
- 31.ElMeshad A.N., El Hagrasy A.S. Characterization and optimization of orodispersible mosapride film formulations. AAPS PharmSciTech. 2011;12:1384–1392. doi: 10.1208/s12249-011-9713-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cilurzo F., Cupone I.E., Minghetti P., Selmin F., Montanari L. Fast dissolving films made of maltodextrins. Eur J Pharm Biopharm. 2008;70:895–900. doi: 10.1016/j.ejpb.2008.06.032. [DOI] [PubMed] [Google Scholar]
- 33.Fahmy R.H., Badr-Eldin S.M. Novel delivery approach for ketotifen fumarate: dissofilms formulation using 32 experimental design: in vitro/in vivo evaluation. Pharm Dev Technol. 2014;19:521–530. doi: 10.3109/10837450.2013.800108. [DOI] [PubMed] [Google Scholar]
- 34.Li-Li X, ALi-Li S, Qing-Ri C, Wei-Juan X, Yue C, Xiao-Yin Z, et al. Formulation and in vitro characterization of novel sildenafil citrateloaded polyvinyl alcohol-polyethylene glycol graft copolymer-based orally dissolving films. Int J Pharm 2014;473:398–406. [DOI] [PubMed]
- 35.Abdelbary A., Bendas E.R., Ramadan A.A., Mostafa D.A. Pharmaceutical and pharmacokinetic evaluation of a novel fast dissolving film formulation of flupentixol dihydrochloride. AAPS PharmSciTech. 2014;15:1603–1610. doi: 10.1208/s12249-014-0186-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.New York Academy of Sciences. Interdisciplinary principles and guidelines for the use of animals in research, testing, and education. A report of the Ad Hoc Committee on Animal Research., New York: New York Academy of Sciences.; 1988.
- 37.Kim T.K., Kim I.S., Hong S.H., Choi Y.K., Kim H., Yoo H.H. Determination of dapoxetine in rat plasma by ultra-performance liquid chromatography–tandem mass spectrometry. J Chromatogr B. 2013;926:42–46. doi: 10.1016/j.jchromb.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 38.Moyano J.R., Ginés J.M., Arias M.J., Rabasco A.M. Study of the dissolution characteristics of oxazepam via complexation with β-cyclodextrin. Int J Pharm. 1995;114:95–102. doi: 10.1016/0378-5173(94)00220-Y. [DOI] [Google Scholar]
- 39.Badr-Eldin S.M., Elkheshen S.A., Ghorab M.M. Inclusion complexes of tadalafil with natural and chemically modified β-cyclodextrins. I: Preparation and in-vitro evaluation. Eur J Pharm Biopharm. 2008:70. doi: 10.1016/j.ejpb.2008.06.024. [DOI] [PubMed] [Google Scholar]
- 40.Dixit R.P., Puthli S.P. Oral strip technology: Overview and future potential. J Control Release. 2009;139:94–107. doi: 10.1016/j.jconrel.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 41.Al-Mahallawi A.M., Abdelbary A.A., Aburahma M.H. Investigating the potential of employing bilosomes as a novel vesicular carrier for transdermal delivery of tenoxicam. Int J Pharm. 2015;485:329–340. doi: 10.1016/j.ijpharm.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 42.Jantrawut P., Chaiwarit T., Jantanasakulwong K., Brachais C.H., Chambin O. Effect of plasticizer type on tensile property and in vitro indomethacin release of thin films based on low-methoxyl pectin. Polymers (Basel) 2017:9. doi: 10.3390/polym9070289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Batista P., Castro P., Madureira A.R., Sarmento B., Pintado M. Development and characterization of chitosan microparticles-in-films for buccal delivery of bioactive peptides. Pharmaceuticals. 2019;12:1–15. doi: 10.3390/ph12010032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bin Liew K, Tan Y.T.F., Peh K.-K. Effect of polymer, plasticizer and filler on orally disintegrating film. Drug Dev Ind Pharm. 2014;40:110–119. doi: 10.3109/03639045.2012.749889. [DOI] [PubMed] [Google Scholar]
- 45.Jadhav Y.G., Galgatte U.C., Chaudhari P.D. Overcoming poor solubility of dimenhydrinate: Development, optimization and evaluation of fast dissolving oral film. Adv Pharm Bull. 2018;8:721–725. doi: 10.15171/apb.2018.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dangre P.V., Phad R.D., Surana S.J., Chalikwar S.S. Quality by design (QbD) assisted fabrication of fast dissolving buccal film for clonidine hydrochloride: Exploring the quality attributes. Adv Polym Technol. 2019;2019. doi: 10.1155/2019/3682402. [DOI] [Google Scholar]
- 47.Bala R., Sharma S. Formulation optimization and evaluation of fast dissolving film of aprepitant by using design of experiment. Bull Fac Pharmacy, Cairo Univ. 2018;56:159–168. doi: 10.1016/j.bfopcu.2018.04.002. [DOI] [Google Scholar]
- 48.Costa P., Sousa Lobo J.M. Modeling and comparison of dissolution profiles. Eur J Pharm Sci. 2001;13:123–133. doi: 10.1016/S0928-0987(01)00095-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.