Abstract
Primary myelofibrosis (PMF) is a rare myeloproliferative neoplasm characterized by stem-cell-derived clonal over-proliferation of mature myeloid lineages, bone marrow fibrosis, osteosclerosis, defective erythropoiesis, and pro-inflammatory cytokine over-expression. The aim of the present study was to highlight possible differences in the transcriptome among CD34+ cells from peripheral blood (PB) of PMF patients. Therefore, we merged two microarray datasets of healthy control subjects and PMF (34 JAK2V617F MUTATED and 28 JAK2 wild-type). The GO analysis of upregulated genes revealed enrichment for JAK2/STAT1 pathway gene set in PB CD34+ cells of PMF patients with and without the JAK2V617F mutation comparing to the healthy control subjects, and in particular a significant upregulation of immunoproteasome (IP)-belonging genes as PSMB8, PSMB9, and PSMB10. A more detailed investigation of the IFN-gamma (IFNG) pathway also revealed that IFNG, IRF1, and IFNGR2 were significantly upregulated in PB CD34+ cells of PMF patients carrying the mutation for JAK2V617F compared to JAK2 wild-type PMF patients. Finally, we showed an upregulation of HLA-class I genes in PB CD34+ cells from PMF JAK2V617F mutated patients compared to JAK2 wild-type and healthy controls. In conclusion, our results demonstrate that IPs and IFNG pathways could be involved in PMF disease and in particular in patients carrying the JAK2V617F mutation.
Keywords: immunoproteasome, JAK2V617F, primary myelofibrosis, bioinformatics, CD34+ cells, HLA-class I, innate immunity
1. Introduction
Primary Myelofibrosis (PMF) is a Philadelphia-negative myeloproliferative neoplasm (MPNs), characterized by stem cell-derived clonal proliferation of one or more myeloid lineage cells [1]. It is associated with bone marrow fibrosis, osteosclerosis, angiogenesis, extramedullary hematopoiesis, and adnormal cytokine levels [2]. Most patients with PMF carry one of three mutually exclusive somatic driver mutations JAK2V617F (about 60%) [3], Calreticulin (CALR) (about 20%) [4] and MPL (about 5%) [5,6]. These genetic markers have been recently included in the major diagnostic criteria for PMF, and the presence of JAK2V617F mutant confers an inferior outcome than the CALR mutant. More recently, the molecular landscape of PMF has become increasingly well characterized, leading to the development of genetically-based prognostic scoring systems such as MIPPS70, MIPSS70+ version 2.0, and GIPPS [7,8,9]. Before the discovery of JAK2 mutation, one of the most important prognostic factors of evolution toward blast transformation in PMF was the absolute number of circulating CD34+ cells in peripheral blood [10]. In the post-genomic era, CD34+ cells in peripheral blood >10/μL can still distinguish PMF from other MPNs with high sensitivity and specificity [6]. PMF patients have few therapeutics options because there is limited information on its biology. Ruxolitinib (RUX) is a first-in-class oral JAK1/JAK2 inhibitor approved for the treatment of patients with myelofibrosis based on the results of two randomized clinical trials (COMFORT-I and COMFORT-II) [11]. Clinical benefits of RUX are partially derived from the reduction of inflammatory cytokines, with an early relief of clinical symptoms and reduction of spleen size after 4 weeks post-treatment [12,13]. Only in a few cases the drug reverts bone marrow fibrosis or reduces the allele burden [14], suggesting that other intracellular signaling in the neoplastic clone or in the host-tumor interaction can affect the clinical course of PMF.
Several papers have shown evidence of a dysregulation of the immune system in the MPNs. PMF is considered as an inflammatory disease where the higher cytokine secretion creates a pro-inflammatory milieu influencing the immune system [15]. It has been demonstrated that several immune defects are principally associated with the presence/absence of the JAK2V617F mutation [16,17]. Overall, these anomalies could contribute to the development of an immune deficiency state with the potential to promote immune evasion, cancer progression and increased susceptibility to infections [18]. Furthermore, a better understanding of immune biology in the context of PMF would be important for the design of new therapies for PMF.
In eukaryotic cells, the proteasomes (c-20S) are ubiquitously-expressed cellular proteases involved in the degradation of intracellular oxidized proteins following an oxidative insult, through an ATP-independent mechanism [19]. Being ubiquitously expressed, these proteins represent a potential pharmacological target even though with several limitations [20]. To this regard, Bortezomib, a potent and clinically relevant proteasome inhibitor, is intermittently used for multiple myeloma treatment (MM) [21,22] and other inflammatory disease [23,24,25], in order to limit toxic effects [26]. In cells of hematopoietic origins, the classical proteasome is replaced by a different proteasome with an immunological role called immunoproteasome (IPs) [27]. The origin of this term arises from the fact that it was discovered during studies of antigen presentation on the cell surface for T-cell recognition to stimulate the immune response in collaboration with major histocompatibility class I (MHC class I) molecules. Both innate immunity (lymphocytes) and acquired immunity (monocytes, dendritic cells, and macrophages) [28] cells during inflammatory processes express the 20s immunoproteasome subunits (i-20) [29]. Additionally, stimulation with type I Interferon [30], Tumor Necrosis Factor alpha (TNFα) [31], or IFNG [32], cytokines that are essential for both innate and adaptive immune response to viral and bacterial infections, stimulates new i-20S. Considerable interest has been focused on developing immunoproteasome-specific inhibitors (IPSIs) for applications in autoimmune disorders such as systemic lupus erythematosus [33], inflammatory bowel disease [34], and rheumatoid arthritis [35]. The i-20S proteasome is generally expressed in the spleen, thymus, bone marrow, and lymph nodes, all of which are associated with lymphocyte maturation [36]. Furthermore, the proteasome inhibition also represents an attractive potential anticancer therapy. Since Bortezomib was able to inhibit the NF-kappaB pathway in MM [21], it was believed that it could also be effective for PMF patients. However, the first clinical studies on PMF patients did not show encouraging results [37], although the pre-clinical results on the mouse model seemed very promising, having determined a decrease in the transformation of growth factor-β1 and osteoprotegerin levels, a reduction in osteosclerosis, and as a direct consequence an increase in survival [38]. Lack of clinical efficacy of Bortezomib in myelofibrosis may be linked to the need for blocking oncogenic driver mutations including Janus Kinase 2 and Calreticulin.
With the aim of identifying new possible molecular targets, we used the datasets available in GEODataset [39] in order to describe the main differences in the transcriptome of CD34+ hematopoietic progenitor cells circulating in peripheral blood (PB) of healthy individuals, and in wild-type or JAK2V617F mutated PMF patients, trying to draw a starting line for future investigations.
2. Results
2.1. Identification of Potential Genes Modulated in JAK2V617F Mutated Compared to JAK2 Wild-Type PMF Patients
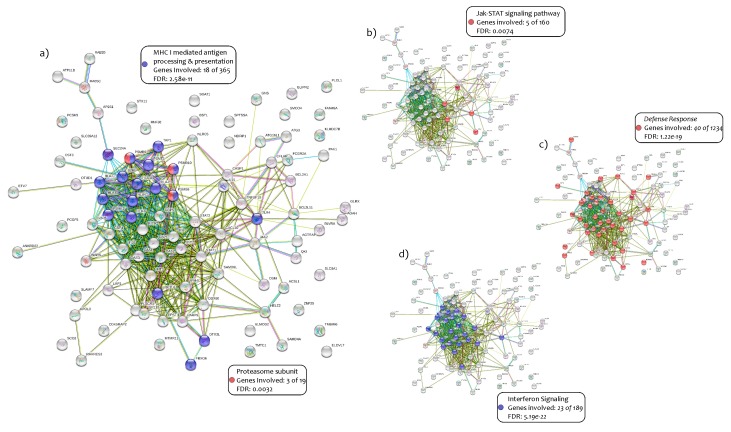
From microarray datasets, we selected 34 PMF patients carrying the JAK2V617F mutation and 28 JAK2 wild-type patients. We compared the two groups of study and obtained 1278 upregulated and 2070 downregulated genes in JAK2V617F mutated patients compared to the JAK2 wild-type (Supplementary Table S1). A Gene Ontology (GO) analysis performed on the first 100 most significant modulated genes (p < 0.0001) showed impressive results (Figure 1) (Supplementary Table S1). Then we identified 18 genes out of 365 (4.9%) belonging to the pathway of MHC class I mediated antigen processing and presentation (p = 2.58 × 10−11) and three genes out of 19 (15.7%) belonging to the Immunoproteasome (IPs) (PSMB8, PSMB9 and PSMB10) (p = 0.0032) (Figure 1a) (Supplementary Table S1).
Figure 1.
GO analysis in 100 genes upregulated in JAK2V617F mutated patients.The GO analysis performed with the online tool GeneMANIA and GHATER showed the following results: 18 genes out of 365 belonging to the pathway of MHC class I-mediated antigen processing and presentation (p = 2.50 × 10−11) (a); 3 genes out of 19 belonging to the Immunoproteasome (IPs) (p = 0.0032) (a); the involvement of JAK-STAT signal pathways (p = 0.0074) (b); the Immuno-Defense-Response (40 out of 1234 genes) (p = 1.22 × 10−19) (c); 23 genes out of 189 belonging to the IFNG pathways (p = 5.19 × 10−22) (d).
Furthermore, as expected, the involvement of JAK-STAT signaling pathways in JAK2V617F mutated patients with the transcription of JAK2, STAT1, STAT2 and OSM genes was confirmed (p = 0.0074) (Figure 1b) (Supplementary Table S1). A large number of genes belonging to the Immuno-Defense-Response were highlighted (40 out of 1234 genes) (3.2%) (p = 1.22 × 10−19) (Figure 1c) (Supplementary Table S1). Moreover, the IFNG signaling pathways were significantly involved through the expression of 23 genes out of 189 available (p = 5.19 × 10−22, 12.1%) (Figure 1d) (Supplementary Table S1). In our analysis, we also observed several antiviral response activated pathways, such as the double-strand RNA virus (OAS1, OAS2 and OAS3) (three out of nine genes; p = 0.00066, 33.3%) [40,41,42,43,44], the Herpes simplex (14 out of 181 genes; p = 1.10 × 10−10, 7.7%), and Influenza A virus (10 out 168 genes; p = 5.29 × 10−7, 5.9%) (Supplementary Table S1). These specific activated pathways could be due to the IFNG signaling.
2.2. Immunoproteasome (IPs) Genes Expression in PMF Patients
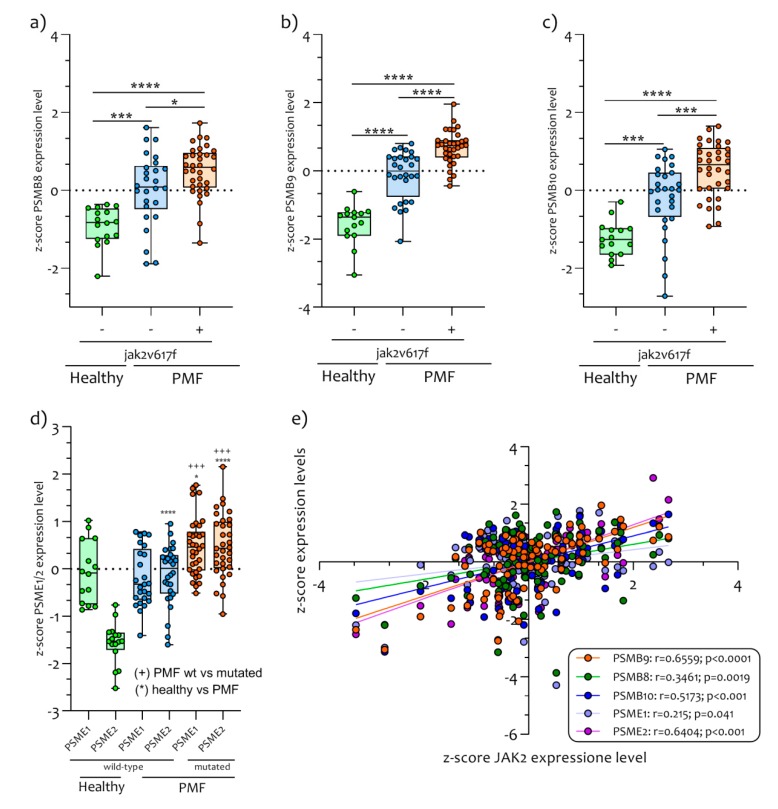
Our analysis showed that PSMB9 is the most significantly modulated gene in PB CD34+ cells of PMF patients, both with and without JAK2V617F mutation, compared with healthy subjects (p < 0.00001) (Figure 2) (Supplementary Table S1).
Figure 2.
IPs genes expression in PB CD34+ Cells of JAK2V617F mutated/wild-type PMF patients and healthy control subjects. The genes belonging to the IPs family are PSMB8 (a), PSMB9 (b), PSMB10 (c) and PSME1/2 (d). The patients affected by primary myelofibrosis express significant upregulated levels of IPs compared to healthy controls. In addition, the PMF patients mutated for JAK2V617F express significant upregulated levels of IPs genes compared to wild-type patients. The JAK2 gene expression levels in PB CD34+ cells of PMF patients were significantly correlated with IPs genes expression. Data are expressed as z-score intensity expression levels and presented as vertical scatter dot plots. p values < 0.05 were considered to be statistically significant (* p < 0.05; *** p < 0.0005; **** p < 0.00005).
This gene, together with another two catalytic subunits (PSMB8 and PSMB10), constitute most of the IPs that are constitutively expressed in hematopoietic cells and induced by pro-inflammatory cytokine such as IFNG. Furthermore, the expression of PSMB8 (p < 0.00001), PSMB9 (p < 0.00001), PSMB10 (p < 0.00001) and PA28α and β (PSME1 and PSME2 respectively) (Figure 2) were significantly upregulated in JAK2V617F mutated PMF patients compared to healthy JAK2V617F wild-type PMF and to controls subjects (PSMB8, p < 0.00001; PSMB9, p < 0.00001; PSMB10, p < 0.0001; PSME1, p = 0.0001; PSME2, p < 0.0001) (Figure 2a–d). We also showed that all IPs genes were significantly correlated to the JAK2 gene expression levels (PSMB8 r = 0.3461, p = 0.0019; PSMB9 r = 0.6559, p < 0.0001; PSMB10 r = 0.5173, p < 0.001; PSME1 r = 0.215, p = 0.041; PSME2 r = 0.6404, p < 0.0001) (Figure 2e). Furthermore, we observed that JAK2 and STAT1 genes expression levels were significantly modulated in JAK2V617F mutated PMF patients compared to PMF JAK2V617F wild-type (JAK2, p < 0.00001 and STAT1, p < 0.00001) and to healthy controls (JAK2, p < 0.00001 and STAT1, p < 0.00001) (Figure 3a,b).
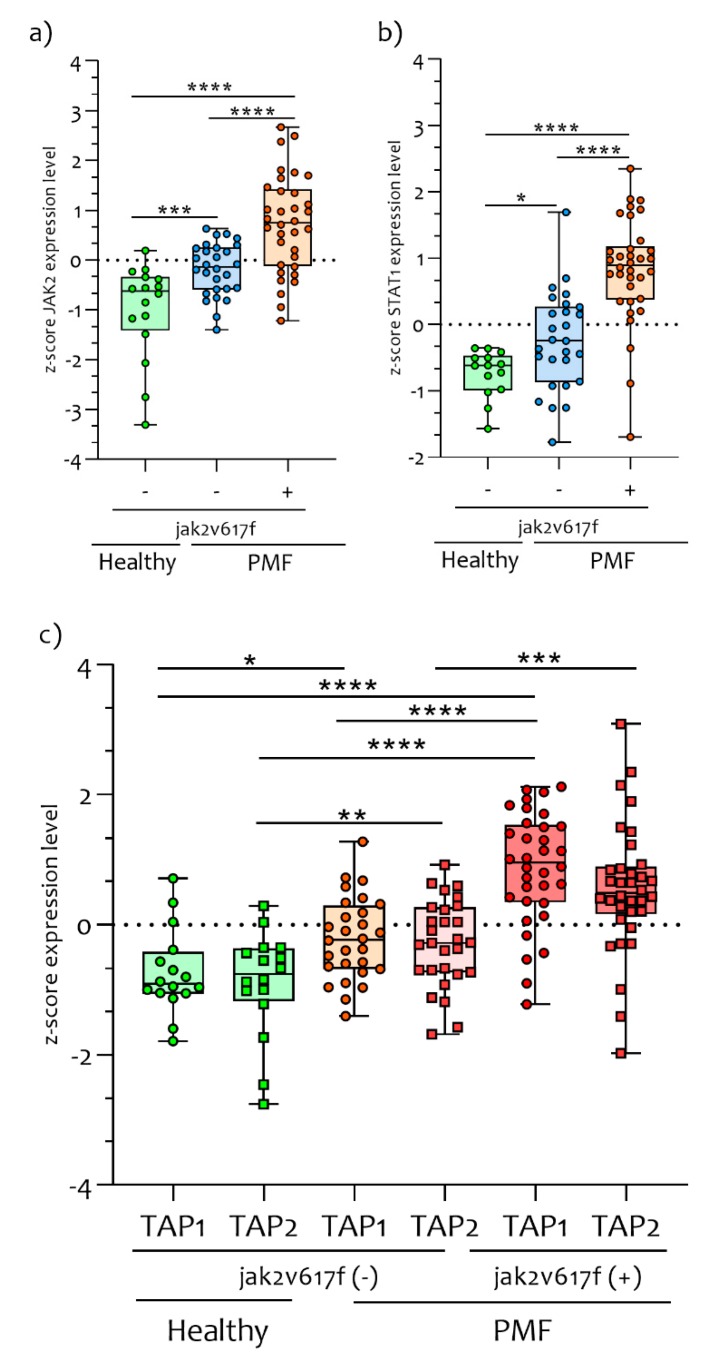
Figure 3.
JAK2/STAT1 and TAPs gene expression levels in PMF patients and healthy control subjects. The JAK2/STAT1 expression levels are closely linked to the PMF condition. During our analysis, we showed that JAK2/STAT1 gene expression levels were significantly upregulated in PB CD34+ cells of PMF patients compared to healthy controls subjects (a and b). Furthermore, the PMF patients who had the JAK2V617F mutation had significantly upregulation of JAK2/STAT1 compared to wild-type. Transporters associated with Antigen Processing 1 and 2 are proteins that in humans are encoded by the TAP1 and TAP2 genes. These genes are involved in the degradation of peptides in order to assemble at the class I molecules. In CD34+ cells of PMF patients, we showed that TAP1 and TAP2 expression levels were significantly upregulated compared to healthy controls subjects (c). Furthermore, PMF JAK2V617F mutated patients presented significantly upregulated levels of TAP1 and TAP2 compared to PMF JAK2V617F wild-type. Data are expressed as z-score intensity expression levels and presented as vertical scatter dot plots. p values < 0.05 were considered to be statistically significant (* p < 0.05; ** p < 0.005; *** p < 0.0005; **** p < 0.00005).
Significant differences in JAK2 (p = 0.0007) and STAT1 (p = 0.024) expression levels were observed by comparing healthy controls to PMF patients who are wild-type for the JAK2V617F mutation. These results seem to indicate an activation of the JAK2 pathway in both mutated and wild-type PB CD34+ cells of PMF patients (Figure 3a,b).
Deeping our investigation on IPs pathways, we observed a significant upregulation in the expression levels of TAP1 (p < 0.01) and TAP2 (p < 0.001) in PB CD34+ cells of PMF patients compared to healthy controls subjects (Figure 3c). Furthermore, the TAP1 (p < 0.00001) and TAP2 (p < 0.0001) expression levels were significantly upregulated in JAK2V617F mutated compared to JAK2 wild-type patients (Figure 3c). Significant differences in TAP1 (p < 0.00001) and TAP2 (p = 0.0003) expression levels were observed by comparing PMF patients with and without JAK2V617F mutation (Figure 3c).
Furthermore, we verified the trend of the constituent isoforms of the proteasome (PSMB5, PSMB6, and PSMB7). None of the three components showed significant changes between JAK2V617F mutated PMF patients and wild-type patients (Figure S1a). The gene expression levels of the PSMB5 and PSMB6 subunits were significantly increased in PMF patients, regardless of the presence of the mutation. With regards to the gene expression levels of the PSMB7 subunit, they were downregulated in PMF patients, effectively preventing the formation of the proteasome complex in PMF patients. To confirm this, the expression levels of the PSMB7 subunit were inversely related to the expression of JAK2 (Figure S1b).
2.3. IFNG Pathways Activation in PB CD34+ Cells of PMF Patients
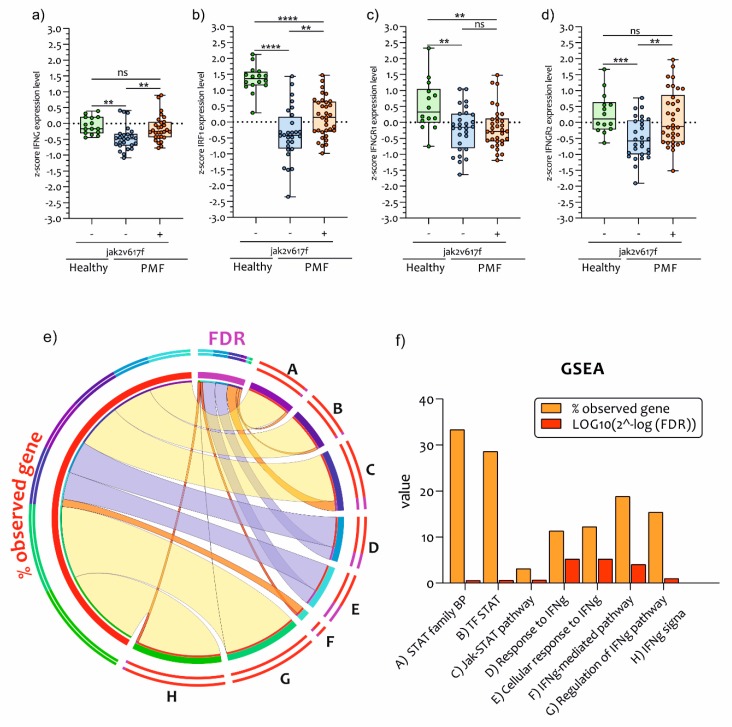
Our GO analysis highlighted the activation of the IFNG pathway. We have further investigated the gene expression levels of IFNG, IRF1, and IFNGR1/2 gene expression. We have showed that there was a significant downregulation in IFNG (p < 0.001) expression levels in JAK2 wild-type PMF PB CD34+ cells compared to healthy controls subjects. Patients presenting the JAK2V617F mutation had significant upregulation of IFNG (p < 0.001) expression levels compared to PMF JAK2V617F wild-type patients (Figure 4a).
Figure 4.
IFNG genes pathways expression levels in PB CD34+ Cells of PMF patients. JAK2 is necessary and sufficient for IFNG-induced transcription of genes involved in immuno-response against antigens self/non-self. In our analysis, we showed that IFNG gene expression levels were significantly downregulated in PB CD34+ cells of PMF patients wild-type for JAK2V617F mutation compared to healthy controls subjects (a), but not compared to JAK2V617F mutated patients. Similar trends were observed for IRF1 (b) and IFNGR2 (d). The IFNGR1 modulation was an exception (c). GSEA of IFNG and STAT pathways. The data visualization was obtained by tool CIRCOS. The ribbons are expressed by weighted percentage (Q1 = red; Q2 = orange; Q3 = yellow; Q4 = purple). For Q1 and Q2 we used a transparency of 4 and no stroke (e). GSEA of IFNG and STAT1 pathways are expressed in a bar chart (f). Data are expressed as z-score intensity expression levels and presented as vertical scatter dot plots. p values < 0.05 were considered to be statistically significant (** p < 0.005; *** p < 0.0005; **** p < 0.00005).
The same trend was observed for both the expression levels of IRF1 (p = 0.0073) and IFNGR2 (p = 0.015) (Figure 4b,d) (Supplementary Table S1). By contrast, IFNGR1 expression was significantly downregulated in JAK2 wild-type (p = 0.0033) and mutated (p = 0.0027) CD34+ PMF patient PB cells compared to healthy subjects, while there was no significant difference between JAK2 wild-type and mutated patients (p = 0.8148) (Figure 4c). This data was confirmed by GSEA for IFNG and STAT1/2 pathways (Figure 4e,f). About 33.3% of the genes involved in STAT1-activated pathways were upregulated in PMF JAK2 mutated patients. Furthermore, the IFNG pathways were significantly modulated (FDR = 5.21 × 10−18) in mutated PMF patients compared to wild-type PMF.
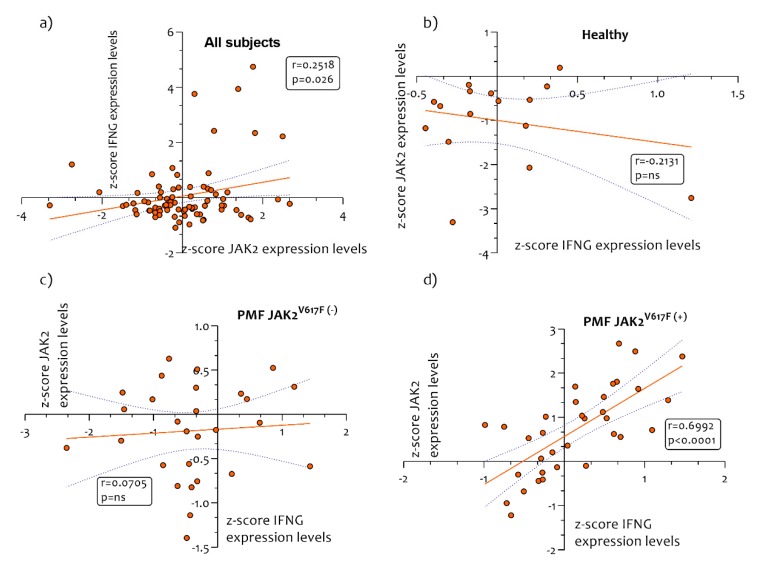
In order to verify whether IFNG gene expression was dependent on JAK2 expression, we performed a Pearson correlation analysis. We showed a positive correlation (r = 0.2518, p = 0.026) in all subjects recruited in the study between IFNG versus JAK2 expression levels (Figure 5a).
Figure 5.
Correlation analysis between IFNG/JAK2 expression levels. A Pearson correlation analysis was performed in order to verify the potential correlation between JAK2 and IFNG in healthy controls subjects and in PMF patients. We showed a positive correlation (r = 0.2518, p = 0.026) in all the subjects recruited in the study between IFNG/JAK2 expression levels (a). No correlation was observed in healthy controls subjects (b) and in PMF patient’s wild-type for JAK2V617F mutation (B/C). A significantly positive correlation was observed in PMF patients mutated for JAK2V617F (r = 0.6992, p < 0.0001) (c). p values < 0.05 were considered to be statistically significant.
Furthermore, no correlation was observed in healthy control subjects and in PMF patient who were wild-type for JAK2V617F mutation (Figure 5b,c). However, we observed a positive correlation between the expression levels of JAK2 and IFNG in PMF patients mutated for JAK2V617F (r = 0.6992, p < 0.0001) (Figure 5c).
2.4. Antigen Exposition Pathways in PB CD34+ Cells of PMF Patients
Following IFNG, JAK2, and IPs pathway activation we further investigated the possible involvement of the MHC class I (HLA class I)-mediated recognition system consistently with the GO analysis (Figure 1). In order to test this hypothesis, we analyzed the HLA family genes expression in PMF patients compared to healthy controls subjects. Our analysis showed a significant upregulation in the expression levels of the HLA-A, HLA-B, HLA-C, HLA-E, HLA-F and HLA-G genes in PB CD34+ cells from PMF JAK2V617F mutated patients compared to JAK2 wild-type patients and healthy control subjects (Figure 6a–d). In particular, we showed a significant upregulation in the expression of HLA-A (the most modulated gene among the HLAs genes) (Figure 6a,c,d) and B2M (Figure 6b) in PB CD34+ cells from JAK2V617F mutated PMF patients compared to JAK2 wild-type patients (HLA-A, p < 0.00001 and B2M p < 0.00001) and healthy controls subjects (HLA-A, p < 0.0001 and B2M, p < 0.00001).
Figure 6.
HLA-A and B2M genes expression are modulated in PB CD34+ Cells of PMF patients. HLA-A expression levels clearly differed between PMF patients with JAK2V617F mutation compared to wild-type patients and healthy control subjects. A significant upregulation was observed in HLA-A expression levels (a) and in B2M (b) in PMF patients mutated for JAK2V617F compared to wild-type patients and healthy controls subjects. Heatmap of HLAs class I gene expressed in PB CD34+ Cells of healthy, PMF patients JAK2 mutated and wild-type (c). Z-score expression levels of HLAs class I gene in in PB CD34+ Cells of healthy, PMF patients JAK2 mutated and wild-type (d). Data are expressed as z-score intensity expression levels and presented as vertical scatter dot plots and violin plot. p values < 0.05 were considered to be statistically significant (* p < 0.05; *** p < 0.0005; **** p < 0.00005).
In addition, JAK2V617F wild-type PMF patients presented a significant downregulation of HLA-A expression levels compared to healthy controls subjects (p < 0.01) (d). No significant modulation was observed in B2M expression levels between healthy controls subjects and JAK2V617F wild-type PMF patients (p = 0.056) (Figure 6b). Finally, compared to healthy controls, CD34+ cells from PMF patients showed significative up-regulation of ARG1, which correlated with the JAK2 expression levels in JAK2V617F mutated patients (r = 0.4181 and p = 0.0139) (Figure S2a–c).
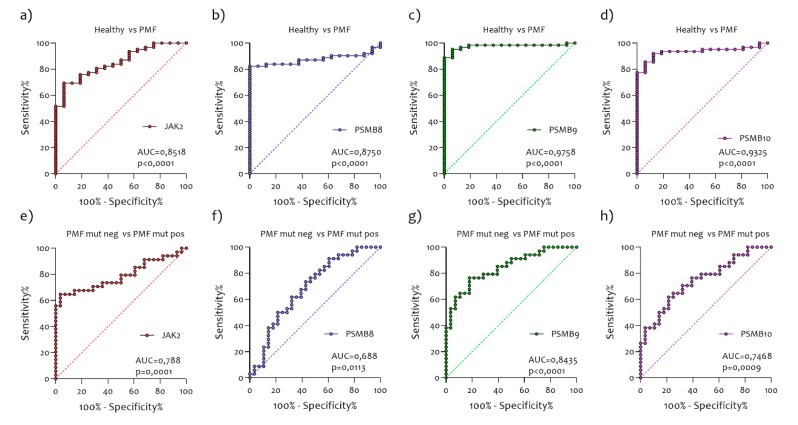
2.5. Diagnostic Accuracy of mRNA PSMB8, PSMB9, and PSMB10 for PMF Patients
We tested accuracies for PMF wild-type patients versus PMF mutated and versus healthy using logistic regression models (Figure 7). PSMB8 (AUC = 0.8750), PSMB9 (AUC = 9758), and PSMB10 (AUC = 0.9325) were all significant predictors of PMF, all with a higher AUC than JAK2 (AUC = 0.8518) (Figure 7a–d). For single predictors, PSMB9 had the highest accuracy, followed by PSMB10 and PSMB8. For PMF wild-type versus PMF mutated, PSMB9 is a significant individual predictor (AUC = 0.8435) (Figure 8g), while JAK2 (AUC = 0.788) (Figure 8e) was the following predictor (PSMB8 AUC = 0.688, PSMB10 AUC = 0.7468) (Figure 7f,h).
Figure 7.
Diagnostic accuracy of JAK2 (a,e), PSMB8 (b,f), PSMB9 (c, g), and PSMB10 (d, h) mRNA for PMF patients. For single predictors, PSMB9 (c) had the highest accuracy, followed by PSMB10 (d) and PSMB8 (b). For PMF wild-type versus PMF mutated, PSMB9 (g) is a significant individual predictor.
Figure 8.
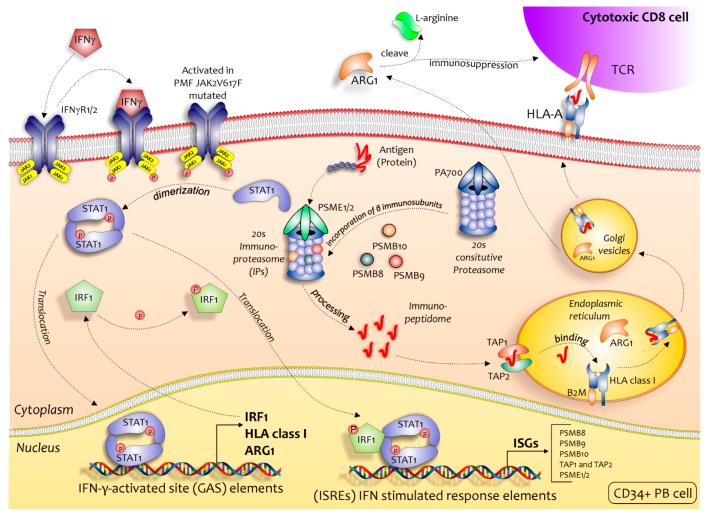
Regulatory role of the IPs in immune surveillance in PB CD34+ Cells of PMF JAK2V617F mutated patients. The activation of JAK2 pathway, in a classical manner through the binding of IFNG to its receptor (IFNGR1/2) or through the JAK2V617F mutation, induces the expression of the immunoproteasome-specific subunits β1i (PSMB9), β2i (PSMB10), β5i (PSMB8), PA28 (PSME1), and PA28 (PSME2) (via STAT1 and IRF1) that result in the preferred assembly of the immunoproteasome over the regular proteasome. The resulting immuno-peptidome more effectively binds to MHC class I molecules (induced during the activation of JAK2), such that after processing in the endoplasmic reticulum (ER) (TAP1 and TAP2) and Golgi apparatus the individual peptides presented on the cell surface can be recognized by T-cell receptors on CD8+ cells, initiating an immune response (increased ARG1 expression is known to result in arginine deficiency, which leads to immunosuppression by impairing lymphocyte proliferation and activation).
3. Discussion
In this manuscript, we hypothesized that there are significant differences in transcriptomes among PB CD34+ cells of PMF patients with and without JAK2V617F mutation. To address our hypothesis, we merged two microarray datasets available on a GEO Dataset, for a total of 31 healthy control subjects and 62 PMF patients (34 with and 28 without JAK2V617F mutation). Our transcriptome analysis of circulating CD34+ cells wild-type and JAK2V617F mutated PMF patients disclosed a dysregulation in the antigen presentation signaling involving immunoproteasome and upregulation of HLA class I genes. As expected, in JAK2V617F circulating CD34+ cells there was an involvement in the JAK2/STAT1 and IFNG gene pathways.
During inflammatory processes, in response to stimulation with type I interferon [45], TNFα [31], or IFNG [46], cells of hematopoietic origins can replace the c-20S with the so-called immunoproteasome (i20S) [27], as discovered during studies of antigen presentation on the cell surface for T-cell recognition to stimulate the immune response in collaboration with major histocompatibility class I (MHC class I) molecules. With the expression of the i-20s subunit, the standard catalytic subunits 1, 2 and 5 of c-20s are substituted with the subunits 1i (LMP2 or PSMB9), 2i (MECL-1 or PSMB10), and 5i (LMP7 or PSMB8) respectively [47]. Once the IP was activated, this promoted helper T (Th) cell differentiation (including pro-inflammatory Th1 and Th17 cells) and effector T cell expansion (cytotoxic CD8 cells), while repressing regulatory T (Treg) cell induction, admittedly through yet unidentified pathways [48]. It has been observed that IPs inhibition suppresses the expression of the pro-inflammatory IFNG, TNF-α, GM-CSF, and IL-6 cytokines in activated T cells [49]. All these cytokines are highly expressed in PB of PMF patients and might play a key role in the progression of the disease [50,51,52]. These evidences are in accordance with our results.
Recently, numerous transcriptome analyses have been performed to study the main Philadelphia-negative myeloproliferative neoplasms (MPNs). These analyses have shown promising new target genes for the various pathologies examined. The impairment of the immunologic framework has emerged almost always, showing an alteration of the pro-inflammatory, pro-differentiation and anti-apoptotic transcription lines. As an example, in idiopathic myelofibrosis (IM) [53], and in PMF [54,55,56] it emerged from the analyses that the WT1 gene is highly modulated. A T-cell receptor (TCR) that specifically reacts with WT1 peptide in the context of HLA-A * 24:02 has been identified [57]. The receptor recognition mechanism passes through the activation of the IP. As shown recently by Stetka et al. [58], numerous genes belonging to immuno-activation have been identified to be highly modulated in PV. In this manuscript, the authors treated the JAK2 wild-type and JAK2V617F CD34+ progenitors with medium without or with inflammatory cytokines (IFN-gamma, TNF-α, and TGF-β). They showed that among the top 20 differentially overexpressed genes shared by both types of progenitors (JAK2 wild-type and V617F mutant) treated with inflammatory factors are some members from our gene set of differentially expressed genes, including IRF1, STAT1, B2M, and TAP1. These data suggest that the expression signature characterizing the JAK2V617F mutated PMF patients may result not only from intrinsic V617F-driven expression program, but also from extrinsic inflammatory cytokine-driven activation, which could be different in JAK2V617F mutated and JAK2 wild-type PMF.
Immune dysfunction in PMF is an intriguing emerging field [59]. Differently from other MPNs [60,61], T-cells count is preserved, but there is an altered regulatory T cell frequency, expansion of myeloid-derived suppressor cells, and CD4/natural killer cell dysfunction [62], while data on CD8+ are lacking. Our analysis would suggest that, based on interaction with hematopoietic progenitors, CD8 T cells are more active in patients with PMF. This is in line with the clinical observation that hematopoietic progenitors could respond to chronic inflammation in the context of a systemic autoimmune disease favoring fibroblast activation leading to bone marrow fibrosis and progressive cytopenias, in both primary and secondary myelofibrosis [63]. Moreover, we found that HLA class I genes expression levels were closely related to PMF disease and JAK2V617F mutation, indicating a potential relationship with CD8+ T-cells [64]. The downregulation of class I and II HLA genes is used by tumor cells to escape antitumor T-cell-mediated immune responses. Although the expression levels of HLA genes are high in MPNs, there is no evidence in PMF patients [65,66]. The upregulation of HLA class I genes is important for tumor immune surveillance by IFNG treatment in PMF. This mechanism might enhance the cytotoxic potential of immune cells against PMFs. Unfortunately, as mentioned above there is no available data that indicate CD34+ PMF cells as a potential target for the cytotoxic action of CD8+ T cells.
From our analysis, it seems that the JAK2V617F mutation increases, on one hand, the capacity of immunological response with the activation of IPs pathways, but at the same time the immune response against CD34+ PMF cells seems to be ineffective. We could speculate that elevated endoplasmic reticulum stress induces the release of damage-associated molecular patterns to the tumor microenvironment, which activates IFN-gamma signaling in PMF cells. The elevated IFN-gamma signaling induces higher activity in the IPs, which might improve antigen presentation and result in the recruitment of TILs to the bone marrow, the release of pro-inflammatory cytokine and as a consequence, the increase of fibrosis [67]. In this regard, the activation of IPs determines the ability of the PMF cells to be potentially recognized by cytotoxic CD8+ cells (Figure 8).
Knowing this, blocking the IPs action could have direct repercussions on the pro-inflammatory cytokines expression levels in PMF and subsequently on its clinical course, making IPs an extremely interesting candidate in the search for anticancer drugs.
IP modulation is extremely varied in the different types of tumors, since IPs can be upregulated in some scenarios (e.g., prostate cancer and lung cancer) [68,69] and down-regulated in others (e.g., colon [70], kidney, skin, neck, head, and esophagus) [20]. The selective i-20S inhibitor carfilzomib has shown clinical activity in vitro in primary CD34+ PMF cells and it is safe in combination with ruxolitinib in patients affected by several hematological malignancies (clinical trial.gov, NCT03773107), suggesting that targeting IPs is worth being investigated in PMF. We must bear in mind that, abnormal MHC class I expression and the loss of antigen processing are features of malignant cells [71]. T cell‒mediated immune tumor suppression is a complex process with numerous requirements, among which is antigen processing by the IPs and presentation through MHC class I surface molecules expressed on tumor cells. The IPs genes are regulated by both cell-intrinsic and cell-extrinsic factors in different types of cancer. In PMF patients, regardless of the JAK2V617F mutation, it would appear that the entire IPs activation pathways are transcribed. In fact, from our analysis, it was shown that ARG1 was also upregulated in PMF patients compared to healthy control subjects.
An interesting hypothesis to be demonstrated of the activation of the IP in the PMF could be the presence of a previous viral infection underlying the activation of IPs [72]. In this case, the MHCs class I would carry viral antigens ready to be recognized, but due to the immune escape activated by the tumor cells, with the production of ARG1, LAG3, and CTLA4 (Supplementary Table S1), they do not recognize it.
4. Materials and Methods
4.1. Data Selection
The NCBI Gene Expression Omnibus (GEO) database [73] was used to select transcriptome datasets to analyze genes expression in primary myelofibrosis (PMF) patients. Mesh terms “myelofibrosis”, “JAK2V617F”, “JAK2”, “CD34+” and “Human” were used to identify potential datasets of interest. We sorted the obtained datasets by the number of samples (High to Low), age, gender, and for clinical data made available by the authors. Because of the few PMF studies, only two datasets (GSE53482, GSE41812,) were selected. A total of 78 samples (16 healthy control and 62 PMF patients) were analyzed. Data sample collection are available in Table 1. Supplementary information of the sample recruited are available in Series Matrix File (s).
Table 1.
Dataset information.
The GSE53482 (platform GPL13667), was composed of Peripheral Blood (PB) CD34+ Cells from 16 healthy donors and 42 PMF patients (23 PMF patients carrying the mutation JAK2V617F and 19 JAK2 wild-type samples) [74]. We selected data from GSE41812 (platform GPL13667) relative to PB CD34+ cells of 20 PMF patients (11 carrying the mutation JAK2V617F, and 9 were wild-type) [75].
4.2. Data Processing and Experimental Design
In order to process and identify Significantly Different Expressed Genes (SDEG) in all selected datasets, we used the MultiExperiment Viewer (MeV) software (The Institute for Genomic Research (TIGR), J. Craig Venter Institute, La Jolla, USA). In cases where multiple genes probes insisted on the same GeneID, we used those with the highest variance. The significance threshold level for all data sets was p < 0.05. The genes with p < 0.05 were identified as SDEG and selected for further analysis. For all datasets we performed a statistical analysis with GEO2R, applying a Benjamini & Hochberg (False discovery rate) to adjust p values for multiple comparisons [42,76,77,78].
From all datasets, we performed a comparison analysis of significantly expressed genes in PB CD34+ Cells from PMF patients carrying the mutation JAK2V617F compared to JAK2 wild-type PMF patients. We obtained 1278 upregulated and 2070 downregulated genes (Supplementary Table S1) in JAK2V617F mutated patients compared to JAK2 wild-type. The genes ontology analysis was performed using the web utility GeneMANIA [79] and GHATER (Gene Annotation Tool to Help Explain Relationships) [80] (Supplementary Table S1).
4.3. Statistical Analysis
For statistical analysis, Prism 8 software (GraphPad Software, La Jolla, CA, USA) was used. Based on Shapiro–Wilk test, almost all data were skewed, so nonparametric tests were used. Significant differences between groups were assessed using the Mann–Whitney U test, and Kruskal–Wallis test was performed to compare data between all groups followed by Dunn’s post hoc test. Correlations were determined using Spearman’s ρ correlation. All tests were two-sided and significance was determined at p < 0.05. The analysis of microarray data by Z-score transformation was used in order to allow the comparison of microarray data independent of the original hybridization intensities [81]. Raw intensity data for each experiment is log10 transformed and then used for the calculation of Z scores. Z scores are calculated by subtracting the overall average gene intensity (within a single experiment) from the raw intensity data for each gene, and dividing that result by the SD of all of the measured intensities, according to the formula:
| Z score (intensity G—mean intensity G1. Gn)/SDG1. Gn | (1) |
where G is any gene on the microarray and G1. Gn represent the aggregate measure of all of the genes [82].
The GSEA were expressed in weighted percentage and FDR as log10(2^-FDR) and graphically rendered in a circular diagram format using freely available CIRCOS software (Canada’s Michael Smith Genome Sciences Centre, Vancouver, Canada) [83]. CIRCOS can be applied to the exploration of data sets involving complex relationships between large numbers of factors.
Diagnostic accuracies were tested in logistic regression models separately for PMF versus healthy and PMF mutated versus PMF wild type. All models were evaluated for significance of the included biomarkers, overall diagnostic accuracy (area under the receiver operator characteristics curve, AUC), and overall fit penalized for the number of predictors (Akaike information criterion, AIC). Differences between AUCs were calculated in a bootstrap procedure with resampling (B = 1000 iterations).
5. Conclusions
Circulating CD34+ cells have a differential gene expression signature in PMF patients carrying the JAK2V617F mutation, involving a dysregulation in immunoproteasome and class I HLA genes that could affect the interactions between neoplastic cells and the microenvironment. Further in-depth analysis looking at the type of antigens carried by the MHCs class I in the circulating CD34+ cells could disclose how the involvement of the IPs pathways can affect the clinical outcome of PMF.
Acknowledgments
We would like to show our gratitude to the authors of microarray datasets (GSE53482, GSE41812) made available online, for consultation and re-analysis.
Abbreviations
| c-20S | Proteasomes |
| MM | multiple myeloma |
| IPs | Immunoproteasome |
| TNFα | tumor necrosis factor alpha |
| IFNG | interferon gamma |
| LMP2 or PSMB9 | subunits β1i |
| MECL-1 or PSMB10 | subunits β2i |
| GEO | Gene Expression Omnibus |
| GHATER | Gene Annotation Tool to Help Explain Relationships |
| SDEG | Significantly Different Expressed Genes |
| MeV | MultiExperiment Viewer |
| MHC class I or HLA class I | Major Histocompatibility Complex class I |
| Th | helper T cell |
| TAP1 and TAP2 | Transporter associated with Antigen Processing 1 and 2 |
| PB | Peripheral Blood |
Supplementary Materials
Supplementary materials can be found at https://www.mdpi.com/1422-0067/21/8/2926/s1.
Author Contributions
Conceptualization, M.D.R., C.G., G.A.P.; methodology, M.D.R., D.T., G.M., I.B.; software, M.D.R.; validation, M.D.R., G.A.P. and G.M.; formal analysis, M.D.R., R.I., P.C., D.T.; investigation, M.D.R., A.R., D.T.; data curation, M.D.R., D.T., I.B., G.L.V.; writing—original draft preparation, M.D.R., C.G., A.R., R.I., P.C., G.L.V., G.A.P.; supervision, M.D.R., G.A.P. Please turn to the CRediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Arber D.A., Orazi A., Hasserjian R., Thiele J., Borowitz M.J., Le Beau M.M., Bloomfield C.D., Cazzola M., Vardiman J.W. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–2405. doi: 10.1182/blood-2016-03-643544. [DOI] [PubMed] [Google Scholar]
- 2.Arber D.A. The 2016 WHO classification of acute myeloid leukemia: What the practicing clinician needs to know. Semin. Hematol. 2019;56:90–95. doi: 10.1053/j.seminhematol.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Baxter E.J., Scott L.M., Campbell P.J., East C., Fourouclas N., Swanton S., Vassiliou G.S., Bench A.J., Boyd E.M., Curtin N., et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365:1054–1061. doi: 10.1016/S0140-6736(05)71142-9. [DOI] [PubMed] [Google Scholar]
- 4.Klampfl T., Gisslinger H., Harutyunyan A.S., Nivarthi H., Rumi E., Milosevic J.D., Them N.C., Berg T., Gisslinger B., Pietra D., et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. N. Engl. J. Med. 2013;369:2379–2390. doi: 10.1056/NEJMoa1311347. [DOI] [PubMed] [Google Scholar]
- 5.Pikman Y., Lee B.H., Mercher T., McDowell E., Ebert B.L., Gozo M., Cuker A., Wernig G., Moore S., Galinsky I., et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 2006;3:e270. doi: 10.1371/journal.pmed.0030270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palumbo G.A., Stella S., Pennisi M.S., Pirosa C., Fermo E., Fabris S., Cattaneo D., Iurlo A. The Role of New Technologies in Myeloproliferative Neoplasms. Front. Oncol. 2019;9:321. doi: 10.3389/fonc.2019.00321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tefferi A., Guglielmelli P., Lasho T.L., Gangat N., Ketterling R.P., Pardanani A., Vannucchi A.M. MIPSS70+ Version 2.0: Mutation and Karyotype-Enhanced International Prognostic Scoring System for Primary Myelofibrosis. J. Clin. Oncol. 2018;36:1769–1770. doi: 10.1200/JCO.2018.78.9867. [DOI] [PubMed] [Google Scholar]
- 8.Guglielmelli P., Lasho T.L., Rotunno G., Mudireddy M., Mannarelli C., Nicolosi M., Pacilli A., Pardanani A., Rumi E., Rosti V., et al. MIPSS70: Mutation-Enhanced International Prognostic Score System for Transplantation-Age Patients With Primary Myelofibrosis. J. Clin. Oncol. 2018;36:310–318. doi: 10.1200/JCO.2017.76.4886. [DOI] [PubMed] [Google Scholar]
- 9.Tefferi A., Guglielmelli P., Nicolosi M., Mannelli F., Mudireddy M., Bartalucci N., Finke C.M., Lasho T.L., Hanson C.A., Ketterling R.P., et al. GIPSS: Genetically inspired prognostic scoring system for primary myelofibrosis. Leukemia. 2018;32:1631–1642. doi: 10.1038/s41375-018-0107-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barosi G., Viarengo G., Pecci A., Rosti V., Piaggio G., Marchetti M., Frassoni F. Diagnostic and clinical relevance of the number of circulating CD34(+) cells in myelofibrosis with myeloid metaplasia. Blood. 2001;98:3249–3255. doi: 10.1182/blood.V98.12.3249. [DOI] [PubMed] [Google Scholar]
- 11.Vannucchi A.M., Kantarjian H.M., Kiladjian J.J., Gotlib J., Cervantes F., Mesa R.A., Sarlis N.J., Peng W., Sandor V., Gopalakrishna P., et al. A pooled analysis of overall survival in COMFORT-I and COMFORT-II, 2 randomized phase III trials of ruxolitinib for the treatment of myelofibrosis. Haematologica. 2015;100:1139–1145. doi: 10.3324/haematol.2014.119545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bjorn M.E., Hasselbalch H.C. The impact of ruxolitinib treatment on inflammation-mediated comorbidities in myelofibrosis and related neoplasms. Clin. Case Rep. 2015;3:499–503. doi: 10.1002/ccr3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Padron E., Dezern A., Andrade-Campos M., Vaddi K., Scherle P., Zhang Q., Ma Y., Balasis M.E., Tinsley S., Ramadan H., et al. A Multi-Institution Phase I Trial of Ruxolitinib in Patients with Chronic Myelomonocytic Leukemia (CMML) Clin. Cancer Res. 2016;22:3746–3754. doi: 10.1158/1078-0432.CCR-15-2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kvasnicka H.M., Thiele J., Bueso-Ramos C.E., Sun W., Cortes J., Kantarjian H.M., Verstovsek S. Long-term effects of ruxolitinib versus best available therapy on bone marrow fibrosis in patients with myelofibrosis. J. Hematol. Oncol. 2018;11:42. doi: 10.1186/s13045-018-0585-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasselbalch H.C. Chronic inflammation as a promotor of mutagenesis in essential thrombocythemia, polycythemia vera and myelofibrosis. A human inflammation model for cancer development? Leuk Res. 2013;37:214–220. doi: 10.1016/j.leukres.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 16.Parker B.S., Rautela J., Hertzog P.J. Antitumour actions of interferons: Implications for cancer therapy. Nat. Rev. Cancer. 2016;16:131–144. doi: 10.1038/nrc.2016.14. [DOI] [PubMed] [Google Scholar]
- 17.Silver R.T., Kiladjian J.J., Hasselbalch H.C. Interferon and the treatment of polycythemia vera, essential thrombocythemia and myelofibrosis. Expert Rev. Hematol. 2013;6:49–58. doi: 10.1586/ehm.12.69. [DOI] [PubMed] [Google Scholar]
- 18.Eran Z., Zingariello M., Bochicchio M.T., Bardelli C., Migliaccio A.R. Novel strategies for the treatment of myelofibrosis driven by recent advances in understanding the role of the microenvironment in its etiology. F1000Res. 2019;8 doi: 10.12688/f1000research.18581.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Craiu A., Gaczynska M., Akopian T., Gramm C.F., Fenteany G., Goldberg A.L., Rock K.L. Lactacystin and clasto-lactacystin beta-lactone modify multiple proteasome beta-subunits and inhibit intracellular protein degradation and major histocompatibility complex class I antigen presentation. J. Biol. Chem. 1997;272:13437–13445. doi: 10.1074/jbc.272.20.13437. [DOI] [PubMed] [Google Scholar]
- 20.Miller Z., Ao L., Kim K.B., Lee W. Inhibitors of the immunoproteasome: Current status and future directions. Curr. Pharm. Des. 2013;19:4140–4151. doi: 10.2174/1381612811319220018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Field-Smith A., Morgan G.J., Davies F.E. Bortezomib (Velcadetrade mark) in the Treatment of Multiple Myeloma. Ther. Clin. Risk Manag. 2006;2:271–279. doi: 10.2147/tcrm.2006.2.3.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tibullo D., Di Rosa M., Giallongo C., La Cava P., Parrinello N.L., Romano A., Conticello C., Brundo M.V., Saccone S., Malaguarnera L., et al. Bortezomib modulates CHIT1 and YKL40 in monocyte-derived osteoclast and in myeloma cells. Front. Pharmacol. 2015;6:226. doi: 10.3389/fphar.2015.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang W., Lin X., Xu H., Sun W., Bouta E.M., Zuscik M.J., Chen D., Schwarz E.M., Xing L. Attenuated Joint Tissue Damage Associated With Improved Synovial Lymphatic Function Following Treatment With Bortezomib in a Mouse Model of Experimental Posttraumatic Osteoarthritis. Arthritis Rheumatol. 2019;71:244–257. doi: 10.1002/art.40696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mohty M., Brissot E., Savani B.N., Gaugler B. Effects of bortezomib on the immune system: A focus on immune regulation. Biol Blood Marrow Transplant. 2013;19:1416–1420. doi: 10.1016/j.bbmt.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 25.Szychlinska M.A., Trovato F.M., Di Rosa M., Malaguarnera L., Puzzo L., Leonardi R., Castrogiovanni P., Musumeci G. Co-Expression and Co-Localization of Cartilage Glycoproteins CHI3L1 and Lubricin in Osteoarthritic Cartilage: Morphological, Immunohistochemical and Gene Expression Profiles. Int J. Mol. Sci. 2016;17:359. doi: 10.3390/ijms17030359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kane R.C., Bross P.F., Farrell A.T., Pazdur R. Velcade: U.S. FDA approval for the treatment of multiple myeloma progressing on prior therapy. Oncologist. 2003;8:508–513. doi: 10.1634/theoncologist.8-6-508. [DOI] [PubMed] [Google Scholar]
- 27.Noda C., Tanahashi N., Shimbara N., Hendil K.B., Tanaka K. Tissue distribution of constitutive proteasomes, immunoproteasomes, and PA28 in rats. Biochem. Biophys. Res. Commun. 2000;277:348–354. doi: 10.1006/bbrc.2000.3676. [DOI] [PubMed] [Google Scholar]
- 28.Malaguarnera L., Imbesi R., Di Rosa M., Scuto A., Castrogiovanni P., Messina A., Sanfilippo S. Action of prolactin, IFN-gamma, TNF-alpha and LPS on heme oxygenase-1 expression and VEGF release in human monocytes/macrophages. Int Immunopharmacol. 2005;5:1458–1469. doi: 10.1016/j.intimp.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 29.Kammerl I.E., Meiners S. Proteasome function shapes innate and adaptive immune responses. Am. J. Physiol. Lung Cell Mol. Physiol. 2016;311:L328–L336. doi: 10.1152/ajplung.00156.2016. [DOI] [PubMed] [Google Scholar]
- 30.Shin E.C., Seifert U., Kato T., Rice C.M., Feinstone S.M., Kloetzel P.M., Rehermann B. Virus-induced type I IFN stimulates generation of immunoproteasomes at the site of infection. J. Clin. Invest. 2006;116:3006–3014. doi: 10.1172/JCI29832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hallermalm K., Seki K., Wei C., Castelli C., Rivoltini L., Kiessling R., Levitskaya J. Tumor necrosis factor-alpha induces coordinated changes in major histocompatibility class I presentation pathway, resulting in increased stability of class I complexes at the cell surface. Blood. 2001;98:1108–1115. doi: 10.1182/blood.V98.4.1108. [DOI] [PubMed] [Google Scholar]
- 32.Boes B., Hengel H., Ruppert T., Multhaup G., Koszinowski U.H., Kloetzel P.M. Interferon gamma stimulation modulates the proteolytic activity and cleavage site preference of 20S mouse proteasomes. J. Exp. Med. 1994;179:901–909. doi: 10.1084/jem.179.3.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ichikawa H.T., Conley T., Muchamuel T., Jiang J., Lee S., Owen T., Barnard J., Nevarez S., Goldman B.I., Kirk C.J., et al. Beneficial effect of novel proteasome inhibitors in murine lupus via dual inhibition of type I interferon and autoantibody-secreting cells. Arthritis Rheum. 2012;64:493–503. doi: 10.1002/art.33333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Basler M., Dajee M., Moll C., Groettrup M., Kirk C.J. Prevention of experimental colitis by a selective inhibitor of the immunoproteasome. J. Immunol. 2010;185:634–641. doi: 10.4049/jimmunol.0903182. [DOI] [PubMed] [Google Scholar]
- 35.Muchamuel T., Basler M., Aujay M.A., Suzuki E., Kalim K.W., Lauer C., Sylvain C., Ring E.R., Shields J., Jiang J., et al. A selective inhibitor of the immunoproteasome subunit LMP7 blocks cytokine production and attenuates progression of experimental arthritis. Nat. Med. 2009;15:781–787. doi: 10.1038/nm.1978. [DOI] [PubMed] [Google Scholar]
- 36.Al-Homsi A.S., Lai Z., Roy T.S., Kouttab N. Effect of novel proteasome and immunoproteasome inhibitors on dendritic cell maturation, function, and expression of IkappaB and NFkappaB. Transpl. Immunol. 2013;29:1–6. doi: 10.1016/j.trim.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 37.Mesa R.A., Verstovsek S., Rivera C., Pardanani A., Hussein K., Lasho T., Wu W., Tefferi A. Bortezomib therapy in myelofibrosis: A phase II clinical trial. Leukemia. 2008;22:1636–1638. doi: 10.1038/leu.2008.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wagner-Ballon O., Pisani D.F., Gastinne T., Tulliez M., Chaligne R., Lacout C., Aurade F., Villeval J.L., Gonin P., Vainchenker W., et al. Proteasome inhibitor bortezomib impairs both myelofibrosis and osteosclerosis induced by high thrombopoietin levels in mice. Blood. 2007;110:345–353. doi: 10.1182/blood-2006-10-054502. [DOI] [PubMed] [Google Scholar]
- 39.Barrett T., Wilhite S.E., Ledoux P., Evangelista C., Kim I.F., Tomashevsky M., Marshall K.A., Phillippy K.H., Sherman P.M., Holko M., et al. NCBI GEO: Archive for functional genomics data sets--update. Nucleic. Acids. Res. 2013;41:D991–D995. doi: 10.1093/nar/gks1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Musumeci G., Castrogiovanni P., Barbagallo I., Tibullo D., Sanfilippo C., Nunnari G., Pellicano G.F., Pavone P., Caltabiano R., Di Marco R., et al. Expression of the OAS Gene Family Is Highly Modulated in Subjects Affected by Juvenile Dermatomyositis, Resembling an Immune Response to a dsRNA Virus Infection. Int. J. Mol. Med. 2018;19:2786. doi: 10.3390/ijms19092786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanfilippo C., Pinzone M.R., Cambria D., Longo A., Palumbo M., Di Marco R., Condorelli F., Nunnari G., Malaguarnera L., Di Rosa M. OAS Gene Family Expression Is Associated with HIV-Related Neurocognitive Disorders. Mol. Neurobiol. 2018;55:1905–1914. doi: 10.1007/s12035-017-0460-3. [DOI] [PubMed] [Google Scholar]
- 42.Fagone P., Nunnari G., Lazzara F., Longo A., Cambria D., Distefano G., Palumbo M., Nicoletti F., Malaguarnera L., Di Rosa M. Induction of OAS gene family in HIV monocyte infected patients with high and low viral load. Antiviral. Res. 2016;131:66–73. doi: 10.1016/j.antiviral.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 43.Malaguarnera L., Nunnari G., Di Rosa M. Nuclear import sequence identification in hOAS3 protein. Inflamm. Res. 2016;65:895–904. doi: 10.1007/s00011-016-0972-8. [DOI] [PubMed] [Google Scholar]
- 44.Scarpino M., Pinzone M.R., Di Rosa M., Madeddu G., Foca E., Martellotta F., Schioppa O., Ceccarelli G., Celesia B.M., d’Ettorre G., et al. Kidney disease in HIV-infected patients. Eur. Rev. Med. Pharmacol. Sci. 2013;17:2660–2667. [PubMed] [Google Scholar]
- 45.McCarthy M.K., Malitz D.H., Molloy C.T., Procario M.C., Greiner K.E., Zhang L., Wang P., Day S.M., Powell S.R., Weinberg J.B. Interferon-dependent immunoproteasome activity during mouse adenovirus type 1 infection. Virol. 2016;498:57–68. doi: 10.1016/j.virol.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Niewerth D., Kaspers G.J., Assaraf Y.G., van Meerloo J., Kirk C.J., Anderl J., Blank J.L., van de Ven P.M., Zweegman S., Jansen G., et al. Interferon-gamma-induced upregulation of immunoproteasome subunit assembly overcomes bortezomib resistance in human hematological cell lines. J. Hematol. Oncol. 2014;7:7. doi: 10.1186/1756-8722-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gaczynska M., Rock K.L., Goldberg A.L. Gamma-interferon and expression of MHC genes regulate peptide hydrolysis by proteasomes. Nat. 1993;365:264–267. doi: 10.1038/365264a0. [DOI] [PubMed] [Google Scholar]
- 48.Kalim K.W., Basler M., Kirk C.J., Groettrup M. Immunoproteasome subunit LMP7 deficiency and inhibition suppresses Th1 and Th17 but enhances regulatory T cell differentiation. J. Immunol. 2012;189:4182–4193. doi: 10.4049/jimmunol.1201183. [DOI] [PubMed] [Google Scholar]
- 49.Basler M., Mundt S., Bitzer A., Schmidt C., Groettrup M. The immunoproteasome: A novel drug target for autoimmune diseases. Clin. Exp. Rheumatol. 2015;33:S74–S79. [PubMed] [Google Scholar]
- 50.Tefferi A., Vaidya R., Caramazza D., Finke C., Lasho T., Pardanani A. Circulating interleukin (IL)-8, IL-2R, IL-12, and IL-15 levels are independently prognostic in primary myelofibrosis: A comprehensive cytokine profiling study. J. Clin. Oncol. 2011;29:1356–1363. doi: 10.1200/JCO.2010.32.9490. [DOI] [PubMed] [Google Scholar]
- 51.Panteli K.E., Hatzimichael E.C., Bouranta P.K., Katsaraki A., Seferiadis K., Stebbing J., Bourantas K.L. Serum interleukin (IL)-1, IL-2, sIL-2Ra, IL-6 and thrombopoietin levels in patients with chronic myeloproliferative diseases. Br. J. Haematol. 2005;130:709–715. doi: 10.1111/j.1365-2141.2005.05674.x. [DOI] [PubMed] [Google Scholar]
- 52.Macedo L.C., de Cesare Quintero F., Pagliari E.S.S., Pagnano K.B., Rodrigues C., de Alencar J.B., Sell A.M., Visentainer J.E. Association of TNF polymorphisms with JAK2 (V617F) myeloproliferative neoplasms in Brazilian patients. Blood Cells Mol. Dis. 2016;57:54–57. doi: 10.1016/j.bcmd.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 53.Guglielmelli P., Zini R., Bogani C., Salati S., Pancrazzi A., Bianchi E., Mannelli F., Ferrari S., Le Bousse-Kerdiles M.C., Bosi A., et al. Molecular profiling of CD34+ cells in idiopathic myelofibrosis identifies a set of disease-associated genes and reveals the clinical significance of Wilms’ tumor gene 1 (WT1) Stem. Cells. 2007;25:165–173. doi: 10.1634/stemcells.2006-0351. [DOI] [PubMed] [Google Scholar]
- 54.Calura E., Pizzini S., Bisognin A., Coppe A., Sales G., Gaffo E., Fanelli T., Mannarelli C., Zini R., Norfo R., et al. A data-driven network model of primary myelofibrosis: Transcriptional and post-transcriptional alterations in CD34+ cells. Blood Cancer J. 2016;6:e439. doi: 10.1038/bcj.2016.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Steunou V., Le Bousse-Kerdiles M.C., Colin-Micouin A., Clay D., Chevillard S., Martyre M.C., French I.R.N.o.M.M.M. Altered transcription of the stem cell leukemia gene in myelofibrosis with myeloid metaplasia. Leukemia. 2003;17:1998–2006. doi: 10.1038/sj.leu.2403089. [DOI] [PubMed] [Google Scholar]
- 56.Pennucci V., Zini R., Norfo R., Guglielmelli P., Bianchi E., Salati S., Sacchi G., Prudente Z., Tenedini E., Ruberti S., et al. Associazione Italiana per la Ricerca sul Cancro Gruppo Italiano Malattie Mieloproliferative, I., Abnormal expression patterns of WT1-as, MEG3 and ANRIL long non-coding RNAs in CD34+ cells from patients with primary myelofibrosis and their clinical correlations. Leuk. Lymphoma. 2015;56:492–496. doi: 10.3109/10428194.2014.910661. [DOI] [PubMed] [Google Scholar]
- 57.Dao T., Korontsvit T., Zakhaleva V., Jarvis C., Mondello P., Oh C., Scheinberg D.A. An immunogenic WT1-derived peptide that induces T cell response in the context of HLA-A*02:01 and HLA-A*24:02 molecules. Oncoimmunol. 2017;6:e1252895. doi: 10.1080/2162402X.2016.1252895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stetka J., Vyhlidalova P., Lanikova L., Koralkova P., Gursky J., Hlusi A., Flodr P., Hubackova S., Bartek J., Hodny Z., et al. Addiction to DUSP1 protects JAK2V617F-driven polycythemia vera progenitors against inflammatory stress and DNA damage, allowing chronic proliferation. Oncogene. 2019;38:5627–5642. doi: 10.1038/s41388-019-0813-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tefferi A. Primary myelofibrosis: 2019 update on diagnosis, risk-stratification and management. Am. J. Hematol. 2018;93:1551–1560. doi: 10.1002/ajh.25230. [DOI] [PubMed] [Google Scholar]
- 60.Keohane C., Kordasti S., Seidl T., Perez Abellan P., Thomas N.S., Harrison C.N., McLornan D.P., Mufti G.J. JAK inhibition induces silencing of T Helper cytokine secretion and a profound reduction in T regulatory cells. Br. J. Haematol. 2015;171:60–73. doi: 10.1111/bjh.13519. [DOI] [PubMed] [Google Scholar]
- 61.Elli E.M., Barate C., Mendicino F., Palandri F., Palumbo G.A. Mechanisms Underlying the Anti-inflammatory and Immunosuppressive Activity of Ruxolitinib. Front. Oncol. 2019;9:1186. doi: 10.3389/fonc.2019.01186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barosi G. An immune dysregulation in MPN. Curr. Hematol. Malig. Rep. 2014;9:331–339. doi: 10.1007/s11899-014-0227-0. [DOI] [PubMed] [Google Scholar]
- 63.Maekawa T., Osawa Y., Izumi T., Nagao S., Takano K., Okada Y., Tachi N., Teramoto M., Kawamura T., Horiuchi T., et al. Myeloproliferative leukemia protein activation directly induces fibrocyte differentiation to cause myelofibrosis. Leukemia. 2017;31:2709–2716. doi: 10.1038/leu.2017.112. [DOI] [PubMed] [Google Scholar]
- 64.Yao Y., Li L., Yang S.H., Gao C.Y., Liao L.H., Xie Y.Q., Yin X.Y., Yang Y.Q., Fei Y.Y., Lian Z.X. CD8(+) T cells and IFN-gamma induce autoimmune myelofibrosis in mice. J. Autoimmun. 2018;89:101–111. doi: 10.1016/j.jaut.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 65.Skov V., Riley C.H., Thomassen M., Kjaer L., Stauffer Larsen T., Bjerrum O.W., Kruse T.A., Hasselbalch H.C. The impact of interferon-alpha2 on HLA genes in patients with polycythemia vera and related neoplasms. Leuk. Lymphoma. 2017;58:1914–1921. doi: 10.1080/10428194.2016.1262032. [DOI] [PubMed] [Google Scholar]
- 66.Tibullo D., Longo A., Vicario N., Romano A., Barbato A., Di Rosa M., Barbagallo I., Anfuso C.D., Lupo G., Gulino R., et al. Ixazomib Improves Bone Remodeling and Counteracts sonic Hedgehog signaling Inhibition Mediated by Myeloma Cells. Cancers (Basel) 2020;12:323. doi: 10.3390/cancers12020323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zahr A.A., Salama M.E., Carreau N., Tremblay D., Verstovsek S., Mesa R., Hoffman R., Mascarenhas J. Bone marrow fibrosis in myelofibrosis: Pathogenesis, prognosis and targeted strategies. Haematologica. 2016;101:660–671. doi: 10.3324/haematol.2015.141283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wehenkel M., Ban J.O., Ho Y.K., Carmony K.C., Hong J.T., Kim K.B. A selective inhibitor of the immunoproteasome subunit LMP2 induces apoptosis in PC-3 cells and suppresses tumour growth in nude mice. Br. J. Cancer. 2012;107:53–62. doi: 10.1038/bjc.2012.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Keller I.E., Vosyka O., Takenaka S., Kloss A., Dahlmann B., Willems L.I., Verdoes M., Overkleeft H.S., Marcos E., Adnot S., et al. Regulation of immunoproteasome function in the lung. Sci. Rep. 2015;5:10230. doi: 10.1038/srep10230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cabrera C.M., Jimenez P., Cabrera T., Esparza C., Ruiz-Cabello F., Garrido F. Total loss of MHC class I in colorectal tumors can be explained by two molecular pathways: Beta2-microglobulin inactivation in MSI-positive tumors and LMP7/TAP2 downregulation in MSI-negative tumors. Tissue Antigens. 2003;61:211–219. doi: 10.1034/j.1399-0039.2003.00020.x. [DOI] [PubMed] [Google Scholar]
- 71.Kaur G., Batra S. Emerging role of immunoproteasomes in pathophysiology. Immunol. Cell Biol. 2016;94:812–820. doi: 10.1038/icb.2016.50. [DOI] [PubMed] [Google Scholar]
- 72.McCarthy M.K., Weinberg J.B. The immunoproteasome and viral infection: A complex regulator of inflammation. Front. Microbiol. 2015;6:21. doi: 10.3389/fmicb.2015.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Clough E., Barrett T. The Gene Expression Omnibus Database. Methods Mol. Biol. 2016;1418:93–110. doi: 10.1007/978-1-4939-3578-9_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Norfo R., Zini R., Pennucci V., Bianchi E., Salati S., Guglielmelli P., Bogani C., Fanelli T., Mannarelli C., Rosti V., et al. Associazione Italiana per la Ricerca sul Cancro Gruppo Italiano Malattie Mieloproliferative, I., miRNA-mRNA integrative analysis in primary myelofibrosis CD34+ cells: Role of miR-155/JARID2 axis in abnormal megakaryopoiesis. Blood. 2014;124:e21–e32. doi: 10.1182/blood-2013-12-544197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vannucchi A.M., Lasho T.L., Guglielmelli P., Biamonte F., Pardanani A., Pereira A., Finke C., Score J., Gangat N., Mannarelli C., et al. Mutations and prognosis in primary myelofibrosis. Leukemia. 2013;27:1861–1869. doi: 10.1038/leu.2013.119. [DOI] [PubMed] [Google Scholar]
- 76.Xiao J., Cao H., Chen J. False discovery rate control incorporating phylogenetic tree increases detection power in microbiome-wide multiple testing. Bioinformatics. 2017;33:2873–2881. doi: 10.1093/bioinformatics/btx311. [DOI] [PubMed] [Google Scholar]
- 77.Smyth G.K. Linear models and empirical bayes methods for assessing differential expression in microarray experiments. Stat. Appl. Genet. Mol. 2004;3:Article3. doi: 10.2202/1544-6115.1027. [DOI] [PubMed] [Google Scholar]
- 78.Davis S., Meltzer P.S. GEOquery: A bridge between the Gene Expression Omnibus (GEO) and BioConductor. Bioinformatics. 2007;23:1846–1847. doi: 10.1093/bioinformatics/btm254. [DOI] [PubMed] [Google Scholar]
- 79.Zuberi K., Franz M., Rodriguez H., Montojo J., Lopes C.T., Bader G.D., Morris Q. GeneMANIA prediction server 2013 update. Nucleic Acids Res. 2013;41:W115–W122. doi: 10.1093/nar/gkt533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chang J.T., Nevins J.R. GATHER: A systems approach to interpreting genomic signatures. Bioinformatics. 2006;22:2926–2933. doi: 10.1093/bioinformatics/btl483. [DOI] [PubMed] [Google Scholar]
- 81.Cheadle C., Vawter M.P., Freed W.J., Becker K.G. Analysis of microarray data using Z score transformation. J. Mol. Diagn.: JMD. 2003;5:73–81. doi: 10.1016/S1525-1578(10)60455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sanfilippo C., Castrogiovanni P., Imbesi R., Tibullo D., Li Volti G., Barbagallo I., Vicario N., Musumeci G., Di Rosa M. Middle-aged healthy women and Alzheimer’s disease patients present an overlapping of brain cell transcriptional profile. Neurosci. 2019;406:333–344. doi: 10.1016/j.neuroscience.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 83.Krzywinski M., Schein J., Birol I., Connors J., Gascoyne R., Horsman D., Jones S.J., Marra M.A. Circos: An information aesthetic for comparative genomics. Genome Res. 2009;19:1639–1645. doi: 10.1101/gr.092759.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.