Abstract
A rare case of methamphetamine induced testicular ischemia, a 35-year-old man with clinical and sonographic features of left epididymitis. However, Ultrasound incidentally showed a lack of vascularity of the right testicle despite being asymptomatic on the right hemi-scrotum. He was a known intravenous methamphetamine user, admitting his last injection was 4 h prior to his presentation.
The left epididymitis was treated with antibiotics, analgesia and scrotal support, while right testicle was treated conservatively with serial ultrasounds. Repeat ultrasound in 20 h confirmed the return of normal vascularity of the right testicle confirming methamphetamine induced testicular ischemia, no surgical intervention needed.
Keywords: Testicular ischemia, Epididymitis, Methamphetamine, Vasoconstriction
Introduction
Methamphetamine is a central nervous system stimulant affecting the brain by increasing the release and blocking the reuptake of dopamine, a neurotransmitter responsible for the motivation and pleasure centers of the brain1, the brain reaches an intense euphoric or grandeur feeling thus giving it high potential for abuse.
Dopamine also causes an increased heart rate and is known to cause vasoconstriction in other areas of the body1 this is the result of stimulation of the α-adrenergic and β-adrenergic receptors by methamphetamine resulting in vasospasm or vasoconstriction and ultimately producing dramatically lowered arterial perfusion and ischemia.2 These mechanisms are cited as instrumental in the development of methamphetamine related deaths due to ischaemic strokes, mesenteric ischemia and acute myocardial infarction.3
Case presentation
A fit and well 35-year-old male who works as FIFO (fly-in, fly-out) employee in one of the remote mining sites, presenting with sudden onset of left scrotal pain. He has no history of lower urinary tract symptoms and no recent urinary or sexually transmitted diseases. He admitted to regular methamphetamine use during his off weeks, including the use of intravenous methamphetamine injection into his right upper limb only approximately of 4 h prior to his presentation.
On examination initially, his observations showed a tachycardia of 110 and a low-grade fever of 37.7. Blood pressure and respiratory markers were within normal range. Scrotal examination showed bilateral scrotal swelling (right more than left) and erythema along with left testicular tenderness. No pain or tenderness over the right testicle. Urine dipstick was positive for leucocytes. Clinically a diagnosis of left epididymo-orchitis was given.
Blood tests showed haemoglobin of 142 g/L, white cell count of 18.74 and normal renal and liver functions initially, then the white cell count normalised upon discharge. No amphetamine level was done as thought it will not change the management.
With his significant tachycardia an ultrasound of the scrotum was arranged to exclude testicular abscess, although it was felt most likely the tachycardia was secondary to his methamphetamine use.
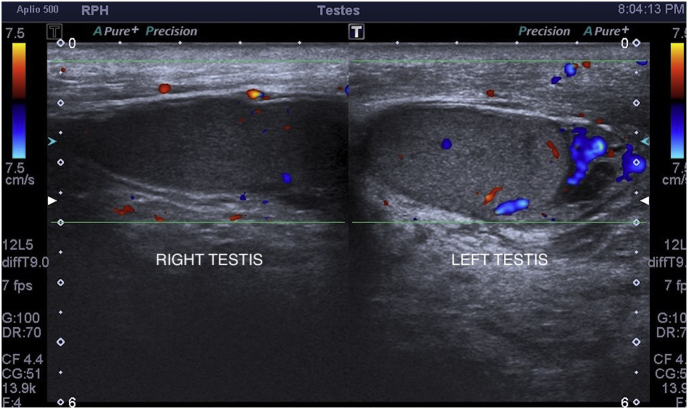
Ultrasound confirmed the diagnosis of left epididymitis with no abscess [Fig. 1]. But interestingly showed mildly asymmetrically large and hypoechoic right testicle, without vascularity [Fig. 2].
Fig. 1.
First scrotal ultrasound at the time of presentation confirmed increased vascularity of the left epididymis and lacking vascularity of the right testicle.
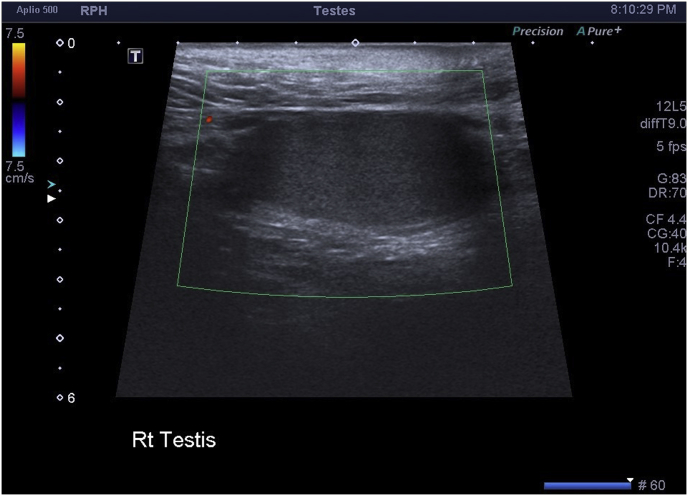
Fig. 2.
Right hemiscrotal ultrasound at the time of presentation demonstrating the lack of right testicular vascularity.
In view of pathology on the contralateral side the patient was re-assessed for history and examination, to ensure no mistake for side was made. He continued to deny any pain or symptoms on the right and clinically examination showed again left swelling erythema and tenderness.
It was decided no scrotal exploration to be done immediately and to be treated with wait and watch with repeating ultrasound with 24 hours as he was asymptomatic over the right side. However, the acute left epididymo-orchitis was treated with 14 days of oral ciprofloxacin and simple analgesia.
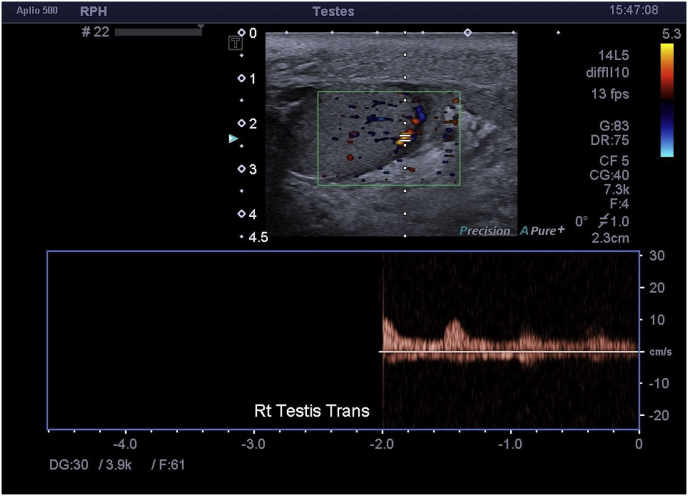
Repeat scrotal ultrasound 20 h later, showed returned vascularity of the right testicle [Fig. 3] along with the same known left epididymitis.
Fig. 3.
Ultrasound doppler image demonstrating the normal arterial trace in the right testicle 20 h post prior ultrasound with avascular right testicle.
He was discharged 72 hours later with strong recommendation against continued methamphetamine use. Examination at 5 weeks post discharge showed normal clinical examination and complete resolution of the pain, swelling and tenderness. No repeat ultrasound was needed.
Discussion
Methamphetamine induced testicular ischemia is rare with only a few case reports in the literature. In other reported cases, scrotal exploration was performed to exclude a diagnosis of testicular torsion.4
In these cases, there is a clearly documented use of intravenous methamphetamine prior to the onset of testicular pain and presentation to an emergency department, without any evidence of torsion and with the exclusion of other potential differential diagnoses. Whilst the exact mechanism of methamphetamine induced ischemia is uncertain, ischemia in other organs post methamphetamine use is well documented, especially in its effects on cerebral, cardiac and intestinal ischemia.
Our case allowed us the opportunity of conservative management as this was an incidental finding of asymptomatic testicular ischemia in the contralateral testes, alongside an acute case of epipdiymo-orchitis.
It is generally believed that the testis suffers irreversible damage after 8 h of ischemia,5 therefore scrotal exploration is the mainstay of management of suspected torsion and ischemia to restore blood flow. However, ischemia secondary to methamphetamine use is unlikely to improve with surgical exploration and only increases the surgical and anaesthetic risks to the patient. Prevalence of methamphetamine use has doubled in Australia over the last ten years, therefore good history and clinical suspicions are vital to enable correct diagnosis and prevent unnecessary surgical procedures.
Consent
Consent been obtained from the patient directly including his signature on the consent form, consenting for publishing the case presentation.
Declaration
All data are available electronically within Royal Perth Hospital medical records and subject to confidentiality upon requesting. The datasets generated and/or analysed during the current study are not publicly available due confidentiality but are available from the corresponding author on reasonable request.
I, Mohammed Al-Zubaidi and all authors have not received a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. There is no conflict of interests among authors.
Authors contributed in finalising the case in the following shares, Mohammed Al-Zubaidi had the major contribution in collecting date, consenting the patient, writing the case and preparing it to be published. Andrew Stuart contributed in writing the abstract, Thilina Jayaratne contributed in supplying a de-identified ultrasound images. Emma Marsdin is the supervisor.
References
- 1.National Institute on Drug Abuse http://www.drugabuse.gov/publications/infofacts/methamphetamine
- 2.Lappin M., Darke S., Farrell M. Stroke and Methamphetamine use in young adults: a review. J Neurol Neurosurg Psychiatry. 2017;88:1079–1091. doi: 10.1136/jnnp-2017-316071. [DOI] [PubMed] [Google Scholar]
- 3.Butany J., Ahn E., Luk A. Drug-related cardiac pathology. J Clin Pathol. 2009;62:1074–1084. doi: 10.1136/jcp.2008.058255. [DOI] [PubMed] [Google Scholar]
- 4.Michael H., Doherty B.S., Eugenio O., Gerscovich M.D., Michael T. Corwin MD Stephen R. Wilkendorf RDMS. Methamphetamine use can mimic testicular torsion. 2013 Sep;41(7):461–463. doi: 10.1002/jcu.22049. [DOI] [PubMed] [Google Scholar]
- 5.Dunne P.J., O'Loughlin B.S. Testicular torsion: time is the enemy. Aust N Z J Surg. 2000;70:441. doi: 10.1046/j.1440-1622.2000.01853.x. [DOI] [PubMed] [Google Scholar]