Abstract
Aim
Advance care planning (ACP) is a strategy to align future care and treatment with preferences of patients and families. This study assesses the experiences of ACP among paediatricians caring for children with life‐limiting conditions.
Methods
Paediatricians from five Dutch university hospitals and the national oncology centre completed a survey during May to September 2017, which investigated experiences with ACP in their most recent case of a deceased child and with ACP in general.
Results
A total of 207 paediatricians responded (36%). After exclusion of responses with insufficient data (n = 39), 168 were analysed (29%). These included experiences with an individual case in 86%. ACP themes were discussed with parents in all cases. Topics common to many cases were diagnosis, life expectancy, care goals, the parent's fears and code status. ACP conversations occurred with children in 23% of cases. The joy in living was the most frequent topic. The frequency of ACP conversations was insufficient according to 49% of the respondents. In 60%, it was stated that ACP has to result in a documented code status.
Conclusion
Paediatricians reported having ACP conversations mainly with parents focusing on medical issues. There was limited insight into the child's preferences for care and treatment.
Keywords: advance care planning, communication, paediatric palliative care, shared decision‐making
Abbreviation
- ACP
Advance care planning
Key Notes.
We surveyed 168 paediatricians about their experiences with advance care planning (ACP) in their most recent case of a child who died, and with ACP in general.
Among paediatricians who reported on a case (86%), indicated discussions on ACP themes were mainly with parents focusing on the medical domain.
Few paediatricians reported having had ACP conversations with children. Thus, the child's preferences were unclear in most cases.
1. INTRODUCTION
Medical and technological advances have increased the chances of survival among seriously ill children, resulting in a growing population of children living with life‐limiting conditions.1 These children and their families receive complex chronic and palliative care. As such, they often need support in communicating with the medical team and in medical decision‐making.2 Parents feel that adequate medical decision‐making, designed to serve the best interest of their child, is a central element of their parenting role.3 Clinicians in paediatrics need to identify individual parental wishes and needs in order to be able to support parents in caring for their child until the end of life.4 Medical associations emphasise the importance of anticipating future care and care decisions for children with life‐limiting conditions.5, 6 In 2017, an international panel of experts in palliative care defined advance care planning (ACP), a supportive strategy to identify, discuss and document preferences and goals for future treatment and care in collaboration with family and healthcare providers.7 Although research on paediatric ACP is still in its infancy, growing evidence suggests that healthcare providers and families value the concept of ACP.8, 9 In adult medicine, a growing body of evidence suggests that ACP improves the quality of end of life care and contributes to preferences‐concordant care in various patient populations and countries.10 Physicians in adult medicine recognise the importance of ACP, but encounter barriers such as a lack of knowledge and the discontinuity of care.11 A single centre paediatric study from the United States showed that paediatricians in intensive care medicine and oncology felt prepared to conduct ACP discussions. They perceived parental factors, such as, unrealistic expectations, understanding of the prognosis and readiness to have the conversation, as the most significant barriers.12, 13 It is largely unknown whether these results can be generally applied to European countries, because specific healthcare contexts influence attitudes and medical decision‐making.14 Besides that, it is unknown whether general paediatricians and other subspecialties have similar experiences and skills. In the Netherlands, the concept of ACP is not well known among paediatricians, although we hypothesised that they integrate elements of ACP in their daily practice. Insight into paediatricians’ actual experiences with ACP, or elements of ACP, is essential to inform a systematic development of programmes and policies to support further implementation of ACP in paediatrics and to develop strategies to overcome perceived barriers. Therefore, we invited university hospital paediatricians, both in general and from all subspecialties, plus those from the Dutch national oncology centre, to share their experiences, attitudes and skills regarding ACP. We aimed to identify how paediatricians intergrate elements of ACP in their daily practice and how paediatricians envisage the concept of ACP in general.
2. METHODS
2.1. Study population
From May to September 2017, we performed an observational cross‐sectional online survey of paediatricians providing tertiary care for children, under the age of 18, with a life‐limiting or life‐threatening disease. All seven university paediatric care centres in the Netherlands were invited to participate. Two centres refused to participate for reasons unknown. Five participated in the study: the Amalia Children's Hospital, Nijmegen; the Beatrix Children's Hospital, Groningen; the Emma Children's Hospital, Amsterdam; the Sophia Children's Hospital, Rotterdam and the Wilhelmina Children's Hospital, Utrecht. The national oncology centre, the Princess Máxima Centre for Paediatric Oncology, in Utrecht also took part. All paediatricians, including fellows, in active employment in the centres mentioned above were invited to participate. The Participant Information Sheet indicated that the study focused on paediatricians who were the primary providers of care of children under 18 years of age with life‐limiting or life‐threatening diseases. It was up to the participants themselves to decide whether they were eligible for participation or not. Residents in paediatrics were not eligible to participate as they rarely take care of children with life‐limiting conditions without the involvement of a supervisor. All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committees and the Helsinki Declaration and its later amendments. Participants were informed about the study by a separate online page before the survey started. Informed consent was obtained by virtue of completion.
2.2. Data collection
All paediatricians received an invitation by email with a link to the survey via contacts in the centres participating. The survey was conducted using the electronic software NETQ CollectorPremium, Version: 2015.Q2 (Survalyzer BV). A reminder email was sent twice at approximate intervals of three weeks to all non‐responders.
2.3. Survey development
Advance care planning was defined on the introduction page of the survey, since paediatricians in the Netherlands are not familiar with the concept of ACP in general. ACP was defined for this survey as: ‘communication with seriously ill children and their families about the goals and preferences for future medical care and treatment’. We used the theory of planned behaviour to identify which determinants might influence experiences and perspectives regarding ACP among paediatricians.15 The theory of planned behaviour consists of three determinants that influence one's intention to perform certain behaviour. These are as follows: perceived behavioural control; attitudes towards the behaviour; and subjective norms. In order to address those determinants, we asked respondents how they perceive their own communication skills, relevant in ACP, in both their most recent case of a child who subsequently died and in general. In addition, questions were asked about what they expect from ACP and what they perceive as subjective norms for the timing, frequency and content of ACP. The survey was divided into two parts. Part one of the survey explored the ACP experiences of paediatricians in their most recent case of a child who died. The second part concerned the skills, attitudes and perspectives regarding ACP in general. The survey consisted of 73 items and was based on an existing questionnaire12, 13 and items developed from the beginning of the research based on the previous work of the study team.7, 16 An expert panel of five paediatricians performed pilot surveys, which resulted in several linguistic adjustments. (See Appendix S1 for the questionnaire).
2.4. Statistical analysis
Data were analysed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp). The descriptive statistics were reported. Data are reported as means with standard deviations or ranges for quantitative variables, and as frequency distributions for categorical data.
3. RESULTS
Of the 572 paediatricians invited to participate, 207 responded (36%). A total of 39 responses were excluded from further analysis due to incomplete data (<10/73 items) (19%). The characteristics of the remaining 168, out of 572 paediatricians, (29%) are reported in Table 1. A total of 84% of the participants whose responses were analysed had practiced for more than ten years. Nearly one‐third of these physicians worked in general paediatrics (27%).
Table 1.
Respondent characteristics
| Characteristics | Respondents |
|---|---|
| Involved as primary physician until child's death (n = 168), n (%) | |
| Yes | 145 (86) |
| No | 23 (14) |
| Gender (n = 160), n (%) | |
| Female | 102 (64) |
| Male | 58 (36) |
| Mean age (n = 158), years (SD) | 46.0 (± 8.6) |
| Mean working experience (n = 160), years (SD) | 18.3 (±8.8) |
| Working experience (n = 160), n(%) | |
| <10 y | 25 (16) |
| 10‐20 y | 84 (53) |
| >20 ys | 51 (32) |
| Subspecialty (n = 160), n (%) | |
| General paediatrics | 43 (27) |
| Neonatology | 31 (19) |
| Oncology | 25 (16) |
| ICU | 19 (12) |
| Neurology | 12 (8) |
| Other | 74 (46) |
3.1. Experiences with a case of a child who died
Among the responses analysed, 145 paediatricians reported on their most recent case of a child who died after a life‐limiting condition (86%). The case characteristics are presented in Table 2. The majority of cases concerned a child who had died in the past two years (81%). Cancer (16%), neurologic disorders (18%) and conditions originating in the perinatal period (17%) were the most common diagnoses. The respondents had been involved as the child's primary physician for a mean period of 2.2 years (SD ± 3.8). Some respondents, (27%), were involved in all phases of the disease trajectory, from diagnosis to death. In 40% of the cases, children died within their first year of life. In 37%, children died at an age of 1‐12 years, and 23% died at or older than 12 years of age. A hospital was the place of death in 70% of the cases. Children were judged by the respondents to be competent during their disease trajectory in 17% of the cases. These children had a mean age at death of 13.1 years (range 3.9‐18.0, SD ± 4.2). In 42%, these children were aged under 12 at the time of death. The common reasons for being judged incompetent were their young age (55%) and developmental disorders (18%).
Table 2.
Case characteristics
| Characteristics | Children who died |
|---|---|
| Gender (n = 145), n (%) | |
| Male | 88 (61) |
| Female | 57 (39) |
| Year of death (n = 145), n (%) | |
| <2015 | 19 (13) |
| 2015 | 9 (6) |
| 2016 | 37 (26) |
| 2017 | 80 (55) |
| Mean age at death (n = 145), years (SD, range) | 6.0 (±6.2,range 0.0‐18.0) |
| Place of death (n = 145), n (%) | |
| Home | 42 (29) |
| Hospital | 100 (69) |
| Hospice | 2 (1) |
| Elsewhere | 1 (1) |
| Diagnosis (n = 145), n (%) | |
| Neoplasms | 23 (16) |
| Neurologic disorders | 26 (18) |
| Congenital anomalies | 14 (10) |
| Perinatal disorders | 24 (17) |
| Other | 58 (40) |
| Competent (n = 145), n (%) | |
| Yes | 24 (17) |
| No, due to young age | 79 (55) |
| No, due to developmental disorder | 26 (18) |
| No, due to low consciousness | 12 (8) |
| No, due to emotional distress | 2 (1) |
| No, due to other cause | 2 (1) |
| Involvement of respondent as primary physician in … (n = 145), N (%) | |
| Diagnostic phase | 82 (57) |
| Stable phase | 79 (55) |
| Phase of decline | 121 (83) |
| End of life phase | 118 (81) |
| Mean duration of involvement as primary physician (n = 145), years (SD, range) | 2.2 (3.8,range 0.0‐17.0) |
An overview of how ACP was addressed in the cases described is presented in Table 3. Paediatricians discussed one or more topics related to ACP with parents in all cases. Topics commonly discussed with parents were the child's diagnosis (91%), life expectancy (90%), goals of care (87%), fears and worries (87%) and code status (86%). Discussion of ACP themes with children occurred in 23% of the cases. Of these children, 67% were judged to be competent. The children who were not judged as competent, but were still involved in the conversations, had a mean age of 8.9 years (range 2.2‐12.2) at death. With two competent children, none of the topics, previously listed, were discussed. Common topics discussed with children were as follows: their joy of life (19%); their diagnosis (17%); their fears and worries (17%); the goals of care (15%); and their hopes (15%). Location of death (5%) and code status (5%) were the least reported as being discussed with the children.
Table 3.
Elements of ACP in the reported cases
| Elements of ACP | With parents | With children |
|---|---|---|
| Themes discussed (n = 145), n (%) | ||
| Diagnosis | 132 (91) | 25 (17) |
| Life expectancy | 131 (90) | 17 (12) |
| Goals of care and treatment | 126 (87) | 22 (15) |
| Fears and worries | 126 (87) | 25 (17) |
| Code status/treatment limitations | 125 (86) | 7 (5) |
| Future physical functioning | 122 (84) | 15 (10) |
| Symptoms in end of life period | 122 (84) | 10 (7) |
| Coping with feelings of loss | 117 (81) | 15 (10) |
| Social network | 116 (80) | 10 (7) |
| Capacities of the family | 108 (75) | 10 (7) |
| Practical issues daily care | 107 (74) | 12 (8) |
| Hopes | 102 (70) | 21 (15) |
| Location of death | 95 (66) | 7 (5) |
| Child's joy in living | 92 (63) | 28 (19) |
| Future social functioning | 93 (64) | 10 (7) |
| Cases | ||
|---|---|---|
|
Self‐reported documentation of preferences and goals of care in the medical record (n = 145), n (%) | ||
| Yes | 80 (55) | |
| No | 11 (8) | |
| Partial | 54 (37) | |
| Discussions about legal representative (n = 145), n (%) | ||
| Yes, with child | 6 (4) | |
| Yes, with father | 61 (42) | |
| Yes, with mother | 71 (49) | |
| Yes, with someone else | 2 (1) | |
| No | 70 (48) | |
|
Reported documentation of legal representative in the medical record (n = 145), n (%) | ||
| Yes | 60 (41) | |
| No | 85 (59) | |
|
If yes, who was documented as the legal representative in the medical record (n = 60), n (%) | ||
| Both parents | 46 (77) | |
| Father | 2 (3) | |
| Mother | 11 (18) | |
| Someone else | 1 (2) | |
|
Perceived agreement of care with preferences as discussed in conversations (n = 143), n (%) | ||
| Not at all/not really | 7 (5) | |
| Somewhat | 5 (3) | |
| Very much/Totally | 131 (92) | |
| With preferences parents | With preferences child | |
|---|---|---|
|
Perceived agreement of care (n = 145), n (%) | ||
| Not at all/not really | 2(1) | 1 (1) |
| Somewhat | 11 (8) | 1 (1) |
| Very much/Totally | 125 (86) | 36 (25) |
| Unclear | 7 (5) | 107 (74) |
Paediatricians reported that in 92% of the cases, some goals and preferences for future medical treatment and care had been documented in the medical record. An absence of any documentation of goals and preferences for future medical treatment and care in the medical record was reported in 8%. Discussions about whom to identify as the legal representative of the child occurred in 52%. In 41% of all cases, the legal representative was documented in the medical record, being both parents in 77%, and the mother alone in 18% of those cases.
The care provided was perceived as in line with the parent's preferences in 86% of the cases reported. In 5%, the respondents reported it was unclear to them whether the care provided was in line with the parent's preferences. Paediatricians reported that in 25% of cases, they perceived the care provided as in line with the child's preferences. In 74%, they reported the degree of agreement was unclear to them. The care provided was reported as in line with prior ACP conversations in 92%. The paediatricians reported being satisfied with their own role in communicating in 95% of the cases reported.
3.2. Attitudes regarding ACP
Attitudes regarding ACP in general are represented in Table 4. Sixty‐six per cent of the respondents reported that ACP discussions are indicated in all phases of the disease trajectory. The respondents confirmed that ACP can improve the quality of care (97%) and shared decision‐making (98%). They confirmed in 81% that ACP can contribute to the use of palliative care. Twenty‐three per cent of the participants indicated that ACP conversations occur often enough. Sixty per cent of the paediatricians stated that ACP has to result in the documentation of a code status. One‐third (37%) confirmed ACP conversations are mainly intended to inform children and their parents. The majority of physicians (68%) supported the statement that ACP conversations give children and families more control.
Table 4.
Attitudes regarding ACP in general
| Statement | Strongly disagree/disagree | Neutral | Agree/Strongly agree |
|---|---|---|---|
| In current practice, ACP conversations occur often enough (n = 160), n (%) | 79 (49) | 44 (28) | 37 (23) |
| ACP conversations improve the quality of medical care (n = 160), n (%) | 1 (1) | 4 (3) | 155 (97) |
| ACP conversations improve the use of palliative care (n = 160), n (%) | 5 (3) | 25 (16) | 130 (81) |
| ACP conversations have to result in a documented code status or treatment limitations (n = 159), n (%) | 26 (16) | 38 (24) | 95 (60) |
| ACP conversations are intended mainly to inform child/parents (n = 159), n (%) | 58 (36) | 42 (26) | 59 (37) |
| ACP conversations put parents in control (n = 160), n (%) | 9 (6) | 42 (26) | 109 (68) |
| ACP conversations improve shared decision‐making (n = 160), n (%) | 0 (0) | 4 (3) | 156 (98) |
3.3. Barriers and facilitators
The respondents were asked to rate previously stated factors, deemed facilitators of, and barriers to ACP. Uncertainty about life expectancy (24%), the emotional distress of patient and family (24%) and an inability of the child and family to assess their situation (19%), were most commonly indicated as barriers. (Figure 1) Most commonly perceived facilitators were continuity of care by the same physician (97%), the presence of a nurse at ACP conversations (79%) and prior multidisciplinary consultation (74%). (Figure 2).
Figure 1.
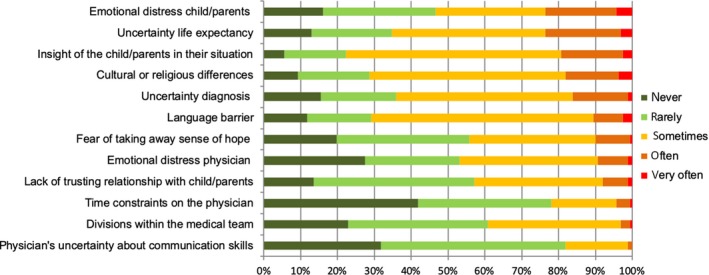
Frequencies of perceived barriers to advance care planning
Figure 2.
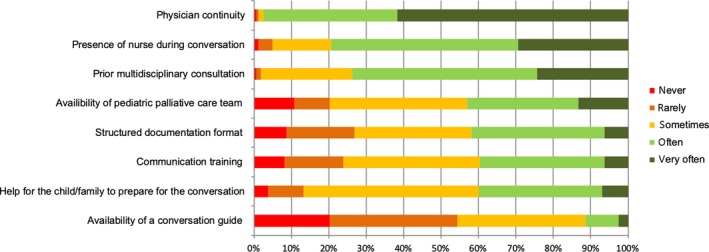
Frequencies of perceived facilitators of advance care planning
3.4. Self‐perception of communication skills
Physicians indicated that they were able to explore, adequately, parent's fears, feelings and expectations in 97% of the responses, to discuss with parents bad news in 96% and code status in 91%. They were also able to explore, adequately, children's fears, feelings and expectations in 63%, discuss bad news with children in 61% and discuss a code status with a child in 52%. (Figure 3) Physicians agreed in 94% that they were also able to check, adequately, the understanding of their conversation partners and to deal with emotions in the conversations in 89%.
Figure 3.
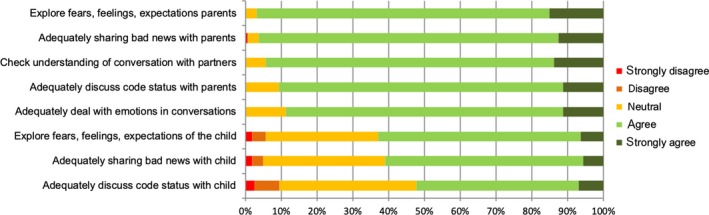
Physicians’ agreements with their ability to demonstrate different communication skills
4. DISCUSSION
To the best of our knowledge, this was the first survey, which evaluated paediatricians’ self‐reported ACP behaviour in actual cases. Our study elicits the following three key issues.
Firstly, although a broad range of ACP topics were reported by the paediatricians as regularly being discussed with parents, their conversations seem to predominantly focus on medical issues. In addition to this, a substantial number of paediatricians believed key elements of ACP were the provision of information and discussion of code status or treatment limitations. This might be a barrier to an early and open exploration of the family's perspective on living with a child's illness and living well. This is including the family's views on physical, psychosocial and spiritual domains. ACP originally focused on the completion of advance directives. But, today, there is consensus that the key elements of ACP are the exploration of personal values and preferences regarding living with an illness, now, or in the future, and sharing of these values and preferences with others.7, 17 It remains unclear whether paediatricians conduct ACP conversations with families in an informative way with a focus on treatment decisions or whether they are able to engage in deeper explorations of the child's and family's underlying individual values and preferences. An analysis of the content of actual ACP conversations might give more insight into their approach.
Secondly, the exploration of the child's perspectives appears to be difficult. In our study, paediatricians reported in the majority of cases to have no insight into whether the child's preferences were in line with the care as provided. ACP conversations with children occurred in a minority of cases. Most children were considered incapable of expressing their wishes due to their young age, or because of developmental issues. However, some children were involved in the conversations about, at least, some topics, even at a very young age and without being considered competent. The involvement of children in ACP and in decision‐making in general is challenging.18 Evidence about interventions to engage children in decisions related to their health is limited. A systematic review identified only five interventions, including one ACP intervention.19 Within the triad of child, parents and healthcare professionals, the perspectives and the best interests of the child need to be identified. It is of pivotal importance to support parents in their role as substitute decision maker, because the child might be unable to present his or her own perspectives and preferences.4 In our sample, the legal representative was explicitly defined in only half of cases and infrequently documented. It seems natural in paediatrics to rely on the parents for decision‐making in the best interest of the child. However, it is known that neither parents nor professionals reflect the voice of the child routinely, and even less in stressful times during the end of life phase.20, 21 Although the vast majority of paediatricians were satisfied with their communications skills with regard to parents, only a small minority of physicians confirmed they had adequate skills to communicate about ACP topics with children. This is supported by findings from literature, where paediatricians felt unprepared for discussing ACP with adolescents or conducting family conferences.12 It is known that parents too feel difficulties in discussing these issues with their children.20
Thirdly, although paediatricians were satisfied with their approach in the cases reported, in their communication skills in general and in particular on the benefits of ACP, only a small minority confirmed ACP conversations occur often enough. This is in line with a retrospective chart review in the United Kingdom, which showed that there was no documentation of any ACP conversation in the medical record of 25% of the children approaching the end of life.22 Other research showed that more than 70% of paediatric clinicians thought that ACP discussions often occur too late.12, 13, 23 An improvement in the frequency and timing of ACP conversations might be challenging. In our sample, paediatricians themselves see barriers to ACP mainly in parental factors. This is in line with earlier findings where parent‐related factors such as unrealistic expectations, a perceived lack of parental readiness to discuss end of life issues and not wanting to burden parents were perceived as key barriers to ACP in paediatrics.8, 13 Research suggests, however, that parents want to be involved in decision‐making and many prefer open, honest and complete information about end of life care.24, 25, 26 They do not, however, always actively search for it.27 Parents consider engagement in ACP important but perceive it as difficult. They need a sensitive, affective, individualised and gradual approach, with room for patterns of hopeful thinking.9, 28 The perceived facilitators of ACP were mainly associated with the healthcare professional, with a focus on a team‐based approach. This is consistent with earlier research, which showed clinicians prefer to discuss end of life decisions within a medical team prior to conversations with parents.29
These key issues might indicate that interventions to support ACP in paediatrics need to focus on education about the concept of ACP and about the involvement of the child in ACP. In addition, physicians might need more insight into the background of perceived parental barriers to ACP. These barriers are persistently reported by physicians, even though parents themselves report clear preferences to ACP. The integration of multidisciplinary approaches, such as multidisciplinary consultations prior to ACP conversations, and involving different professions in the conversation itself, might be valued by paediatricians and might support them to engage in ACP more often.
This study had some strengths and limitations. The invitation to participate in this survey study was sent to all paediatricians working in the hospitals participating in order to prevent selection bias based on subspecialty. As a result, our study population included a broad range of paediatric subspecialties. Our broad invitation strategy might have led to a lower overall response rate. The focus on children with life‐limiting conditions in the introduction of the survey might have held back some readers from participation since not all paediatricians in university care centres serve this population. Nevertheless, this aligns with the idea that response representativeness might be more important than response rate in survey research.30 The responders turned out to be a selection of experienced paediatricians with a mean working experience in paediatrics of 18.3 years. This is possibly an adequate reflection of the fact that in paediatric medical practice in the Netherlands, the more experienced professionals take care of the more complex medical cases.
Although the care for seriously ill children in the Netherlands is concentrated in the university medical care centres, these children receive care from other paediatricians and general practitioners as well. Therefore, our results might underestimate the full range of ACP activities provided to seriously ill children and their families. The focus on the most recent case of a child who died might have both underestimate and overestimate current ACP activities. It could be that for an individual respondent, the most recent case was not a good model for their actual ACP activities. We focused on the most recent case to prevent selection bias by the respondents. However, we could not check whether the respondents really reported on their most recent case. They might have chosen a case, which came directly to mind, or a case in which they valued the conversations they have had. This may have biased the results.
In addition, our data collection did not cover any data from non‐responders, which complicates comparisons between our sample and the total group of eligible participants. Another limitation of the study is that we do not know at what moment in the disease trajectory elements of ACP were discussed and with what intention. Respondents might have labelled conversations in hindsight as part of a longitudinal ACP process, whereas they, at that actual moment, did not discuss these items intentionally as part of ACP.
5. CONCLUSION
Dutch paediatricians caring for children living with life‐limiting conditions reported mainly having ACP conversations with parents. Conversations with children occur only in a minority of cases. Paediatricians acknowledge the benefits of ACP and report that they are competent in ACP communication. Conversations about code status or treatment limitations are considered key parts of ACP. A minority feel that ACP conversations occur often enough. The barriers to ACP conversations are mainly perceived as related to parents. Education in the explorative nature of ACP, the involvement of the child in ACP and parental preferences for ACP might contribute to the further engagement of paediatricians in ACP.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
Supporting information
ACKNOWLEDGEMENTS
We thank all respondents for their contribution to this study. We thank Elmar Hulstijn for his support with NETQ Healthcare. We thank Tony Sheldon for his language editing service. We are grateful to the people with whom we liaised in the centres participating for their assistance in inviting paediatricians to participate in the study.
Fahner JC, Rietjens JAC, van der Heide A, van Delden JJM, Kars MC. Survey of paediatricians caring for children with life‐limiting conditions found that they were involved in advance care planning. Acta Paediatr. 2020;109:1011–1018. 10.1111/apa.15061
Funding information
This study was supported the Netherlands Organisation for Health Research and Development (Grant number 844001206). The funding source had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication. The authors declare that they have no financial relationship with this organisation that sponsored the research
REFERENCES
- 1. Fraser ALK, Miller M, Hain R, et al. Rising national prevalence of life‐limiting conditions in children in England. Pediatrics. 2012;129(4):e923‐e929. [DOI] [PubMed] [Google Scholar]
- 2. Feudtner C, Tammy I, Hexem KR, et al. Pediatric palliative care patients: a prospective multicenter cohort study. Pediatrics. 2011;127:1094‐1101. [DOI] [PubMed] [Google Scholar]
- 3. Verberne LM, Kars MC, Schouten-van Meeteren AYN, et al. Aims and tasks in parental caregiving for children receiving palliative care at home: a qualitative study. Eur J Pediatr. 2017;176(3):343‐354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hinds PS, Oakes LL, Hicks J, et al. “Trying to be a good parent” as defined by interviews with parents who made phase I, terminal care, and resuscitation decisions for their children. J Clin Oncol. 2009;27(35):5979‐5985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. End of life care for infants, children and young people with life‐limiting conditions: planning and management [Internet]. NICE guideline; 2016. [cited 2019 Jan 14].
- 6. American Academy of Pediatrics . Pediatric palliative care and hospice care commitments, guidelines, and recommendations. Pediatrics. 2013;132:966‐972. [DOI] [PubMed] [Google Scholar]
- 7. Rietjens JAC, Sudore PRL, Connolly M, et al. Review definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18(9):e543‐e551. [DOI] [PubMed] [Google Scholar]
- 8. Lotz JD, Jox RJ, Borasio GD, Führer M. Pediatric advance care planning from the perspective of health care professionals: a qualitative interview study. Palliat Med. 2015;29(3):212‐222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lotz JD, Daxer M, Jox RJ, Borasio GD, Führer M. “ Hope for the best, prepare for the worst ”: a qualitative interview study on parents ’ needs and fears in pediatric advance care planning. Palliat Med. 2016;31(8):764‐771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brinkman‐stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end‐of‐life care: a systematic review. Palliat Med. 2016;28(8):1000‐1025. [DOI] [PubMed] [Google Scholar]
- 11. de Vleminck A, Houttekier D, Pardon K, et al. Barriers and facilitators for general practitioners to engage in advance care planning: a systematic review. Scand J Prim Health Care. 2013;32:215‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sanderson A, Hall AM, Wolfe J. Advance care discussions: pediatric clinician preparedness and practices. J Pain Symptom Manage. 2016;51(3):520‐528. [DOI] [PubMed] [Google Scholar]
- 13. Durall A, Zurakowski D, Wolfe J. Barriers to conducting advance care discussions for children with life‐threatening conditions. Pediatrics. 2012;129(4):e975‐e982. [DOI] [PubMed] [Google Scholar]
- 14. van der Steen JT, Kruse RL, Ooms ME, et al. Treatment of nursing home residents with dementia and lower respiratory tract infection in the United States and the Netherlands: An Ocean Apart. J Am Geriatr Soc. 2004;52:691‐699. [DOI] [PubMed] [Google Scholar]
- 15. Ajzen I. The theory of plannend behavior. Organ Behav Hum Dec. 1991;50:179‐211. [Google Scholar]
- 16. Kars M, Grypdocnk M, van Delden JJM. Being a parent of a child with cancer throughout the end‐of‐life course. Oncol Nurs Forum. 2011;38(4):2011. [DOI] [PubMed] [Google Scholar]
- 17. Fahner JC, Beunders AJM, van der Heide A, et al. Interventions guiding advance care planning conversations: a systematic review. J Am Med Dir Assoc. 2019;20(3):227‐248. [DOI] [PubMed] [Google Scholar]
- 18. Hein IM, Troost PW, Broersma A, de Vries MC, Daams JG, Lindauer RJL. Why is it hard to make progress in assessing children ’ s decision‐making competence ? BMC Med Ethics. 2015;16(1):1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Feenstra B, Boland L, Lawson ML, et al. Interventions to support children’s engagement in health‐related decisions: a systematic review. Bmc Pediatr. 2014;14:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kars M, Grypdonck M, de Bock L, van Delden JJM. The parents’ ability to attend to the “voice of their child” with incurable cancer during the palliative phase. Heal Psychol. 2015;34(4):446‐452. [DOI] [PubMed] [Google Scholar]
- 21. Bluebond‐langner M, Belasco JB, Goldman A, Belasco C. Understanding parents ’ approaches to care and treatment of children with cancer when standard therapy has failed. J Clin Oncol. 2007;25(17):2414‐2419. [DOI] [PubMed] [Google Scholar]
- 22. Heckford E, Beringer AJ. Advance care planning: challenges and approaches for pediatricians. J Palliat Med. 2014;17(9):1049‐1053. [DOI] [PubMed] [Google Scholar]
- 23. Basu S, Swil K. Paediatric advance care planning: physician experience and education in initiating difficult discussions. J Pediatr Child Heal. 2017;54(5):510‐514. [DOI] [PubMed] [Google Scholar]
- 24. de Vos MA, Bos AP, Plötz FB, van Heerde M, de Graaff BM. Talking with parents about end‐of‐life decisions for their children. Pediatrics. 2015;135(2):e465‐e467. [DOI] [PubMed] [Google Scholar]
- 25. Meyer EC, Ritholz MD, Burns JP, Truog RD. Improving the quality of end‐of‐life care in the pediatric intensive care unit: parents’ priorities and recommendations. Pediatrics. 2006;117(3):649‐657. [DOI] [PubMed] [Google Scholar]
- 26. Gordon C, Barton E, Meert KL, Eggly S. Accounting for medical communication: parents’ perceptions of communicative roles and responsibilities in the pediatric intensive care unit. Commun Med. 2012;6(2):177‐188. [PMC free article] [PubMed] [Google Scholar]
- 27. Kars M, Grypdocnk M, de Korte‐Verhoef M, et al. Parental experience at the end‐of‐life in children with cancer: “ preservation ” and “ letting go ” in relation to loss. Support Care Cancer. 2011;19:27‐35. [DOI] [PubMed] [Google Scholar]
- 28. Feudtner C, Carroll KW, Hexem KR, Silberman J, Kang TI, Kazak AE. Parental hopeful patterns of thinking, emotions, and pediatric palliative care decision making. Arch Pediatr Adolesc Med. 2010;164(9):831‐839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. de Vos MA, van der Heide A,Maurice‐Stam H, et al. The process of end‐of‐life decision‐making in pediatrics: a national survey in the Netherlands. Pediatrics. 2011;127:e1004‐e1012. [DOI] [PubMed] [Google Scholar]
- 30. Cook C, Heath F, Thompson RL. A meta‐analysis of response rates in web‐ or Internet‐based surveys. Educ Psychol Meas. 2000;60(6):821‐836. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


