Abstract
Background: Activities of daily living (ADL), which are divided into basic (BADL) and instrumental (IADL), allows us to survive and to live in the society. Cognitive skills are a key aspect in BADL outcomes. After reviewing existing BADL tools for Spanish schoolchildren, issues such as not covering the full age range or not having a BADL-centred vision were found. We aim to develop a new tool for BADL assessment in Spanish schoolchildren. Methods: The new tool was administered to 375 participants (47.2% boys and 52.8% girls) from 6 to 12 years of age. Analyses were carried out to find out the structure (semiconfirmatory factor analysis) and internal consistency (ordinal alpha) of BADL. Results: Four scales formed the instrument (Eating, Personal Hygiene, Getting Dressed, and General Functioning) with an interpretable solution of 12 factors (Manual Dexterity, Proprioception, Oral Sensitivity, Good Manners, Hygiene and Grooming, Toileting Needs Communication, Bladder and Bowel Control, Showering, Independent Dressing Tasks, Full Dressing, Executive Functions, and Self-Regulation) with 84 items + 6 qualitative items for girls. The reliability values obtained were acceptable (.70–.88). Conclusions: The tool seems to be a practical and reliable instrument to assess BADL and cognitive skills during BADL in Spanish schoolchildren.
Keywords: activities of daily living, executive function, emotional regulation, assessment, child
1. Introduction
Activities of daily living (ADL) are a set of activities performed by humans both for survival and for living in the society [1]. Depending on their objectives, complexity, and level of privacy, ADL are divided into basic ADL (BADL) or instrumental ADL (IADL). On the one hand, BADL include care activities for basic needs, are considered to be universal, and require minimal cognitive effort, like bathing, toileting and personal hygiene, dressing, feeding, functional mobility, taking care of own devices, and sexual activity. On the other hand, IADL refer to activities for home management or taking care of others, depend on the culture, and require a more considerable cognitive effort [2,3], such as communication management, community mobility, taking care of others, health maintenance, money, shopping, home management, and involvement in spiritual activities [1,4,5]. Humans learn ADL throughout their whole life, but childhood and early adolescence are critical periods. Good performance of these activities is essential to be functional, to develop an independent and self-determined life, and for social inclusion [6,7,8,9,10,11]. Under the occupational therapy (OT) practitioners’ view, BADL are one of the human occupations. Occupations, Client Factors, Performance Skills, Performance Patterns, Context and Environment interact with each other and with the person, so all of them are critical topics for OT [1], as shown in Table 1.
Table 1.
Aspects of the domain of occupational therapy [1].
| Occupations | Client Factors | Performance Skills | Performance Patterns | Context and Environment |
|---|---|---|---|---|
| Basic ADL Instrumental ADL Rest and sleep Education Work Play Leisure Social participation |
Values, beliefs, and spirituality Body functions Body structures |
Motor Process Social interaction |
Habits Routines Rituals Roles |
Cultural Personal Physical Social Temporal Virtual |
ADL: activities of daily living.
Within the Performance Skills group, some neurobiological processes are relevant for ADL performance [12,13]: executive function (EF) and self-regulation (SR). EF belongs to the group of cognitive processes related to behavior, including acceptably solving internal and external problems [14,15], and plays an essential role in facing new situations [16]. EF should include three main domains: updating/working memory (keeping online relevant information during a task), inhibition (stopping predominant thoughts or actions), and flexibility (being able to change one’s perspective) [17,18]. Proper EF functioning is necessary for adaptive ADL performance [19,20,21], as we continually plan and sequence, solve problems [22,23], keep organized and focused during daily activities. SR refers to being able to manage thoughts, attention, feelings, responses related to stimuli [24] and behaviors to enable goal-directed actions [25]. SR is necessary for successful adaptation to the environment, including the performance of occupations such as eating, dressing, bathing, sleeping, and learning [26]. Some of the EF processes support SR, so EF should be a necessary but not sufficient condition for good SR performance [27,28].
Clinical intervention in OT includes assessment, planning, and treatment. With regards to evaluation, sometimes OT practitioners use tools from other disciplines. This is not a problem itself, except if theoretical bases of the tool can implicate results of the occupational diagnosis [29,30]. If we compare ADL and adaptive behavior concepts, then we can see that they are not the same: ADL refer to people’s daily self-care activities, come from the OT field, and include BADL and IADL. Adaptive behavior comes from psychology and intellectual disability, and it is defined as appropriate behaviors that people perform to live independently, including some or other domains depending on the author [3]. So it should be reasonable to ask ourselves if using an adaptive behavior assessment we obtain the information that we are searching for ADL. Although a wide range of instruments to measure BADL performance in Spanish schoolchildren exists, we have found some issues that can influence the final occupational diagnosis: some of them are translated into Spanish, but no cultural adaptation information was found (e.g., Vineland Adaptive Behavior Scales II and PEDI-CAT); others measure daily skills, but are focused on early childhood (e.g., Portage Guide to Early Education, Merrill–Palmer-Revised Scales of Development, and Battelle Developmental Inventory), not covering the full school age range; and last, most of the tools come from an adaptive behavior point of view, not from an ADL-centered perspective (see Table 2).
Table 2.
Summary of BADL and adaptative behavior measurements for Spanish children.
| Tool | Spanish Translated/ Validated |
Full 6–12 Years Age Range | BADL-Centered Assessment |
|---|---|---|---|
| Adaptive Behavior Assessment System II – ABAS II [31,32] | yes/yes | yes | no |
| Checklist of Adaptive Living Skills – CALS [33,34] | yes/yes | yes | no |
| Inventory for Client and Agency Planning – ICAP [35,36] | yes/yes | yes | no |
| Vineland Adaptive Behavior Scales II – VABS II [37] | yes/no | yes | no |
| Pediatric Evaluation of Disability Inventory—Computer Adaptive Test – PEDI-CAT [38] | yes/no | yes | yes |
| Supports Intensity Scale – SIS [39,40] | yes/yes | yes | no |
| Battelle Developmental Inventory – BDI [41,42] | yes/yes | no | no |
| Merrill–Palmer-Revised Scales of Development – MP-R [43,44] |
yes/yes | no | no |
| Portage Guide to Early Education [45,46] | yes/yes | no | no |
BADLs: basic activities of daily living.
To the best of our knowledge, a comprehensive tool to evaluate a full range of BADL is needed, especially to help OT practitioners in their clinical interventions. It is not our intention to develop a diagnostic measurement, but to describe as broadly as possible the performance of the pediatric population in BADL. We also aim to obtain screening information about the cognitive processes that influence BADL. The study aims to present a new tool to evaluate BADL performance in Spanish schoolchildren from 6 to 12 years of age showing its psychometric properties.
2. Materials and Methods
2.1. Participants
Inclusion criteria were being from 6 to 12 years old with typical development and providing a written informed consent form signed by legal guardians to the investigators. 375 schoolchildren of both genders participated in the study (177 boys, 47.2%, and 198 girls, 52.8%). Their age ranged from 6 to 12 years old (M = 8.5 years, SD = 2.1 for the total; M = 8.4 years, SD = 2 for boys; and M = 8.6 years, SD = 2.1 for girls). A probabilistic polietapic sample design was used, recruited through regular schools and sporting events in the community of Extremadura (Spain).
2.2. Instruments
The material used was the Activities of Daily Living Evaluation in Schoolchildren (ADL-E), a new tool created for Spanish schoolchildren, which covers a wide range of BADL. The instrument is made up of 4 different scales: 3 for measuring BADL (Eating, Personal Hygiene, and Getting Dressed) and 1 scale for cognitive aspects that influence BADL performance. The final version has 84 items + 6 qualitative items for girls (Table 3).
Table 3.
Qualitative ADL-E items for girls on the Personal Hygiene scale.
| 1. She can do hairstyles with bobby pins, make pigtails, etc. |
| 2. She understands what menstruation is. |
| 3. She knows how to apply a pad. |
| 4. The pad is changed at an appropriate frequency, without too many accidents. |
| 5. She leaves used pads inside containers. |
| 6. She washes her hands after changing the pad. |
| ADL-E: Activities of Daily Living Evaluation in Schoolchildren. |
The Eating scale has 20 items. Aspects related to choosing, manipulating, chewing food, or drinks and keeping good manners during mealtime are explored. The Personal Hygiene scale is composed of 29 items. They help to obtain information about grooming, washing, brushing, showering, toileting, using supplies and cosmetics, and bladder and bowel control. Within this scale, 6 extra qualitative items about hairstyle and menstruation management for girls were included. The Getting Dressed scale has 19 items and explores aspects about choosing and adjusting clothes and accessories, and the dressing and undressing sequence, including shoes. The General Functioning scale has 18 items, which provide information about cognitive aspects related to EF and SR.
The ADL-E must be completed by conducting a family–therapist interview with caregivers, which must provide answers based on the behaviors they observe in their children. Each item must be answered by marking one of the four response options (Table 4). Therapists should obtain evidence/s that parents’ answers are as detailed as possible, so blank spaces for observations are provided.
Table 4.
Activities of Daily Living Evaluation in Schoolchildren (ADL-E) response options.
| Response Options | Explanation |
|---|---|
| Always | The child can perform the task/activity independently. It always happens. |
| Sometimes | The child is learning to do the task/activity. The child needs help (visual, verbal, or physical) from an adult. It happens sometimes. |
| Never | The child cannot perform the task/activity. An adult does the essential parts of the activity’s tasks. It never happens. |
| Not known; no opportunity | The informant cannot answer. The child has never faced that situation. |
2.3. Procedure
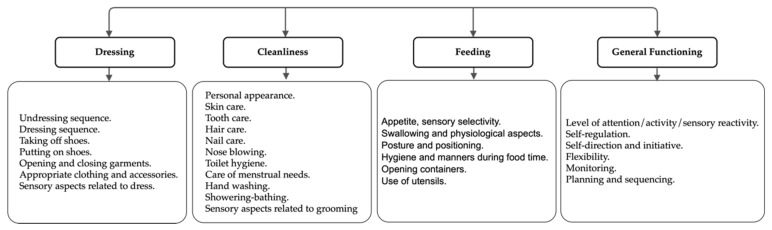
After reviewing available instruments, it was decided to create a new one which meets several conditions: being culturally adapted, suitable for schoolchildren (6–12 years), and with an ADL-centered perspective. Cognitive items that influence occupational performance were added to help OT practitioners in their clinical intervention or recommending a thorough evaluation of dysfunction suspicion. A group of experts in the fields of psychology and OT created a preliminary version using the OT practice framework [1] and their clinical experience as the baseline (Figure 1).
Figure 1.
Initial categorization of the items.
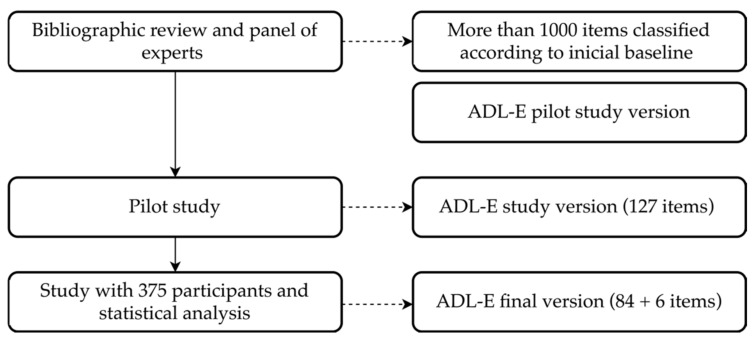
A pilot study was carried out with 15 families obtaining the version used for this study. Once administered to the sample, the items were analyzed by the group of experts, discarding those which did not fit on the theoretical model. This process resulted in the final version of the ADL-E as shown in Figure 2. This protocol adhered to the updates of the Declaration of Helsinki [47], and it was approved by the Committee on Biomedical Ethics of the University of Extremadura (198/2019).
Figure 2.
Activities of Daily Living Evaluation in Schoolchildren (ADL-E) creation procedure.
2.4. Statistics
Microsoft OfficeTM Excel v.16, FACTOR v.10.10.02, and IBMTM SPSS v.25 were used for data analysis. An exploratory factor analysis (EFA) was carried out to find out the internal structure of every scale and to check the factorial weights of every item. Before the EFA, the two necessary conditions were verified: adjustment of the data to the normal curve and adequate sample adjustment indicators through the Kaiser–Meyer–Olkin (KMO) and Bartlett’s sphericity tests [48,49].
Due to the ordinal nature of the data, the EFA was used for the calculation of polychoric correlations using the robust unweighted least squares method (RULS) for the extraction of factors with oblique rotation because we started from the premise that factors were correlated. Items with factorial weights < .30 were maintained, and those with lower values were deleted [50]. This procedure, carried out with FACTOR, also allowed us to explore the goodness-of-fit data for each of the factor solutions [51,52]. This semiconfirmatory factor analysis of the items (SCFA) is suitable to prevent errors such as the ones of the “Little Jiffy” approach in psychometry [53,54,55].
To evaluate the goodness-of-fit of the model, the following were used: a) the chi-squared probability taking as appropriate non-significant values (p > .05); b) the comparative fit index (CFI) and the non-normed fit index (NNFI) considering > .90 as an indicator of good fit; c) the root mean square error of approximation (RMSEA), considering values < .06 acceptable; and e) the root mean square of residuals (RMSR) considering values < .05 acceptable [49,56]. Thus, the study of the EFA and the matrix of correlations between the factors together with the bibliographic review provided elements of judgment for the establishment of a theoretical model of relationships between the different scales and their factors.
To find out the internal consistency of the ADL-E, the ordinal alpha was used, which is an alternative to the Cronbach’s Alpha more accurate with Likert scale responses, including ordinal items. Preferred values are between < .80 and >.90, but .70 is considered acceptable [57,58].
3. Results
After performing the analyses, the items from the ADL-E were reduced from 124 (study version) to 84 + 6 qualitative items in the final version. The 4 scales are easily explained by a conceptual model with 12 factors. Each scale with its factors is explained below.
3.1. Eating Scale
The Eating scale aims to obtain information about choosing, manipulating, chewing food, or drinks, keeping good manners, and other aspects during mealtime. We found an interpretable solution with 4 factors (Table 5): Manual Dexterity (6 items), Proprioception (4 items), Oral Sensitivity (3 items), and Good Manners (7 items). The Manual Dexterity factor consists of the items related to the use of tools to open or manipulate food and drinks with manual or bimanual coordination requirements. The items in Proprioception are about the correct application of strength to manage food, drinks, or containers. In the Oral Sensitivity factor, the items are about sensory processing of food. The Good Manners during Mealtime factor groups items into several categories: cognitive, attentional, executive, sensory, motor, behavioral, and cultural ones. For example, a child who cannot stay seated during mealtime can have inhibition issues (executive), postural problems (sensory or motor), or he/she may not be interested in food (behavioral). Despite this, we named it Good Manners, because they all are considered correct behaviors in our society.
Table 5.
Eating scale factorial solution.
| Item Number | Item | Factorial Weight |
|---|---|---|
| Factor 1: Manual Dexterity while Eating. | ||
| 19 | He/she uses tools to open containers (e.g., a can opener). | 0.393 |
| 24 | He/she uses a knife to spread. | 0.780 |
| 25 | He/she uses a knife to cut food. | 0.927 |
| 26 | He/she uses several cutleries at the same time in a coordinated way (e.g., a knife and a fork). | 0.860 |
| 27 | He/she can serve food from a bowl or tray. | 0.770 |
| 28 | He/she chooses the right cutlery. | 0.447 |
| Factor 2: Proprioception. | ||
| 11 | He/she licks foods like ice cream or candy. | 0.383 |
| 16 | He/she opens containers with pressure plugs. | 0.545 |
| 17 | He/she unscrews screw caps. | 0.800 |
| 21 | He/she sips on a straw. | 0.302 |
| Factor 3: Oral Sensitivity. | ||
| 3 | He/she is reluctant to try new foods. | 0.825 |
| 4 | He/she is unwilling to eat food with certain textures (purees, crunchy...). | 0.875 |
| 5 | He/she shows disgust when certain foods are within his/her mouth. | 0.744 |
| Factor 4: Good Manners during Mealtime. | ||
| 2 | He/she only puts edible substances into his/her mouth. | 0.331 |
| 7 | He/she tests the food carefully to check its temperature. | 0.470 |
| 9 | He/she chews with his/her mouth closed. | 0.543 |
| 12 | He/she maintains a proper posture during mealtime. | 0.795 |
| 13 | He/she keeps seated at the table during mealtime. | 0.727 |
| 14 | He/she uses napkins properly. | 0.628 |
| 15 | He/she tries to maintain good manners during mealtime. | 0.848 |
For the KMO test, a value of .71, and for the Bartlett’s test, p <.0.001 were found, both considered good to perform the EFA. Initially, this scale was formed by 28 items, but 8 items did not reach the weight of < .30, so they were not kept (Table 6). Thus, a total of 20 items form this scale in the final version of the instrument.
Table 6.
Deleted items from the Eating scale.
| Item Number | Item |
|---|---|
| 1 | He/she asks for food or water when hungry or thirsty. |
| 6 | If necessary, he/she collaborates, taking his/her medication. |
| 8 | He/she drinks liquids without spilling from the glass or the bottle. |
| 10 | He/she chews food until crushed before swallowing. |
| 18 | He/she can open wrappers. |
| 20 | He/she can eat pieces of food with his/her hands. |
| 22 | He/she can use a spoon without spilling food. |
| 23 | He/she can prick food with a fork. |
3.2. Personal Hygiene Scale
The Personal Hygiene scale aims to obtain information about taking care of oneself. We found an interpretable solution with 4 factors (Table 7): Hygiene and Grooming (18 items), Toileting Needs Communication (2 items), Bladder and Bowel Control (4 items), and Showering (5 items). In the Hygiene and Grooming factor, information about hair, skin, and nail care, use of cosmetics, nose-blowing, washing hands, brushing teeth, and toilet management, but also about keeping everything clean and caring about having a good appearance is grouped. Factors 2 and 3 are about Bladder and Bowel Control: the first one is about being able to communicate toilet needs, and the second one is about being aware of these needs. Factor 4 contains all the items related to showering/bathing.
Table 7.
Personal Hygiene scale factorial solution.
| Item Number | Item | Factorial Weight |
|---|---|---|
| Factor 1: Hygiene and Grooming. | ||
| 7 | In the bathroom, he/she acceptably get clean with toilet paper. | 0.381 |
| 9 | When he/she is done using the toilet, he/she lowers the lid and pulls the chain. | 0.469 |
| 10 | He/she washes his/her hands after using the toilet. | 0.541 |
| 11 | In the bathroom, he/she cares about his/her privacy. | 0.493 |
| 12 | He/she collaborates using cologne or moisturizer. | 0.448 |
| 13 | He/she keeps his/her nails clean. | 0.662 |
| 14 | He/she brushes his/her hair. | 0.460 |
| 16 | He/she checks his/her appearance before leaving home. | 0.418 |
| 17 | He/she brushes his teeth after eating without being told by an adult. | 0.638 |
| 19 | He/she brushes most or all areas of his/her mouth. | 0.636 |
| 20 | He/she spits into the wash when brushing his/her teeth. | 0.835 |
| 21 | After brushing his/her teeth, he/she checks there are no traces of paste left in his/her mouth or face. | 0.591 |
| 22 | He/she leaves the sink clean and picks up everything after brushing. | 0.506 |
| 24 | He/she is aware when he/she needs to wipe his/her nose. | 0.590 |
| 25 | He/she can blow his nose. | 0.494 |
| 26 | He/she can adjust the water pressure. | 0.492 |
| 28 | When washing his/her hands, soap and water are given to full hands. | 0.602 |
| 29 | When washing his/her hands, he/she uses an adequate amount of soap. | 0.523 |
| Factor 2: Toileting Needs Communication. | ||
| 5 | He/she communicates his/her need to go to the bathroom. | 0.508 |
| 6 | He/she warns an adult when he/she has had an accident (peed or pooped). | 0.777 |
| Factor 3: Bladder and Bowel Control. | ||
| 1 | Usually, he/she stays poopless at night. | 0.673 |
| 2 | Usually, he/she stays dry at night, without peeing. | 0.600 |
| 3 | He/she keeps clean during the day, without pooping him/herself. | 0.723 |
| 4 | He/she keeps dry during the day, without peeing him/herself. | 0.927 |
| Factor 4: Showering. | ||
| 32 | In the shower, he/she soaps up all over the body. | 0.920 |
| 33 | In the shower, he/she rinses until all foam is removed. | 0.850 |
| 34 | In the shower, he/she lathers and rinses his/her intimate parts carefully. | 0.846 |
| 35 | In the shower, he/she uses the towel until he/she is relatively dry. | 0.564 |
| 36 | In the shower, he/she lathers his/her hair in an acceptable way. | 0.780 |
For the KMO test, a value of .921, and for the Bartlett’s test, p <.0.001 were found, both considered good to perform the EFA. Initially, this scale was formed by 42 items, but 7 items did not reach the weight of < .30, so they were not kept (Table 8). The 6 qualitative items for girls were not included in the EFA. Thus, a total of 29 + 6 items forms this scale in the final version of the instrument.
Table 8.
Deleted items from the Personal Hygiene scale.
| Item Number | Item |
|---|---|
| 8 | He/she can lower or raise his/her clothes to use the toilet. |
| 18 | He/she brushes for at least one minute. |
| 23 | He/she is stressed while brushing teeth. |
| 27 | He/she can check and adjust the water temperature. |
| 30 | When he/she washes his/her hands, he/she wipes himself/herself completely dry. |
| 31 | He/she can wash his/her face. |
| 37 | He/she is stressed when nails or hair are cut. |
3.3. Getting Dressed Scale
The Getting Dressed scale aims to obtain information about dressing tasks. We found an interpretable solution with 2 factors (Table 9): Independent Dressing Tasks (13 items) and Full Dressing (4 items). In the Independent Dressing Tasks factor, all the items are related to specific and individual tasks needed for dressing (accessories, zippers). These can be tasks with essential cognitive functions (choosing and taking care of clothes) or about manual dexterity and praxis (fastening and adjusting clothes and accessories). In the Full Dressing factor, the items are about the complete activity of getting dressed or undressed.
Table 9.
Getting Dressed scale factorial solution.
| Item Number | Item | Factorial Weight |
|---|---|---|
| Factor 1: Independent Dressing Tasks. | ||
| 4 | He/she can choose his/her clothing and accessories depending on the weather conditions. | 0.580 |
| 5 | He/she makes sure that the label of the clothes is in the right place. | 0.601 |
| 6 | He/she distinguishes when his/her clothes are clean or dirty. | 0.491 |
| 8 | He/she can put his/her socks properly. | 0.739 |
| 14 | He/she undresses completely, including using zippers on garments. | 0.447 |
| 15 | He/she takes off his/her clothes, leaving them on the right side (label inside). | 0.468 |
| 16 | He/she can put on a coat or an open garment. | 0.360 |
| 20 | He/she puts on accessories (e.g., gloves, scarf, hat, etc.). | 0.518 |
| 22 | He/she clasps snap buttons (click type). | 0.718 |
| 24 | He/she can zip clothes up. | 0.601 |
| 26 | He/she opens buttons. | 0.775 |
| 27 | He/she can undo his/her shoes’ lacing. | 0.807 |
| 28 | He/she can tie a knot in his/her shoes. | 0.715 |
| Factor 2: Full Dressing. | ||
| 17 | He/she can put on stretching pants. | 0.856 |
| 18 | He/she can put on a T-shirt or an upper garment. | 0.840 |
| 19 | He/she can get dressed without help (not including closures). | 0.738 |
| 30 | He/she can get dressed without help (including closures and accessories). | 0.520 |
For the KMO test, a value of .92, and for the Bartlett’s test, p < .0.001 were found, both considered good to perform the EFA. Initially, this scale was formed by 30 items, but 13 items did not reach the weight of < .30, so they were not kept (Table 10). Thus, a total of 17 items form this scale in the final version of the instrument.
Table 10.
Deleted items from the Getting Dressed scale.
| Item Number | Item |
|---|---|
| 1 | Labels or certain fabrics bother him/her. |
| 2 | He/she does not seem to notice that garments are misplaced. |
| 3 | He/she always wants to wear the same clothing. |
| 7 | He/she can remove socks. |
| 9 | He/she can put footwear on his/her feet. |
| 10 | He/she places a shoe on the right foot. |
| 11 | He/she can remove shoes without fasteners. |
| 12 | He/she can remove shoes with fasteners. |
| 13 | He/she can remove simple garments without closures (pants, underwear). |
| 21 | He/she opens and closes Velcro fasteners. |
| 23 | He/she can zip up and down. |
| 25 | He/she can unbutton. |
| 29 | He/she can tie his/her shoes. |
3.4. General Functioning Scale
The General Functioning scale aims to obtain information about the cognitive aspects that can influence BADL performance. We found an interpretable solution with 2 factors (Table 11): Executive Function (8 items) and Self-Regulation (10 items). The Executive Function factor contains several subprocesses related to planning, sequencing, keeping focused on the task, time control, and solving problems. In the Self-Regulation factor, all the items are about self-control and being able to manage thoughts, attention, feelings, and responses related to stimuli.
Table 11.
General Functioning scale factorial solution.
| Item Number | Item | Factorial Weight |
|---|---|---|
| Factor 1: Executive Function. | ||
| 2 | He/she begins his/her activities of daily life in a reasonable time from the adult’s direction. | 0.540 |
| 3 | In general, he/she can perform his/her activities of daily living without the help of an adult. | 0.556 |
| 6 | He/she persists in their activities of daily life although he/she finds difficulties (e.g., while he is cutting a steak). | 0.519 |
| 10 | He/she finishes his/her activities of daily living at an appropriate time, not too early, not too late (e.g., washing hands). | 0.599 |
| 11 | He/she becomes aware of the mistakes he/she makes in his/her daily life activities (e.g., if the lacing of his/her shoe gets loose). | 0.523 |
| 12 | He/she tries to solve problems while performing an activity (e.g., he/she knows what to do if the toothpaste is over). | 0.649 |
| 13 | He/she can perform his/her daily activities without unnecessary stops. | 0.662 |
| 15 | He/she performs his/her daily activities in a logical order (e.g., putting on the underwear before a garment). | 0.688 |
| Factor 2: Self-Regulation. | ||
| 4 | He/she gets frustrated quickly when he/she cannot perform some of his/her daily activities. | 0.363 |
| 5 | He/she has more tantrums than expected for a child of his/her age. | 0.502 |
| 7 | He/she finds it difficult to get adapted to changes in the environment. | 0.769 |
| 8 | It is difficult for him/her to assimilate changes in his/her routine. | 0.801 |
| 9 | It is difficult for him/her to stop performing one activity to move on to another, especially if he/she enjoys the activity he/she is doing. | 0.526 |
| 14 | He/she has difficulties performing activities of daily living with two or more steps (e.g., brushing teeth or getting fully dressed). | 0.581 |
| 16 | He/she often leaves his/her activities of daily living unfinished (e.g., when he/she dries his/her hands, they remain wet). | 0.591 |
| 17 | He/she loses his/her attention performing his/her daily activities if there is any external noise. | 0.598 |
| 18 | Sometimes he/she spins or rocks excessively, which makes it difficult to perform his/her daily activities. | 0.595 |
| 19 | He/she does not perform his/her activities of daily life properly due to excessive movement. | 0.545 |
For the KMO test, a value of .65, and for the Bartlett’s test, p < .0.001 were found, both considered good to perform the EFA. Initially, this scale was formed by 19 items, but 1 item, "Asks for help when necessary in his/her daily life activities", did not reach < .30, so it was not kept.
3.5. Correlations Between Factors
Correlations between factors were also explored, as showed in Table 12 [59].
Table 12.
Correlations between factors.
| Eat-F1 | Eat-F2 | Eat-F3 | Ea-F4 | PH-F1 | PH-F2 | PH-F3 | PH-F4 | Dre-F1 | Dre-F2 | GF-F1 | GF-F2 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eat-F1 | 1 | |||||||||||
| Eat-F2 | −0.43 ** | 1 | ||||||||||
| Eat-F3 | 0.05 | −0.17 ** | 1 | |||||||||
| Eat-F4 | −0.42 ** | 0.40 ** | −0.08 | 1 | ||||||||
| PH-F1 | −0.55 ** | 0.40 ** | −0.07 | 0.58 ** | 1 | |||||||
| PH-F2 | 0.03 | 0.06 | 0.09 | −0.01 | −0.02 | 1 | ||||||
| PH-F3 | −0.07 | 0.06 | −0.10 * | 0.02 | 0.04 | 0.02 | 1 | |||||
| PH-F4 | 0.46 ** | −0.35 ** | 0.01 | −0.37 ** | −0.61 ** | −0.06 | −0.03 | 1 | ||||
| Dre-F1 | −0.61 ** | 0.44 ** | −0.11 * | 0.44 ** | 0.60 ** | 0.03 | 0.09 | −0.48 ** | 1 | |||
| Dre-F2 | −0.15 ** | 0.10 * | −0.14 ** | 0.07 | 0.06 | −0.08 | 0.27 ** | −0.15 ** | 0.25 ** | 1 | ||
| GF-F1 | 0.18 ** | −0.17 ** | 0.24 ** | −0.33 ** | −0.32 ** | 0.08 | −0.06 | 0.19 * | −0.23 ** | 0.08 | 1 | |
| GF-F2 | −0.45 ** | 0.36 ** | −0.17 ** | 0.61 ** | 0.59 ** | 0.03 | 0.02 | −0.38 ** | 0.55 ** | 0.11 * | −0.36 ** | 1 |
* Correlation is significant at the 0.05 level (2-tailed). ** Correlation is significant at the 0.01 level (2-tailed). Eat-F1: Eating scale—factor 1; PH-F1: Personal Hygiene scale—factor 1; Dre-F1: Getting Dressed scale—factor 1; GF-F1: General Functioning scale—factor 1. The same is applied to factors 2, 3, and 4.
High correlations were found between Dre-F1/ Eat-F1, GF-F2/ Ea-F4, PH-F4/PH-F1, Dre-F1/ PH-F1, and GF-F2/ PH-F1. Moderate correlations were also found between Eat-F2/Eat-F1, Eat-F4/Eat-F1, PH-F1/Eat-F1, PH-F4/Eat-F1, GF2/ Eat-F1, Eat-F4/Eat-F2, PH-F1/ Eat-F2, Dre-F1/Eat-F2, PH-F1/Eat-F4, Dre-F1/Eat-F4, Dre-F1/ PH-F4, and GF-F2/Dre-F1.
3.6. Goodness-of-Fit Indices
As mentioned previously, the FACTOR software explores the goodness-of-fit data (see Table 13). All the indices are acceptable [49,56].
Table 13.
ADL-E goodness-of-fit indices.
| ADL-E scales | Results | Cutoff |
|---|---|---|
| Eating scale | ||
| p (χ2) | p = 0.18 | > 0.05 |
| CFI | 0.99 | > 0.90 |
| NNFI | 0.99 | > 0.90 |
| RMSEA | 0.03 | < 0.06 |
| RMSR | 0.05 | < 0.08 |
| Personal Hygiene scale | ||
| p (χ2) | p = 0.01 | > 0.05 |
| CFI | 0.99 | > 0.90 |
| NNFI | 0.99 | > 0.90 |
| RMSEA | 0.02 | < 0.06 |
| RMSR | 0.06 | < 0.08 |
| Getting Dressed scale | ||
| p (χ2) | p = 0.24 | > 0.05 |
| CFI | 0.98 | > 0.90 |
| NNFI | 0.99 | > 0.90 |
| RMSEA | 0.05 | < 0.06 |
| RMSR | 0.08 | < 0.08 |
| General Functioning scale | ||
| p (χ2) | p = 0.00 | > 0.05 |
| CFI | 0.98 | > 0.90 |
| NNFI | 0.99 | > 0.90 |
| RMSEA | 0.04 | < 0.06 |
| RMSR | 0.07 | < 0.08 |
p (χ2): chi-squared probability; CFI: comparative fit index; NNFI: non-normed fit index, RMSEA: root mean square error of approximation; RMSR: root mean square of residuals.
3.7. Reliability
To find out the internal consistency of the ADL-E, ordinal alpha was used (Table 14). As mentioned previously, the preferred values are < .80 and > .90, but < .70 is considered acceptable.
Table 14.
Internal consistency of the ADL-E.
| ADL-E Factors | α |
|---|---|
| Eating scale | |
| Manual Dexterity while Eating. | 0.85 |
| Proprioception. | 0.70 |
| Oral Sensitivity. | 0.85 |
| Good Manners during Mealtime. | 0.81 |
| Personal Hygiene scale | |
| Hygiene and Grooming. | 0.85 |
| Toileting Needs Communication. | 0.70 |
| Bladder and Bowel Control. | 0.85 |
| Showering. | 0.81 |
| Getting Dressed scale | |
| Independent Dressing Tasks. | 0.88 |
| Full Dressing. | 0.82 |
| General Functioning scale | |
| Executive Function | 0.81 |
| Self-Regulation | 0.84 |
4. Discussion
Our main contribution is to present a new tool to assess BADL performance in Spanish schoolchildren. To our knowledge, no valid and reliable tool that covers the complete school age range and is BADL-centered to capture the occupational performance exists. Finally, 4 scales form the ADL-E: Eating, Personal Hygiene, Getting Dressed + General Functioning. A total of 12 factors offer a conceptual model we think is relevant: the Eating scale is formed by 4 factors: Manual Dexterity while Eating (6 items), Proprioception (4 items), Oral Sensitivity (3 items), and Good Manners (7 items); the Personal Hygiene scale is formed by 4 factors: Hygiene and Grooming (18 items), Toileting Needs Communication (2 items), Bladder and Bowel Control (4 items), and Showering (5 items); the Getting Dressed scale is formed by 2 factors: Independent Dressing Tasks (13 items) and Full Dressing (4 items); and the General Functioning scale is formed by 2 factors: Executive Function (8 items) and Self-Regulation (10 items). This structure is different and more accurate than the one presented by other instruments: for example, Adaptive Behavior Assessment System II (ABAS II) groups all the BADL items in a single section called Self-Care; the Inventory for Client and Agency Planning (ICAP) joins all the BADL items in the Personal Life Skills section; Vineland Adaptive Behavior Scales II (VABS II)—in the Daily Living Skills Domain—Personal; the Merrill–Palmer-Revised Scales of Development (MP-R)—in Adaptive Behavior and Self-Care, and the Portage Guide to Early Education—in the Self-Care section. More specific, but not BADL-centered, are the Battelle Developmental Inventory (BDI) with the following sections in the Adaptive Scale: Attention, Mealtime, Getting Dressed, Personal Responsibility, and Hygiene; and the CALS, with Socialization, Mealtime, Hygiene and Grooming, Toileting, Getting Dressed, Health Care (this is an IADL), and Sexuality. The Computer Adaptive Test (PEDI-CAT), which is the closest to the ADL-E, is formed by 4 domains: Daily Activities (including BADL and IADL), Mobility, Social/Cognitive, and Responsibility, but it is not culturally validated in Spain.
Related to correlations between factors, several facts need to be considered. Manual Dexterity in the Eating factor has a strong correlation with the Independent Dressing Tasks factor, which can be explained by the critical motor requirements of that kind of tasks/activities. Good Manners during Mealtime and Self-Regulation also have a strong correlation, which also can be explained by the need to inhibit and manage behaviors to keep seated following cultural customs. The Hygiene and Grooming factor also has a high correlation with Showering (some of the steps in hygiene are common in showering), Independent Dressing Tasks (also requires developed motor skills) and the Self-Regulation factor (high demand of self-control while performing these tasks). The ADL-E shows good psychometric properties, both in validity and reliability (internal consistency).
Continuing with the ADL-E structure and exploring the number of items, the final number is 84 + 6 qualitative items for girls, so the time to complete the interview should be 45–90 minutes, which can be reasonable and accessible for OT practitioners and other professionals. Some of the reviewed tools have a much lower number of items, so perhaps they do not provide enough information (e.g., the ICAP with 21 items, ABAS II with 24, or the Vineland with 41), and others had a much higher number, so maybe the professionals have not got the time to properly administer them (e.g., the CALS with 814 items). The ADL-E can be a useful tool to help therapists to make clinical decisions. As mentioned previously, OT practitioners need assessments to help them to characterize the BADL performance, because it is one of the most demanded interventions within their scope. The ADL-E can also be useful for educational professionals and families to have a reference about the right acquisition of BADL abilities by their students or children.
This research had some limitations. The sample was recruited in the community of Extremadura. We tried to establish a development trajectory for the BADL considered universal, but maybe social and cultural differences in this kind of activities should be more deeply checked. Another important aspect is that the information is completed through caregivers. Although instruments completed by families are considered to be valid tools [60], some authors warn us to be careful, because parents could overestimate or underestimate development of their children [61,62]. We also need to improve concurrent validity using well-established tools.
Concerning future lines of research, we have several appreciations to do. In the occupational therapy, tools to measure BADL are necessary. For physically disabled children, we have specific tools to assess the issues they usually have with their ADL: for example, the Pediatric Evaluation of Disability Inventory (PEDI) [63], or the Functional Independence Measure for Children (WeeFIM) [64], which are very focused on physical problems with mobility BADL. So, an important future line should be using the ADL-E with specific populations with cognitive disorders or impairments, because to the best of our knowledge, there is blank space in this area. For example, children diagnosed with neurodevelopmental disorders suffering from alterations or delays in the development of functions related to the maturation of the central nervous system that causes difficulties to adapt to the environment [65] should be an interesting group to explore. Within this group, autism spectrum disorders (ASD), intellectual disability (ID), attention deficit and hyperactivity disorders (ADHD), motor disorders, specific learning disorder, communication disorders, etc. are included. Some authors have found differences in ADL profiles between these populations: worse performance in ASD children in hygiene or dressing than in the ID population [66] or worse performance in dressing, personal hygiene, and eating skills, including postural control and fine motor skills, in children with developmental coordination disorder compared with normally developed children [11], so it should be interesting to try to find specific BADL profiles.
5. Conclusions
The ADL-E is a practical and easy-to-apply tool which assesses BADL (Eating, Personal Hygiene, and Getting Dressed) in Spanish schoolchildren aged 6–12. The ADL-E also offers monitoring of the influence of EF and SR during these activities, showing good psychometric properties in both validity and reliability.
Acknowledgments
We want to thank all the participants who kindly dedicated their time to help us in this research.
Author Contributions
Conceptualization, S.B.-F., M.G., D.R.-A.; Methodology, A.G.-G., M.Á.H.-M.; Software, A.G.-G., M.Á.H.-M.; Formal analysis, A.G.-G., M.Á.H.-M.; Writing—original draft preparation, S.B.-F.; Writing—review and editing, S.B.-F., M.G., D.R.-A.; Visualization, S.B.-F.; Supervision, S.B.-F., M.G., A.G.-G., D.R.-A., M.Á.H.-M.; Funding acquisition, S.B.-F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially funded by Colegio Profesional de Terapeutas Ocupacionales de Extremadura (COPTOEX).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.American Occupational Therapy Association Occupational therapy practice framework: Domain and process 3a ed. Am. J. Occup. Ther. 2014;68:S1–S48. doi: 10.5014/ajot.2014.682006. [DOI] [Google Scholar]
- 2.Moruno Miralles P., Romero Ayuso D.M. Actividades de la Vida Diaria. Masson; Madrid, Spain: 2006. [Google Scholar]
- 3.Romero D.M. Actividades de la vida diaria. An. Psicol. 2007;23:264–271. [Google Scholar]
- 4.American Occupational Therapy Association Occupational Therapy Practice Framework: Domain and Process. Am. J. Occup. Ther. 2002;56:609–639. [PubMed] [Google Scholar]
- 5.American Occupational Therapy Association Occupational Therapy Practice Framework: Domain and process 2nd Edition. Am. J. Occup. Ther. 2008;62:625–683. doi: 10.5014/ajot.62.6.625. [DOI] [PubMed] [Google Scholar]
- 6.Jefatura del Estado . Ley 39/2006, de 14 de diciembre, de Promoción de la Autonomía Personal y Atención a las Personas en Situación de Dependencia. Boletín Oficial del Estado; Madrid, Spain: 2006. [Google Scholar]
- 7.Schalock R.L., Verdugo M.A. Quality of Life for Human Service Practitioners. American Association on Mental Retardation; Washington, DC, USA: 2003. [Google Scholar]
- 8.Organización Mundial de la Salud . Clasificación Internacional del Funcionamiento de la Discapacidad y de la Salud. Organización Mundial de la Salud; Geneva, Switzerland: 2001. [Google Scholar]
- 9.Gantschnig B.E., Fisher A.G., Page J., Meichtry A., Nilsson I. Differences in activities of daily living (ADL) abilities of children across world regions: A validity study of the assessment of motor and process skills: ADL differences in children across world regions. Child Care Health Dev. 2015;41:230–238. doi: 10.1111/cch.12170. [DOI] [PubMed] [Google Scholar]
- 10.Günal A., Bumin G., Huri M. The Effects of Motor and Cognitive Impairments on Daily Living Activities and Quality of Life in Children with Autism. J. Occup. Ther. Sch. Early Interv. 2019;12:1–11. doi: 10.1080/19411243.2019.1604286. [DOI] [Google Scholar]
- 11.Summers J., Larkin D., Dewey D. Activities of daily living in children with developmental coordination disorder: Dressing, personal hygiene, and eating skills. Hum. Mov. Sci. 2008;27:215–229. doi: 10.1016/j.humov.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Beaussart M.-L., Barbarot S., Mauger C., Roy A. Systematic Review and Meta-analysis of Executive Functions in Preschool and School-Age Children with Neurofibromatosis Type 1. J. Int. Neuropsychol. Soc. 2018;24:977–994. doi: 10.1017/S1355617718000383. [DOI] [PubMed] [Google Scholar]
- 13.Gray-Burrows K., Taylor N., O’Connor D., Sutherland E., Stoet G., Conner M. A systematic review and meta-analysis of the executive function-health behaviour relationship. Health Psychol. Behav. Med. 2019;7:253–268. doi: 10.1080/21642850.2019.1637740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Papazian O., Alfonso I., Luzondo R.J. Trastornos de las funciones ejecutivas. Rev. Neurol. 2006;42:45–50. doi: 10.33588/rn.42S03.2006016. [DOI] [PubMed] [Google Scholar]
- 15.Martos Pérez J., Paula Pérez I. Una aproximación a las funciones ejecutivas en el trastorno del espectro autista. Rev. Neurol. 2011;52:S147–S153. doi: 10.33588/rn.52S01.2010816. [DOI] [PubMed] [Google Scholar]
- 16.Collette F., Hogge M., Salmon E., Van der Linden M. Exploration of the neural substrates of executive functioning by functional neuroimaging. Neuroscience. 2006;139:209–221. doi: 10.1016/j.neuroscience.2005.05.035. [DOI] [PubMed] [Google Scholar]
- 17.Miyake A., Friedman N.P., Emerson M.J., Witzki A.H., Howerter A., Wager T.D. The Unity and Diversity of Executive Functions and Their Contributions to Complex “Frontal Lobe” Tasks: A Latent Variable Analysis. Cogn. Psychol. 2000;41:49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- 18.Tirapu Ustárroz J., Bausela Herreras E., Cordero Andrés P. Modelo de funciones ejecutivas basado en análisis factoriales en población infantil y escolar: Metaanálisis. Rev. Neurol. 2018;67:215–225. doi: 10.33588/rn.6706.2017450. [DOI] [PubMed] [Google Scholar]
- 19.Estévez González A., García Sánchez C., Barraquer i Bordas L. Los lóbulos frontales: El cerebro ejecutivo. Rev. Neurol. 2000;31:566–577. doi: 10.33588/rn.3106.2000258. [DOI] [PubMed] [Google Scholar]
- 20.Ismael N., Lawson L.M., Hartwell J. Relationship Between Sensory Processing and Participation in Daily Occupations for Children with Autism Spectrum Disorder: A Systematic Review of Studies That Used Dunn’s Sensory Processing Framework. Am. J. Occup. Ther. 2018;72:7203205030p1–7203205030p9. doi: 10.5014/ajot.2018.024075. [DOI] [PubMed] [Google Scholar]
- 21.Elbasan B., Kayıhan H., Duzgun I. Sensory integration and activities of daily living in children with developmental coordination disorder. Ital. J. Pediatr. 2012;38:14. doi: 10.1186/1824-7288-38-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hofmann W., Schmeichel B., Baddeley A. Executive functions and self-regulation. Trends Cogn. Sci. 2012;16:174–180. doi: 10.1016/j.tics.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 23.McMahon K., Anand D., Morris-Jones M., Rosenthal M.Z. A Path from Childhood Sensory Processing Disorder to Anxiety Disorders: The Mediating Role of Emotion Dysregulation and Adult Sensory Processing Disorder Symptoms. Front Integr. Neurosci. 2019;13:1–11. doi: 10.3389/fnint.2019.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martini R., Cramm H., Egan M., Sikora L. Scoping Review of Self-Regulation: What Are Occupational Therapists Talking About? Am. J. Occup. Ther. 2016;70:7006290010p1–7006290010p15. doi: 10.5014/ajot.2016.020362. [DOI] [PubMed] [Google Scholar]
- 25.Murray D., Rosanbalm K., Hamoudi A. Self-Regulation and Toxic Stress: Foundations for Understanding Self-Regulation from an Applied Developmental Perspective. Office of Planning, Research and Evaluation; Administration for Children and Families, U.S. Department of Health and Human Services; Washington, DC, USA: 2015. [Google Scholar]
- 26.DeGangi G.A. Pediatric Disorders of Regulation in Affect and Behavior: A Therapist’s Guide to Assessment and Treatment. 2nd ed. Elsevier/Academic Press; London, UK; San Diego, CA, USA: 2017. Practical resources for the mental health professional. [Google Scholar]
- 27.Howard S.J., Vasseleu E. Self-Regulation and Executive Function Longitudinally Predict Advanced Learning in Preschool. Front. Psychol. 2020;11:49. doi: 10.3389/fpsyg.2020.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Howard S.J., Vasseleu E., Batterham M., Neilsen-Hewett C. Everyday Practices and Activities to Improve Pre-school Self-Regulation: Cluster RCT Evaluation of the PRSIST Program. Front. Psychol. 2020;11:137. doi: 10.3389/fpsyg.2020.00137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Payne S. Standardised Tests: An Appropriate Way to Measure the Outcome of Paediatric Occupational Therapy. Br. J. Occup. Ther. 2016;65:117–122. doi: 10.1177/030802260206500303. [DOI] [Google Scholar]
- 30.Piernik-Yoder B., Beck A. The Use of Standardized Assessments in Occupational Therapy in the United States. Occup. Ther. Health Care. 2012;26:97–108. doi: 10.3109/07380577.2012.695103. [DOI] [PubMed] [Google Scholar]
- 31.Harrison P.L., Oakland T. ABAS II. Psychological Corp.; San Antonio, TX, USA: 2003. [Google Scholar]
- 32.Montero D., Fernández-Pinto I. ABAS® II: Sistema Para la Evaluación de la Conducta Adaptativa: Manual. TEA; Madrid, Spain: 2013. [Google Scholar]
- 33.Bruininks R.L. Adaptive Living Skills Curriculum: Manual. The Riverside Pub. Co.; Chicago, IL, USA: 1991. [Google Scholar]
- 34.Morreau L.E., Bruininks R.H., Montero Centeno D., Universidad de Deusto. Instituto de Ciencias de la Educación . Inventario de Destrezas Adaptativas (CALS): Manual. Mensajero; Bilbao, Spain: 2006. [Google Scholar]
- 35.Bruininks R.K., Hill B.K., Weatherman R.F., Woodcock R.W. Inventary for Client and Agency Planning. The Riverside Pub. Co.; Chicago, IL, USA: 1986. [Google Scholar]
- 36.Montero D. Evaluación de la conducta adaptativa en personas con discapacidades. Mensajero; Bilbao, Spain: 1999. [Google Scholar]
- 37.Sparrow S.S., Cichetti D.V., Balla D.A. Vineland Adaptive Behavior Scales. 2nd ed. American Guidance Service; Circle Pines, MN, USA: 2005. [Google Scholar]
- 38.Haley S., Coster W., Ludlow L., Haltiwanger J., Andrellos P. Pediatric Evaluation of Disability Inventory (PEDI). Development, Standardization and Manual Administration. Trustees of Boston University; Boston, MA, USA: 1992. [Google Scholar]
- 39.Thompson J.R., Verdugo M.A. Escala de Intensidad de Apoyos - SIS: Manual. Tea; Madrid, Spain: 2007. [Google Scholar]
- 40.Thompson J.R., Bryant B.R., Campbell E.M., Craig E.M., Hughes C.M., Rotholz D.A. Supports Intensity Scale User’s Manual. American Association on Mental Retardation; Washington, DC, USA: 2004. [Google Scholar]
- 41.Cruz M.V.d.l., González Criado M., Newborg J. Battelle, Inventario de Desarrollo: Manual de Aplicación. TEA; Madrid, Spain: 1996. [Google Scholar]
- 42.Newborg J., Stock J.R., Wnek L., Guidubaldi J., Svinicki J. Battelle Developmental Inventory: Examiner’s Manual. DLMLINC Associates; Allen, TX, USA: 1984. [Google Scholar]
- 43.Roid G.H., Sampers J. Merrill-Palmer-Revised Scales of Development. Soelting Co.; Illinois, IL, USA: 2004. [Google Scholar]
- 44.Sánchez F., Santamaría P., Fernández-Pinto I., Arribas D. Escalas de Desarrollo Merrill-Palmer Revisadas. TEA; Madrid, Spain: 2011. [Google Scholar]
- 45.Bluma S., Sherer M., Frohman A., Hilliard J. Guía Portage de Educación Preescolar. TEA; Madrid, Spain: 1978. [Google Scholar]
- 46.Shearer M.S., Shearer D.E. The Portage Project: A model for early childhood education, Exceptional Children. Except Child. 1972;39:210–217. doi: 10.1177/001440297203900304. [DOI] [PubMed] [Google Scholar]
- 47.World Medical Association Declaración de Helsinki de la AMM—Principios éticos para las investigaciones médicas en seres humanos. [(accessed on 24 October 2019)]; Available online: https://www.wma.net/es/policies-post/declaracion-de-helsinki-de-la-amm-principios-eticos-para-las-investigaciones-medicas-en-seres-humanos/
- 48.Jöreskog K.G., Sörbom D. LISREL 8: User’s Reference Guide. 2nd ed. Scientific Software International; Chicago, IL, USA: 1996. [Google Scholar]
- 49.Frías-Navarro M.D.F., Pascual-Soler M.P. Prácticas del análisis factorial exploratorio (AFE) en la investigación sobre conducta del consumidor y marketing. Suma Psicol. 2012;19:47–58. [Google Scholar]
- 50.Beavers A.S., Lounsbury J.W., Richards J.K., Huck S.W., Skolits G.J., Esquivel S.L. Practical considerations for using exploratory factor analysis in educational research. PARE. 2013;18:1–13. [Google Scholar]
- 51.Ferrando P.J., Lorenzo-Seva U. El análisis factorial exploratorio de los ítems: Algunas consideraciones adicionales. An. Psicol. 2014;30:1170–1175. doi: 10.6018/analesps.30.3.199991. [DOI] [Google Scholar]
- 52.Lorenzo-Seva U.F.P.J. FACTOR 9.2: A Comprehensive Program for Fitting Exploratory and Semiconfirmatory Factor Analysis and IRT Models. Appl. Psychol. Meas. 2013;37:497–498. doi: 10.1177/0146621613487794. [DOI] [Google Scholar]
- 53.Ferrando P.J., Lorenzo-Seva U. Program FACTOR at 10: Origins, development and future directions. Psicothema. 2017:236–240. doi: 10.7334/psicothema2016.304. [DOI] [PubMed] [Google Scholar]
- 54.Lloret S., Ferreres A., Hernández A., Tomás I. The exploratory factor analysis of items: Guided analysis based on empirical data and software. An. Psicol. 2017;33:417–432. doi: 10.6018/analesps.33.2.270211. [DOI] [Google Scholar]
- 55.Watkins M.W. Exploratory Factor Analysis: A Guide to Best Practice. J. Black Psychol. 2018;44:219–246. doi: 10.1177/0095798418771807. [DOI] [Google Scholar]
- 56.Ferrando P.J., Anguiano-Carrasco C. El análisis factorial como técnica de investigación en psicología. Pap. del Psicól. 2010;31:18–33. [Google Scholar]
- 57.Gadermann A., Guhn M., Zumbo B.D. Ordinal Alpha. In: Michalos A.C., editor. Encyclopedia of Quality of Life and Well-Being Research. Springer; Dordrecht, The Netherlands: 2014. pp. 4513–4515. [Google Scholar]
- 58.Dominguez-Lara S. Fiabilidad y alfa ordinal. Actas Urol. Esp. 2018;42:140–141. doi: 10.1016/j.acuro.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 59.Mukaka M.M. Statistics Corner: A guide to appropriate use of Correlation coefficient in medical research. Malawi. Med. J. 2012;24:69–71. [PMC free article] [PubMed] [Google Scholar]
- 60.Ministerio de Sanidad, Servicios Sociales e Igualdad . Encuesta Nacional de Salud: España 2011/12. Salud Mental y Calidad de Vida en la Población Infantil. Ministerio de Sanidad, Servicios Sociales e Igualdad; Madrid, Spain: 2014. (Serie Informes monográficos no2). [Google Scholar]
- 61.Van Gameren-Oosterom H.B.M., van Dommelen P., Schönbeck Y., Oudesluys-Murphy A.M., van Wouwe J.P., Buitendijk S.E. Prevalence of overweight in Dutch children with Down syndrome. Pediatrics. 2012;130:e1520–e1526. doi: 10.1542/peds.2012-0886. [DOI] [PubMed] [Google Scholar]
- 62.Pardo-Guijarro M.J., Martínez-Andrés M., Notario-Pacheco B., Solera-Martínez M., Sánchez-López M., Martínez-Vizcaíno V. Self-reports versus parental perceptions of health-related quality of life among deaf children and adolescents. J. Deaf. Stud. Deaf. Educ. 2015;20:275–282. doi: 10.1093/deafed/env018. [DOI] [PubMed] [Google Scholar]
- 63.Haley S.M., Coster W.J., Dumas H.M., Fragala-Pinkham M.A., Moed R. PEDI-CAT: Development, Standardization and Administration Manual. Boston University; Boston, MA, USA: 2012. [Google Scholar]
- 64.Guide for the Functional Independence Measure for Children (WeeFIM) of the Uniform Data System for Medical Rehabilitation, Version 4.0. State University of New York; Buffalo, NY, USA: 1993. [Google Scholar]
- 65.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association Publishing; Washington, DC, USA: 2013. [Google Scholar]
- 66.Kilincaslan A., Kocas S., Bozkurt S., Kaya I., Derin S., Aydin R. Daily living skills in children with autism spectrum disorder and intellectual disability: A comparative study from Turkey. Res. Dev. Disabil. 2019;85:187–196. doi: 10.1016/j.ridd.2018.12.005. [DOI] [PubMed] [Google Scholar]