Abstract
Background and aims
COVID-19 is an emerging pandemic due to droplet infection of 2019-novel coronavirus (2019-nCoV). Due to its rapid transmission and high case-fatality rate, recognition of its risk and prognostic factor is important. Obesity has been associated with impaired immune system, increasing the susceptibility for 2019-nCoV infection. We aimed to study the impact of obesity to the prognosis and disease severity of COVID-19.
Methods
A systematic search and handsearching was conducted in four databases: Cochrane, MEDLINE, EMBASE, and PubMed. The identified articles were screened using the chosen eligibility criteria. We obtained three retrospective cohort studies (Wu J et al., Lighter J et al., and Simonnet A et al.) to be critically appraised using Newcastle Ottawa Scale.
Results
The findings of all included studies were consistent in stating the contribution of obesity as a risk factor to increase the requirement for advanced medical care. Study with the highest quality, Simonnet A et al., reported an increase need of invasive mechanical ventilation in COVID-19 patients with body mass index higher than 35 kg/m2, OR: 7.36 (1.63–33.14; p = 0.021). This is associated with a higher mortality rate in obese population infected with COVID-19.
Conclusion
Obesity is an independent risk and prognostic factor for the disease severity and the requirement of advanced medical care in COVID-19. This systematic review highlights a particularly vulnerable group – obese, and emphasises on the importance of treatment aggression and disease prevention in this population group.
Keywords: COVID-19, Obesity, Prognosis, Predictor
1. Introductions
Coronavirus disease-2019/COVID-19 is a new emerging pandemic. Its rapid transmission, progressivity and high case fatality rate had affected global social welfare and economy [2]. Per 25 April 2020, the total confirmed coronavirus cases globally reached 2,902,708 along with 202,179 death [1].
The prognosis of COVID-19 has been consistently reported to worsen in advanced age [3,4] and with the presence of other comorbidities, such as hypertension, cardiovascular diseases, diabetes mellitus, and pulmonary diseases [[3], [4], [5], [6]]. Nevertheless, the growing rate of hospitalization in younger population has been reported and associated with obesity [7,8], a condition of having excessive adipose tissue. The growing prevalence of obesity globally have risen the concern on its additional impact to worsen this pandemic [11].
Obesity has been associated with a condition of chronic inflammation and decreased immune system, increasing the susceptibility of an individual to infections [12,13]. Hence, this evidence suggests that obesity might act as an independent risk factor for a poor disease progression of COVID-19. Nevertheless, a meta-analysis by Ni Y (2017) reported the protective factor of obesity in Acute Respiratory Distress Syndrome (ARDS) patients [14]. Having ARDS as one of the devastating clinical manifestations of COVID-19 [4], this contradicting views raises doubts on the impact of obesity in the disease severity and prognosis of COVID-19.
Hence, we aim to investigate the impact of obesity to the requirement of advanced medical treatment in positively-identified COVID-19 patients, with the hypothesis of obesity being a poor prognostic factor for COVID-19.
2. Methods
2.1. Protocol and Registration
This systematic review was conducted based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) Statement [15]. The protocol of this systematic review has been registered in The International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42020183068).
2.2. Eligibility criteria
We included longitudinal cohort studies or randomised controlled trials which observed the effect of BMI to the requirement of in-hospital critical care in patients infected with 2019-novel coronavirus (COVID-19). Exclusion criteria include infection of unspecific coronaviruses or other respiratory viruses.
2.3. Search strategy
A systematic literature search was performed on April 12–14th, 2020 using four different databases: Cochrane, MEDLINE, EMBASE, and PubMed; along with manual handsearching using keywords as listed in Table 1 . Literature selection was performed without time limitation but restricted to only published English or Indonesian articles.
Table 1.
Search queries of this systematic review.
| Databases | Search query | Hits |
|---|---|---|
| Cochrane | (covid-19 OR coronavirus OR sars-cov-2) AND (comorbid∗ OR obes∗ OR overweight OR high BMI OR unhealthy weight) AND (hospitali?ation OR admission OR hospital stay OR mortality OR morbidity) | 8 |
| EBSCO | (covid-19 or coronavirus or 2019-ncov or sars-cov-2 or cov-19) AND ((comorbidity or comorbidities or coocurence or comorbid) OR (obesity or overweight or fat or obese or unhealthy weight or high bmi)) AND ((hospitalization or hospitalization or admission or hospital stay or care episode) OR (mortality or mortality rate or death or death rate or morbidity)) | 147 |
| EMBASE | ((covid-19 or coronavirus or 2019-ncov or sars-cov-2 or cov-19).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]) AND ((comorbid∗ or obes∗ or overweight or high BMI or unhealthy weight).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]) AND ((hospitali?ation or admission or hospital stay or care episode or mortality or morbidity).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]) | 197 |
| PubMed | ((covid-19 or coronavirus or 2019-ncov or sars-cov-2 or cov-19) and (comorbid∗ or obes∗ or overweight or high bmi or unhealthy weight)) and (hospital?action or admission or hospital stay or care episode or mortality or morbidity) | 208 |
| Handsearching | “obesity” AND “COVID-19” | 13 |
2.4. Data collection
Data from each study was extracted in a standardised form, compiling study citations, baseline characteristics of the included subjects, appropriate intervention, and the study findings. Study citations included the name of the first author, year of publication, and title of the study. Meanwhile, characteristics of each study refered to study design, location of the study, patients’ characteristics (age, ethnicity, gender, sample size, BMI and presence of other comorbidities). We specified the extracted comorbidities to hypertension, respiratory system disease, cardiovascular disease, diabetes mellitus, and dyslipidaemia according to the acknowledged comorbidities for COVID-19 by other systematic reviews and meta-analysis [6,16]. The study findings extracted involved the hazard ratio/odds ratio analysed in each study.
2.5. Quality assessment and data synthesis
Two independent reviewers conducted the quality assessment of the studies (AT and DLT). The included studies were critically appraised using Newcastle Ottawa Quality Assessment Scale (NOS). Any discrepancies of NOS score between reviewers were discussed until it reached a conclusion. High-quality studies were defined as studies fulfilling NOS score of minimum 7.
Data was synthesised based on a minimum of three different and high-quality studies with consistent finding. The obtained data was analysed considering the method of variable analysis used, study size, odds/hazard ratio, along with its confidence interval.
3. Results
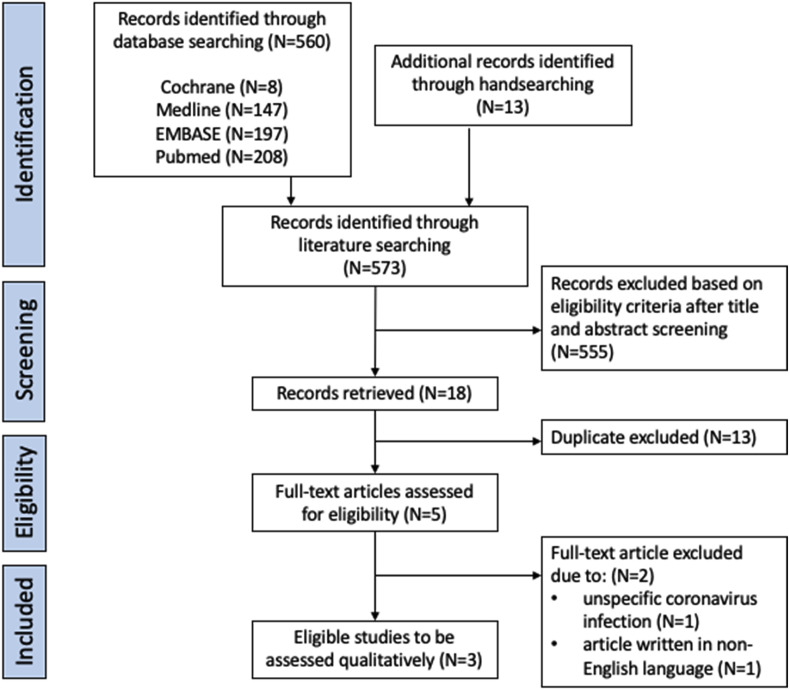
Literature searching performed using keywords as listed in Table 1 yielded several studies. Out of 573 articles identified, 18 articles were retrieved after title and abstract screening. After the exclusion of duplicates, five studies were assessed in full-text. Three studies remained after full-text screening using eligibility criteria, which were studies by Wu J et al. [17], Lighter J et al. [18], and Simonnet A et al. [19]. The exclusion of the remaining two studies was due to the usage of language other than English/Indonesian and investigation on other types of coronaviruses. The flow of our study selection is presented according to PRISMA Statement (Fig. 1 ).
Fig. 1.
PRISMA flowchart of study selection.
The summary of baseline study characteristics is presented in Table 2 . All studies had level 2 of evidence based on Oxford 2011 and were considered high-quality based on each NOS score. The results of the critical appraisal could be seen in Table 3 . All studies used retrospective cohort design to explain the relationship between obesity (exposure) and COVID-19 severity. While studies by Simonnet et al. and Lighter J et al. used a body mass index (BMI) of more than 30 kg/m2 to define obesity, study by Wu J et al. used 25 kg/m2. These criteria were in accordance with the proposed criteria for obesity in Caucasian [9] and Asian population [10], respectively.
Table 2.
Summary of baseline characteristics and outcomes of the included studies.
| Authors | Date (MM/DD) | Study location | Age (years) | Sample size |
BMI (kg/m2) |
Comorbidities; N(%) |
Findings (OR to develop severe COVID-19) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | M/F | Mild-moderate | Severe | Hyper-tension | Respiratory diseases | CVD | DM | Dyslipi-daemia | |||||
| Wu J et al. [17] | 03/27 | China | 43.12 ± 19.02 | 280 | 151/129 | 23.6 (20.4–26.8) | 25.8 (24.0–27.6) | NA | 6 (2.14) | 57 (20.36) | 34 (12.14) | Obesity grade Ia: 1.30 (1.09–1.54; p = 0.003) | |
| Lighter J et al. [18] | 04/09 | USA | <60 | 402 | NA | 30–34 | 35 | NA | NA | NA | NA | NA | Obesity grade Ia: 1.8 (1.2–2.7; p < 0.006) Obesity grade IIa: 3.6 (2.5–5.3; p < 0.0001) |
| Simonnet A et al. [19] | 04/09 | France | 60 (51–70) | 124 | 90/34 | 27 (25.3–30.8) | 31.1 (27.3–37.5) | 60 (49) | NA | NA | 28 (23) | 34 (28) | Obesity grade IIb: 7.36 (1.63–33.14; p = 0.021) |
Notes.
CVD: Cardiovascular Disease.
DM: Diabetes Mellitus.
NA: not available/not known/not stated.
Normo- and over-weight comparator group.
Normoweight comparator group.
Table 3.
Quality assessment of the included studies using Newcastle Ottawa Scale.
Using a multivariate analysis, study by Simonnet A et al. demonstrated that COVID-19 patients with obesity grade II had 7.36 (1.63–33.14; p = 0.021) times increased risk of having invasive mechanical ventilation during in-hospital care, compared to normoweight COVID-19 [19]. Meanwhile, study by Lighter J et al. stratified their study subjects by their age, dividing them into less than 60 years and over 60 years age-groups. Compared to normo- and over-weight groups, the rate of hospitalization increased 2.0 (1.6–2.6; p < 0.0001) and 2.2 (1.7–2.9; p < 0.0001) times in younger patient group with obesity grade I and II, respectively. Moreover, younger group patients with obesity grade I and II had an increased likelihood to receive critical care 1.8 (1.2–2.7; p < 0.006) and 3.6 (2.5–5.3; p < 0.0001) times respectively, compared to normoweight and overweight groups [18]. Study by Wu J et al. also reported an increased risk of 1.30 (1.09–1.54; p = 0.003) times in COVID-19 patients with BMI higher than 25 kg/m2 to develop severe COVID-19 compared to normo- and over-weight patients [17], however, it was attenuated in multivariate analysis.
4. Discussions
COVID-19 is a devastating infectious disease worldwide, commonly manifests in acute respiratory distress syndrome (ARDS) [4]. Its rapid transmission and considerably high case-fatality rate have called for the recognition of important risk factors and high-risk population for better prevention and treatment approach. Obesity has been speculated to act independently in increasing the risk and worsening the prognosis of COVID-19 patients. In this systematic review, three included studies are consistent, despite a moderate degree of variability, in showing the deleterious effect of obesity in COVID-19 severity, inducing critical and advanced hospital care.
The findings from the included studies acknowledged the increased risk of COVID-19 severity in obesity. Nevertheless, those three studies reported a variable degree of association between obesity and severe COVID-19, which might be related to the differences in the definition of the reported outcome (invasive mechanical ventilation, ICU admission, severe infection), comparator group, sample size, and to a lesser extent, the use of different BMI cut off points for obesity.
In the aspect of sample size, study by Lighter J et al. was very precise with their findings statistically [18]. Meanwhile, study by Simonnet A, the highest quality study in overall aspects, had a lower sample size. This probably explains the need of a higher BMI to exceed statistical differences (35 kg/m2) [19]. On the other hand, study by Lighter J only required 30 kg/m2 to show a statistically significant impact of obesity to the necessity of advanced hospital care [18]. However, unlike Simonnet A study, the inclusion of other important comorbidities in multivariate analysis in Lighter J study was not known [19].
Furthermore, a careful interpretation of studies by Lighter J and Wu J should be made due to the use of different comparator group. Studies by Lighter J and Wu J compared the data of obese groups with both normo- and over-weight groups, whereas Simonnet A study compared the obese with normoweight patients. This might lead to an underestimated risk ratio measured by Lighter J and Wu J studies. Moreover, study by Wu J et al. reported the lowest relative risk, and even considered obesity not as an independent risk factor for COVID-19 disease severity [17] as the statistical significance was completely attenuated in the multivariate analysis.
Article with the highest quality was written by Simonnet et al. [19]. Although its sample size was the smallest among them, this research included multivariate analysis to omit the possibilities of other important comorbidities affecting the study outcome. Different to other prognostic studies, this study did not differentiate the mortality rate of obese and non-obese patients; hence, might not directly reflect a poorer prognosis of disease severity in obese COVID-19 patients. Nevertheless, a paper by Yang X et al. showed higher mortality rate of patients requiring mechanical ventilation [4]. Thus, choosing the necessity of mechanical ventilation in obese COVID-19 might be an appropriate outcome to assess prognosis and hospital cost.
Possible mechanisms related to disease severity in obesity are speculated to occur through higher ACE-2 concentration, chronic inflammation, and functional restrictive capacity of obese lung. ACE-2 receptor has been recognised as a coreceptor for 2019-nCoV entry and known to be expressed in many parts of human body: gastrointestinal tract, lung, heart and kidney [20]. A recent publication has reported the increased expression of ACE-2 receptor in adipose tissue [21]. This means having more adipocytes is equal to be having more ACE-2 receptors to catch 2019-nCoV. Moreover, chronic inflammation in obesity is apparent with the increased interleukin 6 (IL-6) level, adipokines, and pro-inflammatory cytokines (e.g., TNF-a, inferferon), inducing a chronic low-grade inflammatory state in obesity and impairing immune response [12,13,19]. The total lung capacity has also been reported to be reduced in obese patients, and improved by bariatric surgery [22,23]. Moreover, a study by Campos et al. also emphasised the impact of obesity to reduce lung function in sedentary subjects [23]. Hence, obese patients tend to be more susceptible to COVID-19 infection and rapid severe disease progression due to its lower baseline lung functional capacity than normoweight people.
On the other hand, a meta-analysis by Ni Y et al. (2017) reported the protective impact of obesity in ARDS patients. Study by Ni Y et al. correlated obesity to a higher rate of heparin prophylaxis and hypertension. Heparin helped to reduce coagulation and systematic inflammatory response whereas hypertension reduced fluid or vasopressor requirement in circulatory failure [14]. This condition was thought to contribute to a diminished potential of disease progression to ARDS. However, Ni Y study made no attempt to explain the direct effect of obesity and ARDS, in contrast to the previous explanation through molecular and lung functional capacity changes in obesity. Hence, our study also shed light on the contrasting view of ARDS and obesity. The severity of ARDS and overall COVID-19 clinical manifestations increased in obese patients infected with COVID-19 and this population even showed a higher need of invasive mechanical ventilation [19]. Findings from COVID-19 which were discussed in this study were also in line with previous coronaviruses studies: coronavirusHKU1 [24] and MERS-CoV virus [25]. These studies had previously stated the increased prevalence and risk of obese people to coronavirus infection.
The limitations of this study arise from the exclusion of articles written in languages other than English and Indonesian and unexplored grey literatures. We also failed to assess the baseline characteristics and variable analysis of Lighter J article. Moreover, this systematic review could not be proceeded to a quantitative analysis (meta-analysis) due to the heterogenous use of variable analysis. Thus, we recommended future studies to adjust comorbidities to their risk ratio presentation to clearly portray the effect of obesity to the disease severity of COVID-19.
Taken together, this is the first systematic review to proclaim obesity as an independent risk and prognostic factor for the requirement of advanced medical treatment due to COVID-19. Hence, the results from this study are important in the aspect of treatment aggression and disease prevention. Obese patients with COVID-19 should be treated as a higher risk population. In the aspect of prevention, while staying home has been campaigned globally to reduce COVID-19 rapid transmission, in long term, it may simultaneously increase the susceptibility of people to develop obesity, a risk factor to develop severe COVID-19.
Funding
This systematic review was funded by the Universitas Indonesia’s research grant. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author contribution
Idea and study design: DLT; Data collection and analysis: AT, DLT; Article draft writing: AT; Draft revision: DLT; Writing supervision: DLT. All authors have read the manuscript and have approved this submission.
Declaration of competing interest
The authors declare no conflict of interest.
References
- 1.Worldometer. Coronavirus update (live): 2,902,708 Cases and 202,179 deaths from COVID-19 virus pandemic. 2020. https://www.worldometers.info/coronavirus/#countries [Internet], [cited 2020 Apr 26]. Available from:
- 2.Guarner J. Three emerging coronaviruses in two decades: the story of SARS, MERS, and now COVID-19. Am J Clin Pathol. 2020;153(4):420–421. doi: 10.1093/ajcp/aqaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020. http://www.ncbi.nlm.nih.gov/pubmed/32250385 [Internet]Available from: [DOI] [PMC free article] [PubMed]
- 4.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang B., Li R., Lu Z., Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 2020;12(7):6049–6057. doi: 10.18632/aging.103000. http://www.ncbi.nlm.nih.gov/pubmed/32267833 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020;S1201–9712(20) doi: 10.1016/j.ijid.2020.03.017. 30136–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dietz W., Santos-Burgoa C. Obesity and its implications for COVID-19 mortality. Obesity. 2020 doi: 10.1002/oby.22818. https://onlinelibrary.wiley.com/doi/full/10.1002/oby.22818 [DOI] [PubMed] [Google Scholar]
- 8.Davenport L., Nainggolan L. Obesity link to severe COVID-19, especially in the under 60s. 2020. https://www.medscape.com/viewarticle/928836 [Internet] [cited 2020 Apr 18]. Available from:
- 9.World Health Organisation . vol. 894. World Health Organization technical report series; Switzerland: 2000. Obesity: preventing and managing the global epidemic. (Report of a WHO consultation). [PubMed] [Google Scholar]
- 10.Consultation W.E. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004 Jan 10;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 11.World Health Organisation Obesity and overweight. 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [Internet] [cited 2020 Apr 25]. Available from:
- 12.De Heredia F.P., Gómez-Martínez S., Marcos A. Chronic and degenerative diseases: obesity, inflammation and the immune system. Proc Nutr Soc. 2012;71(2):332–338. doi: 10.1017/S0029665112000092. [DOI] [PubMed] [Google Scholar]
- 13.Hegde V., Dhurandhar N.V. Microbes and obesity-interrelationship between infection, adipose tissue and the immune system. Clin Microbiol Infect. 2013;19:314–320. doi: 10.1111/1469-0691.12157. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 14.Ni Y.N., Luo J., Yu H., Wang Y.W., Hu Y.H., Liu D. Can body mass index predict clinical outcomes for patients with acute lung injury/acute respiratory distress syndrome? A meta-analysis. Crit Care. 2017;21:36. doi: 10.1186/s13054-017-1615-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D., Liberati A., Tetzlaff J., Altman D.G., Altman D., Antes G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E., Villamizar-Peña R., Holguin-Rivera Y., Escalera-Antezana J.P. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101623. [Internet] (March):101623. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu J., Li W., Shi X., Chen Z., Jiang B., Liu J. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19) J Intern Med. 2020 doi: 10.1111/joim.13063. https://onlinelibrary.wiley.com/doi/full/10.1111/joim.13063 [DOI] [PubMed] [Google Scholar]
- 18.Lighter J., Philips M., Hochman S., Sterling S., Johnson D., Francois F. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin Infect Dis. 2020;ciaa415 doi: 10.1093/cid/ciaa415. https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa415/5818333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22831. https://onlinelibrary.wiley.com/doi/abs/10.1002/oby.22831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuba K., Imai Y., Rao S., Gao H., Guo F., Guan B. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11(8):875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jia X., Yin C., Lu S., Chen Y., Liu Q., Bai J. Two things about COVID-19 might need attention. Preprints. 2020 doi: 10.20944/preprints202002.0315.v1. https://www.preprints.org/manuscript/202002.0315/v1 [DOI] [Google Scholar]
- 22.Watson R.A., Pride N.B., Thomas E.L., Fitzpatrick J., Durighel G., McCarthy J. Reduction of total lung capacity in obese men: comparison of total intrathoracic and gas volumes. J Appl Physiol. 2010/03/18. 2010 Jun;108(6):1605–1612. doi: 10.1152/japplphysiol.01267.2009. https://pubmed.ncbi.nlm.nih.gov/20299612 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Campos E.C., Peixoto-Souza F.S., Alves V.C., Basso-Vanelli R., Barbalho-Moulim M., Laurino-Neto R.M. Improvement in lung function and functional capacity in morbidly obese women subjected to bariatric surgery. Clin (Sao Paulo). 2018;73:e20. doi: 10.6061/clinics/2018/e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moser J.A.S., Galindo-Fraga A., Ortiz-Hernández A.A., Gu W., Hunsberger S., Galán-Herrera J.F. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influ Other Respi Viruses. 2019;13:3–9. doi: 10.1111/irv.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Badawi A., Ryoo S.G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]