Abstract
Introduction
The role of the accessory maxillary ostium, a common anatomical variant, in the development of chronic sinusitis remains unclear. This study aimed to examine the association between chronic sinusitis and presence of an accessory maxillary ostium using computed tomography (CT) of the paranasal sinuses.
Methods
We conducted a retrospective study of 1188 paranasal sinus CT scans performed in a major tertiary medical center between January 1, 2016 and December 31, 2016. Axial and coronal and views were reviewed to evaluate the presence of accessory maxillary ostia and maxillary and ethmoid sinusitis.
Results
Nine hundred twenty-eight patients were included for analysis. A 52.8% were male. Mean patient age was 33.8 years. A right accessory maxillary ostium was detected in 274 patients (29.5%), which was the same number of patients with a left accessory maxillary ostium. Bilateral accessory maxillary ostia were found in 172. The presence of right maxillary sinusitis was significantly associated with male gender and the presence of a right accessory maxillary ostium. Male gender was the only factor significantly associated with the presence of left sinusitis. Left or right ethmoidal sinusitis was significantly associated with male gender and the presence of left or right maxillary sinusitis, respectively.
Conclusion
The presence of an accessory maxillary ostium may contribute to the development of maxillary and ethmoidal sinusitis. Further studies are needed to elucidate this association and determine indications for incorporating the natural and accessory ostia when performing middle meatus antrostomy during endoscopic sinus surgery.
Keywords: CT scan, maxillary, sinusitis, paranasal sinus
Introduction
The accessory ostium of the maxillary air sinus is an anatomical variation that may play a role in the development of chronic sinusitis.1,2 Accessory maxillary ostia are most commonly located in the posterior nasal fontanelle of the middle meatus and may occur unilaterally or bilaterally.3,4 Accessory maxillary ostium is usually located on the lateral nasal wall, and should not be confused with the maxillary hiatus. Between the uncinate process and the inferior concha there is a membranous area on the lateral nasal wall, covered by mucoperiosteum. This area is the fontanelle, the fontanelle is separated into anterior and posterior fontanelle by the ethmoid process of the inferior concha.5
In most individuals, the maxillary sinus opens to the anterior part of the posterior fontanelle, on the inferior part of the ethmoid infundibulum. The active mucociliary transport in the maxillary sinus is directed toward the natural ostium only. Accessory maxillary ostium does not contribute to the physiological transport inside the maxillary sinus even if the natural ostium is blocked.5 Accordingly, it may have a role in the development of chronic sinusitis. Accessory maxillary ostium is reported to be present in 30% of the patients diagnosed with chronic maxillary sinusitis and in 10–20% of normal individuals.6,7 It is unclear whether chronic sinusitis leads to accessory ostium formation or the presence of an accessory ostium leads to chronic sinusitis by recirculation of mucus secretions.8–10 Only one previous study reported the significant association between the accessory maxillary ostium and chronic maxillary sinusitis by computed tomography (CT) in 377 individuals in Turkey.5
This study aimed to investigate the association between the presence of the accessory maxillary ostium and the occurrence of chronic maxillary and ethmoidal sinusitis using computed tomography (CT) examination of the paranasal sinuses. This study aimed to establish the association in a larger number of individuals from a new ethnicity.
Methods
We conducted a retrospective evaluation of paranasal sinus CT scans performed in 1188 patients between January 1, 2016 and December 31, 2016 at a major tertiary medical center. This study was conducted in accordance with the principles of the Declaration of Helsinki and institutional review board approval was obtained (number 464–2018). Patients aged <13 years and those with nasal polyps, previous sinus surgery, acute sinusitis, inverted papilloma, choanal atresia, and severe nasal septal deviation touching the lateral nasal wall were excluded (268 patients). Nine hundred twenty-eight patients were finally included for analysis. In every patient, we considered the maxillary and ethmoid sinuses and osteomeatal complex of each side as one unit (total 1856 units). The CT utilized is the Philips 128 Slice Ingenuity scanner and images were acquired in both axial and coronal planes. Patient position was supine. Slice thickness for axial and coronal planes was 1mm and inter-space was 1mm.
Axial and coronal views were reviewed to evaluate the presence of accessory maxillary ostia (Figures 1 and 2), obliteration of the osteomeatal complex, and the presence of maxillary and ethmoid sinusitis (Figures 3 and 4). Maxillary and ethmoid sinus opacification graded 1 and 2 using the Lund–Mackay scoring system were considered indicative of chronic sinusitis. The Lund–Mackay system works as follows: the right or left sinuses were, respectively, divided into six portions, including maxillary sinus, anterior ethmoid sinuses, posterior ethmoid sinuses, sphenoid sinus, frontal sinus, and osteomeatal complex. The severity of sinus mucosal inflammation or fluid accumulation was scored as 0 (complete lucency), 1 (partial lucency) or 2 (complete opacity).11 To quantify the volume of inflammatory opacification, the soft tissue density rate was assessed with a computer workstation. Radiological data was statistically analyzed using the chi-square test to compare percentages and binary logistic regression to determine the association between chronic sinusitis and presence of an accessory maxillary ostium after adjusting for age and gender. P < 0.05 was considered significant.
Figure 1.
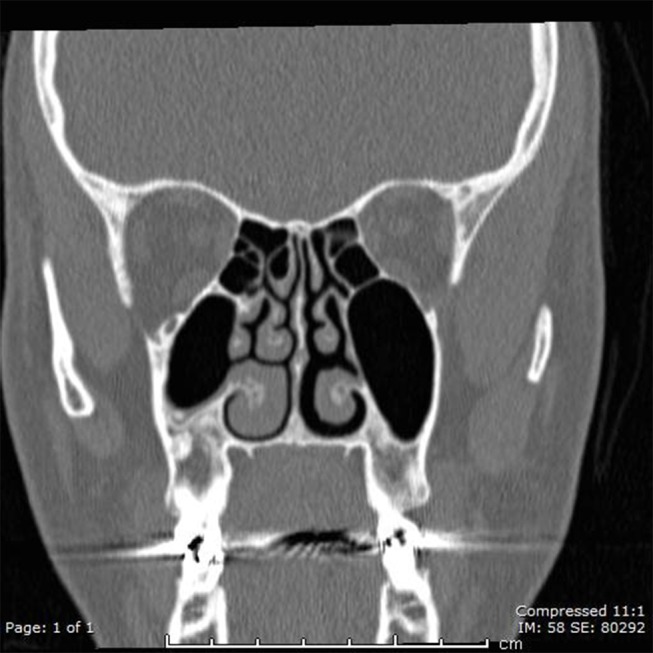
Paranasal CT scan showed the right accessory ostium.
Figure 2.
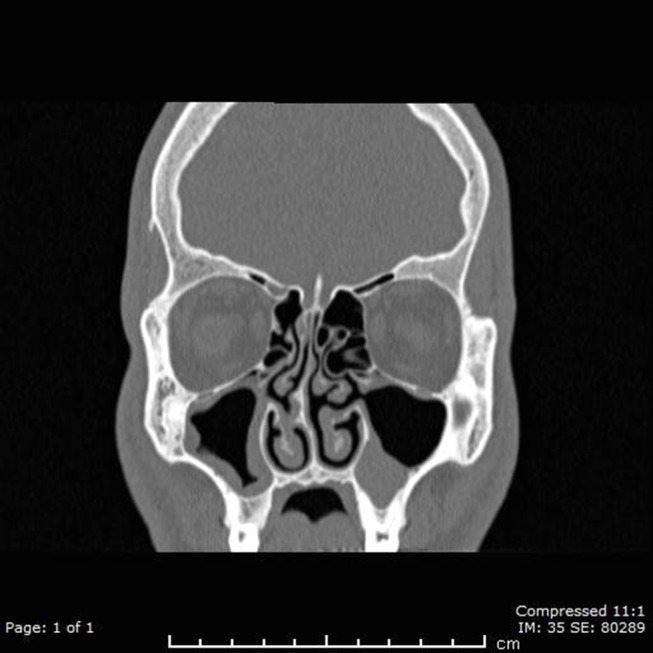
Paranasal CT scan demonstrated left accessory ostium with bilateral sinusitis.
Figure 3.
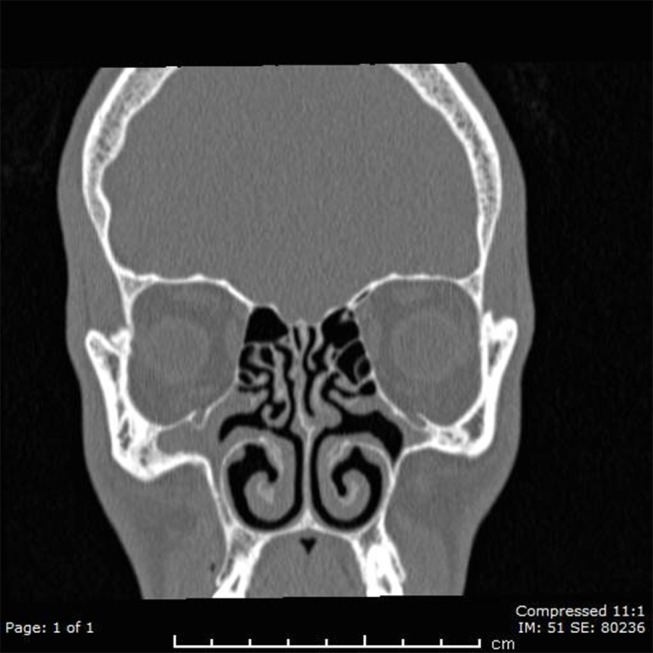
Paranasal CT scan indicated bilateral accessory ostia with sinusitis.
Figure 4.

Paranasal CT scan showed bilateral accessory ostia and bilateral maxillary and ethmoidal sinusitis.
Results
Among the 928 study patients, 47.2% were female and 52.8% male. Mean age was 33.8 years (range, 13–83 years). A right accessory maxillary ostium was detected in 274 patients (29.5%), which was equal to the number of patients with a left accessory maxillary ostium. Bilateral accessory maxillary ostia were detected in 172 patients (18.5%). Right maxillary, left maxillary, and bilateral maxillary sinusitis was present in 410, 403, and 326 patients, respectively. Right ethmoidal, left ethmoidal sinusitis, and bilateral ethmoidal sinusitis was present in 305, 292, and 238 patients, respectively. Patient characteristics are summarized in (Table 1).
Table 1.
Demographic Distribution and Clinical Characteristics
| Pre- and Post-Operative Variables | Number | Percent (%) |
|---|---|---|
| Mean ± SE | ||
| Sex | ||
| Male | 490 | 52.8 |
| Female | 438 | 47.2 |
| Age (y) | 33.8 ± 0.5 | |
| Right maxillary accessory ostium | 274 | 29.5 |
| Left maxillary accessory ostium | 274 | 29.5 |
| Bilateral maxillary accessory ostium | 172 | 18.5 |
| Right maxillary sinusitis | 410 | 44.2 |
| Left maxillary sinusitis | 403 | 43.4 |
| Bilateral maxillary sinusitis | 326 | 35.1 |
| Right ethmoidal sinusitis | 305 | 32.9 |
| Left ethmoidal sinusitis | 292 | 31.5 |
| Bilateral ethmoidal sinusitis | 238 | 25.6 |
Abbreviation: SE, standard error.
The prevalence of right maxillary sinusitis was significantly higher in males (P = 0.002). A right accessory ostium was present in a significantly greater proportion of patients with right sinusitis compared to those without right sinusitis (33.2% vs 26.6%, P = 0.018). There was no significant difference in the prevalence of right maxillary sinusitis according to patient age, presence of left accessory ostium, or presence of bilateral accessory ostia. Male gender was the only factor significantly associated with the presence of left maxillary sinusitis (P = 0.004, Table 2). Prevalence of left or right ethmoidal sinusitis was significantly associated with male gender and the presence of either right or left maxillary sinusitis, respectively. Neither gender nor age were associated with the presence of a right or left accessory ostium (Table 3).
Table 2.
Analysis of Factors Associated with Right and Left Maxillary Sinusitis
| Variables | Right Maxillary Sinusitis | Left Maxillary Sinusitis | ||||
|---|---|---|---|---|---|---|
| Presence N (% from Presence) |
Absence N (% from Absence) |
P-value | Presence N (% from Presence) |
Absence N (% from Absence) |
P-value | |
| Sex | 0.002 | 0.004 | ||||
| Male | 239 (58.3) | 251 (48.5) | 233 (57.8) | 257 (49.0) | ||
| Female | 171 (41.7) | 267 (51.5) | 170 (42.2) | 268 (51.0) | ||
| Age (y) | 34.3 ± 0.7 | 33.4 ± 0.6 | NS | 34.4 ± 0.7 | 33.3 ± 0.6 | NS |
| Right maxillary accessory ostium | 136 (33.2) | 138 (26.6) | 0.018 | 119 (29.5) | 155 (29.5) | NS |
| Left maxillary accessory ostium | 116 (28.3) | 158 (30.5) | NS | 123 (30.5) | 151 (28.8) | NS |
| Bilateral maxillary accessory ostium | 77 (18.8) | 95 (18.3) | NS | 74 (18.4) | 98 (18.7) | NS |
Abbreviations: N, number; NS, not significant.
Table 3.
Analysis of Factors Associated with Right and Left Ethmoidal Sinusitis
| Variables | Right Ethmoidal Sinusitis | Left Ethmoidal Sinusitis | ||||
|---|---|---|---|---|---|---|
| Presence N (% from Presence) |
Absence N (% from Absence) |
P-value | Presence N (% from Presence) |
Absence N (% from Absence) |
P-value | |
| Sex | 0.000 | 0.000 | ||||
| Male | 206 (67.5) | 284 (45.6) | 190 (65.1) | 300 (47.2) | ||
| Female | 99 (32.5) | 339 (54.4) | 102 (34.9) | 336 (52.8) | ||
| Age (y) | 33.6 ± 0.8 | 33.9 ± 0.6 | NS | 33.0 ± 0.8 | 34.2 ± 0.6 | NS |
| Right maxillary accessory ostium | 83 (27.2) | 191 (30.7) | NS | 78 (26.7) | 196 (30.8) | NS |
| Left maxillary accessory ostium | 90 (29.5) | 184 (29.5) | NS | 80 (27.4) | 194 (30.5) | NS |
| Bilateral maxillary accessory ostium | 51 (16.7) | 121 (19.4) | NS | 41 (14.0) | 131 (20.6) | 0.02 |
| Right maxillary sinusitis | 238 (78.0) | 172 (27.6) | 0.000 | 216 (74.0) | 194 (30.5) | 0.000 |
| Left maxillary sinusitis | 234 (76.7) | 169 (27.1) | 0.000 | 234 (80.1) | 169 (26.6) | 0.000 |
Abbreviations: N, number; NS, not significant.
Male gender and presence of a right accessory ostium were significant independent factors associated with the presence of right maxillary sinusitis. Male gender was the only significant independent factor associated with the presence of left maxillary sinusitis. Significant independent factors associated with presence of right ethmoidal sinusitis were male gender, right and left maxillary sinusitis, and right accessory ostium. Only gender and presence of maxillary sinusitis (right and left) were significant independent factors associated with left ethmoidal sinusitis.
Discussion
This study investigated the prevalence and association of a paranasal sinus anatomical variant on the presence of maxillary and ethmoidal sinusitis using CT in a relatively large patient sample. Accessory maxillary ostia were detected in 40.5% (376) of patients without any gender differences. Male gender was significantly associated with the presence of both maxillary and ethmoidal sinusitis. In addition to male gender, the presence of a right maxillary accessory ostium was associated with the presence of both right maxillary and ethmoidal sinusitis; a significant coexistence of maxillary and ethmoidal sinusitis was clear. The relationship between the accessory maxillary ostium and acute sinusitis has been shown in a previous animal study.12 Clinical studies have also found this relationship. The presence of an accessory maxillary ostium is reportedly more frequent in patients with chronic sinusitis.1 Another study also showed this association and recommended including the posterior or anterior fontanelle when performing middle meatal antrostomy to reduce mucus recirculation.2 In addition, Capelli et al found that maxillary mucosa thickness ≥2 mm and closure of the natural maxillary ostium were significantly associated with chronic rhinosinusitis; common anatomical variants, including concha bullosa, Haller cells, and accessory maxillary ostia, were not.13 Yenigun et al reported that the presence of accessory maxillary ostium was associated with an approximately threefold increase in the incidence of mucus retention cysts and a two-fold increase in the incidence of mucosal thickening and maxillary sinusitis.5
A previous study reported the development of accessory maxillary ostia after induction of sinusitis in rabbits.12 The greater frequency of accessory maxillary ostia in patients with a previous history of multiple episodes of maxillary sinusitis suggests that accessory ostia may occur as a consequence of pathology. Guerra-Pereira et al stated that radiological imaging is an important tool in maxillary sinus pathology diagnosis and CT can complement the diagnosis of odontogenic sinusitis.14 Using a fiberoptic endoscope to investigate accessory ostia in patients with chronic rhinosinusitis, Mladina et al reported a 19.3% prevalence of accessory maxillary ostia; 68% of them were bilateral.10 CT scan is currently the modality of choice in the evaluation of paranasal sinuses.15
A possible mechanism for the development of accessory ostia is impediment of the main ostium by mucosal edema due to chronic sinusitis or other anatomical or pathological factors in the middle meatus that leads to rupture of membranous part of the lateral nasal wall. Fontanelle defects and formation of accessory ostia could serve to maintain chronic inflammation of the maxillary sinus by permitting mucus recirculation between adjacent openings.16,17
Reports regarding gender distribution of chronic rhinosinusitis are variable; some mention that females have almost double the rate of males,18,19 while others have found no difference.20,21 Lal et al reported that women who elected endoscopic sinus surgery had a lower Lund–Mackay CT score but higher total Sino-nasal Outcome Test–22 score. In our study, males had a higher prevalence of maxillary and ethmoidal sinusitis.22
This study is limited by its retrospective nature and use of radiographic data. Its design did not investigate the exact cause–effect relationship between sinusitis and accessory maxillary ostia.
Conclusion
The study revealed a significant association between chronic sinusitis and presence of an accessory maxillary ostium, specifically on the right side. Further studies are needed to elucidate the cause–effect relationship between accessory maxillary ostia and acute and recurrent sinusitis and determine indications for incorporating the natural and accessory ostia when performing middle meatus antrostomy during endoscopic sinus surgery.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author.
Ethics Approval and Consent to Participate
This study was reviewed and approved by the Institutional Review Board of King Abdullah University Hospital and Jordan University of Science and Technology. This study was conducted in accordance with the Declaration of Helsinki. The consent was waived due to the retrospective nature of the study. We confirm that the privacy of the participants was saved, and the data was anonymized and maintained with confidentiality.
Disclosure
The authors have no conflicts of interest to disclose.
References
- 1.Sahin C, Ozcan M, Unal A. Relationship between development of accessory maxillary sinus and chronic sinusitis. Med J DY Patil Univ. 2015;8(5):606–608. doi: 10.4103/0975-2870.164978 [DOI] [Google Scholar]
- 2.Ghosh P, Kumarasekaran P, Sriraman G. Incidence of accessory ostia in patients with chronic maxillary sinusitis. Int J Otorhinolaryngol Head Neck Surg. 2018;4(2):443–447. doi: 10.18203/issn.2454-5929.ijohns20180705 [DOI] [Google Scholar]
- 3.Prasanna LC, Mamatha H. The location of maxillary sinus Ostium and its clinical application. Indian J Otolaryngol Head Neck Surg. 2010;62(4):335–337. doi: 10.1007/s12070-010-0047-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singhal MD, Singhal DMK. Anatomy of accessory maxillary sinus ostium with clinical application. Int J Med Sci Public Health. 2014;3(3):327–329. doi: 10.5455/ijmsph.2013.301220131 [DOI] [Google Scholar]
- 5.Yenigun A, Fazliogullari Z, Gun C, Uysal II, Nayman A, Karabulut AK. The effect of the presence of the accessory maxillary ostium on the maxillary sinus. Eur Arch Otorhinolaryngol. 2016;273(12):4315–4319. doi: 10.1007/s00405-016-4129-8 [DOI] [PubMed] [Google Scholar]
- 6.Joe JK, Ho SY, Yanagisawa E. Documentation of variations in sinonasal anatomy by intraoperative nasal endoscopy. Laryngoscope. 2000;110(2 Pt 1):229–235. doi: 10.1097/00005537-200002010-00008 [DOI] [PubMed] [Google Scholar]
- 7.Jones NS. CT of the paranasal sinuses: a review of the correlation with clinical, surgical and histopathological findings. Clin Otolaryngol Allied Sci. 2002;27(1):11–17. doi: 10.1046/j.0307-7772.2001.00525.x [DOI] [PubMed] [Google Scholar]
- 8.Sindel A, Turhan M, Ogut E, Akdag M, Bostancı A, Sindel M. An endoscopic cadaveric study: Accessory maxillary ostia. Dicle Med J. 2014;41(2):262–267. doi: 10.5798/diclemedj.0921.2014.02.0413 [DOI] [Google Scholar]
- 9.Matthews BL, Burke AJ. Recirculation of mucus via accessory ostia causing chronic maxillary sinus disease. Otolaryngol Head Neck Surg. 1997;117(4):422–423. doi: 10.1016/S0194-5998(97)70139-6 [DOI] [PubMed] [Google Scholar]
- 10.Mladina R, Vuković K, Poje G. The two holes syndrome. Am J Rhinol Allergy. 2009;23(6):602–604. doi: 10.2500/ajra.2009.23.3375 [DOI] [PubMed] [Google Scholar]
- 11.Lund VJ, Mackay IS. Staging in rhinosinusitis. Rhinology. 1997;117(3 Pt 2):S35–S40. [DOI] [PubMed] [Google Scholar]
- 12.Genc S, Ozcan M, Titiz A, Unal A. Development of maxillary accessory ostium following sinusitis in rabbits. Rhinology. 2008;46(2):121–124. [PubMed] [Google Scholar]
- 13.Capelli M, Gatti P. Radiological study of maxillary sinus using CBCT: Relationship between mucosal thickening and common anatomic variants in chronic rhinosinusitis. J Clin Diagn Res. 2016;10(11):MC07–MC10. doi: 10.7860/JCDR/2016/22365.8931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guerra-Pereira I, Vaz P, Faria-Almeida R, Braga AC, Felino A. CT maxillary sinus evaluation–A retrospective cohort study. Med Oral Patol Oral Cir Bucal. 2015;20(4):e419–e426. doi: 10.4317/medoral.20513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aygun N, Zinreich SJ. Radiology of the nasal cavity and paranasal sinuses In: Cummings Otolaryngology: Head & Neck Surgery. 5th ed Philadelphia, PA: Elsevier Mosby; 2010:662–663. [Google Scholar]
- 16.Anon JB, Jacobs MR, Poole MD, et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004;130(1 Suppl):1–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar H, Choudhry R, Kakar S. Accessory maxillary ostia: topography and clinical application. J Anat Soc India. 2001;50(1):3–5. [Google Scholar]
- 18.Schiller JS, Lucas JW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2011. Vital Health Stat 10. 2012;256:1–218. [PubMed] [Google Scholar]
- 19.Chen Y, Dales R, Lin M. The epidemiology of chronic rhinosinusitis in Canadians. Laryngoscope. 2003;113(7):1199–1205. doi: 10.1097/00005537-200307000-00016 [DOI] [PubMed] [Google Scholar]
- 20.Hastan D, Fokkens WJ, Bachert C, et al. Chronic rhinosinusitis in Europe: An underestimated disease. A GA2LEN study. Allergy. 2011;66(9):1216–1223. doi: 10.1111/j.1398-9995.2011.02646.x [DOI] [PubMed] [Google Scholar]
- 21.Min YG, Jung HW, Kim HS, Park SK, Yoo KY. Prevalence and risk factors of chronic sinusitis in Korea: Results of a nationwide survey. Eur Arch Otorhinolaryngol. 1996;253(7):435–439. doi: 10.1007/BF00168498 [DOI] [PubMed] [Google Scholar]
- 22.Lal D, Rounds AB, Divekar R. Gender-specific differences in chronic rhinosinusitis patients electing endoscopic sinus surgery. Int Forum Allergy Rhinol. 2016;6(3):278–286. doi: 10.1002/alr.21667 [DOI] [PubMed] [Google Scholar]


