Abstract
Background and purpose
The aim was to investigate the clinical impact of the duration of artificial ventilation in stroke patients receiving mechanical thrombectomy (MT) under general anaesthesia.
Methods
All consecutive ischaemic stroke patients who had been treated at our centre with MT for anterior circulation large vessel occlusion under general anaesthesia were identified over an 8‐year period. Ventilation time was analysed as a continuous variable and patients were grouped into extubation within 6 h (‘early’), 6–24 h (‘delayed’) and >24 h (‘late’). Favourable outcome was defined as modified Rankin Scale scores of 0–2 at 3 months post‐stroke. Pneumonia rate and reasons for prolonged ventilation were also assessed.
Results
Amongst 447 MT patients (mean age 69.1 ± 13.3 years, 50.1% female), the median ventilation time was 3 h. 188 (42.6%) patients had a favourable 3‐month outcome, which correlated with shorter ventilation time (Spearman’s rho 0.39, P < 0.001). In patients extubated within 24 h, early compared to delayed extubation was associated with improved outcome (odds ratio 2.40, 95% confidence interval 1.53–3.76, P < 0.001). This was confirmed in multivariable analysis (P = 0.01). A longer ventilation time was associated with a higher rate of pneumonia during neurointensive care unit/stroke unit stay (early/delayed/late extubation: 9.6%/20.6%/27.7%, P < 0.01). Whilst stroke‐associated complications represented the most common reasons for late extubation (>24 h), delayed extubation (6–24 h) was associated with admission outside of core working hours (P < 0.001).
Conclusions
Prolonged ventilation time after stroke thrombectomy independently predicts unfavourable outcome at 3 months and is associated with increased pneumonia rates. Therefore, extubation should be performed as early as safely possible.
Keywords: endovascular procedures, intensive care, mechanical ventilation, neurocritical care, pneumonia, prognosis, stroke, thrombectomy
Background
Mechanical thrombectomy (MT) has become the recommended treatment for acute ischaemic stroke caused by anterior circulation large vessel occlusion 1. Currently, there is no consensus whether this procedure should be performed under a specific form of anaesthesia, as previous studies have provided conflicting evidence whether general anaesthesia (GA), conscious sedation or local anaesthesia lead to better functional neurological outcome 2, 3, 4. Therefore, all three methods are frequently used in clinical routine 5.
General anaesthesia with intubation offers the advantage of full patient immobilization, which might be associated with improved angiographic image quality and shorter procedure time. In contrast, GA and intubation could delay time to groin puncture and consecutively vessel recanalization. GA might also increase the risk of relevant blood pressure drops, thereby impeding cerebral blood flow due to vasodilatory side effects of most anaesthetic drugs, as well as (ventilator‐associated) pneumonia 6.
In general, longer ventilation time augments the risk for both of the latter complications in neurocritical care patients 7, 8. However, rash extubation may cause complications such as blood pressure surges, aspiration and respiratory difficulties. To date, there is no guideline regarding the optimal timing of extubation after MT. Only one retrospective study addressed this topic and found worse outcome in patients who were extubated after more than 24 h. Interestingly, the authors did not identify outcome differences between patients who were extubated at different time points within 24 h, but this might be explained by the rather small sample size (n = 103) of their study cohort 9.
In the present study, the clinical impact of ventilation time was investigated in a large cohort of consecutive patients undergoing MT for anterior circulation large vessel occlusion. It was hypothesized that a longer ventilation time (particularly >24 h) would be associated with a higher pneumonia rate and unfavourable functional outcome at 3 months. Furthermore, it was specifically analysed whether ‘early’ (<6 h) compared to ‘delayed’ extubation (6–24 h) had an effect on the clinical prognosis, and what reasons caused delays in extubation after MT.
Methods
For this cohort study, all consecutive patients ≥18 years who had received MT because of anterior circulation large vessel occlusion stroke (occlusion of the internal carotid and/or middle cerebral artery in the M1 or M2 segments) between January 2011 and April 2019 were identified. At our centre, MT is routinely performed by interventional radiologists using stent retrievers under GA provided by neuroanaesthesiologists. Patients were excluded from this study if MT was done under conscious sedation (n = 15) or if a subsequent decompressive hemicraniectomy was performed (n = 4). A study flowchart is shown in Fig. 1.
Figure 1.
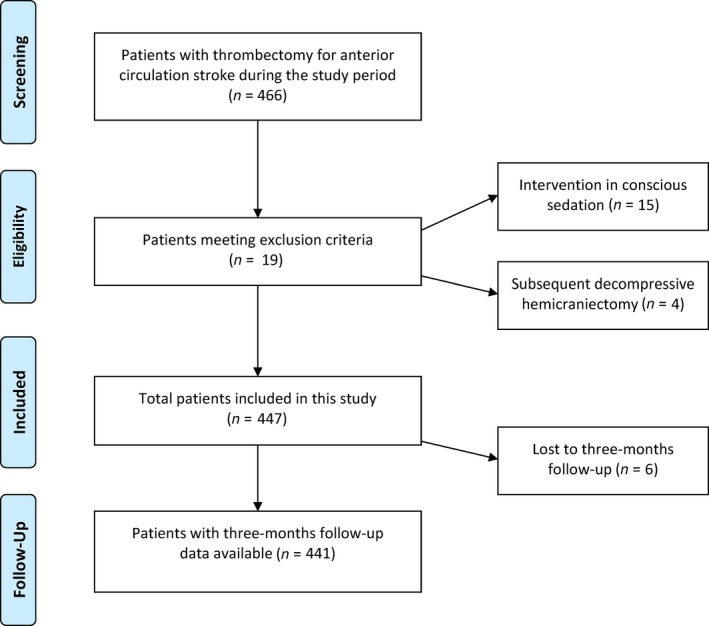
Study flowchart.
Clinical data including the duration of ventilation, the exact time point of extubation and early stroke complications within the neurointensive care unit or stroke unit stay such as pneumonia were prospectively and electronically recorded as part of an ongoing thrombectomy cohort registry at our centre 10. Pneumonia was defined according to established criteria: the presence of an infiltrate on chest X‐ray, plus at least two of fever >38°C, leucocytosis or leukopenia, purulent secretions 11, 12.
The time from intubation to extubation was analysed as a continuous variable. Furthermore, patients were trichotomized according to three predefined subgroups in order to depict common clinical scenarios: (i) ‘early’ extubation within 6 h, in order to encompass all patients extubated directly after the procedure in the angio suite or within the first hours of admission at the neurointensive care unit; (ii) ‘delayed’ extubation (6–24 h); and (iii) ‘late’ extubation (>24 h).
The primary outcome variable was defined as functional neurological outcome at 3 months according to the modified Rankin Scale (mRS), dichotomized into favourable (scores of 0–2) versus unfavourable (scores 3–6) outcome. Three‐month mRS scores were rated by experienced stroke physicians during an in‐person visit at the stroke outpatient department or by telephone interview if the former was not possible.
The study was approved by the ethics committee of the Medical University of Graz. Because this was a retrospective registry study, individual consent was waived.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, NY, USA). Normally distributed continuous variables were compared by the unpaired Student’s t test; for other distributions the Mann–Whitney U test was used. For categorical variables, the chi‐squared test was used. Furthermore, a binary multivariable regression model for predictors of favourable outcome at 3 months was calculated entering all baseline variables with P < 0.1 in the univariable analysis; then stepwise backward elimination was performed using a threshold of P < 0.1. P values equal to or less than 0.05 were considered statistically significant.
Results
Patient characteristics and outcome
In all, 447 patients (mean age 69.1 ± 13.3 years, 50.1% female) were identified and in 441 3‐month follow‐up data were available. The majority of patients had an M1‐segment occlusion of the middle cerebral artery (65.3%); 58.6% had been treated with intravenous thrombolysis before MT. Median National Institutes of Health Stroke Scale (NIHSS) at admission was 15 (interquartile range 11–18) and successful recanalization (thrombolysis in cerebral infarction grades 2b–3) was achieved in 88.5% of the patients (Table 1).
Table 1.
Clinical data and timing of extubation in the study cohort regarding 3‐month outcome
|
Study cohort n = 441 |
mRS 0–2 n = 188 (42.6%) |
mRS 3–6 n = 253 (57.4%) |
P value | |
|---|---|---|---|---|
| Clinical data | ||||
| Age (years, mean ± SD) | 69.1 ± 13.3 | 64.3 ± 13.4 | 72.4 ± 12.2 | <0.001 |
| Male sex | 220 (49.9%) | 96 (51.0%) | 124 (49.0%) | 0.67 |
| Arterial hypertension | 307 (69.6%) | 106 (56.4%) | 201 (79.4%) | <0.001 |
| Dyslipidaemia | 98 (20.7 %) | 39 (20.7%) | 59 (23.3%) | 0.52 |
| Chronic heart disease a | 84 (19.0 %) | 26 (13.8%) | 58 (22.9%) | 0.02 |
| Diabetes mellitus | 73 (16.6%) | 19 (10.1%) | 54 (21.3%) | 0.002 |
| Atrial fibrillation | 182 (41.3%) | 60 (31.9%) | 122 (48.2%) | 0.001 |
| Stroke of unknown symptom onset | 90 (20.4%) | 35 (18.6%) | 55 (21.7%) | 0.42 |
| Pre‐stroke mRS (median, IQR) | 0 (0–0) | 0 (0–0) | 0 (0–0) | <0.001 |
| NIHSS at admission (median, IQR) | 15 (11–18) | 13 (9–16) | 16 (13–19) | <0.001 |
| MCA/M1 occlusion | 288 (65.3%) | 122 (64.9%) | 166 (65.6%) | 0.88 |
| MCA/M2 occlusion | 59 (13.4%) | 32 (17.0%) | 27 (10.7%) | 0.06 |
| Intracranial ICA occlusion | 93 (21.1%) | 31 (16.5%) | 62 (24.5%) | 0.05 |
| Acute stroke treatment | ||||
| Intravenous thrombolysis | 258 (58.6%) | 118 (62.8%) | 140 (55.6%) | 0.13 |
| Symptom onset to groin puncture (min, median, IQR) | 200 (160–247) | 200 (158–244) | 200 (160–252) | 0.61 |
| Symptom onset to recanalization (min, median, IQR) | 260 (215–310) | 250 (204–303) | 266 (225–315) | 0.42 |
| Successful recanalization (TICI 2b–3) | 385 (88.5%) | 181 (97.3%) | 204 (81.9%) | <0.001 |
| Peri‐interventional dissection | 12 (2.7%) | 8 (4.3%) | 4 (1.6%) | 0.09 |
| Timing of extubation | ||||
| Time to extubation (h, median, range) | 3 (1–530) | 2 (1–115) | 11 (1–530) | <0.001 |
| Early extubation (within 6 h) | 256 (58.0%) | 142 (75.5%) | 114 (45.1%) | <0.001 |
| Delayed extubation (6–24 h) | 121 (27.4%) | 41 (21.8%) | 80 (31.6%) | <0.001 |
| Late extubation (>24 h) | 64 (14.5%) | 5 (2.7%) | 59 (23.3%) | <0.001 |
ICA, internal carotid artery; IQR, interquartile range; MCA, middle cerebral artery; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; TICI, thrombolysis in cerebral infarction;
P‐values <0.05 are shown in bold font.
Coronary artery disease, heart failure, cardiomyopathy or valve disease.
At 3 months post‐stroke 188 patients (42.6%) had a favourable outcome (mRS 0–2). In univariable analysis, higher age, higher NIHSS at admission, the presence of arterial hypertension, chronic heart disease, diabetes mellitus, atrial fibrillation and unsuccessful recanalization were associated with unfavourable functional outcome at 3 months (Table 1).
Ventilation time
Median ventilation time was 3 h (range 1–530); seven patients (1.6%) were admitted to our hospital already intubated by prehospital emergency physicians or in the referring hospital. The majority of patients (85.5%) were extubated within 24 h; only 65 patients (14.5%) had late extubation (>24 h). 258 patients (57.7%) were extubated early (within 6 h of intubation), whilst 124 patients (27.7%) had delayed extubation (6–24 h, Table 2).
Table 2.
Clinical differences between patients with early, delayed or late extubation after stroke thrombectomy
|
Early extubation (≤6 h) n = 258 (57.7%) |
Delayed extubation (6–24 h) n = 124 (27.7%) |
P value |
Late extubation (>24 h) n = 65 (14.5%) |
P value a | |
|---|---|---|---|---|---|
| Clinical data | |||||
| Age (years, mean ± SD) | 68.6 ± 13.3 | 70.8 ± 13.2 | 0.15 | 67.6 ± 13.4 | 0.34 |
| Male sex | 132 (51.2%) | 67 (54.0%) | 0.34 | 35 (53.8%) | 0.52 |
| Arterial hypertension | 172 (66.7%) | 92 (74.2%) | 0.14 | 49 (75.4%) | 0.31 |
| Dyslipidaemia | 59 (22.9%) | 32 (25.8%) | 0.53 | 8 (12.3%) | 0.04 |
| Chronic heart disease b | 42 (16.3%) | 25 (20.2%) | 0.35 | 20 (30.8%) | 0.01 |
| Diabetes mellitus | 37 (14.3%) | 21 (16.9%) | 0.51 | 16 (24.6%) | 0.06 |
| Atrial fibrillation | 99 (38.4%) | 59 (47.6%) | 0.09 | 27 (41.5%) | 0.98 |
| Stroke of unknown symptom onset | 64 (24.8%) | 19 (15.3%) | 0.04 | 8 (12.3%) | 0.08 |
| Pre‐stroke mRS (median, IQR) | 0 (0–0) | 0 (0–0) | 0.12 | 0 (0–1) | 0.02 |
| NIHSS at admission (median, IQR) | 14 (10–17) | 15 (13–18) | <0.001 | 17 (14–19) | <0.001 |
| MCA/M1 occlusion | 172 (66.7%) | 80 (64.5%) | 0.68 | 41 (63.1%) | 0.65 |
| Intracranial ICA occlusion | 49 (19.0%) | 25 (20.2%) | 0.79 | 20 (30.8%) | 0.04 |
| Admission outside core working hours | 111 (43.0%) | 102 (82.3%) | <0.001 | 43 (66.2%) | 0.12 |
| Intervention | |||||
| Intravenous thrombolysis | 147 (57.2%) | 67 (54.0%) | 0.56 | 46 (70.8%) | 0.03 |
| Time to groin puncture (min, median, IQR) | 195 (154–245) | 210 (169–250) | 0.16 | 204 (160–254) | 0.78 |
| Time to recanalization (min, median, IQR) | 250 (204–306) | 279 (233–324) | 0.06 | 277 (222–302) | 0.94 |
| Successful recanalization (TICI 2b–3) | 235 (92.5%) | 106 (86.2%) | 0.05 | 49 (76.6%) | 0.001 |
| Peri‐interventional dissection | 10 (3.9%) | 2 (1.6%) | 0.24 | 0 (0%) | 0.15 |
| Outcome parameters | |||||
| Pneumonia rate within NICU/stroke unit | 20 (9.6%) | 22 (20.6%) | 0.007 | 18 (27.7%) | 0.004 |
| Symptomatic intracranial haemorrhage | 7 (2.7%) | 2 (1.6%) | 0.51 | 6 (9.2%) | 0.004 |
| Duration of stay in the NICU/stroke unit (days, median, IQR) | 3 (2–6) | 4 (2–5) | 0.86 | 6 (2–11) | <0.001 |
| NIHSS at discharge from NICU/stroke unit (median, IQR) | 5 (2–12) | 10 (5–18) | <0.001 | 18 (10–22) | <0.001 |
| mRS 3 months post‐stroke c (median, IQR) | 2 (1–4) | 4 (2–5) | <0.001 | 6 (4–6) | <0.001 |
| Favourable outcome at 3 months (mRS 0–2) | 142 (55.5%) | 41 (33.9%) | <0.001 | 5 (7.8%) | <0.001 |
ICA, internal carotid artery; IQR, interquartile range; MCA, middle cerebral artery; mRS, modified Rankin Scale; NICU, neurointensive care unit; NIHSS, National Institutes of Health Stroke Scale; TICI, thrombolysis in cerebral infarction;
P‐values <0.05 are shown in bold font.
Calculated between patients with late extubation versus early or delayed extubation;
Coronary artery disease, heart failure, cardiomyopathy or valve disease;
Six patients were lost to follow‐up.
Time of mechanical ventilation correlated with higher mRS values at 3 months (Spearman’s rho 0.39, P < 0.001). Similarly, patients with favourable outcome (mRS 0–2) at 3 months had lower median ventilation times (2 h, interquartile range 1–6, vs. 11 h, interquartile range 2–24, in patients with mRS 3–6; P < 0.001).
Differences between early, delayed and late extubation
Patients with late extubation (>24 h) more frequently had concomitant heart disease (30.8% vs. 17.5%, P = 0.01), more severe strokes (median NIHSS 17 vs. 14, P < 0.001), more frequently received intravenous thrombolysis (70.8% vs. 56.2%, P = 0.03) and had lower rates of successful recanalization after MT (76.6% vs. 90.5%, P = 0.001). Favourable functional 3‐month outcome was rather rare in this subgroup (7.8%, Table 2).
Analysing only those patients who had been extubated within 24 h, patients with early extubation (within 6 h) had a higher frequency of stroke of unknown onset (24.8% vs. 15.3%, P = 0.04) and slightly lower NIHSS scores at admission (median 14 vs. 15, P < 0.001) compared to patients with delayed extubation (6–24 h, Table 2). Early extubation was associated with favourable outcome [odds ratio (OR) 2.40, 95% confidence interval (CI) 1.53–3.76, P < 0.001].
In a multivariable model investigating the effect of early versus delayed extubation on functional neurological outcome and entering all outcome‐relevant baseline variables with a P value of <0.1 in univariable analysis (Table 1), hypertension, atrial fibrillation, chronic heart disease, occlusion location and periprocedural dissection were removed using stepwise backward elimination.
Early extubation remained a significant predictor of favourable functional outcome at 3 months (OR 1.93, 95% CI 1.15–3.24, P = 0.01), together with successful recanalization (OR 6.97, 95% CI 2.38–20.4). Age (OR 0.95 per year, 95% CI 0.93–0.97), NIHSS at admission (OR 0.90 per point, 95% CI 0.86–0.95) and pre‐stroke mRS (OR 0.66 per point, 95% CI 0.47–0.93) were significant predictors of unfavourable outcome (Table 3).
Table 3.
Binary multivariable logistic regression model for the target variable ‘favourable outcome’ (modified Rankin Scale 0–2) in patients extubated within 24 h
| Test variable | Odds ratio | 95% confidence interval | P value |
|---|---|---|---|
| Clinical data and intervention | |||
| Age (per year) | 0.95 | 0.93–0.97 | <0.001 |
| Pre‐stroke mRS (per point) | 0.66 | 0.47–0.93 | 0.02 |
| NIHSS at admission (per point) | 0.90 | 0.86–0.95 | <0.001 |
| Peri‐interventional management | |||
| Successful recanalization (TICI 2b–3 vs. 0–2a) | 6.97 | 2.38–20.4 | <0.001 |
| Early extubation (within 6 h vs. 6–24 h) | 1.93 | 1.15–3.24 | 0.01 |
mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; TICI, thrombolysis in cerebral infarction.
P‐values <0.05 are shown in bold font.
Reasons for delayed and late extubation
Of the 65 patients with late extubation (>24 h), reasons for prolonged ventilation were brain oedema (44.6%), insufficient alertness for other reasons (26.1%), respiratory insufficiency (15.9%), status epilepticus (4.6%) and oronasopharyngeal bleeding (3.1%, multiple reasons possible). However, 16.9% of patients with late extubation did not have an obvious medical reason documented for late extubation – all of those patients were extubated within 24–48 h. Symptomatic intracranial haemorrhage was more frequent in patients with late extubation (9.2%); there was no difference between patients with early (2.7%) and delayed extubation (1.6%; Table 2).
In the group of 121 patients with delayed extubation (6–24 h), none of the patients had failed an earlier wake‐up trial. Delayed extubation was associated with patient admission outside of core working hours (within core working hours 86.8% of patients were extubated early, whilst outside core working hours only 52.1% of patients were extubated early; OR 6.06, 95% CI 3.59–10.22, P < 0.001, Table 2).
Pneumonia
Overall, early pneumonia rate within the neurointensive care unit/stroke unit stay was 15.8%. Time to extubation was strongly associated with early pneumonia (median ventilation time 15 h in patients with pneumonia versus 3 h in those without, P < 0.001). Patients with delayed extubation (6–24 h) more frequently had pneumonia compared to patients with early extubation (20.6% vs. 9.6%, OR 2.43, 95% CI 1.26–4.69, P = 0.007). Likewise, patients with late extubation (>24 h) showed even higher rates of pneumonia (27.7% vs. 13.3% in all patients who were extubated within 24 h, OR 2.49, 95% CI 1.76–4.69, P = 0.004, Table 2).
Discussion
In this large cohort of consecutive ‘real world’ patients undergoing MT for anterior circulation large vessel occlusion under GA, prolonged ventilation time was associated with a higher pneumonia rate and, besides well‐known prognostic factors such as age, NIHSS and unsuccessful recanalization, independently predicted unfavourable functional outcome at 3 months post‐stroke. Whilst it was not surprising that patients with late extubation (>24 h) had worse outcome, the most interesting and novel finding of our work was the independent prognostic effect of early extubation within the first 24 h.
To the best of our knowledge, there exists only one previously published report on this topic. In that German study investigating the clinical impact of the duration of mechanical ventilation in 103 stroke patients after MT, patients who were ventilated longer than 24 h had worse 3‐month outcome and a higher frequency of pneumonia, but no differences were observed within the group of patients with ventilation times ≤24 h 9. The weaknesses of that study include the rather small sample size, the retrospective data collection and the relatively long median overall ventilation time of 18.5 h compared to 3 h in our cohort. Furthermore, reasons for late extubation were not specifically investigated. Conversely to that work, a strong indication for a dose‐dependent effect of ventilation time on functional neurological outcome at 3 months was found. In particular, early extubation (within 6 h) after stroke thrombectomy was strongly associated with a favourable 3‐month prognosis. This finding is novel and clinically relevant for the post‐interventional management of stroke patients treated with MT under GA. Based on our results, MT patients with anterior circulation large vessel occlusion undergoing the procedure under GA should be extubated early after the intervention, unless there are medical reasons against it. However, it is important to note that our results are most probably not transferable to patients who are treated with thrombectomy for large vessel occlusion of the vertebrobasilar circulation, as brainstem infarction often affects functional pathways responsible for respiration, swallowing and protective reflexes, which may cause additional difficulties regarding extubation.
When interpreting our work, important potential confounding factors have to be considered. In clinical practice, physicians might be more reluctant to swiftly extubate patients if they have severe strokes, more comorbidities or if a critical disease course is expected (e.g. a failed thrombectomy in a younger patient). This is probably the main explanation for the unfavourable outcome of patients with late extubation >24 h. In most of those patients, it was possible to identify specific medical reasons leading to later extubation (most frequently neurological and/or respiratory stroke complications). However, those factors mostly did not apply to extubations within 24 h in our study cohort. On the contrary, it was found that admission outside core working hours was an important predictor of delayed extubation. This means that non‐medical reasons played an important role in the decision to extubate early or delayed within the first 24 h after MT.
It was also found that patients with delayed extubation had slightly higher NIHSS scores at admission. Nonetheless, multivariable analysis including all assessed outcome‐relevant factors still identified early extubation as an independent prognostic factor at 3 months post‐stroke. There are multiple possible reasons for unfavourable outcome resulting from delayed extubation. First, it is well known that pneumonia leads to worse outcome in stroke patients 13. Ventilator‐associated pneumonia is one of the most important complications of mechanical ventilation and its occurrence is strongly associated with the duration of ventilation 14. This was also seen in our study, where patients with late extubation had the highest pneumonia rate, whilst patients who were extubated early had pneumonia much less frequently. Importantly, pneumonia occurrence was only assessed within the first days when patients were admitted on the neurointensive care unit/stroke unit. This could be seen as a limitation of this study; however, our primary aim was to analyse pneumonia as a complication of mechanical ventilation rather than stroke‐related pneumonia, which occurs at variable time points during the hospital stay and depends on different circumstances. Respiratory insufficiency was a reason for prolonged ventilation >24 h in 11 patients and may have been caused by pneumonia in some of those cases.
Delayed extubation also requires sedative drugs to be given for longer periods. The majority of sedative drugs can cause hypotension, which might negatively affect cerebral blood flow in the critical time period after recanalization, possibly influencing final infarct size. Additionally, hyperoxaemia may be present for a longer time in patients with delayed extubation, which might contribute to secondary brain injury and worse outcomes 15, 16. Furthermore, early diagnostic stroke workup may be impeded in patients who remain intubated for a longer time, potentially leading to delays in specific treatment of stroke causes. Moreover, early rehabilitative measures including mobilization are only possible to a limited extent in intubated patients.
Extubation outside core working hours and in particular during night‐time are often considered more prone to complications with an increased mortality rate, as recently described in a large cohort study across different US intensive care unit settings 17. In contrast, several smaller studies have shown that in specific settings night‐time extubation may even be associated with better patient outcomes such as decreased reintubation rates, length of ventilation and hospital stay 18, 19.
Whilst our study has several strengths such as the large cohort of consecutive MT patients, the high follow‐up rate and the exact documentation of reasons for delayed extubation, its main limitation is the retrospective design. Even though data were collected prospectively and our study showed a strong association of delayed extubation and unfavourable 3‐month outcome, the study design cannot prove causality. Furthermore, uniform pre‐ and post‐interventional imaging to assess infarct size and blood pressure data were not available. Therefore, our findings should be seen as hypothesis‐generating and need to be confirmed in prospective studies.
Conclusion
Prolonged ventilation time in patients undergoing endovascular stroke treatment under GA is independently related to unfavourable neurological outcome at 3 months post‐stroke. This finding is clinically relevant for the post‐interventional management of patients with ischaemic stroke of the anterior cerebral circulation, and indicates that extubation after stroke thrombectomy should be performed as early as safely possible.
Disclosure of conflicts of interest
The authors declare no financial or other conflicts of interest.
Data availability statement
The datasets generated during this study are available from the corresponding author upon reasonable request.
References
- 1. Goyal M, Menon BK, van Zwam WH, et al Endovascular thrombectomy after large‐vessel ischaemic stroke: a meta‐analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 2. Campbell BCV, van Zwam WH, Goyal M, et al Effect of general anaesthesia on functional outcome in patients with anterior circulation ischaemic stroke having endovascular thrombectomy versus standard care: a meta‐analysis of individual patient data. Lancet Neurol 2018; 17: 47–53. [DOI] [PubMed] [Google Scholar]
- 3. Ilyas A, Chen C‐J, Ding D, et al Endovascular mechanical thrombectomy for acute ischemic stroke under general anesthesia versus conscious sedation: a systematic review and meta‐analysis. World Neurosurg 2018; 112: e355–e367. [DOI] [PubMed] [Google Scholar]
- 4. Zhang Y, Jia L, Fang F, Ma L, Cai B, Faramand A. General anesthesia versus conscious sedation for intracranial mechanical thrombectomy: a systematic review and meta‐analysis of randomized clinical trials. J Am Heart Assoc 2019; 8: e011754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fargen KM, Arthur AS, Spiotta AM, et al A survey of neurointerventionalists on thrombectomy practices for emergent large vessel occlusions. J Neurointerv Surg 2017; 9: 142–146. [DOI] [PubMed] [Google Scholar]
- 6. Hindman BJ, Dexter F. Anesthetic management of emergency endovascular thrombectomy for acute ischemic stroke, part 2: Integrating and applying observational reports and randomized clinical trials. Anesth Analg 2019; 128: 706–717. [DOI] [PubMed] [Google Scholar]
- 7. Coplin WM, Pierson DJ, Cooley KD, Newell DW, Rubenfeld GD. Implications of extubation delay in brain‐injured patients meeting standard weaning criteria. Am J Respir Crit Care Med 2000; 161: 1530–1536. [DOI] [PubMed] [Google Scholar]
- 8. Asehnoune K, Roquilly A, Cinotti R. Respiratory management in patients with severe brain injury. Crit Care 2018; 22: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nikoubashman O, Schürmann K, Probst T, et al Clinical impact of ventilation duration in patients with stroke undergoing interventional treatment under general anesthesia: the shorter the better? AJNR Am J Neuroradiol 2016; 37: 1074–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kneihsl M, Niederkorn K, Deutschmann H, et al Abnormal blood flow on transcranial duplex sonography predicts poor outcome after stroke thrombectomy. Stroke 2018; 49: 2780–2782. [DOI] [PubMed] [Google Scholar]
- 11. Johanson WG, Pierce AK, Sanford JP, Thomas GD. Nosocomial respiratory infections with Gram‐negative bacilli. The significance of colonization of the respiratory tract. Ann Intern Med 1972; 77: 701–706. [DOI] [PubMed] [Google Scholar]
- 12. Rea‐Neto A, Youssef NCM, Tuche F, et al Diagnosis of ventilator‐associated pneumonia: a systematic review of the literature. Crit Care 2008; 12: R56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Finlayson O, Kapral M, Hall R, et al Risk factors, inpatient care, and outcomes of pneumonia after ischemic stroke. Neurology 2011; 77: 1338–1345. [DOI] [PubMed] [Google Scholar]
- 14. Kalanuria AA, Ziai W, Zai W, Mirski M. Ventilator‐associated pneumonia in the ICU. Crit Care 2014; 18: 208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Taccone FS, Crippa IA, Vincent J‐L. Normobaric hyperoxia after stroke: a word of caution. Expert Rev Neurother 2018; 18: 91–93. [DOI] [PubMed] [Google Scholar]
- 16. Robba C, Bonatti G, Battaglini D, Rocco PRM, Pelosi P. Mechanical ventilation in patients with acute ischaemic stroke: from pathophysiology to clinical practice. Crit Care 2019; 23: 388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gershengorn HB, Scales DC, Kramer A, Wunsch H. Association between overnight extubations and outcomes in the intensive care unit. JAMA Intern Med 2016; 176: 1651–1660. [DOI] [PubMed] [Google Scholar]
- 18. Everhart KK, Khorsand S, Khandelwal N, Michaelsen KE, Spiekerman CF, Joffe AM. Nighttime extubation does not increase risk of reintubation, length of stay, or mortality: experience of a large, urban, teaching hospital. Anesth Analg 2019; 128: 918–923. [DOI] [PubMed] [Google Scholar]
- 19. Tischenkel BR, Gong MN, Shiloh AL, et al Daytime versus nighttime extubations: a comparison of reintubation, length of stay, and mortality. J Intensive Care Med 2016; 31: 118–126. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during this study are available from the corresponding author upon reasonable request.


