Abstract
Active transportation (AT), or walking or bicycling for transportation, represents one way individuals can achieve recommended physical activity (PA) levels. This study describes AT prevalence and temporal trends, and examines associations between AT levels and measured CVD risk factors (hypertension, hypercholesterolemia, low high-density [HDL] cholesterol, diabetes, and obesity) among U.S. adults.
National Health and Nutrition Examination Survey (NHANES) 2007–2016 data (analyzed in 2017) were used to conduct overall trend analyses of reported AT in a typical week [none (0–9 min/week); low (10–149 min/week); or high (≥150 min/week)]. Logistic regression was used to examine associations between AT level and each CVD risk factor from NHANES 2011–2016 (n = 13,943). Covariates included age, sex, race/Hispanic origin, education, income, smoking, survey cycle, non-transportation PA, and urbanization level.
U.S. adults who engaged in high AT levels increased from 13.1% in 2007–2008 to 17.9% in 2011–2012, and then decreased to 10.6% in 2015–2016 (p for quadratic trend = 0.004). Over the same period, the quadratic trend for low AT was not significant. During 2011–2016, 14.3% of adults engaged in high AT, 11.4% in low AT, and 74.4% in no AT. High AT levels were associated with decreased odds of each CVD risk factor assessed, compared to no AT. Low AT (versus no AT) was associated with decreased odds of hypertension (aOR = 0.77, 95% CI 0.64, 0.91) and diabetes (aOR = 0.68, 95% CI 0.54, 0.85).
AT prevalence among adults has fluctuated from 2007 to 2016. Despite favorable associations between AT and CVD risk factors, most U.S. adults do not engage in any AT.
Keywords: Active transportation, Walking, Bicycling, Cardiovascular disease
1. Introduction
Regular physical activity (PA) can reduce the risk of developing several chronic diseases, including cardiovascular disease (CVD), and also reduces the risk of early mortality (U.S. Department of Health and Human Services, 2008; Physical Activity Guidelines Advisory Committee, 2008). PA is often categorized into four domains based on the location or purpose of activity, including leisure, domestic, occupational, and transportation (Craig et al., 2003; World Health Organization). Active transportation (AT) is defined as any self-propelled human-powered mode of transportation, which primarily includes walking or bicycling. AT is increasingly recognized as one of many ways individuals can achieve recommended PA levels outlined in the 2008 National PA Guidelines (U.S. Department of Health and Human Services, 2008; United States Department of Health and Human Services, 2015; U.S. Department of Health and Human Services, 2015; Centers for Disease Control and Prevention, 2011), which encourage adults to engage in ≥150 min of moderate-intensity PA per week (Physical Activity Guidelines Advisory Committee, 2008; Furie and Desai, 2012).
To promote population-based AT, several national initiatives and priorities have recently emerged (U.S. Department of Health and Human Services, 2008; United States Department of Health and Human Services, 2015; U.S. Department of Health and Human Services, 2015; Centers for Disease Control and Prevention, 2011). These include, but are not limited to, AT-related objectives that are outlined in Healthy People 2020, such as PA-13 (Increase the proportion of trips made by walking) and PA-14 (Increase the proportion of trips made by bicycling), and the 2015 Surgeon General’s Call to Action to Promote Walking and Walkable Communities (United States Department of Health and Human Services, 2015; U.S. Department of Health and Human Services, 2015). The Surgeon General’s report promotes walking across multiple PA domains, including transportation, and encourages communities to improve access to safe and convenient places to walk, bike, use a wheelchair, and be active in other ways (U.S. Department of Health and Human Services, 2015). In 2016, the U.S. Community Preventive Services Task Force determined there was sufficient evidence on the association between the built environment and AT to recommend built environment strategies to improve pedestrian and bicycle transportation systems, and land use and environmental design interventions to encourage PA (Centers for Disease Control and Prevention, 2017a). Despite these national initiatives and priorities to promote AT among individuals and in communities, data from various national surveillance systems have demonstrated inconsistent trends in the prevalence of AT among adults (Whitfield et al., 2015).
Few studies to date have described the health benefits of AT among U.S. adults (Furie and Desai, 2012; Gordon-Larsen et al., 2009; Boone-Heinonen et al., 2009). To our knowledge, only one study has reported significant associations between AT and measured CVD risk factors (Furie and Desai, 2012). Using nationally representative data from 2007 to 2010, the investigators found that adults engaging in AT had lower odds of hypertension and diabetes. Additionally, adults engaging in AT had a lower body mass index (BMI) and smaller waist circumference (Furie and Desai, 2012).
However, it is unknown whether national initiatives and priorities implemented over the past several years have influenced the uptake and prevalence of AT. Furthermore, the associations between AT and CVD health previously reported could be examined with a wider array of measured outcomes (Furie and Desai, 2012). The objectives of this study were to (1) describe the prevalence of and assess trends in AT among adults (≥20 years) using data from the National Health and Nutrition Examination Survey (NHANES) over five cycles (2007–2008, 2009–2010, 2011–2012, 2013–2014, and 2015–2016) and (2) to comprehensively examine the associations between AT levels and measured CVD risk factors from the most recent NHANES cycles (2011–2016).
2. Methods
The NHANES is a nationally representative survey of the U.S. civilian, non-institutionalized population with a complex, multistage sampling design. Since 1999, NHANES has operated continuously and data are released in 2-year cycles. Participants completed in-home interviews and physical examinations in a mobile examination center. NHANES was approved by the National Center for Health Statistics (NCHS) Research Ethics Review Board and written informed consent was obtained from participants. Additional details are available elsewhere (Centers for Disease Control and Prevention, 2012; Centers for Disease Control and Prevention, 2014).
2.1. Study sample
In 2007, a measurement change was made to assess AT on the NHANES physical activity questionnaire, which has also resulted in improved concordance with the 2008 PA Guidelines for Americans (U.S. Department of Health and Human Services, 2008; Physical Activity Guidelines Advisory Committee, 2008). Therefore, we examined trends using data from adults aged ≥20 years from the 2007–2016 NHANES cycles. The unweighted interview response rate ranged from 64.3% to 72.9% (National Center for Health Statistics, 2017).
Interview and examination data from the 2011–2016 NHANES cycles (16,381 adults aged ≥20 years) were analyzed to examine whether previously observed associations between AT and CVD risk factors remained robust (Furie and Desai, 2012). The examination response rate for this age group was 62.6% in 2011–2012, 63.7% in 2013–2014, and 54.8% in 2015–2016 (National Center for Health Statistics, 2017). Participants who were pregnant (n = 192) or reported physical mobility limitations (needing special equipment to walk, much difficulty or inability to walk for ¼ mile, or much difficulty or inability to walk up to ten steps without resting, n = 2225) were excluded from analysis, yielding an initial analytic sample of 13,964 adults. Participants missing data for AT level (n = 21) were further excluded, resulting in a final analytic sample of 13,943 adults.
Participants missing responses for one or more CVD risk factors were excluded from the specific analysis for that risk factor; 378 individuals were excluded from the hypertension analysis (2.7% missing from analytic sample), 638 individuals were excluded from the hypercholesterolemia analysis (4.6%), 743 individuals were excluded from the low HDL cholesterol analysis (5.3%), 554 individuals were excluded from the diabetes analysis (4.0%), and 89 individuals were excluded from the analysis on obesity (0.6%).
2.2. Measures
2.2.1. Dependent variables
Hypertension was defined as measured systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or self-reported current use of hypertension medication, according to hypertension guideline recommendations in effect through 2016 (Bakris et al., 2015). Hypercholesterolemia was defined as serum total cholesterol ≥240 mg/dL or self-reported current use of cholesterol-lowering medication. Low HDL cholesterol was defined as serum HDL cholesterol < 40 mg/dL. Diabetes was defined as self-reported physician diagnosis of diabetes or hemoglobin A1c ≥6.5%. Obesity was defined as BMI (measured weight in kilograms divided by measured height in meters squared) ≥30.
2.2.2. Independent variables
The main independent variable was level of AT, or walking or bicycling for transportation. As part of the NHANES physical activity questionnaire, participants were asked “Do you walk or use a bicycle for at least 10 minutes continuously to get to and from places?” (e.g., to work, for shopping, to school). Only participants responding yes were then asked “In a typical week, on how many days do you walk or bicycle for at least 10 minutes continuously to get to and from places?” and “How much time do you spend walking or bicycle for travel on a typical day?” (Centers for Disease Control and Prevention, 2012; Centers for Disease Control and Prevention, 2014) Minutes/week were calculated by multiplying the number of days/week on which AT was reported by the number of minutes/day. AT levels were categorized for the entire sample as none (0–9 min/week, which includes participants who responded “no” to the first question asking “Do you walk or use a bicycle for at least 10 min continuously to get to and from places?”), low (10–149 min/week), or high (≥150 min/week). The categories reflect the 2008 aerobic PA Guidelines (Physical Activity Guidelines Advisory Committee, 2008; Furie and Desai, 2012). NHANES does not assess self-reported intensity of AT.
Other covariates (selected a priori based on previous research (Furie and Desai, 2012; Gordon-Larsen et al., 2009; Berger et al., 2017)) included the following self-reported characteristics: age group (20–39, 40–59, ≥60 years), sex (male or female), race/Hispanic origin (Hispanic, non-Hispanic white, non-Hispanic black, and non-Hispanic Asian), highest level of education attained by participant (< high school, high school, some college, ≥college), poverty income ratio (a measure of family income to poverty guidelines specific to survey year), smoking status (never smoked, former smoker, current smoker), survey cycle (2011–2012, 2013–2014, and 2015–2016), non-transportation PA, and urbanization level.
Non-transportation PA was assessed separately from AT with participant report of the combined frequency and duration of all other PA domains excluding AT assessed in the NHANES physical activity questionnaire. This included moderate leisure activity, vigorous leisure activity, moderate work activity, and vigorous work activity in a typical week. Minutes of moderate-intensity PA for leisure and work were combined with vigorous-intensity PA for leisure and work to estimate total non-transportation PA. Vigorous-intensity minutes for non-transportation PA were multiplied by 2 to achieve an equivalent combination of moderate-and vigorous-intensity PA (U.S. Department of Health and Human Services, 2008; Physical Activity Guidelines Advisory Committee, 2008). Combined minutes were categorized as none (0–9 min/week), low (10–149 min/week), or high (≥150 min/week). Domestic PA, or carrying out household chores, was assessed within the vigorous-and moderate-intensity work-related PA items (World Health Organization; Centers for Disease Control and Prevention, 2017a, 2017b).
Urbanization level was categorized according to the 2006 (for NHANES 2011–2012) and 2013 (for NHANES 2013–2014) NCHS Urban-Rural Classification Scheme for Counties (six categories ranging from highly urbanized metropolitan to remote rural areas) based on respondent county of residence. However, the updated schemes were not yet available for 2015–2016. Therefore, urbanization level was assigned to each 2015–2016 NHANES participant based on county location of the NHANES primary sampling unit (PSU) available through CDC’s Research Data Center. Unweighted agreement between urbanization level based on county of residence for NHANES 2007–2016 and county location for the PSU for NHANES 2015–2016 was 99.9%. For this analysis, urbanization level was collapsed into the following three categories: urban (large central metropolitan); suburban (large fringe metropolitan, medium metropolitan, and small metropolitan); and rural (micropolitan and noncore).
2.3. Statistical analysis
Trends from 2007 to 2016 in the proportion of adults who reported high AT levels (≥150 min/week) and low AT levels (10–149 min/week) were assessed using orthogonal polynomial contrasts. Chi-square tests were used to examine the bivariate associations of demographic characteristics with AT level. Separate multivariable logistic regression models were used to examine relationships between AT level and each CVD risk factor. All models were adjusted for age group, sex, race/Hispanic origin, education, poverty income ratio, smoking, survey cycle, non-transportation PA, and urbanization level. Statistical significance was defined as α-level of 0.05. Analyses were conducted in 2017 using SAS (version 9.4) and SUDAAN (version 11.0.1) to account for the complex survey design (Centers for Disease Control and Prevention, 2013a). Trend analyses incorporated interview sampling weights. All other analyses incorporated examination sampling weights (Centers for Disease Control and Prevention, 2013b).
3. Results
Fig. 1 presents AT prevalence among adults aged ≥20 years who were interviewed in the 2007–2016 NHANES cycles and responded affirmatively to engaging in at least 10 min of AT in a typical week. For adults engaging in at least 10 min of AT in a typical week, the prevalence of high AT (≥150 min/week) increased from 13.1% in 2007–2008 to 17.9% in 2011–2012, and then decreased in 2015–2016 to 10.6%, suggesting a statistically significant quadratic trend (p = 0.004), or a nonlinear trend in the data over time (e.g., change in direction). No significant trend for low AT was observed (p = 0.069 for quadratic trend).
Fig. 1.
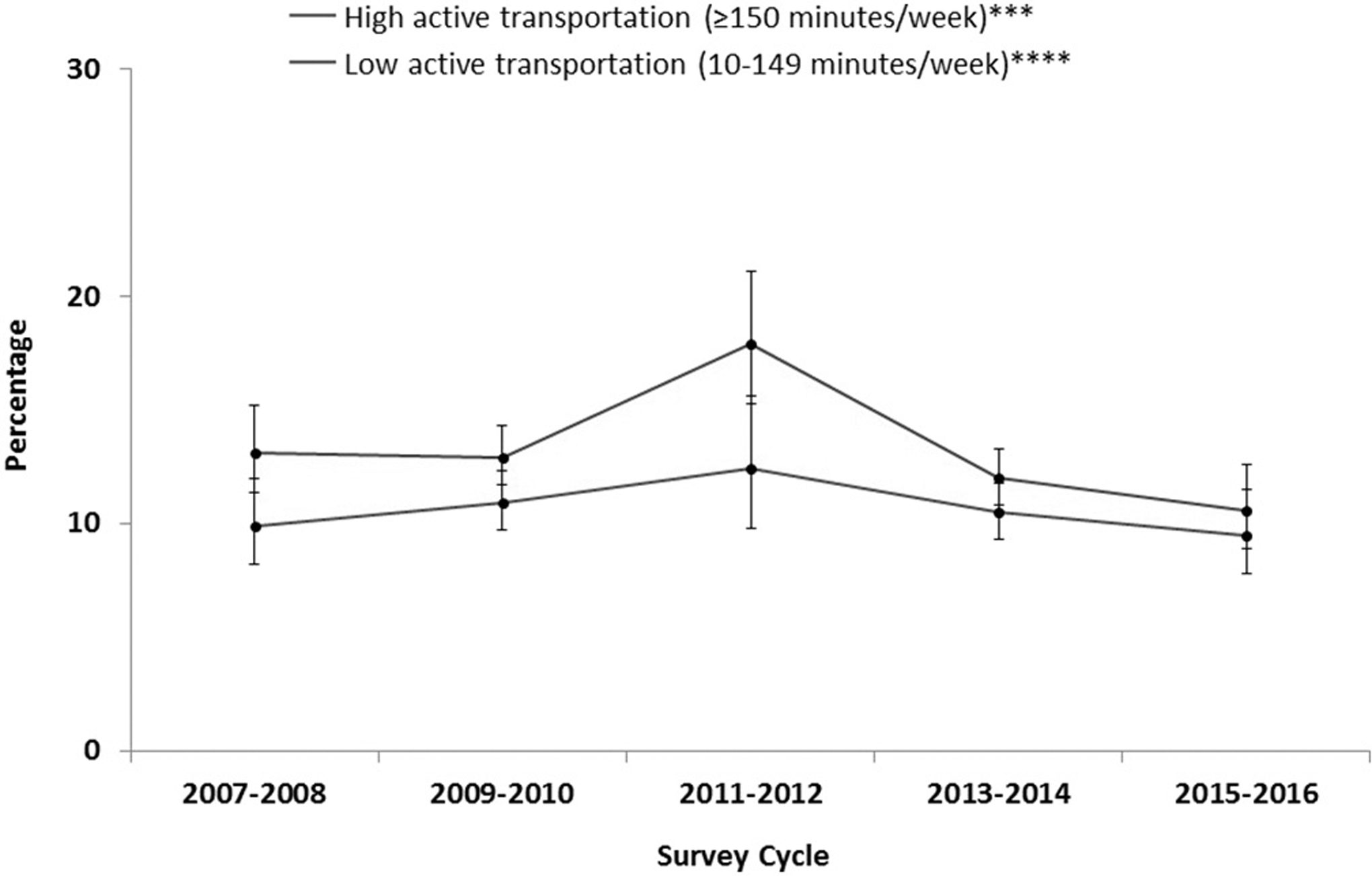
Active transportation prevalence* among adults ≥20 years**, by survey year – NHANES, 2007–2016.
*With 95% confidence intervals indicated with error bars.
**Analytic sample includes adults aged ≥20 years who were interviewed in the 2007–2016 NHANES cycles and responded affirmatively to “Do you walk or use a bicycle for at least 10 minutes continuously to get to and from places?” (e.g., to work, for shopping, to school).
***Based on the following questions: “In a typical week, on how many days do you walk or bicycle for at least 10 minutes continuously to get to and from places?” and “How much time do you spend walking or bicycling for travel on a typical day?” Minutes/week were calculated by multiplying the number of days/week on which active transportation was reported by the number of minutes/day and active transportation levels were categorized to reflect the 2008 aerobic PA Guideline recommendations. High active transportation was categorized as ≥150 min of moderate-intensity PA per week.
****Based on the following questions: “In a typical week, on how many days do you walk or bicycle for at least 10 minutes continuously to get to and from places?” and “How much time do you spend walking or bicycling for travel on a typical day?” Minutes/week were calculated by multiplying the number of days/week on which active transportation was reported by the number of minutes/day and active transportation levels were categorized to reflect the 2008 aerobic PA Guideline recommendations. Low active transportation was categorized as 10–149 min of moderate-intensity PA per week.
Note: Significant quadratic trends found for high active transportation at p < 0.05.
Source: CDC/NCHS. National Health and Nutrition Examination Survey Data. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2007–2016. Available at http://www.cdc.gov/nchs/nhanes.htm.
Table 1 presents descriptive characteristics of U.S. adults aged ≥20 years who were examined in the most recent NHANES cycles (2011–2016) by AT level. The majority of adults (74.4%) did not walk or bike for > 10 min for transportation in a typical week, 11.4% engaged in low AT levels, and 14.3% engaged in high AT levels. Compared to the percentages of adults who reported no AT, higher percentages of adults who engaged in low and high levels of AT were younger, male, reported a race/Hispanic origin other than non-Hispanic white, less educated, lower income, were current smokers, met national PA guidelines from non-transportation PA, and resided in urban areas. The prevalence of CVD risk factors—hypertension, hypercholesterolemia, low HDL cholesterol, diabetes, and obesity—generally decreased with increasing AT level.
Table 1.
Characteristicsa by active transportation (AT) level in adults aged ≥20 years in the United States, 2011–2016.
| Characteristic | Total | AT level | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No AT (0–9 min/week) | Low AT (10–149 min/week) | High AT (≥ 150 min/week) | |||||||
| n | % (SE) | n | % (SE) | n | % (SE) | n | % (SE) | ||
| All, n | 13,943 | 100.0 (0.0) | 10,083 | 74.4 (1.3) | 1674 | 11.4 (0.7) | 2186 | 14.3 (0.7) | |
| Age (years) | < 0.001 | ||||||||
| 20–39 | 5285 | 38.7 (1.1) | 3569 | 35.8 (0.9) | 766 | 46.6 (2.1) | 950 | 47.9 (2.4) | |
| 40–59 | 4866 | 38.0 (0.8) | 3599 | 39.2 (0.7) | 565 | 37.3 (1.8) | 702 | 32.7 (1.6) | |
| ≥ 60 | 3792 | 23.3 (0.7) | 2915 | 25.1 (0.7) | 343 | 16.2 (1.3) | 534 | 19.4 (1.8) | |
| Sex | < 0.001 | ||||||||
| Male | 6927 | 49.6 (0.4) | 4871 | 48.0 (0.5) | 821 | 50.0 (1.5) | 1235 | 57.4 (1.4) | |
| Female | 7016 | 50.4 (0.4) | 5212 | 52.0 (0.5) | 853 | 50.0 (1.5) | 951 | 42.6 (1.4) | |
| Race/Hispanic originb | 0.004 | ||||||||
| Hispanic | 3420 | 15.1 (1.5) | 2457 | 14.6 (1.5) | 404 | 16.0 (2.1) | 559 | 17.0 (1.8) | |
| Non-Hispanic White | 5118 | 65.3 (2.1) | 3884 | 67.0 (2.1) | 565 | 61.9 (3.1) | 669 | 59.6 (2.9) | |
| Non-Hispanic Black | 3073 | 11.0 (1.1) | 2158 | 10.5 (1.1) | 384 | 12.2 (1.4) | 531 | 12.8 (1.6) | |
| Non-Hispanic Asian | 1913 | 5.8 (0.6) | 1303 | 5.4 (0.6) | 263 | 6.9 (0.9) | 347 | 7.0 (0.8) | |
| Education level | < 0.001 | ||||||||
| < High school | 2902 | 14.0 (1.0) | 1989 | 13.3 (0.9) | 344 | 13.9 (1.5) | 569 | 17.8 (1.8) | |
| High school | 2970 | 20.3 (0.7) | 2204 | 21.5 (0.8) | 325 | 16.1 (1.1) | 441 | 17.7 (1.2) | |
| Some college | 4266 | 32.5 (0.9) | 3124 | 32.8 (0.8) | 506 | 30.9 (1.8) | 636 | 32.3 (2.2) | |
| ≥ College | 3802 | 33.1 (1.5) | 2765 | 32.4 (1.5) | 499 | 39.2 (2.5) | 538 | 32.1 (2.4) | |
| Poverty income ratio categoryc | < 0.001 | ||||||||
| Lowest (< 130%) | 3983 | 20.0 (1.0) | 2614 | 17.8 (1.0) | 586 | 25.0 (1.8) | 783 | 27.6 (2.4) | |
| Middle (130%- < 350%) | 4648 | 32.5 (0.9) | 3537 | 34.1 (1.0) | 462 | 27.0 (1.8) | 649 | 29.0 (1.6) | |
| Highest (≥ 350%) | 4110 | 40.7 (1.6) | 3114 | 41.6 (1.6) | 459 | 41.1 (2.7) | 537 | 36.0 (2.2) | |
| Missing | 1202 | 6.7 (0.4) | 818 | 6.6 (0.4) | 167 | 7.0 (0.6) | 217 | 7.3 (0.7) | |
| Smoking status | 0.002 | ||||||||
| Never | 8262 | 57.8 (0.7) | 5964 | 57.4 (0.7) | 1031 | 61.1 (2.1) | 1267 | 57.1 (1.5) | |
| Former | 2991 | 23.4 (0.7) | 2285 | 24.4 (0.7) | 310 | 20.5 (1.7) | 396 | 20.6 (1.4) | |
| Current | 2676 | 18.8 (0.6) | 1824 | 18.2 (0.7) | 331 | 18.5 (1.4) | 521 | 22.4 (1.2) | |
| Non-transportation PAd | < 0.001 | ||||||||
| None (0–9 min/week) | 4084 | 24.5 (0.6) | 3022 | 25.5 (0.7) | 460 | 22.5 (1.3) | 602 | 21.1 (1.0) | |
| Low (10–149 min/week) | 1812 | 13.3 (0.3) | 1372 | 13.8 (0.4) | 261 | 15.4 (1.2) | 179 | 9.0 (1.0) | |
| High (2150 min/week) | 8007 | 62.2 (0.7) | 5660 | 60.7 (0.8) | 947 | 62.1 (1.9) | 1400 | 69.9 (1.4) | |
| Urbanization levele | |||||||||
| Urban | 5246 | 31.0 (4.1) | 3374 | 27.2 (3.9) | 746 | 38.8 (5.5) | 1126 | 44.3 (5.6) | < 0.001 |
| Suburban | 6519 | 51.0 (5.5) | 5023 | 53.6 (5.6) | 710 | 47.2 (6.2) | 786 | 40.5 (5.8) | |
| Rural | 2178 | 18.0 (3.3) | 1686 | 19.2 (3.9) | 218 | 14.0 (2.4) | 274 | 15.2 (2.0) | |
| Cardiovascular disease risk factor | |||||||||
| Hypertensive (n = 13,565) | 4409 | 29.2 (0.7) | 3410 | 31.4 (0.7) | 395 | 21.7 (1.4) | 604 | 23.8 (1.6) | < 0.001 |
| Hypercholesterolemia (n = 13,305) | 3620 | 27.7 (0.6) | 2776 | 28.9 (0.6) | 374 | 23.9 (1.7) | 470 | 21.1 (1.4) | < 0.001 |
| Low HDL cholesterol (n = 13,200) | 2440 | 18.2 (0.6) | 1818 | 18.8 (0.6) | 283 | 17.2 (1.5) | 339 | 15.7 (1.1) | 0.019 |
| Diabetic (n = 13,389) | 1863 | 10.3 (0.4) | 1439 | 11.4 (0.5) | 178 | 6.8 (0.7) | 246 | 7.6 (0.6) | < 0.001 |
| Obesity (n = 13,854) | 4931 | 35.5 (0.8) | 3773 | 37.5 (0.8) | 562 | 33.4 (1.9) | 596 | 26.7 (1.4) | < 0.001 |
Source: CDC/NCHS. National Health and Nutrition Examination Survey.
Note: Analytic sample includes non-pregnant adults aged 20 years or older who participated in both the interview and mobile examination center and reported no physical mobility limitations. Bold denotes statistical significance at p < 0.05. AT, active transportation; SE, standard error.
Estimates (except sample size) are weighted using examination survey weights and standard error is calculated accounting for complex survey design.
Persons of “Other” race/Hispanic origin were included in analysis, but percentages are not shown separately.
Poverty status categories based on family income-to-poverty ratio.
Non-transportation PA: calculated from the average minutes/week participants reported participating in moderate-or vigorous-intensity PA in a typical week for leisure and work, where vigorous PA was doubled and added to moderate PA to compute an equivalent combination of moderate and vigorous PA. Minutes/week were categorized as None = 0–9 min/week; Low = 10–149 min/week; High = ≥150 min/week.
Urbanization level based on 2013 National Center for Health Statistics Urban-Rural Classification Scheme for Counties: Urban = residing in large central metro county; Suburban = residing in large fringe metro, medium metro, or small metro county; Rural = residing in a micropolitan or non-core county.
Table 2 presents the unadjusted and adjusted results from the multivariable logistic regression models examining the associations between AT level and each CVD risk factor. Adjustment attenuated observed associations for all CVD risk factors, except low HDL cholesterol. While attenuated, the adjusted associations between high AT levels and all CVD risk factors remained significant. Most of the adjusted associations between low AT levels and the CVD risk factors also remained significant, except for hypercholesterolemia and obesity. After adjustment for all covariates, compared to reporting no AT, engaging in high AT levels was inversely associated with most CVD risk factors including hypertension (aOR = 0.84, 95% CI 0.71, 0.99), hypercholesterolemia (aOR = 0.79, 95% CI 0.64, 0.97), low HDL cholesterol (aOR = 0.70, 95% CI 0.58, 0.85), diabetes (aOR = 0.69, 95% CI 0.56, 0.84), and obesity (aOR = 0. 66, 95% CI 0.58, 0.76). Compared with no AT, low AT was associated with a decreased odds of hypertension (aOR = 0.77, 95% CI 0.64, 0.91) and diabetes (aOR = 0.68, 95% CI 0.54, 0.85).
Table 2.
Associations between active transportation (AT) levela and cardiovascular disease risk factors: U.S., 2011–2016.
| Level of AT | Hypertension (n = 13,565) | Hypercholesterolemia (n = 13,305) | Low HDL cholesterol (n = 13,200) | Diabetes (n = 13,389) | Obesity (n = 13,854) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Unadjusted | ||||||||||
| No AT | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | |||||
| Low AT | 0.61 (0.52, 0.72) | < 0.001 | 0.77 (0.64, 0.93) | 0.009 | 0.89 (0.74, 1.07) | 0.222 | 0.57 (0.46, 0.72) | < 0.001 | 0.83 (0.70, 1.00) | 0.046 |
| High AT | 0.68 (0.57, 0.83) | < 0.001 | 0.66 (0.55, 0.78) | < 0.001 | 0.80 (0.68, 0.94) | 0.008 | 0.64 (0.54, 0.78) | < 0.001 | 0.60 (0.52, 0.70) | < 0.001 |
| Adjustedb | ||||||||||
| No AT | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | |||||
| Low AT | 0.77 (0.64, 0.91) | 0.004 | 0.98 (0.80, 1.21) | 0.883 | 0.86 (0.71, 1.04) | 0.119 | 0.68 (0.54, 0.85) | 0.001 | 0.90 (0.76, 1.08) | 0.251 |
| High AT | 0.84 (0.71, 0.99) | 0.039 | 0.79 (0.64, 0.97) | 0.027 | 0.70 (0.58, 0.85) | 0.001 | 0.69 (0.56, 0.84) | < 0.001 | 0.66 (0.58, 0.76) | < 0.001 |
Note: Analytic sample includes non-pregnant adults aged 20 years or older who participated in both the interview and mobile examination center and reported no physical mobility limitations. Bold denotes statistical significance at p < 0.05. AT, active transportation; HDL, high-density lipoprotein; OR, odds ratio; CI, confidence interval.
Level of AT: None = 0–9 min/week; Low = 10–149 min/week; High = ≥150 min/week.
Models were adjusted for age, sex, race/Hispanic origin, education, poverty, smoking, survey cycle, non-transportation PA, and urbanization level. Reference groups for each logistic regression model: age group: 20–39 years, sex: male, race/Hispanic origin: non-Hispanic white, highest level of education attained by a participant: ≥college, poverty income ratio category: lowest income group (< 130%), smoking status: never smoked, survey cycle: 2015–2016, non-transportation PA: engaged in no PA for leisure or work, and urbanization level: urban.
4. Discussion
The current study described AT prevalence and trends, and examined associations between AT level and a comprehensive set of CVD risk factor measures among a national representative sample of adults aged 20 years and over. Despite the increased attention to AT from several national initiatives implemented or sustained in the past few years (United States Department of Health and Human Services, 2015; U.S. Department of Health and Human Services, 2015; Centers for Disease Control and Prevention, 2017a), we observed a quadratic trend in the prevalence of high AT, with a peak prevalence in 2011–2012, followed by a decline through 2015–2016, which resulted in lower levels to those observed in the beginning of the study period. In an evaluation of AT surveillance data through 2012 across multiple national household health and transportation surveys that utilize a variety of AT measures, AT prevalence from 2007 to 2012 was relatively stable across these varying data sources. This evaluation also included data from NHANES 2007–2012, which was the only data source that showed an increase in 2011–2012 (Whitfield et al., 2015). However, our analysis showed that this increase in 2011–2012 was not sustained and that prevalence of high AT, as measured by NHANES in 2007–2008 and 2015–2016, was similar. In addition to the Call to Action to Promote Walking and Walkable Communities by the Office of the Surgeon General of the U.S. Department of Health and Human Services (U.S. Department of Health and Human Services, 2015), other national multisectoral efforts were made during the current study’s time period to promote AT. The Federal Highway Administration developed a Strategic Agenda for Pedestrian and Bicycle Transportation, which aimed to guide federal pedestrian and bicycle activities (Federal Highway Administration, 2016). In 2016, an update to the National Physical Activity Plan was released by a coalition of organizations across nine sectors to promote walking and walkable communities through crosssector collaborations (National Physical Activity Plan, 2016). The extent to which these previously reported national efforts contributed to the observed trends in this analysis is not known, and more research may be needed to evaluate the effectiveness of national initiatives that promote AT (Centers for Disease Control and Prevention, 2017b).
As with other studies, our results suggested that engaging in AT was more prevalent among adults reporting certain demographic characteristics, specifically adults who were younger, male, Hispanic or non-Hispanic black, within lower education or income groups, meeting PA guidelines through other domains, and residing in urban areas (Furie and Desai, 2012; Whitfield et al., 2015). Continued surveillance of AT over time, using consistent measures, and among diverse population subgroups may inform initiatives to increase AT uptake (Whitfield et al., 2015). Additional surveillance and research may also be needed to monitor neighborhood and environmental features that can support increased AT uptake across these varied population subgroups (U.S. Department of Health and Human Services, 2015; Centers for Disease Control and Prevention, 2017b; Fulton et al., 2016).
Few studies exist that have examined the associations between AT and CVD risk factors among U.S. adults (Furie and Desai, 2012; Gordon-Larsen et al., 2009; Berger et al., 2017), and only one study conducted in 2011 utilized objective measures to assess CVD risk (Furie and Desai, 2012). Using the most recent nationally representative data, we found that high AT levels were associated with a decreased odds of all of the CVD risk factors assessed, including hypertension, hypercholesterolemia, low HDL cholesterol, diabetes, and obesity. Additionally, compared to no AT, adults who engaged in low AT levels had lower odds of having hypertension and diabetes. Furie and Desai used combined NHANES data from 2007 to 2010 and reported inverse associations between AT and hypertension, diabetes, lower BMI, and waist circumference. In contrast to our study’s findings which demonstrated high AT was associated with decreased odds of low HDL cholesterol, the investigators found no significant associations for low HDL cholesterol (Furie and Desai, 2012). Another study by Gordon-Larsen and colleagues investigated associations between walking or bicycling to work and various measured CVD risk factors and serum measures among young adults aged 18–30 years from Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California. They found that active commuting to work was inversely associated with blood pressure, triglyceride levels, insulin level, BMI, and obesity among men (Gordon-larsen et al., 2013). Finally, a study conducted by Berger and colleagues of a convenience sample of adults in Minnesota reported significant associations between bicycling for AT and decreased odds of hypertension and obesity (Berger et al., 2017). While these investigations provide information on the relationships between AT and various CVD risk factors, these studies either did not utilize recent nationally representative data, assessed only younger adults, focused on one mode of AT or only AT for commuting to and from work, or did not adjust for urbanization level. Additionally, some of these studies relied on self-reported measures. Given prior research has demonstrated differences between self-reported and device-based measures when examining associations between total PA and measured CVD risk factors at the national level (Tucker et al., 2016; Atienza et al., 2011), future research may be needed to examine these differences between self-reported and device-based measures of AT and associations with objective CVD outcomes.
The present study’s findings were also consistent with studies published from other countries. In a meta-analysis of eight studies that examined the relationship between active commuting and various CVD risk factors in Europe and Japan (Hamer and Chida, 2008), active commuting demonstrated a protective effect on cardiovascular outcomes, including coronary heart disease (Hu et al., 2007; Wagner et al., 2002), stroke (Hu et al., 2005), hypertension (Barengo et al., 2005; Hayashi et al., 1999), and diabetes (Hu et al., 2003). Similar to the aforementioned studies conducted in the U.S., the studies in the meta-analysis were subject to limitations in that they only considered AT to and from work and did not adjust for urbanization level (Hamer and Chida, 2008).
4.1. Strengths and limitations
Strengths of the current study include the use of data from a nationally representative sample, the use of laboratory and examination measures to define CVD risk factors, adjustment for non-transportation-PA, and the assessment of AT for any purpose rather than only for commuting to work. Our study also has several limitations. Causality cannot be inferred because of the cross-sectional design of the study. We combined three cycles of NHANES data (2011–2016) to improve the stability of the prevalence estimates of adults who engaged in high and low AT levels. While the prevalence of high AT changed over that time period, the associations between AT and CVD risk factors were similar to those observed in a study in the previous period (2007–2010) (Furie and Desai, 2012). The measure for AT was self-reported, which may have introduced recall and social desirability bias. The measure also does not distinguish between walking and bicycling separately, so we could not assess whether there were differences by mode of transport. Additionally, the intensity at which AT was performed was not assessed. Further, the exclusion of participants with missing data for the dependent variables could bias results. However, a low percentage of eligible participants were excluded for missing responses (the dependent variable with the highest percentage of missing data was low HDL cholesterol, 5.3%), and excluding missing data when the rate of missingness is < 10% is generally less likely to result in bias than including a separate missing category (Knol et al., 2010).
5. Conclusions
The current study revealed fluctuating trends in AT prevalence from 2007 to 2016, and inverse associations between AT and certain CVD risk factors in recent years. Despite the potential health benefits and national recommendations that have identified AT as one of many ways individuals can achieve recommended PA levels (U.S. Department of Health and Human Services, 2008; Physical Activity Guidelines Advisory Committee, 2008; United States Department of Health and Human Services, 2015), the majority of U.S. adults do not engage in any AT. After increasing through 2012, the prevalence of high AT has since declined to levels comparable to those in 2007–2008. These results may inform public health research designed to promote AT, such as those outlined in the Surgeon General’s Call to Action to Promote Walking and Walkable Communities (U.S. Department of Health and Human Services, 2015) and the Guide to Community Preventive Services (Centers for Disease Control and Prevention, 2017a).
Acknowledgments
We acknowledge Yutaka Aoki and Craig Hales for their assistance with data management and analysis of the urbanization level variable.
Footnotes
Conflict of interest statement
No conflicts of interest were reported by the authors of this paper.
Financial disclosure
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The findings and conclusions in this report are those of the authors and not necessarily the official position of the Centers for Disease Control and Prevention.
References
- Atienza AA, Moser RP, Perna F, et al. , 2011. Self-reported and objectively measured activity related to biomarkers using NHANES. Med. Sci. Sports Exerc 815–821. [DOI] [PubMed] [Google Scholar]
- Bakris GL, Black HR, Cushman WC, et al. , 2015. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment. J. Am. Med. Assoc 289 (19), 2560–2573. [DOI] [PubMed] [Google Scholar]
- Barengo NC, Hu G, Kastarinen M, et al. , 2005. Low physical activity as a predictor for antihypertensive drug treatment in 25–64-year-old populations in eastern and south-western Finland. J. Hypertens 23 (2), 293–299. [DOI] [PubMed] [Google Scholar]
- Berger AT, Qian XL, Pereira MA, 2017. Associations between bicycling for transportation and cardiometabolic risk factors among Minneapolis-Saint Paul area commuters: a cross-sectional study in working-age adults. Am. J. Health Promot 32 (3), 631–637. [DOI] [PubMed] [Google Scholar]
- Boone-Heinonen J, Jacobs DR, Sidney S, Sternfeld B, Lewis CE, Gordon-Larsen P, 2009. A walk (or cycle) to the park: active transit to neighborhood amenities, the CARDIA study. Am. J. Prev. Med 37 (4), 285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2011. Transportation Health Impact Assessment Toolkit Atlanta, GA: http://www.cdc.gov/healthyplaces/transportation/promote_strategy.htm. [Google Scholar]
- Centers for Disease Control and Prevention, 2012. National Health and Nutrition Examination Surveys: NHANES 2011–2012 https://wwwn.cdc.gov/Nchs/Nhanes/ContinuousNhanes/Default.aspx?BeginYear=2011, Accessed date: 9 February 2017 (Published).
- Centers for Disease Control and Prevention, 2013a. NHANES Sample Design https://www.cdc.gov/nchs/tutorials/nhanes/SurveyDesign/SampleDesign/intro.htm, Accessed date: 2 August 2018 (Published).
- Centers for Disease Control and Prevention, 2013b. NHANES Weighting https://www.cdc.gov/nchs/tutorials/NHANES/SurveyDesign/Weighting/intro.htm, Accessed date: 2 August 2018 (Published).
- Centers for Disease Control and Prevention, 2014. National Health and Nutrition Examination Surveys: NHANES 2013–2014 https://wwwn.cdc.gov/Nchs/Nhanes/ContinuousNhanes/Default.aspx?BeginYear=2013, Accessed date: 9 February 2017 (Published).
- Centers for Disease Control and Prevention, 2017a. The Community Guide: Physical Activity and Built Environment Approaches https://www.thecommunityguide.org/findings/physical-activity-built-environment-approaches, Accessed date: 9 February 2017 (Published).
- Centers for Disease Control and Prevention, 2017b. Status Report for Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities Atlanta, GA: https://www.cdc.gov/physicalactivity/walking/call-to-action/pdf/status-report.pdf. [Google Scholar]
- Centers for Disease Control and Prevention, 2017a. National Health and Nutrition Examination Survey, 2013–2014 Physical Activity Questionnaire Documentation
- Centers for Disease Control and Prevention, 2017b. National Health and Nutrition Examination Survey, 2011–2012 Physical Activity Questionnaire Documentation
- Craig CL, Marshall AL, Sjöström M, et al. , 2003. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc 35 (8), 1381–1395. [DOI] [PubMed] [Google Scholar]
- Federal Highway Administration, 2016. Strategic Agenda for Pedestrian and Bicycle Transportation https://www.fhwa.dot.gov/environment/bicycle_pedestrian/publications/strategic_agenda/, Accessed date: 2 August 2018 (Published).
- Fulton JE, Carlson SA, Ainsworth BE, et al. , 2016. Strategic priorities for physical activity surveillance in the United States. Med. Sci. Sports Exerc 9, 2057–2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furie GL, Desai MM, 2012. Active transportation and cardiovascular disease risk factors in U.S. adults. Am. J. Prev. Med 43 (6), 621–628. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Boone-Heinonen J, Sidney S, 2009. Active commuting and cardiovascular disease risk: the CARDIA study. Arch. Intern. Med 169 (13), 1216–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-larsen P, Boone-heinonen J, Sidney S, Sternfeld B, Jacobs D, Lewis CE, 2013. Active commuting and cardiovascular disease risk. Arch. Intern. Med 169 (13), 1216–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M, Chida Y, 2008. Active commuting and cardiovascular risk: a meta-analytic review. Prev. Med 46 (1), 9–13. [DOI] [PubMed] [Google Scholar]
- Hayashi T, Tsumura K, Suematsu C, Okada K, Fujii S, Endo G, 1999. Walking to work and the risk for hypertension in men: the Osaka health survey. Ann. Intern. Med 131 (1), 21–26. [DOI] [PubMed] [Google Scholar]
- Hu G, Qiao Q, Silventoinen K, et al. , 2003. Occupational, commuting, and leisure-time physical activity in relation to risk for Type 2 diabetes in middle-aged Finnish men and women. Diabetologia 46 (3), 322–329. [DOI] [PubMed] [Google Scholar]
- Hu G, Sarti C, Jousilahti P, Silventoinen K, Barengo NC, Tuomilehto J, 2005. Leisure time, occupational, and commuting physical activity and the risk of stroke. Stroke 36 (9), 1994–1999. [DOI] [PubMed] [Google Scholar]
- Hu G, Jousilahti P, Borodulin K, et al. , 2007. Occupational, commuting and leisure-time physical activity in relation to coronary heart disease among middle-aged Finnish men and women. Atherosclerosis 194 (2), 490–497. [DOI] [PubMed] [Google Scholar]
- Knol MJ, Janssen KJM, Donders ART, et al. , 2010. Unpredictable bias when using the missing indicator method or complete case analysis for missing confounder values: an empirical example. J. Clin. Epidemiol 63 (7), 728–736. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics, 2017. NHANES Response Rates and Population Totals https://www.cdc.gov/nchs/nhanes/response_rates_cps.htm, Accessed date: 18 May 2017 (Published).
- National Physical Activity Plan, 2016. U.S. National Physical Activity Plan http://www.physicalactivityplan.org/NationalPhysicalActivityPlan.pdf, Accessed date: 2 August 2018 (Published).
- Physical Activity Guidelines Advisory Committee, 2008. Physical Activity Guidelines Advisory Committee Report Washington, DC.. [Google Scholar]
- Tucker JM, Welk GJ, Beyler NK, Kim Y, 2016. Associations between physical activity and metabolic syndrome: comparison between self-report and accelerometry. Am. J. Health Promot 30 (3), 155–163. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2008. 2008. Physical Activity Guidelines for Americans Washington, DC.. [Google Scholar]
- U.S. Department of Health and Human Services, 2015. Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities Washington, DC.. [PubMed] [Google Scholar]
- United States Department of Health and Human Services, 2015. Healthy People 2020 Physical Activity Objectives http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=33 (Published).
- Wagner A, Simon C, Evans A, et al. , 2002. Physical activity and coronary event incidence in Northern Ireland and France the prospective epidemiological study of myocardial infarction (PRIME). Circulation 105 (19), 2247–2252. [DOI] [PubMed] [Google Scholar]
- Whitfield GP, Paul P, Wendel AM, 2015. Active transportation surveillance - United States, 1999–2012. MMWR Surveill. Summ 64 (Suppl 7(7)), 1–17. [PubMed] [Google Scholar]
- World Health Organization, 2010. Global Recommendations on Physical Activity for Health [PubMed]


