Abstract
In this study, We report on the use of fluorine 18-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) scan examinations for the diagnosis of COVID-19 respiratory syndrome in asymptomatic left ventricular assist device (LVAD) recipients. Thus, extreme caution and thoughtful approaches should be taken for a timely detection in delicate LVAD populations, especially if patients are living in a high-density COVID-19-infected area, and the potential intention for LVAD treatment is bridge to transplantation.
Keywords: heart failure, pandemic, left ventricular assist device
A novel enveloped RNA betacoronavirus, which is phylogenetically similar to SARS-CoV (thus renamed as SARS-CoV-2) and causes a severe acute respiratory syndrome (SARS) (hence designated as COVID-19), emerged in the planet Earth, causing a cluster of pneumonia cases in Wuhan, China, in December 2019.1–7 The virus, initially named “novel Coronavirus” (2019-nCoV), has been designated as a pandemic by the World Health Organization (WHO), on March 11, 2020.1 As of March 20, 2020, COVID-19 outbreak has been confirmed in 188 countries and territories, with 319,145 cases globally and 13,688 deaths.1–3 Currently, the majority of infections are reported in China followed by Italy, Spain, and Iran. Italy has gone into official lockdown on March 9, 2020, followed by other countries or focal biocontainment territories.1–3
Its rate of transmission is high: an infected individual may spread the disease to one to three others.2,3 According to the initial reports from Wuhan, China, the most common symptoms related to COVID-19 are fever (99%), fatigue (70%), and dry cough (59%), with dyspnea noted in one third of the total cases.2,3,6 As mentioned in the larger reports from China, fever cases were seen among 44% at presentation, but 89% during hospitalization (cough 68%, one third of the cases with productive cough, fatigue 38%, dyspnea 19%).2–7
Comorbidities account for 23%–46%.1–3,6 Incubation results to be 4–5 days (up to 14–27 days). The majority of COVID-19 cases (87%) belonged to those aged between 30 and 79 years and most of such cases (81%) are mild. The remaining 14% were present with severe symptoms, while 5% required care in an intensive care unit (ICU).5 The case-fatality rate has been touted to be 2.3% overall (mostly people were aged >75 years).1–3,6 Those with cancer and patients with multiple comorbidities are at a higher risk for severe illness.1,6 Presentation and prognosis of COVID-19 in solid organ transplantation or left ventricular assist device (LVAD) systems has not been adequately reported.1–3,6
Significant environmental contamination (including washbasin, toilet bowl, and surfaces of the air outlet fan) has been noted in hospitalized patients.1–3 Thus, it is prudent to advise transplant and LVAD recipients to ardently practice mitigation strategies such as social distancing, sanitization, hand hygiene, and avoidance of areas known to harbor potentially infected individuals. These recommendations extend to their care providers as well.
Report
A 55 year old male patient suffering from refractory end-stage heart failure due to an idiopathic dilative cardiomyopathy underwent a less invasive HeartWare HVAD implantation (HeartWare Inc., Miami, FLA; Medtronic Inc., Minneapolis, MN) at our institution. Surgery was performed on November 2016 and accomplished, less invasively, through an upper “J” mini-sternotomy and left lateral minithoracotomy, on beating heart and femoro-femoral cardiopulmonary bypass establishment. LVAD system has been running uneventfully for 1,170 postoperative days, and the patient has joined a routine monthly ambulatory visit at our transplant outpatient care unit. Laboratory, echo, chest x-ray, angio-computed tomography (CT) scan evaluations have been historically acceptable and never of notice. The patient has returned to a quite normal daily life, thus rejoining his own family and friends, driving and travelling as being always asymptomatic and feeling personally confident with a strict self-management of LVAD peripherals, tools, and wound site medications and dressing, as well.
After 1,155 days of LVAD support, the patient has recently asked a check of the driveline wound site. At our institution, we noticed no local signs of percutaneous site infection, but rubor and tumor associated with a pain on the left upper abdominal quadrant (mid-tract of abdominal LVAD lead tunneling) were evident in the patient. Thus, a fluorine 18-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) scan has been planned and performed, urgently, to check both superficial and deep lead tract.8 Laboratory and inflammatory parameters were regular. He had no fever. Blood cultures and wound site swabs resulted to be negative.
A PET scan examination revealed pathologic 18F-FDG accumulation at the second and third level (superficial tract) of driveline tunneling (standardized uptake value [SUV] max = 15.3), thus showing an inflammatory pattern with local active infection and potential evolution into a subcutaneous abdominal fistula (Figure 1). Moreover, multilobular and subpleural ground-glass opacities and consolidation were casually evident, focusing especially on both the left inferior and right inferior lobes (SUV max = 10.3 and 10.6, respectively), thus showing a pattern of an active infective interstitial lung disease that seemed to be typical of the current COVID-19 disease (Figure 2), as suggested by our nuclear medicine and infectology consultants.4–7
Figure 1.
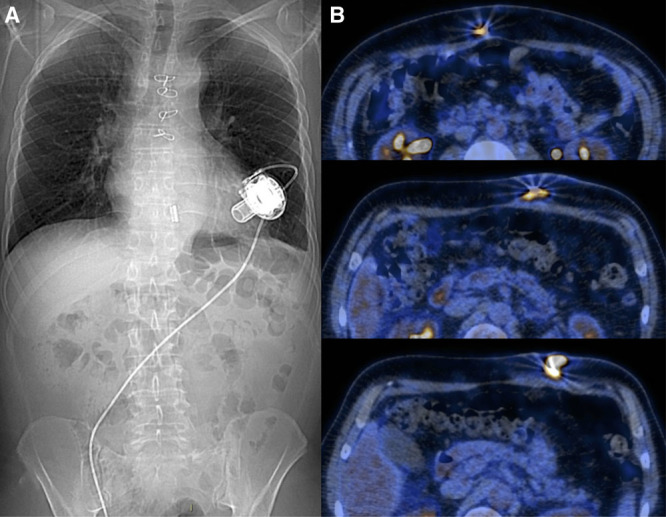
A: Chest x-ray view; left ventricular assist device system placement and driveline tunneling line. B: Positron emission tomography scan lead view; pathologic fluorine 18-fluorodeoxyglucose accumulation located at the second and third (superficial) driveline tunneling tract.
Figure 2.
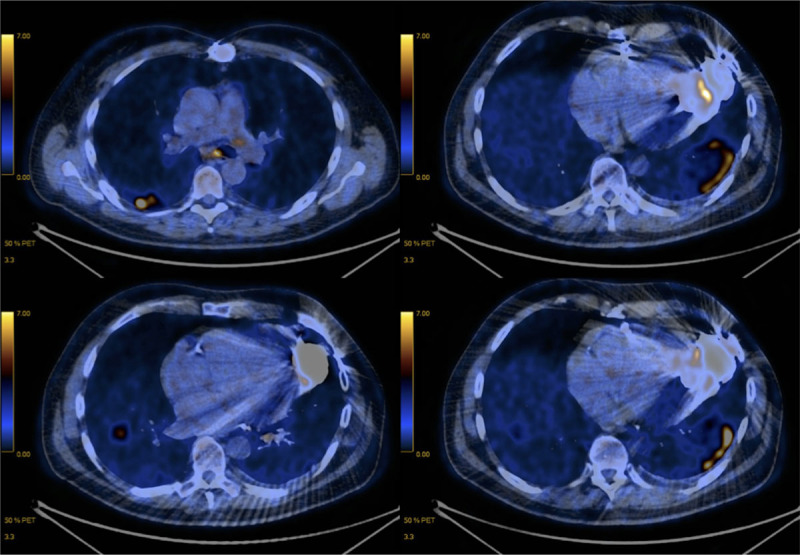
Positron emission tomography scan chest view. Pathologic fluorine 18-fluorodeoxyglucose accumulation located at the left inferior and right inferior pulmonary lobes (multilobular and subpleural ground-glass opacities and consolidation).
Our LVAD recipient lives in Piacenza, a city in the north of Italy with a high density of COVID-19 infection.1 He has been informed and returned home getting an official isolation (self and societal quarantining with the use of mask and gloves,1–3 for three weeks) after acknowledgement of local caregivers and our institutional heart failure physicians. Rapid test-polymerase chain reaction (RT-PCR) of 2019-nCoV (throat swab) has been performed, locally in Piacenza, which resulted to be negative, at the first examination, but became positive 8 days later, in the second test.2,3,6 Although the patient had been asymptomatic so far, he had a weak dry cough only recently.
Driveline percutaneous site medication and dressing are currently performed, two times a week, by the LVAD patient himself. We recommended vigilance for eventual visual score lead site negative evolution and development of symptoms, typically for COVID-19 severe illness, by using telehealth options and self-monitoring at home (such as daily temperature checks and symptoms diary), as well.
Italy accounts for 53,578 infected cases (positive tests), with the majority reported in Lombardia (25,515 cases) and Emilia-Romagna (6,705 cases), both being regions in the north of the country.1 So far, overall deaths in Italy totaled 4,825 cases (and serious critical 2,857). Our LVAD patient, unfortunately, belongs to the most COVID-19-infected and first red-line area in Italy: Piacenza, a city of the Emilia-Romagna region.1
PET/CT examinations in asymptomatic patients may not be surprising, but this is the first report, to our knowledge, on COVID-19 infection in a LVAD recipient with such kind of a clinical scenario and nuclear medicine imaging casual pattern that has been suggestive of COVID-19 disease.4–7
The majority of patients with coronavirus will recover spontaneously, without requiring any medical attention. Patients with mild symptoms can generally be discharged home, with instructions to isolate themselves.1–3,6 These decisions should be made in coordination with local health departments, who can assist in follow-up.1–3,6
Shi et al.4 performed CT scanning in a group of healthcare workers who were exposed to COVID-19 before they became symptomatic. Ground-glass opacification on CT scan was seen in the vast majority of patients.3–7 This confirms the emergence of CT abnormality before symptoms could be consistent with the existence of an asymptomatic carrier state.6 Sensitivity of chest x-ray is lower than CT scan for subtle opacities.3–7 Guan et al.3 showed a chest x-ray sensitivity of 59%, compared with 86% for CT scan. Sensitivity among patients with positive RT-PCR is high.3–7 The exact numbers vary, likely reflecting variability in how scans are interpreted. There currently does not seem to be any precise definition of what constitutes a “positive” CT scan.3–7 Ai et al.5 reported on a CT scan sensitivity of 97%. However, among patients with only constitutional symptoms (but not respiratory symptoms), CT scan may be less sensitive (<50%).3–7
Additionally, in COVID-19 syndrome, at laboratory, white blood cell (WBC) count tends to be normal.3,6 Lymphocytopenia is common (seen in about 80% of patients) due to the damages of cytoplasmic component by SARS-CoV viral particles.3,6 Mild thrombocytopenia is common, but platelet (PLT) counts are rarely <100 × 109/L.3,6 Lower PLT count is a poor prognostic sign. However, in our LVAD patient, WBCs’ count was 6.5 × 109/L, while PLTs’ was 185.
First RT-PCR may be negative in the window period and the asymptomatic stage.2,3,6 Immunoglobulin (Ig) M becomes detectable at the onset of symptoms, mostly on postinfection day (PID) 7–14, as in our LVAD patient, and disappears on PID 18–21 (decline). IgG becomes detectable on PID 14–25 (convalescence) and disappears on PID 30–38. This is why a new RT-PCR needs to be eventually performed in our patient, within 30–40 days since the first positive test.
Conclusions
In summary, PET and CT scan examinations remain sensitive and indicative of COVID-19 respiratory disease even in case of clinically asymptomatic or less symptomatic patients.4–7 Thus, extreme caution and thoughtful approaches for timely detection should be taken for our delicate LVAD recipient population during routine ambulatory outpatient visits, especially if patients are living in a high-density COVID-19-infected area and the potential intention for LVAD treatment is bridge to transplantation.1–3,6
So far, no evidence has been published to suggest that cardiothoracic transplant recipients are at a greater risk of developing severe illness.2–7 Evolution into symptomatic COVID-19 disease may be life threatening; thus, early detection (via any instrument), timing, and radical intensive anti-inflammatory/respiratory treatment are currently the keys to preserve life.2–7
Additionally, this experience highlights and confirms the diagnostic value of 18F-FDG PET scan in detecting the localization and extension of infection to internal LVAD components.8 After PET evaluation, we are going to consider surgery, negative pressure wound therapy (NPWT), and antibiotic therapy adoption to treat the potential lead tunneling fistula evolution in our reported patient, soon.
Footnotes
Disclosure: The authors have no conflicts of interest to report.
References
- 1.WHO: Rolling Updates on Coronavirus Disease (COVID-19). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed March 20, 2020.
- 2.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med 202026: 382, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. doi: 10.1056/NEJMoa2002032. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect Dis 2020; 20:425–434.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology 2020. 200642, doi: 10.1148/radiol.2020200642. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang W, Cao Q, Qin L, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): A multi-center study in Wenzhou city, Zhejiang, China. J Infect 202080: 388–393, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernheim A, Mei X, Huang M, et al. Chest CT findings in coronavirus disease-19 (COVID-19): Relationship to duration of infection. Radiology 2020. 200463, doi: 10.1148/radiol.2020200463. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dell’Aquila AM, Avramovic N, Mastrobuoni S, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography for improving diagnosis of infection in patients on CF-LVAD: Longing for more ‘insights’. Eur Heart J Cardiovasc Imaging 201819: 532–543, [DOI] [PubMed] [Google Scholar]


