Abstract
Background
A novel coronavirus disease (COVID-19) was first reported in December 2019 in China and was soon declared a pandemic by World Health Organization. Many elective and non-essential surgeries were postponed worldwide in an effort to minimize spread of disease as well as to conserve resources. Our goal with this article is to review current practice guidelines in setting of the COVID-19 pandemic, based on available data and literature.
Methods
Websites pertaining to surgical and medical societies, and government agencies were reviewed, along with recently published literature to identify recommendations related to COVID-19 and plastic surgery procedures.
Results
Clinical practice modifications are recommended during the pandemic, in outpatient and perioperative settings. Use of personal protective equipment is critical for aerosol generating procedures such as surgery in the head and neck area. Care for trauma and malignancy should continue during the pandemic, however definitive reconstruction could be delayed for select cases. Specific recommendations were made for surgical treatment of cancer, trauma and semi-urgent reconstructive procedures based on available data and literature.
Conclusion
The risk and benefit of each reconstructive procedure should be carefully analyzed in relation to necessary patient care, minimized COVID-19 spread, protection of health care personnel and utilization of resources. Recommendations in this manuscript should be taken in the context of each institute’s resources and prevalance of COVID-19 in the region. It should be emphasized that the guidelines provided are a snapshot of current practices and are subject to change as the pandemic continues to evolve.
Keywords: COVID-19, Pandemic, plastic surgery, triage, reconstruction, Head and Neck, maxillofacial, Breast reconstruction, skin cancer, Hand Surgery, SARS-CoV-2, Coronavirus
BACKGROUND
A novel human coronavirus named “severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)” was first reported in Wuhan, China in December 2019, and the outbreak of coronavirus disease 2019 (COVID-19) was declared a pandemic by World Health Organization on March 11th, 2020.1 As of April 24th 2020, there are 2,626,321 confirmed cases of COVID-19 worldwide, 181,938 of which resulted in death.2 In comparison to prior coronavirus outbreaks (2003 SARS pandemic and 2012 MERS outbreak) SARS-CoV-2 so far has shown a lower case-fatality rate. 3,4 However, potential transmission from minimally symptomatic and even asymptomatic patients 3,5 has posed difficulties in regards to case detection and isolation strategies. 3 Means of transmission include respiratory droplets, direct human contact, fecal-oral route, aerosol and fomite (contaminated surface) transmission. 4,6–11 Duration of viral shedding has been reported from 1 to 37 days 12,13 and critically ill patients may possess an enhanced ability of viral shedding. 14
As the outbreak spreads, intensive research on vaccine development and medical treatment continues worldwide. 15–21 However, to-date, there is no widely available and effective medical treatment or prevention against COVID-19. Health care personnel (HCP) continue to work at the frontlines, at risk of contracting the disease, while providing care to many patients in need. A recent publication from the Chinese Center for Disease Control and Prevention reported that out of 44,672 COVID-19 cases, 3.8% were HCP. 22 This number was reported be as high as 9% in Italy.23
In the midst of the pandemic, non-essential procedures have been postponed or deferred in many countries per government recommendations. Almost all surgical disciplines have modified their operative approach in an attempt to off load the health care system. In the United States, as of March 2020, plastic surgeons have stopped performing elective procedures, in accordance with guidance from American Society of Plastic Surgeons, American College of Surgeons, American Medical Association, and Centers for Medicare & Medicaid Services .24–27 As we continue to carry out necessary reconstructive surgeries, the risk and benefit of each surgical procedure should be carefully analyzed. Our practice should reflect a balance of patient care, protection of HCP, minimized COVID-19 spread, and resource conservation.
Our goal with this article is to summarize practices in plastic surgery during the COVID-19 pandemic and provide recommendations regarding perioperative care and case prioritization based on current evidence. As more data becomes available, it is likely that the strategies outlined in this document will change accordingly.
OUTPATIENT VISITS
During the pandemic it is imperative that patients avoid unnecessary travel to health care facilities where they could expose themselves or others’ to further illness. Telemedicine services (audio and video calls) are now being offered for many non-urgent appointments, routine surveillance encounters, and follow-ups. In the United States, these visits are considered the same as in-person visits and are paid at same rate as regular, as per CMS guidelines.28 Physicians are encouraged to maintain relationship with patients using virtual visits to reassure continuation of care, instead of simply cancelling or postponing appointments.
If an in-person visit is indicated, patients must be querried about COVID-19 symptoms before they come in to the facility. During the visit, patients should be kept in one physical location if feasible and their interaction with multiple HCP should be minimized. Practitioners should carry out an expedient visit, use appropriate PPE, and perform a more focused physical exam.29 Clinical scenarios with a higher risk of disease transmission to practitioner include examination of ear, nose, mouth or throat, placement/removal of nasal packing, tracheostomy care or any procedure that involves manipulation of mucosa. Such procedures should be limited to patients who have a clear indication as infectious aerosols can remain in the room for three hours or more.10 Patients who are asymptomatic and untested should be approached as COVID-19 positive.
SURGICAL PROCEDURES
A judicious approach in clinical practice would be to to postpone all elective surgery, carrying out urgent and emergency procedures only, to preserve resources and minimize viral spread. (Table 1) 25,26,30,31 Allowable and appropriate operations are those where a delay would have significant negative impact on outcome of the condition. There are valuable resources from surgical and medical societies, and government agencies to help guide the decision making process in patient and procedure selection. We should also realize that regional prevalence of COVID-19 and individual institutional factors such as the availability of resources or patient’s need for postoperative care (i.e Intensive care unit (ICU) care) will impact decision making.
Table 1.
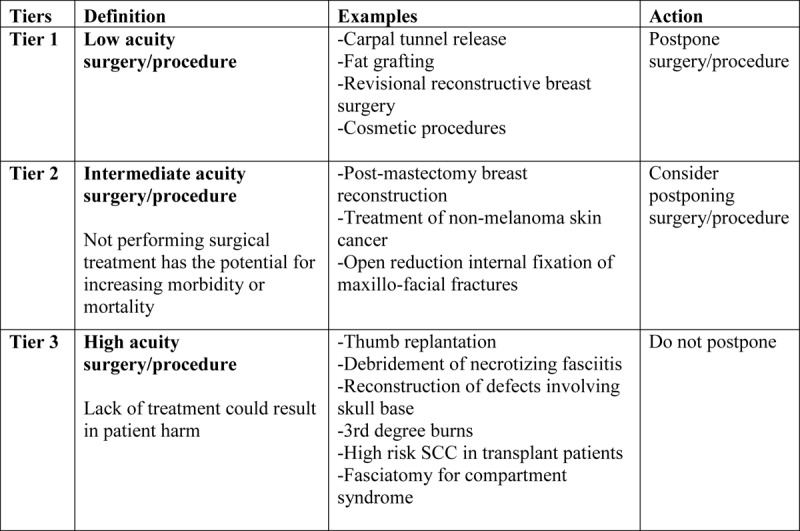
As the pandemic continues to evolve and hopefully declines, the scope of practice can be broadened according to emerging guidelines. Transitioning to normal function should be undertaken in a tiered approach. Recommendations in Table 1 can be employed in reverse order, i.e gradually resuming treatment of skin cancers, breast reconstructions and eventually phasing in all elective surgeries and cosmetic procedures. The transition is subject to change depending on the number of cases in that particular region, resources of individual institutions, as well as capacity of the health care system in general.
Below, we present recommendations for perioperative care as well as management of specific medical conditions, as it relates to plastic surgery practice.
Perioperative Care
The patient’s COVID-19 status should be determined prior to surgery, if possible. 25,32 Reverse transcriptase polymerase chain reaction (RT-PCR) is the preferred laboratory-test to-date 33,34, with diagnostic accuracy in the range of 56%-83%. 35,36 As availability and reliability of PCR tests increase, preoperative assessment of COVID-19 status will presumably become standard of practice. Patients who are positive should be operated in designated operating rooms with a team dedicated to their care.14,37–39 The positive pressure airflow environment of the operating room may enhance the risk of viral transmission, therefore conversion to negative-pressure airflow room should be considered.14 Since the viral pathogen survives on environmental surfaces for extended periods of time, usual cleaning practices may be inadequate and need adjustment. 10,40–42 Multi-faceted perioperative infection control will ensure that the patients are appropriately cared while the HCP is protected. 38,43,44 (Table 2)
Table 2.
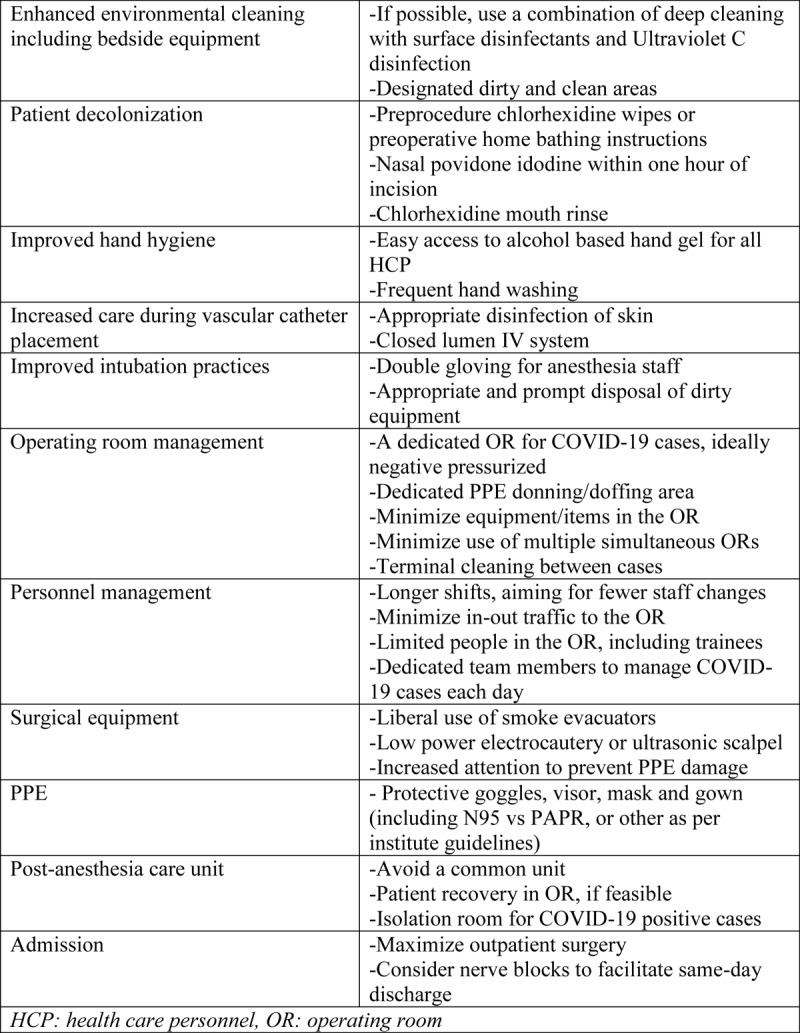
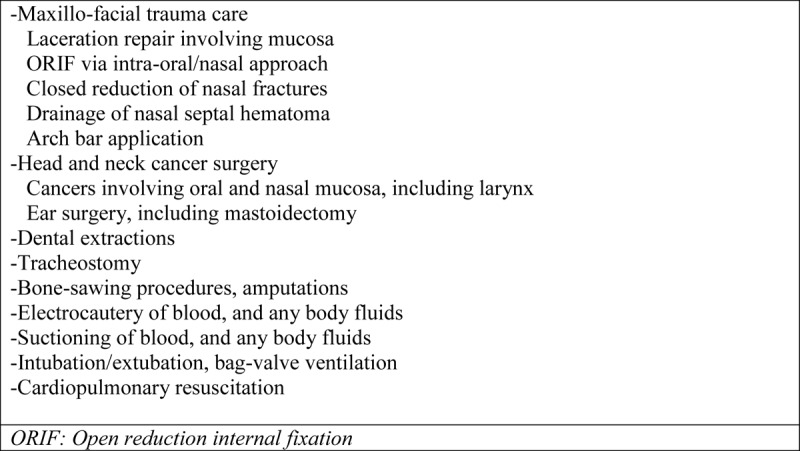
Another important step in delivering health care is identification of aerosol-generating procedures (AGPs), where more stringent precautions are advised due to a higher risk of disease transmission to health care personnel. Such procedures typically involve airway manipulation (i.e intubation), breach of mucosa, gastrointestinal tract surgery and thoracic surgery 14,29,45,46 The coronaviruses have been shown to be also present in the blood stream and body fluids 6,7,14,25,37,44 thus bone-sawing procedures and electro-cautery use is also related with increased potential exposure.44,47 A list of high risk AGPs that plastic surgeons may encounter are summarized in Table 3. 25,29,48
Table 3.
One of the most commonly debated topics in setting of COVID-19 pandemic is choice of personal protective equipment (PPE). Despite conflicting practices worldwide, use of respirator masks that efficiently filtrate airborne particles (i.e N95 respirator), eye protection and isolation gowns are usually recommended. 14,25,38,49 Most institutions have developed individual protocols adapted from guidelines of World Health Organization.50 Utilization of appropriate PPE during head and neck surgery is particularly important due to high risk of viral transmission. When performing high-risk aerosol generating procedures, health care personnel should wear a N95 mask with goggles/face shield, or powered air purifying respirators (PAPR), gown and double gloves to achieve adequate protection. 29 Practitioners are advised to take precautions regardless of COVID-19 status, as asymptomatic cases are not uncommon and testing may be limited.
Cancer care
Though cancer surgery is not considered elective, surgical interventions need prioritization. With diminished resources oncologists must consider what treatments are most likely to be successful, symptom relieving, or lifesaving. For select patients, delays in surgical treatment may be acceptable as they undergo neoadjuvant treatment.51 A multidisciplinary tumor board conference is most helpful to determine if the patient is a candidate for surgery versus alternative treatments or observation and should be documented in patient’s chart. Evidence shows that cancer patients have a higher risk of contracting COVID-19 and developing severe events related to disease necessitating ICU admission, along with higher mortality rate.52,53
Breast Cancer and Reconstruction
Depending on stage and receptor status of the tumor, endocrine therapy or neoadjuvant chemotherapy may precede surgery.54 Post-mastectomy reconstruction options will be limited, thus patients are encouraged to undergo breast conserving surgery when possible. A definitive mastectomy and/or reconstruction could be performed in a delayed fashion.54,55 Surgeons should consider only addressing the cancer side, and avoid contralateral operations that might prolong surgery. Delayed and revisional breast reconstruction surgeries are elective and thus should be postponed.55
Decisions about immediate breast reconstruction are less straightforward since the patient is being brought to the operating room by the breast surgeon. In general, plastic surgeons should err on the side of caution and delay reconstruction.55 Immediate reconstruction has higher risk of complications compared to mastectomy only, and utilizes additional resources such as PPE, operative time, multiple office visits. Tissue expander or direct to implant reconstruction can be offered on a case-by-case basis after careful evaluation of patient’s individual risk factors and a change in future reconstructive options (i.e anticipated radiation therapy).55 Autologous reconstruction (excluding cases that need wound coverage) should be deferred due to excessive use of resources.54–56
Skin Cancer
Surgical treatment of non-melanoma skin cancers with slow growth rate such as basal cell carcinoma (BCC) and low risk squamous cell carcinoma (SCC) are not regarded as urgent and may be postponed. Surgery can be considered for patients with high risk SCC (>4 cm, deep invasion, perineural invasion, or poor differentiation) 57, malignancies close to critical anatomical areas such as skull base, eyes and lip and rapidly progressing tumors in transplant patients. Non-surgical treatment options for advanced BCC and SCC such as cryotherapy, radical-intent radiotherapy, neoadjuvant use of cemiplimab or vismodegib may be considered as an alternative treatment approach, especially in high risk patients (i.e age>70, presence of comorbidities, immunosuppression).58–61 Merkel cell carcinoma excisions with/without sentinel lymph node biopsy (SLNB) should not be deferred during the pandemic as delay may cause progression and even distant metastasis.62
Diagnostic excisional biopsies for suspected melanoma are carried out with intent to remove the clinical lesion. For the biopsy proven malignant melanoma (any thickness) with clear histologic margins or in situ melanoma present at peripheral transection, wide local excision (WLE) can be delayed for up to 3 months. SLNB that is indicated for melanomas thicker than 0.8mm may be delayed for up to 3 months unless a WLE in the OR is planned, in which case SLNB may be performed simultaneously. Therapeutic lymph node dissections can be postponed and nodes kept under surveillance using US, CT, PET and MRI. If clinically palpable lymph nodes are present, neoadjuvant systemic therapy can be offered. In cases of metastatic nodes invading vital structures and those failing systemic therapy, therapeutic lymphadenectomy should be considered 63.
Head and Neck Cancer
Majority of the head and neck cutaneous and salivary gland malignancies are slow growing and treatment can be delayed for a few weeks or months with limited impact on oncologic outcome.58 However, oral mucosa cancers, human papilloma virus (HPV) negative oropharyngeal SCC and advanced laryngeal cancer are considered aggressive malignancies and therefore may need urgent surgical intervention to prolong survival, preserve organ function and/or avoid further harm from underlying disease.26 As a general rule, complex free flap reconstructions should be avoided. Primary closure, skin grafts, local/regional flaps are preferred to minimize morbidity and mortality that could result from extended operations and prolonged recovery period. Alternative treatment options such as chemotherapy and radiotherapy can be utilized in select cases. 64–66
Trauma and Emergency Care
As a result of diminished industrial work and restricted travel, there is reduced volume of acute injuries presenting to Emergency Rooms. Surgery should be performed if delaying the procedure may cause significant harm to the patient, is likely to prolong the hospital stay, or if there is no non-surgical treatment option. Plastic surgeons are frequently consulted for maxillofacial fractures and hand injury, approach to which is discussed in detail below. Other emergency room encounters needing immediate care include 3rd degree burns, necrotizing soft tissue infections, compartment syndromes and limb threatening injury.67 Select cases of lower extremity trauma with soft tissue loss may be temporized with vacuum assisted wound therapy until definitive reconstruction. However, majority of open fractures require immediate debridement and adequate soft tissue coverage, especially Gustilo-Anderson Type III fractures which involve extensive soft tissue damage. Vascular repair should not be delayed in Type IIIC fractures. 68–70
Maxillofacial trauma
Facial lacerations or other minor injuries should be repaired in the Emergency Room under local anesthesia. Most facial fractures do not require urgent treatment and definitive reconstruction could be postponed. Operative repair of orbital floor fractures can be delayed if there is no sign of orbital apex/fissure syndrome and no entrapment of extraocular muscles that can lead to necrosis.71 Similarly, nasal, mid-face, and zygomaticomaxillary complex fractures can be treated conservatively if there is no significant functional impairment.71 Plan for same day discharge should be made for all such cases unless airway compromise is a significant risk.
Patients with complex maxillofacial trauma (i.e panfacial fractures, significant soft tissue injury, those with airway obstruction or vision changes) may require urgent surgical management and admission. While the management plan should be at the discretion of the surgeon as to whether open reduction and internal fixation (ORIF) is warranted, less invasive procedures such as maxillomandibular fixation using hybrid arch bars should be considered.
Hand Surgery
American Academy of Orthopaedic Surgeons recommends that every locality should be making their own decisions based on the prevalance of COVID-19 and the availability of resources and personnel.68 Semi-urgent cases such as lacerations with tendon or nerve involvement, acute fractures of the hand and wrists, comminuted fractures of the joints should still be performed considering the poor functional outcome if not treated or with a delay in treatment.72,73 If possible, these procedures should be done in the outpatient setting to minimize utilization of resources. As the virus becomes more prevalent and resources become of more paramount importance, the option for surgery becomes much more limited. Under these conditions, injuries in which immediate surgical intervention would prevent significant impairment of function should be considered, including compartment syndromes, open fracture and irreducible joint dislocations, septic joints, abscesses and amputation/subamputation with devascularization of upper extremity segments. Among replantations, thumb amputation, multiple amputated fingers, pediatric amputations and proximal amputations of the dominant/non-dominant hand should still be considered absolute indications.74 Replantation of individual digits distal to the insertion of the flexor digitorum superficialis and ring avulsion injuries are relative indications and pros and cons of surgery should be discussed with the patient.
Patients for whom surgery is deemed “non-essential” are those with chronic problems whose surgery can certainly be delayed without significant harm to the patient or eventual outcome. Although an argument can be made for the need for surgery in some individuals due to pain or functional impairment, the determining principle is that delaying treatment will not significantly alter the eventual outcome. Such conditions are: tendonitis of the hand, wrist, elbow, trigger finger, De Quervain’s tendonitis, medial and lateral elbow epicondylitis, nerve compression syndromes and degenerative joint disease. All these patients can be assessed and followed-up with virtual visits and prescribed NSAIDS or oral steroid and placed in splints. Injections of steroid into the tendon sheaths and joints in the hand and wrist can be considered for patients who failed the first line of treatment.69
CONCLUSION
Plastic surgery practice during the pandemic is curtailed to urgent and emergent care, in an effort to reduce risk of disease transmission and to prevent shortage of valuable resources. As the outbreak gradually resolves, the scope of practice will broaden accordingly. The recommendations that are summarized in this article are a snapshot of current practices which are subject to change, however they also provide a valuable resource on how to practice under unusual circumstances that we may encounter in the future. Finally, all suggestions should be taken in the context of each institute’s resources and prevalance of disease in the region.
Footnotes
Conflicts of interest and sources of funding: none declared.
REFERENCES
- 1.World Health Organization Coronavirus disease 2019 (COVID-2019) Situation Report-51. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10. Accessed April 24, 2020.
- 2.World Health Organization Coronavirus disease 2019 (COVID-19) Situation Report – 95. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200424-sitrep-95-covid-19.pdf?sfvrsn=e8065831_4. Accessed April 24, 2020.
- 3.Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020. doi: 10.1056/NEJMc2001737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan W, Ni Z, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020. doi: 10.1056/nejmoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bai Y, Yao L, Wei T, et al. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA - J Am Med Assoc. 2020. doi: 10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.02.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020. doi: 10.1016/S2468-1253(20)30048-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang W, Du RH, Li B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020. doi: 10.1080/22221751.2020.1729071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) from a Symptomatic Patient. JAMA - J Am Med Assoc. 2020. doi: 10.1001/jama.2020.3227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020. doi: 10.1056/nejmc2004973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020. doi: 10.1038/s41586-020-2196-x [DOI] [PubMed] [Google Scholar]
- 12.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020. doi: 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic Features and Clinical Course of Patients Infected with SARS-CoV-2 in Singapore. JAMA - J Am Med Assoc. 2020. doi: 10.1001/jama.2020.3204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth. 2020. doi: 10.1007/s12630-020-01591-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pasteur S, Cadila Z, Vector V, Vector V, Vector V, Bio V. Draft landscape of COVID19 candidate vaccines- 13 March 2020. 2020;(February).
- 16.Wu J, Li W, Shi X, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med. 2020:0-2. doi: 10.1111/joim.13063 [DOI] [PubMed] [Google Scholar]
- 17.Shen C, Wang Z, Zhao F, et al. Treatment of 5 Critically Ill Patients With COVID-19 With Convalescent Plasma. Jama. 2020;(29):1–8. doi: 10.1001/jama.2020.4783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shanmugaraj B, Siriwattananon K, Wangkanont K, Phoolcharoen W. Perspectives on monoclonal antibody therapy as potential therapeutic intervention for Coronavirus disease-19 (COVID-19). Asian Pacific J allergy Immunol. 2020. doi: 10.12932/AP-200220-0773 [DOI] [PubMed] [Google Scholar]
- 19.Fauci AS, Lane HC, Redfield RR. Covid-19 - Navigating the Uncharted. N Engl J Med. 2020. doi: 10.1056/NEJMe2002387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gautret P, Lagier J-C, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020. doi: 10.1016/j.ijantimicag.2020.105949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang W, Zhao Y, Zhang F, et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The experience of clinical immunologists from China. Clin Immunol. 2020. 10.1016/j.clim.2020.108393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China. JAMA. 2020. doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 23.International Council of Nurses High proportion of healthcare workers with COVID-19 in Italy is a stark warning to the world: protecting nurses and their colleagues must be the number one priority. https://www.icn.ch/sites/default/files/inline-files/PR_09_COVID-19-Italy.pdf. Accessed April 24, 2020.
- 24.American Society of Plastic Surgeons ASPS Guidance Regarding Elective and Non-Essential Patient Care. http://email.plasticsurgery.org/q/12EC50dbrptNnCCaBimf8m0W/wv. Accessed April 24, 2020.
- 25.American College of Surgeons COVID-19: Elective Case Triage Guidelines for Surgical Care. https://www.facs.org/covid-19/clinical-guidance/elective-case. Accessed April 24, 2020.
- 26.Centers for Medicare & Medicaid Services Non-Emergent, Elective Medical Services, and Treatment Recommendations. https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf. Accessed April 24, 2020.
- 27.American Medical Association AMA praises government on elective surgery guidelines during pandemic. https://www.ama-assn.org/press-center/ama-statements/ama-praises-government-elective-surgery-guidelines-during-pandemic. Accessed April 24, 2020.
- 28.Centers for Medicare & Medicaid Services Medicare Telemedicine Health Care Provider Fact Sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed April 24, 2020.
- 29.Givi B, Schiff BA, Chinn SB, et al. Safety Recommendations for Evaluation and Surgery of the Head and Neck during the COVID-19 Pandemic. JAMA Otolaryngol - Head Neck Surg. 2020. doi: 10.1001/jamaoto.2020.0780 [DOI] [PubMed] [Google Scholar]
- 30.Vascular Access Society of the Americas Maintaining lifelines for ESKD patients - ASDIN and VASA joint statement. http://www.vasamd.org/_resources/documents/Maintaining_lifelines_VASA_ASDIN.pdf. Accessed April 24, 2020.
- 31.New York’s Division of Military and Naval Affairs Office-Based Surgery Guidance. http://dmna.ny.gov/covid19/docs/all/DOH_COVID19_OfficeBasedSurgeryGuidance_040420.pdf. Accessed April 24, 2020.
- 32.Society of American Gastrointestinal and Endoscopic Surgeons SAGES and EAES Recommendations Regarding Surgical Response to COVID-19 Crisis. https://www.sages.org/recommendations-surgical-response-covid-19/. Accessed April 24, 2020.
- 33.Vashist SK. In Vitro Diagnostic Assays for COVID-19: Recent Advances and Emerging Trends. Diagnostics (Basel, Switzerland). 2020;10(4). doi: 10.3390/diagnostics10040202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lu R, Wang J, Li M, Wang Y, Dong J, Cai W. SARS-CoV-2 detection using digital PCR for COVID-19 diagnosis, treatment monitoring and criteria for discharge. medRxiv. 2020. doi: 10.1101/2020.03.24.20042689 [DOI] [Google Scholar]
- 35.Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020. doi: 10.1148/radiol.2020200642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ioannis D, Selby K, Bernard P, Genton B, Cornuz J. Performance du frottis nasopharyngé-PCR pour le diagnostic du Covid-19 Recommandations pratiques sur la base des premières. 2020:699–701. [PubMed]
- 37.Tien HC, Chughtai T, Jogeklar A, Cooper AB, Brenneman F. Elective and emergency surgery in patients with severe acute respiratory syndrome (SARS). Can J Surg. 2005. [PMC free article] [PubMed] [Google Scholar]
- 38.Dexter F, Parra MC, Brown JR, Loftus RW. Perioperative COVID-19 Defense: An Evidence-Based Approach for Optimization of Infection Control and Operating Room Management. Anesth Analg. 2020. doi: 10.1213/ANE.0000000000004829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.US Centers for Disease Control and Prevention Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Finfection-control%2Fcontrol-recommendations.html. Accessed April 24, 2020.
- 40.Moore G, Ali S, Cloutman-Green EA, et al. Use of UV-C radiation to disinfect non-critical patient care items: A laboratory assessment of the Nanoclave Cabinet. BMC Infect Dis. 2012. doi: 10.1186/1471-2334-12-174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Loftus RW, Koff MD, Burchman CC, et al. Transmission of pathogenic bacterial organisms in the anesthesia work area. Anesthesiology. 2008. doi: 10.1097/ALN.0b013e318182c855 [DOI] [PubMed] [Google Scholar]
- 42.Loftus RW, Brown JR, Koff MD, et al. Multiple reservoirs contribute to intraoperative bacterial transmission. Anesth Analg. 2012. doi: 10.1213/ANE.0b013e31824970a2 [DOI] [PubMed] [Google Scholar]
- 43.Brindle M, Gawande A. Managing COVID-19 in Surgical Systems. Ann Surg. 2020. doi: 10.1097/sla.0000000000003923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng MH, Boni L, Fingerhut A. Minimally Invasive Surgery and the Novel Coronavirus Outbreak: Lessons Learned in China and Italy. Ann Surg. 2020. doi: 10.1097/SLA.0000000000003924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kohn WG, Harte JA, Malvitz DM, Collins AS, Cleveland JL, Eklund KJ. Guidelines for infection control in dental health care settings - 2003. J Am Dent Assoc. 2004. doi: 10.14219/jada.archive.2004.0019 [DOI] [PubMed] [Google Scholar]
- 46.O’Neil CA, Li J, Leavey A, et al. Characterization of aerosols generated during patient care activities. Clin Infect Dis. 2017. doi: 10.1093/cid/cix535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wenner L, Pauli U, Summermatter K, Gantenbein H, Vidondo B, Posthaus H. Aerosol Generation During Bone-Sawing Procedures in Veterinary Autopsies. Vet Pathol. 2017. doi: 10.1177/0300985816688744 [DOI] [PubMed] [Google Scholar]
- 48.World Health Organization Health workers exposure risk assessment and management in the context of COVID-19 virus. https://apps.who.int/iris/bitstream/handle/10665/331340/WHO-2019-nCov-HCW_risk_assessment-2020.1-eng.pdf. Accessed April 24, 2020.
- 49.US Centers for Disease Control and Prevention Guidance for the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings. https://www.cdc.gov/HAI/pdfs/ppe/PPEslides6-29-04.pdf. Accessed April 24, 2020.
- 50.World Health Organization Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19). https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf. Accessed April 24, 2020.
- 51.Ueda M, Martins R, Hendrie PC, et al. Managing Cancer Care During the COVID-19 Pandemic: Agility and Collaboration Toward a Common Goal. J Natl Compr Canc Netw. 2020;18(4):1–4. doi: 10.6004/jnccn.2020.7560 [DOI] [PubMed] [Google Scholar]
- 52.Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 Transmission in Patients With Cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol. 2020. doi: 10.1001/jamaoncol.2020.0980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.American College of Surgeons COVID-19 Guidelines for Triage of Breast Cancer Patients. https://www.facs.org/covid-19/clinical-guidance/elective-case/breast-cancer. Accessed April 24, 2020.
- 55.American Society of Plastic Surgeons ASPS Statement on Breast Reconstruction in the face of COVID-19 Pandemic. https://www.plasticsurgery.org/documents/medical-professionals/COVID19-Breast-Reconstruction-Statement.pdf. Accessed April 24, 2020.
- 56.The American Society of Breast Surgeons Recommendations for Prioritization, Treatment and Triage of Breast Cancer Patients During the COVID-19 Pandemic: Executive Summary. https://www.breastsurgeons.org/docs/news/The_COVID-19_Pandemic_Breast_Cancer_Consortium_Recommendations_EXECUTIVE_SUMMARY.pdf?01. Accessed April 24, 2020.
- 57.Clayman GL, Lee JJ, Holsinger FC, et al. Mortality risk from squamous cell skin cancer. J Clin Oncol. 2005. doi: 10.1200/JCO.2005.02.155 [DOI] [PubMed] [Google Scholar]
- 58.Day AT, Sher DJ, Lee RC, et al. Head and neck oncology during the COVID-19 pandemic: Reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol. 2020:104684. doi: 10.1016/j.oraloncology.2020.104684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Migden MR, Rischin D, Schmults CD, et al. PD-1 blockade with cemiplimab in advanced cutaneous squamous-cell carcinoma. N Engl J Med. 2018. doi: 10.1056/NEJMoa1805131 [DOI] [PubMed] [Google Scholar]
- 60.H F., H L., B M., et al. Follow-up of patients with complete remission of locally advanced basal cell carcinoma treated with vismodegib after treatment discontinuation: A retrospective multicentric French study. J Clin Oncol. 2017. [Google Scholar]
- 61.Soon SL, Ibrahim SF, Arron ST. A randomized phase II study evaluating vismodegib as neoadjuvant treatment of basal cell carcinoma preceding Mohs micrographic surgery: results and lessons learned. Br J Dermatol. 2019. doi: 10.1111/bjd.17623 [DOI] [PubMed] [Google Scholar]
- 62.National Comprehensive Cancer Network Advisory Statement for Non-Melanoma Skin Cancer Care During the COVID-19 Pandemic. https://www.nccn.org/covid-19/pdf/NCCN-NMSC.pdf. Accessed April 24, 2020.
- 63.National Comprehensive Cancer Network Short-Term Recommendations for Cutaneous Melanoma Management During COVID-19 Pandemic. https://www.nccn.org/covid-19/pdf/Melanoma.pdf. Accessed April 24, 2020.
- 64.Ellis MA, Graboyes EM, Wahlquist AE, et al. Primary Surgery vs Radiotherapy for Early Stage Oral Cavity Cancer. Otolaryngol - Head Neck Surg (United States). 2018. doi:10.1177/0194599817746909 [DOI] [PubMed] [Google Scholar]
- 65.Wendt CD, Peters LJ, Delclos L, et al. Primary radiotherapy in the treatment of stage I and II oral tongue cancers: Importance of the proportion of therapy delivered with interstitial therapy. Int J Radiat Oncol Biol Phys. 1990. doi: 10.1016/0360-3016(90)90299-Y [DOI] [PubMed] [Google Scholar]
- 66.Sher DJ, Thotakura V, Balboni TA, et al. Treatment of oral cavity squamous cell carcinoma with adjuvant or definitive intensity-modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2011. doi: 10.1016/j.ijrobp.2011.02.023 [DOI] [PubMed] [Google Scholar]
- 67.American College of Surgeons COVID-19 Guidelines for Triage of Emergency General Surgery Patients. https://www.facs.org/covid-19/clinical-guidance/elective-case/emergency-surgery. Accessed April 24, 2020.
- 68.American Academy of Orthopaedic Surgeons AAOS Guidelines for Elective Surgery During the COVID-19 Pandemic. https://www.aaos.org/about/covid-19-information-for-our-members/aaos-guidelines-for-elective-surgery/. Accessed April 24, 2020.
- 69.American College of Surgeons COVID-19 Guidelines for Triage of Orthopaedic Patients. https://www.facs.org/covid-19/clinical-guidance/elective-case/orthopaedics. Accessed April 24, 2020.
- 70.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (Severe) open fractures: A new classification of type III open fractures. J Trauma - Inj Infect Crit Care. 1984. doi: 10.1097/00005373-198408000-00009 [DOI] [PubMed] [Google Scholar]
- 71.Edwards SP, Kasten S, Nelson C, Elner V, McKean E. Maxillofacial Trauma Management During COVID-19: Multidisciplinary Recommendations. Facial Plast Surg aesthetic Med. 2020;22(3):10–12. doi: 10.1089/fpsam.2020.0158 [DOI] [PubMed] [Google Scholar]
- 72.Rigo IZ, Røkkum M. Predictors of outcome after primary flexor tendon repair in zone 1, 2 and 3. J Hand Surg Eur Vol. 2016. doi: 10.1177/1753193416657758 [DOI] [PubMed] [Google Scholar]
- 73.Shimizu T, Omokawa S, Akahane M, Horiuchi T, Nakano K, Tanaka Y. Predictors of the Postoperative Range of Finger Motion for Comminuted Hand and Finger Fractures Treated with a Titanium Plate. J Hand Surg Am. 2011. doi: 10.1016/s0363-5023(11)60047-6 [DOI] [PubMed] [Google Scholar]
- 74.Higgins James P. Replantation. In: Wolfe Scott, Pederson William, Kozin MC Scott H., ed. Green’s Operative Hand Surgery : 7th Edition Elsevier; 2016:1476–1485. [Google Scholar]


