Abstract
A 77 year-old man was referred to Urology with an enlarging left adrenal mass after treatment with androgen deprivation therapy for metastatic castrate-resistant prostate cancer. He underwent a robotic-assisted left radical adrenalectomy, with pathology revealing metastatic adenocarcinoma consistent with a primary prostate adenocarcinoma. The patient had a durable oncological response to metastasectomy with no evidence of biochemical or radiological recurrence after 5 years of follow-up. Adrenal metastases from prostate cancer are extremely rare, representing only 1% of metastatic cases. Surgical resection of oligometastatic prostate cancer recurrences may be considered in select patients and may improve progression-free survival.
Keywords: Adrenal metastasis, Adrenalectomy, Oligometastasis, Prostate cancer
INTRODUCTION: Prostate cancer (PCa) is the most common non-cutaneous cancer diagnosed in American men.1 Metastatic PCa has a well-recognized pattern of spread, most commonly to pelvic lymph nodes and bones. Less common metastatic sites include distant lymph nodes, lungs, and liver.2 Adrenal metastasis is considered extremely rare, accounting for only 1% of all metastatic cases.2 While androgen deprivation therapy (ADT) is the standard treatment in metastatic PCa, metastasis-directed therapy (MDT) may be considered in selected men with oligometastatic PCa. Herein, we report a case of complete biochemical response following metastasectomy of a solitary adrenal recurrence in a man with metastatic castrate-resistant PCa.
CASE PRESENTATION: A 77-year-old man was referred to the Urology clinic with an enlarging left adrenal mass. He had initially presented to his local physician with vague abdominal discomfort three years earlier. His prostate specific antigen (PSA) was noted to be elevated to 11 ng/mL. His other laboratory tests were unremarkable. Computerized tomography (CT) imaging of the abdomen at the time demonstrated left hydronephrosis with a transition point at the ureteropelvic junction and enlarged retroperitoneal lymph nodes. The hydronephrosis was managed with serial ureteral stent exchanges. A retroperitoneal node was biopsied, and immunohistochemistry demonstrated staining for prostatic acid phosphatase, supporting the diagnosis of metastatic prostate adenocarcinoma. He responded well to ADT with a luteinizing hormone-releasing hormone agonist injection every three months, leading to an undetectable PSA and regression of his retroperitoneal nodes. His PSA gradually rose to 1.0 ng/mL and surveillance CT imaging revealed a 5.9 cm left adrenal mass, and an atrophic left kidney. He was then referred to our institution for further management. Repeat laboratory testing confirmed a further rise in PSA to 3.6 ng/mL, despite ADT. Follow-up chest and abdominal CT scans demonstrated that the left adrenal mass increased in size to 7.6 cm with no other evidence of regional lymphadenopathy or distant metastasis (Fig. 1, Fig. 2). Whole body bone scan demonstrated no evidence of bony metastasis and functional nuclear medicine renogram revealed a poorly-functioning left kidney. The left adrenal mass was biopsied and microscopic examination was consistent with poorly differentiated metastatic carcinoma of prostatic origin. The patient elected to proceed with surgical resection of the solitary metastasis to the adrenal gland with concurrent simple nephrectomy. With the patient in the right lateral decubitus position, pneumoperitoneum was established, and a six-port transperitoneal technique with the da Vinci surgical system was used. Following mobilization of the colon, dense desmoplastic reaction was noted around the left ureter, aorta, and left renal hilum. The medial aspect of Gerota's fascia was very adherent to the periaortic tissue. Intraoperative ultrasonography was used to localize and delineate the adrenal mass. The mass was densely adherent to the upper pole of the kidney. An en-bloc left radical adrenalectomy and left simple nephrectomy with para-aortic hilar lymphadenectomy was performed. Total operating time was 4 hours and the estimated blood loss was 50 mL. There were no intra-operative complications. The patient had mild postoperative atelectasis, which was managed with incentive spirometry and physical therapy, and he was discharged home on postoperative day 5. The final pathology revealed a 3.3 × 3.4 × 4.6 cm poorly differentiated metastatic adenocarcinoma consistent with primary prostate adenocarcinoma with negative resection margins and no nodal metastasis. The renal parenchyma showed chronic tubulointerstitial nephritis and diffuse glomerulosclerosis. His first post-operative PSA three months after surgery was undetectable, and he was maintained on ADT. At 5 years follow-up after adrenal metastasectomy, the patient was asymptomatic and had an Eastern Cooperative Oncology Group performance status of 0. He had an undetectable PSA, no evidence of recurrence on CT and bone scan imaging, and required no chemotherapy or other adjuvant therapies.
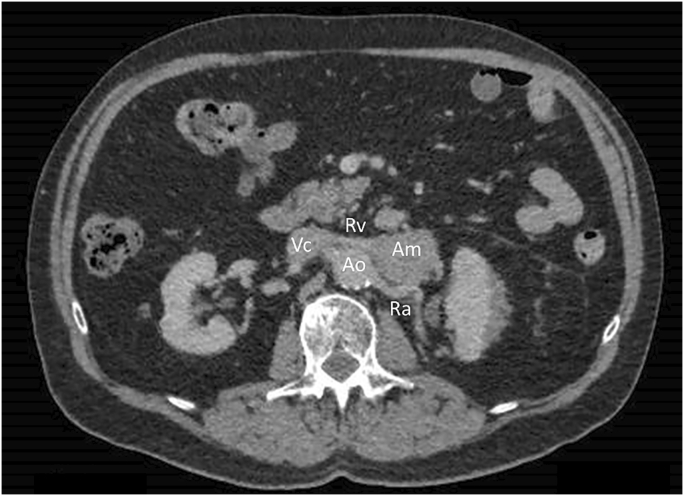
Fig. 1.
Computed tomography scan of abdomen in the axial plane demonstrating a left adrenal mass abutting the left renal vein. Ao = aorta. Vc = vena cava. Rv = renal vein. Ra = renal artery. Am = adrenal mass.
Fig. 2.
Computed tomography scan of abdomen in the coronal plane showing a 4.6 × 4.3 × 7.6 cm left adrenal mass. Ao = aorta. Vc = vena cava. Ra = renal artery. Am = adrenal mass.
DISCUSSION: Isolated adrenal metastasis from PCa is extremely rare. In a retrospective study of 508 patients with PCa, Long et al. reported only 1 patient (0.2%) with an adrenal metastasis compared to 95 patients (18.7%) with nodal metastases.3 In an analysis of 74,826 patients with metastatic PCa from the Nationwide Inpatient Sample between 1998 and 2010, metastasis to bone was identified in 84%, followed by distant lymph nodes (11%), liver (10%), thorax (9%), brain (3%), digestive system (3%), kidney (1%), and adrenal gland (1%).2 In patients with a single-site metastasis, kidney and adrenal were involved in 0.3%. Of note, 15% of patients had visceral metastases at presentation without secondary bone disease.
Oligometastatic PCa is most commonly defined as the presence of ≤5 metastatic lesions on imaging studies. While ADT is the mainstay of management, MDT may be a viable treatment option for selected men with low-volume oligometastatic disease, in the form of stereotactic ablative radiation therapy (SABR) or metastasectomy. There are several potential advantages of offering MDT in selected patients, including delay to ADT, delay to other adjuvant therapies, and improved progression-free survival. While the literature on metastasectomy for visceral PCa metastasis is scarce, MDT with SABR has demonstrated promising results in two recent prospective trials.4,5 The Observation vs Stereotactic Ablative Radiation for Oligometastatic Prostate Cancer (ORIOLE) trial demonstrated improved 6-month and median progression-free survival with SABR compared to observation in men with hormone-sensitive oligometastatic PCa.4 In the Surveillance or Metastasis-Directed Therapy for Oligometastatic Prostate Cancer Recurrence (STOMP) trial, where the MDT arm allowed salvage surgery or SABR, the median ADT-free survival was significantly improved with MDT compared to surveillance.5 To our knowledge, this is the first report of a durable biochemical response following adrenal metastasectomy in oligometastatic castrate-resistant PCa. This CASE demonstrates that although technically challenging, robotic-assisted adrenal metastasectomy is feasible in experienced hands with good perioperative surgical outcomes. At 5 years follow-up, PSA levels remained undetectable, and there was no evidence of biochemical or radiological progression. Surgical resection of oligometastatic lesions should be limited to well-selected patients, and discussed in a multidisciplinary tumor board prior to definitive management.
Conclusion: While adrenal metastases from PCa are extremely rare, robotic-assisted adrenal metastasectomy is feasible. This case demonstrates that metastasectomy may provide a durable biochemical response, and improve progression-free survival in men with oligometastatic PCa.
Declaration of competing interest
None.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics. Ca - Cancer J Clin. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 2.Gandaglia G., Abdollah F., Schiffmann J. Distribution of metastatic sites in patients with prostate cancer: a population-based analysis. Prostate. 2013;74:210–216. doi: 10.1002/pros.22742. [DOI] [PubMed] [Google Scholar]
- 3.Long M.A., Husband J.E. Features of unusual metastases from prostate cancer. Br J Radiol. 1999;72:933–941. doi: 10.1259/bjr.72.862.10673942. [DOI] [PubMed] [Google Scholar]
- 4.Phillips R., Shi W.Y., Deek M. Outcomes of observation vs stereotactic ablative radiation for oligometastatic prostate cancer: the ORIOLE phase 2 randomized clinical trial. JAMA Oncol. 2020 doi: 10.1001/jamaoncol.2020.0147. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ost P., Reynders D., Decaestecker K. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter phase II trial. J Clin Oncol. 2018;36:446–453. doi: 10.1200/JCO.2017.75.4853. [DOI] [PubMed] [Google Scholar]