Abstract
Introduction
Population-based data on the prevalence, correlates, and treatment utilization of post-traumatic stress disorder by gender and veteran status are limited. With changes in post-traumatic stress disorder diagnostic criteria in 2013, current information from a uniform data source is needed.
Methods
This was a secondary analysis of the 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions-III, which consisted of in-person interviews that were conducted with a representative sample of U.S. adults. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-5 Version was used to assess past-year and lifetime post-traumatic stress disorder among veterans (n=3,119) and civilians (n=32,982). Data were analyzed from January to March 2017.
Results
Adjusting for age and race/ethnicity, women veterans reported the highest rates of lifetime and past-year post-traumatic stress disorder (13.4%, 95% CI=8.8%, 17.9%, and 11.7%, 95% CI=7.1%, 16.4%) compared with women civilians (8.0%, 95% CI=7.4%, 8.6%, and 6.0%, 95% CI=5.5%, 6.6%); men veterans (7.7%, 95% CI=6.5%, 8.8%, and 6.7%, 95% CI=5.7%, 7.8%); and men civilians (3.4%, 95% CI=3.0%, 3.9%, and 2.6%, 95% CI=2.2%, 2.9%). Traumatic event exposure, correlates of lifetime post-traumatic stress disorder, and treatment seeking varied across subgroups. Men and women veterans were more likely than civilians to use a variety of treatment sources, with men civilians being least likely to seek treatment and men veterans exhibiting the longest delay in seeking treatment.
Conclusions
Post-traumatic stress disorder is a common mental health disorder that varies by gender and veteran status. Women veterans’ high rates of post-traumatic stress disorder highlight a critical target for prevention and intervention, whereas understanding treatment barriers for men veterans and civilians is necessary.
INTRODUCTION
Post-traumatic stress disorder (PTSD), a mental health disorder that can occur after exposure to trauma or a life-threatening event, has significant health consequences, including worse physical health, greater mental health comorbidities, lower quality of life, and early mortality.1–5 In the adult U.S. population, the lifetime prevalence rate of PTSD has ranged from 4% to 6% for men and 8% to 13% for women.6–10 Possible reasons for women’s higher PTSD rates are varied and may include gender differences in trauma type exposure, genetics, emotional learning, and memory processing.11
PTSD is considered one of the “signature wounds” of U.S. military veterans.12 The veteran population, although predominantly male, has changed significantly in the past decade. Women veterans are the fastest-growing group of Veterans Health Administration (VA) users, representing 10% of the veteran population by 2018 and 14% by 2033.13 This shift in gender distribution among veterans, alongside the different health profiles and experiences of men and women veterans from civilians,14,15 make it important to ascertain accurate estimates of PTSD by gender and veteran status.
Several studies have estimated the prevalence of PTSD among men and women veterans based on convenience samples. Estimates of current PTSD among women veterans in the VA have ranged from 4% (measured by clinician interview)16 to 21% (measured by self-report).17 Because of the range of reported rates and restricted sampling (i.e., veterans enrolled in VA), it is difficult to compare the prevalence of current PTSD with civilian samples. One study compared current prevalence between veterans and civilians within the same data set (25.7% vs 12.6%), although the sample was restricted to college students, used a short screen, and did not stratify by gender.18 Additionally, there have been mixed findings regarding differences in PTSD prevalence between men and women veterans. Some studies suggest that women veterans are as likely to meet current PTSD criteria as their male counterparts,19–21 whereas others found higher rates among men veterans.16 Few studies of veterans have directly compared lifetime PTSD rates by gender, and none have included a civilian comparator.
Recently, Wisco and colleagues22 provided estimates of PTSD prevalence in a nationally representative veteran sample. Based on the DSM-IV version of the PTSD Checklist, they estimated lifetime and past-year rates of 19% and 6% for women veterans and 7% and 5% for men veterans, respectively. Compared with other epidemiologic studies,6–10 the lifetime rate for men veterans is similar to civilians but much higher for women veterans compared with civilians. Nonetheless, this comparison is limited because of marked differences in demographics, methodology, and diagnostic tools used across studies. Furthermore, in the change from DSM-IV to DSM-5 in 2013, the new PTSD definition includes additional symptoms and significant changes in symptom clusters.10
The current study analyzes data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) to examine differences in PTSD by gender and veteran status. Specifically, differences in traumatic exposures, DSM-5 PTSD diagnoses (lifetime and past-year), demographic and trauma type correlates of PTSD, and treatment utilization for PTSD are evaluated between women and men veterans and civilians.
METHODS
Study Sample
NESARC-III sampled from a representative sample of non-institutionalized U.S. residents aged ≥18 years who were not current active-duty military using multistage probability sampling in 2012–2013.23,24 The total sample size was 36,309 and the overall response rate was 60.1%, comparable with other national surveys.25,26
Veteran status was assessed using the question: Have you ever served on Active Duty in the U.S. Armed Forces, Military Reserves, or National Guard? Respondents answering: Yes, on active duty in past, but not now were classified as veterans.
Measures
The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-5 Version (AUDADIS-5) is a structured, in-person diagnostic interview designed for use by non-clinician interviewers.27 This instrument operationalizes DSM-5 criteria for PTSD in addition to other disorders.
Respondents were queried about 19 potentially traumatic events they may have directly experienced, and 13 they may have witnessed or learned about. If a respondent reported more than four events, only the four most severe events were recorded. Respondents were asked to nominate which event was their worst trauma. Personally experienced events were organized thematically under childhood abuse, interpersonal violence, combat or war zone, serious/life-threatening illness or injury, natural disaster, juvenile detention or jail, and other.
An AUDADIS-5/DSM-5 PTSD diagnosis required reporting at least one traumatic event. Respondents were assessed for remaining criteria concerning the event they nominated as their worst trauma. Respondents had to report at least one symptom of persistent intrusion (Criterion B); at least one of avoidance of stimuli (Criterion C); and three or more each of negative mood or cognitive changes (Criterion D) and increased arousal (Criterion E) for the NESARC-derived PTSD diagnosis, yielding a relatively narrow diagnostic definition. Respondents further had to report duration of ≥1 month and clinically significant impairment or distress. Past-year and prior to the past-year diagnoses were combined into a lifetime measure. Test–retest reliability of past-year and prior to the past–year PTSD diagnoses was fair (0.41 and 0.44, respectively), and reliability of the dimensional PTSD criteria scale was good (intraclass correlation coefficient=0.69).28 Procedural validity of PTSD assessment, evaluated as concordance between the AUDADIS-5 PTSD and the clinician-administered Psychiatric Research Interview for Substance and Mental Disorders, DSM-5 version,29,30 in a general population sample, was fair to moderate across time frames (0.34–0.46); concordance of dimensional criteria scales between the instruments was good (interclass correlation coefficient=0.69).31
Individuals with PTSD were asked if they ever sought help to get over reactions they experienced from the stressful event from (1) any health professional (e.g., counselor, therapist, or other medical professional); (2) a self-help or support group, hotline, or Internet chat room; or if they ever (3) stayed in a hospital for at least one night because of symptoms; (4) went to an emergency room for help with symptoms; and (5) were prescribed any medicines for help with symptoms. Respondents were also asked whether they sought help in the past year, age of onset of PTSD, and age the first time they sought help.
Statistical Analysis
Data were analyzed from January to March 2017. Sample demographics and the prevalence of experiencing traumatic events, percentage who reported each event as their worst trauma, and past-year and lifetime PTSD were estimated by gender and veteran status. Given that age and race/ethnicity are non-mutable demographic factors that vary by gender and veteran status, age-and race/ethnicity-adjusted prevalence and 95% CIs of PTSD diagnoses were calculated from logistic regression equations,32 with pairwise comparisons made using chi-square tests. To jointly estimate associations of demographic characteristics and trauma types with lifetime PTSD, logistic regression with separate models for each of the four subgroups were used. Natural disaster and juvenile detention/jail were not included as specific trauma types because they were rare (<5% to 12%). Among those with lifetime PTSD, the prevalence of help-seeking behaviors, mean age at PTSD onset, mean age when first talked to someone, and mean number of years between onset and talking to someone were calculated by gender and veteran status. Pairwise comparisons were made using chi-square tests for categorical variables and t-tests for continuous variables.
Finally, the narrow definition of PTSD might have missed some mild cases, possibly underestimating prevalence rates and biasing associations. Thus, lifetime prevalence and demographic and trauma correlates were reanalyzed using a broad definition of PTSD provided in NESARC-III. Under that definition, respondents were classified as having lifetime PTSD if they met DSM-5 Criteria A through E (two or more symptoms each required for Criteria D and E), with or without duration of >1 month and with or without impairment or distress. All analyses were conducted using Stata, version 14, and accounted for the sample design of NESARC-III. The IRB at VA Puget Sound Health Care System approved this study.
RESULTS
Of the 36,309 individuals included in the NESARC-III, those who indicated only having training in the National Guard/Reserve (n=200) or with unknown veteran status (n=8) were excluded. The analytic sample of 36,101 participants included 20,386 women of whom 1.8% were veterans (n=379) and 15,715 men of whom 18.3% were veterans (n=2,740). Descriptively, veterans were older, more likely to be white, and have higher income and some college compared with their civilian counterparts (Appendix Table 1, available online).
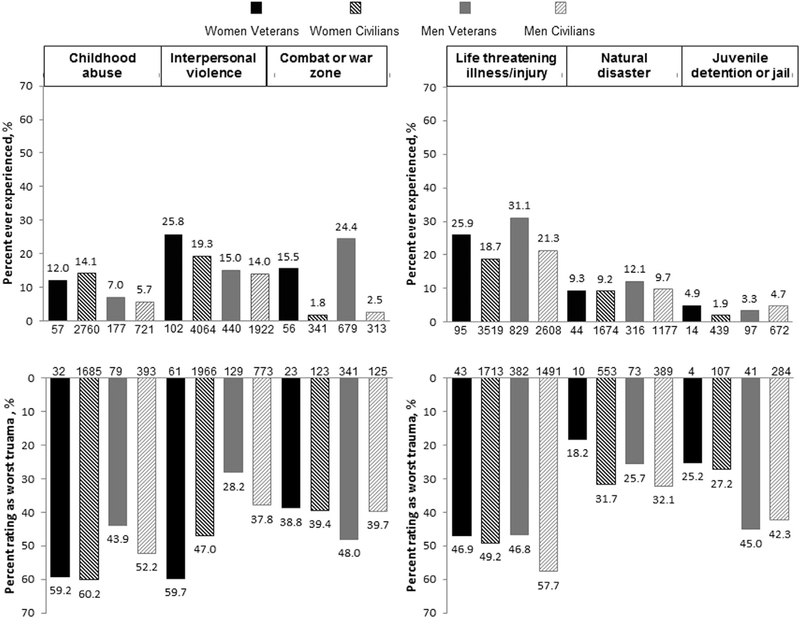
Childhood abuse was more commonly reported by women veterans and civilians than by men veterans or civilians (Figure 1, Appendix Table 2, available online). Among those reporting childhood abuse, women were also more likely to report that it was their worst traumatic event. Compared with the other three subgroups, women veterans were the most likely to report experiencing interpersonal violence, particularly adult sexual assault and being beaten up by a partner, and were also the most likely among those with such experiences to report it as being the worst traumatic event. Men and women veterans were more likely than civilians to have experienced combat or exposure to a war zone, whereas men veterans were the most likely to report it as worst. Similarly, men and women veterans were the most likely to report experiencing life-threatening illness or injury, with men civilians being most likely to report it as their worst event. Of the four subgroups, men veterans were the most likely to report experiencing a natural disaster, but men and women civilians with such an experience were more likely than veterans to report it as the worst event. Only small differences were evident in reporting experiencing juvenile detention or jail.
Figure 1. Prevalence of traumatic event types by gender and veteran status.
Note: Percents (%) are weighted and indicated either above or below each bar. The numbers along the x-axis represent the relevant sample size (the numerator). The denominator for reporting “ever” experiencing the trauma type is n=379 women veterans, n=20,007 women civilians, n=2,740 men veterans, and n=12,975 men civilians. The denominator for reporting a trauma type as the “worst” is the number of people reporting “ever” experiencing the trauma (i.e., the numerator reported above for each group).
Men and women veterans were the most likely to report at least one traumatic event (66.2% and 60.5%) compared with their civilian counterparts (47.8% and 49.9% respectively; Appendix Table 1, available online). The number of traumas personally experienced was similar among men and women veterans, with approximately 12% of both subgroups reporting three traumatic events and 11% to 12% at least four traumatic events.
The unadjusted lifetime and past-year prevalence of PTSD was 13.2% and 11.4% for women veterans, respectively; 7.9% and 6.0% for women civilians; 6.2% and 5.2% for men veterans; and 3.6% and 2.7% for men civilians (Table 1). Women veterans had significantly higher rates of both lifetime and past-year PTSD than the other three subgroups. Women civilians and men veterans had similar prevalence rates, which were significantly higher than men civilians’ prevalence rates. Differences were still apparent after adjustment for age and race/ethnicity.
Table 1.
Prevalence of Past-Year and Lifetime PTSD by Gender and Veteran Status
| Women |
Men |
|||||||
|---|---|---|---|---|---|---|---|---|
| Veterans (n=379)a,b,c,d,e,f |
Civilians (n=20,007)c,f,g,h |
Veterans (n=2,740)c,f,g,h |
Civilians (n=12,975)a,b,d,e,g,h |
|||||
| PTSD | n (% unadj) | % adj (95% CI)i | n (% unadj) | % adj (95% CI)i | n (% unadj) | % adj (95% CI)i | n (% unadj) | % adj (95% CI)i |
| Past-year PTSD | 39 (11.4) | 11.7 (7.1, 16.4) | 1,214 (6.0) | 6.0 (5.5, 6.6) | 153 (5.2) | 6.7 (5.7, 7.8) | 370 (2.7) | 2.6 (2.2, 2.9) |
| Lifetime PTSD | 48 (13.2) | 13.4 (8.8, 17.9) | 1,610 (7.9) | 8.0 (7.4, 8.6) | 181 (6.2) | 7.7 (6.5, 8.8) | 496 (3.6) | 3.4 (3.0, 3.9) |
Past-year PTSD p < 0.05 compared with women civilians.
Past-year PTSD p < 0.05 compared with men veterans.
Past-year PTSD p < 0.05 compared with men civilians.
Lifetime PTSD p < 0.05 compared with women civilians.
Lifetime PTSD p < 0.05 compared with men veterans.
Lifetime PTSD p < 0.05 compared with men civilians.
Past-year PTSD p < 0.05 compared with women veterans.
Lifetime PTSD p < 0.05 compared with women veterans.
Adjusted for age and race/ethnicity.
Adj, adjusted; PTSD, post-traumatic stress disorder; Unadj, unadjusted.
Associations of demographics and traumatic events with lifetime PTSD varied across subgroups (Table 2). No significant associations were evident for women veterans, likely because of small sample size. Among women civilians and men veterans, younger age was associated with lifetime PTSD. Among all but women veterans, lower income, childhood abuse, and life-threatening illness or injury were also associated with PTSD diagnosis. Not being married or living with someone and interpersonal violence were associated with lifetime PTSD among women and men civilians, with interpersonal violence appearing to have stronger effects among women civilians. Among women civilians, being black was associated with lower likelihood of lifetime PTSD relative to being white, but among men veterans it was associated with increased likelihood. Among men civilians, being other, non-Hispanic was associated with decreased likelihood of lifetime PTSD relative to being white. Exposure to combat or war was only associated with PTSD among men veterans.
Table 2.
Associations of Demographic Characteristics and Trauma Types With Lifetime PTSD by Gender and Veteran Status
| Women |
Men |
|||
|---|---|---|---|---|
| Variables | Veterans, OR (95% CI) (n=379) | Civilians, OR (95% CI) (n=20,007) | Veterans, OR (95% CI) (n=2,740) | Civilians, OR (95% CI) (n=12,975) |
| Age (5-year increments) | 0.91 (0.80, 1.04) | 0.91 (0.89, 0.93) | 0.89 (0.83, 0.95) | 0.95 (0.91, 1.00) |
| Race/ethnicity | ||||
| Black, non-Hispanic | 0.63 (0.20, 2.03) | 0.70 (0.57, 0.87) | 2.22 (1.25, 3.94) | 1.03 (0.76, 1.41) |
| Other, non-Hispanic | 2.81 (0.52, 15.28) | 0.91 (0.58, 1.42) | 2.20 (0.95, 5.11) | 0.53 (0.29, 0.97) |
| Hispanic | 0.35 (0.08, 1.47) | 0.72 (0.59, 0.89) | 1.39 (0.69, 2.80) | 1.14 (0.82, 1.60) |
| Annual household income <$20,000 | 0.83 (0.28, 2.41) | 1.47 (1.21, 1.78) | 1.85 (1.10, 3.13) | 1.51 (1.14, 1.99) |
| Not married/living with someone | 2.21 (0.73, 6.74) | 1.18 (1.01, 1.38) | 1.53 (0.98, 2.40) | 1.43 (1.06, 1.94) |
| No college | 0.68 (0.18, 2.59) | 1.17 (1.00, 1.36) | 1.18 (0.76, 1.84) | 1.44 (1.08, 1.92) |
| Sexual minority | 0.36 (0.08, 1.64) | 1.40 (0.99, 1.96) | 1.18 (0.31, 4.53) | 1.56 (0.96, 2.54) |
| Childhood abuse | 2.21 (0.82, 5.96) | 4.75 (4.01, 5.62) | 3.92 (2.07, 7.43) | 4.89 (3.71, 6.46) |
| Interpersonal violence | 1.18 (0.52, 2.69) | 4.00 (3.35, 4.77) | 1.27 (0.77, 2.07) | 2.42 (1.80, 3.25) |
| Combat or war zone | 2.65 (0.83, 8.41) | 0.99 (0.55, 1.76) | 5.05 (3.60, 7.10) | 1.38 (0.67, 2.83) |
| Serious/life-threatening illness or injury | 2.60 (0.94, 7.21) | 1.86 (1.55, 2.22) | 2.32 (1.55, 3.47) | 3.16 (2.38, 4.19) |
Note: Referent group for race/ethnicity is non-Hispanic white. Reference groups for childhood abuse, interpersonal violence, combat or war zone, and serious/life-threatening illness or injury were those not reporting that they experienced the specific trauma. Boldface indicates statistical significance (p < 0.05).
PTSD, post-traumatic stress disorder.
Among those with lifetime PTSD, men civilians were the least likely to have sought treatment, whereas veterans were sources (Table 3). Specifically, both women and men veterans were more likely than civilians to use medications, and men veterans were more likely than men and women civilians to have sought counseling or therapy, attend self-help groups, been hospitalized because of PTSD symptoms, and to have sought help in the past 12 months. Nonetheless, men veterans on average had the longest delay in seeking treatment.
Table 3.
PTSD Treatment Utilization Among Those With Lifetime PTSD by Gender and Veteran Status
| Women |
Men |
|||
|---|---|---|---|---|
| PTSD treatment utilization | Veterans, n (% unadj) (n=48) | Civilians, n (% unadj) (n=1,610) | Veterans, n (% unadj) (n=181) | Civilians, n (% unadj) (n=496) |
| Counselor/therapist | 34 (71.4)a | 871 (55.1)a,b | 118 (64.2)a | 225 (48.2) |
| Self-help group/hotline/chat room | 13 (28.8) | 274 (17.4)a,b | 45 (27.1)a | 58 (11.1) |
| Hospitalization | 12 (14.3) | 177 (10.4)b | 38 (22.5)a | 47 (7.7) |
| Emergency room | 7 (9.3) | 201 (12.1) | 25 (15.1) | 49 (9.5) |
| Medicine/drugs | 25 (54.4)a,c | 513 (32.7)b | 85 (48.9)a | 140 (30.5) |
| Sought help in the past 12 months | 18 (51.5) | 373 (38.3)b | 63 (54.8)a | 97 (38.8) |
| Ever sought treatment | 36 (73.3)a | 950 (60.4)a | 123 (67.0)a | 247 (52.3) |
| Age at first onset, M (SD) | 25.7 (2.7) | 24.9 (0.6) | 26.1 (1.2) | 24.7 (0.8) |
| Age when first talked to someone, M (SD)d | 28.7 (1.7)b | 29.6 (0.7)b | 37.4 (2.5)a | 29.9 (1.3) |
| Delay to first talking to someone, M (SD)d | 4.7 (1.5)b | 5.2 (0.7)b | 10.6 (2.4) | 4.4 (1.0)b |
Note: Percentages are weighted.
p < 0.05 compared with men civilians.
p < 0.05 compared with men veterans.
p < 0.05 compared with women civilians.
Sample size includes only those who ever sought treatment (n=36 women veterans, n=950 women civilians, n=123 men veterans, and n=247 men civilians).
PTSD, post-traumatic stress disorder; unadj, unadjusted.
The prevalence of broadly defined PTSD was considerably higher than the narrower lifetime definition (women veterans 20.5%, women civilians 13.5%, men veterans 10.2%, and men civilians 7.1%). Pairwise comparisons across groups, however, demonstrated the same patterns as seen with the narrower definition (data not shown). Additionally, the directions and magnitudes of associations with demographics and trauma types were similar to those observed with the narrowly defined lifetime PTSD, although some associations became statistically significant (Appendix Table 3, available online). Finally, to examine whether the narrow NESARC-derived definition significantly underestimated DSM-5–defined PTSD, an alternate PTSD variable was created that aligned with DSM-5 criteria (i.e., broadly defined PTSD plus impairment/distress and 1-month symptom duration). This resulted in an identical lifetime sample size as the NESARC-derived definition, increasing confidence in the accuracy of NESARC’s definition.
DISCUSSION
In this nationally representative sample, there were variations in traumatic event exposure, prevalence and correlates of PTSD, and PTSD treatment utilization by gender and veteran status. Veterans were more likely than civilians to experience at least one traumatic event, and the number of traumas was similarly distributed between men and women veterans, suggesting that across gender, veterans are more vulnerable to experiencing traumatic events than civilians. Men veterans reported the highest levels of war zone exposure and women veterans reported the highest levels of interpersonal violence, particularly sexual assault and intimate partner violence. This is consistent with several studies demonstrating women veterans’ high rates of sexual and physical assault.21,33,34
Lifetime and past-year prevalence of PTSD tended to be lower across subgroups compared with rates reported in some other population-based studies,6,7,22 potentially as a result of use of DSM-5 instead of DSM-IV.10 Women veterans’ significantly higher rates of lifetime and past-year PTSD compared with other groups is a finding that has been frequently hypothesized because of rates observed in convenience samples,17,35 but until now has not been examined in a nationally representative sample of the general population including civilians. It also suggests a need for effective preventive and intervention services targeting women veterans. Additionally, differences between lifetime and past-year rates of PTSD were relatively small, implying that PTSD is a chronic condition that does not appear to remit with time. Indeed, clinical trials suggest that even after receipt of evidence-based treatment, diagnostic rates are still high (60%–72%).36
Demographic characteristics and trauma types were generally associated with lifetime PTSD as expected.8 The association between interpersonal violence and lifetime PTSD was stronger among women than men civilians, which may reflect greater severity of these traumas among women civilians. Notably, the highest OR for both women and men civilians was childhood abuse, whereas the highest OR for men veterans was combat exposure. Combat exposure was not a significant correlate for women veterans, likely as a result of limited power, but it was in a similar direction as for the men. A recent study with Navy personnel found that when women and men had similar combat experiences, the risk of PTSD was significantly higher among women.37 Moreover, during the time of survey collection, women were prohibited from serving in many combat roles. With a shift in policy in 2015,38 women’s risk for combat-related PTSD may increase and should be evaluated in future studies. Finally, additional potential correlates of PTSD, such as other mental health and substance use disorders, likely also vary by gender and veteran status and should be considered in future studies.
Among individuals with lifetime PTSD, rates of lifetime treatment seeking ranged from 52% to 73%. These rates may over-report true treatment seeking, as they include visits to the emergency room or stays in the hospital (which may occur as a result of trauma-related wounds), as well as attempts at self-help. Nonetheless, men civilians demonstrated the lowest rates whereas veterans were more likely than civilians to use a variety of treatment sources. This could reflect greater societal and cultural awareness of PTSD among veterans as well as efforts made by VA to engage veterans in PTSD services.39 As an integrated healthcare system, access to psychiatric medications and psychotherapy may also be more common and easily facilitated for patients compared with care received in the private sector.
Despite veterans’ greater use of certain types of PTSD treatment than civilians, and men veterans’ greater likelihood of seeking help in the past year than civilians, men veterans were also the group with the longest delay in seeking help. This may reflect concerns about what military-related disclosures are permissible or concerns about stigma.40 Male gender has been associated with increased stigma related to mental health care,41 and this may be particularly true among veterans, who tend to highly value stoicism and self-reliance.42,43 Research that further examines mechanisms that explain men veterans’ greater delay in seeking care is necessary as are interventions that address barriers to care.
Limitations
Study limitations include the NESARC-III’s cross-sectional design, which precluded examination of prevalence estimates and predictors over time. Questions about PTSD treatment did not provide information about the site of care (VA/military versus civilian) or the quality or length of time engaged in treatment. There was a relatively small number of women veterans, which limited power. As the number of women veterans continues to increase,44 it will be important to conduct larger, fully powered studies. Finally, the narrow definition of PTSD included two additional symptoms than required for DSM-5 diagnosis, potentially missing milder cases and underestimating prevalences. Nonetheless, sensitivity analysis demonstrated consistency with DSM-5 criteria and that directions and magnitudes of associations did not differ substantially between the narrow and broader definitions, similar to findings by another study using the NESARC-III.8 Moreover, prior studies on PTSD using NESARC-III have also used this narrow definition,8,45 and validation work on the past-year and lifetime designations provided by NESARC-III have shown good reliability and procedural validity.28,29,31
CONCLUSIONS
The NESARC-III, which included a representative sample of the U.S. population and incorporated a detailed PTSD diagnostic assessment, provided a unique opportunity to identify differences by gender and veteran status. Veterans were more likely than civilians to be exposed to at least one traumatic event, and women were more likely than men to experience childhood abuse and interpersonal violence. At the intersection of these identities, women veterans had the highest prevalence of both lifetime and past-year PTSD, highlighting a significant need for targeted prevention and intervention. At the same time, men civilians were least likely to seek treatment and men veterans exhibited the longest delay between onset of PTSD and help seeking, indicating the importance of understanding and reducing treatment barriers for these groups. Finally, even though between one half to two thirds of those with lifetime PTSD sought treatment, the similarity between lifetime and past-year prevalence rates suggests that PTSD is a chronic mental health condition. Clinical practice guidelines strongly support the use of trauma-focused psychological treatments for the treatment of PTSD,46 and enhancing access, treatment options, and the evidence base will likely be critical for years to come.
Supplementary Material
ACKNOWLEDGMENTS
The original data set for the National Epidemiologic Survey on Alcohol and Related Conditions is available from the National Institute on Alcohol Abuse and Alcoholism (www.niaaa.nih.gov).
Drs. Lehavot and Katon were supported by VA Clinical Science Research & Development (CX000867) and Health Services Research & Development (CDA 13-266) Career Development Awards, respectively. Dr. Chen was supported by a VA Office of Academic Affiliations Advanced Fellowship in Health Services Research and Development (#TPP 61-000-14). The views expressed in this article are solely those of the authors and do not reflect an endorsement or the official policy or position of the Department of Veterans Affairs. The authors have no conflicts of interest to report.
Footnotes
No financial disclosures were reported by the authors of this paper.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2017.09.008.
REFERENCES
- 1.Boscarino JA. Posttraumatic stress disorder and mortality among U.S. army veterans 30 years after military service. Ann Epidemiol. 2006;16 (4):248–256. 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am J Psychiatry. 2007;164(1):150–153. 10.1176/ajp.2007.164.1.150. [DOI] [PubMed] [Google Scholar]
- 3.Perkonigg A, Kessler RC, Storz S, Wittchen HU. Traumatic events and post-traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatr Scand. 2000;101(1):46–59. 10.1034/j.1600-0447.2000.101001046.x. [DOI] [PubMed] [Google Scholar]
- 4.Schnurr PP, Friedman MJ, Sengupta A, Jankowski MK, Holmes T. PTSD and utilization of medical treatment services among male Vietnam veterans. J Nerv Ment Dis. 2000;188(8):496–504. 10.1097/00005053-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Schnurr PP, Hayes AF, Lunney CA, McFall M, Uddo M. Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(4):707–713. 10.1037/0022-006X.74.4.707. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 7.Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 1993;61(6):984–991. 10.1037/0022-006X.61.6.984. [DOI] [PubMed] [Google Scholar]
- 8.Goldstein RB, Smith SM, Chou SP, et al. The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Soc Psychiatry Psychiatr Epidemiol. 2016;51(8):1137–1148. 10.1007/s00127-016-1208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25 (3):456–465. 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537–547. 10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Committee on the Assessment of Ongoing Effects in the Treatment of Posttraumatic Stress Disorder, National Academy of Medicine. Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 12.Tanielian T, Jaycox LH. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2013. [Google Scholar]
- 13.Yano E, Hayes P, Wright S, et al. Integration of women veterans into VA quality improvement research efforts: what researchers need to know. J Gen Intern Med. 2010;25(suppl 1):56–61. 10.1007/s11606-009-1116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences: U.S. military, veteran, and civilian men. Am J Prev Med. 2012;43(5):483–489. 10.1016/j.amepre.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 15.Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. Am J Prev Med. 2012;42(5):473–480. 10.1016/j.amepre.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Magruder KM, Frueh BC, Knapp RG, et al. Prevalence of posttraumatic stress disorder in Veterans Affairs primary care clinics. Gen Hosp Pscyhiatry. 2005;27(3):169–179. 10.1016/j.genhosppsych.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 17.Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164(4):394–400. 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- 18.Fortney JC, Curran GM, Hunt JB, et al. Prevalence of probable mental disorders and help-seeking behaviors among veteran and non-veteran community college students. Gen Hosp Psychiatry. 2016;38:99–104. 10.1016/j.genhosppsych.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang H, Dalager N, Mahan C, Ishii E. The role of sexual assault on the risk of PTSD among Gulf War veterans. Ann Epidemiol. 2005;15 (3):191–195. 10.1016/j.annepidem.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Pereira A Combat trauma and the diagnosis of post-traumatic stress disorder in female and male veterans. Mil Med. 2002;167(1):23–27. [PubMed] [Google Scholar]
- 21.Vogt DS, Pless AP, King LA, King DW. Deployment stressors, gender, and mental health outcomes among Gulf War I veterans. J Trauma Stress. 2005;18(3):272–284. 10.1002/jts.20018. [DOI] [PubMed] [Google Scholar]
- 22.Wisco BE, Marx BP, Wolf EJ, Miller MW, Southwick SM, Pietrzak RH. Posttraumatic stress disorder in the U.S. veteran population: results from the National Health and Resilience in Veterans Study. J Clin Psychiatry. 2014;75(12):1338–1346. 10.4088/JCP.14m09328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grant BF, Amsbary M, Chu A, et al. Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2014. [Google Scholar]
- 24.Bureau of the Census. American Community Survey, 2012. Suitland, MD: Bureau of the Census; 2013. [Google Scholar]
- 25.Substance Abuse and Mental Health Services Administration. Results From the 2013 National Survey on Drug Use and Health-Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC). Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2012. Hyattsville, MD: National Center for Health Statistics; 2014. [Google Scholar]
- 27.Grant BF, Goldstein RB, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule—Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Version (AUDADIS-5). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2011. [Google Scholar]
- 28.Grant BF, Goldstein RB, Smith SM, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug Alcohol Depend. 2015;148:27–33. 10.1016/j.drugalcdep.2014.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hasin DS, Aivadyan C, Greenstein E, Grant BF. Psychiatric Research Interview for Substance Use and Mental Disorders, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (PRISM-5) Version. New York, NY: Columbia University, Department of Psychiatry; 2011. [Google Scholar]
- 30.Hasin D, Samet S, Nunes E, et al. Diagnosis of comorbid psychiatric disorders in substance users assessed with the Psychiatric Research Interview for Substance and Mental Disorders for DSM-IV. Am J Psychiatry. 2006;163(4):689–696. 10.1176/ajp.2006.163.4.689. [DOI] [PubMed] [Google Scholar]
- 31.Hasin DS, Shmulewitz D, Stohl M, et al. Procedural validity of the AUDADIS-5 depression, anxiety and post-traumatic stress disorder modules: substance abusers and others in the general population. Drug Alcohol Depend. 2015;152:246–256. 10.1016/j.drugalcdep.2015.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams R Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12(2): 308–331. [Google Scholar]
- 33.Lehavot K, Simpson T. Trauma, posttraumatic stress disorder, and depression among sexual minority and heterosexual women veterans. J Couns Psychol. 2014;61(3):392–403. 10.1037/cou0000019. [DOI] [PubMed] [Google Scholar]
- 34.Zinzow HM, Grubaugh AL, Monnier J, Suffoletta-Maierle S, Frueh BC. Trauma among female veterans: a critical review. Trauma Violence Abuse. 2007;8(4):384–400. 10.1177/152483-8007307295. [DOI] [PubMed] [Google Scholar]
- 35.Surís A, Lind L, Kashner TM, Borman PD, Petty F. Sexual assault in women veterans: an examination of PTSD risk, health care utilization, and cost of care. Psychosom Med. 2004;66(5):749–756. 10.1097/01.psy.0000138117.58559.7b. [DOI] [PubMed] [Google Scholar]
- 36.Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489–500. 10.1001/jama.2015.8370. [DOI] [PubMed] [Google Scholar]
- 37.MacGregor AJ, Clouser MC, Mayo JA, Galarneau MR. Gender differences in posttraumatic stress disorder among U.S. Navy healthcare personnel. J Womens Health. 2017;26(4):338–344. 10.1089/jwh.2014.5130. [DOI] [PubMed] [Google Scholar]
- 38.Rosenberg M, Phillips D. All combat roles now open to women, defense secretary says. New York Times. December 3, 2015. [Google Scholar]
- 39.Karlin BE, Cross G. From the laboratory to the therapy room: national dissemination and implementation of evidence-based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69(1):19–33. 10.1037/a0033888. [DOI] [PubMed] [Google Scholar]
- 40.Hoge CW, Grossman SH, Auchterlonie JL, Riviere LA, Milliken CS, Wilk JE. PTSD treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. Psychiatr Serv. 2014;65(8):997–1004. 10.1176/appi.ps.201300307. [DOI] [PubMed] [Google Scholar]
- 41.Kuehn B Men face barriers to mental health care. JAMA. 2006;296 (9):2303–2304. 10.1001/jama.296.19.2303. [DOI] [PubMed] [Google Scholar]
- 42.Vogt D Mental health-related beliefs as a barrier to service use for military personnel and veterans: a review. Psychiatr Serv. 2011;62(2): 135–142. 10.1176/ps.62.2.pss6202_0135. [DOI] [PubMed] [Google Scholar]
- 43.Whealin JM, Kuhn E, Pietrzak RH. Applying behavior change theory to technology promoting veteran mental health care seeking. Psychol Serv. 2014;11(4):486–494. 10.1037/a0037232. [DOI] [PubMed] [Google Scholar]
- 44.Office of the Actuary, Department of Veterans Affairs. Veteran population projections: FY2010 to FY2040. www.va.gov/vetdata/docs/QuickFacts/Population_quickfacts.pdf. Published 2011 Accessed June 21, 2017.
- 45.Smith SM, Goldstein RB, Grant BF. The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). J Psychiatr Res. 2016;82:16–22. 10.1016/j.jpsychires.2016.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Department of Veterans Affairs, Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal.pdf. Published 2017 Accessed July 5, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.