Supplemental Digital Content is available in the text.
Keywords: benefit, first come first served, intensive care unit, pandemic, triage
Abstract
Objectives:
Coronavirus disease 2019 patients are currently overwhelming the world’s healthcare systems. This article provides practical guidance to front-line physicians forced to make critical rationing decisions.
Data Sources:
PubMed and Medline search for scientific literature, reviews, and guidance documents related to epidemic ICU triage including from professional bodies.
Study Selection:
Clinical studies, reviews, and guidelines were selected and reviewed by all authors and discussed by internet conference and email.
Data Extraction:
References and data were based on relevance and author consensus.
Data Synthesis:
We review key challenges of resource-driven triage and data from affected ICUs. We recommend that once available resources are maximally extended, triage is justified utilizing a strategy that provides the greatest good for the greatest number of patients. A triage algorithm based on clinical estimations of the incremental survival benefit (saving the most life-years) provided by ICU care is proposed. “First come, first served” is used to choose between individuals with equal priorities and benefits. The algorithm provides practical guidance, is easy to follow, rapidly implementable and flexible. It has four prioritization categories: performance score, ASA score, number of organ failures, and predicted survival. Individual units can readily adapt the algorithm to meet local requirements for the evolving pandemic. Although the algorithm improves consistency and provides practical and psychologic support to those performing triage, the final decision remains a clinical one. Depending on country and operational circumstances, triage decisions may be made by a triage team or individual doctors. However, an experienced critical care specialist physician should be ultimately responsible for the triage decision. Cautious discharge criteria are proposed acknowledging the difficulties to facilitate the admission of queuing patients.
Conclusions:
Individual institutions may use this guidance to develop prospective protocols that assist the implementation of triage decisions to ensure fairness, enhance consistency, and decrease provider moral distress.
Patients with life-threatening illnesses admitted to ICUs have lower mortalities than patients not admitted (1, 2). Despite international variations in ICU services (3), demand for ICU beds frequently exceeds their supply (1, 2). Whereas resource-driven triage decisions are uncommon in North America, they are more frequent in Europe (2). During a pandemic or mass disaster medical resources may become desperately inadequate with patients dying because of the lack ventilators or ICU beds as is currently occurring in the coronavirus disease 2019 (COVID-19) pandemic (4). The present recommendations are based on the joint collaboration of several worldwide clinicians who have been involved in ICU triage during epidemics and other surge conditions for several decades.
ICU TRIAGE UNDER “NORMAL” CONDITIONS
Once patients meet ICU inclusion criteria, the most commonly recommended triage criteria for ICU admission under “normal” circumstances are “medical benefit” or “first come, first served” (5, 6). Patients who are “too well” or “too sick” to achieve a substantial benefit threshold would not be part of the potential pool. The now quite old Society of Critical Care Medicine triage consensus (5) stated that “The foremost consideration in triage decisions is the expected outcome of the patient in terms of survival and function, which turns on the medical status of the patient. In general, patients with good prognoses for recovery have priority over patients with poor prognoses.” In contrast, the American Thoracic Society recommended that “when demand for ICU beds exceeds supply, medically appropriate patients should be admitted on a first-come, first-served basis” (6).
An updated triage consensus statement unanimously found that triage decisions should give priority for patients with greater benefit and not be made on a “first come, first served basis” (7). Interestingly, in an attempt to develop a survival cutoff for triage decisions, only 77% of respondents agreed to a survival cutoff of 0.1% (7). This may be related to intensivists attempting to rescue with an ICU trial even patients with little chance of surviving knowing that they can later discharge the patient or limit treatments (7). Recent statements on ICU triage also recommended that patients be admitted based on their potential for benefit (8–10). Most statements declared that triage criteria should be explicit, fair, disclosed in advance and not be based on race, ethnicity, sex, sexual preference, financial status, or social worth (5–10). Unfortunately, current triage tools using objective prioritization, diagnosis, or parameter models are unable to provide ICU admission and exclusion criteria with demonstrated improved outcomes (8). Although attempts have been made to develop objective, triage scores (11), none are currently being used. Some triage scoring tools have been specifically developed for use in epidemics; however, none have been validated in a crisis setting (12–17).
The question arises as to how should “first come, first served” and “medical benefit” be defined for ICU admission? As only a few patients are admitted to an ICU every day and beds are either available for incoming patients or can be made available by discharging patients, the “first come, first served” criteria can usually be used for one patient after another. Unfortunately, there are occasions where more than one patient is vying for the last ICU bed. How should the “first patient” be defined when determining “first come, first served” criteria? Is it the first patient admitted to the emergency department, the first patient that the triage officer heard about, the patient in the operating room for whom an ICU bed was reserved, or the first patient that the triage physician accepted? In addition, if there is more than one ICU admission candidate how should “medical benefit” be defined? Is it saving the most lives or saving the most life-years with ICU care for potential patients or the incremental medical benefit between ICU care versus ward care in these patients (10)? If the latter, how much larger must the difference in benefit be? The South African consensus guideline recommended a benefit difference of 15–25% (10). Although intensivists prognosticate more accurately than scoring systems (18), uncertainty remains and physicians’ accuracy lacks the consistency and precision patient desire.
TRIAGE DURING A PANDEMIC OR MASS DISASTER WITH OVERWHELMING SHORTAGES
This article deals only with ICU triage. Complete information related to surge capacity, coordination and collaboration, manpower, essential equipment, pharmaceuticals and supplies, protection of patients and staffing, medical procedures, and education for pandemics can be found elsewhere (19). As difficult as triage decisions are during everyday practice, they are even more challenging during pandemics or mass disasters. Pandemics produce countless critically ill patients that overrun healthcare resources (19). In extreme situations, customary interventions and standards of practice may be unachievable leading to avertible deaths (20, 21). Establishing equitable and just strategies for “the greatest good for the greatest number” of patients may demand decreasing ICU therapies to patients who ordinarily would be expected to benefit from them under conditions of adequate resources (20, 21).
Because of these dilemmas several objective, ICU triage protocols, tools, and scores were developed to prioritize limited reserves, reduce additional deaths and help avoid clinical judgments which might be more protracted and less reliable (12–17). Unfortunately, these tools have been shown to have inadequate performance and many patients classified as too sick to require admission survived (14, 16).
ICU triage of patients remains challenging and controversial in pandemics when resources are overwhelmed. Recommendations for ICU triage for appropriate candidates during pandemics have suggested that either “medical benefit” or a “first come, first served” is acceptable (20, 21) or an improved incremental survival rather than a “first come, first served basis” (22). More recently proposals have been for saving the most lives (23) or saving the most life-years (24). The current COVID-19 pandemic has witnessed the use of age as a criteria, primarily because advanced age appears strongly associated with poorer outcomes (4).
INFORMATION FROM THE PRESENT COVID-19 PANDEMIC
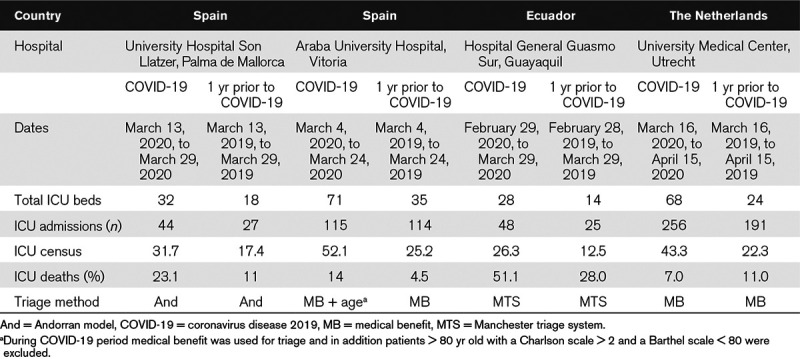
China, Italy, Spain, and the Americas have had major severe acute respiratory syndrome coronavirus 2 outbreaks and mortality. Triage data from some ICUs affected by the COVID-19 pandemic are shown in Table 1. ICU beds and daily census increased approximately double from the previous year. It is too early to evaluate mortality which should be relevant at 28 days after admission. Recent reports of moderately high population mortality from COVID-19 in China (61.5%) (25) and high ICU mortality in the United States (67%) (26) are worrisome. It has been suggested that the high mortality maybe related to the large bed expansion without adequate healthcare resources (27). This has implications for expansions that are currently occurring worldwide. Experience from severe acute respiratory syndrome (SARS) showed that rapid and excessive expansion may overwhelm staff leading to excess infections in healthcare workers and compromising care (28). Thus expansion should be matched by safe staffing to guarantee an appropriate quality of care and staff safety which necessarily limits expansion. A consensus group with first-hand experience of outbreak expansion during SARS concluded that safe expansion is realistically limited by availability of acceptably trained staff and limited to a maximum expansion of 50–100% of baseline capacity (29). Hospitals must also balance ICU needs and the potential decreasing benefits of increasing ICU capacity due to excess workload with other hospital needs (20).
TABLE 1.
ICU Utilization and Outcomes in Three Countries During the Coronavirus Disease 2019 Pandemic Surge
Compassionate care should be offered to patients with low-level priorities. There are anecdotal reports that they can survive or delay intubation until more resources are available using awake prone position (30) in hospital wards because of the shortage of ventilators or ICU beds (J. Rello, personal communication, 2020).
ICU TRIAGE DURING A PANDEMIC
How should triage decisions be made during the COVID-19 pandemic? It is strongly recommended that institutions develop prospective, objective protocols or algorithms to assist the implementation of their triage decisions to enhance consistency (31) and decrease moral distress among providers (24, 32). First, when demand surges hospitals must increase ICU capacity by 100–200% (20, 33) before triage is instituted. Triage protocols should only be triggered when resources across a broad geographic area are or will be overwhelmed despite efforts to extend them and systems move from contingency to crisis mode (20). As we can predict a wave of incoming patients from an impending peak in COVID-19, it might be prudent to start rationing prior to expending all resources on early cases with low probabilities for survival when it is clear that maximum surge capacity will certainly be exceeded in the near future. If hospitals cannot provide services, they should consider transferring patients to cities where ICU beds are still available (20). Second, the potential ICU patients should be those that meet inclusion and no exclusion criteria. There is no perfect tool. In deciding which tool to use, we chose a tool that was simple, easy to understand and use and most important providing for quick assessments. As different countries and regions have different infrastructures and resources, laws, cultures, and religions, we attempted to offer flexibility in our recommendations along with explanations for the differing opinions so each region or country can choose what is most appropriate for them.
An illustrative example of inclusion and exclusion criteria and an algorithm for ICU triage is found in Figure 1 and Supplemental Figure 1 (Supplemental Digital Content 1, http://links.lww.com/CCM/F519; legend, Supplemental Digital Content 2, http://links.lww.com/CCM/F520). Admission priority is given to patients from priority 1 to 4 based on their performance scores, ASA score, number of organ failures, and predicted survival. If there are more priority 1 patients than beds, allocation will be based on incremental ICU benefit defined as saving the most life-years (evaluating mortality from both acute and chronic disorders) (24). If there is a tie for ICU candidates, clinicians should use first come, first served (34) which they are accustomed to using and not a random allocation with a lottery (which they are not familiar using, losing valuable time). We recommend that the first-come patient should be defined as the first patient that the triage officer was informed of. The triage algorithm should apply equally to all ICU candidates with and without COVID-19 (35). When the triage protocol commences, all ICU patients must be reevaluated for remaining in the ICU based on these same criteria.
Figure 1.
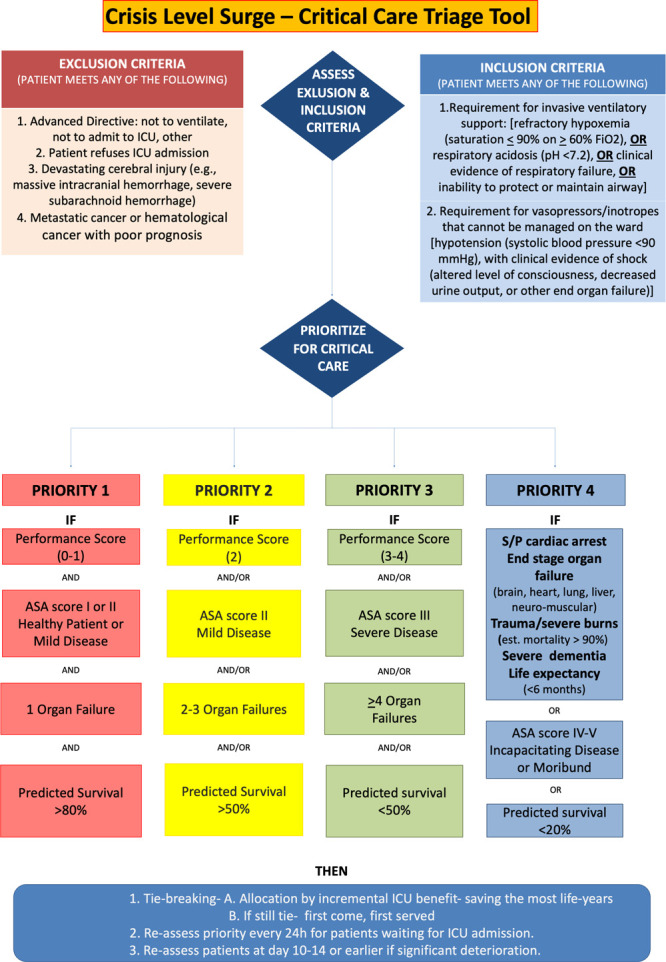
This tool provides an element of objectivity to help enhance consistency. It is not considered, however, a complete substitute for the carefully considered judgment of an experienced intensive care clinician. The presented algorithm is an example and each institution can decide on which performance score, comorbidities, and organ system failures to use based on their experience and what their staff ifs most comfortable using. A triage (prioritization) decision is a complex clinical decision made when ICU beds are limited. A structured decision-making process is important to maximize transparency and improve consistency in decision-making. A clinical estimation of likely benefit (outcomes from ICU admission compared with outcomes expected if the patient remained on the ward/other care area) is necessary so that patients who will benefit most from ICU are given priority. Examples of clinical conditions that the expert group believe would likely result in a failure of a patient to meet sufficient priority for admission is provided (priority 4). This conceptual algorithm outlines a recommended process for making an individual triage decision, based on a likelihood that survival without ICU care would be low (5–10% or less), and if admission criteria as laid out are met, survival would be estimated to be in excess of 50% short- to medium-term survival. The initial exclusion criteria are based on exclusion criteria used under “normal” conditions so that the same patients are eligible during pandemic conditions and given priority based on their likelihood to benefit. Then patients must meet one of the inclusion criteria. Priorities are then based on those to be “considered first” (priority 1 and then priority 2) and “considered last” (priority 3 and then priority 4) with priority ranking from priority 1 to 4. These exclusions should help foster trust in a fairer triage system with less chance of discrimination. Each decision is assisted on the basis of an agreed criterion thresholds for the particular ICU at a specific time and will be dependent on available resources and the number of patients queuing for admission (e.g., stricter thresholds may be required during the peak of the pandemic, and less strict thresholds at the beginning and toward the end). The performance scores, comorbidities, and organ system failure variables chosen for this example are those that are the quickest to assess. Performance scores: The premorbid baseline condition can be assessed using the Eastern Cooperative Oncology Group Performance Score, the Clinical Frailty Score, the Karnofsky Performance Scale, or other functional impairment tool the user is accustomed. Comorbidities can be assessed using the ASA score, number, or severity of comorbidities. Organ system failures can be assessed using the number of organ system failures or Sequential Organ Failure Assessment. Reevaluations for admitted and refused patients should be performed ideally every 24 hr. At reassessment of patients at days 10–14 or if significant deterioration or lack of improvement in the patient’s condition occurs decreasing the patient’s predicted survival to below the current priority group receiving critical care, reallocation of ventilator/ICU bed (following review by triage committee) should be considered. Status/post (S/P) cardiac arrest refers to patients with a recent cardiac arrest or one leading to significant anoxic brain damage.
Who Will Perform the Triage?
In an ideal situation, we should have a separate triage officer/committee for making admission and discharge triage decisions (5, 35). Whether this is feasible will depend on the country and magnitude of the crisis. Many intensivists believe that only a senior physician with triage experience can make these decisions and be part of such a committee. Are there enough intensivists to provide care and be part of a triage committee? Can other physicians along with other professionals without triage experience triage patients in a pandemic? If an institution creates a committee, it could include doctors (expertise in administration or palliative care maybe particularly helpful), nurses, social workers, and ethicists. Decisions should be made by senior physicians with triage experience. As intensivists who have become invested in the care of a patient over time may have difficulties withdrawing ventilation (32) or discharging patients to wards under these difficult conditions, the institutional triage or ethics committee could be helpful in affirming and endorsing the decision taken by a senior intensivist or making the decisions themselves. Admission, discharge or limitation decisions must be communicated to the patient or family. The public prefers that triage be performed by senior doctors and that predetermined criteria be used (36). If patient surge exceeds the number of available critical care trained specialists, intensivists should supervise nonintensivist physicians (20).
Patient Priority
1) Healthcare and other essential workers: There is controversy in the literature and there were differences of opinion among authors about prioritizing front-line healthcare and other essential workers. A consensus stated that it is unlikely that workers becoming critically ill during a pandemic will recover sufficiently for them to return to work (31). In addition, conferring priority for healthcare workers could hinder societal trust in the triage mechanism at a time when public trust is essential. On the other hand, healthcare and other essential workers put themselves at high-risk supporting or saving others and are irreplaceable and essential for society and patient care (24, 35). Some workers have been infected because they were not provided with adequate protection (37). As COVID-19 may have a long duration and could recur, it is increasingly plausible that healthcare workers could return later to work. However, as healthcare workers have a clear conflict of interest as “self advocates,” we recommend this prioritization should be decided and implemented by societal and governmental agencies. Defining essential workers at the time of triage poses a practical problem, but consideration could be given to those workers excluded from lockdown as defined by official national, regional, and local orders. Because of the controversy, each country should decide what is most appropriate for their citizenry.
2) Younger patients: Age has also been suggested for ICU triage decisions. In Italy, patients are dying from COVID-19 because they have been triaged not to receive a ventilator because of their age (4). Advocates suggest that younger patients should be prioritized to have an equal opportunity to pass through the stages of life (24). Despite the fact that elderly patients have a higher ICU mortality than younger patients, the incremental ICU benefit is greater for the elderly as patients more than 65 years had a greater difference in mortality between admitted and rejected patients compared with younger patients (2). Although age should be taken into consideration along with other variables, age should not be the sole determining factor in triage decisions (7). What is important is physiologic and not chronological age (7). Younger patients have been taken into consideration by using incremental ICU benefit defined as saving the most life-years.
Staff Protection
Staff will have anxiety about personal and family risks, distress about avoidable deaths and patient limitations, potential failings from working outside areas of normal expertise, or excessive workload and death of family, friends, and colleagues (38). Therefore, institutions must do their utmost to decrease clinical risks, providing adequate protective supplies and education, maintain staff confidence and safety by minimizing risks and maintaining appropriate services and reassurance with legal protection so there are adequate staff to man the beds (38).
ICU Discharge Criteria
Even under “normal” circumstances intensivists agree that patients with little or no anticipated benefit from continued ICU interventions may be discharged from the ICU (7). During a pandemic, all admitted patients should be admitted with the intention of carrying out a time-limited trial of therapy (39) so that if ICU care does not significantly improve the patient’s condition after a reasonable time, the patient should be discharged and/or therapies limited (7). Reevaluations for admitted and refused patients should be performed when appropriate and feasible ideally every 24 hours. As COVID-19 patients tend to have longer ICU durations (25) reassessments for remaining in the ICU should occur later, at days 10–14. When faced with overwhelming resource restrictions, it may be justified to limit life support therapy or discharge a patient with very poor survival prognosis after admission to ICU to allow queuing patients with a much higher probability of benefit to be admitted. This process will be difficult to implement, and we recommend that such decisions which are not as time critical be made by broad consensus. A decision by more than one senior ICU clinician, an independent physician and possibly the triage committee could serve to enhance fairness, consistency and mitigate the moral distress associated with such decisions.
Monitoring
Because different parts of the world have different views on trust and empowerment, requirements for decisions to be reviewed regularly by monitoring committees to ensure that there are no inappropriate inequities and to regularly review the triage tool will vary (4). It is also essential that the outcome of patients who are triaged is tracked to ensure that triage is effectively targeting resources to those who are most likely to benefit as indicated by improved survival rates overall.
As there can be no universal formula to guide the implementation of ICU triage, each region or country will have to make its own decisions as to what will be best for its system. We do, however, recommend that these protocols be guided by the principles discussed in this article and be flexible based on the severity of the pandemic demands and available resources. Most importantly prospectively defined criteria and protocols should be announced in advance, be explicit, fair and just without biases, and provide maximize consistency in decision-making. Changes may be required in the triage tool and other recommendations as more knowledge about COVID-19 develops. Although intensivists make difficult decisions daily, they pale with the triage decisions currently being made with the COVID-19 pandemic. Courage lies not in making gut-wrenching, triage decisions but living with them. Failing to make and implement necessary triage is certainly worse than making a poor choice. During these difficult times, it is important to maintain our professionalism but also preserve our humanity and sensitivity to suffering patients and families, especially those with different cultures and religions.
ACKNOWLEDGMENTS
We thank our colleagues who provided coronavirus disease 2019 (COVID-19) data while caring for their many patients. Marcio Borges Sa, MD, and Maria Aranda Perez, MD, ICU, University Hospital Son Llatzer, IDISBA, Palma de Mallorca, Spain; Department of Intensive Care Medicine, Araba University Hospital, Vitoria, Spain; José Vergara Centeno, MD and Cynthia Campozano Burgos, MD, Hospital General Guasmo Sur, Guayaquil, Ecuador; and Jozef Kesecioglu, MD, PhD, University Medical Center, Utrecht, The Netherlands. We offer our heartfelt thanks to healthcare workers around the world for their skill in caring for COVID-19 patients and who also cared for two of the contributors to this article with COVID-19.
Supplementary Material
Footnotes
*See also pp. 1241 and 1243.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
REFERENCES
- 1.Simchen E, Sprung CL, Galai N, et al. Survival of critically ill patients hospitalized in and out of intensive care units under paucity of intensive care unit beds. Crit Care Med 2004; 32:1654–1661 [DOI] [PubMed] [Google Scholar]
- 2.Sprung CL, Artigas A, Kesecioglu J, et al. The Eldicus prospective, observational study of triage decision making in European intensive care units. Part II: Intensive care benefit for the elderly. Crit Care Med 2012; 40:132–138 [DOI] [PubMed] [Google Scholar]
- 3.Wunsch H, Angus DC, Harrison DA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med 2008; 36:2787–2793, e1–e9 [DOI] [PubMed] [Google Scholar]
- 4.Rosenbaum L. Facing Covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020 Mar 18. [online ahead of print] doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 5.Consensus statement on the triage of critically ill patients. Society of Critical Care Medicine. Ethics Committee. JAMA 1994; 271:1200–1203 [PubMed] [Google Scholar]
- 6.American Thoracic Society Bioethics Task Force. Fair allocation of intensive care unit resources. Am J Respir Crit Care Med 1997; 156:1282–1301 [DOI] [PubMed] [Google Scholar]
- 7.Sprung CL, Danis M, Iapichino G, et al. Triage of intensive care patients: Identifying agreement and controversy. Intensive Care Med 2013; 39:1916–1924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nates JL, Nunnally M, Kleinpell R, et al. Intensive care unit admission, discharge, and triage guidelines: A framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med 2016; 44:1553–1602 [DOI] [PubMed] [Google Scholar]
- 9.Blanch L, Abillama FF, Amin P, et al. Council of the World Federation of Societies of Intensive and Critical Care Medicine. Triage decisions for ICU admission: Report from the Task Force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care 2016; 36:301–305 [DOI] [PubMed] [Google Scholar]
- 10.Joynt GM, Gopalan DP, Argent AA, et al. The Critical Care Society of Southern Africa Consensus Statement on ICU Triage and Rationing (ConICTri). S Afr Med J 2019; 109:613–629 [DOI] [PubMed] [Google Scholar]
- 11.Sprung CL, Baras M, Iapichino G, et al. The Eldicus prospective, observational study of triage decision making in European intensive care units: Part I–European intensive care admission triage scores. Crit Care Med 2012; 40:125–131 [DOI] [PubMed] [Google Scholar]
- 12.Talmor D, Jones AE, Rubinson L, et al. Simple triage scoring system predicting death and the need for critical care resources for use during epidemics. Crit Care Med 2007; 35:1251–1256 [DOI] [PubMed] [Google Scholar]
- 13.Christian MD, Hamielec C, Lazar NM, et al. A retrospective cohort pilot study to evaluate a triage tool for use in a pandemic. Crit Care 2009; 13:R170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guest T, Tantam G, Donlin N, et al. An observational cohort study of triage for critical care provision during pandemic influenza: ‘clipboard physicians’ or ‘evidenced based medicine’? Anaesthesia 2009; 64:1199–1206 [DOI] [PubMed] [Google Scholar]
- 15.Adeniji KA, Cusack R. The Simple Triage Scoring System (STSS) successfully predicts mortality and critical care resource utilization in H1N1 pandemic flu: A retrospective analysis. Crit Care 2011; 15:R39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shahpori R, Stelfox HT, Doig CJ, et al. Sequential organ failure assessment in H1N1 pandemic planning. Crit Care Med 2011; 39:827–832 [DOI] [PubMed] [Google Scholar]
- 17.Myles PR, Nguyen-Van-Tam JS, Lim WS, et al. Comparison of CATs, CURB-65 and PMEWS as triage tools in pandemic influenza admissions to UK hospitals: Case control analysis using retrospective data. PLoS One 2012; 7:e34428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sinuff T, Adhikari NK, Cook DJ, et al. Mortality predictions in the intensive care unit: Comparing physicians with scoring systems. Crit Care Med 2006; 34:878–885 [DOI] [PubMed] [Google Scholar]
- 19.Sprung CL, Cohen R, Adini B; European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster: Recommendations and standard operating procedures for intensive care unit and hospital preparations for an influenza epidemic or mass disaster. Intensive Care Med 2010; 36(Suppl 1):S4–S79 [DOI] [PubMed] [Google Scholar]
- 20.Sprung CL, Zimmerman JL, Christian MD, et al. ; European Society of Intensive Care Medicine Task Force for Intensive Care Unit Triage during an Influenza Epidemic or Mass Disaster: Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: Summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med 2010; 36:428–443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christian MD, Joynt GM, Hick JL, et al. ; European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster: Chapter 7. Critical care triage. Recommendations and standard operating procedures for intensive care unit and hospital preparations for an influenza epidemic or mass disaster. Intensive Care Med 2010; 36(Suppl 1):S55–S64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Christian MD, Sprung CL, King MA, et al. ; Task Force for Mass Critical Care: Triage: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014; 146:e61S–e74S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ventilator Allocation Guidelines: New York State Task Force on Life and the Law New York State Department of Health. 2015. Available at: https://www.health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf. Accessed April 28, 2020
- 24.White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020 Mar 27 doi: 10.1001/jama.2020.5046. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020 Feb 24. [online ahead of print] doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020; 323:1612–1614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ji Y, Peppelenbosch MK, Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health 2020; 8:e480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Report of the Select Committee to Inquire Into the Handling of the Severe Acute Respiratory Syndrome Outbreak by the Government and the Hospital Authority. 2004 Available at: https://www.legco.gov.hk/yr03-04/english/sc/sc_sars/reports/sars_rpt.htm. Accessed April 28, 2020.
- 29.Gomersall CD, Tai DY, Loo S, et al. Expanding ICU facilities in an epidemic: Recommendations based on experience from the SARS epidemic in Hong Kong and Singapore. Intensive Care Med 2006; 32:1004–1013 [DOI] [PubMed] [Google Scholar]
- 30.Bamford P, Bentley A, Dean J, et al. Intensive Care Society Guidance for Prone Positioning of the Conscious COVID Patient 2020. Available at: https://emcrit.org/wp-content/uploads/2020/04/2020-04-12-Guidance-for-conscious-proning.pdf. Accessed April 28, 2020.
- 31.Biddison LD, Berkowitz KA, Courtney B, et al. ; Task Force for Mass Critical Care: Ethical considerations: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014; 146:e145S–e155S [DOI] [PubMed] [Google Scholar]
- 32.Truog RD, Mitchell C, Daley GQ. The toughest triage - allocating ventilators in a pandemic. N Engl J Med. 2020 Mar 23. [online ahead of print] doi: 10.1056/NEJMp2005689. [DOI] [PubMed] [Google Scholar]
- 33.Devereaux A, Christian MD, Dichter JR, et al. ; Task Force for Mass Critical Care: Summary of suggestions from the Task Force for Mass Critical Care summit, January 26–27, 2007. Chest 2008; 133(Suppl 5):1S–7S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Winsor S, Bensimon CM, Sibbald R, et al. Identifying prioritization criteria to supplement critical care triage protocols for the allocation of ventilators during a pandemic influenza. Healthc Q 2014; 17:44–51 [DOI] [PubMed] [Google Scholar]
- 35.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020 Mar 23 doi: 10.1056/NEJMsb2005114. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 36.Cheung W, Myburgh J, McGuinness S, et al. A cross-sectional survey of Australian and New Zealand public opinion on methods to triage intensive care patients in an influenza pandemic. Crit Care Resusc 2017; 19:254–265 [PubMed] [Google Scholar]
- 37.Ranney ML, Griffeth V, Jha AK. Critical supply shortages - the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020 Mar 25 doi: 10.1056/NEJMp2006141. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 38.Taylor BL, Montgomery HE, Rhodes A, et al. ; European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster: Chapter 6. Protection of patients and staff during a pandemic. Recommendations and standard operating procedures for intensive care unit and hospital preparations for an influenza epidemic or mass disaster. Intensive Care Med 2010; 36(Suppl 1):S45–S54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vink EE, Azoulay E, Caplan A, et al. Time-limited trial of intensive care treatment: An overview of current literature. Intensive Care Med 2018; 44:1369–1377 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


